Abstract
Purpose
The Coronavirus Disease 2019 pandemic disrupted healthcare, but the impact on vaccination missed opportunities (MOs, vaccine-eligible visits without vaccination) is unknown. We evaluated pandemic-related trends in MOs at adolescent well-care visits for three vaccines: human papillomavirus; quadrivalent meningococcal conjugate; and tetanus, diphtheria, and acellular pertussis (Tdap).
Methods
We analyzed electronic health record data from 24 pediatric primary care practices in 13 states from 1/1/2018 to 12/31/2021. Segmented logistic regression estimated risk differences for MOs during the pandemic relative to prepandemic trends.
Results
Among 106,605 well-care visits, we observed decreases in MOs prepandemic followed by an increase in MOs during the pandemic for all three vaccines. Relative to prepandemic, MOs increased for human papillomavirus (+15.9%, 95% confidence interval [CI]: 11.7%, 20.1%), meningococcal conjugate (+9.4%, 95% CI: 5.2%, 13.7%), and tetanus, diphtheria, and acellular pertussis (Tdap) (+ 8.2%, 95% CI: 4.3%, 12.1%).
Discussion
Increases in vaccine MOs during the pandemic equaled or exceeded pre-pandemic decreases. Reducing MOs in adolescent well-care could raise vaccine coverage.
Keywords: Pediatric research in office settings (PROS), Vaccination, COVID-19 pandemic, Missed opportunities
Implications and Contribution.
Using electronic health record (EHR) data, this study demonstrated a significantly increasing trend of missed opportunities for three recommended adolescent immunizations during the Coronavirus Disease 2019 (COVID-19) pandemic through December 2021. These findings highlight the urgent need to reduce vaccine missed opportunities in adolescent well-care to mitigate long-term gaps in vaccine coverage.
The COVID-19 pandemic disrupted healthcare delivery, causing many children to fall behind on routine immunizations [1]. This disruption is particularly concerning for adolescents as they seek healthcare less frequently than younger children and may take longer to catch up on missed vaccinations [2,3]. To avoid vaccine delay, clinicians can capitalize on all adolescent healthcare visit opportunities for vaccination. However, the impact of the pandemic on vaccination missed opportunities (MOs), office visits when vaccine-eligible patients do not receive a recommended vaccine, is unknown [4]. The pandemic might reduce MOs if practices pay particular attention to vaccinations during this period of fewer visits. Conversely, the pandemic might increase MOs due to disruptions in practice staffing and workflows. Rising parental vaccine hesitancy might also increase MOs. In this secondary data analysis, we examined MOs at adolescent well-care visits, which are the visits where vaccines are most commonly administered [2]. We aimed to describe how MOs changed over time in relation to the pandemic for three recommended vaccines: human papillomavirus (HPV, frequently associated with parental hesitancy), as well as quadrivalent meningococcal conjugate (MenACWY), and tetanus, diphtheria, and acellular pertussis (Tdap), none of which is commonly associated with parental hesitancy [5,6].
Methods
Using an observational longitudinal design [7], we analyzed EHR data from 24 pediatric primary care practices collected as part of a randomized controlled trial [8]. This study was approved or exempted by institutional review boards at the American Academy of Pediatrics, University of California, Los Angeles, Children's Hospital of Philadelphia, and University of Pennsylvania. A waiver of informed consent was granted for patients/families.
For this analysis, we used data from the 24 control group practices that received no intervention as part of a cluster randomized trial. Sites were located across 13 US states and included 16 independent practices and eight practices belonging to one of two large health systems (Austin Regional Clinic and Children's Minnesota). We analyzed visits with patients 11 through 17 years of age who were eligible for HPV (any dose), MenACWY (either dose), or Tdap vaccines according to the Advisory Committee on Immunization Practices [9]. We evaluated only in-person (nontelehealth) well-care visits to capture visits where vaccines are typically given [2] and because vaccine administration was very rare at other visit types both before and during the pandemic. We divided the data into two periods: 1/1/2018 to 2/29/2020 (prepandemic) and 6/1/2020 to 12/31/2021 (pandemic). We excluded data early in the pandemic (3/1/2020-5/31/2020) due to extremely low visit volumes with widespread shutdowns.
We used Stata version 16 to conduct segmented, or piecewise, logistic regression to evaluate changes in MOs (outcome) levels and trajectories between the prepandemic and pandemic periods. To account for the cluster-randomized design in estimating variance, we used the survey package with practice site as the primary sampling unit, an approach equivalent to generalized estimating equations with clustering by practice and independence working correlation. We included as covariates a pandemic indicator (pre-pandemic/pandemic), vaccine due as a categorical variable (HPV, Tdap, or MenACYW), time in months as a continuous variable and all their two- and three-way interactions. We also included calendar month as a categorical covariate to adjust for seasonal variation in MO rates [10]. From the model, we estimated expected values of missed opportunity rates by predictive margins, a method that standardizes estimates to adjust for covariates. Using Stata's “margins” command, we estimated predicted proportions (risks) of MOs at the beginning and end of each time period. We then calculated risk differences to estimate changes in predicted risk across each period for each vaccine and pandemic period. We considered a change over time, and differences in those changes, to be statistically significant if the 95% confidence interval (CI) excluded 0. As a descriptive assessment, we additionally calculated the proportion of practices with improving/worsening MOs across each time period.
Results
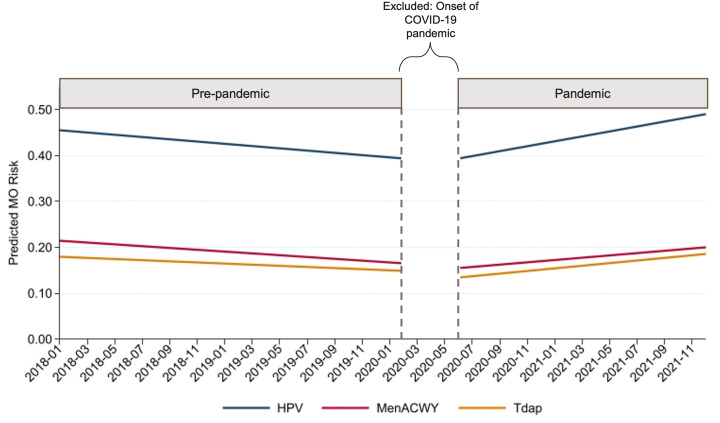
We analyzed 106,605 well-care visits (59,955 prepandemic and 46,650 pandemic). HPV, MenACWY, and Tdap vaccines were due at 86,546; 63,155; and 31,449 visits, respectively. For all three vaccines, we observed changes in trend, with MOs decreasing during the prepandemic period and increasing during the pandemic period (see Figure). Relative to the pre-pandemic period, MO risk increased significantly for HPV (any dose; +15.9%, 95% CI: 11.7%–20.1%), MenACWY (either dose; +9.4%, 95% CI: 5.2%–13.7%), and Tdap (+8.2%, 95% CI: 4.3%–12.1%) during the pandemic period (Table , Figure ). This pandemic-related increase was larger for HPV compared to MenACWY by 6.5% points (95% CI: 2.8%–10.3%) and larger for HPV than for Tdap by 7.7% points (95% CI: 3.1%–12.3%).
Figure.
Proportion of adolescent vaccine missed opportunitiesa at well-care visits by month. MO = missed opportunity; HPV = human papillomavirus vaccine; MenACWY = quadrivalent meningococcal conjugate vaccine; Tdap = tetanus, diphtheria, and acellular pertussis vaccine. a Missed opportunities are defined as office visits when vaccine-eligible patients do not receive a recommended vaccine. Data between dashed lines (March-May 2020) were excluded due to unusually low visit volume at the onset of the pandemic.
Table.
Changes in the riska of missed opportunitiesb for vaccination at well-child care visits before and during the Coronavirus Disease 2019 pandemic
| MOs at start of period, %c | MOs at end of period, %d | Change in risk from start to end of period (95% CI), % points | |
|---|---|---|---|
| HPV | |||
| Prepandemic (Jan. 2018-Feb. 2020) | 45.5 | 39.4 | −6.2 |
| Pandemic (June 2020-Dec. 2021) | 39.3 | 49.1 | 9.8 |
| Pandemic versus prepandemic | 15.9 (11.7–20.1) | ||
| MenACWY | |||
| Prepandemic (Jan. 2018-Feb. 2020) | 21.4 | 16.5 | −4.9 |
| Pandemic (June 2020-Dec. 2021) | 15.5 | 20.0 | 4.4 |
| Pandemic versus pre-pandemic | 9.4 (5.2–13.7) | ||
| Tdap | |||
| Prepandemic (Jan. 2018-Feb. 2020) | 18.0 | 14.9 | −3.1 |
| Pandemic (June 2020-Dec. 2021) | 13.4 | 18.6 | 5.2 |
| Pandemic versus pre-pandemic | 8.2 (4.3–12.1) |
CI = confidence interval; HPV = human papillomavirus vaccine; MenACWY = quadrivalent meningococcal conjugate vaccine; MO = missed opportunity; Tdap = tetanus, diphtheria, and acellular pertussis vaccine.
Estimated using logistic regression, standardized for calendar month to account for seasonality.
An office visit was considered a missed opportunity if an eligible vaccine was not administered. We evaluated only in-person (nontelemedicine) well-care visits during which vaccines are most commonly administered.
Monthly MO rate at the start of each period: January 2018 for the prepandemic period and June 2020 for the pandemic period. Estimated using logistic regression.
Monthly MO rate at the end of each period: February 2020 for the prepandemic period and December 2021 for the pandemic period. Estimated using logistic regression.
Among the 24 practices in the study, 67%, 54%, and 58% of practices experienced decreasing MOs during the pre-pandemic period for HPV, MenACWY, and Tdap vaccines, respectively; 83%, 79%, and 63% experienced increases during the pandemic period.
Discussion
From the summer of 2020 to the end of 2021, rates of MOs increased for all three recommended adolescent vaccines compared to prepandemic trends. Increases in MOs during the pandemic equaled or exceeded the decrease in MOs seen prior to the pandemic. Possible explanations include disruptions in staffing and workflow (including medical assistant and nursing shortages) [11,12] or increased parental vaccine hesitancy during the COVID-19 pandemic [13]. These increasing rates in MOs could result in long-term gaps in vaccine coverage [14].
One limitation is that while we included EHR data and a nationally diverse sample of independent primary care practices plus practices belonging to health systems, practices volunteered for the STOP-HPV trial and therefore might not be nationally representative. Additionally, this study did not include a direct assessment of reasons for MOs and did not have reliable information on COVID-19 vaccination to determine how that may have affected our results.
Our findings highlight another impact of the pandemic and the urgent need to reduce vaccine MOs during adolescent well-child care visits. Future research should investigate reasons for reductions in MOs prior to the pandemic and reasons for pandemic-related MO increases. Further exploration of methods to optimize vaccine delivery such as delivery of vaccines in school settings or vaccinating at nonpreventive visits will also be crucial as the pandemic evolves.
Footnotes
Conflicts of interest: Dr. Stephens-Shields served as an expert witness contracted by a law firm on behalf of Gilead Sciences, though this work is unrelated to vaccination. The other authors have no conflicts of interest to disclose.
Disclaimer: The sponsor did not participate in the study design, the collection, analysis, and interpretation of data, the writing of the report, or the decision to submit the manuscript for publication.
Funding Sources
National Cancer Institute of the National Institutes of Health under Award Number R01CA202261. Additional infrastructure funding was provided by the American Academy of Pediatrics and the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) under UA6MC15585 - National Research Network to Improve Children's Health and U5DMC39344 - Pediatric Research Network Program. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA/HHS, or the US Government.
References
- 1.DeSilva M.B., Haapala J., Vazquez-Benitez G., et al. Association of the COVID-19 pandemic with routine childhood vaccination rates and proportion up to date with vaccinations across 8 US health systems in the vaccine safety datalink. JAMA Pediatr. 2022;176:68. doi: 10.1001/jamapediatrics.2021.4251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rand C.M., Goldstein N.P.N. Patterns of primary care physician visits for US adolescents in 2014: Implications for vaccination. Acad Pediatr. 2018;18:S72–S78. doi: 10.1016/j.acap.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 3.Uddin S.G., O’Connor K.S., Ashman J.J. Physician office visits by children for well and problem-focused care: United States, 2012. NCHS Data Brief. 2016;248:1–8. [PubMed] [Google Scholar]
- 4.Williams C.L., Walker T.Y., Elam-Evans L.D., et al. Factors associated with not receiving HPV vaccine among adolescents by metropolitan statistical area status, United States, National Immunization Survey-Teen, 2016-2017. Hum Vaccin Immunother. 2020;16:562–572. doi: 10.1080/21645515.2019.1670036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Szilagyi P.G., Albertin C.S., Gurfinkel D., et al. Prevalence and characteristics of HPV vaccine hesitancy among parents of adolescents across the US. Vaccine. 2020;38:6027–6037. doi: 10.1016/j.vaccine.2020.06.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pingali C., Yankey D., Elam-Evans L.D., et al. National vaccination coverage among adolescents aged 13–17 Years — national immunization survey-Teen, United States, 2021. MMWR Morb Mortal Wkly Rep. 2022;71:1101–1108. doi: 10.15585/mmwr.mm7135a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fitzmaurice G.M., Laird N.M., Ware J.H., editors. Applied longitudinal analysis. 2nd ed. Wiley; Hoboken: 2011. [Google Scholar]
- 8.Szilagyi P.G., Humiston S.G., Stephens-Shields A.J., et al. Effect of training pediatric clinicians in human papillomavirus communication strategies on human papillomavirus vaccination rates: A cluster randomized clinical trial. JAMA Pediatr. 2021;175:901–910. doi: 10.1001/jamapediatrics.2021.0766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Child and adolescent imunization schedule. Centers for disease control and prevention. 2022. https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html#birth-15 Available at:
- 10.Moss J.L., Reiter P.L., Rimer B.K., et al. Summer Peaks in Uptake of human papillomavirus and other adolescent vaccines in the United States. Cancer Epidemiol Biomark Prev. 2016;25:274–281. doi: 10.1158/1055-9965.EPI-15-0574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization COVID-19 continues to disrupt essential health services in 90% of countries. 2021. https://www.who.int/news/item/23-04-2021-covid-19-continues-to-disrupt-essential-health-services-in-90-of-countries Available at:
- 12.Harrop Chris. Medical assistants remain elusive for practices navigating a staffing crisis. MGMA. 2022. https://www.mgma.com/data/data-stories/medical-assistants-remain-elusive-for-practices-na Available at:
- 13.He K., Mack W.J., Neely M., et al. Parental Perspectives on immunizations: Impact of the COVID-19 pandemic on childhood vaccine hesitancy. J Community Health. 2022;47:39–52. doi: 10.1007/s10900-021-01017-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saxena K., Marden J.R., Carias C., et al. Impact of the COVID-19 pandemic on adolescent vaccinations: Projected time to reverse deficits in routine adolescent vaccination in the United States. Curr Med Res Opin. 2021;37:2077–2087. doi: 10.1080/03007995.2021.1981842. [DOI] [PubMed] [Google Scholar]