Abstract
Tuberculous spondylitis is a common spinal infection. If surgical intervention is necessary, anterior debridement and anterior fixation are typically performed. However, a minimally invasive surgical strategy under local anesthesia seems rarely implemented.
A 68-year-old man presented with severe pain in the left flank. Whole spinal magnetic resonance imaging revealed abnormal intensity of vertebral bodies from T6–9. A bilateral paravertebral abscess extending from T4–10 was suspected. The T7/T8 intervertebral disc was destroyed, but severe vertebral deformity or spinal cord compression was not observed. Bilateral percutaneous transpedicular drainage under local anesthesia was planned. The patient was set in the prone position. Under the guide of a biplanar angiographic system, the bilateral drainage tubes were placed paravertebrally in the abscess cavity. The left flank pain improved after the procedure. Laboratory culture of the pus specimen confirmed a diagnosis of tuberculosis. A chemotherapy regimen for tuberculosis was soon initiated. The patient was discharged during postoperative week 2, with continuation of chemotherapy for tuberculosis.
Percutaneous transpedicular drainage under local anesthesia can be effective in the management of thoracic tuberculous spondylitis without severe vertebral deformity or compression of the spinal cord by an abscess.
Keywords: tuberculosis spondylitis, minimum invasive surgery, transpedicular drainage, thoracic spine
Key Messages
Thoracic tuberculous spondylitis can be detected with severe deformity of the multiple vertebral bodies and paravertebral/perispinal abscess.
In our case, the vertebral bodies of T7 and T8 were partially invaded by the paravertebral abscess; however, severe vertebral deformity was not recognized.
Percutaneous transpedicular drainage of the paravertebral abscess under local anesthesia was effective in our case.
To place the drainage tubes directly in the paravertebral space, we modified the transpedicular puncture direction bilaterally, utilizing a biplane angiographic system.
Introduction
Tuberculous spondylitis is a subtype of granulomatous spondylitis and is a common cause of spinal infection. 1 2 Approximately 25 to 60% of skeletal infections result from tuberculosis, half of which is located in the spine, mainly in the thoracic vertebrae. 2 3 4 5 6 Tuberculous spondylitis is typically located in the anterior cancellous bone. The inflammation spreads vertically to the end plates of the adjacent vertebral bodies. The intervertebral body may even be destroyed, paravertebral, paraspinal, or intraspinal abscesses may appear. 2 7 8 9 These manifestations may result in severe kyphotic deformity of the spine and/or paraplegia. 8 10 11 Chemotherapy is essential for the treatment of thoracic tuberculous spondylitis. Physiotherapy and immobilization have been proposed as conservative management, 2 while surgical management is indicated in cases where there is severe pain, abscess formation, refractory infection, local kyphosis, segmental instability, and neurological paralysis. 2 8 9 12 13 14 Intervention consisting of debridement with either anterior or posterior fixation is widely used as the surgical strategy of choice for thoracic tuberculous spondylitis. 15 16 17 18 19 20 Minimally invasive surgery for thoracic tuberculous spondylitis has also been reported 21 22 23 ; however, to the best of our knowledge, percutaneous transpedicular drainage of a paravertebral abscess under local anesthesia has not been described in detail.
Here, we present a case of thoracic tuberculous spondylitis successfully managed by bilateral percutaneous transpedicular drainage of the paravertebral abscess under local anesthesia. We mainly focus on the effectiveness of bilateral percutaneous transpedicular drainage under local anesthesia as a minimally invasive surgery for tuberculosis spondylitis.
Case Report
A 68-year-old man presented to our department of neurosurgery. He had a past medical history of stomach cancer and diabetes mellitus. The patient had not had any episodes of tuberculosis but did have a family history of the disease, with his father having a history of the disease. He had begun to suffer from pain in the region of the inferior margin of the left scapula 3 years earlier when carrying heavy objects on his back. The area of pain had extended to the left flank 12 months before his presentation to our department, and the pain had continued to worsen in severity even at rest, causing severe distress over the last month. Neurological examination did not reveal any symptoms apart from pain. Osteolysis and osteosclerosis of T7–8 were revealed on radiography and computed tomography (CT). Osteolysis was confirmed in the right inferior part of the vertebral body of T7, whereas in the left superior part of the vertebral body of T8 ( Fig. 1A,B ). However, severe thoracic vertebral deformity was not observed. The patient was hospitalized on the same day for further examination. Blood tests revealed an inflammatory response: white blood cell count, 8.9 × 10 3 /µL; platelet count, 30.3 × 10 4 /µL; erythrocyte sedimentation rate, 48.0 mm/h; C-reactive protein, 1.43 mg/mL; and β-d-glucan, less than 2.2 pg/mL. In the following day, whole spine magnetic resonance imaging (MRI) showed a lesion located mainly from T7 to T8. The T7/T8 intervertebral disc was destroyed. The vertebral bodies from T6–9 also showed signal changes. A bilateral paravertebral lesion from T4 to T10 was observed ( Fig. 1C – E ). The spinal cord was not compressed by the paravertebral lesion. The left nerve root of T7 was not clearly observed ( Fig. 2 ). No lesions were detected in the cervical or lumbar vertebrae. As we suspected the existence of a paravertebral abscess, the patient was started on 3 mg/day cefmetazole; however, his left flank pain did not subside. We deduced that the pain could be as a result of left T7 nerve root compression caused by the possible abscess. To obtain a culture specimen and to release the compression by the possible abscess, we planned bilateral percutaneous transpedicular drainage under local anesthesia in an angiography room on admission day 3.
Fig. 1.
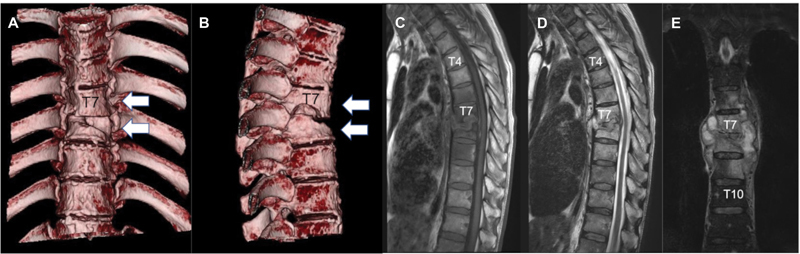
Preoperative radiological images ( A . B ) three-dimensional reconstructed computed tomography images. ( C – E ) magnetic resonance images. ( C ): T1-weighted image, ( D ); T2-weighted image and ( E ) short-T1 inversion recovery (STIR) image). Three-dimensional reconstructed computed tomography images showing osteolysis of the T7 and T8 vertebral bodies ( white arrows ) ( A : anteroposterior projection and B , lateral projection). The paravertebral lesion showing hypointensity on T1-weighted image, hyperintensity on T2-weighted image, and hyperintensity on STIR image inversion recovery. The vertebral bodies from T6 to T9 demonstrate hypointensity on T1-weighted images and hyperintensity on T2-weighted images. The intervertebral disc between T7 and T8 is destroyed. The spinal cord is intact ( C – E ).
Fig. 2.
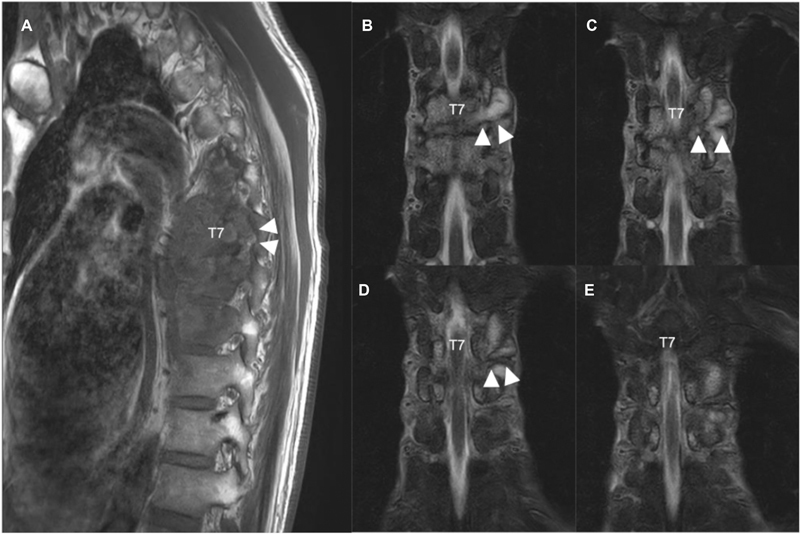
Preoperative magnetic resonance images ( A : A sagittal image of T1-weighted image, B–D and E : coronal images of short-T1 inversion recovery images). ( A ) The foramen and left T7 nerve root are obscure (white arrowheads). ( B–D , and E ) The left T7 nerve root is not clearly seen due to the paravertebral lesion.
Operation
The patient was placed in the prone position. We used a biplanar angiographic system (Artis zee biplane, Siemens Healthineers, Japan). Before skin puncture, we confirmed the vertebral bodies of T7 and T8. As the suspected paravertebral abscess invaded the right inferior part of the T7 vertebral body and the left superior part of the T8 vertebral body, we aimed to place drainage tubes through the right and left pedicles of T7 and T8, respectively. We approached the suspected paravertebral abscess from the left-side injecting local anesthesia into the subcutaneous tissue and peduncular periosteum of T8. A neurosurgeon held an 8G bone marrow biopsy needle in the center of the left pedicle of T8 while referring to an anteroposterior projection perspective image. He then hit the needle with a hammer, aiming it in the direction of the left pedicle of T8. To avoid damage to the nerve root, the needle was inserted relatively to the upper-lateral part of the pedicle. The inner sheath of the needle was then extracted once the surgeon had confirmed that the needle had reached the affected vertebral body space on the lateral projection perspective image. Pus from the abscess was aspirated using a syringe attached to the outer sheath of the needle. The collected pus was submitted for laboratory culture. A guide wire from a JINRO Nephrostomy Catheter Kit 10.3 Fr (Boston Scientific, Japan) was then introduced to the abscess cavity through the remaining outer sheath of the needle. The outer sheath of the needle was removed, and pus drained spontaneously from the site. Finally, the JINRO catheter was placed in the abscess cavity through the guide wire ( Fig. 3A – D ). The same procedure was then followed to place a catheter on the right side of the spine at the level of T7. As the T7 vertebral body was inferiorly affected by the abscess, the puncture was directed from the cranial margin of the pedicle to the inferior margin of the vertebral body ( Fig. 3E – H ). After confirming that both the drainage tubes were placed in the paravertebral abscess space, we stitched the drainage tubes to the skin. The operation time was 32 minutes, and total radiation dose was 198 mGy.
Fig. 3.
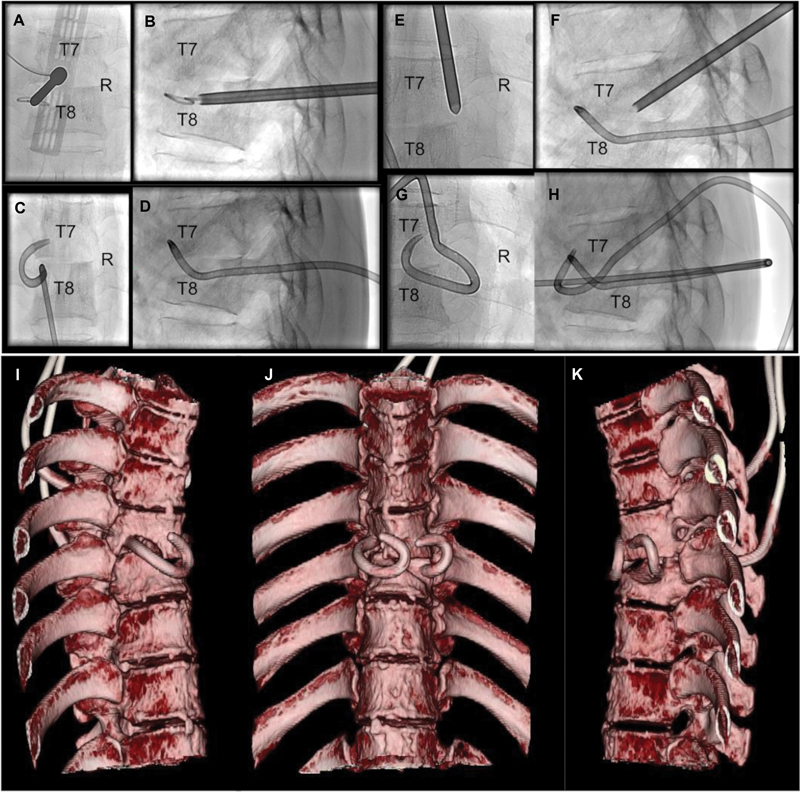
Intraoperative radiological images ( A–D : left transpedicular drainage, E–H : right transpedicular drainage). ( A ) An 8G bone marrow biopsy needle is set in the center of the left pedicle of T8. ( B ) A catheter is transpedicularly introduced through a guidewire. ( C, D ) A catheter is placed in the left paravertebral abscess cavity ( C , anterior posterior projection and D , lateral projection). ( E ): An 8G bone marrow biopsy needle is set in the cranial margin of the right pedicle of T7. ( F ) An 8G bone marrow biopsy needle was introduced in the direction of the inferior margin of the T7 vertebral body. ( G, H ) A catheter is placed in the right paravertebral abscess cavity ( G : anterior posterior projection, H : lateral projection). Postoperative three-dimensional reconstructed computed tomography images demonstrating the placement of bilateral drainage catheters in the paravertebral abscess cavity ( I–K ).
Postoperative Course
The left flank pain subsided soon after the transpedicular drainage was performed. The specimen collected confirmed tuberculosis by polymerase chain reaction. Antituberculosis chemotherapy consisting of daily doses of isonicotinic acid hydrazide (300 mg), rifampicin (450 mg), ethambutol (875 mg), and pyrazinamide (1,500 mg) was transorally initiated. The drainage tubes were removed on postoperative day 14 after we confirmed that active continuous excretion of the abscess had ceased. Skin trouble did not occur. The patient was discharged from the hospital on day 19. Chemotherapy was continued for 2 months after which only isonicotinic acid hydrazide and rifampicin were continued at their initial doses for 7 months. The patient was followed-up in the outpatient clinic, and the abscess showed gradual shrinkage on MRI. Postoperative kyphotic change was not apparently observed ( Fig. 4 ).
Fig. 4.
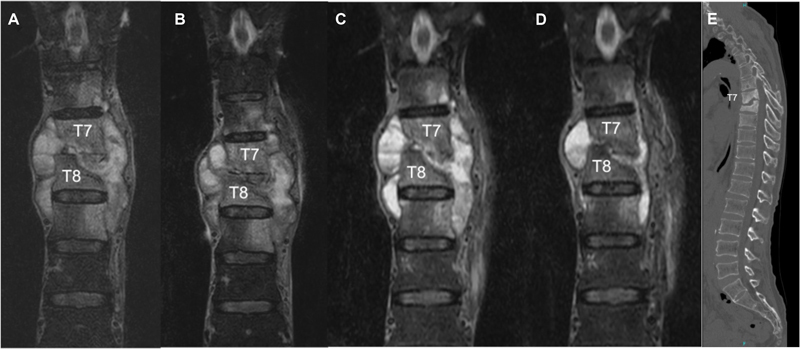
Postoperative images. Short-T1 inversion recovery (STIR) images showing gradual shrinkage of the paravertebral abscess ( A : preoperative image, B : postoperative week 3, C : postoperative month 3, and D : postoperative month 5). Kyphotic change was not observed on computed tomography image ( E : postoperative month 5).
Discussion
We report a case of thoracic tuberculous spondylitis treated with bilateral percutaneous transpedicular drainage under local anesthesia.
Tuberculous spondylitis progresses insidiously over a relatively long period 2 and can cause severe vertebral deformity or paraplegia as a result of spinal cord compression from abscess formation or deformed vertebral bodies. To resolve the sequelae related to thoracic tuberculous spondylitis, surgical treatment using an anterior approach for debridement of the abscess and interbody fusion has been typically described. 17 24 However, this approach does not seem to be ideal in cases of multiple lesions or severe kyphotic deformity. A combined anteroposterior approach has also been proposed, but this approach has been associated with a high rate of morbidity and mortality. 25 26 27 28 The posterior approach for debridement and instrument fixation is still applied in the management of thoracic or lumbar tuberculous spondylitis. 15 18 20 29 30 31 Our patient started to complain of pain near the left scapula 3 years before he presented at our hospital. Severe vertebral deformity or spinal cord compression fortunately did not occur in his case. Thus, no fixation was necessary.
Less-invasive surgical treatment using an anterior or posterior approach has been reported. 21 22 23 Transpedicular debridement for thoracic tuberculous spondylitis was described in two cases by Garg and Vohra. 23 They performed only transpedicular debridement in two cases of thoracic tuberculous spondylitis because more than two infected segments were preoperatively identified. They utilized a microscope and an endoscope for surgery, thus differing from our maneuver. Percutaneous drainage surgery under local anesthesia has previously been reported. 32 33 However, in previous studies, the drainage tube was inserted into the intervertebral space. In our case, the bilateral drainage tubes were placed in the paravertebral abscess space via the affected vertebral bodies of T7 and T8. The T7 vertebral body was inferiorly affected, and that of T8 was superiorly affected. To use the bone window of the T7 and T8 vertebral bodies, we modified the puncture direction of the percutaneous drainage, relatively caudally on the right T7 and relatively cranially on the left T8. The percutaneous tubes should be stably placed to drain the paravertebral abscess well; thus, the drainage route was favorable via the pedicle, not via the soft tissue. The placement of drainage tubes through intercostal spaces can be a risk factor for damage to organs such as the lungs or major blood vessels. In addition, erroneous placement of drainage tubes in the thoracic cavity can occur. Zhang et al introduced tubes for thoracic tuberculous abscesses above the transverse processes of the vertebrae. 33 Their maneuver can be also effective and minimally invasive, but drainage tube placement above the transverse process can be a risk factor for damage to the nerve roots. Therefore, we believe that transpedicular puncture is a relatively safe route to drain a paravertebral abscess. We did not use a mobile C-arm for drainage but opted to use a biplanar angiographic system to accurately and simultaneously confirm the placement direction of the drainage tubes on the biplanar panels. This system seems to be an important factor in performing transpedicular drainage safely and effectively. Besides, operation time was short enough and total radiation dose was not high in our case which seems to be advantageous in our surgical technique.
After drainage of the paravertebral abscess, the pain in the left flank was resolved. This is likely a result of the left T7 nerve root being released when the compression due to the paravertebral abscess was resolved. Continuous drainage of the paravertebral abscess can be also more effective, in case tuberculosis is multidrug resistant. The drainage tubes were removed 14 days after the surgery in our case, and skin complication did not occur. However, long-term tube placement may predispose to formation of a cold fistula. Therefore, surgeons should consider removal of the replaced tubes relatively in short-term if active drainage of the abscess ceases.
Conclusion
In a case of thoracic tuberculous spondylitis where there was osteolysis of the vertebral bodies but no severe vertebral deformity, our minimally invasive surgical technique proved successful. Percutaneous transpedicular drainage under local anesthesia for a paravertebral abscess may be a safe and effective minimally invasive treatment for thoracic tuberculous spondylitis.
Acknowledgment
We would like to thank Editage ( www.editage.com ) for English language editing. We thank also Dr. Ryota Ishibashi for his collaboration with this study.
Conflict of Interest None declared.
Authors' Contributions
Y.M. contributed in drafting the article. M.T. contributed in revising the article critically and final approval of the manuscript to be submitted. K.G. contributed in the conception and design of the study and acquisition of data.
References
- 1.Zhang N, Zeng X, He L. The value of MR imaging in comparative analysis of spinal infection in adults: pyogenic versus tuberculous. World Neurosurg. 2019;128:e806–e813. doi: 10.1016/j.wneu.2019.04.260. [DOI] [PubMed] [Google Scholar]
- 2.Lee K Y. Comparison of pyogenic spondylitis and tuberculous spondylitis. Asian Spine J. 2014;8(02):216–223. doi: 10.4184/asj.2014.8.2.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsiodras S, Falagas M E. Clinical assessment and medical treatment of spine infections. Clin Orthop Relat Res. 2006;444(444):38–50. doi: 10.1097/01.blo.0000203454.82264.cd. [DOI] [PubMed] [Google Scholar]
- 4.Wu W, Li Z, Wang S, Zhang H, Lin R, Lin J. One-stage surgical treatment for consecutive multisegment thoracic spinal tuberculosis with kyphosis by posterior-only debridement, interbody fusion, and instrumentation. World Neurosurg. 2019;128:e238–e244. doi: 10.1016/j.wneu.2019.04.122. [DOI] [PubMed] [Google Scholar]
- 5.Turgut M. Spinal tuberculosis (Pott's disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev. 2001;24(01):8–13. doi: 10.1007/pl00011973. [DOI] [PubMed] [Google Scholar]
- 6.Ansari S, Amanullah M F, Ahmad K, Rauniyar R K. Pott's spine: diagnostic imaging modalities and technology advancements. N Am J Med Sci. 2013;5(07):404–411. doi: 10.4103/1947-2714.115775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.An H S, Seldomridge J A. Spinal infections: diagnostic tests and imaging studies. Clin Orthop Relat Res. 2006;444(444):27–33. doi: 10.1097/01.blo.0000203452.36522.97. [DOI] [PubMed] [Google Scholar]
- 8.Zhang H, Zeng K, Yin X, Huang J, Tang M, Guo C. Debridement, internal fixation, and reconstruction using titanium mesh for the surgical treatment of thoracic and lumbar spinal tuberculosis via a posterior-only approach: a 4-year follow-up of 28 patients. J Orthop Surg Res. 2015;10:150. doi: 10.1186/s13018-015-0292-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rajasekaran S. Kyphotic deformity in spinal tuberculosis and its management. Int Orthop. 2012;36(02):359–365. doi: 10.1007/s00264-011-1469-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang H, Hou K, Zhang L. Minimally invasive surgery through the interlaminar approach in the treatment of spinal tuberculosis: a retrospective study of 31 patients. J Clin Neurosci. 2016;32:9–13. doi: 10.1016/j.jocn.2015.11.036. [DOI] [PubMed] [Google Scholar]
- 11.Jain A K, Kumar J. Tuberculosis of spine: neurological deficit. Eur Spine J. 2013;22 04:624–633. doi: 10.1007/s00586-012-2335-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaloostian P E, Gokaslan Z L.Current management of spinal tuberculosis: a multimodal approach World Neurosurg 201380(1,2):64–65. [DOI] [PubMed] [Google Scholar]
- 13.Pellisé F. Tuberculosis and Pott's disease, still very relevant health problems. Eur Spine J. 2013;22 04:527–528. doi: 10.1007/s00586-012-2531-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tuli S M. Historical aspects of Pott's disease (spinal tuberculosis) management. Eur Spine J. 2013;22 04:529–538. doi: 10.1007/s00586-012-2388-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhao C, Pu X, Zhou Q. Can a posterior approach effectively heal thoracic and lumbar tuberculosis? Microbiology outcomes of the operative area. J Orthop Surg Res. 2019;14(01):24. doi: 10.1186/s13018-019-1063-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang B, Lv G, Liu W, Cheng I. Anterior radical debridement and reconstruction using titanium mesh cage for the surgical treatment of thoracic and thoracolumbar spinal tuberculosis: minimium five-year follow-up. Turk Neurosurg. 2011;21(04):575–581. [PubMed] [Google Scholar]
- 17.Liu J, Wan L, Long X, Huang S, Dai M, Liu Z. Efficacy and safety of posterior versus combined posterior and anterior approach for the treatment of spinal tuberculosis: a meta-analysis. World Neurosurg. 2015;83(06):1157–1165. doi: 10.1016/j.wneu.2015.01.041. [DOI] [PubMed] [Google Scholar]
- 18.Güzey F K, Emel E, Bas N S. Thoracic and lumbar tuberculous spondylitis treated by posterior debridement, graft placement, and instrumentation: a retrospective analysis in 19 cases. J Neurosurg Spine. 2005;3(06):450–458. doi: 10.3171/spi.2005.3.6.0450. [DOI] [PubMed] [Google Scholar]
- 19.Chen W J, Wu C C, Jung C H, Chen L H, Niu C C, Lai P L. Combined anterior and posterior surgeries in the treatment of spinal tuberculous spondylitis. Clin Orthop Relat Res. 2002;(398):50–59. doi: 10.1097/00003086-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Zhang H, Sheng B, Tang M. One-stage surgical treatment for upper thoracic spinal tuberculosis by internal fixation, debridement, and combined interbody and posterior fusion via posterior-only approach. Eur Spine J. 2013;22(03):616–623. doi: 10.1007/s00586-012-2470-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gan F, Jiang J, Xie Z. Minimally invasive direct lateral interbody fusion in the treatment of the thoracic and lumbar spinal tuberculosisMini-DLIF for the thoracic and lumbar spinal tuberculosis. BMC Musculoskelet Disord. 2018;19(01):283. doi: 10.1186/s12891-018-2187-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lv G H, Wang B, Li J, Liu W D, Yin G H, Ma Z M. Thoracoscopy-assisted mini-open surgery for anterior column reconstruction in thoracic spinal tuberculosis. Orthop Surg. 2009;1(04):293–299. doi: 10.1111/j.1757-7861.2009.00043.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garg N, Vohra R. Minimally invasive surgical approaches in the management of tuberculosis of the thoracic and lumbar spine. Clin Orthop Relat Res. 2014;472(06):1855–1867. doi: 10.1007/s11999-014-3472-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benli I T, Acaroğlu E, Akalin S, Kiş M, Duman E, Un A. Anterior radical debridement and anterior instrumentation in tuberculosis spondylitis. Eur Spine J. 2003;12(02):224–234. doi: 10.1007/s00586-002-0403-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang Y P, Lin J H, Chen X P, Wu G, Chen X W. Preliminary experience in treating thoracic spinal tuberculosis via a posterior modified transfacet debridement, instrumentation, and interbody fusion. J Orthop Surg Res. 2018;13(01):292. doi: 10.1186/s13018-018-0994-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li M, Du J, Meng H, Wang Z, Luo Z. One-stage surgical management for thoracic tuberculosis by anterior debridement, decompression and autogenous rib grafts, and instrumentation. Spine J. 2011;11(08):726–733. doi: 10.1016/j.spinee.2011.06.009. [DOI] [PubMed] [Google Scholar]
- 27.Zhang H Q, Lin M Z, Shen K Y. Surgical management for multilevel noncontiguous thoracic spinal tuberculosis by single-stage posterior transforaminal thoracic debridement, limited decompression, interbody fusion, and posterior instrumentation (modified TTIF) Arch Orthop Trauma Surg. 2012;132(06):751–757. doi: 10.1007/s00402-012-1473-z. [DOI] [PubMed] [Google Scholar]
- 28.Zhang H Q, Guo C F, Xiao X G, Long W R, Deng Z S, Chen J. One-stage surgical management for multilevel tuberculous spondylitis of the upper thoracic region by anterior decompression, strut autografting, posterior instrumentation, and fusion. J Spinal Disord Tech. 2007;20(04):263–267. doi: 10.1097/01.bsd.0000211281.68400.1b. [DOI] [PubMed] [Google Scholar]
- 29.Zhang H Q, Li J S, Zhao S S. Surgical management for thoracic spinal tuberculosis in the elderly: posterior only versus combined posterior and anterior approaches. Arch Orthop Trauma Surg. 2012;132(12):1717–1723. doi: 10.1007/s00402-012-1618-0. [DOI] [PubMed] [Google Scholar]
- 30.Pu X, Zhou Q, He Q. A posterior versus anterior surgical approach in combination with debridement, interbody autografting and instrumentation for thoracic and lumbar tuberculosis. Int Orthop. 2012;36(02):307–313. doi: 10.1007/s00264-011-1329-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee S H, Sung J K, Park Y M. Single-stage transpedicular decompression and posterior instrumentation in treatment of thoracic and thoracolumbar spinal tuberculosis: a retrospective case series. J Spinal Disord Tech. 2006;19(08):595–602. doi: 10.1097/01.bsd.0000211241.06588.7b. [DOI] [PubMed] [Google Scholar]
- 32.Shibuya S, Komatsubara S, Yamamoto T, Arima N, Kanda Y, Oka S. Percutaneous discectomy-continuous irrigation and drainage for tuberculous lumbar spondylitis: a report of two cases. Case Rep Med. 2009;2009:632981. doi: 10.1155/2009/632981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang Z, Hao Y, Wang X. Minimally invasive surgery for paravertebral or psoas abscess with spinal tuberculosis - a long-term retrospective study of 106 cases. BMC Musculoskelet Disord. 2020;21(01):353. doi: 10.1186/s12891-020-03344-9. [DOI] [PMC free article] [PubMed] [Google Scholar]


