Abstract
Background
Low- and middle-income countries account for most of the global burden of coronary artery disease. There is a paucity of data regarding epidemiology and outcomes for ST-segment elevation myocardial infarction (STEMI) patients in these regions.
Objectives
The authors studied the contemporary characteristics, practice patterns, outcomes, and sex differences in patients with STEMI in India.
Methods
NORIN-STEMI (North India ST-Segment Elevation Myocardial Infarction Registry) is an investigator-initiated prospective cohort study of patients presenting with STEMI at tertiary medical centers in North India.
Results
Of 3,635 participants, 16% were female patients, one-third were <50 years of age, 53% had a history of smoking, 29% hypertension, and 24% diabetes. The median time from symptom onset to coronary angiography was 71 hours; the majority (93%) presented first to a non-percutaneous coronary intervention (PCI)-capable facility. Almost all received aspirin, statin, P2Y12 inhibitors, and heparin on presentation; 66% were treated with PCI (98% femoral access) and 13% received fibrinolytics. The left ventricular ejection fraction was <40% in 46% of patients. The 30-day and 1-year mortality rates were 9% and 11%, respectively. Compared with male patients, female patients were less likely to receive PCI (62% vs 73%; P < 0.0001) and had a more than 2-fold greater 1-year mortality (22% vs 9%; adjusted HR: 2.1; 95% CI: 1.7-2.7; P < 0.001).
Conclusions
In this contemporary registry of patients with STEMI in India, female patients were less likely to receive PCI after STEMI and had a higher 1-year mortality compared with male patients. These findings have important public health implications, and further efforts are required to reduce these gaps.
Key Words: cardiovascular disease, disparities, female patients, sex differences, STEMI
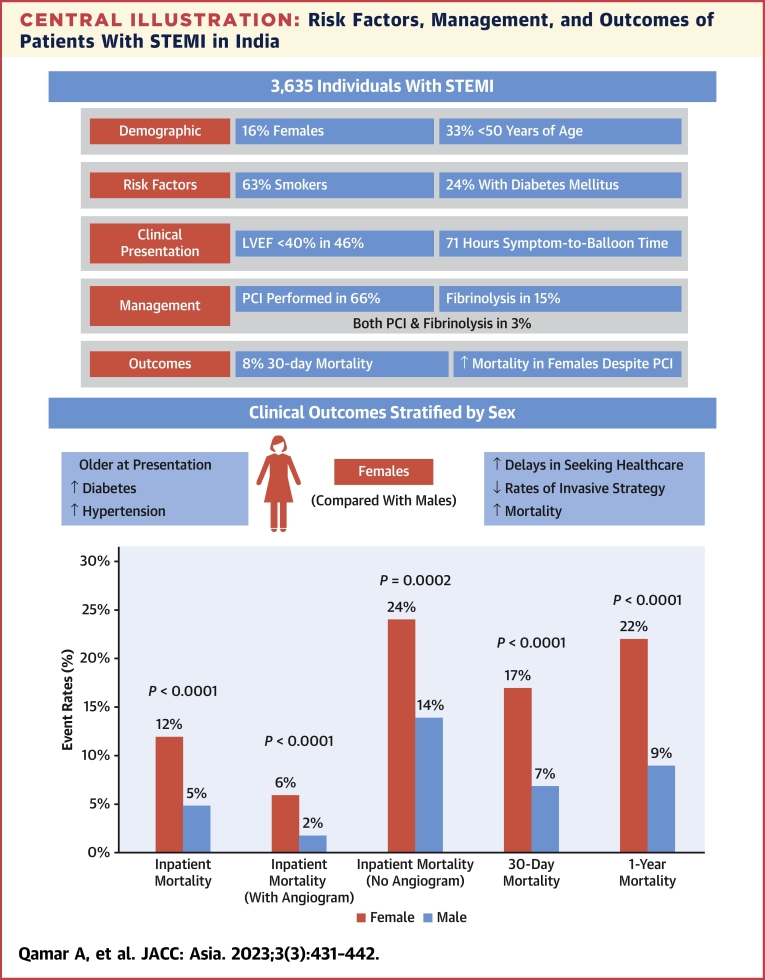
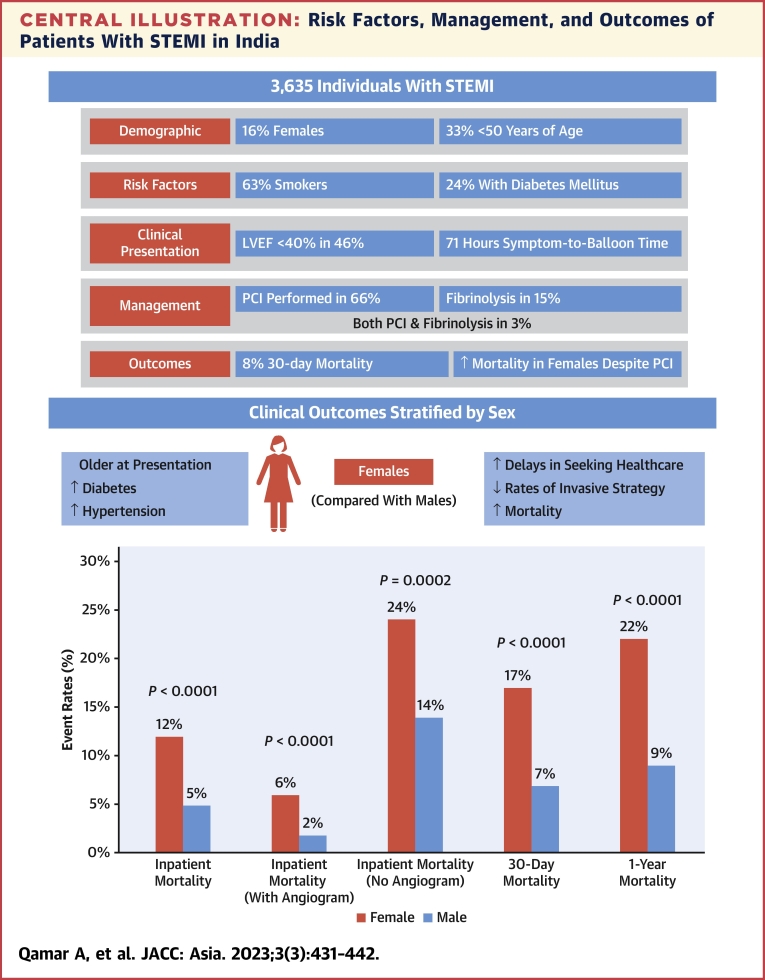
Central Illustration
In the last 2 decades, low- and middle-income countries such as India have seen an epidemiological transition in disease burden from infectious diseases to atherosclerotic cardiovascular diseases (ASCVD). India now accounts for a major percentage of the global ASCVD burden, and has more annual ASCVD deaths than any other country in the world.1, 2, 3 ST-segment elevation myocardial infarction (STEMI), a common and dreaded manifestation of ASCVD has historically been associated with high rates of mortality. High-income countries have adopted and effectively implemented strategies such as reducing door to balloon time, which have dramatically improved outcomes in patients with STEMI.4 These strategies remain elusive for countries like India, despite an alarming increase in the incidence of STEMI.5 Additionally, awareness about prevention of ASCVD, early recognition, and timely management of STEMI continues to lag behind other priorities in India. Public health care expenditure for treatment and research remains miniscule, and the majority of the population continues to spend out of pocket when faced with acute health emergencies such as STEMI.5, 6, 7
Cardiovascular disease has long been seen as a disease primarily affecting male patients, but the proportional burden of STEMI in female patients has increased in the last 2 decades.8 Despite this trend, female patients were less likely to receive timely care or undergo evidence-based invasive procedures after STEMI8, 9, 10 and are less likely to receive guideline-directed medical therapies, resulting in higher mortality rates in the setting of STEMI, even in high-income countries.10, 11, 12, 13, 14 Such sex disparities in receiving quality care for STEMI may be exaggerated in India.7,15,16 The present study aims to improve our understanding of contemporary risk factor profiles, patterns of presentation, clinical management, and outcomes of patients with STEMI in this population, and further stratify these by sex.
Methods
Study Population
The design and rationale of the NORIN-STEMI (North India ST-Segment Elevation Myocardial Infarction Registry) have been described previously.17 In brief, the NORIN-STEMI registry is a prospective study of patients hospitalized with STEMI in India. The registry enrolled all consenting patients >18 years of age who present at either Gobind Ballabh Pant Institute of Postgraduate Medical Education and Research and Janakpuri Superspecialty Hospital in New Delhi, India. Both hospitals have PCI capabilities and are government funded, providing cardiovascular care largely free of cost to patients. Therefore, they are 2 major cardiac centers serving many surrounding states in the region, including Delhi, Haryana, Punjab, Uttar Pradesh, Madhya Pradesh, Bihar, and the North-Eastern States.
Enrollment
The study protocol was approved by the Institutional Review Board at both institutions. All adults ≥18 years of age presenting with STEMI to 2 tertiary medical centers in Delhi from January 1, 2019, to February 2020 participated in this registry. Written informed consent was obtained from patients or next of kin if the patient lacked decisional capacity. ST-segment elevation was defined by the European Society of Cardiology/American College of Cardiology/American Heart Association/World Heart Federation Task Force for the fourth Universal Definition of Myocardial Infarction as new ST-segment elevation at the J point in at least 2 contiguous leads of ≥2.0 mm in male patients or ≥1.5 mm in female patients in leads V2 to V3 and/or of ≥1 mm in other contiguous chest leads or limb leads.18 Patients presenting ≥21 days after symptom onset were excluded.
Data Ascertainment
Baseline demographics were reported by patients and included mode of transportation to the hospital, education, occupation, diet, physical activity, sleep, stress, socioeconomic status, and health care coverage. Family history of coronary artery disease was defined as a myocardial infarction (MI) or coronary revascularization in any first-degree relative; premature coronary artery disease was defined as the above before 55 years of age in male patients and 65 years of age in female patients. Risk factors were first evaluated by detailed medical record review and self-report; prior diagnosis and treatment for all risk factors was ascertained. Chronic kidney disease was defined by an estimated glomerular filtration rate of <60 mL/min/m2 before admission. History of smoking was categorized as current (within the last month), former, or never; pack-years were calculated. To account for missed screening opportunities, several risk factors were also evaluated on presentation. Hypertension was defined as systolic blood pressure of ≥140 mm Hg and a diastolic blood pressure of ≥90 mm Hg. Dyslipidemia was defined per National Cholesterol Education Plan criteria as a total cholesterol of ≥240 mg/dL, serum triglycerides of ≥150 mg/dL, or high-density lipoprotein cholesterol of <40 mg/dL in male patients or <50 mg/dL in female patients.19 Diabetes mellitus (DM) was defined as a glycated hemoglobin of ≥6.5%. A medication reconciliation was completed and use of lipid-lowering medications, antihypertensives, oral or intramuscular DM medications, and insulin was recorded.
On presentation, patients self-reported clinical symptoms, duration of symptoms, preceding activity, time since symptom onset, and location of first evaluation. Objective vitals including height, weight, heart rate, and blood pressure were recorded. Licensed physicians in the departments of cardiology interpreted presenting electrocardiographs and determined MI territory (anterior, lateral, inferior, posterior). Guideline-directed acute coronary syndrome (ACS) therapy including aspirin, statin, beta-blocker, anticoagulation, and P2Y12 inhibitor use were documented both in-hospital and on discharge. In-hospital thrombolytic use was also recorded. Each patient received an echocardiogram on presentation, which was evaluated for regional wall motion abnormalities, left ventricular ejection fraction, mitral regurgitation grade, and mechanical complications such as papillary muscle rupture, acute mitral regurgitation, interventricular septum rupture, ventricular septal defect, cardiac tamponade, and left ventricular aneurysm by experienced cardiologists. Laboratory values collected at presentation included creatinine, hemoglobin, hemoglobin A1c, total cholesterol, calculated low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and triglycerides.
Clinical events of interest included use of coronary angiography, PCI, and mortality. Findings of angiography were interpreted by licensed cardiologists and included the number of diseased vessels, infarct-related artery (arteries), and infarct territory. Complications of interest related to STEMI were repeat infarction, mechanical ventilation, dialysis, ventricular arrhythmias, bleeding, cardiogenic shock, in-hospital mortality, and PCI-related complications, such as stent thrombosis, stroke, access site complications, and contrast-induced nephropathy. Mechanical complications were also assessed with echocardiogram as described elsewhere in this article.
All study participants were followed at 30 days and 1 year via prospective telephone calls and/or in-clinic follow-up visits, as well as a detailed medical record review. Mortality, adherence to guideline-directed therapies, smoking cessation, rehospitalization, and complications such as stent thrombosis, contrast nephropathy, bleeding, stroke, reinfarction, and reintervention via PCI or coronary artery bypass grafting were evaluated.
Outcomes and Definitions
For the present study, primary outcomes of interest included in-hospital, 30-day, and 1-year mortality. Sex was self-reported. Outcomes were collected by phone call, in-office visit, or through a detailed review of medical records. Cardiovascular risk factors were identified via history or by laboratory findings at presentation. Dyslipidemia and DM were defined on history or presentation, as descried elsewhere in this article.
Statistical Analysis
Descriptive statistics were used to evaluate the distributions of continuous variables and frequencies of categorical variables. Bivariable comparisons were performed between female patients and male patients using analysis of variance, Kruskal-Wallis test, chi-square test, and Fisher exact test where appropriate.
We developed a multivariable logistic regression model to identify predictors of in-hospital and 30-day mortality. Characteristics of interest were identified both a priori and by bivariable analyses and adjusted OR and the corresponding 95% CIs were reported. Potential predictors included age, sex, location of first presentation (PCI capable vs referral site), dietary status, physical activity, socioeconomic status, substance use, time from symptom onset to health care contact, PCI, history of diabetes, hypertension, atrial fibrillation, congestive heart failure, stroke, MI, coronary artery bypass grafting, peripheral artery disease, and baseline use of medications. Additionally, a multivariable Cox proportional hazards model was then used to examine the association of female sex with mortality to 1 year, and multivariable logistic regression evaluated the association of female sex with other outcomes of interest. Both models were adjusted for age, history of hypertension, DM (established or newly detected), heart failure, prior MI, prior cerebrovascular accident, tobacco use, and obesity. The proportional hazards assumption was assessed using the Supremum test as well as visually examined Schoenfeld residuals. All analyses were performed using SAS 9.4 (SAS Institute).
Results
Baseline Characteristics of Patients with STEMI
A total of 3635 patients were enrolled in the registry from January 2019 to February 2020, of whom 582 (16%) were female patients and 3053 (84%) were male patients. The median age of enrolled patients was 55 years (IQR: 45-62 years) and 51% self-reported illiteracy. A history of hypertension was present in 29%, diabetes in 24%, and obesity in 11%. A total of 53% used tobacco products including cigarettes, beedi, and/or hookah at the time of presentation. Before their presentation with STEMI, 11% reported daily aspirin use and 11% were on statins. Female patients were older (median age 60 years vs 53 years) and more likely to have a history of diabetes, hypertension, obesity, and illiteracy compared with male patients. Female patients were less likely to use tobacco, drink alcohol, or be physically active. Baseline characteristics of patients enrolled in the registry stratified by sex are shown in Table 1.
Table 1.
Baseline Characteristics of Patients in the NORIN-STEMI Registry, Stratified by Sex
| All (N = 3,635) | Female (n = 582,16%) | Male (n = 3,053,84%) | P Value (2-Sided) | |
|---|---|---|---|---|
| Age, y | 55 (45-62) | 60 (52-65) | 53 (45-60) | <0.0001 |
| ≥60 | 1,336 (37) | 325 (56) | 1,011 (33) | |
| 50-59 | 1,106 (30) | 147 (25) | 959 (31) | <0.0001 |
| 40-49 | 874 (24) | 95 (16) | 779 (26) | |
| <40 | 319 (9) | 15 (3) | 304 (10) | |
| Medical history | ||||
| Diabetes mellitus | 855 (24) | 215 (37) | 640 (21) | <0.0001 |
| Hypertension | 1,039 (29) | 264 (45) | 775 (25) | <0.0001 |
| Cancer | 7 (0) | 0 (0) | 7 (0) | 0.60 |
| Atrial fibrillation | 76 (2) | 8 (1) | 68 (2) | 0.19 |
| Hemodialysis | 1 (0) | 0 (0) | 1 (0) | 0.99 |
| Heart failure | 38 (1) | 9 (2) | 29 (1) | 0.19 |
| Dyslipidemia | 77 (2) | 17 (3) | 60 (2) | 0.14 |
| Prior cerebrovascular accident | 43 (1) | 5 (1) | 38 (1) | 0.43 |
| Prior myocardial infarction | 443 (12) | 64 (11) | 379 (12) | 0.34 |
| Prior CABG | 6 (0) | 0 (0) | 6 (0) | 0.60 |
| Peripheral artery disease | 4 (0) | 0 (0) | 4 (0) | 0.99 |
| Tobacco use | ||||
| Never | 1,349 (37) | 486 (84) | 863 (28) | <0.0001 |
| Former | 272 (7) | 17 (3) | 255 (8) | |
| Current, some days | 103 (3) | 11 (2) | 92 (3) | |
| Current, every day | 1,909 (53) | 67 (12) | 1,842 (60) | |
| Physical activity | ||||
| Yes | 482 (13) | 49 (8) | 433 (14) | 0.0002 |
| BMI | ||||
| Underweight (<18.5 kg/m2) | 90 (2) | 28 (5) | 62 (2) | <0.0001 |
| Normal body weight (18.5-25 kg/m2) | 1,564 (43) | 260 (45) | 1,304 (43) | |
| Overweight (25-30 kg/m2) | 1,565 (43) | 202 (35) | 1,363 (45) | |
| Obese (>30 kg/m2) | 416 (11) | 92 (16) | 324 (11) | |
| Socioeconomic factors | ||||
| Education | ||||
| College graduate | 271 (7) | 16 (3) | 255 (8) | <0.0001 |
| High school | 557 (15) | 33 (6) | 524 (17) | |
| Middle school | 951 (26) | 93 (16) | 858 (28) | |
| No formal education | 1,856 (51) | 440 (76) | 1416 (46) | |
| Insurance, self-pay | 3,578 (98) | 577 (99) | 3,001 (98) | 0.12 |
| Income quartile | ||||
| Upper middle | 96 (3) | 11 (2) | 85 (3) | 0.51 |
| Lower middle | 1,184 (33) | 195 (34) | 989 (32) | |
| Upper lower | 1,369 (38) | 226 (39) | 1,143 (37) | |
| Lower | 983 (27) | 150 (26) | 833 (27) | |
| Alcohol | ||||
| Never | 2,737 (75) | 575 (98) | 2,162 (71) | <0.0001 |
| Former | 183 (5) | 1 (0) | 182 (6) | |
| Current, some days | 393 (11) | 6 (1) | 387 (13) | |
| Current, every day | 322 (9) | 0 (0) | 322 (11) | |
| Medications at baseline | ||||
| Aspirin | 389 (11) | 56 (10) | 333 (11) | 0.36 |
| Statin | 386 (11) | 57 (10) | 329 (11) | 0.48 |
| Beta-blocker | 467 (13) | 83 (13) | 384 (13) | 0.27 |
| ACE inhibitor/ARB | 447 (12) | 90 (16) | 357 (12) | 0.01 |
| Calcium channel blocker | 194 (5) | 56 (10) | 138 (5) | <0.0001 |
Values are median (IQR) or n (%).
ACE = angiotensin converting enzyme inhibitors; ARB = angiotensin receptor blockers; BMI = body mass index; CABG = coronary artery bypass grafting; NORIN-STEMI = North India ST-Segment Elevation Myocardial Infarction Registry.
Clinical Presentation and Management
Clinical presentation and in-hospital characteristics are summarized in Table 2 and Supplemental Table 1. Most patients (64%) made health care contact within 1 hour of symptom onset; however, 93% first presented to a non-PCI-capable hospital and were subsequently referred to PCI-capable centers. On arrival, nearly 100% of patients received aspirin, a statin, and a P2Y12 inhibitor (Supplemental Table 2). Laboratory tests at presentation revealed that most of the patients (78%) had dyslipidemia. Female patients were more likely to present with lipid profiles diagnostic of dyslipidemia than male patients (89% vs 76%; P < 0.001). Anterior wall MI was the most common type of MI by electrocardiogram for both sexes (51% vs 54%; P = 0.39). On echocardiogram, 46% of patients had an ejection fraction of <40% with no differences by sex (40% vs 37%; P = 0.40), and 79% had regional wall motion abnormalities, also without any sex difference (78% vs 80%; P = 0.40).
Table 2.
Details of Presentations of Patients in the NORIN-STEMI Registry, Stratified by Sex
| All (N = 3,635) | Female (n = 582,16%) | Male (n = 3,053,84%) |
P Value (2-Sided) |
|
|---|---|---|---|---|
| Presentation | ||||
| Direct | 242 (7) | 38 (7) | 204 (7) | 0.89 |
| Referral | 3,393 (93) | 544 (93) | 2,849 (93) | |
| Mode of transport | ||||
| Ambulance | 190 (5) | 36 (6) | 154 (5) | 0.007 |
| Public transport | 1,346 (37) | 244 (42) | 1,102 (36) | |
| Self/family | 2,099 (58) | 302 (52) | 1,797 (59) | |
| Location of first evaluation | ||||
| Non-PCI center (clinic) | 573 (16) | 91 (16) | 482 (16) | 0.55 |
| Non-PCI center (hospital) | 2,801 (77) | 443 (76) | 2,359 (77) | |
| PCI center | 261 (7) | 48 (8) | 213 (7) | |
| Symptoms onset to first health care contact | ||||
| <1 h | 2,309 (64) | 344 (59) | 1,965 (64) | 0.03 |
| 1-3 h | 516 (14) | 90 (15) | 426 (14) | |
| 3-12 h | 362 (10) | 58 (10) | 304 (10) | |
| 12-24 h | 150 (4) | 26 (4) | 124 (4) | |
| ≥24 h | 285 (8) | 63 (11) | 222 (7) | |
| Reason for delaya | ||||
| Lack of transport | 382 (29) | 71 (30) | 311 (29) | 0.84 |
| Patient/relative unwillingness | 177 (14) | 35 (15) | 142 (13) | |
| Misinterpretation of symptoms | 597 (46) | 104 (44) | 493 (46) | |
| Transient resolution of symptoms | 152 (12) | 25 (11) | 127 (12) | |
| MI type on electrocardiogram | ||||
| Anterior wall MI | 1,975 (54) | 296 (51) | 1,679 (55) | 0.391 |
| Inferior wall MI | 1,553 (43) | 265 (46) | 1,288 (42) | |
| Lateral wall MI | 39 (1) | 11 (2) | 28 (1) | 0.52 |
| Posterior wall MI | 16 (0) | 2 (0) | 14 (0) | |
| Ventricular fibrillation | 24 (1) | 9 (2) | 15 (0) | 0.004 |
| Hours from admission to catheter laboratory arrival | 8 (1-27) | 4 (1-26) | 8 (1-28) | 0.720 |
Values are n (%) or median (IQR).
MI = myocardial infarction; PCI = percutaneous coronary intervention; other abbreviation as in Table 1.
Not available for 2327 patients.
Coronary angiography was performed in 72% of patients. Female patients were significantly less likely to undergo coronary angiography (62% vs 73%; P < 0.0001) and PCI (58% vs 67%; adjusted OR: 1.46; 95% CI: 1.18-1.81; P = 0.0005) than male patients. Most had single vessel disease (68%) and the left anterior descending artery was the most common culprit vessel (55%). PCI was performed in 66% of the overall population. The median time from symptom onset to coronary angiography was 71 hours (IQR: 15-217 hours). Culprit vessels and the number of vessels with significant stenosis on angiography did not differ between the sexes. All patients were discharged on dual antiplatelets, statin and beta-blockers. Clopidogrel was the most common P2Y12 inhibitor used and medications at discharge did not differ between male patients and female patients (Table 3).
Table 3.
Procedural Details and Discharge Medications of Patients in the NORIN-STEMI Registry, Stratified by Sex
| All (N = 3,635) | Female Patients(n = 582,16%) | Male Patients (n = 3,053,84%) | P Value (2-Sided) | |
|---|---|---|---|---|
| Angiography | 2,600 (72) | 361 (62) | 2,239 (73) | <0.0001 |
| Arterial access site | ||||
| Femoral | 2,506 (98) | 349 (97) | 2,157 (98) | 0.621 |
| Radial | 62 (2) | 10 (3) | 52 (2) | |
| Culprit vessels | ||||
| LMCA | 7 (0) | 2 (1) | 5 (0) | 0.539 |
| LAD | 1,103 (55) | 139 (52) | 964 (56) | |
| RCA | 670 (34) | 93 (35) | 577 (33) | |
| LCx | 211 (11) | 34 (13) | 177 (10) | |
| No. of vessels | ||||
| Normal | 28 (1) | 2 (1) | 26 (1) | 0.167 |
| Single-vessel disease | 1,761 (68) | 237 (66) | 1,524 (68) | |
| Double-vessel disease | 600 (23) | 83 (23) | 517 (23) | |
| Triple-vessel disease | 211 (8) | 39 (11) | 172 (8) | |
| PCI | 2,381 (66) | 337 (58) | 2,044 (67) | <0.0001 |
| Thrombolytics | 474 (13) | 94 (16) | 380 (12) | 0.02 |
| Time from symptom onset to PCI | ||||
| ≤12 h | 350 (18) | 56 (20) | 294 (17) | 0.522 |
| 12-24 h | 283 (14) | 37 (13) | 246 (15) | |
| 24-72 h | 240 (12) | 39 (14) | 201 (12) | |
| >72 h | 1,089 (56) | 149 (53) | 940 (56) | |
| Discharge medications | ||||
| Aspirin | 3,353 (100) | 497 (100) | 2,856 (100) | 0.999 |
| Statin | 3,339 (100) | 495 (100) | 2,844 (100) | 0.999 |
| P2Y12 inhibitors | 3,338 (99) | 494 (99) | 2,844 (100) | 0.730 |
| Prasugrel | 21 (1) | 2 (0) | 19 (1) | <0.0001 |
| Clopidogrel | 3255 (97) | 474 (95) | 2781 (97) | |
| Ticagrelor | 62 (2) | 18 (4) | 44 (2) | |
| Beta-blocker | 3,298 (98) | 487 (98) | 2,811 (98) | 0.558 |
| ACE/ARB | 2,961 (88) | 428 (86) | 2,533 (89) | 0.108 |
Mortality
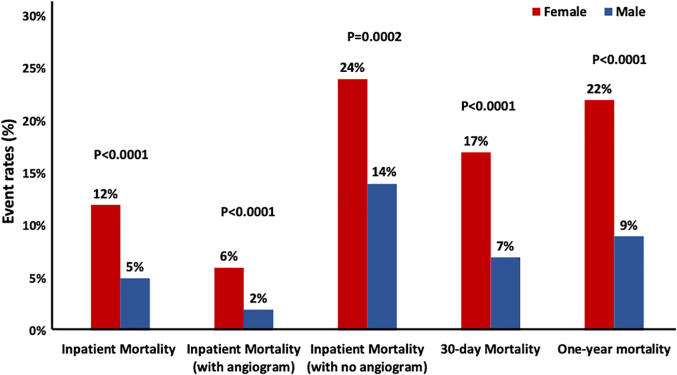
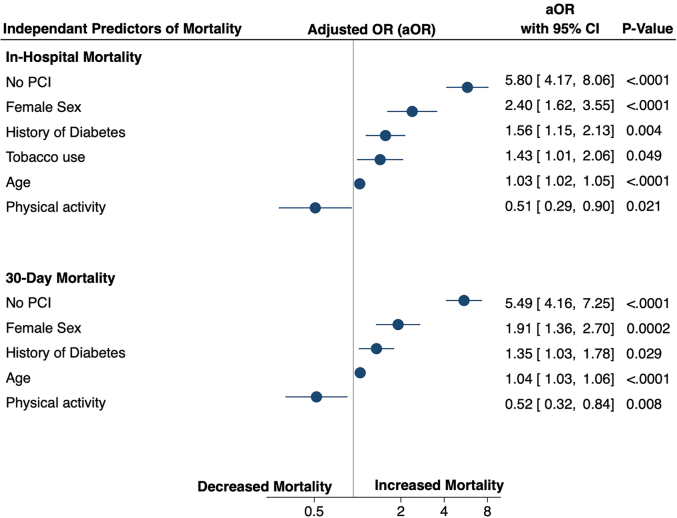
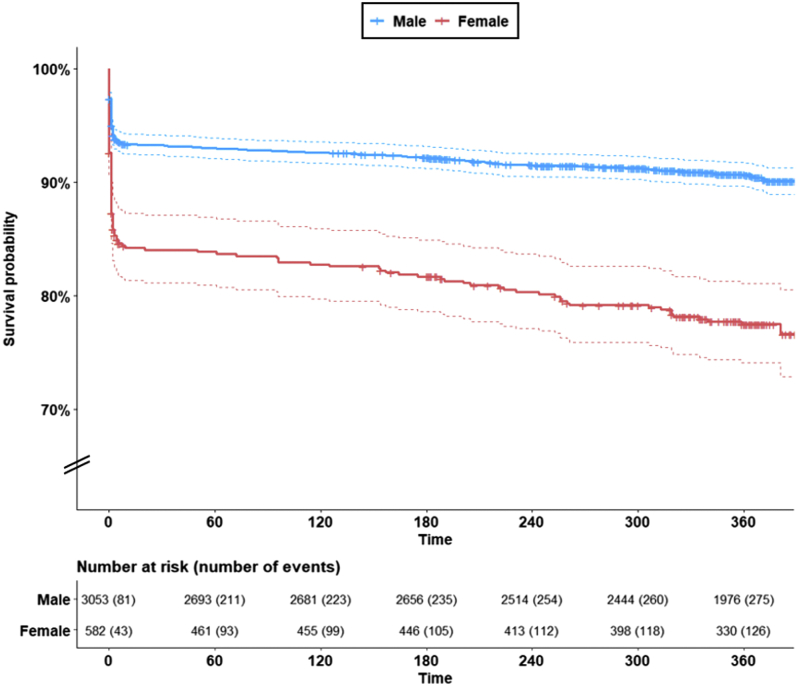
Overall, 216 patients (6%) died during the index hospitalization, 296 (8%) at 30 days, and 410 (11%) at 1 year. The overall rates of inpatient mortality were significantly higher in female patients than in male patients (12% vs 5%; P < 0.0001) (Figure 1). The multivariable regression model identified several risk factors that independently affected inpatient and 30-day mortality (Figure 2). Among these risk factors, lack of revascularization with PCI and being a female patients emerged as the strongest predictors of inpatient and 30-day mortality. The multivariable Cox proportional hazards model further revealed that, even after adjustment for other clinical variables, female patients were twice as likely to die at 1 year after STEMI as compared with male patients (22% vs 9%; adjusted HR: 2.1; 95% CI: 1.7-2.7; P < 0.001) (Figure 3).
Figure 1.
Sex Differences in Clinical Outcomes for Patients With STEMI in India
Event rates for inpatient, 30-day and 1-year mortality stratified by sex. The overall rates of inpatient mortality were significantly higher in female patients than in male patients. Female patients also experienced higher 30-day and 1 year mortality compared with male patients. STEMI = ST-segment elevation myocardial infarction.
Figure 2.
Independent Predictors of In-Hospital and 30-Day Mortality
A multivariable logistic regression model was used to identify predictors of in-hospital and 30-day mortality. Treatment without PCI was the strongest predictor of inpatient mortality, followed by female sex, history of diabetes, tobacco use, and advancing age. Self-reported physical activity was protective. At 30 days, independent predictors of mortality remained largely unchanged. PCI = percutaneous coronary intervention.
Figure 3.
Sex Differences in Mortality in Patients With STEMI in India
A multivariable Cox proportional hazards model was used to generate the survival curves demonstrating the difference in mortality between male patients and female patients presenting with STEMI to tertiary centers in Northern India. Relative to male patients, female patients were twice as likely to die at 1 year after follow-up (adjusted HR: 2.1; 95% CI: 1.7-2.7; P < 0.0001). Abbreviations as in Figures 1 and 2.
Discussion
The present study is the largest contemporary prospective registry evaluating the epidemiology, management patterns, and outcomes of STEMI in an underserved population in Northern India (Central Illustration). Female patients comprised only 16% of our patients. Compared with contemporary data from the United States and Europe or even with prior registry studies from Southern India, the median age in our population was younger and smoking rates were much higher. The prevalence of hypertension, dyslipidemia, and diabetes among patients with STEMI have remained stagnant over the last decade7,20 and highlights the lack of identification and undertreatment of traditional risk factors before presentation. The majority of patients (93%) initially presented to non-PCI-capable facilities, resulting in significant delays during transfer from time of symptom onset to arrival at the PCI-capable centers. These transfer delays resulted in high rates of post-STEMI left ventricular systolic dysfunction and mechanical complications. Only two-thirds of patients received PCI, largely owing to delays in transfer to tertiary facilities and 1-year mortality rates are still higher compared with current data from the United States and Europe. Compared with male patients, female patients were older, were more likely to have diabetes and hypertension, faced longer delays from symptom onset to first health care contact, were significantly less likely to receive PCI, and had a 2-fold increased risk of mortality.
Central Illustration.
Risk Factors, Management, and Outcomes of Patients With STEMI in India
The present analysis provides a contemporary insight into the epidemiology, management pattern and outcomes of STEMI in Northern India. There were 3,635 patients enrolled in the registry and female patients comprised 16% of the total population. Relative to male patients, female patients had a higher comorbidity burden, longer delays in accessing health care with lower rates of invasive management and higher inpatient as well as 1-year mortality. PCI = percutaneous coronary intervention; STEMI = ST-segment elevation myocardial infarction.
Compared with previous registry studies of ACS patients in India (Supplemental Table 3) and in keeping with various cross-sectional surveys,7,20, 21, 22 our study highlights the significant increase in the use of tobacco and tobacco-related products. The increase in prevalence of smoking especially among young adults in India is alarmingly high, even compared with prevalence from the United States and Europe. “Beedi’ smoking was more prevalent than cigarette smoking. Although the association of beedi smoking with ASCVD is unclear, a stronger association with oral cancer than traditional cigarette suggests a higher likelihood of ASCVD patients in these patients.23,24 These products remain unregulated in India and awareness of their deleterious effects remain inadequately understood. This factor is of concern and warrants stringent population-based policy interventions and the intensification of existing health promotion campaigns.
The lack of PCI was the strongest independent predictor of inpatient and 30-day mortality for patients presenting with STEMI. Although the use of coronary angiography and PCI in our study was higher than prior studies in India,6,7,16 it was still lower than observed in the United States or Europe.25,26 The low rates of revascularization were largely due to the time delay from symptom onset to presentation at a PCI capable facility and unclear benefit of PCI ≥12 hours after an event among patients without signs of ongoing ischemia owing to a lack of viability of the infarcted myocardium.27 Despite an increase in PCI-capable centers in India in the last decade, prompt access to these centers remains a major hindrance in STEMI care in this country. In our study, 64% of patients presented to the first health care contact within 1 hour of symptom onset and 78% within 3 hours of symptom onset. Although the average time to health care contact remain comparable with studies from the United States and Europe,25,26 the vast majority of these patients (93%) presented to a non-PCI-capable facility as the initial point of contact. Considering these patients had to rely on self-transport or public transportation to reach PCI-capable centers, there were significant delays in being transported to our PCI centers. The lack of financial means to access medical care at nearby PCI-capable private centers could also have contributed to delays in timely revascularization. Up to 98% of the patients in our cohort had no medical insurance and had to pay out of pocket for their medical costs. Government-funded tertiary care centers such as those included in our study provide medical care largely free of cost; however, these centers are scarce and have high patient volumes, limiting timely evaluation and treatment of patients with STEMI. Unsurprisingly, we found high rates of post-MI left ventricular systolic dysfunction and high 1-year mortality rates in our registry.
A possible solution for increasing PCI use rates comes from the Tamil Nadu STEMI initiative.6 In this referral-based hub-and-spoke model, PCI centers were connected to non-PCI centers through a dedicated ambulance service capable of transmitting electrocardiographs, resulting in decreased in delays in presentation. Although national implementation of this model is limited owing to the wide heterogeneity of health care setups across India, the effectiveness of telehealth as a means for prompt identification and triage of patients with STEMI offers potential ways to address this barrier and expand access to timely revascularization.28
Findings from our registry offer a more contemporary view of STEMI epidemiology and management practices from 2 large PCI-capable tertiary centers catering to patients from multiple states can be used to inform similar future initiatives aimed at improving the standard of care for STEMI in India.
Sex Differences in the Management and Outcomes for STEMI
Sex differences in the management of acute coronary syndrome persist in the contemporary era. In a recent analysis from the Atherosclerosis Risk in Communities Study, these differences in ACS management across sex were even noted in young adults.8 Despite an abundance of studies concentrated on evaluating these differences, studies from India remain limited. Female patients presenting with STEMI were older and had a higher prevalence of hypertension and DM, which is consistent with data from prior registry studies. Even after adjusting for these factors, female sex remained an independent predictor of in-hospital mortality and was associated with a 2-fold risk of mortality at 1 year compared with male sex. Only 16% of our population presenting for STEMI were female patients. The proportion of female patients in prior multicenter registry studies of ACS patients in India varies between 18% and 23%7,16,20 (Supplemental Table 3). This finding contrasts with a global meta-analysis that demonstrated that female patients constituted ≤31% of all patients presenting with STEMI, which suggests that female patients are unable to access medical services in a timely manner compared with male patients.29 These delays were attributed to misinterpretation of symptoms or lack of transport, which are modifiable factors. In the VIRGO (Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients) study,30 young female patients diagnosed with STEMI were more likely to present with chest pain, but also had an increased frequency of accompanying symptoms such as epigastric pain, shoulder, and jaw pain, compared with young male patients. Thus, physicians should have a low threshold for initiating ischemic evaluation in female patients (or male patients) who present with accompanying symptoms if they have a high cardiometabolic risk.31
These sex-related differences can be addressed using systems-based approach to STEMI care.31 In 1 quality improvement trial that was implemented in a quaternary care center in the United States, implementation of standardized care bundles helped to improve the door-to-balloon time and increased rates of goal-directed pharmacotherapy in female patients with STEMI.32 The initiative focused on decreasing the door-to-balloon time by ensuring immediate transfer to PCI-capable facilities, developing STEMI handoff lists, instituting standardized criteria for early triage to the catheterization laboratory, and a preference for a radial approach. This strategy resulted in significant improvements in in-hospital and 30-day mortality, especially in female patients. Similar strategies are urgently needed to improve outcomes in female patients with STEMI in India.
Study Limitations
Our study has certain limitations that must be considered while interpreting the results. Currently, patients were enrolled from 2 large tertiary PCI-capable centers located in a metropolitan city in Northern India. We do not have detailed information on patients with STEMI who were not transferred to our hospitals. Although we plan to recruit patients from additional centers in the future, present data may not be fully reflective of all management practices for STEMI in other Indian states or practice settings. The data analyzed were observational in nature and, despite the use of multivariate analysis, unmeasured confounders may be present. Additionally, clinical events were physician adjudicated, which makes our data susceptible to observer bias. Outcomes regarding hospital readmission were unavailable for many patients, leading to the loss of potentially significant clinical endpoints during follow-up. However, the results of this study provide contemporary data about STEMI care in India. Awareness of the deficiencies is the steppingstone for improving care and making it more equitable.
Conclusions
In this contemporary STEMI registry from India, more than one-third of patients were <50 years of age and the majority were smokers. There were significant delays in reperfusion, largely owing to transportation time to a PCI-capable center. Compared with male patients, female patients presenting with STEMI were older, had a higher burden of traditional risk factors, and sought care later. Female patients were less likely to undergo coronary angiography or PCI and had significantly higher mortality compared with male patients. Urgent strategies and synchronized efforts are needed to improve the outcomes of patients presenting with STEMI in India.
Perspectives.
COMPETENCY IN PATIENT CARE: Patients with STEMI in India continue to face significant delays in receiving timely reperfusion therapy. Compared with male patients, female patients are less likely to undergo coronary revascularization with PCI and have higher in-hospital and 1-year mortality rates.
TRANSLATIONAL OUTLOOK: The current study can provide information to guide future efforts aimed at improving clinical outcomes and sex differences in the care of patients with STEMI in India.
Funding Support and Author Disclosures
Dr Qamar has received institutional grant support from Novo Nordisk, NorthShore Auxiliary Research Scholar Fund, and fees for educational activities from the American College of Cardiology, Society for Vascular Medicine, Society for Cardiovascular Angiography and Interventions, Janssen and Janssen, Pfizer, Medscape, and Clinical Exercise Physiology Association. Dr Bhatt is on the advisory board for AngioWave, Bayer, Boehringer Ingelheim, Cardax, CellProthera, Cereno Scientific, Elsevier Practice Update Cardiology, High Enroll, Janssen, Level Ex, McKinsey, Medscape Cardiology, Merck, MyoKardia, NirvaMed, Novo Nordisk, PhaseBio, PLx Pharma, Regado Biosciences, and Stasys; is on board of directors for AngioWave (stock options), Boston VA Research Institute, Bristol Myers Squibb (stock), DRS.LINQ (stock options), High Enroll (stock), Society of Cardiovascular Patient Care, and TobeSoft; is chair and inaugural chair of the American Heart Association Quality Oversight Committee; is a consultant for Broadview Ventures; is on the Data Monitoring Committees for Acesion Pharma, Assistance Publique-Hôpitaux de Paris, Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Boston Scientific (Chair, PEITHO trial), Cleveland Clinic (including for the ExCEED trial, funded by Edwards Lifesciences), Contego Medical (Chair, PERFORMANCE 2), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo; for the ABILITY-DM trial, funded by Concept Medical), Novartis, Population Health Research Institute; and Rutgers University (for the NIH-funded MINT Trial); has received honoraria from American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Chair, ACC Accreditation Oversight Committee), Arnold and Porter law firm (work related to Sanofi/Bristol Myers Squibb clopidogrel litigation), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; is on the RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim; is on the AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (Editor-in-Chief, Harvard Heart Letter), Canadian Medical and Surgical Knowledge Translation Research Group (clinical trial steering committees), Cowen and Company, Duke Clinical Research Institute (clinical trial steering committees, including for the PRONOUNCE trial, funded by Ferring Pharmaceuticals), HMP Global (Editor-in-Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), K2P (Co-Chair, interdisciplinary curriculum), Level Ex, Medtelligence/ReachMD (CME steering committees), MJH Life Sciences, Oakstone CME (Course Director, Comprehensive Review of Interventional Cardiology), Piper Sandler, Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co-leader, funded by Bayer), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees), and Wiley (steering committee); Other: Clinical Cardiology (Deputy Editor), NCDR-ACTION Registry Steering Committee (Chair), and VA CART Research and Publications Committee (Chair); Patent: Sotagliflozin (named on a patent for sotagliflozin assigned to Brigham and Women's Hospital who assigned to Lexicon; neither I nor Brigham and Women's Hospital receive any income from this patent); Research Funding: Abbott, Acesion Pharma, Afimmune, Aker Biomarine, Amarin, Amgen, AstraZeneca, Bayer, Beren, Boehringer Ingelheim, Boston Scientific, Bristol Myers Squibb, Cardax, CellProthera, Cereno Scientific, Chiesi, CinCor, CSL Behring, Eisai, Ethicon, Faraday Pharmaceuticals, Ferring Pharmaceuticals, Forest Laboratories, Fractyl, Garmin, HLS Therapeutics, Idorsia, Ironwood, Ischemix, Janssen, Javelin, Lexicon, Lilly, Medtronic, Merck, Moderna, MyoKardia, NirvaMed, Novartis, Novo Nordisk, Owkin, Pfizer, PhaseBio, PLx Pharma, Recardio, Regeneron, Reid Hoffman Foundation, Roche, Sanofi, Stasys, Synaptic, The Medicines Company, Youngene, 89Bio; Royalties: Elsevier (Editor, Braunwald’s Heart Disease); Site Co-Investigator: Abbott, Biotronik, Boston Scientific, CSI, Endotronix, St. Jude Medical (now Abbott), Philips, SpectraWAVE, Svelte, and Vascular Solutions; Trustee: American College of Cardiology; Unfunded Research: FlowCo and Takeda. Dr Gulati discloses the following relationships: K2P (Chair, prevention curriculum), WebMD (speaker); President-Elect and Executive Board of the American Society for Preventive Cardiology; Editorial Board of the Journal for Cardiac Failure, Associate Editor of Atherosclerosis. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental tables, please see the online version of this paper.
Appendix
References
- 1.Prabhakaran D., Singh K., Roth G.A., Banerjee A., Pagidipati N.J., Huffman M.D. Cardiovascular diseases in India compared with the United States. J Am Coll Cardiol. 2018;72(1):79–95. doi: 10.1016/j.jacc.2018.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roth G.A., Mensah G.A., Johnson C.O., et al. Global burden of cardiovascular diseases and risk factors, 1990–2019. J Am Coll Cardiol. 2020;76(25):2982–3021. doi: 10.1016/j.jacc.2020.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.India State-Level Disease Burden Initiative CVD Collaborators The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990–2016. Lancet Glob Health. 2018;6(12):e1339–e1351. doi: 10.1016/S2214-109X(18)30407-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krumholz H.M., Herrin J., Miller L.E., et al. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation. 2011;124(9):1038–1045. doi: 10.1161/CIRCULATIONAHA.111.044107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guha S., Sethi R., Ray S., et al. Cardiological Society of India: position statement for the management of ST elevation myocardial infarction in India. Indian Heart J. 2017;69(Suppl 1):S63–S97. doi: 10.1016/j.ihj.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alexander T., Mullasari A.S., Joseph G., et al. A system of care for patients with ST-segment elevation myocardial infarction in India: the Tamil Nadu–ST-Segment Elevation Myocardial Infarction Program. JAMA Cardiol. 2017;2(5):498. doi: 10.1001/jamacardio.2016.5977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohanan P.P., Mathew R., Harikrishnan S., et al. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34(2):121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arora S., Stouffer G.A., Kucharska-Newton A.M., et al. Twenty year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation. 2019;139(8):1047–1056. doi: 10.1161/CIRCULATIONAHA.118.037137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Matetic A., Shamkhani W., Rashid M., et al. Trends of sex differences in clinical outcomes after myocardial infarction in the United States. CJC Open. 2021;3(12, Suppl):S19–S27. doi: 10.1016/j.cjco.2021.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khera S., Kolte D., Gupta T., et al. Temporal trends and sex differences in revascularization and outcomes of ST-segment elevation myocardial infarction in younger adults in the United States. J Am Coll Cardiol. 2015;66(18):1961–1972. doi: 10.1016/j.jacc.2015.08.865. [DOI] [PubMed] [Google Scholar]
- 11.DeFilippis E.M., Collins B.L., Singh A., et al. Women who experience a myocardial infarction at a young age have worse outcomes compared with men: the Mass General Brigham YOUNG-MI registry. Eur Heart J. 2020;41(42):4127–4137. doi: 10.1093/eurheartj/ehaa662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cenko E., Yoon J., Kedev S., et al. Sex Differences in outcomes after STEMI: effect modification by treatment strategy and age. JAMA Intern Med. 2018;178(5):632. doi: 10.1001/jamainternmed.2018.0514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Luca L., Marini M., Gonzini L., et al. Contemporary trends and age-specific sex differences in management and outcome for patients with ST-segment elevation myocardial infarction. J Am Heart Assoc. 2016;5(12) doi: 10.1161/JAHA.116.004202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gulati M. Yentl’s bikini: sex differences in STEMI. J Am Heart Assoc. 2019;8(10) doi: 10.1161/JAHA.119.012873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pagidipati N.J., Huffman M.D., Jeemon P., et al. Association between gender, process of care measures, and outcomes in ACS in India: results from the Detection and Management of Coronary Heart Disease (DEMAT) registry. PLoS One. 2013;8(4) doi: 10.1371/journal.pone.0062061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mahajan K., Negi P.C., Merwaha R., Mahajan N., Chauhan V., Asotra S. Gender differences in the management of acute coronary syndrome patients: one year results from HPIAR (HP-India ACS Registry) Int J Cardiol. 2017;248:1–6. doi: 10.1016/j.ijcard.2017.07.028. [DOI] [PubMed] [Google Scholar]
- 17.Arora S., Qamar A., Gupta P., et al. Design and rationale of the North Indian ST-Segment Elevation Myocardial Infarction Registry: a prospective cohort study. Clin Cardiol. 2019;42(12):1140–1146. doi: 10.1002/clc.23278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thygesen K., Alpert J.S., Jaffe A.S., et al. Fourth universal definition of myocardial infarction (2018) Circulation. 2018;138(20):e618–e651. doi: 10.1161/CIR.0000000000000617. [DOI] [PubMed] [Google Scholar]
- 19.Expert Panel on Detection E and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 20.Xavier D., Pais P., Devereaux P.J., et al. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371 doi: 10.1016/S0140-6736(08)60623-6. 1453-1442. [DOI] [PubMed] [Google Scholar]
- 21.Bhan N., Karan A., Srivastava S., Selvaraj S., Subramanian S.V., Millett C. Have socioeconomic inequalities in tobacco use in India increased over time? Trends from the National Sample Surveys (2000–2012) Nicotine Tob Res. 2016;18(8):1711–1718. doi: 10.1093/ntr/ntw092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reddy K.S., Perry C.L., Stigler M.H., Arora M. Differences in tobacco use among young people in urban India by sex, socioeconomic status, age, and school grade: assessment of baseline survey data. Lancet. 2006;367(9510):589–594. doi: 10.1016/S0140-6736(06)68225-1. [DOI] [PubMed] [Google Scholar]
- 23.Rahman M., Fukui T. Bidi smoking and health. Public Health. 2000;114(2):123–127. doi: 10.1038/sj.ph.1900625. [DOI] [PubMed] [Google Scholar]
- 24.Rahman M., Sakamoto J., Fukui T. Bidi smoking and oral cancer: a meta-analysis. Int J Cancer. 2003;106(4):600–604. doi: 10.1002/ijc.11265. [DOI] [PubMed] [Google Scholar]
- 25.Peterson E.D., Roe M.T., Chen A.Y., et al. The NCDR ACTION Registry-GWTG: transforming contemporary acute myocardial infarction clinical care. Heart. 2010;96(22):1798–1802. doi: 10.1136/hrt.2010.200261. [DOI] [PubMed] [Google Scholar]
- 26.Hanssen M., Cottin Y., Khalife K., et al. French Registry on Acute ST-elevation and non ST-elevation Myocardial Infarction 2010. FAST-MI 2010. Heart. 2012;98(9):699–705. doi: 10.1136/heartjnl-2012-301700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lawton J., Tamis-Holland J., et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization. J Am Coll Cardiol. 2022;79(2):e21–e129. doi: 10.1016/j.jacc.2021.09.006. [DOI] [PubMed] [Google Scholar]
- 28.Mehta S., Grines C.L., Botelho R., et al. STEMI telemedicine for 100 million lives. Catheterization Cardiovasc Interv. 2021;98(6):1066–1071. doi: 10.1002/ccd.29896. [DOI] [PubMed] [Google Scholar]
- 29.Shah T., Haimi I., Yang Y., et al. Meta-analysis of gender disparities in in-hospital care and outcomes in patients with ST-segment elevation myocardial infarction. Am J Cardiol. 2021;147:23–32. doi: 10.1016/j.amjcard.2021.02.015. [DOI] [PubMed] [Google Scholar]
- 30.Lichtman J.H., Leifheit E.C., Safdar B., et al. Sex differences in the presentation and perception of symptoms among young patients with myocardial infarction: evidence from the VIRGO Study (Variation in Recovery: Role of Gender on Outcomes of Young AMI Patients) Circulation. 2018;137(8):781–790. doi: 10.1161/CIRCULATIONAHA.117.031650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gulati M., Levy P.D., et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain. J Am Coll Cardiol. 2021;78(22):e187–e285. doi: 10.1016/j.jacc.2021.07.053. [DOI] [PubMed] [Google Scholar]
- 32.Huded C.P., Johnson M., Kravitz K., et al. 4-Step protocol for disparities in STEMI care and outcomes in women. J Am Coll Cardiol. 2018;71(19):2122–2132. doi: 10.1016/j.jacc.2018.02.039. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.