Abstract
In Japan, as in other countries around the world, acne vulgaris is a common disease and a frequent reason for patients to consult dermatologists. For optimal management of acne, it is important to understand how available products to support skin health can be used both with and without prescription products. Dermocosmetics can be defined as skincare agents with dermatologically active ingredients that directly support or care for the symptoms of various skin conditions (distinct from vehicle effects). There are products with active ingredients—including familiar ones such as niacinamide, retinol derivatives, and salicylic acid—that target important aspects of acne pathophysiology. Others, including ceramides, glyercin, thermal spring water, and panthenols, may have positive effects on skin barrier function that are useful in managing acne. This publication will discuss the roles of dermocosmetics in acne either as monotherapy to manage the milder forms of acne and help prevent relapses, or as adjuncts to prescription therapy to increase efficacy or adherence and assist in prevention of local adverse effects. Dermocosmetics may also have active ingredients that positively impact the skin microbiome.
Keywords: Acne vulgaris, Dermocosmetics, Moisturizers, Cleansers, Japan, Skincare
Key Summary Points
| Acne is a very common skin condition in Japan, as in other parts of the world. |
| There is a wide variety of skincare products marketed for acne, and educating patients about which products to use can be challenging for healthcare professionals. |
| Products with active ingredients (known as dermocosmetics) can have positive effects that are useful in managing acne, both when used alone and when used as adjunct for medical treatments. |
| Ingredients particularly useful in acne include niacinamide, retinol derivatives, salicylic acid, ceramides, glyercin, thermal spring water, and panthenol. |
Introduction
Acne vulgaris is a prevalent dermatologic condition in Japan [1]. Guidelines for the management of acne in Japan were published in 2018 and highlighted the role of prescription therapy with benzoyl peroxide and topical retinoids in combination, along with the need to limit the duration of antibiotic use [2]. Skincare and related treatments were addressed in a very general way, but focused on cleansing, use of makeup, and dietary recommendations. Regarding skincare products, the guidelines “recommend to use the skincare products for acne,” while carefully choosing “low-irritant and non-comedogenic products” [2]. The authors cited several studies of skincare products used either in combination with acne treatments or individually [2]. However, available skincare products are evolving, and it is becoming increasingly important to understand how to optimize skincare regimens in acne both when used alone and when used with prescription treatments [3, 4]. This publication will discuss how dermocosmetics can be an important tool in acne management either as monotherapy for the milder forms of acne, or as adjunct to medical treatments to increase efficacy or adherence and to assist in minimizing the occurrence of local adverse effects. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
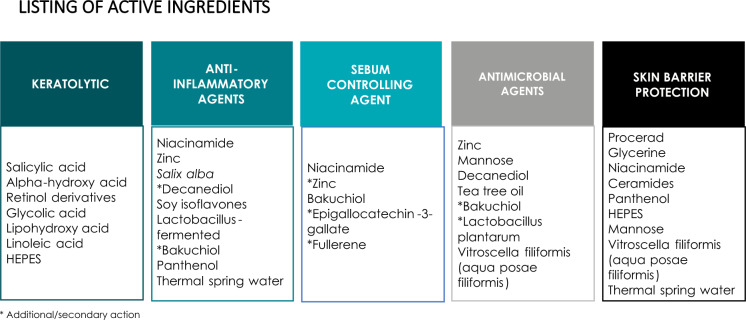
Since “dermocosmetic” is a relatively new term (potentially not familiar to either Japanese patients or healthcare professionals), it is useful to provide a definition. Dermocosmetics are skincare solutions that use sophisticated, dermatologically active ingredients to directly support or care for the symptoms of various skin conditions (in ways which would not occur from use of vehicle alone) [5]. The active ingredients in dermocosmetics, some of which are quite familiar such as niacinamide, zinc, or salicylic acid, may target important aspects of acne pathophysiology [3, 6]. Active ingredients, such as panthenol, ceramides, glycerin, niacinamide, thermal spring water, and mannose, may also act to support skin barrier function, and in turn minimize irritation and other undesirable effects of acne treatment. Figure 1 lists some of the ingredients that may be found in dermocosmetics as well as their actions [3, 4]. Keratolytic agents such as alpha hydroxy acids (AHAs) can support epidermal barrier function by controlling hyperkeratization and increasing epidermal thickness. These ingredients may also normalize the microbiome via peeling effects, and may decrease inflammation via immunomodulation [3]. Additional ingredients, including Aqua Posae Siliformis (APF), a lysate of Vitreoscilla filiformis grown in thermal spring water, are being studied for effects on the skin microbiome [7–9]. With these types of ingredients and sophisticated formulations, dermocosmetics are different from both prescription drugs and cosmetic/mass market products.
Fig. 1.
Active ingredients that may be found in dermocosmetics and their targeted actions. Adapted with permission from Araviiskaia et al. J Dermatol Treat 2011 [4]
Understanding Acne Management in Japan
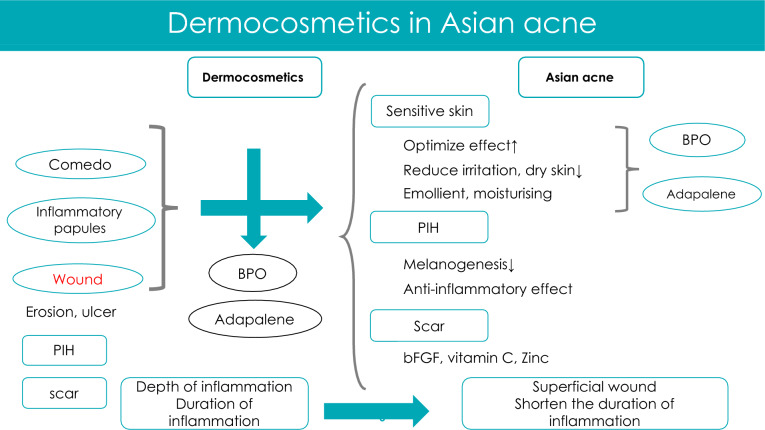
Acne is generally similar in various worldwide populations; however, some specific characteristics of acne in Japanese have been identified. There is a higher likelihood of skin irritation and/or sensitive skin compared with other populations [10]. In addition, postinflammatory hyperpigmentation (PIH) is very common (58.2% of patients) as is the occurrence of micro-scars (in as many as 90.8% of patients) [11, 12]. Patients are likely to report irritation and allergic contact dermatitis with use of benzoyl peroxide (BPO) 3% and for that reason, short-contact therapy is used for both BPO and adapalene in Asian countries [13]. Dermocosmetics can reduce side effects and optimize efficacy, increasing the likelihood of preventing PIH and scar formation [14].
Recently, a web-based questionnaire of Japanese women aged 20–40 years old with acne (n = 618) was conducted [15]. A large proportion of respondents (67.3%) reported being worried about the potential for acne relapse. More than 60% were worried about “dirty appearance,” scarring, and hyperpigmentation. When asked to identify the most bothersome aspect of acne, respondents indicated scarring and pigmentation problems. Respondents also revealed that there are a number of misconceptions and knowledge gaps about acne, particularly in relationship to the impact of diet and skin manipulation (excoriation). They reported receiving information through social networking sources and that there is a high emotional burden of acne, with depression being a concern. Many of these women (32.8%) felt that use of skincare would worsen their acne. They also expressed that the array of skincare products available makes it difficult to know which products they should use. This may pose a challenge for clinicians as well.
Regulations in Japan
Medical therapy for acne in Japan largely relies on BPO and adapalene, as well as antimicrobial agents and Chinese herbal medicines, which may also be used [2]. Current acne guidelines in Japan have very limited mentions of dermocosmetics in part due to how cosmetics and non-drug products are viewed in terms of regulatory restrictions [2]. In Japan, cosmetic products are under the regulatory supervision of the Pharmaceutical and Medical Device Agency (PMDA) and the Ministry of Health, Labor and Welfare (MHLW). Cosmetics are defined as products with mild biologic action that are applied by rubbing, sprinkling, and other methods to clean, beautify, or maintain the appearance of skin or hair. A second category is termed “quasi drugs,” and this includes medicated cosmetics such as those used to manage oily or acne-prone skin. These are not covered by healthcare insurance and physicians may not recommend specific products (it is very difficult to provide such guidance to patients). Claims for actions may not be made for cosmetics, but can in a limited fashion be made for quasi drugs that have been approved by MHLW. Japan also has over-the-counter (OTC) drugs that are managed by pharmacists and ethical pharmaceuticals, prescribed by physicians, and reimbursed by health insurance. Skincare guidance is provided as lifestyle guidance and cosmetics are not usually specified by the physicians. Samples and leaflets may be provided in hospital/clinic. There are products that can contribute to skincare (moisturizers and vitamins), but prescribing such products is only allowed for medical therapeutic uses.
There is currently very sparse education about the impact of skincare in Japan for healthcare practitioners. Medical textbooks typically do not include chapters on skincare, and if included it is explained to the extent of washing, moisturizing, and using sunscreens in diseases. Going forward, it will be important to show the impact of skincare on the epidermal barrier function and how that can be leveraged to improve efficacy of acne management and as a preventive strategy.
Integrating Dermocosmetics into Acne Management
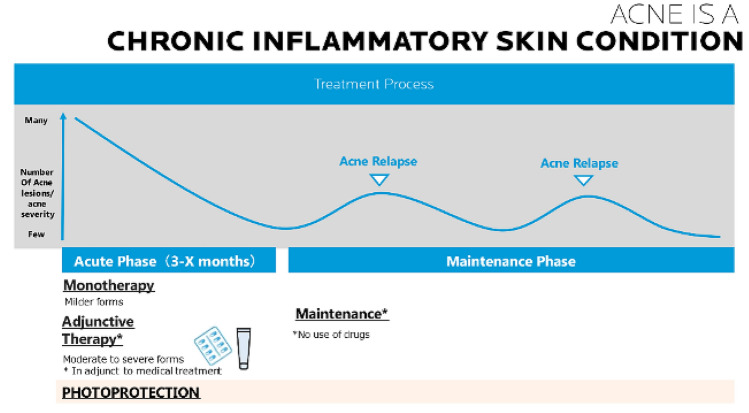
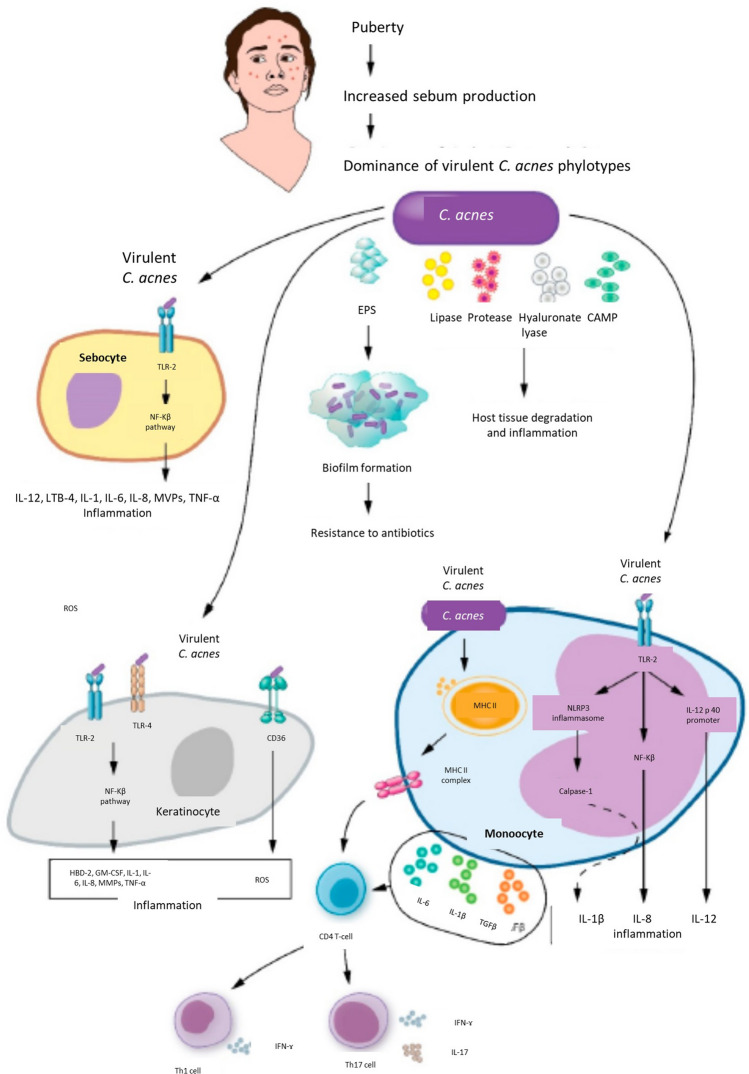
It has long been known that the main actors in acne are the sebaceous gland (hyperseborrhea), epidermis with hyperkeratinization (comedo), inflammation, and activation of innate immunity [16]. Now, the impact of skin surface and follicular microbiome in acne is better appreciated, particularly in regard to Cutibacterium acnes, Staphylococcus epidermidis, and Staphylococcus aureus (Fig. 2) [17]. In acne, skincare products have several mechanisms of action, including: (1) protecting and improving the skin barrier, (2) protecting the skin microbiome, (3) maintaining a healthy cutaneous pH, and (4) protecting against ultraviolet (UV) damage [3]. In turn, protection against UV exposure can help reduce the likelihood of PIH, which, as explained above, is a significant issue in Japanese skin.
Fig. 2.
Timecourse of acne and intervention sequences
Acne is a chronic inflammatory skin condition and there are a number of clinical situations when dermocosmetics may have a beneficial effect in management over the course of disease (Fig. 2). During the acute phase, dermocosmetics may be useful as monotherapy for milder forms of acne, and/or as adjuncts to prescription treatment to maximize tolerance and adherence. Photoprotection is recommended throughout the course. Figure 3 presents a general overview of how dermocosmetics may be used within the acne management plan.
Fig. 3.
General schema for integrating dermocosmetics into acne care
Dermocosmetic Mechanisms
As noted above, protection of the skin barrier is an important mechanism whereby dermocosmetics can improve acne management. Dysfunction of the epidermal barrier can be a feature of the disease and can also occur as a result of acne treatments, including over-the-counter (OTC) products, ethical prescription products, and procedures such as peeling [18]. Clinically, barrier dysfunction manifests as dry skin, irritation in the form of stinging/burning/tingling, tightness, pain, or irritant dermatitis [18]. These are thought to be related to transepidermal water loss (TEWL) and can be at least partially relieved with use of moisturizers [14, 18].
As early as 1995, Yamamoto et al. demonstrated that Japanese acne patients had increased TEWL compared with control subjects [19]. The differences were significant even in patients with mild and moderate acne. These patients also had lower levels of ceramides, which correlated with water barrier function. The authors speculated that the decreased ceramides may contribute to hyperkeratotic barrier dysfunction and formation of comedones [19]. In addition, puberty may be associated with increased TEWL versus younger ages. Finally, a later study confirmed the finding that ceramide reductions in acne correlate with increased TEWL [20]. For these reasons, Marson et al. speculate that “increases in TEWL may be a result of ceramide imbalances due to adrenarche-induced ceramide synthetic dysfunction” [18]. Further, these changes may contribute to development or exacerbation of acne [18]. Beyond that, some acne treatments, such as retinoid-based regimens, can worsen skin dryness and irritation, which may contribute not only to alterations in barrier function, but also an increased likelihood of secondary PIH in darker-skinned patients [21].
Protection of the cutaneous microbiome is also emerging as an important mechanism of dermocosmetics. While the skin provides a physical, chemical, and immune barrier, it also is the habitat for a vast community of microorganisms including bacteria, fungi, mites, and viruses; this habitat is known as the microbiome [18, 22]. Marson et al. note that there is a tenfold greater number of bacterial cells compared with human cells in the body (not to mention the number of other microorganisms), demonstrating the importance of understanding how the microbiome may affect physiologic functioning of the epidermis [23]. The microbiome can be considered as a second skin, and is divided into resident (normal commensal skin microbes) and transient flora (pathogenic microbes) [24, 25]. The central role of the skin microbiome, together with epidermal barrier function, provides a strong rationale for optimizing skincare.
As shown in Fig. 4, the quality and quantity of sebum influence the profile of the microbiome in skin [24]. It is now known that dysbiosis in acne is not related to the quantity of C. acnes, but rather the proliferation of a specific phylotype (IA1) [26, 27]. Further, loss of microbial diversity leads to activation of innate immunity, and in turn, secretion of proinflammatory cytokines. Thus it is important to maintain a healthy biodiversity [27]. At the therapeutic level, the goal is to try to restore the diversity of the microbiome and suppress inflammation via downregulation of innate immunity [27]. In addition, there are important interactions between C. acnes and S. epidermidis that have a pathophysiologic role in acne as well as postinflammatory hyperpigmentation [28, 29]. A full discussion of the mechanisms involved in acne and microbiome is beyond the scope of this publication, but the reader is encouraged to investigate this fascinating new update to acne pathophysiology in more detail; some data on how dermocosmetics may affect microbiome are presented below.
Fig. 4.
Model of acne pathologic processes induced by C. acnes interactions with sebocytes, keratinocytes, and monocytes. Reprinted with permission from Lee et al. [24]. EPS extracellular polymeric substances, CAMP cyclic adenosine monophosphate, TLR toll-like receptor, IL interleukin, TNF tumor necrosis factor, LTB leukotriene B, CD36 cluster of differentiation 36, GM-CSF granulocyte-macrophage colony-stimulating factor, hBD human β-defensin, MMPs matrix metalloproteinases
Appropriate cleansing and moisturizing can be used to maintain a physiologic pH for the skin. As early as 1995, Korting et al. reported that use of an acidic syndet bar (pH 5.5–5.6) was associated with a significant decrease in number of noninflammatory and inflammatory lesions when compared with use of an ordinary soap with pH 8 [30]. Since then, changes in pH have been linked to the pathogenesis of acne via the integrity of the skin barrier, supporting the recommendation of skin cleansing agents with a pH around 5.5 [31]. Sunscreens are an important part of good general skincare, and can help prevent PIH in acne sufferers with darker skin tones. Data on PIH and scarring in Japanese are somewhat sparse, but it seems that this population may be at higher risk of developing PIH compared with some other population groups [11].
Evidence for Use of Dermocosmetics in Acne
The literature base for use of dermocosmetics in acne will be briefly discussed below (a full discussion is beyond the scope of this paper). It should be noted that when compared with existing studies of prescription drugs, dermocosmetic studies often have a smaller sample size, may have a less rigorous design, may not use standardized grading/assessment systems, and may not rigorously define severity of acne in the studied population.
Dermocosmetic Monotherapy in Milder Forms of Acne and/or Prevention of Recurrence
The database of studies showing that dermocosmetics alone can have a positive impact in management of acne is growing. Overall trends in outcomes from available literature suggest that dermocosmetics can improve global assessment, reduce acne lesions, maintain acne clearance after prescription treatment, and may have a beneficial effect in minimizing superficial skin oiliness [3, 4]. These outcomes align with the authors’ clinical experience and indicate that dermocosmetics have a role in management of acne; however, further studies are needed to better understand that role. Ingredients which may have benefit in this setting include, but are not limited to, glycolic acid, LHA, linoleic acid, niacinamide, zinc, piroctone olamine, procerad, and Vitroscella filiformis.
Dermocosmetics as Adjunctive Therapy
Improve Adherence and Reduce Treatment-Induced Irritation
Acne is perhaps uniquely plagued by poor adherence to prescription treatments [32–34]. When adherence is poor, the skin barrier is often compromised. Skincare may contribute to normalizing and maintaining the skin barrier, protecting the microbiome, and preventing activation of innate immunity (skin inflammation).
In 2018, Tan et al. compared acne treatment with adapalene-BPO in four different regimens, one of which involved use of a daily moisturizer [14]. The results showed that the daily moisturizer regimen with daily adapalene-BPO reduced patient reports of drying and scaling. In addition, an every-other-night regimen of adapalene-BPO for the first 4 weeks was associated with better efficacy than every night adapalene-BPO (although overall efficacy rates were similar by week 12 of the study). Thus, the authors concluded that improving local tolerability in the beginning of treatment did not have a negative impact on efficacy and may have improved treatment adherence [14]. Additional studies have also reported positive effects of dermocosmetics in reducing irritation or adverse events when used as adjunctive therapy to prescription regimens [35–42]. Specifically, adding dermocosmetics can result in significantly less erythema, dryness, and scaling along with improved tolerability scores and composite skin sensitivity scores [35–42]. There is also evidence that dermocosmetic use may have a positive effect on adherence, satisfaction, or quality of life. Dermocosmetic ingredients to consider in this setting include niacinamide, zinc, ceramides, shea butter, Vitroscella filiformis, licochalcone A, L carnitine, 1,2-Decanediol, zinc, glycyrrhetinic acid, tocopheryl, and ceramides.
Improve Skin Barrier Function
Skin barrier alteration leads to change in microbiome and activation of innate immunity with penetration of antigens as pathogens. Isoda et al. reported that 4-week use of a weakly acidic foaming facial skin cleanser and moisturizing gel in patients with mild acne and sensitive skin (n = 29) significantly decreased acne. A statistically significant improvement with dermocosmetic use has been shown in skin hydration on corneometry [36, 43]. Further, studies have reported a 10.8% to 29% mean reduction in TEWL, which was statistically significant in two studies [37, 41, 44]. Ingredients to consider in this setting include lichocalcone A, L carnitine, 1,2-Decanediol, salicylic acid, vitamin C, hyaluronic acid, ceramides, zinc, glycyrrhetinic acid, and tocopheryl.
Tan et al. assessed the benefit of a dermocosmetic regimen in management of local cutaneous side effects associated with use of a fixed-dose adapalene-BPO gel in 43 patients with mild–moderate acne [45]. The dermocosmetic regimen consisted of a cream containing maltodextrine and Bixa orellana seed extract, a plant derivative that reduces sebum and hyperkeratinization, along with niacinamide, panthenol, and Aqua Posae Filiformis (APF) to decrease inflammation and improve skin barrier function [45]. The cream was used with a cleanser containing maltodextrine, Bixa orellana seed extract, niacinamide, APF, and citric acid. At day 14 and day 28, the dermocosmetic regimen significantly improved skin sensitivity composite score (P < 0.001 versus baseline) as well as individual scores for erythema, dryness, and desquamation (P < 0.005 each). Acne global assessments and lesion counts also significantly improved at the day 14 and day 28 timepoints (P < 0.0001), while 87% of patients reported their treatment had better overall tolerability.
Normalize Skin Microbiota
Normalizing skin microbiota may be particularly important when using topical drugs that can impair the microbiome or alter barrier function [46]. In this situation, it is helpful to advise patients to avoid intensive washing and to use a moisturizing cream that can maintain the integrity of the microbiome. Moisturizers can help protect the lamellar layer by supplementing ceramides and lipids, which may reduce water loss and support barrier impermeability. In addition, they can support filaggrin and natural moisturizing factor to maintain skin hydration.
Conclusions
Dermocosmetics offer value in the management of acne as monotherapy for milder forms or maintenance and as adjunctive therapy to medical treatments to manage skin irritation/increase adherence, enhance efficacy, and provide photoprotection and other beneficial effects to minimize likelihood of PIH and scarring.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by La Roche Posay International.
Medical Writing
Editorial support and funding for Valerie Sanders of Sanders Medical Writing was provided by La Roche Posay International.
Author Contributions
All authors (Dr. Kurokawa, Dr. Dreno, Dr. Kerob, Dr. Kobayashi, Dr. Abe, and Dr. Nomura) participated in development of content and approved the manuscript prior to submission.
Disclosures
Dr. Kurokawa has received research grants from Aisin Corporation. Dr. Dreno has served as a consultant for Galderma, La Roche Posay, and Pierre Fabre. Dr. Kobayashi has served as a speaker for Maruho and Sun Pharma. Dr Nomura has nothing to declare. Dr. Abe has served as a consultant/speaker/advisor for Torii Pharmaceutical Co, Maruho Co., AbbVie GK, Eli Lilly Japan K.K, Novartis Pharma, Sanofi, UCB Japan, Kyowa Kirin Co, Sun Pharma, and Bristol Myers Squibb. Dr Kerob is an employee of La Roche Posay International, Paris, France.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed for the current publication. Data will be accessible on request and after study by the sponsor of the study. The sponsor reserves the right to refuse if the objective is not admissible. Upon provision, a secure link will be provided.
References
- 1.Tanaka A, Niimi N, Takahashi M, et al. Prevalence of skin diseases and prognosis of atopic dermatitis in primary school children in populated areas of Japan from 2010 to 2019: the Asa Study in Hiroshima, Japan. J Dermatol. 2022;49:1284–90. [DOI] [PubMed]
- 2.Hayashi N, Akamatsu H, Iwatsuki K, et al. Japanese Dermatological Association Guidelines: guidelines for the treatment of acne vulgaris 2017. J Dermatol. 2018;45:898–935. doi: 10.1111/1346-8138.14355. [DOI] [PubMed] [Google Scholar]
- 3.Araviiskaia E, Dreno B. The role of topical dermocosmetics in acne vulgaris. J Eur Acad Dermatol Venereol. 2016;30:926–935. doi: 10.1111/jdv.13579. [DOI] [PubMed] [Google Scholar]
- 4.Araviiskaia E, Lopez Estebaranz JL, Pincelli C. Dermocosmetics: beneficial adjuncts in the treatment of acne vulgaris. J Dermatolog Treat. 2021;32:3–10. doi: 10.1080/09546634.2019.1628173. [DOI] [PubMed] [Google Scholar]
- 5.Varcin M KC. Focus on: cosmeceuticals-definitions, regulations and a review of the market. PMFA News. 2016;3.
- 6.Saint-Leger D. “Cosmeceuticals”. Of men, science and laws. Int J Cosmet Sci. 2012;34:396–401. doi: 10.1111/j.1468-2494.2012.00740.x. [DOI] [PubMed] [Google Scholar]
- 7.Gueniche A, Knaudt B, Schuck E, et al. Effects of nonpathogenic gram-negative bacterium Vitreoscilla filiformis lysate on atopic dermatitis: a prospective, randomized, double-blind, placebo-controlled clinical study. Br J Dermatol. 2008;159:1357–1363. doi: 10.1111/j.1365-2133.2008.08836.x. [DOI] [PubMed] [Google Scholar]
- 8.Nakatsuji T, Gallo RL. Dermatological therapy by topical application of non-pathogenic bacteria. J Invest Dermatol. 2014;134:11–14. doi: 10.1038/jid.2013.379. [DOI] [PubMed] [Google Scholar]
- 9.Mahe YF, Perez MJ, Tacheau C, et al. A new Vitreoscilla filiformis extract grown on spa water-enriched medium activates endogenous cutaneous antioxidant and antimicrobial defenses through a potential Toll-like receptor 2/protein kinase C, zeta transduction pathway. Clin Cosmet Investig Dermatol. 2013;6:191–196. doi: 10.2147/CCID.S47324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goh CL, Tang MB, Briantais P, et al. Adapalene gel 0.1% is better tolerated than tretinoin gel 0.025% among healthy volunteers of various ethnic origins. J Dermatolog Treat. 2009;20:282–288. doi: 10.1080/09546630902763164. [DOI] [PubMed] [Google Scholar]
- 11.Abad-Casintahan F, Chow SK, Goh CL, et al. Frequency and characteristics of acne-related post-inflammatory hyperpigmentation. J Dermatol. 2016;43:826–8. [DOI] [PubMed]
- 12.Hayashi N, Miyachi Y, Kawashima M. Prevalence of scars and “mini-scars”, and their impact on quality of life in Japanese patients with acne. J Dermatol. 2015;42:690–696. doi: 10.1111/1346-8138.12885. [DOI] [PubMed] [Google Scholar]
- 13.Boonchaya P, Rojhirunsakool S, Kamanamool N, et al. Minimum contact time of 1.25%, 2.5%, 5%, and 10% benzoyl peroxide for a bactericidal effect against Cutibacterium acnes. Clin Cosmet Investig Dermatol. 2022;15:403–409. doi: 10.2147/CCID.S359055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tan J, Bissonnette R, Gratton D, et al. The safety and efficacy of four different fixed combination regimens of adapalene 0.1%/benzoyl peroxide 2.5% gel for the treatment of acne vulgaris: results from a randomised controlled study. Eur J Dermatol. 2018;28:502–508. doi: 10.1684/ejd.2018.3367. [DOI] [PubMed] [Google Scholar]
- 15.Data on file. La Roche Posay 2022.
- 16.Dreno B. What is new in the pathophysiology of acne, an overview. J Eur Acad Dermatol Venereol. 2017;31(Suppl 5):8–12. doi: 10.1111/jdv.14374. [DOI] [PubMed] [Google Scholar]
- 17.Dagnelie MA, Corvec S, Timon-David E, et al. Cutibacterium acnes and Staphylococcus epidermidis: the unmissable modulators of skin inflammatory response. Exp Dermatol. 2022;31:406–412. doi: 10.1111/exd.14467. [DOI] [PubMed] [Google Scholar]
- 18.Marson J, Bhatia N, Graber E, et al. The role of epidermal barrier dysfunction and cutaneous microbiome dysbiosis in the pathogenesis and management of acne vulgaris and rosacea. J Drugs Dermatol. 2022;21:SF3502915-SF35029114. doi: 10.36849/JDD.m0922. [DOI] [PubMed] [Google Scholar]
- 19.Yamamoto A, Takenouchi K, Ito M. Impaired water barrier function in acne vulgaris. Arch Dermatol Res. 1995;287:214–218. doi: 10.1007/BF01262335. [DOI] [PubMed] [Google Scholar]
- 20.Pappas A, Kendall AC, Brownbridge LC, et al. Seasonal changes in epidermal ceramides are linked to impaired barrier function in acne patients. Exp Dermatol. 2018;27:833–836. doi: 10.1111/exd.13499. [DOI] [PubMed] [Google Scholar]
- 21.See JA, Goh CL, Hayashi N, et al. Optimizing the use of topical retinoids in Asian acne patients. J Dermatol. 2018;45:522–528. doi: 10.1111/1346-8138.14314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ito Y, Amagai M. Controlling skin microbiome as a new bacteriotherapy for inflammatory skin diseases. Inflamm Regen. 2022;42:26. doi: 10.1186/s41232-022-00212-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marson J, Baldwin H. Dysbiosis, (barrier) dysfunction, and dermatoses: a chicken-and-egg dilemma. J Drugs Dermatol. 2022;21:SF3502913-SF4. doi: 10.36849/JDD.M0922. [DOI] [PubMed] [Google Scholar]
- 24.Lee YB, Byun EJ, Kim HS. Potential role of the microbiome in acne: a comprehensive review. J Clin Med 2019;8(7):987. [DOI] [PMC free article] [PubMed]
- 25.Dreno B, Dagnelie MA, Khammari A, et al. The skin microbiome: a new actor in inflammatory acne. Am J Clin Dermatol. 2020;21:18–24. doi: 10.1007/s40257-020-00531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fitz-Gibbon S, Tomida S, Chiu BH, et al. Propionibacterium acnes strain populations in the human skin microbiome associated with acne. J Invest Dermatol. 2013;133:2152–2160. doi: 10.1038/jid.2013.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dagnelie MA, Corvec S, Saint-Jean M, et al. Cutibacterium acnes phylotypes diversity loss: a trigger for skin inflammatory process. J Eur Acad Dermatol Venereol. 2019;33:2340–2348. doi: 10.1111/jdv.15795. [DOI] [PubMed] [Google Scholar]
- 28.Barnard E, Liu J, Yankova E, et al. Strains of the Propionibacterium acnes type III lineage are associated with the skin condition progressive macular hypomelanosis. Sci Rep. 2016;6:31968. doi: 10.1038/srep31968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Z, Choi JE, Wu CC, et al. Skin commensal bacteria Staphylococcus epidermidis promote survival of melanocytes bearing UVB-induced DNA damage, while bacteria Propionibacterium acnes inhibit survival of melanocytes by increasing apoptosis. Photodermatol Photoimmunol Photomed. 2018;34:405–414. doi: 10.1111/phpp.12411. [DOI] [PubMed] [Google Scholar]
- 30.Korting HC, Ponce-Poschl E, Klovekorn W, et al. The influence of the regular use of a soap or an acidic syndet bar on pre-acne. Infection. 1995;23:89–93. doi: 10.1007/BF01833872. [DOI] [PubMed] [Google Scholar]
- 31.Schmid-Wendtner MH, Korting HC. The pH of the skin surface and its impact on the barrier function. Skin Pharmacol Physiol. 2006;19:296–302. doi: 10.1159/000094670. [DOI] [PubMed] [Google Scholar]
- 32.Dreno B, Thiboutot D, Layton AM, et al. Large-scale international study enhances understanding of an emerging acne population: adult females. J Eur Acad Dermatol Venereol. 2015;29:1096–1106. doi: 10.1111/jdv.12757. [DOI] [PubMed] [Google Scholar]
- 33.Jones-Caballero M, Pedrosa E, Penas PF. Self-reported adherence to treatment and quality of life in mild to moderate acne. Dermatology. 2008;217:309–314. doi: 10.1159/000151441. [DOI] [PubMed] [Google Scholar]
- 34.Sevimli DB. Topical treatment of acne vulgaris: efficiency, side effects, and adherence rate. J Int Med Res. 2019;47:2987–2992. doi: 10.1177/0300060519847367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cannizzaro MV, Dattola A, Garofalo V, et al. Reducing the oral isotretinoin skin side effects: efficacy of 8% omega-ceramides, hydrophilic sugars, 5% niacinamide cream compound in acne patients. G Ital Dermatol Venereol. 2018;153:161–164. doi: 10.23736/S0392-0488.17.05742-X. [DOI] [PubMed] [Google Scholar]
- 36.Chularojanamontri L, Tuchinda P, Kulthanan K, et al. A double-blinded, randomized, vehicle-controlled study to access skin tolerability and efficacy of an anti-inflammatory moisturizer in treatment of acne with 0.1% adapalene gel. J Dermatolog Treat. 2016;27:140–145. doi: 10.3109/09546634.2015.1079298. [DOI] [PubMed] [Google Scholar]
- 37.Draelos ZD BN, Colon G, Dreno B. The effect of ceramide-containing skincare on acne medication-induced barrier dysfunction. Eur Acad Dermatol Venereol. 2021.
- 38.Schorr ES, Sidou F, Kerrouche N. Adjunctive use of a facial moisturizer SPF 30 containing ceramide precursor improves tolerability of topical tretinoin 0.05%: a randomized, investigator-blinded, split-face study. J Drugs Dermatol. 2012;11:1104–1107. [PubMed] [Google Scholar]
- 39.Kerob D, Demessant AL, LeDantec G, et al. Benefits of a dermocosmetic regime in the management of local cutaneous intolerance induced by a gel based on retinoids for acne, previously mitigated inadequately, with adjunct routine skin care. In: RADLA: Reunion Anual de Dermatologos Latinoamericanos. Chile, virtual; 2022.
- 40.Del Rosso JQ, Gold M, Rueda MJ, et al. Efficacy, safety, and subject satisfaction of a specified skin care regimen to cleanse, medicate, moisturize, and protect the skin of patients under treatment for acne vulgaris. J Clin Aesthet Dermatol. 2015;8:22–30. [PMC free article] [PubMed] [Google Scholar]
- 41.Monfrecola G, Capasso C, Russo G, et al. UV-selective face cream (Acne RA-1,2) in acne patients: clinical study of its effects on epidermal barrier function, sebum production, tolerability and therapy adherence. G Ital Dermatol Venereol. 2018;153:26–32. doi: 10.23736/S0392-0488.16.05384-0. [DOI] [PubMed] [Google Scholar]
- 42.Zeichner JA, Patel RV, Haddican M, et al. Efficacy and safety of a ceramide containing moisturizer followed by fixed-dose clindamycin phosphate 1.2%/benzoyl peroxide 2.5% gel in the morning in combination with a ceramide containing moisturizer followed by tretinoin 0.05% gel in the evening for the treatment of facial acne vulgaris. J Drugs Dermatol. 2012;11:748–752. [PubMed] [Google Scholar]
- 43.Dreno B, Khammari A, Duhamel K, et al. A dermocosmetic associated with a fixed combination of adapalene 0.1% and benzoyl peroxide 5% helps to protect the skin barrier in mild to moderate acne. In: American Academy of Dermatology. San Francisco, CA virtual 2021.
- 44.Del Rosso JQ, Brandt S. The role of skin care as an integral component in the management of acne vulgaris: Part 2: tolerability and performance of a designated skin care regimen using a foam wash and moisturizer SPF 30 in patients with acne vulgaris undergoing activetreatment. J Clin Aesthet Dermatol. 2013;6:28–36. [PMC free article] [PubMed] [Google Scholar]
- 45.Tan J. In: Eur Acad Dermatol and Venereol Annual Meeting; 2022.
- 46.Lam M, Hu A, Fleming P, et al. The impact of acne treatment on skin bacterial microbiota: a systematic review. J Cutan Med Surg. 2022;26:93–97. doi: 10.1177/12034754211037994. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed for the current publication. Data will be accessible on request and after study by the sponsor of the study. The sponsor reserves the right to refuse if the objective is not admissible. Upon provision, a secure link will be provided.