Abstract
This paper examines how fragmentation of critical infrastructure impacts the spread of the coronavirus outbreak in New York City at the neighbourhood level. The location of transportation hubs, grocery stores, pharmacies, hospitals and parks plays an important role in shaping spatial disparities in virus spread. Using supervised machine learning and spatial regression modelling we examine how the geography of COVID-19 case rates is influenced by the spatial arrangement of four critical sectors of the built environment during the public health emergency in New York City: health care facilities, mobility networks, food and nutrition and open space. Our models suggest that an analysis of urban health vulnerability is incomplete without the inclusion of critical infrastructure metrics in dense urban geographies. Our findings show that COVID-19 risk at the zip code level is influenced by (1) socio-demographic vulnerability, (2) epidemiological risk, and (3) availability and access to critical infrastructure.
Keywords: built environment, health, inequality, infrastructure, machine learning, social justice, spatial regression analysis
摘要
本文研究关键基础设施的碎片化对纽约市冠状病毒社区传播爆发的影响。交通枢纽、杂货店、药房、医院和公园的位置在决定病毒传播的空间差异方面起着重要作用。我们利用监督机器学习和空间回归模型,研究了在纽约市该突发公共卫生事件期间,新冠肺炎 (COVID-19) 发病率的地理分布如何受到建筑环境中四个关键要素的空间排列的影响,这四个要素即医疗保健设施、移动网络、食物和营养以及开放空间。我们的模型表明,如果不将密集城市地理中的关键基础设施指标包括在内,对城市健康漏洞的分析将是不完整的。我们的研究结果表明,邮政编码级别的新冠肺炎风险受 (1) 社会人口脆弱性、(2) 流行病学风险和 (3) 关键基础设施的可用性和可访问性的影响。
Introduction
The unravelling of the novel virus to pandemic proportions in recent months has drawn considerable global attention to cities, and the particularly urban nature of the public health crisis. New York experienced one of the worst outbreaks of COVID-19 in the US, and was among the hardest hit cities by the summer of 2020, globally. Particularly stark were the differential impacts of the outbreak on the city’s diverse neighbourhoods and populations. Health data shows that neighbourhoods with the highest number of cases per capita are also areas with the lowest median incomes and largest average household sizes (Schwirtz and Cook, 2020). The highest death rates in the city were witnessed in neighbourhoods with high concentrations of Black and LatinX populations, and low-income residents (Godoy and Wood, 2020). It is no longer just about who has been most affected by the virus, but also where people are most likely to be at risk, and why. We argue that understanding the impact of the pandemic on cities requires an analysis of the spatial dynamics of COVID-19 at the neighbourhood level, and urban infrastructure, in its material, social, political, economic and structural forms, is at the centre of such discussions (Enright and Ward, 2021; Powrie, 2020; Rutherford, 2020; World Economic Forum, 2020). This paper contributes to the growing literature on the urban geography of COVID-19 and presents an exploratory analysis of New York City’s (NYC) critical urban infrastructure and its relationship to urban health vulnerability.
The ‘infrastructural turn’ in the social sciences has revealed the importance of infrastructural questions for understanding contemporary social problems (Addie et al., 2020; Anand et al., 2018). According to anthropologist Brian Larkin (2013: 328), infrastructures are built networks that provide the ‘undergirding of modern societies, and generate the ambient environment of everyday life’. Paul Edwards (2003) suggests that infrastructures ‘co-construct’ society. They are learned by membership in a community, in the same way that knowledge of infrastructure is a prerequisite for membership. In New York, residents are fluent in the use of their everyday built environment, taking their regular subway route, navigating to their neighbourhood grocery stores and picking up prescriptions from the local pharmacy. Scholars in the field of techno-politics show that the work of infrastructure remains invisible until it fails (Callon, 1998; Latour, 2007; Mitchell, 2011). For Graham (2010), moments of disruption are heuristics for revealing the hidden politics of urban life and serve to problematise our normative understandings of a city’s stable flow. Public health crises have a history of exposing vulnerabilities in our material and social environments, requiring a rethinking of short-term disaster response as well as long-term urban planning (Acuto, 2020). COVID-19 has been a prism, and an amplifier of the histories of spatial segregation in NYC. The uneven geographies of public health response have revealed inequities in labour, information sharing, resource availability and emergency preparedness. Our findings show that space-based disparities in availability and access to critical infrastructures in New York have implications for increased rates of viral spread and morbidity among at-risk populations.
Many modern urban design systems from housing to sanitation, parks and drinking water were born from disease outbreaks (Gandy, 2006). An important property of epidemics is their ‘spatial spread’, which in dense urban centres, is influenced by factors such as the epidemic mechanism, human mobility and control strategies (Gross et al., 2020). The spread of cholera in London in 1854 was pivotal to developing the city’s sanitation standards. John Snow’s discovery of a contaminated water pump on Broad Street led to a revelation about the relationship between drinking water and disease that enabled cities all over Europe to control viral outbreaks by modernising sanitation systems (Johnson, 2007). Recent authorship in urban geography has argued that urban infrastructures are both a cause of global pandemics and play a role in its effects on urban populations (Connolly et al., 2020; Enright and Ward, 2021). Their absence predisposes populations to greater health risks, while their over presence, as high-trafficked sites of exposure, makes neighbourhoods more vulnerable. Lack of access to local medical care facilities placed an uneven burden of COVID-19 casualties on some neighbourhoods, while in others the density of transportation hubs increased risk of exposure.
Building on recent scholarship attempting to ‘un-black box’ COVID-19’s urban infrastructural condition, this paper examines four key sectors of the built environment that have been critical to the experience of COVID-19 in NYC at the zip code level – healthcare, mobility networks, food and nutrition, and open space – to conduct an exploratory analysis of the role that critical infrastructure plays in the spread and containment of contagious disease. We define ‘critical infrastructure’ (CI) as urban infrastructures that are critical to the mitigation, adaptation and governance of COVID-19 spread, and analyse patterns in the absence and over presence of hospitals, pharmacies, subway stations, width’s of sidewalks determining ability to social distance, food pantries, soup kitchens, grocery stores and parks at the neighbourhood level. For each variable, two spatial vectors are examined, density and distance. Clustering of social and epidemiological risk at the zip code level is determined using data from the Center for Disease Control (CDC). The Social Vulnerability Index (SVI) is used to examine socio-economic vulnerability (Centers for Disease Control, 2020) and RS21’s ‘Urban Health Vulnerability Index’ (UHVI) to spatialise the epidemiological risk of COVID-19 (R2S1, 2020). The spatial regression models presented here suggest that an analysis of urban health vulnerability is incomplete without the inclusion of CI metrics in dense geographies. We propose that COVID-19 risk in NYC is influenced by (1) socio-demographic vulnerability, (2) epidemiological risk, and (3) the availability and access to critical infrastructure.
The choice of NYC as a site to study the spatial dynamics of COVID-19 spread was influenced by the following reasons. First, the spread of COVID-19 was initially concentrated in urban areas before reaching the suburbs and more rural areas; NYC was amongst the hardest hit urban centres worldwide. Second, many of the city’s neighbourhoods with the highest number of cases per capita are areas with the lowest median incomes and largest average household size; the biggest hot spots include areas in the South Bronx, North and Southeast Queens and much of Staten Island. Third, New York has had a long history of disproportionate infrastructural investments in neighbourhoods (Perry et al., 2018). Hot spot analyses suggest that there are higher concentrations of grocery stores, hospitals, pharmacies and subway stations in high-income, predominantly white neighbourhoods. Finally, since the Bloomberg administration, NYC has emerged as a leader in data driven urban governance, and unlike many other cities, offers an immense quantity of publicly available data. The comprehensive open data legislation that was passed in 2012 set a high bar for open information and government transparency, enabling New Yorkers to interrogate the determinants of the city’s COVID-19 spread. NYC serves as an ideal entry point to model and understand the influence of urban infrastructure on the spatial dynamics of a pandemic.
Empirical studies examining inequities in COVID-19 spread in the US have largely relied on CDC defined epidemiological and socio-economic risk factors (Raifman and Raifman, 2020). Others have focused on environmental quality, governance and urban design factors (Sharifi and Khavarian-Garmsir, 2020). This study is, to our knowledge, the first peer-reviewed publication to use spatial regression modelling to investigate the relationship between the spatial arrangement of critical infrastructure and the disparities in COVID-19 spread at the neighbourhood level in NYC. While some research has investigated the impacts of health infrastructure and disease spread (Davis, 2020), ours is the first study to examine built environment variables as critical infrastructure, providing planners and policy makers a guide for possible resource investment in neighbourhoods for present and future urban public health emergencies.
Complicating urban health vulnerability
The global onslaught of the coronavirus has led experts to comment on the imminent ‘death of the city’ (Hernández-Morales et al., 2020). If Glaeser (2020) had been able to predict the events that would follow mere weeks after his publication, ‘Discontents of Urbanisation’, he might have included public health contagion as a ‘demon’ of density in cities. Population density and spatial distance are factors often implicated in the pandemic-fuelled flight from cities. With an average density of 28,000 residents per square mile, during the peak of the city’s coronavirus curve, Governor Andrew Cuomo cited New York City’s ‘spatial closeness’ as a reason for its rise as a viral epicentre (Levenson, 2020). The debate on cities and virus spread is two-fold: on the one hand, density in urban centres means less physical distance between residents, creating an ideal environment for the spread of air-borne diseases. On the other hand, cities benefit from the best aspects of density during times of crisis such as more services and amenities within walking distance or delivered to your door, concentration of medical facilities and pharmacies and decreased risk of isolation.
Recent scholarship from the fields of urban planning and public health suggests that the idea that density inevitably leads to ‘explosive epidemics’ does not stand up to the test. A recent report by the Citizens Housing and Planning Council (2020) found that residential population density is not a key determinant of the impacts of COVID-19, reporting that the city’s ten densest neighbourhoods, located primarily in Upper Manhattan, have reported some of the lowest rates of COVID-19. The data suggests that areas of NYC with the highest rates of COVID-19 in the city (4379 cases per 100,000 people), located in Elmhurst/Corona, have five times fewer residents per square mile than the densest zip codes in the city (Citizens Housing and Planning Council, 2020). A study led by researchers at the Johns Hopkins Bloomberg School of Public Health also found that denser counties, compared with those with greater urban sprawl, tended to have lower death rates, possibly because they enjoyed a higher level of urban development, including health care systems (Hamidi et al., 2020). Similarly, research on the differential exposure to COVID-19 found that crowded spaces play more of an influential role than population density (Almagro and Orane-Hutchinson, 2020). Studies in social epidemiology have found that clustering of COVID-19 cases has tended to be acutely associated with poverty, racialised economic segregation and household crowding (Chen and Krieger, 2020). All of this suggests that further work needs to be done to understand and address the complicated mix of elements present in our urban environments that contribute to the rapid spread of COVID-19.
Cities during the pandemic have not only experienced rapid spread, but also differential spread. There is increasing evidence to suggest that rates of infection, morbidity and mortality from COVID-19 are not evenly distributed, with socio-demographic and clinical risk factors clearly associated with increased risk of transmission and death (Centers for Disease Control, 2020). Data from the CDC indicates that people aged 65 and over, particularly those living in nursing homes, are at elevated risk of the coronavirus (Centers for Disease Control, 2020). Similarly, individuals with underlying medical conditions such as heart disease, lung disease, asthma, obesity, diabetes and several other such conditions are highly vulnerable. Trends in COVID-19 data also suggest that social, economic and racial factors influence individual risk (Choi and Unwin, 2020; Lamb et al., 2021; Millett et al., 2020). In NYC, deaths appear to be concentrated in more diverse neighbourhoods, with Black and LatinX residents experiencing mortality rates that are twice those of white city dwellers (NYC Department of Health, 2020). Some of the highest numbers of cases are clustered in lower income neighbourhoods in the Bronx, Harlem, parts of South Brooklyn and Staten Island. The uneven nature of the virus’s spread in NYC has revealed insights into the relationship between structural inequality and geography, and capital investment in US cities.
The relationship between infrastructure investment and socio-economic disparity has been well established in urban scholarship (Rothstein, 2017; Sugrue, 1996; Squires, 1992). In the context of research on urban health, redlining and racial segregation practices such as mortgage lending have been blamed for disparities in health outcomes across neighbourhoods. Recent studies show that patterns of COVID-19 by neighbourhoods in NYC emulate those of redlining in the 1940s (Choi and Unwin, 2020). Redlining refers to the discriminatory practices used by banks who denied services to specific individuals based on the location of their residences (McCoy, 2007). According to Choi and Unwin (2020), the predominantly white neighbourhoods of Greenwich Village/Soho and Lower Manhattan, which tended to have a high rate of loan acceptance, had the lowest infection rates in NYC. In contrast, in areas such as West Queens and the Rockaways, which were amongst the hardest hit by the pandemic, historic loan acceptance rates were significantly low, raising important questions regarding unequal distribution and access to critical medical resources and assistance, during the crisis in NYC.
Despite the establishment of progressive civil rights laws prohibiting discrimination against minority and low-income neighbourhoods in the 1960s and 1970s, namely, the Fair Housing Act of 1968, the Equal Credit Opportunity Act of 1974 and the Community Reinvestment Act of 1977, patterns of discrimination and disinvestment continue to persist. Black et al. (2015) cite issues such as limited access to nearby health care, poor air and water quality, limited access to open space, crowded living conditions and so on, in their review of literature on racial discrimination and health. The long-term impacts of discriminatory mortgage lending practices have led to the funnelling of credit and investment into mostly white neighbourhoods and suburbs (Ladd, 1998; Turner and Skidmore, 1999). Over the past decades, cities across the US have struggled to implement housing policies that attempt to integrate neighbourhoods, making critical medical infrastructure, desirable open spaces and other valued infrastructures, out of reach for minority and low-income communities.
In New York’s affluent white neighbourhoods, government subsidised developments are far and few between. Despite mayor de Blasio’s campaign agenda focused on ending racial and economic inequality, about three-quarters of the new and preserved housing units financed by the city, during his first term, were in neighbourhoods where the majority of residents are Black or Hispanic (Goldenberg, 2018). According to a recent report by City Council Member Brad Lander, NYC remains more segregated than most metropolitan areas in the US (Lander, 2019). His findings suggest that currently 81.6% of white or Black New Yorkers would have to move to a new neighbourhood to achieve a more even racial distribution in the city (Lander, 2019). The 2016 policy enacted by de Blasio’s administration for ‘Mandatory Inclusionary Housing’ was intended to promote neighbourhood integration by requiring that more affordable homes be built in wealthier areas. Yet, so far, the neighbourhoods selected to be rezoned have been in poorer areas with largely minority populations (Goldenberg, 2018).
The COVID-19 ‘disruption’ sheds light on the politics of infrastructure in NYC, complicating ideas about population density as the catalyst for rapid disease spread in cities. Urban scholarship has long understood infrastructure as a socio-political agenda focused on institutional relations and historical concentrations of power, control and access. As Steele and Legacy (2017) remind us, urban infrastructures shape communities socially, economically and politically. They divide communities and bring them together; they bring development and progress to some and sludge and garbage to others; they are updated and maintained in some areas, while remaining archaic and dismantled in others. NYC’s ‘PAUSE’ policy for non-essential businesses has induced a radical shift in the locations and demand for infrastructural services including energy, transit, medical services and green spaces. It has also revealed decades of history that works to maintain boundaries between segregated communities in NYC. These boundaries, made clear by the differences in capital investment, are now being tested by death rates and disease spread.
Data description and spatial patterns at the neighbourhood level
For our analysis, we use NYC’s zip code level data on COVID-19 case rates, SVI, UHVI and CI described below. More information on the structure of indices used and detailed metadata can be found in Appendix Table 1.
COVID-19 case rate
The data on COVID-19 incidence used in this study is from the NYC Department of Health and Mental Hygiene (DOHMH), which releases daily data on the cumulative count of COVID-19 cases, total residents that have been tested and the total number of deaths, organised by the zip code of residence. For the purpose of this study, we have chosen to focus on COVID-19 ‘cases’ rather than deaths or rates of hospitalisation, as we are primarily concerned with the spread of the virus, rather than the severity of the infection. Death and hospitalisation rates can be influenced to a greater degree by individual health variables such as age and presence of comorbidities. The DOHMH calculates ‘case rate’ in addition to case count, which is the number of cases per 100,000 residents, a more comparable statistic for our purpose. We have collected data from the beginning of the outbreak, 29 February 2020 (as reported by the DOHMH) to 24 September 2020, about seven months of data. At the time the data was downloaded, there were 230,558 cases across NYC, spread across 178 zip codes, with a mean case rate of 2654 per 100,000 residents. Figure 1(a) shows the spatial distribution of COVID-19 case rates by zip code. The map shows a high degree of clustering in the Bronx, and Queens, with values >3000 cases per 100,000 residents, nearly double the mean case rate value. Areas in Manhattan and Brooklyn, in comparison, have far lower-case rates.
Figure 1.
Maps of (a) COVID-19 case rate per 100,000 residents, (b) Social Vulnerability Index (SVI), (c) Urban Health Vulnerability Index (UHVI), and (d) Critical Infrastructure (CI) by Zip Code, NYC (2020).
Social Vulnerability Index (SVI)
The SVI is a widely established measure used in health research, particularly in the fields of medical emergencies and disease mitigation planning (Flanagan et al., 2018). According to the CDC, social vulnerability refers to the degree to which certain social conditions such as high poverty, crowded housing or a community’s minority status may affect the community’s ability to prevent suffering and financial loss in the event of a disaster (Centers for Disease Control, 2020). For our analysis, we obtained 2018 SVI data for NYC available at the census tract level. The SVI, based on 15 different census estimated variables, indicates the relative vulnerability of every US census tract. 1 Each variable is grouped into one of four themes: socio-economic status (below poverty, unemployed, income, no high school diploma), household composition and disability (aged 65 or older, aged 17 or younger, older than age 5 with a disability, single parent households), minority status and language (minority, speaks English ‘less than well’) and housing and transportation (multi-unit structures, mobile homes, crowding, no vehicle, group quarters). To estimate SVI for New York City zip codes, we calculated the average SVI scores of census tracts that intersect each zip code. Figure 1(b) maps the SVI values across NYC by zip codes. In general, there are large areas of vulnerable populations in the Bronx, central Brooklyn and the Rockaway neighbourhood in Queens. The Map suggests Mid to Lower Manhattan, suburban areas of Queens and Staten Island have lower SVIs.
Urban Health Vulnerability Index (UHVI)
There are multiple indices of vulnerability to COVID-19 and its social and health impacts emerging in the US (Davis, 2020; DeCaprio et al., 2020; Surgo Foundation, 2020). We selected RS21’s UHVI for its unique focus on ‘urban health’. RS21’s UHVI extracts the CDC’s ‘500 Cities project’ data on currently established chronic conditions that increase individual risk to COVID-19, namely, asthma, chronic obstructive pulmonary disease (COPD), diabetes, cancer, smoking, coronary heart disease, hypertension, stroke, kidney disease and old age (≥65 years). 2 To normalise the range of variables in the UHVI, we scaled them using percentiles for each zip code. Figure 1(c) shows a map of the UHVI rankings across zip codes census tracts. A clear pattern of urban health vulnerability is visible across central Brooklyn into central Queens around JFK airport. The Bronx also exhibits higher values of UHVI, as expected based on the above SVI scores. A surprising finding is that the neighbourhood of Corona in Queens, a widely reported hot spot of the coronavirus, which shows high values of SVI and COVID-19 case rates, is not at an elevated risk of UHVI (Correal and Jacobs, 2020).
Critical infrastructure (CI)
To establish how availability and access to critical urban infrastructure facilities influence COVID-19 case rates in NYC, we developed a set of metrics along four sectors critical to pandemic response and care: (1) medical care, (2) food and nutrition, (3) mobility, and (4) open space. A total of seven different CI variables were identified: hospitals; pharmacies; grocery stores; soup kitchens and food pantries (meal programmes); subway entrances; sidewalk widths; and open spaces. Geolocations of each were extracted from a combination of publicly available data from the NYC Department of City Planning (NYC DCP) and the NYC Open Data Portal, and proprietary data from the Google Places API. To demonstrate that COVID-19 spread is influenced by availability and access to CI, we calculated the density of, and distance to, each of the above CI variables, allowing us to create a more nuanced picture of the effect of CI’s on COVID-19 spatial spread. Density is defined as the quantity of CI features in each zip, and distance as the locational distance to CI features in each zip (Henriksen et al., 2008). To calculate density, we approximated kernel density for each CI feature; to calculate average distance, we used ‘Euclidean distance’ or the straight-line distance calculated from the centroid of each census tract to the centroid of the nearest CI feature and averaged the distances of the census tracts that intersected the zip code. Figure 1(d) and Table 1 show the density of CI per 100,000 residents in NYC by borough.
Table 1.
Critical infrastructure variables, 2020: Density of CI per 100,000 residents by borough.
| Sector | Variable | NYC | Manhattan | Brooklyn | Queens | Staten Island | TheBronx |
|---|---|---|---|---|---|---|---|
| Medical care | Hospitals | 0.72 | 1.23 | 0.63 | 0.40 | 0.84 | 0.78 |
| Pharmacies | 29.06 | 28.67 | 29.65 | 29.99 | 25.62 | 28.13 | |
| Food andnutrition | Grocery stores | 11.97 | 9.95 | 12.19 | 13.84 | 10.92 | 11.28 |
| Meal programmes | 8.38 | 8.78 | 8.91 | 6.88 | 6.72 | 9.94 | |
| Mobility | Subway entrances | 23.13 | 47.58 | 21.17 | 14.42 | 10.08 | 16.78 |
| Open space | Parks | 14.80 | 11.97 | 14.88 | 13.62 | 28.56 | 15.16 |
In NYC, medical care facilities are not evenly spatially distributed. For example, Queens and Brooklyn have much lower densities of hospitals than the other boroughs, with 0.40 and 0.63 hospitals per 100,000 residents respectively. The Bronx, a region that has very high SVI values, also has narrower sidewalks and lower densities of subway entrances, grocery stores and pharmacies compared with NYC total values, and a higher-than-average density of free meal programmes, consistent with literature on the city’s segregated landscape.
Machine learning for spatial regression modelling
We estimate a series of regression models centring the variables SVI, UHVI and CI, to examine how fragmentation of critical infrastructure impacts the spread of COVID-19 in NYC. We use Elastic Net, a supervised machine learning method that utilises both LASSO (Least Absolute Shrinkage and Selection Operator) and Ridge regression regularisation techniques, to reduce the variance in the model, while introducing some bias. Using Elastic Net can help narrow down the variables that are most significant in influencing COVID-19 spread, and demonstrates whether CI improves the performance of SVI and UHVI. Regularised regression models introduce a penalty term P (λ, β) for having too many variables, with regularisation parameter λ (Zou and Hastie, 2005). LASSO uses shrinkage, a technique by which regression coefficients are shrunk towards zero, and removes variables that are of lower significance. Its penalty term is called L1-norm, which is the sum of the absolute regression coefficients. Ridge regression shrinks the regression coefficients, so that variables with minor contribution to the outcome have their coefficients close to zero. The shrinkage of the coefficients in Ridge is achieved by penalising the regression model with a penalty term called L2-norm, which is the sum of the squared coefficients, rather than the absolute values. Elastic Net produces a regression model that is penalised with both L1-norm and L2-norm. Below, the α values, which are set between 0 and 1, control the amount of Ridge and LASSO that is being applied as the penalty term in the regression. An α = 1 will be all LASSO, while an α = 0 will be all Ridge, and anything in between is a ratio of the two. Elastic Net aims at minimising the following loss function:
| (1) |
where α is the mixing parameter between Ridge (α = 0) and LASSO (α = 1).
Given that traditional regression models are often unreliable when interpreting spatial data, and tend to exhibit a high degree of spatial autocorrelation and heteroscedasticity of residuals, in this analysis we use a spatially lagged variable to account for spatial dependencies that may be present (Fotheringham and Rogerson, 2009). A spatially lagged variable is a weighted sum or a weighted average of the neighbouring values for that variable (Anselin, 1988). The spatial lag regression model according to Fotheringham and Rogerson (2009) can be expressed as:
Where is an observation of the dependent variable, includes the neighbouring locations of and , with . The function is a spatial weights matrix. We include the spatial lag term in our final regression model and interpret its coefficients and p-values.
To test the performance of our model, we use a five-fold cross validation technique. There are two parameters that require tuning in our Elastic Net model, the α and λ hyper parameters, which are cross validated using this technique. To perform the cross validation, we split our dataset into five groups, each unique group is retained as the test data for the model, while the remaining four groups are used as training datasets. The process is repeated five times, with each of the five subsamples used exactly once as the test data, producing a Mean Squared Error (MSE) for each iteration, which is then averaged to produce a single MSE. In this study, we select the model where the MSE is within one standard error of the minimum MSE as the model of best fit, giving the most favourable α and λ values.
As we have introduced spatial variables into an analysis of COVID-19 case rates, performing a spatial autocorrelation on the residuals of the models allows us to see whether CI variables explain some of the variance encountered in models that use SVI and UHVI alone as independent variables. We used the Global Moran’s I function to test for clustering, dispersion and randomness of residuals (ESRI, 2020). The range of possible values for the Moran’s I index falls between −1.0 and +1.0, with values closer to 1.0 indicating clustering of similar values, values near 0 exhibiting complete spatial randomness and values closer to −1.0 indicating that neighbouring values are very different from each other. When there is high spatial autocorrelation, or Moran’s I values are closer to 1.0, the residuals or the errors in the model will either perform well or poorly, in clusters.
Findings: Three models for understanding disease spread,and model diagnostics
In this section we present the results of our three models. In Model 1, we estimate the influence of SVI and UHVI on COVID-19 case rates. This estimation allows us to test the performance of models that explain case rates based on CDC established socio-economic and epidemiological factors, and understand the relative importance of each. It also gives insight into some of the unexplained variance in COVID-19 spread in the model, which may potentially be addressed by spatial variables such as CI. In Model 2, we explore the influence of CI variables on COVID-19 case rates, examining the effects of both density of, and distance to CIs in each zip code. This estimation allows us to inspect whether there are any spatial patterns in COVID-19 spread that may be explained by the disproportionate distribution of CIs in NYC. Model 3 analyses the effects of all three factors, SVI, UHVI and CI, on COVID-19 case rates. In this model, we first introduce a regression estimate that does not consider potential spatial effects 3(a), and another that controls for spatial lag 3(b), to investigate the importance of geography in explaining COVID-19 spread.
Model 1: How well do SVI and UHVI metrics explain the COVID-19 case rates in NYC zip codes?
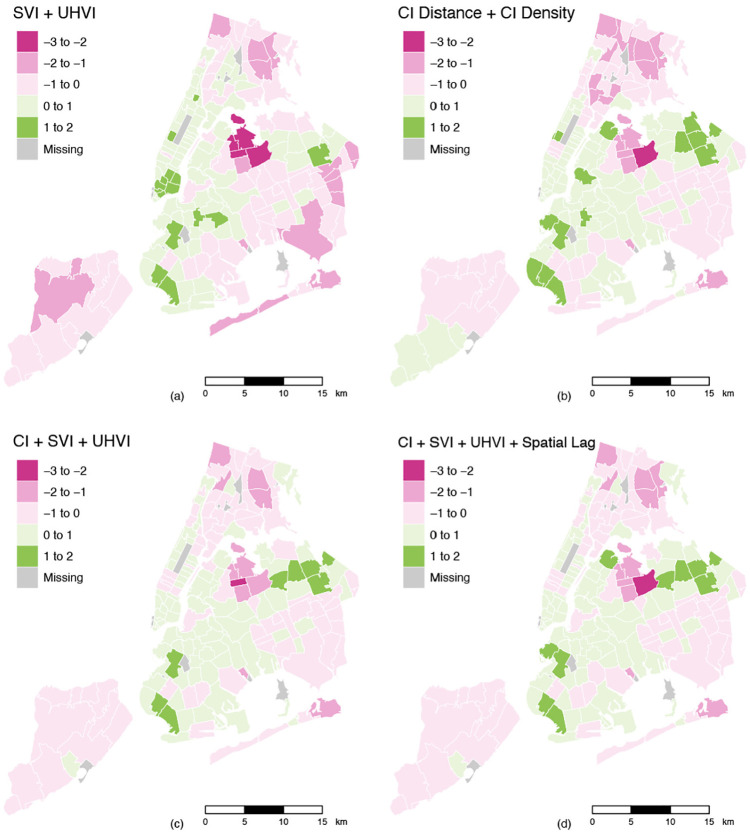
Our baseline model suggests that when taken together, UHVI had a larger explanatory effect than SVI on COVID-19, with coefficient values of 0.298 and 0.242, respectively. Figure 2(a) shows a map of the residuals from the model. The darker areas represent the zip codes with higher error rates, suggesting that this model is not the best for explaining COVID-19 case rates in those zip codes. In Lower Manhattan, where the residuals are high, the model over predicts COVID-19 case rates. In contrast, in neighbourhoods such as Corona in Queens, which experienced one of the highest outbreaks of the coronavirus, the model appears to be under predicting case rates, as indicated by the darker pink zip codes. All of this suggests that there is some unexplained spatial variance present in the model that requires further investigation.
Figure 2.
Maps of residuals for regularised regression models: (a) Social Vulnerability Index + Urban Health Vulnerability Index, (b) Critical Infrastructure Distance + Critical infrastructure Density, (c) Critical Infrastructure + Social Vulnerability Index + Urban Health Vulnerability Index, (d) Critical Infrastructure + Social Vulnerability Index + Urban Health Vulnerability Index + Spatial Lag.
Model 2: To what extent does distance to, and the density of, critical infrastructures in NYC zip codes impact the spread of COVID-19?
Our findings indicate that CI variables are correlated with COVID-19 case rates in NYC. The coefficient plot in Figure 3(a) shows the explanatory value of each of the CI variables with respect to COVID-19 case rates. The variables that are positively correlated with COVID-19 case rates are density of meal programmes, distance to parks and hospitals and density of pharmacies. Variables that are negatively correlated are density of subway entrances and hospitals, mean sidewalk widths, distance to meal programmes and density of parks and grocery stores. Increased distance from parks and hospitals is associated with higher rates of COVID-19, which is consistent with health data findings that show lower income neighbourhoods with poor access to medical facilities and green infrastructure have poorer health outcomes, as seen in our SVI map in Figure 1(b). These neighbourhoods also tend to have a higher proportion of meal programmes such as soup kitchens and food pantries. An interesting finding is that density of pharmacies in neighbourhoods is associated with higher rates of COVID-19, possibly due to an increase in average neighbourhood pharmacy visits during the pandemic or the presence of high-risk essential workers in these sites.
Figure 3.
Coefficient plots for regularised regression models: (a) Social Vulnerability Index + Urban Health Vulnerability Index, (b) Critical Infrastructure Distance + Critical infrastructure Density, (c) Critical Infrastructure + Social Vulnerability Index + Urban Health Vulnerability Index, (d) Critical Infrastructure + Social Vulnerability Index + Urban Health Vulnerability Index + Spatial Lag.
An increase in the density of subway entrances lowers the rate of COVID-19 cases. This finding challenges commonly held notions about population density and increased COVID-19 case rates. In NYC, areas with greater availability of subway entrances include Times Square and the East and West Village. These areas, as our findings suggest, witnessed far lower rates of COVID-19 than other parts of the city. Increase in the mean sidewalk width is also associated with lower rates of COVID-19, which holds up to prevailing social distancing guidelines claiming that an increase in physical distance between people lowers the rate of disease transmission. Moreover, as distance to meal programmes and density of parks and grocery stores increase, the rate of COVID-19 cases decreases, resonating with existing claims that an increase in SVI scores in zip codes is associated with higher COVID-19 cases (Flanagan et al., 2018). Figure 2(b) shows a map of the residuals from the regression model. The residuals suggest that many areas in the Bronx, Rockaways and Corona in Queens are being under predicted by our CI model, while areas like Midtown Manhattan, South Brooklyn and the Northeastern suburban area of Queens are being over predicted.
We ran additional regression models estimating COVID-19 case rates using CI and UHVI, and CI and SVI. Our results show that in both models, SVI and UHVI had very large positive coefficients, indicating the significant effect UHVI and SVI scores have on rates of COVID-19, when combined with CI variables. This suggests that while CI variables have a spatial effect on COVID-19 spread, they perform best when combined with factors affecting socio-economic and health vulnerability in NYC.
Model 3: Can CI, SVI and UHVI together, better explain COVID-19 case rates in NYC zip codes?
Models 3(a) and 3(b) provide a more holistic picture of the variables affecting differential rates of COVID-19 spread in NYC. When SVI, UHVI and CI are taken together, SVI has the largest positive coefficient, followed by UHVI and distance to parks and hospitals. The variables that had a negative correlation to COVID-19 case rates were mean sidewalk widths, density of subway entrances and density of hospitals and parks. These results are consistent with our findings from the previous two regressions. As spatial dependencies are very likely present in our models, we added a spatial lag variable, as explained in the previous methods section. Figure 3(c) and (d) illustrates the difference in coefficients in the model when adding a spatial lag term. We also see that the residual maps for Models 3(a) and 3(b) are nearly identical in Figure 2, the addition of spatial lag minimises the residuals but does not significantly alter the spatial distribution of them. This suggests that the rates of COVID-19 in NYC zip codes are spatially autocorrelated. Importantly, it also suggests that there are many potential socio-spatial factors still to be determined that might explain the density of COVID-19 cases in some areas in NYC. The residual errors in Figure 2(c) and (d) suggest that many areas in the Bronx, Corona and central Queens are being under predicted by our CI model, while areas such as coastal Brooklyn and the Northeastern suburban area of Queens are being over predicted.
Model diagnostics
The hyperparameter values from the Elastic Net regression and the model diagnostics we performed demonstrate which of our models were most significant in explaining COVID-19 cases, illustrated in Table 2 below. We can see that the model with the spatial lag term outperformed the others. The α value is 0.0, showing that the model is defined by Ridge; as the λ value increases, the coefficients get dropped to 0. It’s MSE is 0.428, which is lower than the other models, showing the difference between actual and predicted COVID-19 case rates is smallest. The Moran’s I value is closest to 0 at 0.452, suggesting that the residuals exhibit behaviour closer to complete spatial randomness. We also see that this model has minimised spatial autocorrelation, which other models exhibit to a greater extent.
Table 2.
Elastic net models’ hyperparameter values and model diagnostics.
| Models | MSE (mean squared error) | Moran’s I | α | λ |
|---|---|---|---|---|
| CI distance+density | 0.6469167 | 0.5390432 | 0.0 | 0.5138314 |
| CI+SVI | 0.4504832 | 0.4830474 | 0.6 | 0.3930560 |
| CI+UHVI | 0.5114450 | 0.4850781 | 0.1 | 0.6810454 |
| SVI+UHVI | 0.6204950 | 0.6228640 | 0.0 | 0.5151858 |
| CI+SVI+UHVI | 0.4314099 | 0.4755339 | 0.0 | 0.6810454 |
| CI+SVI+UHVI+spatial lag | 0.4280318 | 0.4518502 | 0.0 | 0.7474464 |
The next best performing model was CI+SVI+UHVI. The α value is 0.0, indicating it is all Ridge as well. Here the MSE is 0.431, and the Moran’s I is 0.476, suggesting that coefficients are still slightly autocorrelated. The CI+SVI and CI+UHVI models performed decently compared with the others. The worst performing model is the SVI+UHVI model. The MSE is 0.621, which is higher than any of the other models, suggesting larger gaps between predicted and actual values of COVID-19 case rates. The Moran’s I value is 0.623, which is also higher than any of the other models, displaying the highest level of autocorrelation. This finding suggests that CI variables are important in explaining some of the differential spread of COVID-19 cases in NYC, and must be included in public health planning and policy analyses of socio-economic and health vulnerability to COVID-19.
Conclusion and future research
This study provides a detailed empirical exploration of the influence of critical infrastructure on urban health vulnerability to COVID-19 at the neighbourhood level in NYC. This analysis (1) explores the relationship between CI, UHVI and SVI and COVID-19 case rates, (2) identifies variables that are most important in explaining case spread in NYC for each of our three models, and (3) examines the influence of spatial dependencies and neighbourhood effects on the determinants of COVID-19 spread. In the face of the coronavirus crisis and the uneven impacts on urban populations globally, our research contributes to literature on the social determinants of health, racial disparities in neighbourhood investment and the infrastructural turn in urban scholarship. This work sheds light on the important history of segregation in NYC and its implications for COVID-19 case spread.
Our results show that while determinants of socio-economic vulnerability and epidemiological risk factors influence the virus’s spatial spread, the absence and presence of key infrastructure facilities such as parks, hospitals and grocery stores are critical in explaining the uneven outcomes of the pandemic at the neighbourhood level. When we included CI variables in models on SVI and UHVI, it consistently improved modelling errors and spatial autocorrelation, thereby explaining more of the spatial effects of the model that were not being captured by the indices. In particular, we found that in looking at two different spatial relationships, distance and density, we were able to provide a more nuanced estimation of COVID-19 cases. In some instances, while density of CI was not very significant in limiting COVID-19, spatial distance was. It is therefore not simply about the quantity of infrastructure facilities available to residents, but also about distance and access to such resources that influences infection rates. Our findings are a first glimpse into the ultimate ‘black-box’ of urban infrastructure (McFarlane, 2011; Rutherford, 2020), quantifying ways in which geolocations of CI, a spatial representation of government decision making and public and private investment are seen to influence health disparities particularly in the case of highly contagious airborne diseases.
The inclusion of a spatial lag term in our model provided two important insights. First, the spatial lag term indicated that spatial autocorrelation was present in our model and that systematic spatial variation in our dependent variable, COVID-19 case rates, exists in NYC. Second, it provides important insights for future research, as it affirms the presence of other spatial phenomena in the model that require further interrogation that are not currently captured by the SVI, UHVI and CI variables we have included. Future research might consider looking at other CI variables of interest such as availability and access to restaurants and food delivery services, broadband and internet services and social infrastructures such as schools, libraries and universities. Further analysis might also consider including control variables such as environmental quality, urban design and other such factors that can influence the spread of COVID-19 that have not been accounted for in our models. Implications of CI and UHVI on COVID-19 mortality rates or hospitalisation rates may also be another valuable avenue of research, providing insights on the importance of CI on severity of epidemiological risk.
Some limitations of our research that require consideration are that the COVID-19 case rate data used here is a measure of reported cases based on local testing, rather than an actual account of positive cases in NYC, and thus the model might be over predicting case rate in some areas. In addition, we have chosen to select a snapshot of data capturing a six-month period of time in NYC under the pandemic, rather than to perform a time-series analysis. While performing an analysis of the timed effects of public health response policies on infrastructural conditions such as street closures, mask requirements, social distancing rules and limits on store capacities would provide nuanced insights on the relationship between CI and COVID-19, due to limitations on data availability and time of study, this type of time series analysis was beyond the scope of this paper. Our hope is to tackle such questions in future avenues for research. We hope our methodology may be applied in other contexts to analyse COVID-19 spread in other metro areas in the US, as well as other densely populated cities with diverse and underrepresented communities.
Table 1.
Index of CI, SVI, and UHVI variables with metadata.
Note: 1. US CDC: Centers for Disease Control and Prevention. 2. NYC DCP: NYC Department of City Planning. 3. NYC DOT: NYC Department of Transportation. 4. MTA: Metropolitan Transportation Authority.
For a detailed description of SVI variable selection rationale and methods, see A Social Vulnerability Index for Disaster Management. Available at: https://www.atsdr.cdc.gov/placeandhealth/svi/img/pdf/Flanagan_2011_SVIforDisasterManagement-508.pdf (accessed 10 September 2020).
For a detailed description of RS21’s methodology, see https://covid.rs21.io/data-sources (accessed 10 September 2020).
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Gayatri Kawlra  https://orcid.org/0000-0001-5990-1549
https://orcid.org/0000-0001-5990-1549
Contributor Information
Gayatri Kawlra, Columbia University, USA.
Kazuki Sakamoto, Columbia University, USA.
References
- Acuto M. (2020) Engaging with global urban governance in the midst of a crisis. Dialogues in Human Geography 10(2): 221–224. [Google Scholar]
- Addie J-PD, Glass MR, Nelles J. (2020) Regionalizing the infrastructure turn: A research agenda. Regional Studies Regional Science 7(1): 10–26. [Google Scholar]
- Almagro M, Orane-Hutchinson A. (2020) The determinants of the differential exposure to COVID-19 in New York City and their evolution over time. SSRN. Available at: https://ssrn.com/abstract=3573619 (accessed 17 September 2020). [DOI] [PMC free article] [PubMed]
- Anand N, Gupta A, Appel H. (2018) The Promise of Infrastructure. Durham, NC, and London: Duke University Press. [Google Scholar]
- Anselin L. (1988) Spatial Econometrics: Methods and Models. Dordrecht, The Netherlands: Kluwer Academic Publishers. [Google Scholar]
- Black LL, Johnson R, VanHoose L. (2015) The relationship between perceived racism/discrimination and health among black American women: A review of the literature from 2003 to 2013. Journal of Racial and Ethnic Health Disparities 2: 11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callon M. (1998) Laws of the Markets. Oxford: Wiley-Blackwell. [Google Scholar]
- Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry/Geospatial Research, Analysis, and Services Program (2020) CDC Social Vulnerability Index Database. New York, NY: Centers for Disease Control and Prevention. [Google Scholar]
- Chen JT, Krieger N. (2020) Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county vs ZIP code analyses. Harvard Center for population and development studies Working Paper Series 19(1). [Google Scholar]
- Choi Y, Unwin J. (2020) Racial impact on infections and deaths due to COVID-19 in New York City. Available at: https://arxiv.org/abs/2007.04743 (accessed 2 October 2020).
- Citizens Housing and Planning Council (2020) Density and COVID-19 in New York City. Report, May. New York: Citizens Housing and Planning Council. [Google Scholar]
- Connolly C, Ali SH, Keil R. (2020) On the relationships between COVID-19 and extended urbanization. Dialogues in Human Geography 10(2): 213–216. [Google Scholar]
- Correal A, Jacobs A. (2020) A tragedy is unfolding: Inside New York’s virus epicenter. The New York Times, 9April. [Google Scholar]
- Davis D. (2020) Covid-19 vulnerability mapping for the US’s 500 largest cities. In: Social progress imperative. Available at: https://socialprogress.blog/2020/04/03/covid-19-vulnerability-mapping-for-the-uss-500-largest-cities/ (accessed 16 October 2020). [Google Scholar]
- DeCaprio D, Gartner J, McCall CJ, et al. (2020) Building a COVID-19 vulnerability index. Journal of Medical Artificial Intelligence 3: 15–15. [Google Scholar]
- Edwards PN. (2003) Infrastructure and modernity: Force, time, and social organization in the history of sociotechnical systems. In: Misa TJ, Brey P, Feenberg A. (eds) Modernity and Technology. Cambridge, MA: MIT Press, pp. 185–225. [Google Scholar]
- Enright T, Ward K. (2021) Governing urban infrastructures under pandemic conditions: Some thoughts. Urban Geography. Epub ahead of print 1 March 2021. DOI: 10.1080/02723638.2021.1893050. [DOI] [Google Scholar]
- ESRI (2020) How spatial autocorrelation (global Moran’s I) works. Available at: https://pro.arcgis.com/en/pro-app/tool-reference/spatial-statistics/h-how-spatial-autocorrelation-moran-s-i-spatial-st.htm (accessed 21 August 2020).
- Flanagan BE, Hallisey EJ, Adams E, et al. (2018) Measuring community vulnerability to natural and anthropogenic hazards: The Centers for Disease Control and Prevention’s Social Vulnerability Index. Journal of Environmental Health 80(10): 34–36. [PMC free article] [PubMed] [Google Scholar]
- Fotheringham A, Rogerson P. (2009) The Sage Handbook of Spatial Analysis. London: SAGE Publications. [Google Scholar]
- Gandy M. (2006) The bacteriological city and its discontents. Historical Geography 34: 14–25. [Google Scholar]
- Glaeser E. (2020) Urbanization and it’s discontents. National Bureau of Economic Research Working Paper 26839. Available at: http://www.nber.org/papers/w26839 (accessed 25 October 2020).
- Godoy M, Wood D. (2020) What do Coronavirus racial disparities look like state by state? Npr/Wnyc, 30May. [Google Scholar]
- Goldenberg S. (2018) 50 years after the Fair Housing Act, New York City still struggles with residential segregation. POLITICO, 23April. [Google Scholar]
- Graham S. (2010) Disrupted Cities: When Infrastructure Fails. London: Routledge. [Google Scholar]
- Gross B, Zheng Z, Liu S, et al. (2020) Spatio-temporal propagation of COVID-19 pandemics. EPL (Europhysics Letters) 131: 1–7. DOI: 10.1209/0295-5075/131/58003. [DOI] [Google Scholar]
- Hamidi S, Sabouri S, Ewing R. (2020) Does density aggravate the COVID-19 pandemic? Journal of the American Planning Association 86(4): 495–509. [Google Scholar]
- Henriksen L, Feighery EC, Schleicher NC, et al. (2008) Is adolescent smoking related to the density and proximity of tobacco outlets and retail cigarette advertising near schools? Preventive Medicine 47(2): 210–214. [DOI] [PubMed] [Google Scholar]
- Hernández-Morales A, Oroschakoff K, Barigazzi J. (2020) The death of the city. POLITICO, 27July. [Google Scholar]
- Johnson S. (2007) The Ghost Map: The Story of London’s Most Terrifying Epidemic – and How It Changed Science, Cities, and the Modern World, reprint edn. New York, NY: Riverhead Books. [Google Scholar]
- Ladd HF. (1998) Evidence on discrimination in mortgage lending. Journal of Economic Perspectives 12(2): 41–62. [Google Scholar]
- Lamb MR, Kandula S, Shaman J. (2021) Differential COVID-19 case positivity in New York City neighborhoods: Socioeconomic factors and mobility. Influenza and Other Respiratory Viruses 15(2): 209–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lander B. (2019) Desegregating NYC: A (very modest) one-year progress report. Report, April. NYC: New York City Council. [Google Scholar]
- Larkin B. (2013) The politics and poetics of infrastructure. Annual Review of Anthropology 42: 327–343. [Google Scholar]
- Latour B. (2007) Reassembling the Social: An Introduction to Actor-Network-Theory. Oxford: Oxford University Press. [Google Scholar]
- Levenson E. (2020) Why New York is the epicenter of the American coronavirus outbreak. CNN, 26March. [Google Scholar]
- McCoy P. (2007) The Home Mortgage Disclosure Act: A synopsis and recent legislative history. Journal of Real Estate Research 29(4): 381–398. [Google Scholar]
- McFarlane C. (2011) The city as assemblage: Dwelling and urban space. Environment and Planning D: Society and Space 29(4): 649–671. [Google Scholar]
- Millett GA, Jones AT, Benkeser D, et al. (2020) Assessing differential impacts of COVID-19 on black communities. Annals of Epidemiology 47: 37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell T. (2011) Carbon Democracy: Political Power in the Age of Oil. New York, NY: Verso. [Google Scholar]
- NYC Department of Health (2020) COVID-19 data: Cases, hospitalizations and deaths [data file and codebook]. Available at: https://github.com/nychealth/coronavirus-data (accessed 21 August 2020).
- Perry AM, Rothwell J, Harshbarger D. (2018) The devaluation of assets in black neighborhoods: The case of residential property. Report for Brookings, Metropolitan Policy Program. November. Washington, DC: Brookings. [Google Scholar]
- Powrie W. (2020) Infrastructure and cities for a COVID-19 world. UKCRIC. Available at: https://www.ukcric.com/insights/infrastructure-and-cities-for-a-covid-19-world/ (accessed 15 June 2021).
- Raifman MA, Raifman JR. (2020) Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. American Journal of Preventive Medicine 59(1): 137–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothstein R. (2017) The Color of Law: A Forgotten History of How Our Government Segregated America. New York, NY: Liverlight. [Google Scholar]
- RS21 (2020) Urban health vulnerability index. Available at: https://covid.rs21.io/ (accessed 2 October 2020).
- Rutherford J. (2020) Redeploying Urban Infrastructure: The Politics of Urban Socio-Technical Futures. Cham: Springer International Publishing. [Google Scholar]
- Schwirtz M, Cook LR. (2020) These N.Y.C. Neighborhoods have the highest rates of virus deaths. The New York Times, 18May. [Google Scholar]
- Sharifi A, Khavarian-Garmsir AR. (2020) The COVID-19 pandemic: Impacts on cities and major lessons for urban planning, design, and management. The Science of the Total Environment 749: 142391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squires GD. (1992) Redlining to Reinvestment. Philadelphia, PA: Temple University Press. [Google Scholar]
- Steele W, Legacy C. (2017) Critical urban infrastructure. Urban Policy and Research 35(1): 1–6. [Google Scholar]
- Sugrue TJ. (1996) The Origins of the Urban Crisis: Race and Inequality in Postwar Detroit. Princeton, NJ: Princeton University Press. [Google Scholar]
- Surgo Foundation (2020) The COVID-19 community vulnerability index map. Available at: https://precisionforcovid.org/ccvi (accessed 15 September 2020).
- Turner MA, Skidmore F. (1999) Mortgage lending discrimination: A review of existing evidence. Report, June. Washigton, DC: Urban Institute. [Google Scholar]
- World Economic Forum (2020) Shaping the future of cities, infrastructure and urban services. World Economic Forum blog series Available at: https://www.weforum.org/events/world-economic-forum-annual-meeting-2020/sessions/shaping-the-future-of-cities-infrastructure-and-urban-services (accessed 2 June 2021).
- Zou H, Hastie T. (2005) Regularization and variable selection via the elastic net. Journal of the Royal Statistical Society: Series B (Statistical Methodology) 67(2): 301–320. [Google Scholar]