Abstract
Cardiac amyloidosis (CA) is caused by deposition of amyloid fibrils in the myocardium and has two main subtypes, transthyretin cardiac amyloidosis (ATTR) and immunoglobulin light chain cardiac amyloidosis (AL). ATTR is further differentiated into wild-type (wtATTR) and hereditary (hATTR), depending on the absence or presence of mutation in the transthyretin gene. The increased recognition of disease with the improvement in diagnostic armamentarium and serendipitous advancements in the therapeutic landscape have changed the status of CA from being a rare and untreatable disease to being a not-so-rare and treatable disease. Both ATTR and AL have certain clinical aspects that can provide early clues for the disease. While electrocardiography followed by echocardiography and subsequently cardiac magnetic resonance can raise suspicion for CA, the definitive diagnosis of ATTR is non-invasively established by bone scintigraphy while that of AL always needs histological confirmation. Severity of CA can be gauged by serum biomarker-based staging of both ATTR and AL. ATTR therapies work by silencing or stabilizing TTR or by degrading amyloid fibrils, while AL is managed with anti-plasma cell therapies and autologous stem cell transplant.
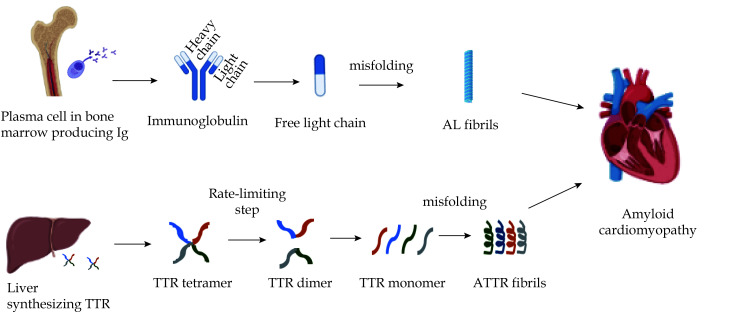
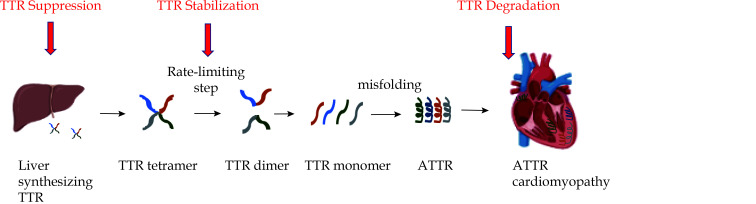
Amyloidosis constitutes a group of diseases that is caused by misfolding and extracellular deposition of proteins in various tissues in bundles of β-sheet fibrillar protein.[1] The deposition of large amounts of amyloid fibrils can disrupt the tissue architecture and result in organ dysfunction. Cardiac involvement is the leading etiology of morbidity and mortality in amyloidosis.[2] Cardiac amyloidosis (CA) manifests as a restrictive cardiomyopathy and has two main subtypes, immunoglobulin light chain cardiac amyloidosis (AL) and transthyretin cardiac amyloidosis (ATTR).[3] In AL, the amyloid fibrils are formed by the N-terminal fragment of a monoclonal immunoglobulin light chain produced by a low proliferating bone marrow plasma cell clone (Figure 1). On the other hand, ATTR is derived from dissociation and misfolding of hepatically-derived transthyretin (TTR) protein, a carrier of thyroxine and retinol binding protein. ATTR is further subdivided into wild-type (wtATTR) and hereditary (hATTR) types, depending on the absence or presence of mutation in the precursor protein gene.
Figure 1.
Pathobiology of the two most common types of cardiac amyloidosis.
AL: immunoglobulin light chain amyloidosis; ATTR: transthyretin amyloidosis; TTR: transthyretin.
CA remains an underdiagnosed and misdiagnosed disease, primarily due to its phenotypic overlap with other diseases including hypertrophic cardiomyopathy. CA has been found in 13% of patients with diastolic heart failure, 16% of patients with degenerative aortic valve stenosis, and 9% of patients who were previously diagnosed as hypertrophic cardiomyopathy.[4,5,6] In addition, postmortem histological studies have revealed that up to one-quarter of octogenarians have myocardial amyloid deposits.[7] While improved testing and expansion in the diagnostic armamentarium to diagnose CA has unleashed notable community prevalence of CA, there is ever-increasing need of recognizing these patients at an early stage in order to maximize the therapeutic potential of new disease-modifying therapies available.
This review aims to highlight pathophysiological and epidemiological differences between wtATTR, hATTR and AL, detail clinical features that could potentially help in the early detection of CA, discuss role of multimodality imaging and endomyocardial biopsy in the diagnostic workup, and finally elaborate management strategies for CA.
EPIDEMIOLOGY AND NATURAL COURSE OF DISEASE
Immunoglobulin light chain amyloidosis (AL)
AL remains the most common type CA, accounting for 55% of all cases.[8] The incidence of AL is approximately 2200 new cases annually in the United States.[9] The median age at diagnosis is about 65 years, with men being affected slightly more compared with women, and the disease course is more aggressive compared with ATTR due to cardiotoxicity associated with amyloidogenic light chains.[10] While AL can involve all organs except the brain, kidney (74%) and heart (60%) are the most frequently affected organs.[11] Cardiac involvement is the key prognostic determinant. AL patients who present with symptomatic heart failure have a median survival of 6 months without successful therapy.[9]
Wild-type transthyretin amyloidosis (wtATTR)
wtATTR is increasingly being recognized as the most common type of CA in the elderly. The incidence of wtATTR has increased exponentially in the past three decades, from less than 3% of all CA cases in the period 1987–2009 to 14% in the period 2010–2015 and eventually to 25% in the period 2016–2019.[8] This trend reflects substantially greater recognition of disease with the emergence of non-invasive imaging modalities for screening and diagnosing wtATTR. wtATTR almost exclusively affects the elderly population, predominantly affects males and Caucasians, and involves the heart in > 90% of cases. The median age at diagnosis is 75 years, and overall survival from diagnosis has been reported to be 3.6 years.[12]
Hereditary transthyretin amyloidosis (hATTR)
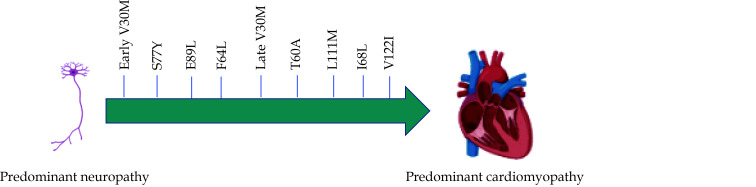
hATTR is caused by > 120 delineated mutations in the TTR gene, which are inherited in an autosomal dominant fashion. hATTR has variable age of onset, geographic distribution, primary phenotypic expression (cardiomyopathy, neuropathy, or mixed) and disease course depending on the mutation and fibril type.[13] The true prevalence of hATTR is not known. In the United States, the most common mutation is the substitution of valine for isoleucine at position 122 (V122I), which is carried by 3%-4% of the African-American population.[14] V122I-hATTR is phenotypically comparable to wtATTR, as it predominantly affects males, causing late-onset cardiomyopathy with minimal neuropathy, and has onset at the age of about 70 years (Figure 2). The second most common mutation in the United States is T60A that has its origins in the Northern part of Ireland, and presents as a mixed cardiomyopathy-neuropathy phenotype.[15] The most common mutation world-wide is V30M, which may manifest as an early-onset or late-onset disease.[16] The early-onset disease (at age less than 50 years) has been considered the more common form of disease in endemic regions of Sweden, Portugal and Japan, presenting with predominantly neurological symptoms, while late-onset variant could be found in nonendemic areas and present with cardiac symptoms in addition to severe neurological symptoms.[17] In addition, L111M variant is commonly found in Denmark, while I68L occurs in Italy.[18]
Figure 2.
Spectrum of phenotypic expression for common transthyretin mutations.
Mutations can manifest as predominantly neuropathy, predominantly cardiomyopathy or mixed.
PATHOPHYSIOLOGY OF CA
There is diffuse extracellular myocardial amyloid deposition in the ventricles, leading to concentric biventricular remodeling and thickening. The term left ventricular hypertrophy (LVH), often used to describe ventricular thickness in CA, is therefore a misnomer. In ATTR, the pattern of deposition is pre-dominantly transmural compared to AL in which subendocardial pattern is more often noted.[19] Ventricular amyloidosis results in stiff, non-dilated and poorly compliant ventricles, leading to elevated diastolic filling pressures. Left ventricular ejection fraction (LVEF) is typically preserved in the early stages of the disease, and deteriorates with disease progression, identifying patients with adverse prognosis. It is worth noting that while LVEF may be preserved in CA, biventricular thickening and stiffness without compensatory ventricular dilation results in fixed, low stroke volume and hence low cardiac output, making CA phenotypically distinct from non-amyloid etiologies of heart failure. CA patients are heart-rate dependent for their cardiac output, and therefore cannot tolerate negative chronotropic agents including beta-blockers and calcium channel blockers.[20,21]
The atrial amyloid infiltration results in atrial myopathy, leading to an unusually higher prevalence of atrial arrhythmias in CA.[21] Atrial arrhythmias and loss of atrial mechanical function increases risk of atrial thrombi, and ultimately cardioembolic strokes.[21] Conduction system involvement in CA leads to conduction delays and atrioventricular (AV) blocks. Conduction defects in the His-Purkinje system are more common and often associated with symptomatic AV block. In addition, aortic and mitral valvular thickening is also commonly noted in CA.
CLINICAL FEATURES AND NON-CARDIAC CLUES
The characteristic clinical presentation of CA is decompensated heart failure, manifesting as progressive dyspnea on exertion, and/or signs of right ventricular failure including peripheral lower extremity edema and jugular venous distention. Ascites can be seen in advanced cases. Cardiogenic shock can rarely be initial presentation in severe cases.[22] CA patients can present with typical angina even in the absence of obstructive epicardial coronary artery disease as a result of coronary microvascular dysfunction.[23,24] It is postulated that deposition of amyloid fibrils in the interstitium, intramyocardial coronary vessels and perivascular regions of the heart causes increased coronary microvascular resistance and decreased coronary flow reserve, leading to ischemic symptoms.[24] Syncope is another common presentation in CA, which could be arrhythmia-induced or triggered by autonomic dysfunction. While atrial fibrillation is the most common arrhythmia in CA, it is not uncommon to see bradyarrhythmia, particularly heart blocks, as the initial presentation in CA. Elderly patients with wtATTR could present with low-flow, low-gradient aortic stenosis.[25]
There are many non-cardiac clues that heighten the suspicion for CA (Figure 3). Orthopedic manifestations are a hallmark of wtATTR. Carpal tunnel syndrome, caused by deposition of amyloid fibrils in the flexor retinaculum and tenosynovial tissue within the carpal tunnel, is the earliest and most common non-cardiac manifestation. Carpal tunnel syndrome is present in about 50% of wtATTR patients, and precedes cardiac involvement by 5-9 years.[26] Studies have demonstrated that about 10%-16% of patients have tenosynovial amyloid deposits at the time of carpal tunnel surgery, while only up to 2% patients have CA at that time.[27] CACTUS (Cardiac Amyloidosis Carpal TUnnel Syndrome) study, which screened patients for CA 5 to 15 years after bilateral carpal tunnel surgery, showed an increased CA prevalence of 5%. Importantly, clinical yield was higher (> 1 in 5 diagnosed with CA) when focusing on nonobese elderly men (BMI of < 30 kg/m2 and age ≥ 70 years), showing potential for systematic screening in selected patient population.[28] Spinal stenosis, caused by amyloid deposition in the ligamentum flavum, is exclusively present in ATTR, specifically wtATTR. Amyloid is detected in more than a third of older adults undergoing surgery for lumbar spinal stenosis, and is more common with advancing age.[29] Spontaneous rupture of the distal biceps tendon represents ATTR deposition in the biceps tendon, and has been reported in 33% of wtATTR patients compared with 2.5% prevalence in non-amyloid heart failure patients.[30] In addition, wtATTR patients have a greater prevalence of total hip and knee arthroplasties compared with the general population.[31]
Figure 3.
Sites involved in systemic amyloidosis in the body.
AL: immunoglobulin light chain amyloidosis; hATTR: hereditary transthyretin amyloidosis; wtATTR: wild-type transthyretin amyloidosis.
AL patients can involve any extra-cardiac site other than the brain. Kidney involvement is most common, usually presenting as nephrotic syndrome and proteinuria due to glomerular deposition of amyloid. In approximately 10% of patients, amyloid deposition occurs in the renal vessels and tubulointerstitium, causing renal insufficiency without significant proteinuria.[32] Rarely, AL can present with acute kidney injury due to intratubular amyloid cast nephropathy.[33] Hepatomegaly is common and can occur either due to amyloid infiltration of the liver or secondary to congestion from right-sided heart failure. Autonomic nervous system involvement causes orthostatic hypotension, gastroparesis, erectile dysfunction, and intestinal dysmotility. Peripheral nervous system involvement results in painful, bilateral, symmetric, distal sensory neuropathy that progresses to motor neuropathy. Soft tissue involvement is characterized by macroglossia, which is a hallmark feature of AL disease.
NON-INVASIVE DIAGNOSTIC EVALUATION AND ROLE OF MULTIMODALITY IMAGING
Electrocardiogram
Low voltage (QRS amplitude less than 5 mm in limb leads or less than 10 mm in precordial leads) on a 12-lead electrocardiogram (EKG) is generally considered to be a classical finding in CA. The mismatch between low voltage on EKG and thickened ventricles on echocardiogram is characteristic of CA, since the thickening is due to amyloid infiltration and not actual cardiomyocyte hypertrophy. Importantly, low voltage is detected only in about 35% of ATTR and 55% of AL patients, and therefore absence of low voltage criteria does not rule out CA.[34] It often manifests in advanced disease stage, and carries prognostic implications.[34,35] The misperception that CA cannot present with high voltage on EKG can lead to underdiagnosis, since approximately 10% of CA patients meet EKG criteria for LVH.[35] A series of 64 hATTR patients with V122I mutation found that 25% patients had EKGs that met LVH criteria on presentation.[36]
Another common EKG finding in CA is pseudo-infarct pattern that could be observed in 50% of patients with CA.[37] Other EKG features that are reflective of the generalized infiltrative nature of this disease include fascicular block, atrial fibrillation/flutter, AV block of varying degree and abnormalities of the QRS complexes, representing intramyocardial conduction abnormalities in these patients.[38] First-degree heart block is a common finding at diagnosis, and potentially identifies patients who are at a high risk for pacemaker implantation in the future.[36]
Echocardiography
Echocardiography is the initial imaging tool that can raise suspicion for CA among other differentials including hypertensive cardiomyopathy, hypertrophic cardiomyopathy, aortic stenosis and Fabry’s disease. Left ventricular (LV) thickness is often striking in these patients, and while it is commonly concentric, asymmetric thickening has been reported in 23% of wtATTR patients.[39] LV thickness often exceeds 15mm, and wtATTR patients generally have a greater wall thickness compared with AL.[40] Importantly, a subset of CA patients can have normal LV thickness of echocardiography.[41] Rarely, patients can have dynamic LV outflow obstruction that mimics hypertrophic obstructive cardiomyopathy.[42] Concomitant right ventricular thickness is often, not always, present in CA, and right ventricular dysfunction is not uncommon secondary to amyloid infiltration. Other common echocardiographic features include smaller left ventricular cavity, right and left atrial enlargement, and interatrial septal thickness. The granular speckled appearance of the myocardium, traditionally thought to be a classic feature of CA, is nonspecific for CA. The presence of low-flow, low-gradient aortic stenosis can raise concern for CA. Diastolic dysfunction characterized by steep deceleration time, low tissue Doppler velocity at the mitral annulus or E, and an elevated E/e ratio is universally present. While LVEF is preserved in majority of CA patients on presentation, it can progressively decrease in late stages of the disease.[43]
Tissue Doppler imaging in CA detects impairment of longitudinal ventricular contraction before the onset of heart failure symptoms and compromise in LVEF. Deformation-based speckled-tracking strain imaging that incorporates global longitudinal strain (GLS) and relative apical sparing has demonstrated superior results compared with conventional echocardiography in discriminating CA from other etiologies of LVH.[44] CA has a classic GLS pattern in which basal and mid segments are severely impaired while apical segment is relatively spared, producing a characteristic “cherry-on-top” bullseye appearance, calculated as the ratio of apical longitudinal strain to the sum of basal and mid longitudinal strain. A relative apical longitudinal strain of 1 is able to differentiate CA from HCM and aortic stenosis with a high sensitivity and specificity.[45]
Cardiac Magnetic Resonance
Cardiac magnetic resonance (CMR) plays a pivotal role in differentiating CA from other hypertrophic phenocopies by providing three-dimensional structural and functional imaging, higher spatial resolution than echocardiography, and quantifiable tissue characterization. It, however, cannot reliably differentiate between ATTR and AL. Amyloid infiltration results in abnormal gadolinium kinetics, seen on post-gadolinium T1 inversion recovery imaging, whereby the gadolinium and the blood null at the same time. In CA, extracellular space often expands due to amyloid infiltration, which is accurately visualized using the administration of gadolinium-based contrast agent. The gadolinium passively distributes in the expanded extracellular space created by amyloid fibrils, producing typical pattern of diffuse, subendocardial and/or transmural late gadolinium enhancement (LGE) on CMR that is pathognomonic for CA.[46] LGE pattern also predicts prognosis, as transmural enhancement represents advanced cardiac amyloidosis and has been associated with a poorer prognosis.[47] The only downside to the use of gadolinium-based contrast agents is the potential risk of developing nephrogenic systemic fibrosis in patients with a glomerular filtration rate of less than 30 mL/min per 1.73 m2.[48]
T1 mapping, a pixel-based quantification of measured longitudinal relaxation times, further extends the ability of CMR to characterize the myocardium and allowing a more comprehensive understanding of the myocyte response. Native T1 (T1 time before the administration of contrast) is a quantifiable and sensitive marker of CA, which is found to be elevated in the early stages of CA prior to the development of ventricular thickening or detectable LGE.[49] Native T1 mapping can not only help in the diagnosis of CA, but used to monitor disease progression. A pre-contrast T1 time > 1044 ms for AL and > 1077 ms for ATTR have been associated with a poor prognosis.[50,51] T1 mapping can be utilized to estimate myocardial extracellular volume (ECV) fraction which is used as a surrogate in quantification of myocardial amyloid burden, and has demonstrated correlation with disease severity in both AL and ATTR.[52] In addition, potential role of ECV has been seen in tracking treatment response in AL patients.[53] Lastly, T2 mapping is another method of tissue characterization through the visualization and quantification of myocardial edema, and serves to complement T1, LGE, and ECV. While T2 is elevated in both ATTR and AL, higher values have been reported in untreated AL patients when compared with treated AL and ATTR patients, and T2 mapping has specifically been shown to be prognostically relevant in AL.[54]
Nuclear Scintigraphy
Nuclear scintigraphy using bone-avid radiotracers is the only imaging modality that can non-invasively diagnose ATTR, obviating the need for endomyocardial biopsy. 99mTc-pyrophosphate (99mTc-PYP) tracer is available in the United States, while 99mTc-hydroxymethylene diphosphonate (99mTc-HMDP) and 99mTc-diphosphono-1,2-propanodicarboxylic acid (99mTc-DPD) are used in Europe, and these traces demonstrate comparable diagnostic performance.[55] Data suggest that microcalcifications underlie the selectivity of bone scintigraphy for ATTR, as the density of microcalcifications is higher is ATTR compared with AL (mean = 16.8 vs. 6.5 per 200 × field, P = 0.008), irrespective of age, cardiac function, and serum levels of calcium and creatinine.[56]
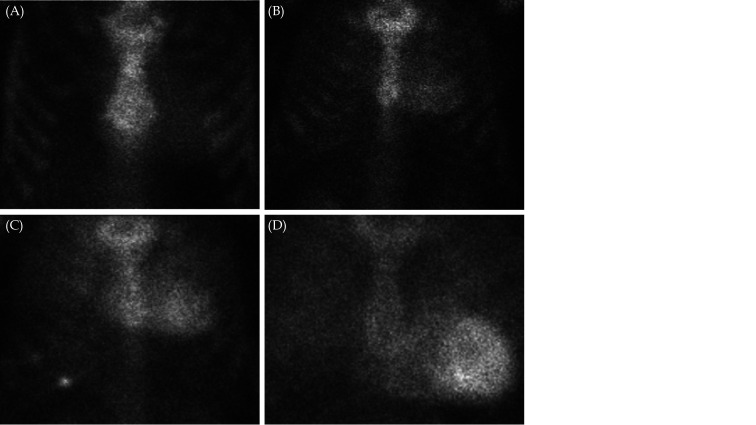
The interpretation of nuclear scintigraphy uses a semiquantitative method of visual grading of tracer uptake. Myocardial tracer uptake is compared with bone uptake of the rib cage with a simple scheme in which a grade of 0 is no myocardial uptake, a grade of 1 is mild myocardial uptake (less than in bone), a grade of 2 is when myocardial uptake is equal to that in bone and a grade of 3 is when there is substantial myocardial uptake (greater than in bone) (Figure 4).[57] A multicentered study comprising of a large cohort of biopsy-proven ATTR patients concluded that these bone avid tracers conferred 100% specificity and positive predictive value for ATTR when grade 2 or 3 uptake was seen in the absence of paraproteinemia.[58] The quantitative assessment of myocardial tracer uptake involves drawing circular regions of interest over the heart and mirrored on the contralateral chest wall, and quantifying radiotracer uptake using the heart-to-contralateral lung (H/CL) ratio. H/CL ratio greater than 1.5 is consistent with the diagnosis of ATTR, and a ratio of ≥ 1.6 is associated with poor survival.[59,60]
Figure 4.
Semiquantitative method of visual grading of tracer uptake in 99mTc-pyrophosphate scintigraphy.
(A): grade 0- no myocardial uptake; (B): grade 1- mild myocardial uptake (less than in bone); (C): grade 2 - myocardial uptake is equal to that in bone; and (D): grade 3- substantial myocardial uptake (greater than in bone).
It is worth emphasizing that nuclear scintigraphy with a visual grade of 2 or 3 describing myocardial uptake showed a high sensitivity of > 99% for ATTR but a lower specificity of 82%–86%, given that a grade of 1 or 2 can be observed in patients with AL.[59,61] Hence, since bone scintigraphy alone cannot definitively establish the diagnosis of ATTR and exclude AL, it is the standard of practice to perform urine and serum immunofixation electrophoresis, as well as obtain serum free light chains and kappa/lambda ratio for AL disease. If urine and serum tests are negative for AL, the specificity of nuclear scintigraphy increases to 100%. Hence, ATTR can be diagnosed with confidence, in the absence of histological confirmation, in a patient who has a typical clinical phenotype (for example, history of bilateral carpal tunnel surgery), has echocardiographic and/or CMR features consistent with CA, has grade 2 or 3 tracer uptake in the heart on 99mTc-PYP scintigraphy and has undetectable monoclonal gammopathy in the blood and urine.
WHEN IS HISTOLOGICAL CONFIRMATION NEEDED?
Histological confirmation and typing of amyloid should be pursued in patients with detectable monoclonal immunoglobulin, which raises the suspicion of AL. The definitive diagnosis of AL always requires biopsy. Tissue diagnosis may be needed occasionally to detect ATTR when nuclear scintigraphy shows visual grade < 2, urine and serum tests are negative for AL, and clinical, echocardiographic and/or MRI findings are suggestive of CA. hATTR associated with the Ser77Tyr and P64L variants has been reported to present with an atypical appearance on nuclear scintigraphy with only grade 1 uptake, despite having classic clinical, morphological and functional features on echocardiography and CMR.[62] For these patients, tissue diagnosis becomes the definitive method to establish diagnosis of ATTR.
The apple-green birefringence pattern on Congo red–stained sections under a polarized light microscope is characteristic for amyloid tissue identification. Amyloid typing, which is essential to determine whether it is AL or ATTR, is performed by immunohistochemistry and mass spectrometry techniques. While endomyocardial biopsy has a 100% sensitivity for the diagnosis of CA, there is potential risk of ventricular perforation and ultimately cardiac tamponade and ventricular arrhythmias.[63,64] Abdominal fat pad fine-needle aspiration biopsy is another option but its low sensitivity, particularly in wtATTR (about 15%), as well as high rate of inadequate specimens makes it a less reliable test.[65]
BIOMARKERS AND STAGING OF CA
The risk stratification and staging currently places great emphasis on blood biomarkers. Natriuretic peptides, including brain natriuretic peptide (BNP) and N-terminal-proBNP, as well as troponin have been looked at extensively for their diagnostic and prognostic value in CA. While elevated BNP and NT-proBNP is universally present in CA, chronically elevated level of serum troponin is not uncommon in CA and predicts poor prognosis.[66]
These biomarkers have been used to propose several staging systems in CA for assessment of severity of the disease. For wtATTR, 2 staging systems exist. The first one used thresholds of troponin T (0.05 ng/mL) and NT-proBNP (3,000 pg/mL). The 4-year overall survival was estimated to be 57%, 42%, and 18% for stage I (both values below cutoff), stage II (one value above cutoff), and stage III (both above cutoff), respectively.[12] A subsequent study that examined both wtATTR and hATTR substituted troponin with estimated glomerular filtration rate (eGFR) of 45 mL/min as threshold. Median survival was 69, 47, and 24 months in stages I, II, and III, respectively.[67]
For AL, Mayo staging system initially proposed utilization of both troponin (troponin-T < 0.035 µg/L or troponin-I < 0.1 µg/L) and NT-proBNP (< 322 ng/L) and defined stages I, II, and III based on whether neither, one, or both of these markers are above the normal limit.[68] Stages I, II and III predicted a median survival of 27.2, 11.1, and 4.1 months, respectively. A subsequent staging system comprising of difference between involved and uninvolved free light chains (FLC-diff), troponin T and NT-proBNP defined stages I, II, III, and IV, based on whether none, one, two, or all three factors were above the normal limit, and correlated with a median overall survival of 94, 40, 14, and 6 months, respectively.[69]
MANAGEMENT OF CA
Congestive Heart Failure
CA patients are at an increased risk of hospitalizations related to heart failure with longer length of stay and higher mortality compared to non-amyloid heart failure populations.[70,71] Loop diuretics remain the mainstay of treatment to mitigate clinical congestion, in combination with sodium-restricted diet. In case of severe fluid retention, metolazone could also be concomitantly administered on intermittent basis, and spironolactone could be an option if renal function permits. Among loop diuretics, while furosemide could be used in CA, the greater bioavailability and more consistent rate of absorption in heart failure make bumetanide and torsemide preferred agents. Importantly, CA patients are unusually sensitive to diuretics due to reduced ventricular compliance, altered ventricular-vascular coupling and age-related autonomic dysfunction; therefore, over diuresis could lead to hypotension and renal dysfunction.[72]
Heart failure management becomes even more challenging in CA patients with systolic dysfunction, as most of the guideline-directed medical therapies are generally poorly-tolerated. Negative chronotropic effect of beta blockers blunts the compensatory increase in heart rate necessary to maintain adequate cardiac output in the context of low fixed stroke volume. Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers can cause symptomatic hypotension and can worsen underlying preexisting renal dysfunction. Non-dihydropyridine calcium channel blockers are not recommended in CA as they bind avidly to amyloid fibrils, causing enhanced negative chronotropic effects that manifest as heart block and shock.[73,74] While digoxin can also bind to amyloid fibrils, cautious use with lower doses and frequent monitoring of serum drug level and kidney function has been found to be safe in CA.[75,76]
Arrhythmias
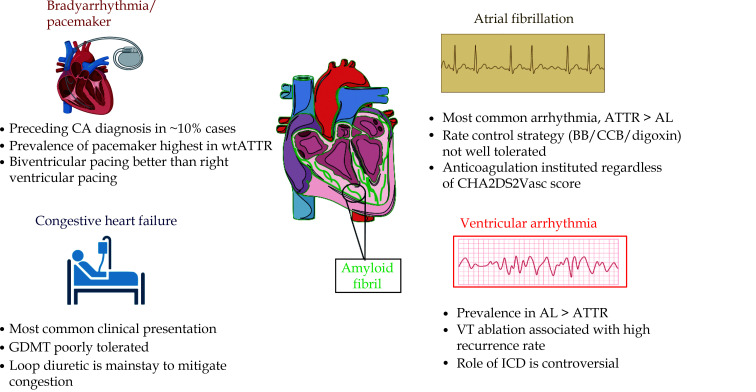
Atrial arrhythmia
Atrial fibrillation is the most common electrophysiological manifestation of CA (Figure 5). CA is associated with a higher prevalence of atrial fibrillation compared with age-matched population without CA, and the prevalence is higher in wtATTR than both hATTR and AL.[77,78] There are different pathophysiological mechanisms that potentiate development of atrial fibrillation in CA including atrial amyloid infiltration, electromechanical disruption from amyloid deposition, increased atrial afterload, increased atrial preload due to tricuspid and/or mitral regurgitation, increased atrial wall stress and remodelling due to chamber dilation, and autonomic dysfunction.[77]
Figure 5.
Summary of key points in the management of congestive heart failure and arrhythmias in cardiac amyloidosis.
AL: immunoglobulin light chain amyloidosis; ATTR: transthyretin amyloidosis; BB: beta blocker; CCB: calcium channel blocker; CA: cardiac amyloidosis; ICD: implantable-cardioverter defibrillator; GDMT: guideline-directed medical therapies; VT: ventricular tachycardia; wtATTR: wild-type transthyretin amyloidosis.
The rate control strategy is often not well tolerated, as administration of these negative chronotropic agents frequently precipitates symptomatic orthostatic hypotension and cardiac decompensation. In addition, loss of much needed atrial ‘kick’ in CA exacerbates ventricular filling impairment due to which atrial fibrillation is often symptomatic. Therefore, restoration of sinus rhythm is preferable. Direct current cardioversion is an effective strategy to restore rhythm in CA, but transesophageal echocardiogram should be performed prior to cardioversion due to high incidence of intracardiac thrombus in these patients.[79] Amiodarone has a favorable profile, as many antiarrhythmic agents are contraindicated in CA either due to cardiomyopathy (such as flecainide and propafenone) or due to significant renal insufficiency (such as sotalol, dronedarone and dofetilide). Atrial fibrillation in CA is associated with particularly heightened of cardioembolic stroke, and therefore guidelines recommend anticoagulation therapy irrespective of CHA2DS2VASc score.[80] Both direct oral anticoagulants and vitamin K antagonists can be used to provide thromboembolic protection in CA, and have comparable efficacy and bleeding rates.[77]
Ventricular arrhythmia
Ventricular arrhythmias are also common in CA, and the prevalence is higher in AL than ATTR. The pathogenetic mechanisms of ventricular arrhythmias include activation of inflammatory cascade from direct amyloid deposition and toxic effect on the myocardium, and electro-mechanical as well as autonomic dysfunction that are uniquely related to systemic amyloid deposition. The role of catheter ablation to treat ventricular arrhythmias in CA has not been examined in large-scale studies, but some case reports have shown successful radiofrequency VT ablation in these patients.[81] Finally, the role of implantable cardioverter-defibrillator is controversial, and while successful termination of life-threatening ventricular arrhythmias has been reported in few studies, there has been no evidence of improvement in survival when used for primary or secondary prevention in CA.[82,83] Guidelines recommend individualized decision making for both primary and secondary prevention with implantable cardioverter-defibrillators in CA.[84]
Bradyarrhythmia
Conduction system disease from amyloid infiltration commonly manifests as AV nodal disease, often preceding the diagnosis of CA and resulting in pacemaker implantation in about 10% of ATTR patients.[85] The prevalence of pacemaker implantation is reported to be highest in patients with wtATTR, potentially attributed to old age and chronic amyloid deposition over the course of many years. Right ventricular pacing burden is a consequence of worsening AV conduction disease in these patients. A study that analyzed cardiac implantable electronic device data in 34 CA patients found that right ventricular pacing increased from an average pacing burden of 35% at 6 months post-implantation to 96% by 5 years of follow-up.[86] Since right ventricular pacing causes interventricular desynchrony and can ultimately lead to development of pacing-induced cardiomyopathy, biventricular pacing has been proposed as a safer and better alternative that has been shown to improve LVEF, New York Heart Association functional class, and severity of mitral regurgitation.[87]
Amyloid-specific Disease-modifying Therapies
Management of ATTR
TTR Silencers
RNA interference (RNAi) has evolved as an endogenous cellular mechanism for controlling gene expression in which small interfering RNAs (siRNAs) inhibit the expression of specific genes by mediating the degradation of messenger RNA.[88] TTR silencers suppress synthesis of TTR (Figure 6), and have been approved by FDA for treatment of hATTR associated neuropathy. Patisiran is the first siRNA medication to achieve FDA approval after a phase III randomized double-blinded placebo-controlled international multicenter study (APOLLO) that demonstrated its efficacy in improving polyneuropathy, quality of life, nutritional status, and autonomic function.[89] It is an intravenous medication, administered as 0.3 mg/kg infusion every 3 weeks (maximum dose of 30 mg), and requires premedication with steroids. The common side effects are infusion-related reactions and vitamin A deficiency, due to which 3,000 IU vitamin A daily is recommended.
Figure 6.
Mechanisms of amyloid-specific therapies for transthyretin cardiac amyloidosis.
Silencers suppress the production of transthyretin in the liver. Stabilizers act to stabilize transthyretin tetramers to prevent dissociation and aggregation into amyloid fibrils. Degraders work by degrading amyloid fibrils and extracting them from the myocardium. ATTR: transthyretin amyloidosis; TTR: transthyretin.
Inotersen is a 2′-O-methoxyethyl-modified phosphorothioate antisense oligonucleotide, and the 2′-phosphorothioate modification enhances nuclease resistance and protein binding, thereby enhancing the potency and efficacy of inotersen.[90] In the NEURO-TTR trial, 300 mg inotersen administered weekly via subcutaneous injection stabilized neuropathy and quality of life in patients with hATTR with polyneuropathy with or without cardiac involvement.[91] Serious adverse events included glomerulonephritis (3%), severe thrombocytopenia of platelet count < 25 × 103/μL (3%), and one death due to intracranial hemorrhage in the setting of severe thrombocytopenia. Inotersen has been approved by the FDA for hATTR polyneuropathy, and its administration requires weekly monitoring of platelet counts and monitoring of renal function and urinary protein every 2 weeks.
TTR stabilizers
TTR stabilizers prevent dissociation of TTR tetramers into monomers, which is the rate-limiting step in amyloid synthesis (Figure 6). Tafamidis is the first oral drug approved by the FDA for both wtATTR and hATTR after an international multicenter double-blinded placebo-controlled phase III trial (ATTR-ACT), comprising of 441 ATTR patients demonstrated reduced all-cause mortality, cardiovascular-related hospitalizations, and decline in functional capacity and quality of life.[92] In a follow-up period of 30 months, relative risk reduction in mortality was 32%, absolute risk reduction was 13%, and numbers needed to treat were 7.5 to prevent 1 death over 30 months and 4 to prevent 1 hospitalization over 12 months. Tafamidis is administered as 80 mg (4 × 20 mg) oral daily (Vyndaqel) or 61 mg oral daily (Vyndamax), and does not have any known side effects.
Diflunisal is an FDA-approved nonsteroidal anti-inflammatory drug (NSAID) that also has TTR stabilizing properties. An international randomized double-blind placebo-controlled study that used diflunisal 250mg twice daily found that it was well tolerated, and it successfully slowed progression of familial amyloid polyneuropathy as well as preserved quality of life.[93] Multiple single center studies have also demonstrated encouraging results with diflunisal in terms of slowing neurological and cardiac function impairment in ATTR, and sustaining a good safety profile.[94] Importantly, the dose used in ATTR, 250 mg twice daily, is half the FDA approved recommended starting dose for diflunisal as an anti-inflammatory, which could potentially explain the low rates of bleeding and less gastric side effects. While low cost and potential efficacy could make diflunisal a reasonable alternative for ATTR patients who cannot afford FDA-approved therapies, it’s use should be avoided in patients with advanced renal dysfunction, refractory heart failure or high bleeding risk.
AG10 is a selective TTR stabilizer that has demonstrated greater potency in stabilizing TTR compared with Tafamidis in vitro.[95] A phase II study showed that AG10-201 achieved ~90% stabilization of TTR in patient serum.[96] A phase III, randomized, double-blind, placebo-controlled study of the efficacy and safety of AG10 in ATTR patients (ATTRibute-CM Trial), comprising of 510 participants, is currently underway (NCT03860935).
TTR Degraders
Therapeutics in this group are under active investigation. NI006 (Neurimmune) is a recombinant IgG1 human monoclonal antibody that targets both wtATTR and hATTR, and study to evaluate its safety and efficacy in ATTR is currently ongoing (NCT04360434). PRX-004 (Prothena Biosciences) is an intravenous monoclonal antibody that binds to ATTR and removes amyloid deposits in the myocardium. The combination of doxycycline and tauroursodeoxycholic acid (TUDCA) has been examined for TTR degradation, but results have not been promising clinically and significant gastrointestinal and dermatologic side effects have been witnessed.[97,98]
Management of AL
AL-specific treatment is usually reserved for the experienced hematologist. Based on the patient’s classification to the appropriate risk group, the most commonly used regimens are anti-plasma cell therapy and autologous stem cell transplant.[99] Anti–plasma cell therapies include proteasome inhibitors (bortezomib or caflizomib), immunomodulatory drugs (lenalidomide and pomalidomide), and monoclonal antibodies against plasma cell surface antigens (daratumumab). Hematological response to treatment is graded as complete (CR), very good partial (VGPR), partial (PR), or none (NR).[100] CR is when serum and urine immunofixation electrophoresis is negative and serum immunoglobulin free light chain ratio is within normal limits. VGPR is when FLC-diff < 4 mg/dL, PR is defined as FLC-diff decrease ≥ 50% and NR is defined as response < PR. Cardiac response is assessed using NT-proBNP levels, and the goal of treatment in cardiac involvement should be a > 30% reduction in NT-proBNP.[100]
CONCLUSIONS
CA is primarily caused by ATTR and AL, and both these subtypes have classic clinical, EKG, echocardiographic and CMR features that can raise suspicion for CA. While ATTR is almost always diagnosed noninvasively with the help of radionuclide scintigraphy using bone-avid tracers, AL always requires biopsy for definitive diagnosis. General management of heart failure and arrhythmias is same for both ATTR and AL, but amyloid-specific therapies are different.
References
- 1.Merlini G, Bellotti V Molecular mechanisms of amyloidosis. N Engl J Med. 2003;349:583–596. doi: 10.1056/NEJMra023144. [DOI] [PubMed] [Google Scholar]
- 2.Falk RH Diagnosis and management of the cardiac amyloidoses. Circulation. 2005;112:2047–2060. doi: 10.1161/CIRCULATIONAHA.104.489187. [DOI] [PubMed] [Google Scholar]
- 3.Masri A, Bukhari S, Eisele YS, et al Molecular imaging of cardiac amyloidosis. J Nucl Med. 2020;61:965–970. doi: 10.2967/jnumed.120.245381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.González-López E, Gallego-Delgado M, Guzzo-Merello G, et al Wild-type transthyretin amyloidosis as a cause of heart failure with preserved ejection fraction. Eur Heart J. 2015;36:2585–2594. doi: 10.1093/eurheartj/ehv338. [DOI] [PubMed] [Google Scholar]
- 5.Castaño A, Narotsky DL, Hamid N, et al Unveiling transthyretin cardiac amyloidosis and its predictors among elderly patients with severe aortic stenosis undergoing transcatheter aortic valve replacement. Eur Heart J. 2017;38:2879–2887. doi: 10.1093/eurheartj/ehx350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maurizi N, Rella V, Fumagalli C, et al Prevalence of cardiac amyloidosis among adult patients referred to tertiary centres with an initial diagnosis of hypertrophic cardiomyopathy. Int J Cardiol. 2020;300:191–195. doi: 10.1016/j.ijcard.2019.07.051. [DOI] [PubMed] [Google Scholar]
- 7.Tanskanen M, Peuralinna T, Polvikoski T, et al Senile systemic amyloidosis affects 25% of the very aged and associates with genetic variation in alpha2-macroglobulin and tau: a population-based autopsy study. Ann Med. 2008;40:232–239. doi: 10.1080/07853890701842988. [DOI] [PubMed] [Google Scholar]
- 8.Ravichandran S, Lachmann HJ, Wechalekar AD Epidemiologic and survival trends in amyloidosis, 1987-2019. N Engl J Med. 2020;382:1567–1568. doi: 10.1056/NEJMc1917321. [DOI] [PubMed] [Google Scholar]
- 9.Kyle RA, Linos A, Beard CM, et al Incidence and natural history of primary systemic amyloidosis in Olmsted County, Minnesota, 1950 through 1989. Blood. 1992;79:1817–1822. doi: 10.1182/blood.V79.7.1817.1817. [DOI] [PubMed] [Google Scholar]
- 10.Shi J, Guan J, Jiang B, et al Amyloidogenic light chains induce cardiomyocyte contractile dysfunction and apoptosis via a non-canonical p38alpha MAPK pathway. Proc Natl Acad Sci U S A. 2010;107:4188–4193. doi: 10.1073/pnas.0912263107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palladini G, Hegenbart U, Milani P, et al A staging system for renal outcome and early markers of renal response to chemotherapy in AL amyloidosis. Blood. 2014;124:2325–2332. doi: 10.1182/blood-2014-04-570010. [DOI] [PubMed] [Google Scholar]
- 12.Grogan M, Scott CG, Kyle RA, et al Natural history of wild-type transthyretin cardiac amyloidosis and risk stratification using a novel staging system. J Am Coll Cardiol. 2016;68:1014–1020. doi: 10.1016/j.jacc.2016.06.033. [DOI] [PubMed] [Google Scholar]
- 13.Pilebro B, Suhr OB, Näslund U, et al (99m)Tc-DPD uptake reflects amyloid fibril composition in hereditary transthyretin amyloidosis. Ups J Med Sci. 2016;121:17–24. doi: 10.3109/03009734.2015.1122687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Buxbaum J, Jacobson DR, Tagoe C, et al Transthyretin V122I in African Americans with congestive heart failure. J Am Coll Cardiol. 2006;47:1724–1725. doi: 10.1016/j.jacc.2006.01.042. [DOI] [PubMed] [Google Scholar]
- 15.Reilly MM, Staunton H, Harding AE Familial amyloid polyneuropathy (TTR ala 60) in north west Ireland: a clinical, genetic, and epidemiological study. J Neurol Neurosurg Psychiatry. 1995;59:45–49. doi: 10.1136/jnnp.59.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bonaïti B, Olsson M, Hellman U, et al TTR familial amyloid polyneuropathy: does a mitochondrial polymorphism entirely explain the parent-of-origin difference in penetrance? Eur J Hum Genet. 2010;18:948–952. doi: 10.1038/ejhg.2010.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Waddington-Cruz M, Wixner J, Amass L, et al THAOS investigators. Characteristics of patients with late- vs. early-onset Val30Met Transthyretin Amyloidosis from the Transthyretin Amyloidosis Outcomes Survey (THAOS) Neurol Ther. 2021;10:753–766. doi: 10.1007/s40120-021-00258-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maurer MS, Hanna M, Grogan M, et al THAOS Investigators. Genotype and phenotype of transthyretin cardiac amyloidosis: THAOS (Transthyretin Amyloid Outcome Survey) J Am Coll Cardiol. 2016;68:161–172. doi: 10.1016/j.jacc.2016.03.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dungu JN, Valencia O, Pinney JH, et al CMR-based differentiation of AL and ATTR cardiac amyloidosis. JACC Cardiovasc Imaging. 2014;7:133–142. doi: 10.1016/j.jcmg.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 20.Griffin JM, Rosenblum H, Maurer MS Pathophysiology and therapeutic approaches to cardiac amyloidosis. Circ Res. 2021;128:1554–1575. doi: 10.1161/CIRCRESAHA.121.318187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bukhari S, Oliveros E, Parekh H, et al Epidemiology, mechanisms, and management of atrial fibrillation in cardiac amyloidosis. Curr Probl Cardiol. 2022;48:101571. doi: 10.1016/j.cpcardiol.2022.101571. [DOI] [PubMed] [Google Scholar]
- 22.Oye M, Dhruva P, Kandah F, et al Cardiac amyloid presenting as cardiogenic shock: case series. Eur Heart J Case Rep. 2021;5:ytab252. doi: 10.1093/ehjcr/ytab252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mueller PS, Edwards WD, Gertz MA Symptomatic ischemic heart disease resulting from obstructive intramural coronary amyloidosis. Am J Med. 2000;109:181–188. doi: 10.1016/S0002-9343(00)00471-X. [DOI] [PubMed] [Google Scholar]
- 24.Dorbala S, Vangala D, Bruyere J Jr, et al Coronary microvascular dysfunction is related to abnormalities in myocardial structure and function in cardiac amyloidosis. JACC Heart Fail. 2014;2:358–367. doi: 10.1016/j.jchf.2014.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nitsche C, Scully PR, Patel KP, et al Prevalence and outcomes of concomitant aortic stenosis and cardiac amyloidosis. J Am Coll Cardiol. 2021;77:128–139. doi: 10.1016/j.jacc.2020.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Milandri A, Farioli A, Gagliardi C, et al Carpal tunnel syndrome in cardiac amyloidosis: implications for early diagnosis and prognostic role across the spectrum of aetiologies. Eur J Heart Fail. 2020;22:507–515. doi: 10.1002/ejhf.1742. [DOI] [PubMed] [Google Scholar]
- 27.Sperry BW, Reyes BA, Ikram A, et al Tenosynovial and cardiac amyloidosis in patients undergoing carpal tunnel release. J Am Coll Cardiol. 2018;72:2040–2050. doi: 10.1016/j.jacc.2018.07.092. [DOI] [PubMed] [Google Scholar]
- 28.Westin O, Fosbøl EL, Maurer MS et al Screening for cardiac amyloidosis 5 to 15 years after surgery for bilateral carpal tunnel syndrome. J Am Coll Cardiol. 2022;80:967–977. doi: 10.1016/j.jacc.2022.06.026. [DOI] [PubMed] [Google Scholar]
- 29.Maurer MS, Smiley D, Simsolo E, et al Analysis of lumbar spine stenosis specimens for identification of amyloid. J Am Geriatr Soc. 2022;70:3538–3548. doi: 10.1111/jgs.17976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Geller HI, Singh A, Alexander KM, et al Association between ruptured distal biceps tendon and wild-type transthyretin cardiac amyloidosis. JAMA. 2017;318:962–963. doi: 10.1001/jama.2017.9236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rubin J, Alvarez J, Teruya S, et al Hip and knee arthroplasty are common among patients with transthyretin cardiac amyloidosis, occurring years before cardiac amyloid diagnosis: can we identify affected patients earlier? Amyloid. 2017;24:226–230. doi: 10.1080/13506129.2017.1375908. [DOI] [PubMed] [Google Scholar]
- 32.Dember LM Amyloidosis-associated kidney disease. J Am Soc Nephrol. 2006;17:3458–3471. doi: 10.1681/ASN.2006050460. [DOI] [PubMed] [Google Scholar]
- 33.Sharma A, Bansal S, Jain R Unique morphology of intratubular light chain casts in multiple myeloma: the amyloid cast nephropathy. Indian J Pathol Microbiol. 2014;57:629–631. doi: 10.4103/0377-4929.142712. [DOI] [PubMed] [Google Scholar]
- 34.Cipriani A, De Michieli L, Porcari A et al Low QRS voltages in cardiac amyloidosis: clinical correlates and prognostic value. JACC Cardio Oncol. 2022;4:458–470. doi: 10.1016/j.jaccao.2022.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cyrille NB, Goldsmith J, Alvarez J, et al Prevalence and prognostic significance of low QRS voltage among the three main types of cardiac amyloidosis. Am J Cardiol. 2014;114:1089–1093. doi: 10.1016/j.amjcard.2014.07.026. [DOI] [PubMed] [Google Scholar]
- 36.Dungu J, Sattianayagam PT, Whelan CJ, et al The electrocardiographic features associated with cardiac amyloidosis of variant transthyretin isoleucine 122 type in Afro-Caribbean patients. Am Heart J. 2012;164:72–79. doi: 10.1016/j.ahj.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 37.Murtagh B, Hammill SC, Gertz MA, et al Electrocardiographic findings in primary systemic amyloidosis and biopsy-proven cardiac involvement. Am J Cardiol. 2005;95:535–537. doi: 10.1016/j.amjcard.2004.10.028. [DOI] [PubMed] [Google Scholar]
- 38.Das MK, Khan B, Jacob S et al Significance of a fragmented QRS complex versus a Q wave in patients with coronary artery disease. Circulation. 2006;113:2495–2501. doi: 10.1161/CIRCULATIONAHA.105.595892. [DOI] [PubMed] [Google Scholar]
- 39.González-López E, Gagliardi C, Dominguez F, et al Clinical characteristics of wild-type transthyretin cardiac amyloidosis: disproving myths. Eur Heart J. 2017;38:1895–1904. doi: 10.1093/eurheartj/ehx043. [DOI] [PubMed] [Google Scholar]
- 40.Falk RH, Alexander KM, Liao R, et al AL (Light-Chain) cardiac amyloidosis: a review of diagnosis and therapy. J Am Coll Cardiol. 2016;68:1323–1341. doi: 10.1016/j.jacc.2016.06.053. [DOI] [PubMed] [Google Scholar]
- 41.Nagy D, Révész K, Peskó G, et al Cardiac amyloidosis with normal wall thickness: prevalence, clinical characteristics and outcome in a retrospective analysis. Biomedicines. 2022;10:1765. doi: 10.3390/biomedicines10071765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vermeer AMC, Janssen A, Boorsma PC, et al Transthyretin amyloidosis: a phenocopy of hypertrophic cardiomyopathy. Amyloid. 2017;24:87–91. doi: 10.1080/13506129.2017.1322573. [DOI] [PubMed] [Google Scholar]
- 43.López-Sainz Á, de Haro-Del Moral FJ, Dominguez F, et al Prevalence of cardiac amyloidosis among elderly patients with systolic heart failure or conduction disorders. Amyloid. 2019;26:156–163. doi: 10.1080/13506129.2019.1625322. [DOI] [PubMed] [Google Scholar]
- 44.Pagourelias ED, Mirea O, Duchenne J, et al Echo parameters for differential diagnosis in cardiac amyloidosis: a head-to-head comparison of deformation and nondeformation parameters. Circ Cardiovasc Imaging. 2017;10:e005588. doi: 10.1161/CIRCIMAGING.116.005588. [DOI] [PubMed] [Google Scholar]
- 45.Phelan D, Collier P, Thavendiranathan P, et al Relative apical sparing of longitudinal strain using two-dimensional speckle-tracking echocardiography is both sensitive and specific for the diagnosis of cardiac amyloidosis. Heart. 2012;98:1442–1448. doi: 10.1136/heartjnl-2012-302353. [DOI] [PubMed] [Google Scholar]
- 46.Maceira AM, Joshi J, Prasad SK, et al Cardiovascular magnetic resonance in cardiac amyloidosis. Circulation. 2005;111:186–193. doi: 10.1161/01.CIR.0000152819.97857.9D. [DOI] [PubMed] [Google Scholar]
- 47.Fontana M, Pica S, Reant P, et al Prognostic value of late gadolinium enhancement cardiovascular magnetic resonance in cardiac amyloidosis. Circulation. 2015;132:1570–1579. doi: 10.1161/CIRCULATIONAHA.115.016567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang L, Krefting I, Gorovets A, et al Nephrogenic systemic fibrosis and class labeling of gadolinium-based contrast agents by the Food and Drug Administration. Radiology. 2012;265:248–253. doi: 10.1148/radiol.12112783. [DOI] [PubMed] [Google Scholar]
- 49.Karamitsos TD, Piechnik SK, Banypersad SM, et al Noncontrast T1 mapping for the diagnosis of cardiac amyloidosis. JACC Cardiovasc Imaging. 2013;6:488–497. doi: 10.1016/j.jcmg.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 50.Banypersad SM, Fontana M, Maestrini V, et al T1 mapping and survival in systemic light-chain amyloidosis. Eur Heart J. 2015;36:244–251. doi: 10.1093/eurheartj/ehu444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Martinez-Naharro A, Kotecha T, Norrington K, et al Native T1 and extracellular volume in transthyretin amyloidosis. JACC Cardiovasc Imaging. 2019;12:810–819. doi: 10.1016/j.jcmg.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 52.Banypersad SM, Sado DM, Flett AS, et al Quantification of myocardial extracellular volume fraction in systemic AL amyloidosis: an equilibrium contrast cardiovascular magnetic resonance study. Circ Cardiovasc Imaging. 2013;6:34–39. doi: 10.1161/CIRCIMAGING.112.978627. [DOI] [PubMed] [Google Scholar]
- 53.Martinez-Naharro A, Abdel-Gadir A, Treibel TA, et al CMR-verified regression of cardiac AL amyloid after chemotherapy. JACC Cardiovasc Imaging. 2018;11:152–154. doi: 10.1016/j.jcmg.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 54.Kotecha T, Martinez-Naharro A, Treibel TA, et al Myocardial edema and prognosis in amyloidosis. J Am Coll Cardiol. 2018;71:2919–2931. doi: 10.1016/j.jacc.2018.03.536. [DOI] [PubMed] [Google Scholar]
- 55.Rapezzi C, Gagliardi C, Milandri A Analogies and disparities among scintigraphic bone tracers in the diagnosis of cardiac and non-cardiac ATTR amyloidosis. J Nucl Cardiol. 2019;26:1638–1641. doi: 10.1007/s12350-018-1235-6. [DOI] [PubMed] [Google Scholar]
- 56.Stats MA, Stone JR Varying levels of small microcalcifications and macrophages in ATTR and AL cardiac amyloidosis: implications for utilizing nuclear medicine studies to subtype amyloidosis. Cardiovasc Pathol. 2016;25:413–417. doi: 10.1016/j.carpath.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 57.Perugini E, Guidalotti PL, Salvi F, et al Noninvasive etiologic diagnosis of cardiac amyloidosis using 99mTc-3, 3-diphosphono-1, 2-propanodicarboxylic acid scintigraphy. J Am Coll Cardiol. 2005;46:1076–1084. doi: 10.1016/j.jacc.2005.05.073. [DOI] [PubMed] [Google Scholar]
- 58.Gillmore JD, Maurer MS, Falk RH, et al Nonbiopsy diagnosis of cardiac transthyretin amyloidosis. Circulation. 2016;133:2404–2412. doi: 10.1161/CIRCULATIONAHA.116.021612. [DOI] [PubMed] [Google Scholar]
- 59.Bokhari S, Castaño A, Pozniakoff T, et al (99m)Tc-pyrophosphate scintigraphy for differentiating light-chain cardiac amyloidosis from the transthyretin-related familial and senile cardiac amyloidoses. Circ Cardiovasc Imaging. 2013;6:195–201. doi: 10.1161/CIRCIMAGING.112.000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Masri A, Bukhari S, Ahmad S, et al Efficient 1-hour technetium-99 m pyrophosphate imaging protocol for the diagnosis of transthyretin cardiac amyloidosis. Circ Cardiovasc Imaging. 2020;13:e010249. doi: 10.1161/CIRCIMAGING.119.010249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Falk RH, Lee VW, Rubinow A, et al Sensitivity of technetium-99m-pyrophosphate scintigraphy in diagnosing cardiac amyloidosis. Am J Cardiol. 1983;51:826–830. doi: 10.1016/S0002-9149(83)80140-4. [DOI] [PubMed] [Google Scholar]
- 62.Musumeci MB, Cappelli F, Russo D, et al Low sensitivity of bone scintigraphy in detecting Phe64Leu mutation-related transthyretin cardiac amyloidosis. JACC Cardiovasc Imaging. 2020;13:1314–1321. doi: 10.1016/j.jcmg.2019.10.015. [DOI] [PubMed] [Google Scholar]
- 63.Ardehali H, Qasim A, Cappola T, et al Endomyocardial biopsy plays a role in diagnosing patients with unexplained cardiomyopathy. Am Heart J. 2004;147:919–923. doi: 10.1016/j.ahj.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 64.Holzmann M, Nicko A, Kühl U, et al Complication rate of right ventricular endomyocardial biopsy via the femoral approach: a retrospective and prospective study analyzing 3048 diagnostic procedures over an 11-year period. Circulation. 2008;118:1722–1728. doi: 10.1161/CIRCULATIONAHA.107.743427. [DOI] [PubMed] [Google Scholar]
- 65.Guy CD, Jones CK Abdominal fat pad aspiration biopsy for tissue confirmation of systemic amyloidosis: specificity, positive predictive value, and diagnostic pitfalls. Diagn Cytopathol. 2001;24:181–185. doi: 10.1002/1097-0339(200103)24:3<181::AID-DC1037>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 66.Takashio S, Yamamuro M, Izumiya Y, et al Diagnostic utility of cardiac troponin T level in patients with cardiac amyloidosis. ESC Heart Fail. 2018;5:27–35. doi: 10.1002/ehf2.12203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gillmore JD, Damy T, Fontana M, et al A new staging system for cardiac transthyretin amyloidosis. Eur Heart J. 2018;39:2799–2806. doi: 10.1093/eurheartj/ehx589. [DOI] [PubMed] [Google Scholar]
- 68.Dispenzieri A, Gertz MA, Kyle RA, et al Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol. 2004;22:3751–3757. doi: 10.1200/JCO.2004.03.029. [DOI] [PubMed] [Google Scholar]
- 69.Kumar S, Dispenzieri A, Lacy MQ, et al Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol. 2012;30:989–995. doi: 10.1200/JCO.2011.38.5724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gilstrap LG, Dominici F, Wang Y, et al Epidemiology of cardiac amyloidosis-associated heart failure hospitalizations among fee-for-service medicare beneficiaries in the United States. Circ Heart Fail. 2019;12:e005407. doi: 10.1161/CIRCHEARTFAILURE.118.005407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sperry BW, Saeed IM, Raza S, et al Increasing rate of hospital admissions in patients with amyloidosis (from the National Inpatient Sample) Am J Cardiol. 2019;124:1765–1769. doi: 10.1016/j.amjcard.2019.08.045. [DOI] [PubMed] [Google Scholar]
- 72.Chan N, Hanna M, Maurer MS The Wiggers Diagram: hemodynamic changes in cardiac amyloidosis. J Card Fail. 2023;29:217–219. doi: 10.1016/j.cardfail.2022.06.008. [DOI] [PubMed] [Google Scholar]
- 73.Gertz MA, Falk RH, Skinner M, et al Worsening of congestive heart failure in amyloid heart disease treated by calcium channel-blocking agents. Am J Cardiol. 1985;55:1645. doi: 10.1016/0002-9149(85)90995-6. [DOI] [PubMed] [Google Scholar]
- 74.Gertz MA, Skinner M, Connors LH, et al Selective binding of nifedipine to amyloid fibrils. Am J Cardiol. 1985;55:1646. doi: 10.1016/0002-9149(85)90996-8. [DOI] [PubMed] [Google Scholar]
- 75.Rubinow A, Skinner M, Cohen AS Digoxin sensitivity in amyloid cardiomyopathy. Circulation. 1981;63:1285–1288. doi: 10.1161/01.CIR.63.6.1285. [DOI] [PubMed] [Google Scholar]
- 76.Muchtar E, Gertz MA, Kumar SK, et al Digoxin use in systemic light-chain (AL) amyloidosis: contra-indicated or cautious use? Amyloid. 2018;25:86–92. doi: 10.1080/13506129.2018.1449744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bukhari S, Khan SZ, Bashir Z Atrial fibrillation, thromboembolic risk, and anticoagulation in cardiac amyloidosis: a review. J Card Fail. 2023;29:76–86. doi: 10.1016/j.cardfail.2022.08.008. [DOI] [PubMed] [Google Scholar]
- 78.Bukhari S, Barakat AF, Eisele YS, et al Prevalence of atrial fibrillation and thromboembolic risk in wild-type transthyretin amyloid cardiomyopathy. Circulation. 2021;143:1335–1337. doi: 10.1161/CIRCULATIONAHA.120.052136. [DOI] [PubMed] [Google Scholar]
- 79.El-Am EA, Dispenzieri A, Melduni RM, et al Direct current cardioversion of atrial arrhythmias in adults with cardiac amyloidosis. J Am Coll Cardiol. 2019;73:589–597. doi: 10.1016/j.jacc.2018.10.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Heidenreich PA, Bozkurt B, Aguilar D, et al 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e876–e894. doi: 10.1161/CIR.0000000000001062. [DOI] [PubMed] [Google Scholar]
- 81.Chung FP, Lin YJ, Kuo L, et al Catheter ablation of ventricular tachycardia/fibrillation in a patient with right ventricular amyloidosis with initial manifestations mimicking arrhythmogenic right ventricular dysplasia/cardiomyopathy. Korean Circ J. 2017;47:282–285. doi: 10.4070/kcj.2016.0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lin G, Dispenzieri A, Kyle R, et al Implantable cardioverter defibrillators in patients with cardiac amyloidosis. J Cardiovasc Electrophysiol. 2013;24:793–798. doi: 10.1111/jce.12123. [DOI] [PubMed] [Google Scholar]
- 83.Higgins AY, Annapureddy AR, Wang Y, et al Survival following implantable cardioverter-defibrillator implantation in patients with amyloid cardiomyopathy. J Am Heart Assoc. 2020;9:e016038. doi: 10.1161/JAHA.120.016038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Al-Khatib SM, Stevenson WG, Ackerman MJ, et al 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2018;15:e73–e189. doi: 10.1016/j.hrthm.2017.10.036. [DOI] [PubMed] [Google Scholar]
- 85.Donnellan E, Wazni OM, Saliba WI, et al Prevalence, incidence, and impact on mortality of conduction system disease in transthyretin cardiac amyloidosis. Am J Cardiol. 2020;128:140–146. doi: 10.1016/j.amjcard.2020.05.021. [DOI] [PubMed] [Google Scholar]
- 86.Rehorn MR, Loungani RS, Black-Maier E, et al Cardiac implantable electronic devices: a window into the evolution of conduction disease in cardiac amyloidosis. JACC Clin Electrophysiol. 2020;6:1144–1154. doi: 10.1016/j.jacep.2020.04.020. [DOI] [PubMed] [Google Scholar]
- 87.Donnellan E, Wazni OM, Saliba WI, et al Cardiac devices in patients with transthyretin amyloidosis: Impact on functional class, left ventricular function, mitral regurgitation, and mortality. J Cardiovasc Electrophysiol. 2019;30:2427–2432. doi: 10.1111/jce.14180. [DOI] [PubMed] [Google Scholar]
- 88.Elbashir SM, Harborth J, Lendeckel W, et al Duplexes of 21-nucleotide RNAs mediate RNA interference in cultured mammalian cells. Nature. 2001;411:494–498. doi: 10.1038/35078107. [DOI] [PubMed] [Google Scholar]
- 89.Adams D, Gonzalez-Duarte A, O'Riordan WD, et al Patisiran, an RNAi therapeutic, for hereditary transthyretin amyloidosis. N Engl J Med. 2018;379:11–21. doi: 10.1056/NEJMoa1716153. [DOI] [PubMed] [Google Scholar]
- 90.Crooke ST, Wang S, Vickers TA, et al Cellular uptake and trafficking of antisense oligonucleotides. Nat Biotechnol. 2017;35:230–237. doi: 10.1038/nbt.3779. [DOI] [PubMed] [Google Scholar]
- 91.Benson MD, Waddington-Cruz M, Berk JL, et al Inotersen treatment for patients with hereditary transthyretin amyloidosis. N Engl J Med. 2018;379:22–31. doi: 10.1056/NEJMoa1716793. [DOI] [PubMed] [Google Scholar]
- 92.Maurer MS, Schwartz JH, Gundapaneni B, et al Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med. 2018;379:1007–1016. doi: 10.1056/NEJMoa1805689. [DOI] [PubMed] [Google Scholar]
- 93.Berk JL, Suhr OB, Obici L, et al Diflunisal Trial Consortium. Repurposing diflunisal for familial amyloid polyneuropathy:a randomized clinical trial. JAMA. 2013;310:2658–2667. doi: 10.1001/jama.2013.283815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sekijima Y, Tojo K, Morita H, et al Safety and efficacy of long-term diflunisal administration in hereditary transthyretin (ATTR) amyloidosis. Amyloid. 2015;22:79–83. doi: 10.3109/13506129.2014.997872. [DOI] [PubMed] [Google Scholar]
- 95.Penchala SC, Connelly S, Wang Y, et al AG10 inhibits amyloidogenesis and cellular toxicity of the familial amyloid cardiomyopathy-associated V122I transthyretin. Proc Natl Acad Sci U S A. 2013;110:9992–9997. doi: 10.1073/pnas.1300761110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Judge DP, Heitner SB, Falk RH, et al Transthyretin stabilization by AG10 in symptomatic transthyretin amyloid cardiomyopathy. J Am Coll Cardiol. 2019;74:285–295. doi: 10.1016/j.jacc.2019.03.012. [DOI] [PubMed] [Google Scholar]
- 97.Karlstedt E, Jimenez-Zepeda V, Howlett JG, et al Clinical experience with the use of doxycycline and ursodeoxycholic acid for the treatment of transthyretin cardiac amyloidosis. J Card Fail. 2019;25:147–153. doi: 10.1016/j.cardfail.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 98.Wixner J, Pilebro B, Lundgren HE, et al Effect of doxycycline and ursodeoxycholic acid on transthyretin amyloidosis. Amyloid. 2017;24:78–79. doi: 10.1080/13506129.2016.1269739. [DOI] [PubMed] [Google Scholar]
- 99.Hasib Sidiqi M, Gertz MA Immunoglobulin light chain amyloidosis diagnosis and treatment algorithm 2021. Blood Cancer J. 2021;11:90. doi: 10.1038/s41408-021-00483-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dispenzieri A, Buadi F, Kumar SK, et al Treatment of immunoglobulin light chain amyloidosis: Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) Consensus Statement. Mayo Clin Proc. 2015;90:1054–1081. doi: 10.1016/j.mayocp.2015.06.009. [DOI] [PubMed] [Google Scholar]