Abstract
Objective To assess the effectiveness of metformin in the incidence of gestational diabetes mellitus (GDM) in obese pregnant women attending a public maternity hospital in Joinville, Santa Catarina, Brazil.
Methods Randomized clinical trial including obese pregnant women with a body mass index (BMI) ≥ 30 kg/m2, divided into two groups (control and metformin). Both groups received guidance regarding diet and physical exercise. The participants were assessed at two moments, the first at enrollment (gestational age ≤ 20) and the second at gestational weeks 24–28. The outcomes assessed were BMI and gestational diabetes mellitus (GDM) diagnosis. The data distribution was assessed with the Friedman test. For all the analytical models, the p-values were considered significant when lower than 0.05. The absolute risk reduction was also estimated.
Results Overall, 164 pregnant women were assessed and further divided into 82 participants per group. No significant difference was observed in BMI variation between the control and metformin groups (0.9 ± 1.2 versus 1.0 ± 0.9, respectively, p = 0.63). Gestational diabetes mellitus was diagnosed in 15.9% (n = 13) of the patients allocated to the metformin group and 19.5% (n = 16) of those in the control group (p = 0.683). The absolute risk reduction was 3.6 (95% confidence interval 8.0–15.32) in the group treated with metformin, which was not significant.
Conclusion Metformin was not effective in reducing BMI and preventing GDM in obese pregnant women.
Keywords: obesity, gestation, gestational diabetes mellitus, metformin
Abstract
Resumo
Objetivo Avaliar a efetividade da metformina na incidência de diabetes mellitus gestacional (DMG) em gestantes obesas de uma maternidade pública de Joinville, Santa Catarina, Brasil.
Métodos Ensaio clínico randomizado desenvolvido com gestantes obesas com índice de massa corporal (IMC) ≥ 30 kg/m2, divididas em dois grupos (controle e metformina). Ambos os grupos receberam orientação sobre dieta e exercício físico. As participantes foram avaliadas em dois momentos, o primeiro na inclusão (com idade gestacional ≤ 20 semanas) e o segundo entre 24 e 28 semanas de gestação. Os desfechos avaliados foram IMC e diagnóstico de diabetes mellitus gestacional (DMG). A distribuição dos dados foi avaliada com o teste de Friedman. Para todos os modelos analíticos, foram considerados significativos os valores de p inferiores a 0,05. Foi estimada também a redução absoluta de risco.
Resultados Foram avaliadas 164 gestantes, divididas em 82 participantes em cada grupo. Não houve diferença significativa na variação do IMC entre os grupos controle e metformina (0,9 ± 1,2 versus 1,0 ± 0,9, respectivamente, p = 0,63). O DMG foi diagnosticado em 15,9% (n = 13) das pacientes alocadas para o grupo metformina e 19,5% (n = 16) das incluídas no grupo controle (p = 0,683). A redução absoluta de risco foi de 3,6 (intervalo de confiança de 95% 8,0–15,32) no grupo metformina, o que não foi significativo.
Conclusão A metformina não foi eficaz em reduzir o IMC e prevenir o DMG em gestantes obesas.
Palavras-chave: obesidade, gestação, diabetes mellitus gestacional, metformina
Introduction
Obesity is one of the major epidemics of this millennium and is considered a public health problem by the World Health Organization (WHO).1 In Brazil, cases of obesity have grown over the last decades; specifically among women, 1.9 million cases were registered in 1975 compared with 18 million in 2014.2 This public health problem affects a great number of women, particularly those in reproductive age.3
Maternal obesity during pregnancy is associated with the development of gestational diabetes mellitus (GDM).4 Gestational diabetes mellitus is the most common metabolic disorder during gestation, affecting 3–25% of all pregnancies, depending on the diagnostic criteria applied and on the population and ethnic groups studied. Between 24–28 weeks of gestation, all pregnant women without a previous diagnosis of diabetes undergo screening for GDM with the oral glucose tolerance test (OGTT) after 8 hours of fasting. The Brazilian Society of Diabetes (Sociedade Brasileira de Diabetes [SBD, in the Portuguese acronym]) recommends that pregnant women should be classified as having GDM when presenting a blood glucose level between 92 and 125 mg/dL at fasting, ≥ 180 mg/dL at 1 hour, or 153–199 mg/dL at 2 hours; an abnormal result at one of the time points of the test characterizes GDM.5
Prevention of hyperglycemia during pregnancy may reduce immediate adverse pregnancy outcomes, childbirth risks, and, consequently, costs to the public health care system directed to GDM treatment.6 Strategies for GDM prevention among women at risk of developing the disease may include changes in lifestyle, reduction of obesity, nutritional intervention, physical activity, and pharmacological measures.7
Women who develop GDM during one of the gestational trimesters require attention during prenatal care to stabilize blood glucose levels to values similar to those of pregnant women without GDM.6 8 Nutritional therapy is the first step in GDM management, but when it fails to achieve glycemic control, it is associated with drug therapy.8 The standard pharmacological treatment of GDM is insulin therapy; however, oral hypoglycemic agents, like metformin, have also been used for glycemic control of overweight and obese women with GDM.9
In obese pregnant women, nutritional intervention and lifestyle changes may reduce many of the problems caused by GDM, achieving reduced blood glucose levels and BMI, as well as controlled blood pressure; however, low adherence by the patients fails to lead to a significant decrease in GDM incidence.10 11
The use of drugs like metformin has a preventive effect, especially in the control of obesity, which is one of the major causes of GDM. In the past, the use of hypoglycemic agents was contraindicated during pregnancy due to a risk of teratogenicity; however, this concept has changed over the past years. Metformin is no longer considered teratogenic; it is now considered a safe drug during pregnancy, with a low incidence of side effects, in addition to being helpful in controlling blood glucose levels and reducing BMI and levels of total cholesterol and fractions.12 13 When associated with lifestyle changes, metformin is also a potentially effective and safe approach to obesity and GDM control.13 14 15
Based on these considerations, this study aimed at evaluating the effectiveness of metformin in the incidence of GDM in obese pregnant women attending a public maternity hospital in Joinville (Santa Catarina, Brazil).
Methods
The present study was a randomized clinical trial analyzing the use of metformin in obese pregnant women, who were randomized into two groups (control group and metformin group). Both groups received counseling regarding diet and physical activity. All pregnant women received care by a multidisciplinary team comprising a nutritionist, nurse, physical therapist, and an obstetrician in a reference maternity hospital in the city of Joinville (Santa Catarina, Brazil).
Considering that GDM has a 2-fold higher risk in obese women and an incidence of 18% in the general population, and with the objective of obtaining a 50% decreased incidence with the drug, with a confidence level of 80%, we found that a sample size of 94 subjects in each group would be adequate. Considering a 10% rate of loss to follow-up, we selected 208 pregnant women to participate in the study, 104 of whom were allocated to the control group and 104 to the metformin group.5
The data were collected at Maternidade Darcy Vargas (MDV, in the Portuguese acronym) from October 31, 2014 to October 1, 2016. The study was initiated after approval by the Research Ethics Committee at Universidade da Região de Joinville (Univille), with the Certificate of Presentation for Appreciation (CAAE, in the Portuguese acronym) approval number 34863514.1.0000.5366, and was made possible by the Research Ethics Committee of Hospital Regional Hans Dieter Schmidt/Sesc/SC, with the CAAE approval number 34863514.1.3001.5363. This study is registered with the Brazilian Registry of Clinical Trials with the code RBR-9rpqdn and identification number U1111–1162–6908. This report follows the recommendations of the Consolidated Standards Reporting Trial (CONSORT).16
Pregnant women with gestational age (GA) ≤ 20 weeks and obesity (body mass index [BMI] ≥ 30 kg/m2) were referred by primary health care units to the gestational obesity outpatient clinic at the MDV. The patients were invited to participate during lectures held at the MDV auditorium about gestational obesity and the effectiveness of metformin in the prevention of GDM, during which the study objectives, as well as its risks and benefits, were explained. The women who agreed to participate in the study signed two copies of a free and informed consent form, one of which was given to the participant and the other was maintained by the principal investigator. The lectures took place on Thursdays at 7:30 am in the MDV auditorium during the period of the study.
The study included pregnant women with a diagnosis of obesity according to the WHO criteria (BMI ≥ 30 kg/m2); age ≥ 18 years; negative GDM screening in early pregnancy (GA ≤ 20 weeks); no history of diabetes before pregnancy; no allergy to metformin; no history or presence of liver, renal, or gastrointestinal disease, or other condition that could interfere with the absorption, distribution, excretion, or metabolism of the drug. We excluded women who interrupted the follow-up, had intolerance or allergic reaction to the drug, or refused to continue participating in the study.
The participants received prenatal care according to the primary protocol recommended by the Brazilian Ministry of Health. Screening for GDM was performed between 24–28 weeks with the OGTT (75 g of glucose diluted at 25%). According to the SBD, a diagnosis of GDM should be established in pregnant women presenting a glucose level between 92 and 125 mg/dL at fasting, ≥ 180 mg/dL at 1 hour, or 153 to 199 mg/dL at 2 hours; an abnormal result at one of the time points of the test characterizes GDM.5
All participants were referred for nutritional care, in which they received dietary guidance with small reductions in their caloric intake of 24 kcal/kg/day, a fractionated diet with five to six daily meals, a daily caloric composition comprising 40–50% of fiber-rich complex carbohydrates, 20% of protein, and 30–40% of unsaturated fats. Daily calories were distributed as 10–20% at breakfast, 20–30% at lunch, 20–30% at dinner, and up to 30% as snacks, including a snack before bedtime to avoid nocturnal hypoglycemia. The participants were referred to physical therapy and received recommendations for physical activity, with a regular walking program of 20 minutes per day.17
Participants in the metformin group received a metformin dose of 1,000 mg twice daily (500 mg at breakfast and 500 mg at dinnertime), as prescribed by the obstetrician. If a diagnosis of GDM was established, metformin was not discontinued, since it was offered free of charge by the Brazilian Unified Health System (SUS, in the Portuguese acronym). Laboratory tests were performed at Laboratório Gimenez Ltda., which is located adjacent to the MDV. All tests performed in the study are part of the clinical and laboratory routine of obese pregnant women seen at MDV.
During the first visit to the gestational obesity outpatient clinic, the participants were randomized with a computerized algorithm using the software Microsoft Excel (Microsoft, Redmond, WA, USA), which generated a random allocation order list in a non-fixed proportion, divided into two groups: a study group, which was treated with metformin and received guidance on diet and physical activity, and a control group, which received only diet and physical activity counseling. The participants received a coded seal on their prenatal follow-up record, which identified them as participants of the multidisciplinary research team during outpatient visits throughout the study.
All patients were identified using a specific research form containing the participant's name; date of birth; age; marital status; occupation; educational level; ethnicity; BMI; GA; allergy to metformin; number of pregnancies; age at birth of first child; interval between deliveries; abortion; type of delivery; use of medication during pregnancy; diagnosis of liver, renal, or gastrointestinal disease; diagnosis of GDM in previous pregnancies; and diagnosis of polycystic ovary disease. The results of the laboratory tests, fasting blood glucose levels, and OGTT throughout the prenatal period were recorded during appointments at the obesity outpatient clinic. The tests were ordered at baseline (GA ≤ 20 weeks) and at 24–28 gestational weeks.
For the statistical analysis, the collected data were entered into a Microsoft Excel version 2016 spreadsheet and were later analyzed using the statistical software IBM SPSS Statistics version 22.0 (IBM Corp., Armonk, NY, USA). The quantitative variables are presented as mean and standard deviation, while the qualitative variables are represented as absolute and relative frequencies. Once the normal distribution of the studied characteristics was confirmed, the Student t-test was applied to analyze quantitative variables and the chi-square test for qualitative ones. To verify the distribution of fasting blood glucose values before and after treatment, box-plot graphs were built, and the Friedman test was used to compare the distribution of the data. For all analytical models, p values below 0.05 were considered significant, and the absolute risk reduction was estimated.
Results
Obese pregnant women with a BMI ≥ 30 kg/m2, classified as having high-risk pregnancies, were referred by the primary health care units to the gestational obesity outpatient clinic at the MDV maternity, as shown in Fig. 1.
Fig. 1.
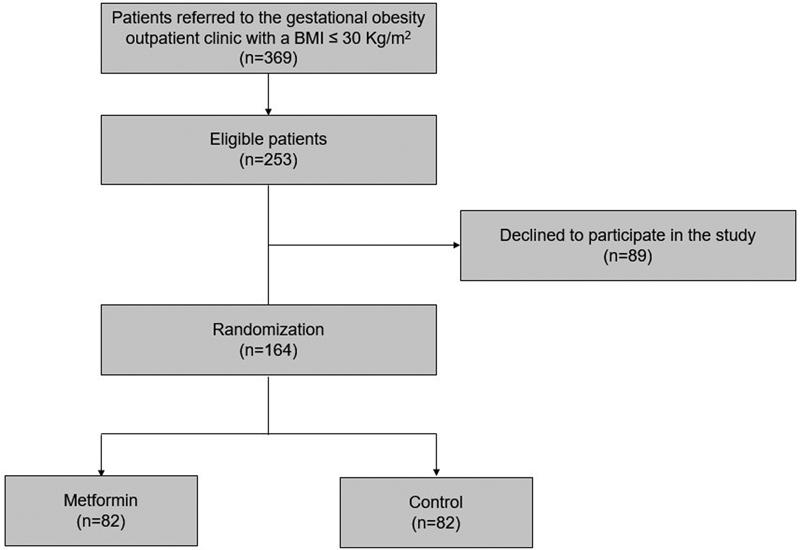
Flowchart of the participants at each stage of the study.
Among the pregnant women referred to the clinic, 116 failed to meet the study's inclusion criteria. Out of 253 eligible obese pregnant women, 89 declined to participate in the study, yielding 164 participants for randomization, of whom 82 were enrolled in the metformin group and 82 in the control group. The main demographic characteristics analyzed in the study were maternal age, marital status, occupation, education level, ethnicity, number of pregnancies, and GA at the first visit. Assessments included the anthropometric characteristic BMI and the metabolic parameter fasting blood glucose level (in mg/dL) Table 1.
Table 1. Characteristics of obese pregnant women at ≤ 20 weeks of gestation.
| Metformin (n = 82) |
Control (n = 82) |
p value | |
|---|---|---|---|
| Age (years) | |||
| Mean (SD) | 28.8 (6.0) | 29.7 (6.3) | 0.36† |
| Range | 18.0–40.0 | 19.0–44.0 | |
| Marital status | |||
| Married | 63 (76.8) | 66 (80.5) | 0.56‡ |
| Single | 19 (23.2) | 16 (19.5) | |
| Occupation | |||
| Working | 82 (100) | 82 (100) | – |
| Not working | 0 (0.0) | 0 (0.0) | |
| Education level | |||
| Elementary school | 27 (32.9) | 25 (30.5) | 0.89‡ |
| High school | 42 (51.2) | 45 (54.9) | |
| Higher education | 13 (15.9) | 12 (14.6) | |
| Ethnicity | |||
| White | 67 (81.7) | 65 (79.3) | 0.86‡ |
| Black | 8 (9.8) | 8 (9.8) | |
| Others | 7 (8.5) | 9 (11.0) | |
| Number of pregnancies | |||
| Mean (SD) | 2.3 (1.3) | 2.6 (1.5) | 0.09† |
| Range | 1.0–6.0 | 1.0–8.0 | |
| GA (first visit) | |||
| Mean (SD) | 15.1 (4.2) | 17.1 (4.6) | < 0.01† |
| Range | 5.0–24.0 | 6.0–26.0 | |
| Fasting glucose (mg/dL) | |||
| Mean (SD) | 79.3 (9.5) | 80.4 (10.2) | 0.47† |
| Range | 52.0–99.0 | 63.0–120.0 | |
| BMI (kg/m2) | |||
| Mean (SD) | 37.5 (4.7) | 37.5 (5.0) | 0.99† |
| Range | 25.3–50.8 | 25.3–49.5 | |
Abbreviations: BMI, body mass index; GA, gestational age; SD, standard deviation.
Student t test.
Chi-square test.
When comparing BMI values in the control and metformin groups prior to metformin treatment, at GA ≤ 20 weeks, and after treatment, at 24–28 gestational weeks, no influence of the drug was observed on BMI increase in the control and metformin groups (0.9 ± 1.2 versus 1.0 ± 0.9, respectively, p = 0.63) Table 2).
Table 2. Body mass index at ≤ 20 weeks and 24–28 weeks of gestation in obese pregnant women in the control and metformin groups.
| Control Group (n = 82) | Metformin Group (n = 82) | Δ Metformin versus Δ Control (p) |
|||||
|---|---|---|---|---|---|---|---|
| ≤ 20 | 24–28 | Δ | ≤ 20 | 24–28 | Δ | ||
| BMI kg/m2
(mean ± SD) |
37.5 ± 4.7* | 38.4 ± 4.9* | 0.9 ± 1.2 | 37.5 ± 5.0* | 38.5 ± 5.1* | 1.0 ± 0.9 | 0.63** |
Abbreviations: Δ, Variation; BMI, body mass index, SD, standard deviation. *Student t-test. **Chi-square test.
Blood glucose levels during the OGTT were comparable among participants allocated to the metformin and control groups: fasting 77.5 (9.0) mg/dL and 78.9 (12.1) mg/dL, respectively (p = 0.66), 1 hour 129.3 (27.5) mg/dL and 134.0 (33.9) mg/dL, respectively (p = 0.50), 2 hours 110.6 (28.1) mg/dL and 111.7 (30.6) mg/dL, respectively (p = 0.99) Fig. 2.
Fig. 2.
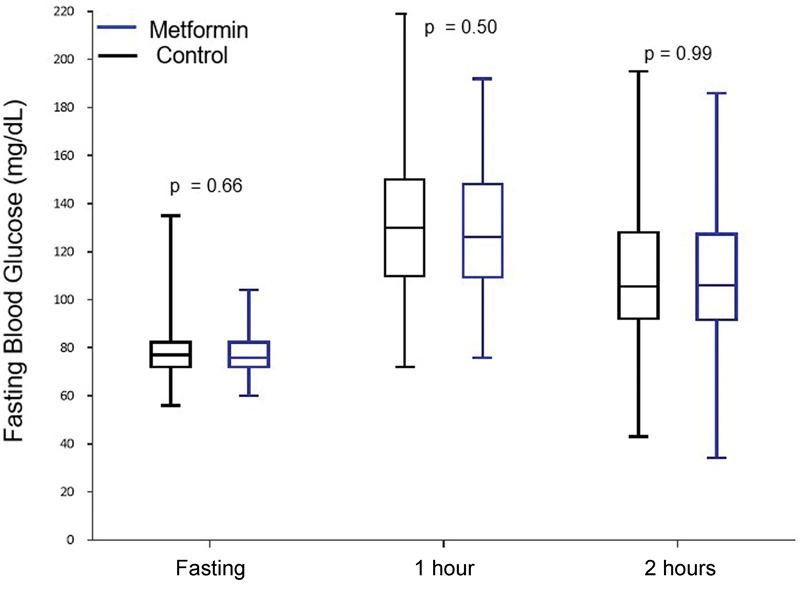
Oral glucose tolerance test (OGTT) at 24–28 gestational weeks in obese pregnant women allocated to the metformin and control groups
The diagnosis of GDM was established in 13 (15.9%) patients in the metformin group and 16 (19.5%) of those in the control group (p = 0.683). The absolute risk reduction in the metformin group was 3.6 (95% confidence interval -8.0 to 15.32), which was not significant. The magnitude of the risk of GDM development in the metformin group was equivalent to 80% of that in the control group, that is, the metformin group had a 20% reduction in the risk of GDM development compared with the control group, as shown in Table 3.
Table 3. Absolute risk reduction in the incidence of gestational diabetes mellitus with metformin in obese pregnant women.
| Group | N (%) | P value | |
|---|---|---|---|
| Gestational diabetes mellitus | Metformin | 13 (15.9) | 0.683 |
| Control | 16 (19.5) | ||
| Absolute risk reduction (95%CI) | NNT | ||
| 3.6% (-0.08–0.15) | 25 | ||
Abbreviation: NNT, number needed to treat; 95%CI, 95% confidence interval.
Discussion
The present study demonstrated that none of the groups (control or metformin) influenced the BMI increase between gestational weeks ≤ 20 and 24–28, and that the efficacy of metformin in preventing the development of GDM in obese pregnant women was not significant. The general characteristics of the participants in each group showed no significant differences, except for GA at the first visit. Similar findings have been observed regarding maternal characteristics and obstetric history in a clinical trial with 202 obese pregnant women treated with metformin.11 Another study with 43 pregnant women, which assessed the glycemic control with metformin during pregnancy in GDM, also found no significant differences in demographic characteristics among the groups.18
The relationship between the pharmacodynamics and pharmacokinetic mechanisms of metformin has not been well elucidated in the scientific literature yet, especially concerning the effect of these mechanisms on obese pregnant women. However, studies have demonstrated the ability of metformin to activate the AMP-activated protein kinase (AMPK), a protein involved in the control of body energy and a metabolic substrate, helping to reduce the BMI.13 14 15 16 17 18 19 Several studies have shown fewer BMI changes among obese women with GDM treated with this drug.20 21 22
The results of the present study identified that participants in both control and metformin groups showed no significant increase in BMI between gestational weeks ≤ 20 and 24–28. The combination of metformin with lifestyle changes represents a potentially effective and safe approach to obesity control.14 According to Fattah et al,15 metformin limits the weight gain throughout pregnancy. A similar finding has been reported in a clinical trial by Syngelaki et al,11 in which obese women without GDM taking prophylactic metformin for 12–18 weeks until delivery achieved lower weight gain during pregnancy, in contrast to the findings of the present study.
Of note, both groups received diet and physical activity counseling in the present study. According to the literature, adherence to these preventive practices by women before, during, and after pregnancy is effective in controlling BMI and blood glucose, and reducing the incidence of GDM.23 24 Promising results in GDM prevention have been observed among obese women adhering to nutritional counseling recommendations.25 26
Physical activity performed early in pregnancy has a beneficial effect in reducing the risk of GDM in obese women.27 28 Among the participants performing physical activity in the present study, GDM developed in 15.9% of those in the metformin group and 19.5% of those in the control group. Depending on the diagnostic criteria applied, GDM has an incidence between 3 and 25%, according to the Brazilian Society of Diabetes.5 A multicenter, prospective study performed in nine European countries compared different approaches to prevent GDM among obese women; the study found that 14% of the women developed GDM between 24 and 28 weeks of gestation, regardless of the interventions used.29 These findings are similar to those in the present study.
Women presenting with increased BMI, elevated fasting blood glucose level, and glucose intolerance have an increased short- and long-term risk of developing diabetes mellitus. However, according to the results of a study assessing the impact of lifestyle and metformin interventions over 10 years in women with a history of GDM in 27 clinical centers,30 this risk can be substantially reduced with lifestyle changes and use of metformin. In the present study, 15.9% of the participants treated with metformin along with diet and physical activity developed GDM. Of note, lifestyle changes must take place during pregnancy to reduce the risk of GDM occurring before the 15th week of gestation in women with obesity.27 31
The differences in the results of the OGTT, performed in both control and metformin groups, were not significant. However, other studies with GDM women support the treatment of GDM with metformin, without an increased risk of maternal hypoglycemia.13 32 33 34 35 In the present study, metformin was administered at a dosage of 1,000 mg twice daily. This dose of 1,000 mg is different from the one used in another study with 104 pregnant women treated with 500 to 2,500 mg of metformin, in which the drug was effective in controlling blood glucose levels during pregnancy.18 A clinical trial with 132 pregnant women also treated with metformin 500–2,500 mg also obtained blood glucose control at 28 weeks of gestation.6 In contrast, a clinical trial with 100 pregnant women treated with metformin 500–1,500 mg found no significant difference in glycemic control.15
Studies performed with pregnant women with polycystic ovary syndrome (PCOS) who underwent lifestyle changes combined with treatment with metformin have shown a relationship between lower BMI increase and improvements in metabolic rate and glycemic control. Of note, metformin has been used for some time in patients with PCOS with promising results when treatment is initiated before pregnancy.35
This study offers a new perspective in GDM prevention in obese women and is aligned with recommendations by other authors describing that prevention, detection, control, and early access to therapy are fundamental and necessary interventions to reduce the occurrence of GDM.36
Conclusion
Limitations of this study include the reduced number of pregnant women randomized to each group and the effectiveness of dietary intervention and physical activity. The study lacks high-quality evidence to offer significant conclusions regarding the benefits of the use of metformin in relation to diet and physical activity since a group without intervention was not used. Further studies are suggested to confirm the efficacy of metformin in a larger number of obese pregnant women in several centers throughout the country and with a metformin dose similar to that used in international clinical trials.
Conflicts of Interest The authors declare that there are no conflicts of interest.
Contributors
Sales W. B., Nascimento I. B., Dienstmann G., Souza M. L. R. and Silva G. D. have contributed with the project conception, analysis, and interpretation of data. Sales WB, Silva JC. Contributed with final approval of the version to be published: Sales W. B., Nascimento I. B., Dienstmann G., Souza M. L. R., Silva G. D., Silva J. C. have contributed with critical review of the intellectual content.
References
- 1.Instituto Brasileiro de Geografia e Estatística (IBGE). Pesquisa de Orçamentos Familiares 2008–2009: Antropometria e Estado Nutricional de Crianças, Adolescentes e Adultos no Brasil Rio de Janeio, RJ: IBGE; 2010 [Google Scholar]
- 2.Cesare M; NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants Lancet 2016387(10026):1377–1396.. Doi: 10.1016/S0140-6736(16)30054-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hajagos-Tóth J, Ducza E, Samavati R, Vari S G, Gaspar R.Obesity in pregnancy: a novel concept on the roles of adipokines in uterine contractility Croat Med J 2017580296–104.. Doi: 10.3325/cmj.2017.58.96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maffeis C, Morandi A.Effect of maternal obesity on foetal growth and metabolic health of the offspring Obes Facts 20171002112–117.. Doi: 10.1159/000456668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oliveira J EP, Vencio S. São Paulo, SP: A.C. Farmacêutica; 2016. Diretrizes da Sociedade Brasileira de Diabetes 2015–2016. [Google Scholar]
- 6.Chiswick C A, Reynolds R M, Denison F Cet al. Efficacy of metformin in pregnant obese women: a randomised controlled trial BMJ Open 2015501e006854. Doi: 10.1136/bmjopen-2014-006854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agha-Jaffar R, Oliver N, Johnston D, Robinson S.Gestational diabetes mellitus: does an effective prevention strategy exist? Nat Rev Endocrinol 20161209533–546.. Doi: 10.1038/nrendo.2016.88 [DOI] [PubMed] [Google Scholar]
- 8.Silva J C, Pacheco C, Bizato J, de Souza B V, Ribeiro T E, Bertini A M.Metformin compared with glyburide for the management of gestational diabetes Int J Gynaecol Obstet 20101110137–40.. Doi: 10.1016/j.ijgo.2010.04.028 [DOI] [PubMed] [Google Scholar]
- 9.Sales W B, Silva M R, Amaral A R, Ferreira B S, Silva J C, Bertini A MA.Eficácia da metformina no tratamento do diabetes mellitus gestacional Rev Bras Pesqui Saúde. 201517133–140.. Doi: 10.21722/rbps.v17i3.14510 [Google Scholar]
- 10.Koivusalo S B, Rönö K, Klemetti M Met al. Gestational diabetes mellitus can be prevented by lifestyle intervention: the Finnish gestational diabetes prevention study (RADIEL): a randomized controlled trial Diabetes Care 2016390124–30.. Doi: 10.2337/dc15-0511 [DOI] [PubMed] [Google Scholar]
- 11.Syngelaki A, Nicolaides K H, Balani Jet al. Metformin versus placebo in obese pregnant women without diabetes mellitus N Engl J Med 201637405434–443.. Doi: 10.1056/NEJMoa1509819 [DOI] [PubMed] [Google Scholar]
- 12.Arshad R, Kanpurwala M A, Karim N, Hassan J A.Effects of diet and metformin on placental morphology in gestational diabetes mellitus Pak J Med Sci 201632061522–1527.. Doi: 10.12669/pjms.326.10872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gray S G, McGuire T M, Cohen N, Little P J.The emerging role of metformin in gestational diabetes mellitus Diabetes Obes Metab 20171906765–772.. Doi: 10.1111/dom.12893 [DOI] [PubMed] [Google Scholar]
- 14.Al-Qallaf S M.Efficacy and safety of metformin in weight loss in bahraini population J Appl Pharm Sci 2016691–95.. Doi: 10.7324/JAPS.2016.60616 [Google Scholar]
- 15.El Fattah E AA.Can metformin limit weight gain in the obese with pregnancy? Int J Reprod Contracept Obstet Gynecol 20165818–825.. Doi: 10.18203/2320-1770.ijrcog20160591 [Google Scholar]
- 16.Schulz K F, Altman D G, Moher D; CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials BMJ 2010340c332. Doi: 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas. Gestação de Alto Risco: Manual Técnico. 5ª ed Brasília, DF: Editora do Ministério da Saúde; 2012 [Google Scholar]
- 18.Beyuo T, Obed S A, Adjepong-Yamoah K K, Bugyei K A, Oppong S A, Marfoh K.Metformin versus insulin in the management of pre-gestational diabetes mellitus in pregnancy and gestational diabetes mellitus at the Korle Bu Teaching Hospital: a randomized clinical trial PLoS One 20151005e0125712. Doi: 10.1371/journal.pone.0125712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bailey C J.Diabetes: insulin plus metformin for T2DM--are there benefits? Nat Rev Endocrinol 2012808449–450.. Doi: 10.1038/nrendo.2012.106 [DOI] [PubMed] [Google Scholar]
- 20.Kalra B, Gupta Y, Singla R, Kalra S.Use of oral anti-diabetic agents in pregnancy: a pragmatic approach N Am J Med Sci 20157016–12.. Doi: 10.4103/1947-2714.150081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhu B, Zhang L, Fan Y Yet al. Metformin versus insulin in gestational diabetes mellitus: a meta-analysis of randomized clinical trials Ir J Med Sci 201618502371–381.. Doi: 10.1007/s11845-016-1414-x [DOI] [PubMed] [Google Scholar]
- 22.Feig D S, Murphy K, Asztalos Eet al. Metformin in women with type 2 diabetes in pregnancy (MiTy): a multi-center randomized controlled trial BMC Pregnancy Childbirth 20161601173. Doi: 10.1186/s12884-016-0954-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hayes L, Mcparlin C, Kinnunen T I, Poston L, Robson S C, Bell R; UPBEAT Consortium. Change in level of physical activity during pregnancy in obese women: findings from the UPBEAT pilot trial BMC Pregnancy Childbirth 20151552. Doi: 10.1186/s12884-015-0479-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.de Wit L, Jelsma J GM, van Poppel M NMet al. Physical activity, depressed mood and pregnancy worries in European obese pregnant women: results from the DALI study BMC Pregnancy Childbirth 201515158. Doi: 10.1186/s12884-015-0595-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Donazar-Ezcurra M, López-Del Burgo C, Bes-Rastrollo M.Primary prevention of gestational diabetes mellitus through nutritional factors: a systematic review BMC Pregnancy Childbirth 2017170130. Doi: 10.1186/s12884-016-1205-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Magro-Malosso E R, Saccone G, Di Mascio D, Di Tommaso M, Berghella V.Exercise during pregnancy and risk of preterm birth in overweight and obese women: a systematic review and meta-analysis of randomized controlled trials Acta Obstet Gynecol Scand 20179603263–273.. Doi: 10.1111/aogs.13087 [DOI] [PubMed] [Google Scholar]
- 27.Song C, Li J, Leng J, Ma R C, Yang X.Lifestyle intervention can reduce the risk of gestational diabetes: a meta-analysis of randomized controlled trials Obes Rev 20161710960–969.. Doi: 10.1111/obr.12442 [DOI] [PubMed] [Google Scholar]
- 28.Wang C, Wei Y, Zhang Xet al. A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women Am J Obstet Gynecol 201721604340–351.. Doi: 10.1016/j.ajog.2017.01.037 [DOI] [PubMed] [Google Scholar]
- 29.Egan A M, Vellinga A, Harreiter Jet al. Epidemiology of gestational diabetes mellitus according to IADPSG/WHO 2013 criteria among obese pregnant women in Europe Diabetologia 201760101913–1921.. Doi: 10.1007/s00125-017-4353-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aroda V R, Christophi C A, Edelstein S Let al. The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up J Clin Endocrinol Metab 2015100041646–1653.. Doi: 10.1210/jc.2014-3761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chasan-Taber L.Lifestyle interventions to reduce risk of diabetes among women with prior gestational diabetes mellitus Best Pract Res Clin Obstet Gynaecol 20152901110–122.. Doi: 10.1016/j.bpobgyn.2014.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kitwitee P, Limwattananon S, Limwattananon Cet al. Metformin for the treatment of gestational diabetes: An updated meta-analysis Diabetes Res Clin Pract 201510903521–532.. Doi: 10.1016/j.diabres.2015.05.017 [DOI] [PubMed] [Google Scholar]
- 33.McGrath R T, Glastras S J, Hocking S, Fulcher G R.Use of metformin earlier in pregnancy predicts supplemental insulin therapy in women with gestational diabetes Diabetes Res Clin Pract 201611696–99.. Doi: 10.1016/j.diabres.2016.04.051 [DOI] [PubMed] [Google Scholar]
- 34.Nachum Z, Zafran N, Salim Ret al. Glyburide versus metformin and their combination for the treatment of gestational diabetes mellitus: a randomized controlled study Diabetes Care 20174003332–337.. Doi: 10.2337/dc16-2307 [DOI] [PubMed] [Google Scholar]
- 35.Zhang J, Si Q, Li J.Therapeutic effects of metformin and clomiphene in combination with lifestyle intervention on infertility in women with obese polycystic ovary syndrome Pak J Med Sci 201733018–12.. Doi: 10.12669/pjms.331.11764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ogurtsova K, da Rocha Fernandes J D, Huang Yet al. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040 Diabetes Res Clin Pract 201712840–50.. Doi: 10.1016/j.diabres.2017.03.024 [DOI] [PubMed] [Google Scholar]


