Abstract
Background:
With health care costs increasing, the cost of caring for older adults is rising. Understanding the costs of surgical care for older adults is crucial in planning for health care services. We hypothesize that increasing age predicts increasing surgical inpatient costs.
Methods:
We conducted a retrospective analysis of general surgical inpatient costs at 4 hospitals over 2 fiscal years. We assessed the cost and number of procedures by age, procedure, hospital, cost category and surgical urgency. Costs were compared between surgical risk profile, urgency and age. Cost differences of 10% or more were considered clinically important.
Results:
We examined the surgical inpatient costs for 12 070 procedures, representing 84% of all admissions in the region. The average cost was $4351 for scheduled admissions and $4054 for unscheduled admissions. Only unscheduled admissions resulted in higher costs in older age groups, more than doubling in patients aged 80 years and older undergoing low- and moderate-risk unscheduled surgery. The higher costs for older adults was primarily because of higher postoperative costs. In addition, the screening of candidates for elective surgery may have resulted in preoperative medical optimization leading to decreased admission costs.
Conclusion:
Older adults requiring surgery incur increased costs only if admitted for emergency surgery. The cost increase associated with unscheduled admissions was primarily for increased postoperative costs. Innovative programs to reduce costs for postoperative care for older adults undergoing emergency surgery should be investigated.
Abstract
Contexte:
Avec la hausse constante des coûts des soins de santé, prendre soin des adultes âgés coûte de plus en plus cher. Comprendre le coût des soins chirurgicaux chez la personne âgée est crucial pour la planification des soins de santé. Selon notre hypothèse, l’avancée en âge permet de prédire la hausse des coûts chez les maladies hospitalisés en chirurgie.
Méthodes:
Nous avons procédé à une analyse rétrospective des coûts d’hospitalisation en chirurgie générale dans 4 hôpitaux sur une période de 2 années financières. Nous avons évalué les coûts et le nombre d’interventions par âge, type d’intervention, hôpital, poste de dépense et urgence chirurgicale. Les coûts ont été comparés entre profil de risque chirurgical, urgence et âge. Les différences de coûts égales ou supérieures à 10 % étaient considérées cliniquement importantes.
Résultats:
Nous nous sommes penchés sur les coûts d’hospitalisation pour 12 070 interventions, représentant 84 % de toutes les admissions dans la région. Le coût moyen était de 4351 $ pour les admissions planifiées et de 4054 $ pour les admissions non planifiées. Seules les admissions non planifiées ont entraîné des coûts plus élevés dans les catégories d’âge plus avancées, soit de plus du double chez les personnes de 80 ans et plus soumises à des interventions non planifiées assorties d’un risque faible et modéré. Les coûts plus élevés associés à l’âge avancé ont été générés principalement par les soins postopératoires. De plus, la sélection des personnes candidates à des chirurgies non urgentes peut avoir donné lieu à une optimisation médicale préopératoire, entraînant une baisse des coûts d’admission.
Conclusion:
Les adultes âgés qui doivent être opérés n’encourent des coûts plus élevés que s’ils sont admis pour une chirurgie urgente. La hausse des coûts associée à une admission non planifiée découle principalement de la hausse des coûts postopératoires. Il faudrait se pencher sur des programmes novateurs afin de réduire les coûts des soins postopératoires chez les adultes âgés soumis à des chirurgies urgentes.
Postoperative complications are more frequent in patients undergoing unscheduled surgery1 and are associated with longer hospital admissions, increased disability, increased hospital admission cost,2,3 loss of independence and death.4,5 Unsurprisingly, unscheduled surgery is more costly than elective surgery.6 In a publicly funded health care system, careful stewardship of scarce resources is critical in controlling ever-increasing budgets. The adverse effects of lost productive years, increased dependency on family and government services and the increased risk of death result in high costs for the patient, their family and society in general.
Expanding surgical treatment criteria has led to more surgical candidates7,8 who are more prone to perioperative morbidity, resulting in a higher marginal cost of delivering care.2,3 As the baby boom generation ages, a large cohort of people will enter the most medically expensive phase of their lives.
The common perception of surgical care is that as patients age, the cost of care increases. Most reports examining the cost of health care will reference increasing cost of providing care, increased disease burden and aging populations as factors in rising health care costs.9,10 In addition, studies examining the cost of surgical intervention frequently report increasing cost being associated with increasing age.11,12 However, few studies have examined the cost of surgical admission in older adults or compared the costs of elective surgery with those of unscheduled (emergent) surgery. It is unclear how much elective compared with unscheduled surgical intervention contributes to the increased health care costs experienced by older adults, although Hofmeister and colleagues13 reported lower costs to provide care to older adults (≥ 65 yr) undergoing emergent abdominal surgery.13 Understanding the costs associated with surgical care for our growing population of older adults will be crucial in planning for health care services. To our knowledge, no studies have examined the association between the cost of inhospital care, age and emergency status (elective v. unscheduled) in a general surgery population. We hypothesized that costs would increase with age for all surgical risks and for elective and unscheduled surgical procedures.
Methods
Mean inpatient cost by case type and case volume were gathered using Lighthouse analytics software (Analysis-Works Inc.) for patients who were admitted between Apr. 1, 2014, and Mar. 30, 2016, and discharged between Apr. 1, 2014, and Sept. 30, 2016. We did not include day-surgery cases. Lighthouse is a business analytics software package designed to improve the management of hospital operations. It gathers patient-level data, using microcosting, and aggregates the data for real-time analytics of procedure costs over time down to the level of an individual surgeon. Data were provided in an aggregated and anonymized fashion and could not be traced back to individual clinical encounters. Ethical approval was obtained from the University of Alberta research ethics office (Pro00068273).
Costs and number of procedures were reported by age (17–64 yr, 65–79 yr and ≥ 80 yr), planned surgical procedure, hospital (University of Alberta Hospital, Royal Alexandra Hospital, Grey Nuns Community Hospital and Misericordia Community Hospital), cost category (operating room [OR] supplies, OR salaries, preoperative inpatient and postoperative inpatient costs) and scheduled compared with unscheduled procedure. Length of hospital stay was reported for inpatient, observation and intensive care beds for each surgical procedure; these data were aggregated by case type only, as we did not have data for length of hospital stay separated by scheduled and unscheduled surgical procedures.
All inpatient general surgery procedures at the 4 hospitals for which data were available were included, representing 84% of all general surgical procedures in the region. The Royal Alexandra Hospital and University of Alberta Hospital have 231 and 181 surgical beds, respectively, and are accredited trauma centres with tertiary and quaternary referral services and perform major roles in surgical education for the University of Alberta. The Misericordia Community Hospital and Grey Nuns Community Hospital have 92 and 60 surgical beds, respectively. Together, the hospitals represent 4 of the 5 primary hospitals for a catchment population of 1.3 million and are the tertiary referral centres for a population of 2.1 million. Only 1 other hospital performs a substantial volume of inpatient general surgical procedures within the Edmonton region, but they do not input data into the Lighthouse database.
Statistical analysis
Standard deviation and variance were not available for our data; the data were provided as means and sample size for the total number of cases and each of 21 surgical interventions for the 4 hospitals studied. We calculated the variance between the mean cost for each procedure at each hospital and the pooled mean for each subgroup analyzed. A 2-tailed Student t test was used to compare the pooled means using the measured variance between means. Degrees of freedom were the number of means used to calculate the pooled mean. Post hoc power analysis was performed with G*Power software (Universitat Kiel).14 To be conservative in power analysis, we assumed a moderate effect size and sample size of 68, which was the number of means used in the variance calculation (21 different surgeries performed at 4 separate sites where data were available). Some sites did not perform all procedures and did not report certain procedures. Costs were compared between community and teaching hospitals, surgical risk profile, surgical urgency and age category. Low-risk surgical procedures included head and neck, breast and superficial procedures, such as open inguinal hernia repair. Moderate-risk procedures entered the peritoneum but did not enter the bowel (cholecystectomy, appendectomy, ventral hernia or laparoscopic inguinal hernia) and included ileostomy reversal. High-risk procedures involved bowel resection of any kind and laparotomy procedures. Cost differences were considered to be statistically significant when the p value was less than 0.05 and clinically important when overall cost differences were 10% or more or cost subgroups differed by more than 25%. Both criteria were defined a priori after discussion among the authors, including a health economist (F.C.). We chose an overall difference of 10% as it represents a large enough difference to be financially important for hospital administrations. We chose a difference of 25% for subgroup analysis to reduce the risk of type I error because some subgroups had much smaller populations, which could result in higher variance in cost without true differences between the groups. The primary outcome was differences in inpatient cost of care between the 3 age groups for similar procedures.
Results
Overall, there were more than 14 000 inpatient general surgery procedures performed in the region over the 2 years studied. There were 12 070 general surgical procedures performed at the 4 hospitals included in this study, with 8870 classified as 1 of 21 predefined surgical interventions; 42.8% of the cases studied were unscheduled. Not all procedures were performed at all 4 hospitals (e.g., abdominoperineal resection was not performed at 1 hospital). There were 16 pooled means included in the low-risk group analysis: 31 in the moderate-risk group analysis and 21 in the high-risk group analysis. Two of every 3 procedures were performed on patients aged younger than 65 years (Table 1). Post hoc power analysis using the number of pooled means (n = 68) as sample size for each arm, a moderate effect size (0.5) and α equalling 0.05 yielded a power of 0.89. If each surgical case was used when calculating sample size, the power was 1.
Table 1.
Scheduled and unscheduled cases with average case cost by age
| Age, yr | Total | Scheduled cases | Unscheduled cases | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| No. of cases | Inpatient cost, $ | No. of cases | Inpatient cost, $ | No. of cases | Inpatient cost, $ | |
| ≤64 | 8451 | 3951 | 4373 | 4422 | 4078 | 3447 |
|
| ||||||
| 65–79 | 2863 | 4794 | 2021 | 4333 | 842 | 5902 |
|
| ||||||
| ≥80 | 756 | 5105 | 500 | 3815 | 256 | 7622 |
|
| ||||||
| Average | 12 070 | 4224 | 6894 | 4351 | 5176 | 4054 |
The average case cost was $4351 for scheduled cases and $4054 for unscheduled cases (n = 12 070). Length of hospital stay increased with age, averaging 4.4 days per case, and was 1.5 days longer at teaching hospitals than community hospitals (Table 2). However, length of stay in hospital was not statistically significant when pooled lengths for each predefined surgical intervention at community or academic centres were compared (Student t test, total cases = 8870, pooled means compared = 68, p = 0.48). We did not have data on length of hospital stay separated by emergent compared with elective procedures for analysis, and cases that were not in our predefined surgical procedures are available only in the overall data set.
Table 2.
Length of hospital stay by acuity of care, hospital type and age for general surgical inpatients
| Age, yr | No. of patients | Acuity of care, d | Total LOS, d | Average LOS, d (no. of patients) | |||
|---|---|---|---|---|---|---|---|
| Acute | Observation | ICU | Community hospital | Teaching hospital | |||
| ≤64 | 8451 | 3.7 | 0.1 | 0.0 | 3.8 | 3.0 (3515) | 4.4 (4936) |
| 65–79 | 2863 | 5.4 | 0.1 | 0.1 | 5.5 | 4.4 (1355) | 6.5 (1508) |
| ≥80 | 756 | 6.7 | 0.1 | 0.1 | 6.8 | 6.3 (367) | 7.4 (389) |
| Overall | 12 070 | 4.3 | 0.1 | 0.0 | 4.4 | 3.5 (5237) | 5.0 (6833) |
ICU = intensive care unit; LOS = length of hospital stay.
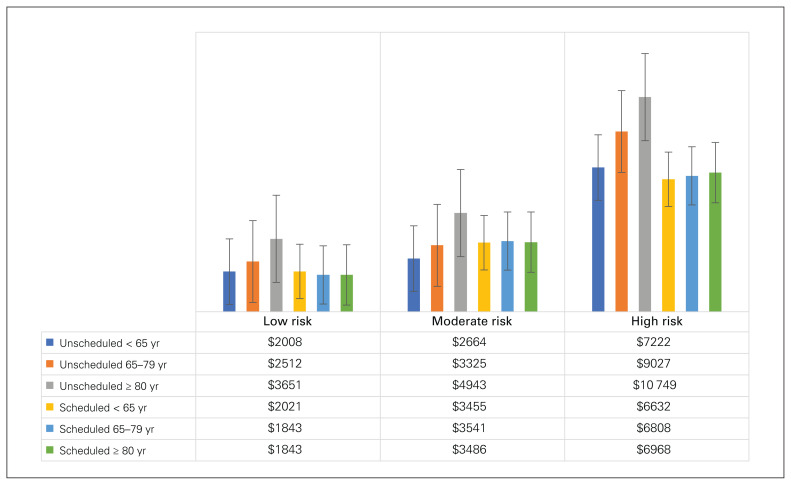
There was less than a 10% difference in cost between patients aged younger than 65 years, patients aged 65–79 years and patients aged 80 years and older for scheduled cases for all 3 surgical risk categories. Overall costs were lower for scheduled low-risk procedures for patients aged 65–79 years (−8.8%, p < 0.001) and patients aged 80 years and older (−8.8%, p < 0.001). Overall costs did not differ for moderate- or high-risk procedures. However, for unscheduled cases, there was a significant increase in cost for patients aged 65–79 years (low risk [48.1%, p < 0.001], moderate risk [36.8%, p = 0.045] and high risk [22.6%, p = 0.04]) and patients aged 80 years and older (low risk [115.3%, p < 0.001], moderate risk [103.3%, p < 0.001] and high risk [46.0%, p < 0.001]) when compared with patients aged younger than 65 years. The total admission costs more than doubled for patients aged 80 years and older undergoing unscheduled low- and moderate-risk surgical procedures (Table 3 and Figure 1) compared with patients aged younger than 65 years.
Table 3.
Percent difference between age groups for total inpatient cost by risk category, urgency and age
| Risk category | Age, yr | No. (% change) | ||
|---|---|---|---|---|
| Overall | Scheduled | Unscheduled | ||
| Low | ≤64 | 1574 (Ref.) | 1258 (Ref.) | 316 (Ref.) |
| 65 to 79 | 678 (−2.9) | 621 (−8.8) | 57 (48.1)* | |
| ≥80 | 244 (8.6) | 206 (−8.8) | 38 (115.3)* | |
| Moderate | ≤64 | 3497 (Ref.) | 760 (Ref.) | 2737 (Ref.) |
| 65 to 79 | 757 (29.7)* | 414 (2.5) | 343 (36.8)* | |
| ≥80 | 132 (63.0)* | 55 (1.5) | 76 (103.3)* | |
| High | ≤64 | 1096 (Ref.) | 600 (Ref.) | 496 (Ref.) |
| 65 to 79 | 679 (9.7) | 424 (2.6) | 255 (22.6) | |
| ≥80 | 186 (25.8)* | 98 (5.1) | 88 (46.0)* | |
Ref. = reference group.
Clinically significant differences.
Fig. 1.
Admission cost ($CAD) by age and surgical risk profile for planned and unplanned general surgical patients. Error bars represent standard error of the mean cost per procedure (n = 16 in the low-risk group, n = 31 in the moderate-risk group and n = 21 in the high-risk group).
When the total admission costs were examined by cost category stratified by age and urgency, there was no significant change between age groups in overall cost for elective procedures (< 65 yr: $3494; 65–79 yr: $3768 [8% increase, p = 0.001]; ≥ 80 yr: $3422 [2% decrease, p = 0.64]); however, overall cost increased with age for unscheduled procedures (< 65 yr: $3306; 65–79 yr: $5473 [66% increase, p < 0.001]; ≥ 80 yr: $7091 [114% increase, p < 0.001]). We examined the preoperative, operative and postoperative costs to determine where the increased costs were accrued. The cost increase in unscheduled admissions were owing to increased postoperative costs in all age groups, particularly the older cohorts. The postoperative care cost for unscheduled admissions was $2 higher than the postoperative care costs for scheduled admissions in patients aged younger than 65 years. The difference increased to $1480 in patients aged 65–79 years and $3143 in patients aged 80 years and older. Case costs were lower for unscheduled cases in patients aged younger than 65 years (Table 4). Operating room supplies and salaries were lower for nearly all risk categories and age groups for unscheduled surgery compared with scheduled surgery, whereas the cost of pre- and postoperative care tended to increase with surgical risk and age for unscheduled surgery more than for elective surgery (Table 5). Postoperative admission costs were the most substantial source of increased cost of unscheduled surgical admission in older age groups.
Table 4.
Cost of surgical admission by age group, urgency and cost category compared with patients aged 65 years and younger
| Age, yr | Surgical admission | No. | OR supplies | OR salaries | Preoperative inpatient | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||
| Cost ± SD, $ | Variance* | % change, (p value) | Cost ± SD, $ | Variance* | % change, (p value) | Cost ± SD, $ | Variance* | % change, (p value) | |||
| < 65 | Scheduled | 2618 | 873 ± 624 | 389 083 | Ref. | 963 ± 389 | 151 547 | Ref. | 38 ± 241 | 58 046 | Ref. |
|
|
|
|
|||||||||
| Unscheduled | 3549 | 585 ± 605 | 366 528 | 719 ± 364 | 132 512 | 381 ± 332 | 110 026 | ||||
|
|
|
|
|||||||||
| Difference in cost | −288 | −244 | 343 | ||||||||
|
| |||||||||||
| 65–79 | Scheduled | 1459 | 904 ± 671 | 450 793 | 4 (0.15) | 918 ± 397 | 157 411 | −5 (< 0.001) | 36 ± 82 | 6720 | −7 (0.62) |
|
| |||||||||||
| Unscheduled | 655 | 599 ± 667 | 444 777 | 2 (0.62) | 813 ± 351 | 123 140 | 13 (< 0.001) | 672 ± 1814 | 3 290 641 | −76 (< 0.001) | |
|
| |||||||||||
| Difference in cost | −305 | −105 | 636 | ||||||||
|
| |||||||||||
| ≥ 80 | Scheduled | 381 | 687 ± 562 | 316 003 | −21 (< 0.001) | 796 ± 391 | 153 005 | −17 (< 0.001) | 52 ± 659 | 434 400 | 36 (0.69) |
|
| |||||||||||
| Unscheduled | 208 | 576 ± 510 | 260 362 | −2 (0.80) | 835 ± 236 | 55 532 | 16 (< 0.001) | 651 ± 236 | 55 532 | 71 (< 0.001) | |
|
| |||||||||||
| Difference in cost | −112 | 39 | 599 | ||||||||
|
|
|
||||||||||
| Age, yr | Surgical admission | No. | Postoperative inpatient | Total | |||||||
|
|
|
||||||||||
| Cost ± SD, $ | Variance* | % change, (p value) | Cost ± SD, $ | Variance* | % change, (p value) | ||||||
|
| |||||||||||
| < 65 | Scheduled | 2618 | 1620 ± 1576 | 2 482 800 | Ref. | 3494 ± 2311 | 5 339 237 | Ref. | |||
|
|
|
||||||||||
| Unscheduled | 3549 | 1621 ± 1835 | 3 365 566 | 3306 ± 2576 | 6 633 869 | ||||||
|
|
|
||||||||||
| Difference in cost | 2 | −187 | |||||||||
|
| |||||||||||
| 65–79 | Scheduled | 1459 | 1911 ± 1943 | 3 776 217 | 18 (< 0.001) | 3768 ± 2571 | 6 607 502 | 8 (0.001) | |||
|
|
|||||||||||
| Unscheduled | 655 | 3390 ± 2479 | 6 146 686 | 109 (< 0.001) | 5473 ± 3925 | 15 407 258 | 66 (< 0.001) | ||||
|
|
|||||||||||
| Difference in cost | 1480 | 1705 | |||||||||
|
| |||||||||||
| ≥ 80 | Scheduled | 381 | 1886 ± 2265 | 5 127 993 | 16 (0.03) | 3422 ± 2915 | 8 497 783 | −2 (0.64) | |||
|
|
|||||||||||
| Unscheduled | 208 | 5029 ± 236 | 55 532 | 210 (< 0.001) | 7091 ± 555 | 307 654 | 114 (< 0.001) | ||||
|
|
|||||||||||
| Difference in cost | 3143 | 3669 | |||||||||
OR = operating room; Ref. = reference group; SD = standard deviation.
Variance of mean cost per procedure by surgical intervention and hospital.
Table 5.
Subcategories of surgical admission cost by age group and urgency compared with patients aged younger than 65 years divided by surgical risk
| Risk category | Age, yr | Surgical admission | No. | OR supplies | OR salaries | Preoperative inpatient | Postoperative inpatient | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||
| Cost, $ | % change, (p value) | Cost, $ | % change, (p value) | Cost, $ | % change, (p value) | Cost, $ | % change, (p value) | ||||
| Low | < 65 | Scheduled | 1258 | 524 | Ref. | 864 | Ref. | 24 | Ref. | 609 | Ref. |
|
|
|
|
|
||||||||
| Unscheduled | 316 | 368 | 607 | 270 | 764 | ||||||
|
|
|
|
|
||||||||
| Increased cost of unscheduled | −156 | −257 | 246 | 154 | |||||||
|
| |||||||||||
| 65–79 | Scheduled | 621 | 463 | −12 (< 0.001) | 747 | −13 (< 0.001) | 23 | −2 (0.85) | 610 | 0 (0.96) | |
|
| |||||||||||
| Unscheduled | 57 | 274 | −26 (0.002) | 579 | −5 (0.22) | 261 | −3 (0.74) | 1398 | 83 (< 0.001) | ||
|
| |||||||||||
| Increased cost of unscheduled | −189 | −168 | 238 | 788 | |||||||
|
| |||||||||||
| ≥ 80 | Scheduled | 206 | 345 | −34 (< 0.001) | 650 | −25 (< 0.001) | 17 | −26 (0.03) | 830 | 36 (< 0.001) | |
|
| |||||||||||
| Unscheduled | 38 | 274 | −26 (0.008) | 684 | 13 (0.01) | 318 | 18 (0.48) | 2375 | 211 (< 0.001) | ||
|
| |||||||||||
| Increased cost of unscheduled | −70 | 33 | 301 | 1545 | |||||||
|
| |||||||||||
| Moderate | < 65 | Scheduled | 760 | 927 | Ref. | 786 | Ref. | 29 | Ref. | 1714 | Ref. |
|
|
|
|
|
||||||||
| Unscheduled | 2737 | 565 | 650 | 341 | 1108 | ||||||
|
|
|
|
|
||||||||
| Increased cost of unscheduled | −362 | −135 | 312 | −606 | |||||||
|
| |||||||||||
| 65–79 | Scheduled | 414 | 955 | 3 (0.46) | 733 | −7 (< 0.001) | 42 | 48 (0.002) | 1811 | 6 (0.25) | |
|
| |||||||||||
| Unscheduled | 343 | 503 | −11 (0.08) | 726 | 12 (< 0.001) | 572 | 68 (0.10) | 1524 | 38 (< 0.001) | ||
|
| |||||||||||
| Increased cost of unscheduled | −453 | −7 | 529 | −287 | |||||||
|
| |||||||||||
| ≥ 80 | Scheduled | 56 | 713 | −23 (0.002) | 747 | −5 (0.48) | 186 | 552 (0.25) | 1840 | 7 (0.61) | |
|
| |||||||||||
| Unscheduled | 76 | 531 | −6 (0.51) | 827 | 27 (< 0.001) | 531 | 56 (0.002) | 3053 | 175 (< 0.001) | ||
|
| |||||||||||
| Increased cost of unscheduled | −181 | 80 | 345 | 1213 | |||||||
|
| |||||||||||
| High | < 65 | Scheduled | 600 | 1534 | Ref. | 1397 | Ref. | 82 | Ref. | 3619 | Ref. |
|
|
|
|
|
||||||||
| Unscheduled | 496 | 960 | 1099 | 672 | 4491 | ||||||
|
|
|
|
|
||||||||
| Increased cost of unscheduled | −574 | −298 | 589 | 872 | |||||||
|
| |||||||||||
| 65–79 | Scheduled | 424 | 1499 | −2 (0.34) | 1348 | −4 (0.02) | 48 | −41 (0.05) | 3913 | 8 (< 0.001) | |
|
| |||||||||||
| Unscheduled | 255 | 800 | −17 (0.004) | 981 | −11 (< 0.001) | 899 | 34 (< 0.001) | 6346 | 41 (< 0.001) | ||
|
| |||||||||||
| Increased cost of unscheduled | −699 | −366 | 851 | 2433 | |||||||
|
| |||||||||||
| ≥ 80 | Scheduled | 98 | 1325 | −14 (0.002) | 1174 | −16 (< 0.001) | 60 | −27 (0.27) | 4409 | 22 (< 0.001) | |
| Unscheduled | 88 | 713 | −26 (< 0.001) | 921 | −16 (< 0.001) | 955 | 42 (< 0.001) | 8160 | 82 (< 0.001) | ||
| Increased cost of unscheduled | −612 | −253 | 895 | 3751 | |||||||
OR = operating room; Ref. = reference group.
Discussion
Currently, 11.4% of Alberta residents and 15.7% of Canadians are aged 65 years and older.15 This proportion is projected to grow to 24% of Canadians by 2036.16 The cost of health care in Canada has been increasing faster than the national inflation rate for decades. It represented 10.9% of the Canadian gross domestic product, or $219.1 billion, in 2015.17 We hypothesized that increasing age would predict increasing operative case costs, mostly owing to prolonged length of hospital stay. Admission costs were increased only for unscheduled procedures. This finding persisted when surgical interventions were divided into surgical risk groups. The increased admission cost was predominantly owing to higher postoperative care costs in patients aged 65–79 years and patients aged 80 years and older. Many factors may contribute to increased costs in older age groups. First, elective surgery may allow for ideal patient selection and preoperative optimization. Second, older adults are often more severely ill than younger patients when they present for emergency surgery, resulting in more complicated postoperative courses in emergency surgery. Finally, older patients have longer stays in hospital owing to more complicated disposition planning and delays in transfer after unexpected hospital admissions. Emergency surgery appears to have affected older adults more than younger people, resulting in higher postoperative costs.
Nonemergent conditions afford the luxury of deciding if and when surgical intervention is appropriate. This could include time for preconditioning, preoperative medical optimization and a thorough risk assessment. It also provides the patient and surgeon an opportunity to assess if the risk of surgical intervention is warranted and decide to forgo surgery if the risk outweighs the benefits. This selects patients who are good candidates for surgery and are more likely to tolerate the surgery and postoperative recovery. This could reduce costs by decreasing post-operative length of hospital stay and morbidity. Older patients are more likely to require complex and time-consuming disposition planning. This could be because of diminished physiological reserve and the need for a higher level of care after a surgical illness. Conversely, emergency surgery precludes much preconditioning and optimization, and more high-risk interventions may be performed emergently as the health risks from the patients’ conditions outweigh the risks of surgery.
Older adults who present for emergency surgery are more likely than younger patients to have diminished physiological reserve, which could lead to higher rates of postoperative complications, admission to the intensive care unit and prolonged stays in hospital. Higher risk pre-operative status would be exacerbated by the surgeon’s inability to medically optimize the patient beforehand. Longer recovery times and greater use of intensive care would lead to increased costs.
Interestingly, the costs of care increased owing to higher postoperative care costs and to a lesser extent, preoperative care for unscheduled surgery, but costs associated with surgery supplies and salaries were actually lower in older populations. The difference is likely owing to longer postoperative admissions for unscheduled surgery. In addition, more investigations before surgery and longer waits for access to the OR for unscheduled procedures lead to increased cost before surgery. Lower costs in the OR may be owing to several factors, including less complex operations that do not involve reconstruction, a greater focus on control of contamination and patient stabilization. Interventions focused on postoperative care and optimization for older adults undergoing unscheduled surgery may be able to reduce these costs.
Our data did not allow us to examine the reasons for higher costs for unscheduled surgery in older adults; however, a Cochrane review by Eamer and colleagues18 found that comprehensive geriatric assessment (CGA) may decrease the risk of death and length of hospital stay, improve functional status at discharge and decrease overall cost. In addition, a systematic review of economic studies of CGA by Eamer and colleagues19 found that a CGA reduced cost and improved clinical outcomes, and a prospective trial found lower costs for emergent surgery in older adults when CGA was performed.13
Limitations
This study was limited by several factors. The data were retrospective and available only as aggregate population-level data. Controlling for patient-specific factors was not possible. Specifically, the lack of frailty data, sepsis or other risk assessment tools limits the importance of our findings. Frailty is well recognized to be a better marker than age for surgical risk; however, there is a correlation between age and frailty, and we deemed it was reasonable to separate our data based on broad age groups.
We calculated variance of means rather than variance of the population, as we did not have access to these data. As such, our calculated variance was likely less than the population variance. However, we feel that given the large sample size — we captured a substantial portion of the population (84% of all procedures performed in the region) — our measured means should be close to the population mean, reducing the error that this method of analysis could introduce. Our administrative database did not distinguish between emergency surgery (e.g., unstable trauma) and urgent non-life-threatening surgical indications (e.g., cholecystitis); therefore, 2 separate populations with differing risks may have been pooled into our unscheduled surgery group. Like most data on health care costs, our data were likely not normally distributed; however, we were unable to test this owing to our data being provided already pooled by intervention, age and location. Subdividing cases into low-, moderate- and high-risk procedures was not perfect as there likely would have been complex procedures incorrectly classified (e.g., a ventral hernia with component separation would still be moderate risk in this data set). However, we used a large data set in which few cases were unusual. As such, we consider our classification to have been reasonable.
Conclusion
Surgical intervention in older adults results in higher costs of care only for unscheduled cases. This finding may be explained by several factors, including patient selection, more complicated postoperative courses owing to the complexity and severity of illness in older patients, and unaccounted factors such as longer length of hospital stay owing to discharge planning in older patients. We do not have the necessary data to conclude which factors led to the increased costs. Innovative approaches to patient care should undergo further study in adults undergoing emergency surgery to mitigate the rising cost of care for older adults. We are unable to draw specific conclusions about the reason for increased costs; therefore, further studies are required.
Acknowledgement
The authors thank AnalysisWorks Inc. for their enthusiasm and assistance with acquiring the data and analytical consultant Ashley Singh in particular, for providing the anonymized data.
Footnotes
Competing interests: Gilgamesh Eamer received travel stipends from the Children’s Hospital of Eastern Ontario and was a board member with the Canadian Network for International Surgery. Ronald Brisebois received payment for medicolegal work with various law firms unrelated to the contents or conclusions of this paper. He was also a surgeon champion for NSQIP and ACS and is also a Pfizer stock holder. No other competing interests were declared.
Contributors: All authors designed the study. G. Eamer and R. Brisebois acquired the data, which G. Eamer, F. Clement and R. Khadaroo analyzed. G. Eamer wrote the article, which R. Brisebois and F. Clement reviewed. All authors approved the final version to be published.
This article was presented at the 2017 Canadian Frailty Network Annual Conference, Toronto, Ont., April 23–24, 2017
Funding: Funding was provided by Alberta Innovates and Alberta Health Services by holding a Partnership for Research and Innovation in the Health System research grant. Funding was also provided by the Canadian Frailty Network Interdisciplinary Fellowship (IFP2016-01) (Gilgamesh Eamer), who did not play a role in study design, implementation or analysis.
References
- 1.Mullen MG, Michaels AD, Mehaffey JH, et al. Risk associated with complications and mortality after urgent surgery vs elective and emergency surgery. JAMA Surg 2017;152:768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vonlanthen R, Slankamenac K, Breitenstein S, et al. the impact of complications on costs of major surgical procedures. Ann Surg 2011;254:907–13. [DOI] [PubMed] [Google Scholar]
- 3.Boltz MM, Hollenbeak CS, Julian KG, et al. Hospital costs associated with surgical site infections in general and vascular surgery patients. Surgery 2011;150:934–42. [DOI] [PubMed] [Google Scholar]
- 4.Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 2010;210:901–8. [DOI] [PubMed] [Google Scholar]
- 5.Hamel MB, Henderson WG, Khuri SF, et al. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc 2005;53:424–9. [DOI] [PubMed] [Google Scholar]
- 6.Haider AH, Obirieze A, Velopulos CG, et al. Incremental cost of emergency versus elective surgery. Ann Surg 2015;262:260–6. [DOI] [PubMed] [Google Scholar]
- 7.Preston SD, Southall ARD, Nel M, et al. Geriatric surgery is about disease, not age. J R Soc Med 2008;101:409–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neuman MD, Bosk CL. The redefinition of aging in American surgery. Milbank Q 2013;91:288–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alemayehu B, Warner KE. The lifetime distribution of health care costs. Health Serv Res 2004;39:627–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National health expenditure trends, 1975 to 2016. Ottawa: Canadian Institute for Health Information; 2016. Available: https://secure.cihi.ca/free_products/NHEX-Trends-Narrative-Report_2016_EN.pdf (accessed 2017 Feb. 15). [Google Scholar]
- 11.Wiktorowicz ME, Goeree R, Papaioannou A, et al. Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporos Int 2001;12:271–8. [DOI] [PubMed] [Google Scholar]
- 12.Muñoz E, Friedman R, Schroder W, et al. Age, resource consumption, and outcome for surgical patients at an academic medical center. Surgery 1988;103:335–43. [PubMed] [Google Scholar]
- 13.Hofmeister M, Khadaroo RG, Holroyd-Leduc J, et al. Cost-effectiveness analysis of the Elder-Friendly Approaches to the Surgical Environment (EASE) intervention for emergency abdominal surgical care of adults aged 65 years and older. JAMA Netw Open 2020;3:e202034–202034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Faul F, Erdfelder E, Lang A-G, et al. *Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007;39:175–91. [DOI] [PubMed] [Google Scholar]
- 15.Population estimates on July 1st, by age and sex. Table 17-10-0005-01 (formerly CANSIM 051-0001). Ottawa: Statistics Canada. Available: http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/demo31d-eng.htm (accessed 2015 Jul. 28). [Google Scholar]
- 16.Projected population, by projection scenario, age and sex, as of July 1 (x 1,000). Table 17-10-0057-01 (formerly CANSIM 052-0005) and Cat. no.: 91-520-X. Ottawa: Statistics Canada; 2014. Available: http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/demo23g-eng.htm (accessed 2015 Jul. 28). [Google Scholar]
- 17.National Health Expenditure Trends, 1975 to 2015. Ottawa: Canadian Institute for Health Information; 2015. Available: https://www.hhr-rhs.ca/images/stories/CIHI_National_Health_Expenditure_Trends_2015.pdf (accessed 2016 Sept. 2). [Google Scholar]
- 18.Eamer G, Taheri A, Chen SS, et al. Comprehensive geriatric assessment for older people admitted to a surgical service. Cochrane Database Syst Rev 2018;1:CD012485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eamer G, Saravana-Bawan B, van der Westuizen B, et al. Economic evaluations of comprehensive geriatric assessment in surgical patients: a systematic review. J Surg Res 2017;218:9–17. [DOI] [PubMed] [Google Scholar]