Patients with advanced heart failure (HF) may require cardiac intensive care unit (CICU) admission, yet little is known about the epidemiology of advanced HF in the community CICU.1-3 Given the potential for referral bias to inflate estimates of advanced HF in the CICU, we sought to describe the epidemiology and outcomes of HF and advanced HF in a community-based sample of residents of Olmsted County, Minnesota admitted to the Mayo Clinic CICU.
The Mayo Clinic Institutional Review Board approved this study under an exception from informed consent. We identified consecutive adult residents of Olmsted County, Minnesota admitted to the Mayo Clinic CICU from January 1, 2007 to December 31, 2017 using data from the first CICU admission during this period crossed with longitudinal data from the Rochester Epidemiology Project.2, 3 The presence of HF and advanced HF were determined using medical record data and confirmed by manual chart review. Advanced HF was identified using the ESC definition applied using a combination of electronic data and manual chart review.1, 4 All-cause 5-year post-discharge mortality among hospital survivors was evaluated by Kaplan-Meier survival curves and multivariable Cox proportional-hazards analysis.
We included 2,034 Olmsted County residents with a median age of 70 (58, 81) years; 785 (39%) were females. A total of 861 (42%) patients had HF, including 342 (40%) with a new diagnosis of HF and 144 (17%) with advanced HF. Patients with HF had more comorbidities, higher illness severity, greater use of critical care therapies, worse laboratory abnormalities, and lower left ventricular ejection fraction (LVEF). Patients with advanced HF had more comorbidities, higher severity of illness, greater use of critical care therapies, and worse laboratory abnormalities (higher blood urea nitrogen [BUN], higher red cell distribution width [RDW], lower chloride) than patients with non-advanced HF (Figure part A). Median LVEF was similar for patients with advanced and non-advanced HF (37% versus 40%, p = 0.11 by Kruskal-Wallis test); 35% of advanced HF and 37% of non-advanced HF patients had LVEF ≥50%. Based on echocardiogram within 1 day of CICU admission (n = 1262), patients with advanced HF had worse right ventricular function, higher pulmonary artery pressures, lower systemic flow, and higher filling pressures. Only 9 patients with advanced HF (6.2%) underwent heart transplantation (n = 1) or LVAD implantation (n = 8) during the index hospitalization.
Figure:
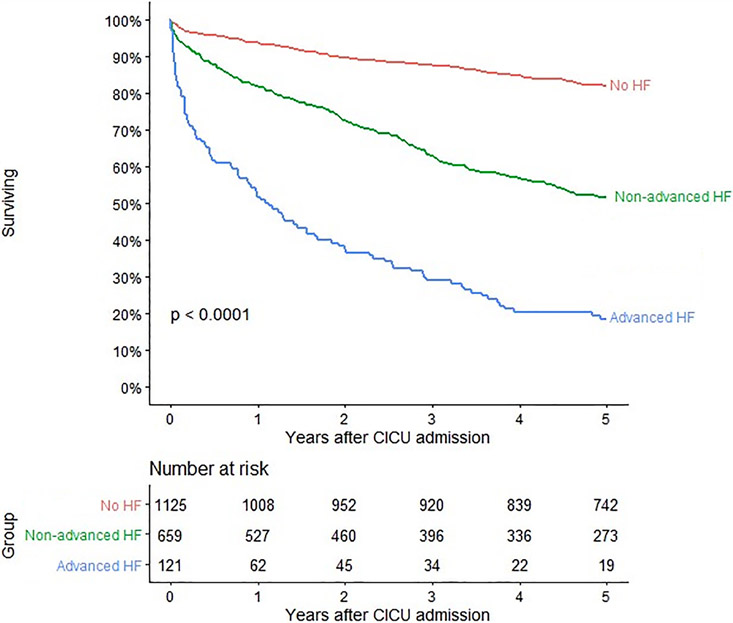
(A) Comparison of patients with HF separated into those with and without advanced HF during hospitalization. (B) Kaplan-Meier survival curves for post-discharge survival among hospital survivors as a function of the presence of advanced or non-advanced HF. P value is for the log-rank test.
In-hospital death occurred in 173 (9%) patients, leaving 1,861 hospital survivors. In-hospital mortality was higher for patients with advanced HF (18%) versus either patients with non-advanced HF (10%) or patients without HF (7%), including after stratification by age, sex, comorbidities, or concomitant admission diagnoses. Hospital survivors with HF had lower post-discharge survival (adjusted hazard ratio [HR] 1.8, 95% CI 1.5-2.2), with an incremental decrease in post-discharge survival for those with non-advanced HF (adjusted HR 1.7, 95% CI 1.4-2.0) or advanced HF (adjusted HR 3.4, 95% CI 2.6-4.5) versus those without HF; advanced HF was associated with higher risk than non-advanced HF (adjusted HR 2.3, 95% CI 1.8-2.9). Among all patients with advanced HF, the overall one-year survival estimate was 47% with a median survival of 0.7 years after CICU admission; estimated 5-year survival was 16%. Among hospital survivors with advanced HF (Figure part B), the overall one-year survival estimate was 52% and median survival was 1.1 years after hospital discharge; estimated 5-year survival was 20%; there was no difference in post-discharge survival according to LVEF.
HF, including advanced HF, is common in the community CICU population. Advanced HF accounted for 1 in 6 community patients admitted to the CICU with HF and presented with preserved LVEF in more than 1 in 3 patients. Patients with advanced HF had higher crude in-hospital mortality. Among hospital survivors, the risk of post-discharge mortality was higher in all HF groups compared to patients without HF. Patients with advanced HF had substantially worse outcomes than other HF patients including less than 50% one-year survival. The median survival of 0.7 years after admission for CICU patients with advanced HF is shorter than the median survival of approximately 1 year reported in the broader population-based cohort from Olmsted County, Minnesota, presumably due to the presence of critical illness in CICU patients.4 The Spanish EPICTER study similarly found that 1 in 4 patients hospitalized with HF had advanced HF; death occurred by 6 months in 48% of hospitalized patients with advanced HF.5
Our data highlight the frequency with which HF and advanced HF are found in the CICU population, document the poor short-term and long-term outcomes of CICU patients with HF, and identify CICU admission as a critical inflection point in the natural history of advanced HF. CICU providers will frequently encounter advanced HF, which may provide justification for the training of providers in the combination of advanced HF and critical care cardiology.
Table 1:
Comparison of patients with HF separated into those with and without advanced HF during hospitalization.
| Non-advanced HF (N=717) |
Advanced HF (N=144) |
HF (N=861) | p value | |
|---|---|---|---|---|
| Age | 76.3 (65.7, 84.3) | 76.4 (66.6, 86.0) | 76.4 (65.8, 84.4) | 0.545 |
| Female | 313 (43.7%) | 67 (46.5%) | 380 (44.1%) | 0.526 |
| Charlson Index | 3.0 (1.0, 6.0) | 5.0 (3.0, 8.0) | 3.0 (1.0, 6.0) | < 0.001 |
| Admission diagnosis of shock | 136 (19.0%) | 21 (14.6%) | 157 (18.2%) | 0.214 |
| Day 1 SOFA | 3.0 (1.0, 6.0) | 4.0 (3.0, 7.0) | 3.0 (2.0, 6.0) | < 0.001 |
| APACHE III | 63.0 (51.0, 78.0) | 69.0 (55.0, 83.0) | 63.0 (51.0, 79.0) | 0.005 |
| LVEF (%) | 40 (30, 55) | 37 (22, 56) | 40 (30, 55) | 0.114 |
| Invasive Vent | 128 (17.9%) | 20 (13.9%) | 148 (17.2%) | 0.250 |
| Noninvasive Vent | 198 (27.6%) | 57 (39.6%) | 255 (29.6%) | 0.004 |
| Vasoactive drugs | 162 (22.6%) | 53 (36.8%) | 215 (25.0%) | < 0.001 |
| Temporary MCS | 77 (10.7%) | 9 (6.2%) | 86 (10.0%) | 0.101 |
| PAC | 53 (7.4%) | 28 (19.4%) | 81 (9.4%) | < 0.001 |
| Dialysis | 31 (4.3%) | 11 (7.6%) | 42 (4.9%) | 0.092 |
| Admission chloride | 102.0 (99.0, 105.0) | 99.0 (95.0, 103.8) | 102.0 (98.0, 105.0) | < 0.001 |
| Admission BUN | 23.0 (17.0, 35.0) | 36.0 (22.0, 58.0) | 24.0 (17.0, 37.0) | < 0.001 |
| Admission creatinine | 1.1 (0.9, 1.6) | 1.5 (1.1, 2.3) | 1.2 (0.9, 1.7) | < 0.001 |
| Admission RDW | 14.4 (13.6, 15.6) | 16.0 (14.6, 17.2) | 14.6 (13.7, 16.0) | < 0.001 |
| In-hospital mortality | 71 (9.9%) | 26 (18.1%) | 97 (11.3%) | 0.005 |
| One-year mortality* | 117 (18.1%) | 56 (47.5%) | 173 (22.6%) | < 0.001 |
| Rehospitalization by 1 year* | 299 (46.4%) | 64 (54.2%) | 363 (47.6%) | 0.115 |
| Death or rehospitalization by 1 year* | 379 (58.8%) | 102 (86.4%) | 481 (63.0%) | < 0.001 |
Among hospital survivors (n = 764)
Sources of funding:
This study was funded in part by the National Institutes of Health (R01 HL144529, PI: Dunlay) and made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health (R01 AG034676). Dr. Jentzer’s time for this work was supported in part by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery.
Footnotes
Financial disclosures: None of the authors has a relevant conflict of interest.
References
- 1.Crespo-Leiro MG, Metra M, Lund LH, Milicic D, Costanzo MR, Filippatos G, Gustafsson F, Tsui S, Barge-Caballero E, De Jonge N, Frigerio M, Hamdan R, Hasin T, Hulsmann M, Nalbantgil S, Potena L, Bauersachs J, Gkouziouta A, Ruhparwar A, Ristic AD, Straburzynska-Migaj E, McDonagh T, Seferovic P and Ruschitzka F. Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018;20:1505–1535. [DOI] [PubMed] [Google Scholar]
- 2.Jentzer JC, Reddy YN, Rosenbaum AN, Dunlay SM, Borlaug BA and Hollenberg SM. Outcomes and Predictors of Mortality Among Cardiac Intensive Care Unit Patients With Heart Failure. J Card Fail. 2022;28:1088–1099. [DOI] [PubMed] [Google Scholar]
- 3.Jentzer JC, van Diepen S, Barsness GW, Katz JN, Wiley BM, Bennett CE, Mankad SV, Sinak LJ, Best PJ, Herrmann J, Jaffe AS, Murphy JG, Morrow DA, Wright RS, Bell MR and Anavekar NS. Changes in comorbidities, diagnoses, therapies and outcomes in a contemporary cardiac intensive care unit population. Am Heart J. 2019;215:12–19. [DOI] [PubMed] [Google Scholar]
- 4.Dunlay SM, Roger VL, Killian JM, Weston SA, Schulte PJ, Subramaniam AV, Blecker SB and Redfield MM. Advanced Heart Failure Epidemiology and Outcomes: A Population-Based Study. JACC Heart Fail. 2021;9:722–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fernandez-Martinez J, Romero-Correa M, Salamanca-Bautista P, Aramburu-Bodas O, Formiga F, Vazquez-Rodriguez P, Conde-Martel A, Garcia-Garcia JA, Paez-Rubio I, Lopez-Reboiro M, Sanchez-Sanchez C, Arias-Jimenez JL and group EI. Prevalence of advanced heart failure and use of palliative care in admitted patients: Findings from the EPICTER study. Int J Cardiol. 2021;327:125–131. [DOI] [PubMed] [Google Scholar]