Abstract
BACKGROUND
Acute pancreatitis (AP) in liver transplant (LT) recipients may lead to poor clinical outcomes and development of severe complications.
AIM
We aimed to assess national trends, clinical outcomes, and the healthcare burden of LT hospitalizations with AP in the United States (US).
METHODS
The National Inpatient Sample was utilized to identify all adult (≥ 18 years old) LT hospitalizations with AP in the US from 2007–2019. Non-LT AP hospitalizations served as controls for comparative analysis. National trends of hospitalization characteristics, clinical outcomes, complications, and healthcare burden for LT hospitalizations with AP were highlighted. Hospitalization characteristics, clinical outcomes, complications, and healthcare burden were also compared between the LT and non-LT cohorts. Furthermore, predictors of inpatient mortality for LT hospitalizations with AP were identified. All P values ≤ 0.05 were considered statistically significant.
RESULTS
The total number of LT hospitalizations with AP increased from 305 in 2007 to 610 in 2019. There was a rising trend of Hispanic (16.5% in 2007 to 21.1% in 2018, P-trend = 0.0009) and Asian (4.3% in 2007 to 7.4% in 2019, p-trend = 0.0002) LT hospitalizations with AP, while a decline was noted for Blacks (11% in 2007 to 8.3% in 2019, P-trend = 0.0004). Furthermore, LT hospitalizations with AP had an increasing comorbidity burden as the Charlson Comorbidity Index (CCI) score ≥ 3 increased from 41.64% in 2007 to 62.30% in 2019 (P-trend < 0.0001). We did not find statistically significant trends in inpatient mortality, mean length of stay (LOS), and mean total healthcare charge (THC) for LT hospitalizations with AP despite rising trends of complications such as sepsis, acute kidney failure (AKF), acute respiratory failure (ARF), abdominal abscesses, portal vein thrombosis (PVT), and venous thromboembolism (VTE). Between 2007–2019, 6863 LT hospitalizations with AP were compared to 5649980 non-LT AP hospitalizations. LT hospitalizations with AP were slightly older (53.5 vs 52.6 years, P = 0.017) and had a higher proportion of patients with CCI ≥ 3 (51.5% vs 19.8%, P < 0.0001) compared to the non-LT cohort. Additionally, LT hospitalizations with AP had a higher proportion of Whites (67.9% vs 64.6%, P < 0.0001) and Asians (4% vs 2.3%, P < 0.0001), while the non-LT cohort had a higher proportion of Blacks and Hispanics. Interestingly, LT hospitalizations with AP had lower inpatient mortality (1.37% vs 2.16%, P = 0.0479) compared to the non-LT cohort despite having a higher mean age, CCI scores, and complications such as AKF, PVT, VTE, and the need for blood transfusion. However, LT hospitalizations with AP had a higher mean THC ($59596 vs $50466, P = 0.0429) than the non-LT cohort.
CONCLUSION
In the US, LT hospitalizations with AP were on the rise, particularly for Hispanics and Asians. However, LT hospitalizations with AP had lower inpatient mortality compared to non-LT AP hospitalizations.
Keywords: Liver transplantation, Pancreatitis, Mortality, Cost, Length of stay
Core Tip: Liver transplant (LT) is a lifesaving intervention for patients with end-stage liver disease. Acute pancreatitis (AP) in LT recipients may lead to poor clinical outcomes and development of severe complications. In this study, we noted an increase in LT hospitalizations with AP at a national level from 305 in 2007 to 610 in 2019 with a rising trend for Hispanics and Asians. However, there was no trend for inpatient mortality, mean length of stay and mean total healthcare charge. After a comparative analysis, LT hospitalizations with AP had lower inpatient mortality compared to the non-LT cohort despite a higher mean age, comorbidity burden, and presence of complications.
INTRODUCTION
Acute pancreatitis (AP), an inflammatory response to injury of the pancreas, is one of the leading causes of hospitalization amongst gastrointestinal disorders in the United States (US). In the general population, the incidence of AP is estimated to be 40-50 per 100000 persons and there are approximately 275000 AP hospitalizations annually in the US[1,2]. Risk factors implicated in the development of AP include cholelithiasis, heavy alcohol use (4-5 drinks daily for > 5 years), hypertriglyceridemia (> 1000 mg/dL), smoking, medications, autoimmune diseases, genetic predispositions, blunt/penetrating abdominal trauma, viral infections, and therapeutic endoscopic procedures such as endoscopic retrograde cholangiopancreatography (ERCP), among others[3-10]. The pathogenesis of AP is multi-factorial, but ultimately involves the unregulated activation of proteolytic enzymes within the pancreas eventually leading to pancreatic ductal obstruction, subsequent inflammation, and in severe cases a systemic-inflammatory response syndrome[11]. The characteristic clinical features of AP include nausea, vomiting, loss of appetite, and epigastric abdominal pain radiating to the back[12]. A diagnosis of AP can be established by the presence of any two of the following three criteria: (1) Characteristic epigastric abdominal pain; (2) serum lipase and/or amylase greater than three times the upper limit of normal; and (3) evidence of AP on abdominal imaging[13]. Over the years, AP hospitalizations are on a rise in the US, with mortality rates ranging from 1%-2% and over 2.5 billion dollars being spent annually on healthcare costs[1,14].
Liver transplant (LT) has revolutionized management for chronic end-stage liver disease with excellent results. Since the first LT in 1967, the procedure has saved close to 500000 Life-years among patients with acute fulminant hepatic failure, hepatocellular carcinoma (HCC), and end-stage liver disease[15,16]. The recipients of the procedure have excellent survival rates. Per the Scientific Registry of Transplant Recipients data, the overall patient survival rate after deceased donor LT was 90% and 77% at 1 year and 5 years, respectively[17]. Moreover, the graft survival rate at 1 year and 5 years after LT was noted to be 89.6% and 72.8%, respectively[18].
AP is an important risk factor for poor surgical outcomes in patients with LT. Studies have reported an incidence rate ranging from 3%-8% for post-LT pancreatitis[19,20]. Common risk factors implicated in the development of post-LT pancreatitis include hepatitis B infection as an indication of transplant, re-transplantation, duration of venous bypass, hypotension with longer procedural time, utilization of ERCP, type of biliary reconstruction, intraoperative calcium chloride administration, and use of an aorto-hepatic graft[19,21,22]. Additionally, surgical manipulation, immunosuppression, infections, and biliary complications before LT may also increase the risk of developing post-LT pancreatitis[23]. In LT recipients, peri-transplant pancreatitis is associated with a two-fold increased risk of mortality[24]. Furthermore, early AP in LT recipients (within 1-2 mo of LT) may have mortality rates as high as 67%[25]. Given the acute-organ shortage worldwide, we must identify LT hospitalizations at high risk of developing AP to maximize patient survival.
Although studies investigating post-LT pancreatitis currently exist, they are primarily limited to small single-center experiences[19,20,22,25-27]. Hence, this study was designed to investigate trends in hospitalization characteristics and clinical outcomes for LT hospitalizations with AP. Furthermore, we performed a comparative analysis between LT and non-LT hospitalizations with AP to determine the influence of LT on clinical outcomes and healthcare burden. Predictors of inpatient mortality for LT hospitalizations with AP were also identified.
MATERIALS AND METHODS
Design and data source
This retrospective study derived the study population from the National Inpatient Sample (NIS) for 2007–2019 which was coded using the International Classification of Diseases, 9th and 10th Revision, Clinical Modification (ICD-9/10- CM) diagnosis codes, and procedure codes. The NIS, maintained by the Healthcare Cost and Utilization Project (HCUP), is one of the largest, publicly available, multi-ethnic databases in the US. HCUP is a family of healthcare databases, related software tools, and products developed through a Federal-State-Industry partnership and sponsored by the Agency for Healthcare Research and Quality. The NIS enables medical researchers to analyze data on more than seven million hospital stays each year in the US. It approximates a 20-percent stratified sample of all discharges from US community hospitals, excluding rehabilitation and long-term acute care hospitals. The NIS database is publicly available at: https://www.hcup-us.ahrq.gov/.
Study population and outcome measures
We utilized the NIS to identify all adult (≥ 18 years old) LT hospitalizations with AP in the US from 2007–2019. National trends of hospitalization characteristics, clinical outcomes, complications, and the healthcare burden were highlighted. Furthermore, non-LT AP hospitalizations served as controls for a comparative analysis of hospitalization characteristics, clinical outcomes, complications, and the healthcare burden with the LT cohort. Predictors of inpatient mortality for LT hospitalizations with AP were also identified.
Statistical analysis
Statistical analysis was conducted using SAS 9.4 (SAS Institute Inc, Cary, NC, United States) to account for weights in the stratified survey design of the NIS. During the statistical estimating process, weights were considered by incorporating the variables for strata, weight to discharges and cluster. Descriptive statistics including mean (± standard error) for continuous variables, and count (%) for categorical variables were provided after statistical analysis. The Cochran-Armitage trend tests were implemented to test the trends for proportions of binary variables. The trends for the averages of age, mean length of stay (LOS) and mean total healthcare charge (THC) were examined by using linear regression. The Rao-Scott design-adjusted chi-square test examined the association between binary variables in LT and non-LT hospitalizations with AP. F-statistics from the weighted regression model was used to test the differences in age, mean LOS, and mean THC in LT and non-LT hospitalizations with AP. Adjusted hazard ratios with 95% confidence interval were obtained through Cox proportional hazards regression to identify factors that influenced mortality. All analytical results were considered statistically significant when P values were less than or equal to 0.05.
Ethical considerations
The NIS database lacks patient and hospital-specific identifiers to protect patient privacy and maintain anonymity. Hence, our study was exempt from Institutional Review Board (IRB) approval as per guidelines put forth by our IRB for analysis of database studies.
RESULTS
Trends of hospitalization characteristics for LT hospitalizations with AP
There was an increase in the total number of LT hospitalizations with AP from 305 in 2007 to 610 in 2019. We did not find a statistically significant trend for gender or mean age; however, there was an increasing trend of LT hospitalizations with AP for patients aged ≥ 65 years (Table 1). Furthermore, LT hospitalizations with AP had an increasing comorbidity burden as the Charlson Comorbidity Index (CCI) score ≥ 3 increased from 41.64% in 2007 to 62.30% in 2019 (P-trend < 0.0001). Interestingly, we also noted a rising trend of LT hospitalizations with AP from 58.89% in 2007 to 82.79% in 2019 at urban teaching hospitals.
Table 1.
Trends of hospitalization characteristics for liver transplant hospitalizations with acute pancreatitis in the United States from 2007–2019, n (%)
| Epidemiologicalvariable |
Years
|
Trend (P value) | ||||||||||||
|
|
2007
|
2008
|
2009
|
2010
|
2011
|
2012
|
2013
|
2014
|
2015
|
2016
|
2017
|
2018
|
2019
|
|
| Total number of hospitalizations | 305 | 600 | 550 | 520 | 453 | 590 | 455 | 500 | 460 | 650 | 505 | 665 | 610 | -- |
| Mean age in yr (standard error) | 53.08 (1.52) | 51.00 (1.35) | 52.01 (1.59) | 51.32 (1.45) | 51.79 (1.49) | 52.02 (1.10) | 52.86 (1.20) | 55.16 (1.22) | 50.27 (1.31) | 51.84 (1.11) | 53.70 (1.26) | 53.32 (1.12) | 54.73 (1.20) | No trend (0.1256) |
| Age groups (yr) | ||||||||||||||
| 18–34 | 30 (9.94) | 82 (13.62) | 76 (13.77) | 62 (11.90) | 50 (11.07) | 80 (13.56) | 45 (9.89) | 55 (11.00) | 90 (19.57) | 105 (16.15) | 50 (9.90) | 70 (10.53) | 55 (9.02) | No trend (0.1345) |
| 35–49 | 61 (19.82) | 180 (29.97) | 117 (21.38) | 111 (21.37) | 84 (18.46) | 145 (24.58) | 100 (21.98) | 90 (18.00) | 115 (25.00) | 120 (18.46) | 100 (19.80) | 185 (27.82) | 165 (27.05) | No trend (0.2379) |
| 50–64 | 164 (53.56) | 236 (39.30) | 270 (49.09) | 281 (54.15) | 276 (60.97) | 280 (47.46) | 255 (56.04) | 225 (45.00) | 170 (36.96) | 295 (45.38) | 260 (51.49) | 265 (39.85) | 200 (32.79) | Decrease (< 0.0001) |
| 65–79 | 46 (14.90) | 103 (17.12) | 87 (15.76) | 62 (11.86) | 38 (8.40) | 85 (14.41) | 55 (12.09) | 120 (24.00) | 75 (16.30) | 125 (19.23) | 85 (16.83) | 135 (20.30) | 190 (31.15) | Increase (< 0.0001) |
| ≥ 80 | < 11 (1.78) | 0 (0.00) | 0 (0.00) | < 11 (0.71) | < 11 (1.09) | 0 (0.00) | 0 (0.00) | < 11 (2.00) | < 11 (2.17) | < 11 (0.77) | < 11 (1.98) | < 11 (1.50) | 0 (0.00) | Increase (0.0157) |
| Gender | ||||||||||||||
| Male | 163 (53.30) | 278 (46.32) | 311 (56.61) | 328 (63.08) | 270 (59.48) | 325 (55.08) | 260 (57.14) | 235 (47.00) | 275 (59.78) | 380 (58.46) | 270 (53.47) | 370 (55.64) | 340 (55.74) | No trend (0.1383) |
| Female | 143 (46.70) | 322 (53.68) | 238 (43.39) | 192 (36.92) | 184 (40.52) | 265 (44.92) | 195 (42.86) | 265 (53.00) | 185 (40.22) | 270 (41.54) | 235 (46.53) | 295 (44.36) | 270 (44.26) | No trend (0.1383) |
| Race | ||||||||||||||
| White | 139 (59.81) | 387 (72.63) | 310 (66.45) | 322 (66.37) | 285 (71.89) | 395 (71.17) | 290 (65.91) | 375 (78.95) | 265 (61.63) | 390 (64.46) | 360 (75.00) | 385 (60.16) | 405 (66.94) | No trend (0.0517) |
| Black | 26 (11.00) | 48 (9.04) | 69 (14.68) | 99 (20.39) | 58 (14.49) | 35 (6.31) | 45 (10.23) | 40 (8.42) | 20 (4.65) | 90 (14.88) | 50 (10.42) | 60 (9.38) | 50 (8.26) | Decrease (0.0004) |
| Hispanic | 38 (16.49) | 63 (11.85) | 54 (11.58) | 43 (8.80) | 39 (9.75) | 65 (11.71) | 70 (15.91) | 35 (7.37) | 95 (22.09) | 80 (13.22) | 35 (7.29) | 135 (21.09) | 80 (13.22) | Increase (0.0009) |
| Asian | < 11 (4.27) | 20 (3.77) | 0 (0.00) | 11 (2.19) | < 11 (2.57) | 35 (6.31) | 20 (4.55) | 15 (3.16) | 20 (4.65) | 30 (4.96) | < 11 (2.08) | 25 (3.91) | 45 (7.44) | Increase (0.0002) |
| Other | 20 (8.42) | 14 (2.71) | 34 (7.28) | 11 (2.26) | < 11 (1.31) | 25 (4.50) | 15 (3.41) | < 11 (2.11) | 30 (6.98) | 15 (2.48) | 25 (5.21) | 35 (5.47) | 25 (4.13) | No trend (0.406) |
| CCI | ||||||||||||||
| CCI = 1 | 130 (42.71) | 232 (38.75) | 174 (31.68) | 147 (28.25) | 138 (30.35) | 185 (31.36) | 130 (28.57) | 155 (31.00) | 150 (32.61) | 160 (24.62) | 120 (23.76) | 160 (24.06) | 145 (23.77) | Decrease (< 0.0001) |
| CCI = 2 | 48 (15.65) | 101 (16.81) | 106 (19.32) | 155 (29.77) | 61 (13.38) | 115 (19.49) | 115 (25.27) | 130 (26.00) | 90 (19.57) | 110 (16.92) | 75 (14.85) | 115 (17.29) | 85 (13.93) | Decrease (0.0036) |
| CCI ≥ 3 | 127 (41.64) | 267 (44.44) | 269 (49.01) | 218 (41.98) | 255 (56.27) | 290 (49.15) | 210 (46.15) | 215 (43.00) | 220 (47.83) | 380 (58.46) | 310 (61.39) | 390 (58.65) | 380 (62.30) | Increase (< 0.0001) |
| Hospital region | ||||||||||||||
| Northeast | 36 (11.70) | 209 (34.76) | 82 (14.99) | 61 (11.73) | 89 (19.75) | 100 (16.95) | 60 (13.19) | 35 (7.00) | 65 (14.13) | 95 (14.62) | 115 (22.77) | 115 (17.29) | 85 (13.93) | Decrease (< 0.0001) |
| Midwest | 64 (20.97) | 98 (16.26) | 213 (38.69) | 134 (25.71) | 144 (31.79) | 130 (22.03) | 125 (27.47) | 140 (28.00) | 130 (28.26) | 125 (19.23) | 130 (25.74) | 140 (21.05) | 130 (21.31) | Decrease (0.0063) |
| South | 105 (34.47) | 121 (20.22) | 119 (21.68) | 244 (47.04) | 169 (37.29) | 185 (31.36) | 180 (39.56) | 205 (41.00) | 170 (36.96) | 270 (41.54) | 145 (28.71) | 265 (39.85) | 230 (37.70) | Increase (< 0.0001) |
| West | 100 (32.86) | 173 (28.77) | 135 (24.64) | 81 (15.52) | 51 (11.18) | 175 (29.66) | 90 (19.78) | 120 (24.00) | 95 (20.65) | 160 (24.62) | 115 (22.77) | 145 (21.80) | 165 (27.05) | No trend (0.2338) |
| Hospital bed-size | ||||||||||||||
| Small | 43 (13.91) | 48 (7.97) | 23 (4.59) | 34 (6.64) | 23 (5.15) | 30 (5.08) | 60 (13.19) | 45 (9.00) | 65 (14.13) | 60 (9.23) | 40 (7.92) | 90 (13.53) | 85 (13.93) | Increase (< 0.0001) |
| Medium | 68 (22.16) | 93 (15.44) | 103 (20.26) | 91 (17.70) | 58 (13.10) | 120 (20.34) | 75 (16.48) | 135 (27.00) | 100 (21.74) | 120 (18.46) | 120 (23.76) | 195 (29.32) | 155 (25.41) | Increase (< 0.0001) |
| Large | 195 (63.93) | 459 (76.59) | 381 (75.16) | 389 (75.67) | 363 (81.75) | 440 (74.58) | 320 (70.33) | 320 (64.00) | 295 (64.13) | 470 (72.31) | 345 (68.32) | 380 (57.14) | 370 (60.66) | Decrease (< 0.0001) |
| Hospital location and teaching status | ||||||||||||||
| Rural | 18 (5.97) | 57 (9.51) | 20 (3.98) | 41 (7.98) | 35 (7.95) | 65 (11.02) | 30 (6.59) | 45 (9.00) | 35 (7.61) | 35 (5.38) | 15 (2.97) | 65 (9.77) | 25 (4.10) | Decrease (0.0238) |
| Urban nonteaching | 107 (35.14) | 145 (24.21) | 171 (33.68) | 156 (30.35) | 84 (18.89) | 190 (32.20) | 140 (30.77) | 70 (14.00) | 85 (18.48) | 125 (19.23) | 110 (21.78) | 110 (16.54) | 80 (13.11) | Decrease (< 0.0001) |
| Urban teaching | 180 (58.89) | 398 (66.28) | 316 (62.34) | 317 (61.67) | 325 (73.16) | 335 (56.78) | 285 (62.64) | 385 (77.00) | 340 (73.91) | 490 (75.38) | 380 (75.25) | 490 (73.68) | 505 (82.79) | Increase (< 0.0001) |
| Disposition | ||||||||||||||
| Discharge Home | 276 (90.47) | 473 (78.88) | 397 (72.25) | 359 (69.05) | 333 (73.51) | 440 (74.58) | 345 (75.82) | 395 (79.00) | 375 (81.52) | 525 (80.77) | 370 (73.27) | 490 (73.68) | 455 (74.59) | No trend (0.1111) |
| Transfer to short-term hospital | < 11 (3.06) | 46 (7.74) | 37 (6.72) | 68 (13.01) | 35 (7.81) | 50 (8.47) | 25 (5.49) | 35 (7.00) | 40 (8.70) | 30 (4.62) | 60 (11.88) | 30 (4.51) | 35 (5.74) | No trend (0.0657) |
| Transfer to another facility (Includes SNF and ICF) | < 11 (3.25) | 20 (3.28) | 34 (6.11) | 26 (5.09) | 13 (2.97) | 25 (4.24) | < 11 (2.20) | < 11 (1.00) | 10 (2.17) | 45 (6.92) | < 11 (0.99) | 70 (10.53) | 15 (2.46) | No trend (0.0532) |
| Home health care | < 11 (3.22) | 30 (5.07) | 51 (9.32) | 62 (11.87) | 42 (9.25) | 60 (10.17) | 60 (13.19) | 50 (10.00) | 30 (6.52) | 45 (6.92) | 55 (10.89) | 55 (8.27) | 60 (9.84) | Increase (0.0426) |
| Discharge against medical advice | 0 (0.00) | 25 (4.16) | 11 (2.00) | < 11 (0.98%) | < 11 (1.11) | < 11 (1.69) | 15 (3.30) | <11 (2.00) | < 11 (1.09) | 0 (0.00) | < 11 (0.99) | 20 (3.01) | 25 (4.10) | No trend (0.1735) |
CCI: Charlson comorbidity index; ICF: Intermediate care facility; SNF: Skilled nursing facility.
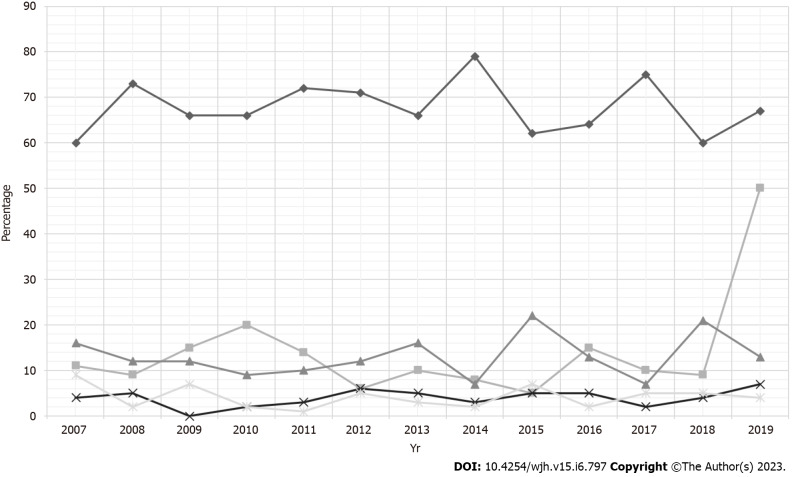
Racial differences in the trends of LT hospitalizations with AP were apparent. Whites made up a majority of the study cohort (Table 1) without a statistically significant trend. We noted an overall increasing trend of Hispanic (16.49% in 2007 to 21.09% in 2018, P-trend = 0.0009) and Asian (4.27% in 2007 to 7.44% in 2019, P-trend = 0.0009) LT hospitalizations with AP (Table 1 and Figure 1). However, Black LT hospitalizations with AP had a declining trend from 11% to 8.26%, P-trend = 0.0004) (Table 1).
Figure 1.
Racial trends for liver transplant hospitalizations with acute pancreatitis in the United States from 2007–2019.
Trends of clinical outcomes, healthcare burden and complications for LT hospitalizations with AP
We did not find a statistically significant trend for inpatient mortality, mean LOS, and mean THC for LT hospitalizations with AP (Table 2). However, we observed a rising trend of complications such as sepsis (1.25% in 2007 to 18.03% in 2019, P-trend < 0.0001), acute kidney failure (AKF) (17.13% to 34.43%, P-trend < 0.0001), acute respiratory failure (ARF) (1.44% to 6.56%, P-trend = 0.0002), abdominal abscesses (0% in 2007 to 0.82% in 2019, P-trend = 0.0006), portal vein thrombosis (PVT) (0% to 4.10%, P-trend < 0.0001) and venous thromboembolism (VTE) (1.82% to 7.38%, P-trend < 0.0001) for LT hospitalizations with AP. Moreover, there was a decline in the need for blood transfusion from 6.09% in 2007 to 0% in 2019 (P-trend < 0.0001) for LT hospitalizations with AP.
Table 2.
Trends of outcomes for liver transplant hospitalizations with acute pancreatitis in the United States from 2007–2019, n (%)
| Outcomes |
|
Years
|
Trend (P value) | |||||||||||
|
|
2007
|
2008
|
2009
|
2010
|
2011
|
2012
|
2013
|
2014
|
2015
|
2016
|
2017
|
2018
|
2019
|
|
| Inpatient mortality | 0 (0.00) | < 11 (0.87) | 20 (3.60) | 0 (0.00) | 24 (5.35) | < 11 (0.85) | 0 (0.00) | < 11 (1.00) | 0 (0.00) | < 11 (0.77) | < 11 (1.98) | 0 (0.00) | 20 (3.28) | No trend (0.3879) |
| Length of stay (d) | 5.62 | 5.44 | 7.09 | 6.02 | 7.85 | 5.40 | 8.53 | 4.53 | 4.86 | 7.33 | 6.62 | 6.23 | 4.55 | No trend (0.6905) |
| Total healthcare charge ($) | 36413 | 53418 | 50432 | 53115 | 68247 | 42107 | 95774 | 41613 | 42319 | 79746 | 80479 | 65054 | 56011 | No trend (0.1946) |
| Complications | ||||||||||||||
| Pancreatic psuedocyst | < 11 (3.41) | 35 (5.88) | 34 (6.13) | 26 (5.06) | 14 (3.01) | < 11 (1.69) | 20 (4.40) | < 11 (2.00) | < 11 (1.09) | 20 (3.08) | 0 (0.00) | 50 (7.52) | 30 (4.92) | No trend (0.1273) |
| Abdominal abscess | 0 (0.00) | 0 (0.00) | 0 (0.00) | 11 (2.07) | < 11 (1.00) | 0 (0.00) | < 11 (1.10) | < 11 (1.00) | 0 (0.00) | < 11 (0.77) | 0 (0.00) | 20 (3.01) | < 11 (0.82) | Increase (0.0006) |
| Sepsis | < 11 (1.25) | 41 (6.91) | 46 (8.37) | 30 (5.69) | 32 (7.15) | 20 (3.39) | 35 (7.69) | 30 (6.00) | 40 (8.70) | 60 (9.23) | 55 (10.89) | 70 (10.53) | 110 (18.03) | Increase (< 0.0001) |
| Acute renal failure | 52 (17.13) | 121 (20.10) | 149 (27.09) | 123 (23.74) | 143 (31.62) | 160 (27.12) | 130 (28.57) | 145 (29.00) | 155 (33.70) | 205 (31.54) | 180 (35.64) | 245 (36.84) | 210 (34.43) | Increase (< 0.0001) |
| Acute respiratory failure | < 11 (1.44) | 37 (6.10) | 21 (3.79) | 21 (4.06) | 28 (6.28) | 0 (0.00) | 15 (3.30) | < 11 (2.00) | 25 (5.43) | 55 (8.46) | 20 (3.96) | 40 (6.02) | 40 (6.56) | Increase (0.0002) |
| Need for blood transfusion | 19 (6.09) | 72 (12.03) | 33 (6.10) | 40 (7.61) | 91 (20.09) | 95 (16.10) | 45 (9.89) | 35 (7.00) | 30 (6.52) | 20 (3.08) | 20 (3.96) | 25 (3.76) | 0 (0.00) | Decrease (< 0.0001) |
| Portal vein thrombosis | 0 (0.00) | < 11 (1.69) | < 11 (0.86) | 0 (0.00) | 0 (0.00) | 0 (0.00) | < 11 (1.10) | < 11 (2.00) | < 11 (1.09) | 15 (2.31) | 15 (2.97) | 15 (2.26) | 25 (4.10) | Increase (< 0.0001) |
| Venous thromboembolism | < 11 (1.82) | < 11 (0.85) | 35 (6.29) | 16 (3.02) | < 11 (1.00) | < 11 (1.69) | < 11 (1.10) | < 11 (1.00) | < 11 (2.17) | 25 (3.85) | 25 (4.95%) | 50 (7.52) | 45 (7.38) | Increase (< 0.0001) |
Comparative analysis of hospitalization characteristics for LT and non-LT hospitalizations with AP
Between 2007–2019, there were 6863 LT hospitalizations with AP which were compared to 5649980 non-LT AP hospitalizations. LT hospitalizations with AP had a slightly higher mean age (53.5 vs 52.55 years, P = 0.017) compared to the non-LT cohort. Furthermore, LT hospitalizations with AP also had a higher proportion of males (55.43% vs 51.13%, P = 0.0046) and patients with a CCI score ≥ 3 (51.46% vs 19.76%, P < 0.0001) compared to non-LT hospitalizations (Table 3). A majority of LT hospitalizations with AP were at large (69.47%), urban teaching (69.73%) hospitals.
Table 3.
Comparative analysis of hospitalization characteristics for liver and non-liver transplant hospitalizations with acute pancreatitis in the United States from 2007–2019, n (%)
|
Outcomes
|
Liver transplant hospitalizations with acute pancreatitis
|
Non-liver transplant hospitalizations with acute pancreatitis
|
P value
|
| Total number of hospitalizations | 6863 | 5649980 | |
| Mean age ± standard error (yr) | 53.50 (0.04) | 52.55 (0.39) | 0.017 |
| Age group (yr) | < 0.0001 | ||
| 18–34 | 12.38 | 16.20 | |
| 35–49 | 22.91 | 26.36 | |
| 50–64 | 46.29 | 29.97 | |
| 65–79 | 17.55 | 18.43 | |
| ≥ 80 | 0.86 | 9.03 | |
| Gender | 0.0046 | ||
| Male | 55.43 | 51.13 | |
| Female | 44.57 | 48.87 | |
| Race | ≤ 0.0001 | ||
| White | 67.91 | 64.57 | |
| Black | 10.85 | 16.11 | |
| Hispanic | 13.11 | 13.12 | |
| Asian | 3.95 | 2.30 | |
| Other | 4.16 | 3.90 | |
| Charlson comorbidity index | < 0.0001 | ||
| CCI = 1 | 29.53 | 28.27 | |
| CCI = 2 | 19.02 | 13.65 | |
| CCI ≥ 3 | 51.46 | 19.76 | |
| Hospital region | 0.0753 | ||
| Northeast | 16.71 | 16.45 | |
| Midwest | 24.80 | 22.02 | |
| South | 35.10 | 40.16 | |
| West | 23.38 | 21.37 | |
| Hospital bed-size | < 0.0001 | ||
| Small | 9.49 | 17.96 | |
| Medium | 21.04 | 28.13 | |
| Large | 69.47 | 53.91 | |
| Hospital location and teaching status | < 0.0001 | ||
| Rural | 7.15 | 12.46 | |
| Urban nonteaching | 23.12 | 36.23 | |
| Urban teaching | 69.73 | 51.32 | |
| Disposition | < 0.0001 | ||
| Routine (Home) | 76.26 | 77.39 | |
| Transfer to short-term hospital | 7.30 | 3.10 | |
| Transfer to another type of facility (Includes SNF and ICF) | 4.20 | 7.64 | |
| Home health care | 8.89 | 6.69 | |
| Discharge against medical advice | 1.98 | 3.00 |
CCI: Charlson comorbidity index; ICF: Intermediate care facility; SNF: Skilled nursing facility.
Racial differences were observed between the LT and non-LT cohorts. We noted a higher proportion of Whites (67.91% vs 64.57%, P < 0.0001) and Asians (3.95% vs 2.3%, P < 0.0001) in the LT cohort, while there was a higher proportion of Blacks and Hispanics in the non-LT cohort (Table 3).
Comparative analysis of clinical outcomes, healthcare burden and complications for LT and non-LT hospitalizations with AP
Overall, the inpatient mortality for LT hospitalizations with AP was lower (1.37% vs 2.16%, P = 0.0479) than the non-LT cohort (Table 4). We did not find a statistical difference in the inpatient mortality rates after stratifying for age, gender, or race. Although the mean LOS was comparable between both groups, the mean THC was higher for LT hospitalizations with AP ($59596 vs $50466, P-trend = 0.0429) compared to the non-LT cohort. Furthermore, LT hospitalizations with AP also had a higher proportion of patients with complications such as AKF (29.41% vs 14.91%, P < 0.0001), need for blood transfusion (7.65% vs 4.75%, P < 0.0001), PVT (1.53% vs 0.64%, P < 0.0001) and VTE (3.5% vs 2.19%, P = 0.0011) compared to non-LT hospitalizations; however, the non-LT cohort had a higher proportion of patients with pancreatic pseudocysts (5.46% vs 3.85%, P = 0.0259) (Table 4).
Table 4.
Comparative analysis of clinical outcomes for liver and non-liver transplant hospitalizations with acute pancreatitis in the United States from 2007–2019, n (%)
|
Outcomes
|
Liver transplant hospitalizations with acute pancreatitis
|
Non-liver transplant hospitalizations with acute pancreatitis
|
P value
|
| Inpatient mortality | 1.37 | 2.16 | 0.0479 |
| Gender-specific inpatient mortality | |||
| Male | 1.43 | 2.34 | 0.1107 |
| Female | 1.31 | 1.97 | 0.2396 |
| Race specific inpatient mortality | |||
| White | 1.48 | 2.23 | 0.1403 |
| Black | 1.45 | 2.00 | 0.6469 |
| Hispanic | 0.00 | 1.60 | --- |
| Asian | 1.99 | 3.20 | 0.6289 |
| Others | 4.01 | 2.23 | 0.3868 |
| Age group specific inpatient mortality | |||
| 18-34 | 0.60 | 0.64 | 0.9583 |
| 35-49 | 0.90 | 1.04 | 0.7855 |
| 50-64 | 1.12 | 2.08 | 0.0921 |
| 65-79 | 3.26 | 3.60 | 0.7784 |
| ≥ 80 | 0.00 | 5.46 | --- |
| Length of stay (d) | 6.14 | 5.80 | 0.3189 |
| Total healthcare charge ($) | 59596 | 50466 | 0.0429 |
| Complications (out of total hospitalizations) | |||
| Pancreatic psuedocyst | 3.85 | 5.46 | 0.0259 |
| Abdominal abscess | 0.81 | 0.53 | 0.1925 |
| Sepsis | 8.35 | 8.78 | 0.5834 |
| Acute renal failure | 29.41 | 14.91 | < 0.0001 |
| Acute respiratory failure | 4.61 | 5.67 | 0.1018 |
| Cholangiocarcinoma | 0.21 | 0.11 | 0.2545 |
| Need for blood transfusion | 7.65 | 4.75 | < 0.0001 |
| Portal vein thrombosis | 1.53 | 0.64 | < 0.0001 |
| Venous thromboembolism | 3.50 | 2.19 | 0.0011 |
Predictors for inpatient mortality for LT hospitalizations with AP
After a regression analysis, Hispanics were noted to have lower odds of inpatient mortality compared to Whites (Table 5). Furthermore, after adjusting for all other variables, every one-point increase in the CCI score was associated with a 67.8% increase in inpatient mortality for LT hospitalizations with AP (Table 5). The presence of complications such as pancreatic pseudocysts (aHR: 14.158, 95%CI 1.642-122.094, P = 0.016), sepsis (aHR: 13.960, 95%CI 2.163-90.093, P < 0.0001), AKF (aHR: 2.684, 95%CI 1.109-6.494, P = 0.029), ARF (aHR: 24.758, 95%CI 1.063-576.522, P = 0.046), need for blood transfusion (aHR: 150.340, 95%CI 17.049-1325.754, P < 0.0001) and VTE (aHR: 75.422, 95%CI 1.637-3475.134, P = 0.027) were also associated with higher odds inpatient mortality for LT hospitalizations with AP after adjusting for all other variables.
Table 5.
Predictors of inpatient mortality for liver transplant hospitalizations with acute pancreatitis in the United States from 2007–2019
|
Variable
|
Adjusted hazard ratio
|
95%CI
|
P value
|
| Gender | |||
| Male | Reference | ||
| Female | 0.596 | (0.150, 2.365) | 0.461 |
| Race | |||
| White | Reference | ||
| Black | 0.306 | (0.017, 5.368) | 0.418 |
| Hispanic | < 0.001 | (< 0.001, < 0.001) | < 0.0001 |
| Asian | 0.042 | (< 0.001, 14.916) | 0.289 |
| Other | 0.064 | (< 0.001, 10.989) | 0.295 |
| Charlson comorbidity index | 1.678 | (1.055, 2.668) | 0.029 |
| Hospital region | |||
| Northeast | Reference | ||
| Midwest | 1.574 | (0.148, 16.692) | 0.706 |
| South | 1.435 | (0.230, 8.955) | 0.699 |
| West | 1.723 | (0.423, 7.014) | 0.447 |
| Hospital bed size | |||
| Small | Reference | ||
| Medium | 1.427 | (0.093, 21.893) | 0.798 |
| Large | 1.974 | (0.093, 42.139) | 0.663 |
| Hospital location and teaching status | |||
| Rural | Reference | ||
| Urban nonteaching | < 0.001 | (< 0.001, 0.048) | 0.003 |
| Urban teaching | 0.551 | (0.053, 5.689) | 0.617 |
| Complications (reference = Without the complication) | |||
| Pancreatic psuedocyst | 14.158 | (1.642, 122.094) | 0.016 |
| Abdominal abscess | < 0.001 | (< 0.001, < 0.001) | < 0.0001 |
| Sepsis | 13.960 | (2.163, 90.093) | 0.006 |
| Acute renal failure | 2.684 | (1.109, 6.494) | 0.029 |
| Acute respiratory failure | 24.758 | (1.063, 576.522) | 0.046 |
| Need for blood transfusion | 150.340 | (17.049, 1325.754) | < 0.0001 |
| Portal vein thrombosis | < 0.001 | (< 0.001, < 0.001) | < 0.0001 |
| Venous thromboembolism | 75.422 | (1.637, 3475.134) | 0.027 |
DISCUSSION
AP is a well-known clinical entity. Although it has been thoroughly studied in the general population, there is a significant paucity of data on AP in solid-organ transplant recipients, particularly those undergoing LT. This is the only study in current literature that investigates trends, clinical outcomes, and the healthcare burden of LT hospitalizations with AP at a national level. In this study, we noted an increase in LT hospitalizations with AP with a rising trend for ethnic minorities i.e. Hispanics and Asians; however, we did not find a statistically significant trend of inpatient mortality, mean LOS and mean THC. Although the LT cohort was slightly older and had a higher comorbidity burden, the overall inpatient mortality was lower (1.37% vs 2.16%, P = 0.0479) compared to the non-LT cohort. Furthermore, LT hospitalizations with AP had a higher proportion of patients with AKF, PVT, VTE, and the need for blood transfusion compared to the non-LT cohort. Increasing CCI and the presence of pancreatic pseudocysts, sepsis, ARF, AKF, VTE, and the need for blood transfusion were associated with increased odds of inpatient mortality for LT hospitalizations with AP. With the increasing rates of liver transplants being performed and relative organ shortage in the US, it is vital to understand patient characteristics, outcomes, and complications of LT hospitalizations with AP to potentially reduce adverse clinical outcomes in these high-risk individuals[18].
As per data available from United Network for Organ Sharing (UNOS), the total number of LT increased from 6494 in 2007 to 8896 in 2019[18]. However, in our study, the total number of LT hospitalizations with AP increased disproportionally, essentially doubling in the same time frame. In the US, the rates of LT for patients ≥ 65 years of age have also been on the rise as there is a general consensus that LT in the elderly is feasible with acceptable short-term and long-term results[28,29]. Similarly, in this study, we noted an increase in the rates of LT hospitalizations with AP for patients > 65 years of age (Table 1). However, it should be noted that AP carries a higher morbidity and mortality burden in the elderly population at baseline, and this is compounded in organ transplant recipients[30].
In the US, there was an increase in LT for Hispanics and Asians from 912 in 2007 to 1498 in 2019 and 325 in 2007 to 363 in 2019, respectively as per the UNOS registry. Current literature lacks data on the racial distribution of AP in LT recipients, particularly for ethnic minorities i.e. Blacks, Hispanics, and Asians. However, studies have demonstrated that ethnic minorities, at baseline, are at a higher risk of developing AP and have greater severity of disease compared to the general population[2,31-35]. In our study, there was an increasing trend of Hispanic and Asian LT hospitalizations with AP (Figure 1) which was disproportionate to the increase in LT for this population. Interestingly, Black LT hospitalizations with AP were noted to have a declining trend between 2007–2019. After a comparative analysis, we observed a higher proportion of Asians in the LT cohort, while there was a higher proportion of Blacks and Hispanics in the non-LT cohort. The exact reason for this variable racial distribution is currently unknown but needs further investigation through large, multi-center prospective studies. Furthermore, we emphasize the need for early recognition and prompt treatment of AP in Hispanic and Asian LT hospitalizations to prevent adverse clinical outcomes.
Statistics have demonstrated continuous improvements in survival rates for liver transplant recipients[36-38]. Over the last few decades, AP-related mortality has also declined due to prompt recognition and improvement in management strategies[1,39]. However, prior literature offers conflicting evidence on ethnic variations in AP-related mortality with some studies reporting increased mortality rates in Whites, while others noted higher mortality rates in Blacks among the general population[14,40]. There continues to be a significant paucity of data on mortality for AP in LT recipients in current literature. In our study, we did not find a statistically significant trend for inpatient mortality in LT hospitalizations with AP (Table 2). Interestingly, after a comparative analysis, LT hospitalizations with AP had lower inpatient mortality rates compared to the non-LT cohort despite a higher mean age, greater comorbidity burden, and higher proportion of patients with complications. Furthermore, we did not find a statistical difference in the inpatient mortality rates after stratifying for age, gender, or race. The exact reason for lower inpatient mortality rates in LT hospitalizations with AP is unknown. However, it may, in part, be due to increased vigilance for complications in these high-risk hospitalizations, overall improvements in management strategies, and a multi-disciplinary team approach for management of these highly complex patients. Additional multi-center prospective studies are needed to further investigate these findings. Nonetheless, lower mortality suggests improved survival rates for LT hospitalizations which is in line with current literature.
Healthcare utilization by LT recipients is on the rise. A study by Habka et al[41] in 2015 predicted that the cost of LT will increase by 33% in 10 years and 81% in the next 20 years. The inpatient cost of management of AP has also almost doubled from 1996 ($3.9 billion) to 2016 ($7.7 billion)[42]. On the contrary, the utilization of the inpatient service (bed days per prevent case) for AP has declined over the years[42]. No data currently exists on healthcare utilization for AP in LT recipients. In our study, we did not find a statistically significant trend in mean LOS and mean THC for LT hospitalizations with AP indicating that the healthcare burden has remained relatively stable over the years despite a higher proportion of patients with complications such as sepsis, AKF, ARF, PVT, VTE, and abdominal abscesses. After a comparative analysis, the mean LOS was comparable between the LT and non-LT cohorts; however, the mean THC for the LT cohort was $9130 higher than that of the non-LT cohort. This may, in part, be attributed to a higher proportion of patients with complications in the LT cohort compared to the non-LT cohort requiring a higher level of care and multi-disciplinary team management (Table 4). Furthermore, after adjusting for all other variables, increasing CCI, and the presence of complications such as pancreatic pseudocysts, sepsis, ARF, AKF, VTE, and need for blood transfusions were associated with higher odds of inpatient mortality for LT hospitalizations with AP. These findings somewhat mirror predictors of inpatient mortality for AP that have been reported in previous population-based studies[43].
Our study has several strengths and a few limitations. Our study population, which was drawn from one of the largest, publicly available, multi-ethnic databases in the US, is a key strength of this study. This is the only study in the current literature that offers a national perspective on hospitalization characteristics, clinical outcomes, complications, and the healthcare burden of LT hospitalizations with AP over 13 years, compared to other single-center experiences which offer limited information. Through a comprehensive and unique analysis technique, we were also able to compare LT and non-LT hospitalizations to understand the influence of AP on LT hospitalizations thereby giving gastroenterologists real world data. Furthermore, as the NIS covers approximately 97% of the US population, the results of our study are applicable to all LT hospitalizations with AP in the US.
However, we do acknowledge the limitations associated with our study. The retrospective study design makes our study susceptible to the biases that are associated with retrospective studies. Additionally, the NIS database does not contain information on the indication of liver transplant, time from LT to development of AP, disease severity, hospital course, treatment aspects of the disease, time from any procedure to development of complications, procedural complications (pre, intra, and post), intraprocedural operator preferences, or performance of any procedure. Lastly, the NIS is an administrative database that uses ICD codes to store data; hence, the possibility of human coding errors always exists. Despite these limitations, our large sample size, unique analysis technique, and multi-faceted outcomes add valuable data to limited literature.
CONCLUSION
LT is a lifesaving procedure for chronic end-stage liver disease patients. However, the development of post-LT pancreatitis may lead to poor surgical outcomes and development of complications. In our study, we noted an increase in LT hospitalizations with AP, particularly for ethnic minorities i.e. Hispanics and Asians; however, there was no trend for inpatient mortality. We also did not find a statistically significant trend mean LOS and mean THC indicating that healthcare utilization has remained relatively stable for LT hospitalizations with AP between 2007–2019. On comparison, LT hospitalizations with AP had lower inpatient mortality compared to non-LT AP hospitalizations despite a higher proportion of patients that were older, had CCI ≥ 3, and had complications such as AKF, PVT, VTE, and need for blood transfusion. Increasing CCI, presence of pancreatic pseudocysts, sepsis, ARF, ARF, VTE, and need for blood transfusion were identified to be independent predictors of inpatient mortality for LT hospitalizations with AP.
ARTICLE HIGHLIGHTS
Research background
The development of Acute Pancreatitis (AP) in Liver Transplant (LT) recipients may be associated with poor clinical outcomes and severe complications.
Research motivation
Although studies investigating post-LT pancreatitis currently exist, they are primarily limited to small single-center experiences. Currently, a national perspective in the United States (US) does not exist. Therefore, this study was designed to investigate trends and outcomes of LT hospitalization with AP.
Research objectives
We aimed to assess national trends of hospitalization characteristics, clinical outcomes, and the healthcare burden of LT hospitalizations with AP in the US. Non-LT hospitalizations with AP were also identified as controls to compare hospitalization characteristics, clinical outcomes, and the healthcare burden with the LT cohort. Furthermore, predictors of inpatient mortality for LT hospitalizations with AP were identified.
Research methods
The National Inpatient Sample was utilized to identify LT and non-LT hospitalizations with AP. The Cochran-Armitage trend was used to test the trends for proportions of binary variables. Linear regression examined the trends for the averages of age, mean length of stay (LOS), and mean total healthcare charge (THC). Rao-Scott design-adjusted chi-square test examined the association between binary variables in LT and non-LT Hospitalizations with AP. F-statistics were used to test the differences in age, mean LOS, and mean THC in LT and non-LT Hospitalizations with AP. Cox proportional hazards regression was used to identify factors that influenced mortality.
Research results
The total number of LT hospitalizations with AP increased from 305 in 2007 to 610 in 2019. We did not find statistically significant trends in inpatient mortality, mean LOS, and mean THC for LT hospitalizations with AP. LT hospitalizations with AP had lower inpatient mortality compared to the non-LT cohort despite having a higher mean age, comorbidity burden, and complications. Increasing CCI, presence of pancreatic pseudocysts, sepsis, acute respiratory failure, acute renal failure, venous thromboembolism, and need for blood transfusion were independent predictors of inpatient mortality for LT hospitalizations with AP.
Research conclusions
LT is a lifesaving procedure for chronic end-stage liver disease patients. In the US, LT hospitalizations with AP increased between 2007 to 2019, particularly for Hispanics and Asians. However, LT hospitalizations with AP had lower inpatient mortality compared to non-LT AP hospitalizations.
Research perspectives
This is the only study in the current literature that offers a national perspective on hospitalization characteristics, clinical outcomes, complications, and the healthcare burden of LT hospitalizations with AP in the US.
Footnotes
Institutional review board statement: The NIS database lacks patient and hospital-specific identifiers to protect patient privacy and maintain anonymity. Hence, our study was exempt from Institutional Review Board (IRB) approval as per guidelines put forth by our IRB for analysis of database studies.
Informed consent statement: The data for this study was collected from the National Inpatient Sample (NIS) database. As the NIS database lacks patient-specific and hospital-specific identifiers, this study did not require informed consent. The NIS database is available at: https://www.hcup-us.ahrq.gov.
Conflict-of-interest statement: All the authors have no conflict of interest to declare.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: March 15, 2023
First decision: April 10, 2023
Article in press: May 6, 2023
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mogahed EA, Egypt; Sahin TT, Turkey S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
Contributor Information
Dushyant Singh Dahiya, Department of Internal Medicine, Central Michigan University College of Medicine, Saginaw, MI 48601, United States. dush.dahiya@gmail.com.
Vinay Jahagirdar, Department of Internal Medicine, University of Missouri-Kansas City, Kansas City, MO 64110, United States.
Saurabh Chandan, Division of Gastroenterology and Hepatology, CHI Creighton University Medical Center, Omaha, NE 68131, United States.
Manesh Kumar Gangwani, Department of Internal Medicine, The University of Toledo, Toledo, OH 43606, United States.
Nooraldin Merza, Department of Internal Medicine, The University of Toledo, Toledo, OH 43606, United States.
Hassam Ali, Department of Internal Medicine, East Carolina University, Greenville, NC 27858, United States.
Smit Deliwala, Division of Digestive Diseases, Emory University School of Medicine, Atlanta, GA 30322, United States.
Muhammad Aziz, Division of Gastroenterology and Hepatology, The University of Toledo, Toledo, OH 43606, United States.
Daryl Ramai, Division of Gastroenterology and Hepatology, The University of Utah School of Medicine, Salt Lake City, UT 84112, United States.
Bhanu Siva Mohan Pinnam, Department of Internal Medicine, John H. Stroger Hospital of Cook County, Chicago, IL 60612, United States.
Jay Bapaye, Department of Internal Medicine, Rochester General Hospital, Rochester, NY 14621, United States.
Chin-I Cheng, Department of Statistics, Actuarial and Data Science, Central Michigan University, Mt. Pleasant, MI 48859, United States.
Sumant Inamdar, Division of Gastroenterology and Hepatology, University of Arkansas for Medical Sciences, Little Rock, AR 72205, United States.
Neil R Sharma, Interventional Oncology and Surgical Endoscopy Programs, Parkview Cancer Institute, Fort Wayne, IN 46845, United States.
Mohammad Al-Haddad, Division of Gastroenterology and Hepatology, Indiana University School of Medicine, Indianapolis, IN 46202, United States.
Data sharing statement
The NIS database is publicly available at: https://www.hcup-us.ahrq.gov/.
References
- 1.Krishna SG, Kamboj AK, Hart PA, Hinton A, Conwell DL. The Changing Epidemiology of Acute Pancreatitis Hospitalizations: A Decade of Trends and the Impact of Chronic Pancreatitis. Pancreas. 2017;46:482–488. doi: 10.1097/MPA.0000000000000783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li CL, Jiang M, Pan CQ, Li J, Xu LG. The global, regional, and national burden of acute pancreatitis in 204 countries and territories, 1990-2019. BMC Gastroenterol. 2021;21:332. doi: 10.1186/s12876-021-01906-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forsmark CE, Vege SS, Wilcox CM. Acute Pancreatitis. N Engl J Med. 2016;375:1972–1981. doi: 10.1056/NEJMra1505202. [DOI] [PubMed] [Google Scholar]
- 4.Apte MV, Pirola RC, Wilson JS. Mechanisms of alcoholic pancreatitis. J Gastroenterol Hepatol. 2010;25:1816–1826. doi: 10.1111/j.1440-1746.2010.06445.x. [DOI] [PubMed] [Google Scholar]
- 5.DiMagno MJ. Oktoberfest binge drinking and acute pancreatitis: is there really no relationship? Clin Gastroenterol Hepatol. 2011;9:920–922. doi: 10.1016/j.cgh.2011.07.022. [DOI] [PubMed] [Google Scholar]
- 6.de Pretis N, Amodio A, Frulloni L. Hypertriglyceridemic pancreatitis: Epidemiology, pathophysiology and clinical management. United European Gastroenterol J. 2018;6:649–655. doi: 10.1177/2050640618755002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thaker AM, Mosko JD, Berzin TM. Post-endoscopic retrograde cholangiopancreatography pancreatitis. Gastroenterol Rep (Oxf) 2015;3:32–40. doi: 10.1093/gastro/gou083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitcomb DC. Genetic risk factors for pancreatic disorders. Gastroenterology. 2013;144:1292–1302. doi: 10.1053/j.gastro.2013.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shaka H, El-Amir Z, Jamil A, Kwei-Nsoro R, Wani F, Dahiya DS, Kichloo A, Amblee A. Plasmapheresis in hypertriglyceridemia-induced acute pancreatitis. Proc (Bayl Univ Med Cent) 2022;35:768–772. doi: 10.1080/08998280.2022.2106531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dahiya DS, Perisetti A, Sharma N, Inamdar S, Goyal H, Singh A, Rotundo L, Garg R, Cheng CI, Pisipati S, Al-Haddad M, Sanaka M. Racial disparities in endoscopic retrograde cholangiopancreatography (ERCP) utilization in the United States: are we getting better? Surg Endosc. 2023;37:421–433. doi: 10.1007/s00464-022-09535-w. [DOI] [PubMed] [Google Scholar]
- 11.Wang GJ, Gao CF, Wei D, Wang C, Ding SQ. Acute pancreatitis: etiology and common pathogenesis. World J Gastroenterol. 2009;15:1427–1430. doi: 10.3748/wjg.15.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Forsmark CE, Baillie J AGA Institute Clinical Practice and Economics Committee; AGA Institute Governing Board. AGA Institute technical review on acute pancreatitis. Gastroenterology. 2007;132:2022–2044. doi: 10.1053/j.gastro.2007.03.065. [DOI] [PubMed] [Google Scholar]
- 13.Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62:102–111. doi: 10.1136/gutjnl-2012-302779. [DOI] [PubMed] [Google Scholar]
- 14.Fagenholz PJ, Castillo CF, Harris NS, Pelletier AJ, Camargo CA Jr. Increasing United States hospital admissions for acute pancreatitis, 1988-2003. Ann Epidemiol. 2007;17:491–497. doi: 10.1016/j.annepidem.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 15.Starzl TE, Groth CG, Brettschneider L, Penn I, Fulginiti VA, Moon JB, Blanchard H, Martin AJ Jr, Porter KA. Orthotopic homotransplantation of the human liver. Ann Surg. 1968;168:392–415. doi: 10.1097/00000658-196809000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rana A, Gruessner A, Agopian VG, Khalpey Z, Riaz IB, Kaplan B, Halazun KJ, Busuttil RW, Gruessner RW. Survival benefit of solid-organ transplant in the United States. JAMA Surg. 2015;150:252–259. doi: 10.1001/jamasurg.2014.2038. [DOI] [PubMed] [Google Scholar]
- 17.Kim WR, Lake JR, Smith JM, Skeans MA, Schladt DP, Edwards EB, Harper AM, Wainright JL, Snyder JJ, Israni AK, Kasiske BL. OPTN/SRTR 2015 Annual Data Report: Liver. Am J Transplant. 2017;17 Suppl 1:174–251. doi: 10.1111/ajt.14126. [DOI] [PubMed] [Google Scholar]
- 18. Health Resources and Services Administration. Organ Procurement & Transplantation Network (OPTN). Accessed: March 1, 2023. Available from: http://optn.transplant.hrsa.gov . [Google Scholar]
- 19.Krokos NV, Karavias D, Tzakis A, Tepetes K, Ramos E, Todo S, Fung JJ, Starzl TE. Acute pancreatitis after liver transplantation: incidence and contributing factors. Transpl Int. 1995;8:1–7. doi: 10.1007/bf00366703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alexander JA, Demetrius AJ, Gavaler JS, Makowka L, Starzl TE, Van Thiel DH. Pancreatitis following liver transplantation. Transplantation. 1988;45:1062–1065. doi: 10.1097/00007890-198806000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xie Q, Liu J, Zhuang L, Zhang W, Li Q, Zheng S. Report of two Cases of Acute Pancreatitis after Liver Transplantation for HCC. Transplantation. 2018;102:S871. [Google Scholar]
- 22.Yanaga K, Shimada M, Gordon RD, Tzakis AG, Makowka L, Marsh JW, Stieber AC, Todo S, Iwatsuki S, Starzl TE. Pancreatic complications following orthotopic liver transplantation. Clin Transplant. 1992;6:126–130. [PMC free article] [PubMed] [Google Scholar]
- 23.Yan L, Qian C, Duan X, Ding J, Zhang W. Poor prognosis of liver transplantation for acute liver failure with acute pancreatitis: Two case reports. Medicine (Baltimore) 2020;99:e22934. doi: 10.1097/MD.0000000000022934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Russell TA, Park S, Agopian VG, Zarrinpar A, Farmer DG, O'Neill S, Korayem I, Ebaid S, Gornbein J, Busuttil RW, Kaldas FM. Peritransplant pancreatitis: A marker of high mortality and graft failure in liver transplant patients. Liver Transpl. 2017;23:925–932. doi: 10.1002/lt.24760. [DOI] [PubMed] [Google Scholar]
- 25.Lupo L, Pirenne J, Gunson B, Nishimura Y, Mirza DF, Patapis P, Mayer AD, Buckels JA, McMaster P. Acute-pancreatitis after orthotopic liver transplantation. Transplant Proc. 1997;29:473. doi: 10.1016/s0041-1345(96)00210-2. [DOI] [PubMed] [Google Scholar]
- 26.Verran DJ, Gurkan A, Chui AK, Dilworth P, Koorey D, McCaughan G, Sheil AG. Pancreatitis in adult orthotopic liver allograft recipients: risk factors and outcome. Liver Transpl. 2000;6:362–366. doi: 10.1053/lv.2000.5203. [DOI] [PubMed] [Google Scholar]
- 27.Camargo CA Jr, Greig PD, Levy GA, Clavien PA. Acute pancreatitis following liver transplantation. J Am Coll Surg. 1995;181:249–256. [PubMed] [Google Scholar]
- 28.Su F, Yu L, Berry K, Liou IW, Landis CS, Rayhill SC, Reyes JD, Ioannou GN. Aging of Liver Transplant Registrants and Recipients: Trends and Impact on Waitlist Outcomes, Post-Transplantation Outcomes, and Transplant-Related Survival Benefit. Gastroenterology. 2016;150:441–53.e6; quiz e16. doi: 10.1053/j.gastro.2015.10.043. [DOI] [PubMed] [Google Scholar]
- 29.Dolnikov S, Adam R, Cherqui D, Allard MA. Liver transplantation in elderly patients: what do we know at the beginning of 2020? Surg Today. 2020;50:533–539. doi: 10.1007/s00595-020-01996-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koziel D, Gluszek-Osuch M, Suliga E, Zak M, Gluszek S. Elderly persons with acute pancreatitis - specifics of the clinical course of the disease. Clin Interv Aging. 2019;14:33–41. doi: 10.2147/CIA.S188520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shaheen MA, Akhtar AJ. Organ failure associated with acute pancreatitis in African-American and Hispanic patients. J Natl Med Assoc. 2007;99:1402–1406. [PMC free article] [PubMed] [Google Scholar]
- 32.Kandasami P, Harunarashid H, Kaur H. Acute pancreatitis in a multi-ethnic population. Singapore Med J. 2002;43:284–288. [PubMed] [Google Scholar]
- 33.Pang Y, Kartsonaki C, Turnbull I, Guo Y, Yang L, Bian Z, Chen Y, Millwood IY, Bragg F, Gong W, Xu Q, Kang Q, Chen J, Li L, Holmes MV, Chen Z. Metabolic and lifestyle risk factors for acute pancreatitis in Chinese adults: A prospective cohort study of 0.5 million people. PLoS Med. 2018;15:e1002618. doi: 10.1371/journal.pmed.1002618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cervantes A, Waymouth EK, Petrov MS. African-Americans and Indigenous Peoples Have Increased Burden of Diseases of the Exocrine Pancreas: A Systematic Review and Meta-Analysis. Dig Dis Sci. 2019;64:249–261. doi: 10.1007/s10620-018-5291-1. [DOI] [PubMed] [Google Scholar]
- 35.Yadav D, Lowenfels AB. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144:1252–1261. doi: 10.1053/j.gastro.2013.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nitski O, Azhie A, Qazi-Arisar FA, Wang X, Ma S, Lilly L, Watt KD, Levitsky J, Asrani SK, Lee DS, Rubin BB, Bhat M, Wang B. Long-term mortality risk stratification of liver transplant recipients: real-time application of deep learning algorithms on longitudinal data. Lancet Digit Health. 2021;3:e295–e305. doi: 10.1016/S2589-7500(21)00040-6. [DOI] [PubMed] [Google Scholar]
- 37.Jackson WE, Malamon JS, Kaplan B, Saben JL, Schold JD, Pomposelli JJ, Pomfret EA. Survival Benefit of Living-Donor Liver Transplant. JAMA Surg. 2022;157:926–932. doi: 10.1001/jamasurg.2022.3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jain A, Reyes J, Kashyap R, Dodson SF, Demetris AJ, Ruppert K, Abu-Elmagd K, Marsh W, Madariaga J, Mazariegos G, Geller D, Bonham CA, Gayowski T, Cacciarelli T, Fontes P, Starzl TE, Fung JJ. Long-term survival after liver transplantation in 4,000 consecutive patients at a single center. Ann Surg. 2000;232:490–500. doi: 10.1097/00000658-200010000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McNabb-Baltar J, Ravi P, Isabwe GA, Suleiman SL, Yaghoobi M, Trinh QD, Banks PA. A population-based assessment of the burden of acute pancreatitis in the United States. Pancreas. 2014;43:687–691. doi: 10.1097/MPA.0000000000000123. [DOI] [PubMed] [Google Scholar]
- 40.Gapp J, Hall AG, Walters RW, Jahann D, Kassim T, Reddymasu S. Trends and Outcomes of Hospitalizations Related to Acute Pancreatitis: Epidemiology From 2001 to 2014 in the United States. Pancreas. 2019;48:548–554. doi: 10.1097/MPA.0000000000001275. [DOI] [PubMed] [Google Scholar]
- 41.Habka D, Mann D, Landes R, Soto-Gutierrez A. Future Economics of Liver Transplantation: A 20-Year Cost Modeling Forecast and the Prospect of Bioengineering Autologous Liver Grafts. PLoS One. 2015;10:e0131764. doi: 10.1371/journal.pone.0131764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ahmed NS, Forbes N, Stukalin I, Singh S, Shaheen AA, Ma C Calgary-UCSD Pancreatitis Study Group. Population-based Trends in Healthcare Utilization and National Healthcare Spending on Pancreatitis in North America. Gastroenterology. 2021;161:1698–1701.e5. doi: 10.1053/j.gastro.2021.08.022. [DOI] [PubMed] [Google Scholar]
- 43.Ingraham NE, King S, Proper J, Siegel L, Zolfaghari EJ, Murray TA, Vakayil V, Sheka A, Feng R, Guzman G, Roy SS, Muddappa D, Usher MG, Chipman JG, Tignanelli CJ, Pendleton KM. Morbidity and Mortality Trends of Pancreatitis: An Observational Study. Surg Infect (Larchmt) 2021;22:1021–1030. doi: 10.1089/sur.2020.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The NIS database is publicly available at: https://www.hcup-us.ahrq.gov/.