Abstract
Integration of Ayurveda into our current health care research programs is critical to making progress in global wellness and in disease prevention and control, especially for cancer. Ayurveda promotes restoration of the innate healing mechanisms existing in the body for optimal immunity, resilience, and health. Ayurveda also has an abundant resource of botanical products containing diverse pharmaco-active ingredients and millennia of experience of clinical applications for health benefits. But there is a lack of evidence–based research to demonstrate its efficacy and potential. This 2-part review is written from the perspective of a western-trained biomedical scientist and student of Ayurveda. It aims to educate research scientist peers about the opportunities and challenges for scientific validation of Ayurvedic herbal compounds, protocols, and modalities and inspire more research in this area. Part 1 will review several aspects of Ayurveda including principles of body constitution (Prakriti), digestion (Agni and Ama) and mind-body health, in relation to cancer. Part 2 [1] will focus on Ayurvedic botanical resources used for cancer and research studies will be discussed on selected herbal compounds. Research gaps and opportunities will be identified to guide development of research programs to validate safety and efficacy of these therapies. Importantly, the use of Ayurvedic modalities is not intended to substitute for allopathic treatments for cancer but as an integrative component for prevention and restoration of strength and immunity post treatment.
Keywords: Ayurveda, Cancer, Prakriti. Agni, Ama
1. Introduction
This review introduces Ayurveda, the traditional medical system of India, which offers a unifying perspective to health with unique paradigms, theories, and protocols to contribute to cancer prevention and post therapy rehabilitation/rejuvenation. It has been over 50 years since the U.S. National Cancer Act of 1971 was enacted to support research into mechanisms and treatments for cancer. Researchers continue to look for unifying concepts to understand the development of cancer. Over the last decades, hundreds of genes, proteins, epigenetic factors, and metabolic pathways have been discovered to be involved in cancer progression. Increasingly complex regulatory factors have been found within the tissue microenvironment, the immune system, and the microbiome. This review will outline perspectives from Ayurveda of additional ecological factors that influence health and disease such as our physiological phenotypes, nutrition, diet and lifestyle, and physical and mental stress. Part 1 of this review covers several aspects of Ayurveda including principles of body constitution (Prakriti), digestion (Agni and Ama) and mind-body health, in relation to cancer. Part 2 [1] will focus on Ayurvedic botanical resources used for cancer and research studies will be discussed on selected herbal compounds. This work begins to explore some basic Ayurvedic concepts and potential integration into heath care research programs.
Ayurveda is a comprehensive integrative healing system more than 5000 years old. “Ayurveda” by definition, is the science of life; Ayus meaning life and Veda meaning knowledge. The three main Ancient texts include the Charaka Samhita, the prime work with basic principles of Ayurveda and internal medicine [2] the Sushruta Samhitas, dealing with surgery and medical concepts [3], and the Ashtanga Hridaya, a more concise and poetic summary of the first 2 texts [4]. The highly detailed texts include recommendations for healthy diets, daily and seasonal routines, and extensive descriptions of over four hundred herbs and thousands of herbal formulations for specifice health conditions. Ayurveda offers a holistic, personalized medicine approach that considers an individual's body type, strength of digestion, immunity, and mental health. The concepts of physiology found in the ancient Ayurvedic texts are remarkably compatible with the modern allopathic understanding of physiology. The texts provide an understanding of normal physiology and pathology with unique perspectives on early stages of disease applicable to early detection strategies. They provide relatively simple, low-tech guidelines to restore and maintain the ecological balance of our bodies and interactions in our physical, social, and natural environments.
Ayurveda has a large resource of herbal medicines and formulations, the chemical constituents of which may target numerous biochemical and cellular pathways. These aim to balance the physiology and support immunity. The practice of Ayurveda also includes the criteria determining when to use these herbs and how to combine with diet, behavior, detoxification, and mind/body techniques to restore health and prevent disease.
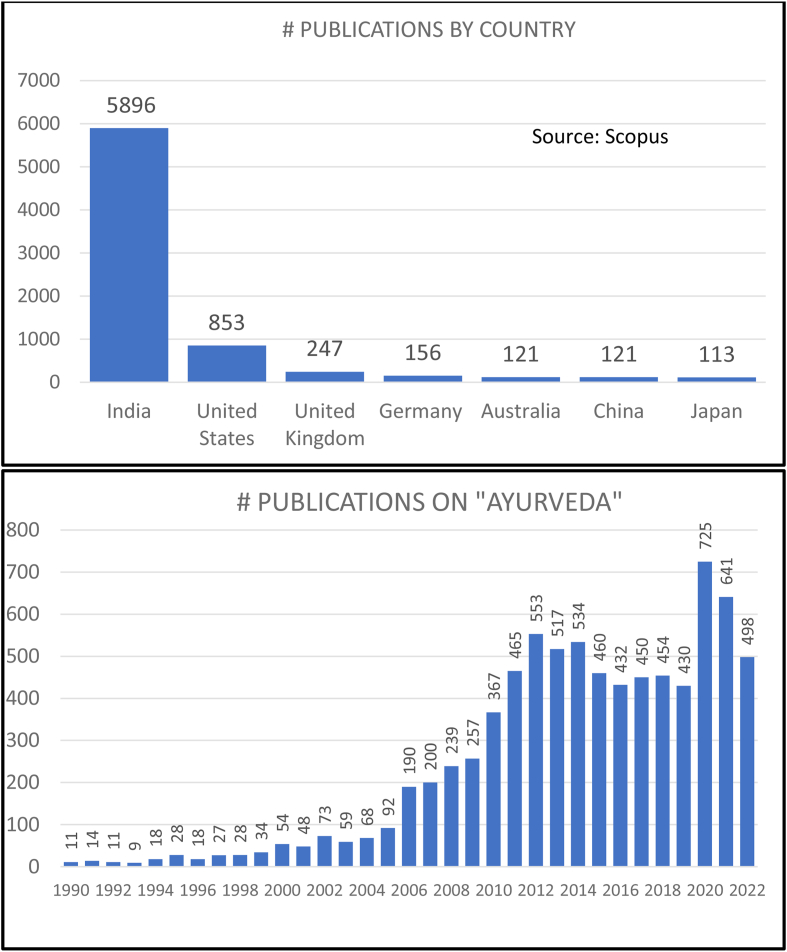
Research studies in Ayurveda in Scopus shows a peak in 2020 with most of the authors from India (See Fig. 1). Much of the research in Ayurveda has reflected the current reductionist experimental paradigm to define mechanisms of isolated chemical components from single herbs such as curcumin or ashwagandha for drug discovery. Yet most diseases, including cancer, have multi-factorial causation and multiple molecular targets. Traditional Ayurvedic herbal preparations combine multiple herbs each with many potentially synergistic chemical compounds and have centuries of clinical application. These complex formulations for complex diseases may possess inherent value. How they have been used in populations over millennia may provide clues to their possible mechanisms and applications, to the discovery of new biomarkers of health and for unique perspectives for prevention and treatments for early and late stages of disease. Research studies on the clinical use of Ayurvedic herbs and protocols are still lacking.
Fig. 1.
Publications on Ayurveda. A search in the Scopus reference data base for the text “Ayurveda” in the title, abstract or key words, produced >7500 documents between 1990 and 2022. They are shown as number of documents per year. Trends of research publications in Ayurveda show a peak in 2020 with most of the authors from India.
Compared to allopathic medicine which is largely disease-focused, and where health is defined mostly as the absence of disease, Ayurveda is person-focused, where health is defined as the optimal functioning of the psycho-physiological systems of the body, the tissues, strength of digestion, the proper elimination of wastes, and immunity. Imbalances between these elements can lead to dysfunction, inflammation, and progression of disease. This review aims to encourage research into mechanisms and safety of Ayurvedic herbs and efficacy of protocols to be integrated into cancer care and prevention.
This paper will briefly introduce several principles and concepts of Ayurveda which may be new to some readers, and somewhat abstract. For a more thorough discussion and deeper understanding of these concepts, a few references are mentioned here. Several comprehensive reviews of the principles of Ayurveda are found here [[5], [6], [7]] and for scientific decoding of some of the core concepts of Ayurveda, see Ref. [8]. Also of interest may be a contemporary review of the perspective of cancer found in the traditional texts of Ayurveda, the Charaka and Sushruta Samhitas, including classification, pathogenesis and traditional treatments [[9], [10], [11]].
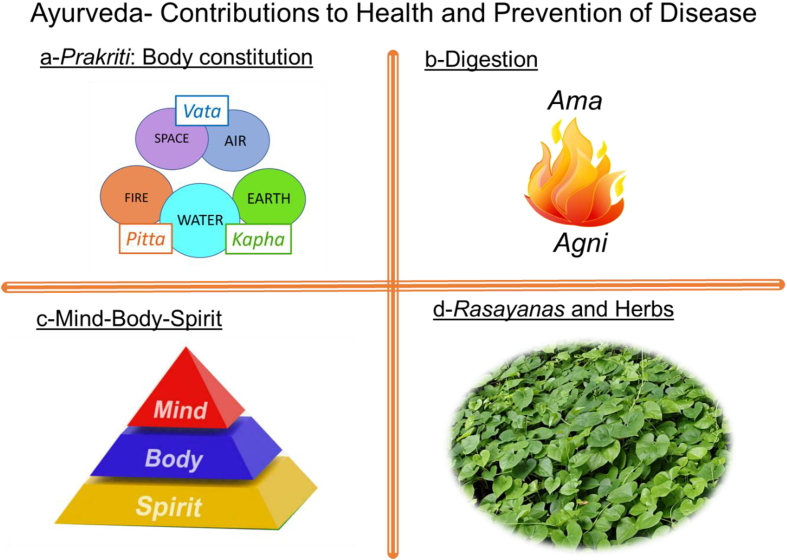
Most of the public perception of Ayurveda and most of the research to date relates to the Ayurvedic herbs or rasayanas (traditional combinations of herbs that support strength, immunity, and longevity). This will be discussed in Part 2 of this review. Beyond the herbs, there is a vast knowledge in the original Ayurvedic texts that contain comprehensive guidelines and protocols for health promotion including addressing body constitution (“Prakriti”), optimizing digestion, and the mind/body/spirit connection (See Fig. 2). These three concepts will be discussed here in Part 1 along with the status of evidence-based validation of these Ayurveda modalities. The discussion section within Part 2 will conclude with research challenges and directions for developing research agendas.
Fig. 2.
Ayurveda- Contributions to Health and Prevention of Disease. This review is divided into 2 parts containing 4 main aspects of Ayurveda that contribute to health and prevention of disease and are discussed in relationship to cancer etiology. Part 1 will cover sections A, B and C. A) Prakriti or body constitution is represented by Vata, Pitta and Kapha expressing the qualities of the basic elements of nature, Space, Air, Fire, Water and Earth. B) Digestion is a critical component of health and depends on strong Agni – or digestive fire. When Agni is insufficient, then Ama, a metabolic toxin accumulates in the tissues resulting in seeds of disease. C) The state and balance of Mind, Body, and Spirit will be discussed as a fundamental component to health. Part 2 of this review is a companion document in this issue and will address D) Rasayanas and herbs in Ayurveda (representative picture of Guduchi, (Tinospora cordifolia), as well as research questions and directions, gaps, and opportunities.
1.1. Role of body constitution/Prakriti in health and disease
A concept pivotal to the Ayurvedic philosophy and science is that different people have different body types or constitutions which contribute to the heterogeneity in disease predisposition, responses to environment, drug effects or resistance. It is understood that in clinical trials men may respond to treatments differently than women; also, children respond differently than adults. Ayurveda would incorporate another distinction for populations considering the constitution of the body called “Prakriti” [12]. This theory considers the human physiology in relation to the five subtle elements: space, air, fire, water, and earth, termed Panchamahabhuta. These 5 elements correspond to the 5 senses, hearing, touch, sight, taste, and smell, respectively. Ayurveda proposes that in biological systems, including humans, these elements are coded into three forces, which govern all life processes and are expressed in the physiology as the Doshas: Vata (V), Pitta (P) and Kapha (K) (See Fig. 2A). Each dosha has five subdoshas that relate their functions within the body's organ systems [13]. The tenets of this “Tridosha theory” is that these three physical and psychological control systems mutually coordinate to perform the normal function of the body [14].
1.1.1. Vata, Pitta and Kapha doshas
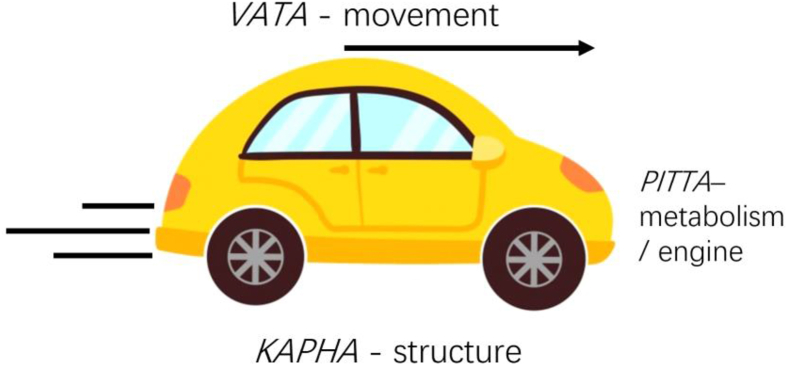
Vata dosha incorporates the elements of air and space and regulates movement, intelligence, direction, and purpose in the body. Physiologically this would include breathing, speaking, blood flow, heart, the nervous system, movement of food through the digestive tract, or communication between cells and nerves. Pitta dosha includes the water and fire elements and contributes to the transformational/metabolic mechanisms of the body, including digestion, appetite, enzymatic functions, and the blood system that carries oxygen and nutrition throughout the body. Kapha dosha incorporates the earth and water elements and forms the structure, strength and lubrication of the body and found in the bones, joints, muscles, and secretory functions. An analogy for how these three processes coordinate is seen in Fig. 3 in the functioning of a car. The Kapha elements of earth and water, structure, and lubrication, are represented by the body and wheels of the car, Pitta elements of fire and water; transformation and metabolism are represented by the engine and drive train, and Vata elements of space and air, movement and intelligence are represented by the motion and direction of movement. All aspects interact and are necessary for efficient functioning of the car, as they are also important for our physiology.
Fig. 3.
Analogy: Three Doshas as expressed in a car. The three doshas of Prakriti can be understood using an analogy of a car. The Kapha elements of earth and water, structure, and lubrication, are represented by the body and wheels and engine oil of the car, Pitta elements of fire and water; transformation and metabolism are represented by the engine, and drive train, and Vata elements of space and air, movement and intelligence are represented by the motion, control of movement, and the intelligence from the driver and dashboard GPS. All aspects interact and are necessary for efficient functioning of the car, like how these 3 doshas interact and support our physiology and psychology.
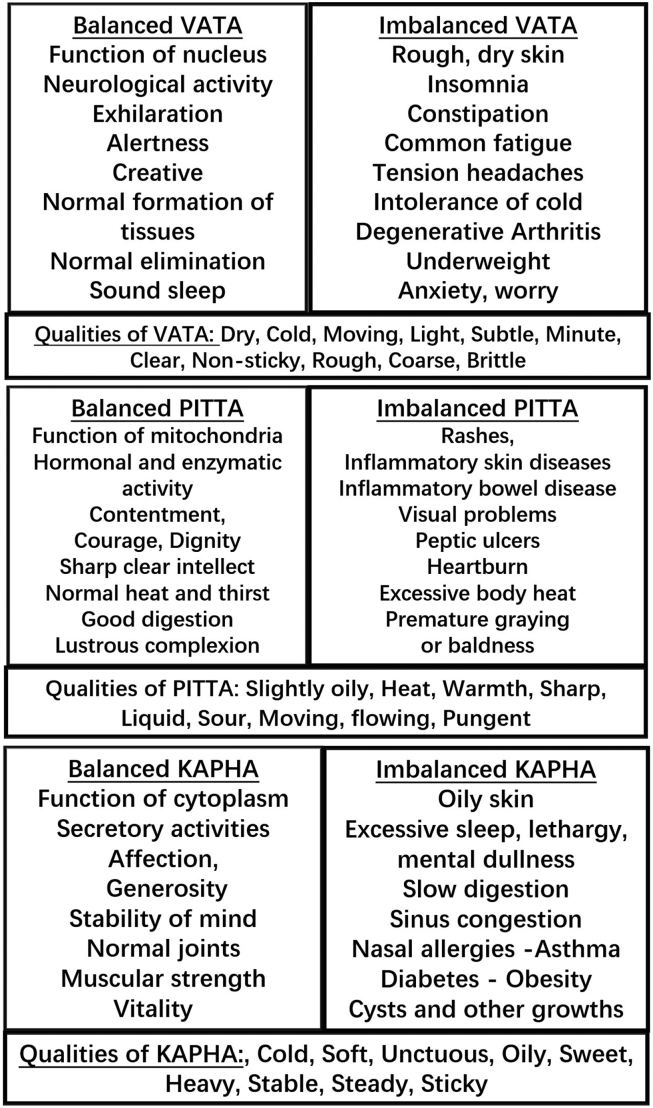
Each person has their own unique Prakriti in which the doshas predominate in their physiology as either a single dosha – V, P, or K, or combinations of any of the doshas - VP, PK, VK, and VPK. An individual's Prakriti can determine how they respond to the external environment including susceptibility to diseases or responses to drugs [15]. When the doshas are in balance, each body type has unique positive tendencies and health attributes, and when the doshas are out of balance these persons have equally unique vulnerabilities (See Fig. 4). The aim of Ayurveda is to maintain balance between these doshas as well as within the seven tissues (dhatus) and the three channels for waste products (malas) ([5]; pages 87–90). Imbalances between these elements can lead to decreased vitality and immunity and to inflammation and disease.
Fig. 4.
Qualities and expression of Vata Pitta and Kapha. Ayurveda proposes that in biological systems, including humans, there are three operators which govern all life processes and are expressed in the physiology as the Doshas: Vata, Pitta and Kapha. They coordinate functioning both in our bodies and in the whole of nature. The qualities of Air and Space are listed as Vata, qualities of Fire and Water are listed as Pitta, the qualities of Earth and Water are listed as Kapha. Characteristics of Vata Pitta and Kapha are listed for how they express in the physiology when they are in balance, and when out of balance.
1.1.2. Assessment of Prakriti
Traditionally Prakriti is assessed subjectively by an Ayurvedic physician, usually by observation, interrogation, and analysis of the pulse. Both Ayurveda and Traditional Chinese Medicine include diagnoses and treatments based on psycho-physiological characteristics of individuals. The determinants of Prakriti are well described and elaborated in Rotti, 2014 [16] and include an extensive list of parameters such as morphological features, tactile features, subjective physical findings, routine and lifestyle, and intellectual and emotional attributes. This team also developed a computer-aided tool, AyuSoft, to evaluate these parameters to determine the Prakriti of 3416 subjects in three centers in south India. When they compared the computer results to assessments by senior Ayurvedic physicians, they found 80% concordance in the results. Another quantitative measure of Tridosha was obtained by using an algorithmic experimental method to include the comprehensive list of qualitative features that are commonly used by Ayurvedic doctors [17].
1.1.3. Research in Prakriti
Research studies in Prakriti have established that there are genetic and epigenetic correlates for the three body types [18,19]. One of the earliest papers from 2005 hypothesized a link between genetics and Prakriti. They evaluated 76 subjects both for their Prakriti and human leucocyte antigen (HLA) DRB1 types and found distinct HLA alleles within the different K, P, or V types supporting the idea of the association between HLA alleles and individual Prakriti types [20]. Collaborations in this field of “Ayurgenomics” have quantitated differences in gene expression, SNP variations, epigentics, and immunophenotyping that correlate with Prakriti and distinctions between the V, P, and K body types. One of these reports determined that people with contrasting Prakriti exhibit significant differences genes related to metabolism, transport, immunity, and cell cycle [21].
Another study showed variability of a key oxygen sensor gene, EGLN1, based on Prakriti types which was linked to high altitude adaptation [22]. Biochemical differences were also found in liver function, lipid profiles, and haemoglobin between Prakriti types [23]. Other studies demonstrated genetic differences in populations based on their Prakriti, such as correlations between CYP2C19 genotypes and Prakriti, which was associated with fast and slow metabolism [24]. In another study a significant difference was seen in 52 SNPS between Prakriti types and one gene, PGM1, correlated with phenotype of Pitta [25].
Prakriti is strongly influenced by epigenetic changes due to lifestyle, diet and environmental influences [26]. Epigentic differences were found in DNA methylation analysis of Prakriti-specific multiple CpG sites in promoters and 5′-UTR such as: LHX1 (Vata Prakriti), SOX11 (Pitta Prakriti) and CDH22 (Kapha Prakriti) [27]. Immunophenotyping of whole blood displayed significant differences in the expression of CD14, CD25 and CD56 markers where CD25 and CD56 expression was significantly higher in Kapha Prakriti samples than other Prakriti groups [28]. Finally, in a pilot study on rheumatoid arthritis, genetic susceptibility markers were found using Prakriti-based subgroups. Inflammatory genes IL1β and CD40 correlated as determinants in the Vata subgroup whereas oxidative stress pathway genes were observed in the Pitta (SOD3; rs2536512 and PON1) and Kapha (SOD3 rs2536512) subgroups [29].
Clinical methods of Prakriti evaluation have been summarized and validated through advanced machine learning approaches [12]. A computational system classified 147 healthy individuals into different Prakriti types where phenotype data fell into three distinct clusters, matching the extreme Prakriti groups as classified by clinicians. This study demonstrated that Prakriti types are “distinct verifiable clusters within a multidimensional space of multiple interrelated phenotypic traits.”
Throughout these studies, different research groups approach the determination of Prakriti through different methods. For rigorous research in this area, it is necessary to develop standard tools or protocols to determine the Prakriti. And for reproducibility, it is essential for Prakriti-based researchers to include the full questionnaires, or tools they use for Prakriti assessment within their publications [30]. Ayurveda provides an historical example of personalized medicine and an opportunity for clinicians to stratify physical and behavioral phenotypes and treat patients according to their Prakrit/psychophysiological constitution.
The Ayurveda concept of Prakriti represents an individualized precision medicine approach and may offer discovery of novel biomarkers for complex diseases. The examples above could contribute to the development of predictive and prognostic markers of disease as well as therapeutic responses. Prakriti may also be another variable used to analyze clinical trial results as to which populations are responsive to treatments, and why others may not be responsive. These research opportunities and others are outlined in the discussion section 4.1.
2. Importance of digestion for optimal health
Both the ancient physician Hippocrates and Ayurvedic physicians understood that “All disease begins in the gut”. Therefore, managing digestion and diet are vital to maintaining health. All the building blocks of the physiology, the cells, and tissues, depend on the quality and purity of the food, air, and liquid we take in. Not only what we eat is important but so also how the food is prepared, when we eat, and how well we digest the food. The Ayurvedic perspective is that improper food consumption, routines or behaviors are causative factors that impair the digestion process. Poor digestion promotes toxic buildup of metabolic waste products that promote inflammation and interfere with cellular and immune functioning. Because the Ayurvedic tradition provides a holistic approach it is not unusual to find that a treatment for a cancer may not only directly target the cancer cellular pathways, but it would also support digestion or support elimination of accumulated toxins. An example is the Ayurvedic formula Triphala that promotes efficient digestion, absorption, and elimination. It also has anti-cancer properties, as will be discussed in Part 2 of this review [31].
2.1. Agni and Ama
Two important Ayurvedic principles related to digestion are Agni and Ama. Agni is the transformational ‘fire’ that is responsible for digestive and metabolic processes and provides fuel for mental and physical activity. Classically there are 13 types of Agni; the focus here is on the component “Jatharagni”, the metabolic processes in the digestive system which digests and transforms food into nourishment (rasa) and waste products (mala). The Ayurvedic hypothesis is that when there is balanced Agni, food is completely digested and broken down to the macromolecules of amino acids, sugars, and lipids, etc. Agni may be strong, irregular, or dull, based on the predominant doshas and on diet, behavioral, and environmental causative factors [32]. Ayurveda theorizes that due to these causative factors and others, the Agni becomes weak, and the food is not completely digested, leaving macromolecules and toxins called Ama.
The body has a constant flow of nutrients, oxygen, and waste products. When these processes are blocked and toxic waste products become lodged in the tissues as Ama it creates seeds for diseases [33]. Ama is described as “uncooked food” or incomplete transformation of nutrients, or toxins, such as metabolic toxins or environmental impurities, reactive oxygen species, or unstable metabolic end products [34]. These toxins can become localized outside of the digestive system due to increased intestinal permeability. Ama gets into the circulation and clogs the channels (Srotas) and can be abnormally deposited in the tissues (Dhatus). The immune system recognizes this Ama as a foreign material and initiates an inflammatory response. If Ama is deposited in the joints, it can result in arthritis, or Ama deposited in the arteries leads to atherosclerosis., etc. Incomplete digestion therefore becomes a source of inflammation, an important aspect of early stages of disease. This reference discuses diet and Ama as a precursor to chronic inflammation and the potential role in the progression of cancer [35].
2.2. Inflammation and the role of the gut microbiome
Inflammation is understood to be an important pre-cancerous condition. Chronic inflammation is carcinogenic, as seen in gastritis or inflammatory bowel disease, pancreatitis, reflux esophagitis, asbestosis-induced mesothelioma, etc. [36]. The quality and content of our food plays a major role in inflammatory and immune responses either directly through micronutrients or through conditioning the composition of the gut microbiome. Nearly 30 trillion microorganisms are living in or on each person with 500–1000 different species. The lower gut contains 99% of microorganisms in body. The microbes in the lumen of the gut have profound influences on the immune system at the local level and systemically [37]. When gut bacteria become disruptive, it can cause increased inflammation and increased intestinal permeability and may promote distribution of digested and undigested products as well as immune factors and bacteria throughout body tissues [38]. This progression provides a modern interpretation of the ancient Ayurvedic concept of Ama [39]. The gut microbiome has been implicated in inflammatory bowel diseases (IBD), Crohn's disease and ulcerative colitis [40]. A vibrant research area has evolved related to the role of the gut microbiome in cancer [41,42]. For instance, in melanoma patients treated with anti-PD-1 checkpoint blockade immunotherapy, significant differences were found in the composition of the gut microbiome in patients that responded to the treatment versus those that did not respond [43]. This underlies the importance of digestion and the microbiome in cancer and disease.
2.3. Ayurvedic perspectives for digestion and the gut microbiome
Dietary habits and lifestyle factors have an impact on intestinal permeability and barrier function. There are known detrimental effects of the western high fat and sugar diet, high alcohol intake, stress, and certain medications on gut microbiota [44]. Ayurveda has protocols specifically for diet, digestion, detoxification, and supporting metabolism [45]. Digestive capacity and efficiency can be variable and dependent on Prakriti. A Vata predominant person may have irregular digestion, sometimes strong, or sometimes they have no appetite; a Pitta Prakriti has a good appetite and digestion but has a tendency towards heartburn or if not fed, becomes “hangry”. A Kapha constitution is prone to weaker Agni and has slower digestion and heaviness [46].
The gut microbiome may play a role in the Prakriti-specific digestive capacity. The gut microbiome has been shown to be different in different Prakriti types. A comprehensive analysis demonstrated a correlation of the predominant Prakriti (Vata, Pitta and Kapha) with analysis of human microbiome from the gut, oral and skin samples of healthy individuals. Samples showed Prakriti-specific differences in abundance and types of multiple bacteria species [47]. Another study was carried out in a healthy genetically homogenous western Indian rural population of similar ages and dietary habits and showed gut microbial diversity based on Prakriti [48]. By using 16S rRNA gene based microbial community profiling they found multiple species of the core microbiome to have differential abundance based on Prakriti types with Prakriti-specific enrichment of bacteria. These studies highlight the importance and value of including Prakriti in analysis to explain the variability of the gut microbiome amongst healthy individuals that could have consequences for an individual's health, disease, and treatment.
The taste of food has an essential value in Ayurveda. Six tastes are defined (sweet, sour, salty, bitter, astringent, and pungent) that can aggravate or pacify Vata, Pitta, and Kapha. Ayurveda values the role of spices not just for flavor but also to support digestion and absorption. An analysis of commonly used therapeutic spices in Ayurveda (turmeric, ginger, black pepper, and pippili) found substrates that improved collective metabolism in gut microbiome communities to support efficient digestion [49]. Ginger, black pepper, and pippili are often combined in equal quantities in the common Ayurvedic formulation called Trikatu, which was found to enhance digestion and increase the bioavailability of a number of drugs [50].
2.4. Ayurvedic description of cancer pathogenesis and early detection of diseases
The traditional Ayurvedic texts describe cancers as inflammatory or non-inflammatory swellings called Arbuda (major neoplasm) or Granthi (minor neoplasm). The translation of these terms has been described differently over time with “Arbuda” translated as round, large, muscular, immovable, or swelling ‘tumor’ and Granthi as a benign cystic node or nodule or swelling, or glandular enlargement. For a deeper understanding of the Ayurvedic perspective of cancer see Balachandran 2005 [9].
Ayurvedic texts have embedded theories of the early detection, etiology and pathogenesis of disease, called Samprapti” or progression of disease. It is described as six stages of pathogenesis “Shat Kriya Kala”. [for further explanation see Ref. [10]]. This is a process that can happen over years, and is a progression of aggravation of the doshas weakened by wrong diet or causative factors, and accumulation of Ama and inflammation in the tissues. An important aspect of this theory is that imbalances in the body can be detected in the early stages of disease and Ayurvedic treatments can reverse the disease processs.
This pathogenic process of the interaction of the Tridoshas and how they are involved in cancer development and progression was reported in the context of a summary of interviews with 10 Ayurvedic physicians (Vaidyas). Dhruva et al. reported the consensus of the Vaidyas’ Ayurvedic descriptions of the pathophysiology of cancer, and approaches for the treatments of cancer. The paper also describes how biomedical treatments often result in depletion and degeneration of the body compared to Ayurvedic treatment which focuses on strengthening digestion, reducing Ama and improving tissue metabolism or Agni. They summarize that “the Tridosha perspective on cancer includes the involvement of Kapha to induce growth of tissue, Pitta in transforming the tissue from normal to malignant and the role of Vata in the spread of cancer outside of the organ such as metastasis.” [51].
Ayurvedic treatments aim to promote the body's self-healing properties and restore the body's natural defenses and immunity, and rejuvenate major body systems and promote long-term recovery from a disease. The Ayurvedic program of Panchakarma, is used as a multi-day cleansing regimen with specific techniques to strengthen Agni, clean out the Srotas, move toxins such as Ama out of the body and assist in the body's self-repair capacity [52]. This theory of Shat Kriya Kala is not yet scientifically validated but would be an interesting and fruitful area of research as applied to early detection of cancers. Other research opportunities related to Ayurveda and digestion are outlined in section 4.2.
3. The role of the mind, body, and spirit
Another influential component in cancer etiology is the relationship of body, mind, and spirit or consciousness. Early childhood exposure to adversity and stress can lead to neuroendocrine, epigenetic and psychological predispositions to cancer at a later age [53]. Ayurveda addresses the mind-body-spirit through techniques of yoga and meditation to remove stress and develop consciousness.
3.1. Research in mind, body, and spirit in relation to cancer
There is increased interest and research in the effect of the mind and spirit on the body and, in reverse, the role of physiology on mental function. The mind and thoughts are connected to neurotropic factors that influence and are influenced by immune function, all of which can affect the cancer microenvironment. This is called psychoneuroimmunology and its role in cancer progression is detailed in Green et al., 2013 [54].
Research has found associations between depression or stress-related psychosocial factors and cancer outcome. There is increased cancer incidence and mortality, and poor prognosis in populations exposed to chronic stress and depression. A meta study found an increased incidence in lung cancer in populations with psychosocial stress as well as decreased survival in populations with cancers of the head and neck, breast, lung, lymphoid or hematopoietic tissues [55]. Mental stress can also affect the biology of tumors such as in the stimulation of the adrenal hormone cortisol, and activation of the sympathetic nervous system and the downstream target effects. A comprehensive review is here [56]. These hormones influence the immune responses and inflammation, and alter tumor angiogenesis, mesenchymal differentiation, and metastasis [57]. This is observed in underrepresented minorities and underserved communities where exposure to stress has an increased impact on cancer survival and quality of life of patients with cancer [56]. The effects of stress may be moderated by an Ayurvedic lifestyle including proper diet, routine and especially stress-reducing techniques of breathing, yoga, and meditation which promote experiences of quieter levels of the mind, and different states of consciousness.
Research studies of the effects of practices of yoga and meditation for health purposes include up to 7071 publications for yoga, with 707 publications related to yoga and cancer, and 878 publications on meditation and cancer (PubMed/August 2022). An 8-week yoga therapy course was given in a randomized controlled trial to 159 patients of different cancer types. Yoga was found to reduce depression and fatigue in cancer patients with the greatest benefit to breast cancer patients [58]. Yoga was part of a multi-modality Ayurvedic nutrition and lifestyle intervention program in breast cancer survivors [59] which explored the feasibility and potential benefit of this approach to reducing symptoms of fatigue, sleep disturbance, anxiety, depression, and perceived stress. The study concluded that the Ayurvedic intervention may “contribute to clinically meaningful improvements in this survivorship population which merits future study in a randomized control trial”. A pilot study on yoga and obesity was important in providing a methodological design and template for Ayurvedic research [60].
The effects of stress reduction on cancer using meditation were explored in a single-blind, randomized control trial in 130 breast cancer patients. Quality of life measures from Functional Assessment of Cancer Therapy- Breast (FACT-B) indicated a positive effect in group using transcendental meditation (TM) plus standard of care (SOC) compared to SOC alone [61]. Also, a survey of use of medical care in TM practitioners found hospital admissions for tumors was decreased by 55.4% compared to other members in the same insurance carrier [62]. And finally, a recent study explored stress-related gene expression profiles of peripheral blood mononuclear cells from long term TM meditators compared to matched controls. Various genes were described with differential expression that correlates to stress effects indicating possible molecular mechanisms for future research [63].
There are many different types of yoga or meditation practices, therefore actual mechanisms may vary; and many practices are not necessarily from the Ayurvedic tradition. Well designed clinical trials and case studies are encouraged to increase evidence of yoga and meditation techniques for prevention of stress-induced tumor progression and inflammation, and for patient support during cancer therapies and in post treatment rejuvenative care. These studies give an important basis for developing clinical trials in research programs to understand the synergistic effects of combinations of mental techniques, herbs, diet, and routines of in Ayurvedic interventions for promoting health. Research opportunities related to Ayurveda and mind/body health are outlined in the discussion section 4.3.
4. Discussion: research challenges and directions
This Review serves as an introduction to Ayurvedic medicine for biomedical research scientists. It has provided an overview of a few of the many theories from Ayurveda and has reviewed some of the already extensive body of research in the traditional tenets of Prakriti, digestion, Agni, and Ama and the realm of mind, body, and spirit or consciousness, and their practical applications to cancer research. The next step is to encourage development of statistically strong and reproducible research methods for integration of these concepts into current health care studies especially for cancer research. This section provides some potential questions related to research gaps and opportunities as stimuli towards developing research programs.
4.1. Research directions: Prakriti
How can body composition and the three doshas, Vata, Pitta and Kapha be integrated into cancer research? Questions are proposed here relate to the role of Prakriti in clinical applications, genomics and epigenomics analysis and expression of the doshas on a cellular level.
-
1.Can we add Prakriti assessment to cancer Clinical Trials?
-
a.How does a patient's Prakriti contribute to differential responses to clinical treatment regimens?
-
b.Can Prakriti be used for preselection of patients to treatment arms in clinical trials?
-
c.If a clinical response is found to be influenced by the patient's Prakriti, what quantitative mechanistic data is measurable?
-
i.What are biomarkers of increase or decrease of each dosha?
-
i.
-
d.Do different body types get different cancers? (brain (V?) vs pancreas (P?) vs breast cancer (K?))?
-
e.How do we standardize assessment of Prakriti using pulse diagnosis, questionnaires, or algorithms for use in clinical trials?
-
a.
-
2.Can analysis of genomic and epigenomic databases be correlated to Prakriti in cancer studies.?
-
a.Can we validate the molecular biomarkers of body constitution or Prakriti using genomic or epigenomic expression profiles? (See recent publication for efforts in this area [64].
-
b.Can we add Prakriti assessment to evaluate existing genomics, epigenomics, metabolomics, and immunophenotyping data bases to correlate these genotypes and phenotypes to the Prakriti of the patients? This could be prospective or retrospective:
-
i.Prospective: Prakriti is determined at time of biospecimen collection and added to patient data
-
ii.Retrospective: For myriads of existing data bases, can we access electronic health records and ‘back-decipher’ the Prakriti – using body frame, disease propensity, body mass index, face/bone structure, etc.? Can we build an artificial intelligence algorithm of the Prakriti factors to include in the analysis of treatment results data?
-
i.
-
a.
-
3.If the qualities of VP&K are expressed in macro and micro manifestations in nature, what would be the intracellular and molecular correlates for VPK?
-
a.Can the Vata qualities of communication, transportation and intelligence be attributed to biomarkers involved in signal transduction, cell movement, or DNA code. Can the vagus nerve be a biomarker for Vata activity? [65].
-
b.Are Pitta qualities of transformation and metabolism seen in mitochondria production of ATP, DNA synthesis, transcription, and translation, enzymatic activities?
-
c.Can the Kapha qualities of structure, lubrication and stability be correlated to the actin cytoskeleton, DNA structure, and cellular membranes?
-
d.How can VPK be represented on the molecular and cellular levels and be developed as biomarkers?
-
a.
-
4.
Can we find biomarkers of diminished or increased V, P, and K? Such as, for “aggravated Vata” how would you measure the Vata qualities of dry, light, moving, etc. in the physiology or mind? Similar questions were raised in a review by Wallace [66]:
4.2. Research directions: digestion
Questions for research in Ayurvedic perspectives on digestion explore the physiological cellular and molecular mechanisms behind the concepts of Ama and Agni and the importance of digestion as basis for disease including cancer. Such questions include:
-
1.
What physiological mechanisms explain how poor digestion promotes toxic buildup of metabolic waste products that interfere with cellular and immune functioning?
-
2.
What are physiological correlates of different states of Agni? How could it be quantified for clinical analysis? What are biomarkers of increased Agni?
-
3.What are the biochemical/physical components of Ama?
-
a.How can we quantitate increased or decreased Ama in the physiology?
-
b.How does Ama induce inflammatory components?
-
c.What are parallels between Ama and increased intestinal permeability? What is role of the microbiome in this process?
-
d.How is the microbiome different in people of different Prakritis (V, P & K)?
-
a.
-
4.
How are toxins (Ama) embedded in the body and manifest as disease?
-
5.
How does the immune system recognize Ama as a foreign material and initiate the immune inflammation process?
-
6.
What are the physiological correlatives to the Ayurvedic protocols for digestion support to strengthen Agni and minimize Ama?
-
•Research in the detoxification protocols of Panchakarma may include:
-
•Efficacy of detoxification procedures
-
•Ability to recover from radiation or chemotherapy toxicity
-
•Changes in quality of life after Panchakarma.
-
•
4.3. Research directions: mind body-spirit
Protocols for research in this area may appear more subjective in defining physiological correlates of mental states and how the health of the body is reflected in the mind. Research studies on mind-body and cancer could examine these topics:
-
1.
What are the mechanisms of how stress affects tumor cell growth and cancer progression?
-
2.
Explore the link between the mind and digestion as through the gut microbiome?
-
3.
Explore use of Ayurvedic modalities in restorative and palliative care.
5. Summary for Part 1
Part 1 of this review has introduced some basic Ayurvedic concepts including body constitution (Prakriti), digestion (Agni and Ama) and mind-body-spirit health and their contributions to disease pathogenesis and their integration into cancer research. It is difficult to represent the depth of the of these concepts from the traditional Ayurvedic texts in the space of this document, and they deserve further study and development for potential applications. As we build research programs in Ayurveda, we need to bridge several gaps of communications. One gap is in the translation of the theories of this traditional medicine into current molecular and cellular terminology and clinical applications. These concepts, often expressed in the Sanskrit language, are unfamiliar and alienating to western biomedical researchers. The opportunity to understand and translate Ayurvedic principles such as Agni, Ama, Prakriti and others, may also contribute to our understanding of physiology and our approach to healing.
Part 2 of this review ([1]) will explore some of the Ayurvedic herbal products, and selected research on their biochemical mechanisms and clinical applications. Also, in Part 2 there will be a summary discussion of gaps and opportunities for research programs in Ayurveda and a consideration of experimental methodologies and clinical studies.
This 2-part review supports the integration of Ayurveda into current health care as a well-timed, low-cost approach to support immunity and optimal disease prevention for the general population and especially for cancer care. The additional value is the discovery of biomarkers of health and of unique perspectives for prevention and treatments for early and late stages of disease.
Disclaimer
This review is prepared as a personal activity of Dr. Julia T. Arnold. The opinions expressed in this article are the author's own and do not reflect the view of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
Funding sources
This review did not receive any specific grant from funding agencies in government, public, commercial, or not-for -profit sectors.
Conflict of interest
None.
Acknowledgements
Thank you to Dr. Perry Skeath and Shraddha Ravani for their conceptual input.
Dr. Arnold is sole author and contributor to the thoughts and ideas expressed here and agrees to the manuscript in its submitted state.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Arnold J.T. Integrating ayurvedic medicine into cancer research programs part 2: Ayurvedic herbs and research opportunities. J Ayurveda Integr Med. 2023;14(1):100677. doi: 10.1016/j.jaim.2022.100677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharma P.V. Chaukhambha Orientalia; Varanasi: 2008. Caraka Samhita. [Google Scholar]
- 3.Sharma P. Chaukhamba Bharati Academy; Varanasi: 2000. Sushruta Samhita. [Google Scholar]
- 4.Murthy K.R.S. Chowkhamba Krishnadas Academy; Varanasi, India: 2001. Ashtanga Hrdayam. [Google Scholar]
- 5.Ninivaggi F.J.M.D. Rowman & Littlefield Publishers, Inc.; Lanham MD: 2010. Ayurveda: a comprehensive guide to traditional Indian medicine for the west; p. 361. [Google Scholar]
- 6.Sharma H., Chandola H.M., Singh G., Basisht G. Utilization of Ayurveda in health care: an approach for prevention, health promotion, and treatment of disease. Part 1--Ayurveda, the science of life. J Alternative Compl Med. 2007;13(9):1011–1019. doi: 10.1089/acm.2007.7017-A. [DOI] [PubMed] [Google Scholar]
- 7.Sharma H., Chandola H.M., Singh G., Basisht G. Utilization of Ayurveda in health care: an approach for prevention, health promotion, and treatment of disease. Part 2--Ayurveda in primary health care. J Alternative Compl Med. 2007;13(10):1135–1150. doi: 10.1089/acm.2007.7017-B. [DOI] [PubMed] [Google Scholar]
- 8.Rastogi S. Building bridges between ayurveda and modern science. Int J Ayurveda Res. 2010;1(1):41–46. doi: 10.4103/0974-7788.59943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balachandran P., Govindarajan R. Cancer--an ayurvedic perspective. Pharmacol Res. 2005;51(1):19–30. doi: 10.1016/j.phrs.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 10.Chauhan A., Semwal D.K., Mishra S.P., Semwal R.B. Ayurvedic concept of Shatkriyakala: a traditional knowledge of cancer pathogenesis and therapy. J Integr Med. 2017;15(2):88–94. doi: 10.1016/S2095-4964(17)60311-X. [DOI] [PubMed] [Google Scholar]
- 11.Medicine M.S.K.I. https://www.mskcc.org/cancer-care/integrative-medicine/herbs/ayurveda Ayurveda [Available from:
- 12.Tiwari P., Kutum R., Sethi T., Shrivastava A., Girase B., Aggarwal S., et al. Recapitulation of Ayurveda constitution types by machine learning of phenotypic traits. PLoS One. 2017;12(10) doi: 10.1371/journal.pone.0185380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hankey A. Establishing the scientific validity of tridosha part 1: doshas, subdoshas and dosha prakritis. Ancient Sci Life. 2010;29(3):6–18. [PMC free article] [PubMed] [Google Scholar]
- 14.Hankey A. Ayurvedic physiology and etiology: Ayurvedo Amritanaam. The doshas and their functioning in terms of contemporary biology and physical chemistry. J Alternative Compl Med. 2001;7(5):567–574. doi: 10.1089/10755530152639792. [DOI] [PubMed] [Google Scholar]
- 15.Chatterjee B., Pancholi J. Prakriti-based medicine: a step towards personalized medicine. Ayu. 2011;32(2):141–146. doi: 10.4103/0974-8520.92539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rotti H., Raval R., Anchan S., Bellampalli R., Bhale S., Bharadwaj R., et al. Determinants of prakriti, the human constitution types of Indian traditional medicine and its correlation with contemporary science. J Ayurveda Integr Med. 2014;5(3):167–175. doi: 10.4103/0975-9476.140478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joshi R.R. A biostatistical approach to ayurveda: quantifying the tridosha. J Alternative Compl Med. 2004;10(5):879–889. doi: 10.1089/acm.2004.10.879. [DOI] [PubMed] [Google Scholar]
- 18.Patwardhan B., Bodeker G. Ayurvedic genomics: establishing a genetic basis for mind-body typologies. J Alternative Compl Med. 2008;14(5):571–576. doi: 10.1089/acm.2007.0515. [DOI] [PubMed] [Google Scholar]
- 19.Patwardhan B., Warude D., Pushpangadan P., Bhatt N. Ayurveda and traditional Chinese medicine: a comparative overview. Evid Based Complement Alternat Med. 2005;2(4):465–473. doi: 10.1093/ecam/neh140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhushan P., Kalpana J., Arvind C. Classification of human population based on HLA gene polymorphism and the concept of Prakriti in Ayurveda. J Alternative Compl Med. 2005;11(2):349–353. doi: 10.1089/acm.2005.11.349. [DOI] [PubMed] [Google Scholar]
- 21.Prasher B., Varma B., Kumar A., Khuntia B.K., Pandey R., Narang A., et al. Ayurgenomics for stratified medicine: TRISUTRA consortium initiative across ethnically and geographically diverse Indian populations. J Ethnopharmacol. 2017;197:274–293. doi: 10.1016/j.jep.2016.07.063. [DOI] [PubMed] [Google Scholar]
- 22.Prasher B., Gibson G., Mukerji M. Genomic insights into ayurvedic and western approaches to personalized medicine. J Genet. 2016;95(1):209–228. doi: 10.1007/s12041-015-0607-9. [DOI] [PubMed] [Google Scholar]
- 23.Prasher B., Negi S., Aggarwal S., Mandal A.K., Sethi T.P., Deshmukh S.R., et al. Whole genome expression and biochemical correlates of extreme constitutional types defined in Ayurveda. J Transl Med. 2008;6:48. doi: 10.1186/1479-5876-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghodke Y., Joshi K., Patwardhan B. Traditional medicine to modern Pharmacogenomics: ayurveda prakriti type and CYP2C19 gene polymorphism associated with the metabolic variability. Evid Based Complement Alternat Med. 2011;2011 doi: 10.1093/ecam/nep206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Govindaraj P., Nizamuddin S., Sharath A., Jyothi V., Rotti H., Raval R., et al. Genome-wide analysis correlates ayurveda prakriti. Sci Rep. 2015;5 doi: 10.1038/srep15786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sharma H., Keith Wallace R. Ayurveda and epigenetics. Medicina. 2020;56(12) doi: 10.3390/medicina56120687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rotti H., Mallya S., Kabekkodu S.P., Chakrabarty S., Bhale S., Bharadwaj R., et al. DNA methylation analysis of phenotype specific stratified Indian population. J Transl Med. 2015;13:151. doi: 10.1186/s12967-015-0506-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rotti H., Guruprasad K.P., Nayak J., Kabekkodu S.P., Kukreja H., Mallya S., et al. Immunophenotyping of normal individuals classified on the basis of human dosha prakriti. J Ayurveda Integr Med. 2014;5(1):43–49. doi: 10.4103/0975-9476.128857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Juyal R.C., Negi S., Wakhode P., Bhat S., Bhat B., Thelma B.K. Potential of ayurgenomics approach in complex trait research: leads from a pilot study on rheumatoid arthritis. PLoS One. 2012;7(9) doi: 10.1371/journal.pone.0045752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bhalerao S., Patwardhan K. Prakriti-based research: good reporting practices. J Ayurveda Integr Med. 2016;7(1):69–72. doi: 10.1016/j.jaim.2015.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Peterson C.T., Denniston K., Chopra D. Therapeutic uses of Triphala in ayurvedic medicine. J Alternative Compl Med. 2017;23(8):607–614. doi: 10.1089/acm.2017.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mukta Rao MV., Arora J. Efficacy of Samsarjanakrama in a patient with Agnimandya due to vyadhi sankar: a case study. J Ayurveda Integr Med. 2021;12(1):182–186. doi: 10.1016/j.jaim.2021.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Byadgi P.S. Critical appraisal of Doshavaha Srotas. Ayu. 2012;33(3):337–342. doi: 10.4103/0974-8520.108819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tripathi J.S., Singh R.H. Possible correlates of free Radicals and free radical mediated Disorders in ayurveda with special reference to Bhutagni Vyapara and Ama at molecular level. Ancient Sci Life. 1999;19(1–2):17–20. [PMC free article] [PubMed] [Google Scholar]
- 35.Sumantran V.N., Tillu G. Cancer, inflammation, and insights from ayurveda. Evid Based Complement Alternat Med. 2012;2012 doi: 10.1155/2012/306346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zitvogel L., Pietrocola F., Kroemer G. Nutrition, inflammation and cancer. Nat Immunol. 2017;18(8):843–850. doi: 10.1038/ni.3754. [DOI] [PubMed] [Google Scholar]
- 37.Vancamelbeke M., Vermeire S. The intestinal barrier: a fundamental role in health and disease. Expet Rev Gastroenterol Hepatol. 2017;11(9):821–834. doi: 10.1080/17474124.2017.1343143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Riccio P., Rossano R. Undigested food and gut microbiota may cooperate in the pathogenesis of neuroinflammatory diseases: a matter of barriers and a proposal on the Origin of organ specificity. Nutrients. 2019;11(11) doi: 10.3390/nu11112714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wallace R.K. The microbiome in health and disease from the perspective of modern medicine and ayurveda. Medicina. 2020;56(9) doi: 10.3390/medicina56090462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.IhiRN Consortium. The integrative human microbiome Project. Nature. 2019;569(7758):641–648. doi: 10.1038/s41586-019-1238-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sepich-Poore G.D., Zitvogel L., Straussman R., Hasty J., Wargo J.A., Knight R. The microbiome and human cancer. Science. 2021;(6536):371. doi: 10.1126/science.abc4552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nicolaro M., Portal D.E., Shinder B., Patel H.V., Singer E.A. The human microbiome and genitourinary malignancies. Ann Transl Med. 2020;8(19):1245. doi: 10.21037/atm-20-2976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gopalakrishnan V., Spencer C.N., Nezi L., Reuben A., Andrews M.C., Karpinets T.V., et al. Gut microbiome modulates response to anti-PD-1 immunotherapy in melanoma patients. Science. 2018;359(6371):97–103. doi: 10.1126/science.aan4236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kendig M.D., Leigh S.J., Morris M.J. Unravelling the impacts of western-style diets on brain, gut microbiota and cognition. Neurosci Biobehav Rev. 2021;128:233–243. doi: 10.1016/j.neubiorev.2021.05.031. [DOI] [PubMed] [Google Scholar]
- 45.Shondelmyer K., Knight R., Sanivarapu A., Ogino S., Vanamala J.K.P. Ancient Thali diet: gut microbiota, immunity, and health. Yale J Biol Med. 2018;91(2):177–184. [PMC free article] [PubMed] [Google Scholar]
- 46.Kuttikrishnan M., Sridhar R., Varghese E. Jatharagni and Prakriti of young Indian adult population: a descriptive cross-sectional study. J Ayurveda Integr Med. 2022;13(1) doi: 10.1016/j.jaim.2021.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chaudhari D., Dhotre D., Agarwal D., Gondhali A., Nagarkar A., Lad V., et al. Understanding the association between the human gut, oral and skin microbiome and the Ayurvedic concept of prakriti. J Biosci. 2019;44(5) [PubMed] [Google Scholar]
- 48.Chauhan N.S., Pandey R., Mondal A.K., Gupta S., Verma M.K., Jain S., et al. Western Indian rural gut microbial diversity in extreme prakriti endo-phenotypes Reveals signature microbes. Front Microbiol. 2018;9:118. doi: 10.3389/fmicb.2018.00118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peterson C.T., Rodionov D.A., Iablokov S.N., Pung M.A., Chopra D., Mills P.J., et al. Prebiotic potential of culinary spices used to support digestion and bioabsorption. Evid Based Complement Alternat Med. 2019;2019 doi: 10.1155/2019/8973704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Johri R.K., Zutshi U. An Ayurvedic formulation 'Trikatu' and its constituents. J Ethnopharmacol. 1992;37(2):85–91. doi: 10.1016/0378-8741(92)90067-2. [DOI] [PubMed] [Google Scholar]
- 51.Dhruva A., Hecht F.M., Miaskowski C., Kaptchuk T.J., Bodeker G., Abrams D., et al. Correlating traditional Ayurvedic and modern medical perspectives on cancer: results of a qualitative study. J Alternative Compl Med. 2014;20(5):364–370. doi: 10.1089/acm.2013.0259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Conboy L., Edshteyn I., Garivaltis H. Ayurveda and Panchakarma: measuring the effects of a holistic health intervention. Sci World J. 2009;9:272–280. doi: 10.1100/tsw.2009.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kelly-Irving M., Mabile L., Grosclaude P., Lang T., Delpierre C. The embodiment of adverse childhood experiences and cancer development: potential biological mechanisms and pathways across the life course. Int J Publ Health. 2013;58(1):3–11. doi: 10.1007/s00038-012-0370-0. [DOI] [PubMed] [Google Scholar]
- 54.Green McDonald P., O'Connell M., Lutgendorf S.K. Psychoneuroimmunology and cancer: a decade of discovery, paradigm shifts, and methodological innovations. Brain Behav Immun. 2013;30(Suppl):S1–S9. doi: 10.1016/j.bbi.2013.01.003. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chida Y., Hamer M., Wardle J., Steptoe A. Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pract Oncol. 2008;5(8):466–475. doi: 10.1038/ncponc1134. [DOI] [PubMed] [Google Scholar]
- 56.Minas T.Z., Kiely M., Ajao A., Ambs S. An overview of cancer health disparities: new approaches and insights and why they matter. Carcinogenesis. 2021;42(1):2–13. doi: 10.1093/carcin/bgaa121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cole S.W., Nagaraja A.S., Lutgendorf S.K., Green P.A., Sood A.K. Sympathetic nervous system regulation of the tumour microenvironment. Nat Rev Cancer. 2015;15(9):563–572. doi: 10.1038/nrc3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zetzl T., Renner A., Pittig A., Jentschke E., Roch C., van Oorschot B. Yoga effectively reduces fatigue and symptoms of depression in patients with different types of cancer. Support Care Cancer. 2021;29(6):2973–2982. doi: 10.1007/s00520-020-05794-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dhruva A., Wu C., Miaskowski C., Hartogensis W., Rugo H.S., Adler S.R., et al. A 4-month whole-systems ayurvedic medicine nutrition and lifestyle intervention is feasible and acceptable for breast cancer survivors: results of a single-arm pilot clinical trial. Glob Adv Health Med. 2020;9 doi: 10.1177/2164956120964712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rioux J., Howerter A. Outcomes from a whole-systems ayurvedic medicine and yoga therapy treatment for obesity pilot study. J Alternative Compl Med. 2019;25(S1) doi: 10.1089/acm.2018.0448. S124-s37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nidich S.I., Fields J.Z., Rainforth M.V., Pomerantz R., Cella D., Kristeller J., et al. A randomized controlled trial of the effects of transcendental meditation on quality of life in older breast cancer patients. Integr Cancer Ther. 2009;8(3):228–234. doi: 10.1177/1534735409343000. [DOI] [PubMed] [Google Scholar]
- 62.Orme-Johnson D. Medical care utilization and the transcendental meditation program. Psychosom Med. 1987;49(5):493–507. doi: 10.1097/00006842-198709000-00006. [DOI] [PubMed] [Google Scholar]
- 63.Wenuganen S., Walton K.G., Katta S., Dalgard C.L., Sukumar G., Starr J., et al. Transcriptomics of long-term meditation practice: evidence for prevention or reversal of stress effects harmful to health. Medicina. 2021;57(3) doi: 10.3390/medicina57030218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Abbas T., Chaturvedi G., Prakrithi P., Pathak A.K., Kutum R., Dakle P., et al. Whole exome sequencing in healthy individuals of extreme constitution types Reveals differential disease Risk: a novel approach towards predictive medicine. J Personalized Med. 2022;12(3) doi: 10.3390/jpm12030489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sumantran V.N., Nair P.P. Can the vagus nerve serve as biomarker for vata dosha activity? J Ayurveda Integr Med. 2019;10(2):146–151. doi: 10.1016/j.jaim.2019.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wallace R.K. Ayurgenomics and modern medicine. Medicina. 2020;56(12) doi: 10.3390/medicina56120661. [DOI] [PMC free article] [PubMed] [Google Scholar]