Abstract
Background
Forcibly displaced people face various challenges and are therefore at higher risk of being affected by mental and physiological distress. The present study aimed to determine levels of psychological well-being, PTSD symptom severity, metabolic syndrome, and associated factors among forcibly displaced people in Greece in response to WHO’s call for evidence-based public health policies and programs for forcibly displaced people.
Methods
We conducted a cross-sectional study among n = 150 (50% women) forcibly displaced people originating from Sub-Sahara Africa and Southwest Asia living in a Greek refugee camp. Self-report questionnaires were used to assess psychological well-being, symptoms of PTSD, depression, generalized anxiety disorder and insomnia, perceived stress, headache, and perceived fitness. Cardiovascular risk markers were assessed to determine metabolic syndrome, and cardiorespiratory fitness was measured with the Åstrand-Rhyming Test of Maximal Oxygen Uptake.
Results
The prevalence of mental distress and physiological disorders was overall elevated. Only 53.0% of participants rated their psychological well-being as high. Altogether, 35.3% scored above the clinical cut-off for PTSD, 33.3% for depression, 27.9% for generalized anxiety disorder, and 33.8% for insomnia. One in four (28.8%) participants met criteria for metabolic syndrome. While the prevalence of moderate or severe insomnia symptoms and metabolic syndrome differed little from the global population, the risk of being affected by mental distress was markedly increased. In multivariable analysis, higher perceived fitness was associated with higher psychological well-being (OR = 1.35, p = 0.003) and a decreased likelihood for metabolic syndrome (OR = 0.80, p = 0.031). Participants with elevated psychiatric symptoms were less likely to report high psychological well-being (OR = 0.22, p = 0.003) and had increased odds for higher PTSD severity (OR = 3.27, p = 0.034). Increased stress perception was associated with higher PTSD symptoms (OR = 1.13, p = 0.002).
Conclusion
There is an elevated risk for mental distress compared to the global population and an overall high mental and physiological burden among people living in a Greek refugee camp. The findings underpin the call for urgent action. Policies should aim to reduce post-migration stressors and address mental health and non-communicable diseases by various programs. Sport and exercise interventions may be a favorable add-on, given that perceived fitness is associated with both mental and physiological health benefits.
Keywords: prevalence, physical health, non-communicable disease, PTSD, stress, migrant, fitness
Introduction
Human-made conflicts and natural disasters have led to a doubling of forced displacement in the past 10 years, reaching an all-time high of 94.7 million affected people in 2021 (1). These figures will likely continue to grow due to armed conflicts, political oppression and environmental changes (2). Even though most people are internally displaced or find refuge in neighboring countries, forced migration to Europe has more than tripled in the past decade (3). Greece has been one of the main entry points for over 1.2 million forcibly displaced people since 2015, as one of the southernmost countries in Europe and due to its close sea border with Asia (1).
Forcibly displaced people are generally challenged with severe mental and physical strains before, during, and after their flight (4). While infectious diseases and injuries are often treated shortly after arrival, new complaints, such as non-communicable diseases, can arise (2). In addition, ongoing post-migration stressors such as uncertainty about migration status, legal barriers, harsh treatment by authorities, socioeconomic hardship, language barriers, discrimination, social exclusion, limited access to health services, and lack of access to healthy food hinder the recovery from pre-migration trauma and increase the risk of being affected by posttraumatic stress disorder (PTSD) (2, 5). While it has been reported that forcibly displaced people show high levels of resilience (6), the likelihood of being affected with mental and non-communicable diseases is markedly increased compared to the host population (7, 8). A recent meta-analysis (9) documented prevalence rates among forcibly displaced people of 31% for PTSD, 25% for depression, and 14% for generalized anxiety disorders. In addition, a series of physical health complaints have been recorded among forcibly displaced people that can be clustered in the metabolic syndrome and are associated with an increased risk for cardiovascular diseases and diabetes (7, 10). Overall, this double burden of mental and physical comorbidities negatively affects the psychological well-being of individuals and families and drastically reduces life expectancy compared to unaffected counterparts (11). Organized sport and exercise activities have shown promising effects in addressing mental and physical complaints (12). At the same time, these complaints are often accompanied by low fitness levels, whereas low fitness levels may contribute to these physical complaints and, at the same time, also be a cause of mental distress and physiological disorders (13).
Prevalence of mental disorders vary widely across studies with forcibly displaced people, ranging from 2 to 88% for PTSD, 5 to 81% for depression, and 1 to 90% for generalized anxiety disorder (14). While heterogeneity in prevalence can be caused to some extent by methodological differences, the discrepancy could also be attributable to sociodemographic and post-migration differences (15). Therefore, it is important to obtain population and context specific data. A recent call has been made by the World Health Organization (8) for more detailed data to accurately monitor and address the health status of forcibly displaced people. This monitoring should also encompass the conjunction of mental and physical determinants (16). Understanding the specific health needs of forcibly displaced people and their circumstances can provide valuable indicators for targeted programs. Timely addressing individual mental and physical challenges could prevent short- and long-term adverse consequences for forcibly displaced people and the host countries. Since the marked increase of forced migration to Europe in 2015, however, only three studies (17–19) have examined the mental health of forcibly resettled adults in Greece. As these studies focused predominantly on one mental condition, a more comprehensive approach that incorporates mental and physical health parameters is needed.
The present study aims to determine levels of mental distress, physiological disorders, and associated factors among people living in a refugee camp in Greece. Specifically, the study explored the prevalence of mental distress and physiological disorders compared to the global population and examined the association of specific socio-demographic characteristics and clinical parameters with psychological well-being, PTSD symptom severity, and metabolic syndrome to identify risk groups and obtain indications for possible interventions.
Methods
Design and setting
This analysis is part of a larger randomized controlled trial that examines the effects of a sport and exercise intervention on mental health, cardiovascular risk markers, and physical fitness among people living in a refugee camp in Greece (ISRCTN16291983). The sample and the procedures of the present study were based on the sampling and the procedures described in the registration of the project (20). In this paper, we present cross-sectional data from the baseline data assessment. Ethical approval was obtained by the Research Ethics Committee of the University of Thessaly, ref. approval no. 39 and the ethical review board of Northwest and Central Switzerland, ref. approval no. AO_2020–00036.
The study was implemented in a refugee camp in central Greece. The camp was founded in 2016 and can host around 1700 people. At present, the camp operates under the management of an officer appointed by the Ministry of Migration and Asylum and serves as a temporary accommodation center where people wait for their asylum applications to be processed. People live in the camp in containers, which we will refer to as households in this study. While a family has a container for itself, individuals share the container with up to four people of the same sex and origin. The containers are equipped with a bathroom, cooking facilities and air conditioning. At the time of data collection an adult received 150 Euros per month for expenses such as food, clothing, telephone bills, hygiene items, and public transportation. In case of health complaints, a medical center with two medical doctors, nurses and two psychologists from the Greek national health service provided primary health services. The camp is located in a rural area. The nearest village with a small grocery store is 15 min walking distance. A town with an ATM, post office, clothing store, or the possibility to print documents is 16 kilometers away and can be reached by public transportation. While adults are not allowed to engage in paid work due to legal barriers, school-age children can attend public schools.
Based on the data provided by the site management, 1,376 residents lived in this camp in February 2021. Among them, 920 (67%) residents were aged 16 to 59 years, and 39% were women. The forcibly displaced population is diverse in terms of sociodemographic background. Most residents were from Afghanistan (45%) and Syria (25%), whereas the remaining 30% were from West Asian (11%), Sub-Saharan zone (17%), or other (2%) regions.
Participants
Eligible to participate in the study were individuals who (a) lived in the selected refugee camp, (b) were between 16 and 59 years old, (c) were able to read in English, Arabic, Farsi, or French, and (d) provided written informed consent. For ethical reasons, a broad age range was defined as an inclusion criterion, in order to enable as many as possible to participate in the sport and exercise activities of the intervention trial. The site management provided a list of camp residents sorted by language. Based on this list, potentially eligible households were screened for sociodemographic background. Recruitment was done by households to avoid exclusion of individuals from the same household. A random sample stratified by sex was finally drawn from all screened and eligible households. Additional households were drawn in case of non-appearance in order for the parent project to have a sufficient number of participants. A minimum sample size of 136 participants was estimated based on a power analysis to detect an intervention effect on PTSD symptoms (20).
Procedure
The screening, recruitment, and assessment processes were carried out in May 2021. At the beginning of the study, as many households as possible were screened to obtain an overview of the sociodemographic background of the camp population. Residents who were about to participate in the study were asked to provide written informed consent before data collection. Information about the purpose and procedure of the study was provided in writing and verbally. All participants were assured that participation is voluntary and that they could withdraw without any negative consequences, particularly concerning their asylum application. This approach protects participants from potential harm, coercion, and exploitation. However, cultural and language differences may lead to misunderstandings, with false expectations compromising voluntary participation (21). To mitigate such misunderstandings, the study recruited 10 research assistants from the camp residents based on the recommendation of the site management. These research assistants played a critical role in approaching residents, explaining the study, obtaining informed consent, translating, and assisting with data collection.
All measures were taken at the nearby Department of Physical Education and Sport Science of the University of Thessaly due to the availability of necessary facilities and equipment. Participants were informed about their results after the assessment and were referred to a specialist if a health risk was indicated. Participants received further compensation for their participation in the form of a meal and sport equipment. The highlighted measures ensured that the research provided reciprocal benefits for those participating in the study.
Measures
Trained research staff were responsible for the data collection of the outcomes (psychological well-being, PTSD symptom severity, and metabolic syndrome) and predictor variables (sociodemographic background, symptoms of depression, generalized anxiety disorder and insomnia, perceived stress, headache, anemia, cardiorespiratory fitness, and perceived fitness) by following a standard operating procedure. All questionnaires were provided in English, Arabic, Farsi, and French matching the native language background of most participants. Additionally, translators were present during the data assessment when needed. The measures have been previously used with forcibly displaced people (15, 22–28), have been validated in English, Arabic, Farsi, and French (29–50), and had acceptable or good internal consistency (Cronbach’s alpha >0.7) in our pilot study (51). We used clinically relevant cut-offs to determine prevalence rates of mental distress. A growing body of literature emphasizes that self-report symptom-based measures are likely to inflate the prevalence of mental distress in populations of forcibly displaced people (52–54). Therefore, more conservative cut-off values were chosen (36, 40, 43, 55). As the instruments for perceived stress, headache, and perceived fitness are not used for diagnostic purposes, the classification into high and low profiles was done via median split. Information on the sociodemographic background of the participants, including sex, age, origin, educational background, number of relatives in the camp, time fleeing (in months), and time in camp (in months) was collected with a questionnaire.
Mental health
Psychological well-being was assessed with the five-item World Health Organization Well-Being Index (WHO-5), which is specifically designed to measure mental well-being (29). Each of the 5 items is scored on a Likert scale from 0 (at no time) to 5 (all the time). Items were summed up and then multiplied by 4, resulting in an overall index between 0 and 100. Psychological well-being was finally dichotomized in high (>50) and low (≤50) well-being (56).
PTSD symptoms were assessed with the 22-item Impact of Event Scale-Revised (IES-R) (50). The instrument is internationally accepted and not culturally specific. The IES-R items refer to DSM-5 (57) and ICD-10 (58) criteria of PTSD. Items were answered on a five-point Likert scale from 0 (not at all) to 4 (extremely), resulting in an overall index between 0 and 88 points. The cut-off for a possible PTSD diagnosis is set at ≥46 (55).
Depressive symptoms were assessed with the 9-item Patient Health Questionnaire (PHQ-9) (36). Items of this instrument refer to DSM-5 criteria for major depression. Answers were given on a four-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). The overall index varies between 0 and 27. A score of ≥15 indicates moderately severe or severe depressive symptoms (36).
Anxiety symptoms were assessed with the 7-item Generalized Anxiety Disorder scale (GAD-7) (40). The instrument refers to DSM-5 criteria for generalized anxiety disorder. Participants were asked to rate the frequency of anxiety symptoms on a four-point Likert scale from 0 (not at all) to 3 (nearly every day). The overall index ranges from 0 to 21, with a score of ≥15 being interpreted as more severe anxiety levels (40).
Insomnia symptoms were assessed with the Insomnia Severity Index (ISI) (43), a brief screening measure of insomnia and an outcome measure in treatment research, which takes into consideration the criteria for insomnia of the DSM-5. The instrument contains 7 items, which were answered on a five-point Likert scale from 0 (no problem) to 4 (very severe problem). The overall index is scored between 0 and 28. Values of ≥15 indicate possible moderate insomnia (43).
Perceived stress was assessed with the 10-item Perceived Stress Scale (PSS-10) (46). Participants were asked how often they find their lives overwhelming, uncontrollable, and unpredictable on a five-point Likert Scale from 0 (never) to 4 (very often). The score of the positively stated items (4, 5, 7, and 8) is reversed before summing up all items. The overall index ranges from 0 to 40, with higher scores indicating a higher level of perceived stress.
Physical health
Cardiovascular risk markers were assessed to determine metabolic syndrome. A flexible tape was used to determine waist circumference. Systolic and diastolic blood pressure was measured after the participant had rested for 5 min while seated. Blood pressure was measured three times within 5 min with an Omron® digital blood pressure monitor. Evidence for the validity of this device has been reported previously (59). The participants’ finger was pricked once for all (capillary) blood analyzes to collect approximately 10 blood drops. One drop was used for the detection of anemia. Thus, hemoglobin (Hb) levels were measured with a HemoCue® Hb 301 system (HemoCue AB; Ängelholm, Sweden). The incidence of anemia was defined as <120 g/L for women and < 130 g/L for men (60). For the assessment of blood lipids (high-density-lipoprotein cholesterol, fasting plasma triglycerides) and average level of blood glucose over the past 3 months (glycosylated HbA1c), blood samples were analyzed with an Afinion 2 analyzer (Abbott, Wädenswil, Switzerland). One drop of blood was taken by the test strip and read by the analyzer. A good correlation exists between the Abbott 2 point-of-care analyzer results and reference laboratory tests for lipid levels and HbA1c (61, 62).
Cardiovascular risk factors and metabolic syndrome were defined according to the International Diabetes Federation (63). Markers and thresholds include abdominal obesity (waist circumference ≥ 80 cm for women or ≥ 94 cm for men), elevated fasting plasma triglycerides (>150 mg/dL), low HDL-C (<50 mg/dL for women or < 40 mg/dL for men), elevated fasting plasma glucose (>100 mg/dL) and hypertension (>130 mmHg systolic BP or > 85 mmHg diastolic BP). Elevated fasting plasma glucose was replaced with elevated HbA1c (>5.7%) (64). Metabolic syndrome is diagnosed if three or more criteria are fulfilled. The continuous metabolic syndrome score was calculated according to Eisenmann’s method (65). First, we standardized the individual cardiovascular risk markers for sex, age, and origin. Since HDL-C is associated with a reduction in metabolic risk, it was multiplied by−1. Finally, we calculated the sum of the standardized residuals to determine the metabolic syndrome score. A higher score indicates a worse metabolic syndrome profile.
Headache over the last week was measured with the Visual Analog Scale for Pain (VAS) (66). The VAS consists of a 100 mm horizontal line with two extremes 0 mm (no pain) and 100 mm (severe pain). Evidence of the validity of the VAS has been reported previously (67).
Cardiorespiratory fitness
Cardiorespiratory fitness was measured with the (submaximal) Åstrand-Rhyming Indirect Test of Maximal Oxygen Uptake (68), performed on a bicycle ergometer. Maximal oxygen uptake (VO2max) was calculated based on sex, a correction factor for age, body weight, mean steady state, and power output (69). The validity of the Åstrand-Rhyming test for deriving VO2max has been documented previously (70). Sex and age-adjusted cut-offs distinguish between poor and fair or better cardiorespiratory fitness (71).
Perceived fitness was assessed with a 1-item fitness measure from 1 (poor fitness) to 10 (excellent fitness) (72). Previous studies showed that perceived fitness is moderately associated with objective fitness measures (73) and more closely with mental and physical health benefits (72).
Statistical analyzes
Data was double-entered, checked, and merged into a single data file. Outliers were then detected using the Inter Quartile Range. After checking for outliers, one implausible value of 91.9 for cardiorespiratory fitness was removed. The individual mean score was used to impute missing values for calculating the total test score in the self-reported measures. Overall, few data were missing for mental (3%) and physical health (4%). Several missing values were detected for cardiorespiratory fitness (21%), mainly due to knee complaints or injuries. Frequencies (n, %) describe the study sample and prevalence, while mean score (M), standard deviation (SD) and confidence interval (95% CI) outline the severity of the outcome variables across predictors. We performed independent t-tests and chi-square tests to examine whether the final sample differs in the sociodemographic background from the broader screened eligible households. Additionally, chi-square tests were used to examine relationships between primary outcomes and predictors. To determine the association between the outcome and predictor variables, we conducted binary and multiple logistic regressions using the individual odds ratio (95% CI). The level of significance was set at p < 0.05 across all analyzes. Variables were included in multiple logistic regression analyzes when they were associated with the outcome variable at p < 0.10 in binary analysis. To reduce the number of variables in the regression models, we summarized the variables for severe depressive, severe anxiety and moderate insomnia symptoms in a factor termed “psychiatric symptoms.” Psychiatric symptoms were defined as scoring above the cut-off for a possible diagnosis of one or more mental disorders (depression, generalized anxiety disorder or insomnia). Sex, age, and origin were included in the multiple logistic regression models independently of their binary association with the outcome variable to control for sociodemographic background. Multicollinearity was checked after running the whole model. Statistical analyzes were performed with SPSS (Version 24, IBM, Armonk, United States) for both descriptive and inferential analysis.
Results
Sample
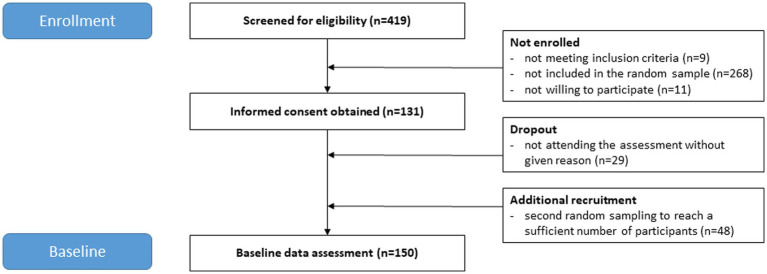
Information on participant flow is provided in Figure 1. The final sample consisted of 150 forcibly displaced individuals (75 female). The overall response rate was 79% (n = 190 invited individuals). Reasons for declining participation included illness, injury, refusal to take the legally required COVID-19 test, or reservations to leave the camp not to miss out on expected feedback from authorities. Characteristics of the study participants are presented in Table 1. The mean age of the total sample was 29.1 years (SD = 9.3). Most study participants were between 16 and 35 years old (n = 113, 79.0%), originated from Afghanistan (n = 79, 52.7%), and lived with one or more family members in the camp (n = 98, 66.2%). Overall, the mean stay in the camp was 14.8 months (SD = 10.2). Noticeable sex differences were the higher number of women without educational qualifications and the low number of university degrees (n = 2, 2.8%) compared to men (n = 18, 25.4%). Furthermore, no man in our sample had to care for a child alone, in contrast to the women (n = 11, 14.9%). After testing for group differences in sociodemographic background (age, origin, education, relatives in camp, time since flight and time in camp), the only difference found was that mean time since flight differed t(382.4) = 2.156, p = 0.032 between screened participants (M = 43.4, SD = 55.2) and the final sample (M = 33.4, SD = 36.5).
Figure 1.
CONSORT flow diagram.
Table 1.
Sociodemographic background of the study participants (n = 150).
| Sociodemographics | Total n (%) | Female n (%) | Male n (%) |
|---|---|---|---|
| Age | |||
| 16–25 | 58 (40.6) | 29 (39.7) | 29 (41.4) |
| 26–35 | 55 (38.5) | 26 (35.6) | 29 (41.4) |
| >35 | 30 (21.0) | 18 (24.7) | 12 (17.1) |
| Origin | |||
| Sub-Sahara Africa | 48 (32.0) | 25 (33.3) | 23 (30.7) |
| Southwest Asia | 102 (68.0) | 50 (66.7) | 52 (69.3) |
| Education | |||
| None | 36 (25.5) | 24 (33.8) | 12 (17.1) |
| Primary | 52 (36.9) | 29 (40.8) | 23 (32.9) |
| High school and above | 53 (37.6) | 18 (25.4) | 35 (50.0) |
| Relatives in camp | |||
| Alone | 50 (33.8) | 18 (24.3) | 32 (43.2) |
| Relatives ≥1 | 98 (66.2) | 56 (75.7) | 42 (56.8) |
| Time since flight (months) | |||
| 0–24 | 62 (48.1) | 32 (50.8) | 30 (45.5) |
| >24 | 67 (51.9) | 31 (49.2) | 36 (54.5) |
| Time in camp (months) | |||
| 0–12 | 71 (51.4) | 37 (53.6) | 34 (49.3) |
| >12 | 67 (48.6) | 32 (46.4) | 35 (50.7) |
Psychological well-being
Summary statistics on psychological well-being across predictor variables are shown in Tables 2, 3. More than half of the participants scored above the cut-off for high psychological well-being. The mean score for psychological well-being was 53.9 (SD = 28.8) across the sample (n = 149, 1 missing). Descriptively, participants who were male, between 26 and 35 years old, or from Sub-Sahara Africa had higher mean scores in psychological well-being. However, differences were not statistically significant. In binary logistic regression analyzes, symptoms of depression, generalized anxiety disorder and insomnia, perceived stress, anemia, headache, and perceived fitness were associated with psychological well-being. There were no associations between psychological well-being, sociodemographic factors, and cardiorespiratory fitness. The results from the multiple logistic regression analysis of psychological well-being regressed on associated factors are shown in Table 4. Sex, age, origin, and all factors that were significantly associated with the outcome in the binary analyzes were included in the final model. In the final model, only psychiatric symptoms and perceived fitness remained significantly associated with psychological well-being. There is strong evidence that psychiatric symptoms were negatively (OR = 0.22, 95% CI 0.08–0.59, p = 0.003) and perceived fitness positively associated (OR = 1.35, 95% CI 1.11–1.63, p = 0.003) with high psychological well-being.
Table 2.
Prevalence of mental distress and physical disorders in comparison with global mean.
| Total % (n) | Female % (n) | Male % (n) | Global mean %b | |
|---|---|---|---|---|
| Mental health | ||||
| High psychological well-being (WHO-5)a | 53.0 (79) | 47.3 (35) | 58.7 (44) | No reference |
| High PTSD symptoms (IES-R)a | 35.3 (53) | 44.0 (33) | 26.7 (20) | 3.9 |
| Severe depressive symptoms (PHQ-9)a | 33.3 (50) | 41.3 (31) | 25.3 (19) | 12.0 |
| Severe anxiety symptoms (GAD-7)a | 27.9 (39) | 38.5 (25) | 18.7 (14) | 16.0 |
| Moderate insomnia symptoms (ISI)a | 33.8 (47) | 37.5 (24) | 30.7 (23) | 33.3 |
| High perceived stress (PSS-10)a | 52.2 (72) | 65.6 (42) | 40.5 (30) | No reference |
| Physical health | ||||
| Metabolic syndromea | 28.8 (40) | 30.0 (21) | 27.5 (19) | 25.0 |
| Abdominal obesitya | 48.0 (71) | 71.2 (52) | 25.3 (19) | 41.5 |
| Dyslipidemiaa | 22.7 (30) | 19.1 (13) | 26.6 (17) | No reference |
| Hypertensiona | 38.9 (58) | 21.6 (16) | 56.0 (42) | 31.1 |
| Prediabetesa | 13.1 (19) | 13.7 (10) | 12.5 (9) | 15.3 |
| Anemiaa | 27.3 (39) | 31.9 (23) | 22.5 (16) | 23.7 |
| High headache (VAS)a | 47.8 (66) | 56.3 (36) | 40.5 (30) | No reference |
| Fitness | ||||
| Fair and higher VO2maxa | 24.6 (29) | 18.9 (10) | 29.2 (19) | No reference |
| High perceived fitnessa | 55.9 (76) | 42.2 (27) | 68.1 (49) | No reference |
aCut-off: WHO-5 (≥50), IES-R (≥46), PHQ-9 (≥15), GAD-7 (≥15), ISI (≥15), PSS-15 (≥median), metabolic syndrome (≥3 out of 5), abdominal obesity (waist circumference ≥ 80 cm for women or ≥ 94 cm for men), dyslipidemia (fasting plasma triglycerides > 150 mg/d and HDL-C < 50 mg/dL for women or < 40 mg/dL for men), hypertension (>130 mmHg systolic BP or > 85 mmHg diastolic BP), prediabetes (HbA1c = 5.7–6.4%), anemia (women < 120 g/L or men < 130 g/L), VAS (≥median), VO2max [based on ACSM guidelines (71)], perceived fitness (≥median).
bAccording to the literature (74–81).
Table 3.
Descriptive statistics of psychological well-being (WHO-5) dichotomized into high vs. low well-being.
| Index Score | High (≥50) | Low (<50) | χ 2 | |
|---|---|---|---|---|
| M (95% CI) | n (%) | n (%) | ||
| Sociodemographics | ||||
| Sex | 0.164 | |||
| Female | 50.7 (43.9–57.5) | 35 (47.3) | 39 (52.7) | |
| Male | 57.0 (50.5–63.5) | 44 (58.7) | 31 (41.3) | |
| Age | 0.174 | |||
| 16–25 | 51.3 (43.9–58.7) | 30 (51.7) | 28 (48.3) | |
| 26–35 | 59.2 (51.3–67.1) | 33 (61.1) | 21 (38.9) | |
| >35 | 47.2 (36.6–57.7) | 12 (40.0) | 18 (60.0) | |
| Origin | 0.073 | |||
| Sub-Sahara Africa | 57.6 (48.8–66.5) | 30 (63.8) | 17 (36.2) | |
| Southwest Asia | 52.1 (46.6–57.7) | 49 (48.0) | 53 (52.0) | |
| Education | 0.828 | |||
| None | 54.6 (44.4–64.7) | 18 (50.0) | 18 (50.0) | |
| Primary | 51.0 (43.0–58.9) | 25 (49.0) | 26 (51.0) | |
| High school and above | 53.3 (45.7–60.8) | 29 (54.7) | 24 (45.3) | |
| Relatives in camp | 0.149 | |||
| Alone | 55.7 (46.9–64.5) | 31 (62.0) | 19 (38.0) | |
| Relatives ≥1 | 53.7 (48.1–59.2) | 48 (49.5) | 49 (50.5) | |
| Time since flight (months) | 0.358 | |||
| 0–24 | 55.1 (47.7–62.5) | 35 (57.4) | 26 (42.6) | |
| >24 | 51.9 (45.1–58.8) | 33 (49.3) | 34 (50.7) | |
| Time in camp (months) | 0.673 | |||
| 0–12 | 52.2 (45.8–58.7) | 37 (52.9) | 33 (47.1) | |
| >12 | 52.6 (45.2–59.9) | 33 (49.3) | 34 (50.7) | |
| Mental health | ||||
| Severe depressive symptoms (PHQ-9)a | <0.001 | |||
| Yes | 35.7 (29.5–41.9) | 11 (22.4) | 38 (77.6) | |
| No | 62.8 (57.2–68.3) | 68 (68.0) | 32 (32.0) | |
| Severe anxiety symptoms (GAD-7)a | <0.001 | |||
| Yes | 33.9 (27.3–40.5) | 8 (20.5) | 31 (79.5) | |
| No | 58.5 (52.9–64.1) | 61 (61.0) | 39 (39.0) | |
| Moderate insomnia symptoms (ISI)a | <0.001 | |||
| Yes | 38.9 (31.8–46.1) | 12 (26.1) | 34 (73.9) | |
| No | 57.4 (51.6–63.3) | 56 (60.9) | 36 (39.1) | |
| High perceived stress (PSS-10)a | <0.001 | |||
| Yes | 43.4 (37.4–49.4) | 26 (36.6) | 45 (63.4) | |
| No | 59.5 (52.3–66.6) | 41 (62.1) | 25 (37.9) | |
| Physical health | ||||
| Anemiaa | 0.047 | |||
| Yes | 48.9 (39.0–58.8) | 16 (41.0) | 23 (59.0) | |
| No | 57.0 (51.6–62.5) | 62 (59.6) | 42 (40.4) | |
| High headache (VAS)a | 0.072 | |||
| Yes | 45.7 (38.9–52.5) | 27 (41.5) | 38 (58.5) | |
| No | 56.4 (49.8–63.1) | 41 (56.9) | 31 (43.1) | |
| Fitness | ||||
| VO2maxa | 0.991 | |||
| Fair and above | 57.8 (46.2–69.4) | 16 (55.2) | 13 (44.8) | |
| Poor and below | 52.0 (46.2–57.8) | 49 (55.1) | 40 (44.9) | |
| High perceived fitnessa | <0.001 | |||
| Yes | 60.0 (53.6–66.4) | 48 (63.2) | 28 (36.8) | |
| No | 39.1 (33.0–45.1) | 18 (30.5) | 41 (69.5) | |
aCut-off: PHQ-9 (≥15), GAD-7 (≥15), ISI (≥15), PSS-10 (≥median), VAS (≥median), anemia (women ≤ 120 g/L or men ≤ 130 g/L), VO2max [based on ACSM guidelines (71)], perceived fitness (≥median).
Table 4.
Logistic models of high psychological well-being (WHO-5), high PTSD symptoms (IES-R), and metabolic syndrome regressed on sex, age, origin, and associated factors.
| Model high psychological well-being (≥50)a | Model high PTSD symptoms (≥46)b | Model metabolic syndrome (≥3 out of 5)c | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Sociodemographics | |||||||||
| Sex | |||||||||
| Female | Reference | Reference | Reference | ||||||
| Male | 0.88 | (0.32–2.45) | 0.802 | 0.77 | (0.29–2.07) | 0.608 | 3.27 | (0.90–11.97) | 0.073 |
| Age | 1.00 | (0.95–1.05) | 0.916 | 1.00 | (0.95–1.05) | 0.951 | 1.02 | (0.96–1.09) | 0.496 |
| Origin | |||||||||
| Sub-Sahara Africa | Reference | Reference | Reference | ||||||
| Southwest Asia | 0.76 | (0.28–2.12) | 0.604 | 1.99 | (0.48–8.29) | 0.345 | 4.02 | (1.02–15.77) | 0.046 |
| Relatives in camp | |||||||||
| Alone | Reference | ||||||||
| Relatives 1 ≤ | 0.70 | (0.17–2.91) | 0.623 | ||||||
| Mental health | |||||||||
| Psychiatric symptomsd | |||||||||
| No | Reference | Reference | |||||||
| Yes | 0.22 | (0.08–0.59) | 0.003 | 3.27 | (1.10–9.74) | 0.034 | |||
| Perceived stress (PSS-10) | 1.00 | (0.93–1.06) | 0.923 | 1.13 | (1.05–1.23) | 0.002 | |||
| Physical health | |||||||||
| Hemoglobin | 1.02 | (0.99–1.06) | 0.184 | ||||||
| Headache | 1.00 | (0.98–1.02) | 0.977 | 1.01 | (1.00–1.03) | 0.136 | |||
| Fitness | |||||||||
| VO2max | 0.92 | (0.86–0.99) | 0.021 | ||||||
| Perceived fitness | 1.35 | (1.11–1.63) | 0.003 | 0.93 | (0.76–1.13) | 0.453 | 0.80 | (0.65–0.98) | 0.031 |
| Nagelkerkes R2 | 0.36 | 0.47 | 0.20 | ||||||
aIncludes the variables sex, age, origin, psychiatric symptoms, perceived stress, hemoglobin, headache and perceived fitness.
bIncludes the variables sex, age, origin, relatives in camp, psychiatric symptoms, perceived stress, headache and perceived fitness.
cIncludes the variables sex, age, origin, VO2max and perceived fitness.
dPsychiatric symptoms is defined as having elevated symptoms in one or more mental disorder: PHQ-9 (≥15), GAD-7 (≥15), or ISI (≥15).
Mental distress
The prevalence of mental distress and high PTSD symptoms across sociodemographic and clinical variables are shown in Tables 2, 5. One out of three participants scored above the clinical cut-off for PTSD, depression, generalized anxiety disorder, and insomnia. Fifty-five (39.8%) participants had considerably elevated symptoms in at least one or more psychiatric disorders. The mean severity score for PTSD was 34.6 (SD = 22.4) in the whole sample (n = 150). Higher PTSD scores were found in female participants aged older than 35 years, originating from Southwest Asia, or living with one or more relatives in the camp. Notably, sex, origin, and living with one or more relatives in the camp were significantly associated with PTSD symptoms in binary logistic regression analyzes besides symptoms of depression, generalized anxiety disorder and insomnia, perceived stress, headache, and perceived fitness. On the contrary, education, time spent in the camp, anemia, and cardiorespiratory fitness were not associated with PTSD symptom severity. The final model of the multiple logistic regression analysis, including age and all associated factors from binary analyzes, is presented in Table 4. In the final model, psychiatric symptoms (OR = 3.27, 95% CI 1.10–9.74, p = 0.034) and perceived stress (OR = 1.13, 95% CI 1.05–1.23, p = 0.002) were associated with the occurrence of high PTSD severity.
Table 5.
Descriptive statistics of PTSD (IES-R) dichotomized into high vs. low PTSD symptom severity.
| Index Score | High (≥46) | Low (<46) | χ 2 | |
|---|---|---|---|---|
| M (95% CI) | n (%) | n (%) | ||
| Sociodemographics | ||||
| Sex | 0.026 | |||
| Female | 39.0 (33.8–44.1) | 33 (44.0) | 42 (56.0) | |
| Male | 30.3 (25.3–35.4) | 20 (26.7) | 55 (73.3) | |
| Age | 0.379 | |||
| 16–25 | 31.6 (25.6–37.6) | 17 (29.3) | 41 (70.7) | |
| 26–35 | 36.2 (30.8–41.6) | 23 (41.8) | 32 (58.2) | |
| >35 | 39.1 (29.8–48.3) | 11 (36.7) | 19 (63.3) | |
| Origin | 0.011 | |||
| Sub-Sahara Africa | 29.3 (23.0–35.4) | 10 (20.8) | 38 (79.2) | |
| Southwest Asia | 37.2 (32.8–41.6) | 43 (42.2) | 59 (57.8) | |
| Education | 0.107 | |||
| None | 36.8 (29.6–43.9) | 14 (38.9) | 22 (61.1) | |
| Primary | 39.1 (32.5–45.6) | 24 (46.2) | 28 (53.8) | |
| High school and above | 31.6 (25.7–37.5) | 14 (26.4) | 39 (73.6) | |
| Relatives in camp | 0.012 | |||
| Alone | 28.7 (22.9–34.4) | 11 (22.0) | 39 (78.0) | |
| Relatives ≥1 | 37.9 (33.3–42.5) | 42 (42.9) | 56 (57.1) | |
| Time since flight (months) | 0.743 | |||
| 0–24 | 34.8 (29.3–40.4) | 23 (37.1) | 39 (62.9) | |
| >24 | 34.7 (29.3–40.2) | 23 (34.3) | 44 (65.7) | |
| Time in camp (months) | 0.933 | |||
| 0–12 | 36.0 (30.9–41.2) | 26 (36.6) | 45 (63.4) | |
| >12 | 35.7 (30.1–41.2) | 25 (37.3) | 42 (62.7) | |
| Mental health | ||||
| Severe depressive symptoms (PHQ-9)a | <0.001 | |||
| Yes | 49.8 (44.2–55.5) | 33 (66.0) | 17 (34.0) | |
| No | 27.1 (23.2–31.0) | 20 (20.0) | 80 (80.0) | |
| Severe anxiety symptoms (GAD-7)a | <0.001 | |||
| Yes | 56.1 (50.9–61.4) | 29 (74.4) | 10 (25.6) | |
| No | 28.0 (24.1–31.9) | 24 (23.8) | 77 (76.2) | |
| Moderate insomnia symptoms (ISI)a | <0.001 | |||
| Yes | 50.4 (44.9–55.9) | 29 (61.7) | 18 (38.3) | |
| No | 28.6 (24.3–32.9) | 24 (26.1) | 68 (73.9) | |
| High perceived stress (PSS-10)a | <0.001 | |||
| Yes | 46.5 (41.7–51.2) | 43 (59.7) | 29 (40.3) | |
| No | 25.0 (20.1–30.0) | 10 (15.2) | 56 (84.8) | |
| Physical health | ||||
| Anemiaa | 0.226 | |||
| Yes | 39.1 (31.5–46.7) | 17 (43.6) | 22 (56.4) | |
| No | 33.7 (29.5–37.9) | 34 (32.7) | 70 (67.3) | |
| High headache (VAS)a | <0.001 | |||
| Yes | 45.9 (40.3–51.4) | 37 (56.1) | 29 (43.9) | |
| No | 27.0 (22.5–31.4) | 16 (22.2) | 56 (77.8) | |
| Fitness | ||||
| VO2max a | 0.138 | |||
| Fair and above | 31.9 (24.2–39.6) | 7 (24.1) | 22 (75.9) | |
| Poor and below | 35.4 (30.5–40.3) | 35 (39.3) | 54 (60.7) | |
| High perceived fitnessa | 0.019 | |||
| Yes | 31.1 (26.2–36.1) | 23 (30.3) | 53 (69.7) | |
| No | 42.8 (37.1–48.6) | 30 (50.0) | 30 (50.0) | |
aCut-off: PHQ-9 (≥15), GAD-7 (≥15), ISI (≥15), PSS-10 (≥median), VAS (≥median), anemia (women ≤ 120 g/L or men ≤ 130 g/L), VO2 max [based on ACSM guidelines (71)], perceived fitness (≥median).
Physical health
The summary statistics on the prevalence of cardiovascular risk factors, anemia, high level of headache, and metabolic syndrome across predictors are shown in Tables 2, 6. Every fourth participant (n = 139, 11 missing) met the inclusion criteria for metabolic syndrome, and three out of four women scored above the cut-off for abdominal obesity. Apart from age, cardiorespiratory and perceived fitness, no other factor was associated with metabolic syndrome in the binary analyzes. The results of the final multiple logistic regression model are presented in Table 4. After including sex, origin, and all associated factors in the regression, only origin, cardiorespiratory and perceived fitness remained significantly associated with metabolic syndrome. Individuals from Southwest Asia (OR = 4.02, 95% CI 1.02–15.77, p = 0.046) were more likely to be affected with metabolic syndrome, whereas participants with higher levels of objectively measured (OR = 0.92, 95% CI 0.86–0.99, p = 0.021) and subjectively perceived fitness (OR = 0.80, 95% CI 0.65–0.98, p = 0.031) were less likely to be affected with metabolic syndrome.
Table 6.
Descriptive statistics of metabolic syndrome dichotomized into present vs. absent metabolic syndrome.
| Index scoreb | Yes (≥3 out of 5) | No (<3 out of 5) | χ 2 | |
|---|---|---|---|---|
| M (95% CI) | n (%) | n (%) | ||
| Sociodemographics | ||||
| Sex | 0.748 | |||
| Female | 0.05 (−0.66–0.76) | 21 (30.0) | 49 (70.0) | |
| Male | 0.16 (−0.47–0.78) | 19 (27.5) | 50 (72.5) | |
| Age | 0.001 | |||
| 16–25 | 0.50 (−0.16–1.16) | 9 (17.0) | 44 (83.0) | |
| 26–35 | −0.33 (−0.99–0.32) | 14 (26.9) | 38 (73.1) | |
| >35 | 0.20 (−1.27–1.66) | 15 (55.6) | 12 (44.4) | |
| Origin | 0.171 | |||
| Sub-Sahara Africa | −0.06 (−0.89–0.77) | 9 (20.9) | 34 (79.1) | |
| Southwest Asia | 0.16 (−0.41–0.73) | 31 (32.9) | 65 (67.7) | |
| Education | 0.185 | |||
| None | −0.12 (−0.95–0.72) | 6 (17.1) | 29 (82.9) | |
| Primary | 0.00 (−0.90–0.89) | 13 (27.7) | 34 (72.3) | |
| High school and above | 0.32 (−0.44–1.08) | 17 (35.4) | 31 (64.6) | |
| Relatives in camp | 0.582 | |||
| Alone | 0.37 (−0.41–1.16) | 12 (25.5) | 35 (74.5) | |
| Relatives ≥1 | 0.02 (−0.58–0.61) | 27 (30.0) | 63 (70.0) | |
| Time since flight (months) | 0.994 | |||
| 0–24 | 0.10 (−0.63–0.83) | 14 (25.5) | 41 (74.5) | |
| >24 | 0.09 (−0.59–0.76) | 16 (25.4) | 47 (74.6) | |
| Time in camp (months) | 0.209 | |||
| 0–12 | −0.19 (−0.84–0.47) | 20 (31.7) | 43 (68.3) | |
| >12 | 0.30 (−0.43–1.02) | 14 (21.9) | 50 (78.1) | |
| Mental health | ||||
| Severe depressive symptoms (PHQ-9)a | 0.271 | |||
| Yes | −0.03 (−0.89–0.83) | 16 (34.8) | 30 (65.2) | |
| No | 0.17 (−0.40–0.74) | 24 (25.8) | 69 (74.2) | |
| Severe anxiety symptoms (GAD-7)a | 0.074 | |||
| Yes | 0.18 (−0.82–1.18) | 15 (40.5) | 22 (59.5) | |
| No | 0.05 (−0.53–0.62) | 23 (24.7) | 70 (75.3) | |
| Moderate insomnia symptoms (ISI)a | 0.165 | |||
| Yes | 0.34 (−0.41–1.10) | 16 (36.4) | 28 (63.6) | |
| No | −0.12 (−0.77–0.52) | 21 (24.7) | 64 (75.3) | |
| High perceived stress (PSS-10)a | 0.961 | |||
| Yes | −0.22 (−0.94–0.49) | 19 (27.9) | 49 (72.9) | |
| No | 0.32 (−0.36–1.01) | 17 (28.3) | 43 (71.7) | |
| Physical health | ||||
| Anemiaa | 0.485 | |||
| Yes | 0.04 (−1.01–1.10) | 9 (24.3) | 28 (75.7) | |
| No | 0.12 (−0.41–0.65) | 31 (30.4) | 71 (69.6) | |
| High headache (VAS)a | 0.674 | |||
| Yes | −0.13 (−0.87–0.62) | 19 (30.6) | 43 (69.4) | |
| No | 0.25 (−0.41–0.91) | 18 (27.3) | 48 (72.7) | |
| Fitness | ||||
| VO2maxa | 0.005 | |||
| Fair and above | −0.61 (−1.52–0.30) | 1 (3.7) | 26 (96.3) | |
| Poor and below | 0.13 (−0.41–0.68) | 25 (30.1) | 58 (69.9) | |
| High perceived fitnessa | 0.044 | |||
| Yes | −0.35 (−0.92–0.23) | 15 (20.8) | 57 (79.2) | |
| No | 0.48 (−0.37–1.33) | 20 (37.0) | 34 (63.0) | |
aCut-off: PHQ-9 (≥15), GAD-7 (≥15), ISI (≥15), PSS-10 (≥median), VAS (≥median), anemia (women ≤ 120 g/L or men ≤ 130 g/L), VO2 max [based on ACSM guidelines (71)], perceived fitness (≥median).
bIndex score is composed of continuous metabolic syndrome score.
Discussion
This study extends existing findings on health challenges of forcibly displaced people by assessing the psychological well-being, PTSD symptom severity, metabolic syndrome, and associated factors among people living in a refugee camp in Greece.
Only half of the study participants rated their psychological well-being as high. In comparison, forcibly displaced adults resettled in Sweden scored 7.1% (M = 57.7, SD = 27.1), and the broader population in Greece during the first year of the COVID-19 pandemic 23.4% (M = 66.5, SD = 22.7) higher (82, 83). Moreover, consistent with previous findings (7, 9, 10, 14, 53, 84, 85), there is a considerably elevated prevalence of mental and physical distress among forcibly displaced people in Greece. Compared to the global mean (74–81), the risk of being affected by PTSD is nine, depression three, and generalized anxiety disorder one and a half times higher among forcibly displaced people. No difference in prevalence was found for moderate or severe insomnia symptoms, metabolic syndrome, abdominal obesity, hypertension, prediabetes, and anemia. Our findings stand in contradiction to a recent large-scale study (86), which collected data at health clinics in Southern European reception centers and reported a prevalence of 0.7% for PTSD and 5.7% for cardiovascular disease. As highlighted by the authors, the discrepant results may be explained by an inadequate recording of health conditions by health professionals. In addition, low mental health help-seeking behavior has been found in this population. Constrained health services, limited health literacy, lack of trust in authorities or cultural barriers such as mental health stigmas could have discouraged individuals from voluntarily seeking a health check and lead to a higher number of unreported cases (87). Another reason for the conflicting results might be the different sociodemographic background of the participants, who, in contrast to our study, were predominantly male (77.7%) and without relatives in the camp (80.3%).
Forcibly displaced people represent a heterogeneous group with different personal traits, sociodemographic backgrounds, and lived experiences. Therefore, the question arises if individuals with specific characteristics are more strongly affected by certain conditions than others. Subgroup analyzes did not identify a specific target group with high mental well-being. However, female Southwest Asian people living with family members in the camp had higher PTSD symptom scores. The differences between sexes have been explained in previous studies (9, 84, 88), with women being at higher risk of sexual violence, childcare pressures, and exploitation. Unlike other results (89), being together with a family member was associated with higher PTSD symptom scores in our sample. This finding may be surprising, as social support has been shown to have a buffering effect against PTSD (90). Possible explanations for this could be that the family does not necessarily provide social support in the face of family conflict and violence (5). Moreover, caring for the whole family can pose an additional challenge and may trigger negative mental states. The life experience that caused the entire family to flee their country rather than as individuals may also explain the difference. However, these remain assumptions and should be further investigated in larger studies with increased statistical power and additional qualitative methods to identify subgroup differences and possible rationales.
Regarding cardiovascular risk factors, older age and origin from Southwest Asia were associated with metabolic syndrome. Similarly, a recent meta-analysis (10) reported a higher risk of cardiovascular disease among older forcibly displaced adults from the Middle East. The elevated risk has been attributed to psychological stress and acculturation processes such as changes in lifestyle and diet (7, 8). In our study, neither psychiatric symptoms nor time spent in the camp were associated with the occurrence of metabolic syndrome. The difference may be due to the fact that the two studies examined migrating populations in general and not exclusively forcibly displaced people who spent a shorter time in the host country. Living in the camp instead of within society may also have led to no or limited acculturation processes. Furthermore, the prevalence of the metabolic syndrome is generally significantly higher in the Eastern Mediterranean Region (91), suggesting that the increased risk is more related to the risk profile of the region of origin than to the specific experience of forced displacement. Overall, the associations between sociodemographic background and mental and physiological outcomes, except for Asian origin, lose statistical significance in multivariable analyzes when the clinical factors are considered.
When living in a precarious situation, time itself does not seem to support recovery from PTSD symptom severity. To date, the mitigating effect of time on PTSD is controversially discussed and ranges from improvement to no effect till exacerbation of PTSD symptomatology (85, 86, 90). Different exposure to post-migration living difficulties could explain the contrasting results. In our study, perceived stress was associated with the occurrence of higher PTSD symptoms, while no relationship between the length of stay and PTSD symptoms was detected. These observations support recent findings (92) that post-migration stressors maintain the severity of PTSD symptoms. The decisive factors are ongoing daily stressors, especially lengthy asylum procedures, uncertain visa status, detention in refugee camps, or legal barriers to work (93).
Particularly noteworthy is that people who perceived their fitness level as higher had better overall health scores. Surprisingly, this did not apply to objectively measured cardiorespiratory fitness, which was associated only with metabolic syndrome. The association between perceived fitness and psychological well-being and metabolic syndrome remained statistically significant after controlling for confounding factors. This suggests that mental health is more closely associated with an individual’s perceived subjective fitness than objective fitness measurement. As such, the process of meaning-making in relation to personal fitness appears to be of particular importance. Our findings add to the small body of knowledge, suggesting that perceived fitness is associated with both mental and physical health benefits (72, 94), pointing out that cognitive factors should be taken into account when studying the effect of sport and exercise activities implemented in a refugee camp. Importantly in the context of a refugee camp, perceived fitness was more strongly associated with psychological functioning and daily coping than cardiorespiratory fitness in a sample of psychology students (73). Furthermore, participants with high perceived fitness scored lower on insomnia, perceived higher sleep quality, and ruminated less about unresolved problems than participants who rated their fitness low (95). This last point requires particular attention because “thinking too much” expresses emotional and cognitive distress in certain Sub-Saharan and Southwest Asian cultures. For forcibly displaced people in a protracted situation, repetitive negative thinking can exacerbate psychological, physical, and social symptoms (96). People with high perceived fitness may be less affected by the cognitive loop about current life situations and past events, which may lead to higher overall well-being.
In line with the current findings of an increased risk for mental distress compared to the global population and the overall high prevalence of mental and physiological distress among people living in a refugee camp in Greece, organizations on-site criticize the lack of early measures (97). The lack of prevention or early treatment favors the development or consolidation of mental disorders and undermines the achievement of the health-related United Nations Sustainable Development Goals by 2030. Based on the results of this and previous studies (4, 5, 15, 92, 93), policies are urgently needed to reduce post-migration stressors and prevent mental health deterioration in Greek refugee camps. Prevention should be of priority, complemented by targeted programs to address population-based health needs and psychological well-being. The extent of diverse health needs and the heterogeneous composition of the population suggests that general health support should go beyond medical treatment and include a set of complementary measures to balance health inequities. These include access to education, a perspective on economic independence, social services, community capacity strengthening, health literacy promotion, and psychosocial activities. In light of the present findings, organized sport and exercise activities might be a favorable add-on intervention to address mental and physiological health.
While sport and exercise activities have successfully been implemented to address mental and physical health (12, 98–100), evidence for similar effects among forcibly displaced people is scarce (101). As these are substantially different contexts, future studies need to investigate the effect and feasibility of regular sport and exercise activities on mental and physiological health among people living in refugee camps. In addition, this study’s results raise the question of whether improvements in perceived fitness are associated with improvements in mental and physical health and, which and how activities should be implemented to address perceived fitness.
Strengths and limitations
This study has certain strengths, such as providing a comprehensive perspective of health and its associated factors among forcibly displaced people living in a refugee camp in Greece. Given the recent developments in forcible displacement and since Greece is one of the main entry points in Europe, an essential contemporary context was studied. Furthermore, we addressed a population that is difficult to reach due to challenging living situations and restricted camp access. Our study is, to our knowledge, one of the first which examines the association of perceived fitness and mental and physiological health among forcibly displaced people within a refugee camp context. Lastly, the study applied methodological rigorousness by following a pre-registered study protocol (20). The shortage of sex-specific results (88) and the barriers to accessing health services, in particular mental health (87), was addressed by a random and stratified sample by sex, including the most represented ethnic groups in the camp.
Limitations include the cross-sectional nature of the present data and the small-to-moderate sample size, increasing the risk that minor associations were overseen. On the other hand, multiple testing might have increased the occurrence of Type I errors. Despite an acceptable response rate, one might assume that selection bias influenced the results. However, when analyzing group differences, only time since flight differed statistically significantly from the broader screened camp population. Generalizability to other settings might be limited, as post-migration life circumstances differ from context to context and significantly impact overall health (4). Expanding the study to other camps, particularly those on the Greek islands, which have been described as more restrictive (97), could therefore provide valuable insights to complement our findings. A key finding of the study was that cardiorespiratory fitness, unlike perceived fitness, was not associated with mental health outcomes. The considerable amount of missing values for cardiorespiratory fitness may have affected this finding. Moreover, recent literature suggests that self-report symptom-based measures tend to overestimate the prevalence of mental distress (52–54). This may also be caused by participants indicating higher initial values in the hope that this will positively influence their asylum procedure (89). These circumstances were addressed by information about study intentions and the use of more conservative, clinically relevant cut-offs. Validated instruments widely used in different cultural contexts have been implemented, though none have been developed explicitly for cross-cultural use (84). The universality of Western-based classification systems to describe mental distress in other contexts is accordingly questioned by some authors (52, 53, 84). Similarly, population-specific cut-offs for cardiovascular risk factors have been recommended (102). The International Diabetes Federation advocates ethnicity-specific cut-offs for central obesity (63). To date, however, these are not available for Sub-Saharan and Eastern Mediterranean populations. Instead, European reference values had to be used, which might lead to inaccuracies in our results.
Conclusion
The findings of this study underpin the call for urgent action to address the health needs of people living in refugee camps in Greece. Compared to the global population, forcibly displaced people in Greece have a considerably higher risk of being affected by mental distress. The prevalence of moderate or severe insomnia symptoms and physiological disorders is likewise elevated. However, they do not differ from the global mean. Therefore, the first priority should be to prevent the deterioration of health conditions by reducing post-migration stress. Second, population-centered programs must be developed to address mental health and non-communicable diseases. Sport and exercise programs could be a favorable adjunct, as perceived fitness, as a potentially protective factor, is associated with mental and physiological health benefits.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Research Ethics Committee of the University of Thessaly. The patients/participants provided their written informed consent to participate in this study.
Author contributions
AH, IM, and MG supervised the study. FK and KF coordinated the fieldwork. FK analyzed the data and drafted the initial manuscript. KF, AH, IM, ET, EH, HS, FC, SL, MM, DQ, YT, RK, UP, and MG contributed to revising and editing the final manuscript. All authors were involved in the design of the study or contributed to the refinement of methods and read and approved the final manuscript.
Funding
This study was partly funded by the Swiss Network for International Studies (SNIS). The funding source had no influence on the design of the study, the collection, management, analysis, and interpretation of the data, the writing of the manuscript, or on the selection of the journal.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors sincere thanks go to the research assistants from the camp community, who have substantially enriched the project with their commitment. The authors would also like to thank everyone who made the effort to participate in the study. The authors would further like to thank the motivated students from the universities of Thessaly and Basel, whose efforts contributed to the study’s success. The authors acknowledge the administrative, logistical, and financial support from the universities involved in this study as well Maria Katapodi and Ina Sonego for their critical review. Finally, the authors thank the Ministry of Migration and Asylum and the camp manager who granted access to the camp for the realization of the study.
Glossary
Abbreviations
- 95% CI
95% Confidence interval
- BMI
Body mass index; BP: Blood pressure
- DSM-5
Diagnostic and Statistical Manual of Mental Disorders (5th edition)
- GAD-7
Generalized Anxiety Disorder scale (7-item version)
- Hb
Hemoglobin
- HbA1c
Glycated hemoglobin
- HDL-C
High-density lipoprotein cholesterol
- ICD-10
International Classification of Diseases (10th version)
- IES-R
Impact of Event Scale-Revised; ISI: Insomnia Severity Index
- ISRCTN
trial registry Primary clinical trial registry recognized by the WHO and ICMJE
- M: Mean
OR: Odds ratio
- PHQ-9
Patient Health Questionnaire (9-item version)
- PSS-10
Perceived Stress Scale (10-item version)
- PTSD
Post-traumatic stress disorder
- SD
Standard deviation
- SPSS
Statistical Package for the Social Sciences
- VAS
Visual analog scale
- VO2max (ml/kg/min)
Maximal oxygen uptake
- WHO
World Health Organization
- WHO-5
5-item World Health Organization Well-Being Index
References
- 1.United Nations High Commissioner for Refugees . Global report: The stories behind the numbers. (2021). Available at: https://www.unhcr.org/the-global-report.html. (Accessed 6 Jan 2023).
- 2.Matlin SA, Depoux A, Schütte S, Flahault A, Saso L. Migrants’ and refugees’ health: towards an agenda of solutions. Public Health Rev. (2018) 39:27. doi: 10.1186/s40985-018-0104-9 [DOI] [Google Scholar]
- 3.United Nations High Commissioner for Refugees . Global trends: a year of crises. (2011). Available at: https://www.unhcr.org/statistics/country/4fd6f87f9/unhcr-global-trends-2011.html. (Accessed Jan 6, 2023).
- 4.Miller KE, Rasmussen A. The mental health of civilians displaced by armed conflict: an ecological model of refugee distress. Epidemiol Psychiatr Sci. (2017) 26:129–38. doi: 10.1017/S2045796016000172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kiselev N, Pfaltz M, Schick M, Bird M, Pernille H, Sijbrandij M, et al. Problems faced by Syrian refugees and asylum seekers in Switzerland. Swiss Med Wkly. (2020) 150:w20381. doi: 10.4414/smw.2020.20381 [DOI] [PubMed] [Google Scholar]
- 6.Hynie M. The social determinants of refugee mental health in the post-migration context: a critical review. Can J Psychiatr. (2018) 63:297–303. doi: 10.1177/0706743717746666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenthal T, Touyz RM, Oparil S. Migrating populations and health: risk factors for cardiovascular disease and metabolic syndrome. Curr Hypertens Rep. (2022) 24:325–40. doi: 10.1007/s11906-022-01194-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . World report on the health of refugees and migrants. (2022). Available at: https://www.who.int/publications/i/item/9789240054462. (Accessed Jan 6, 2023).
- 9.Mesa-Vieira C, Haas AD, Buitrago-Garcia D, Roa-Diaz ZM, Minder B, Gamba M, et al. Mental health of migrants with pre-migration exposure to armed conflict: a systematic review and meta-analysis. Lancet Public Health. (2022) 7:e469–81. doi: 10.1016/S2468-2667(22)00061-5 [DOI] [PubMed] [Google Scholar]
- 10.Al-Rousan T, AlHeresh R, Saadi A, El-Sabrout H, Young M, Benmarhnia T, et al. Epidemiology of cardiovascular disease and its risk factors among refugees and asylum seekers: systematic review and meta-analysis. Int J Cardiol Cardiovasc Risk Prev. (2022) 12:200126. doi: 10.1016/j.ijcrp.2022.200126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiat. (2015) 72:334–41. doi: 10.1001/jamapsychiatry.2014.2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. (2015) 25:1–72. doi: 10.1111/sms.12581 [DOI] [PubMed] [Google Scholar]
- 13.Nilsson H, Gustavsson C, Gottvall M, Saboonchi F. Physical activity, post-traumatic stress disorder, and exposure to torture among asylum seekers in Sweden: a cross-sectional study. BMC Psychiatry. (2021) 21:452. doi: 10.21203/rs.3.rs-274063/v1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morina N, Akhtar A, Barth J, Schnyder U. Psychiatric disorders in refugees and internally displaced persons after forced displacement: a systematic review. Front Psych. (2018) 9:433. doi: 10.3389/fpsyt.2018.00433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malm A, Tinghög P, Narusyte J, Saboonchi F. The refugee post-migration stress scale (RPMS) - development and validation among refugees from Syria recently resettled in Sweden. Confl Heal. (2020) 14:2. doi: 10.1186/s13031-019-0246-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization . Constitution of the World Health Organization. (1946). Available at: https://www.who.int/about/governance/constitution. (Accessed Jan 6, 2023).
- 17.Poole DN, Hedt-Gauthier B, Liao S, Raymond NA, Bärnighausen T. Major depressive disorder prevalence and risk factors among Syrian asylum seekers in Greece. BMC Public Health. (2018) 18:908. doi: 10.1186/s12889-018-5822-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Theofanidis D, Karavasileiadou S, Almegewly WH. Post-traumatic stress disorder among Syrian refugees in Greece. Front Psych. (2022) 13:911642. doi: 10.3389/fpsyt.2022.911642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ben Farhat J, Blanchet K, Juul Bjertrup P, Veizis A, Perrin C, Coulborn RM, et al. Syrian refugees in Greece: experience with violence, mental health status, and access to information during the journey and while in Greece. BMC Med. (2018) 16:40. doi: 10.1186/s12916-018-1028-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gerber M, Colledge F, de Quervain D, Filippou K, Havas E, Knappe F, et al. Effects of an exercise and sport intervention among refugees living in a Greek refugee camp on mental health, physical fitness and cardiovascular risk markers: study protocol for the SALEEM pragmatic randomized controlled trial. Trials. (2021) 22:827. doi: 10.1186/s13063-021-05808-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mackenzie C, McDowell C, Pittaway E. Beyond 'Do no Harm': the challenge of constructing ethical relationships in refugee research. J Refug Stud. (2007) 20:299–319. doi: 10.1093/jrs/fem008 [DOI] [Google Scholar]
- 22.Morina N, Ehring T, Priebe S. Diagnostic utility of the impact of event scale-revised in two samples of survivors of war. PLoS One. (2013) 8:e83916. doi: 10.1371/journal.pone.0083916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Feyera F, Mihretie G, Bedaso A, Gedle D, Kumera G. Prevalence of depression and associated factors among Somali refugee at Melkadida camp, Southeast Ethiopia: a cross-sectional study. BMC Psychiatry. (2015) 15:171. doi: 10.1186/s12888-015-0539-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Georgiadou E, Zbidat A, Schmitt GM, Erim Y. Prevalence of mental distress among Syrian refugees with residence permission in Germany: a registry-based study. Front Psych. (2018) 9:393. doi: 10.3389/fpsyt.2018.00393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Al-Smadi AM, Tawalbeh LI, Gammoh OS, Ashour A, Tayfur M, Attarian H. The prevalence and the predictors of insomnia among refugees. J Health Psychol. (2019) 24:1125–33. doi: 10.1177/1359105316687631 [DOI] [PubMed] [Google Scholar]
- 26.Alhalaiqa F, Masa’Deh R, Al-Yami M, Al-Ghabeesh S, Rayan A, Shawashreh A, et al. Perceived stress among university students: Syrian refugees versus Jordanians. J Public Health (Berl). (2021) 29:1477–86. doi: 10.1007/s10389-020-01261-8 [DOI] [Google Scholar]
- 27.Hermansson AC, Thyberg M, Timpka T, Gerdle B. Survival with pain: an eight-year follow-up of war-wounded refugees. Med Confl Surviv. (2001) 17:102–11. doi: 10.1080/13623690108409564 [DOI] [PubMed] [Google Scholar]
- 28.Sundquist J, Hagströmer M, Johansson S-E, Sundquist K. Effect of a primary health-care-based controlled trial for cardiorespiratory fitness in refugee women. BMC Fam Pract. (2010) 11:55. doi: 10.1186/1471-2296-11-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blom EH, Bech P, Högberg G, Larsson JO, Serlachius E. Screening for depressed mood in an adolescent psychiatric context by brief self-assessment scales--testing psychometric validity of WHO-5 and BDI-6 indices by latent trait analyses. Health Qual Life Outcomes. (2012) 10:149. doi: 10.1186/1477-7525-10-149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sibai AM, Chaaya M, Tohme RA, Mahfoud Z, Al-Amin H. Validation of the Arabic version of the 5-item WHO well being index in elderly population. Int J Geriatr Psychiatry. (2009) 24:106–7. doi: 10.1002/gps.2079 [DOI] [PubMed] [Google Scholar]
- 31.Dadfar M, Momeni Safarabad N, Asgharnejad Farid AA, Nemati Shirzy M, Abarghouie FGP. Reliability, validity, and factorial structure of the World Health Organization-5 well-being index (WHO-5) in Iranian psychiatric outpatients. Trends Psychiatry Psychother. (2018) 40:79–84. doi: 10.1590/2237-6089-2017-0044 [DOI] [PubMed] [Google Scholar]
- 32.Hochberg G, Pucheu S, Kleinebreil L, Halimi S, Fructuoso-Voisin C. WHO-5, a tool focusing on psychological needs in patients with diabetes: the French contribution to the DAWN study. Diabetes Metab. (2012) 38:515–22. doi: 10.1016/j.diabet.2012.06.002 [DOI] [PubMed] [Google Scholar]
- 33.Davey C, Heard R, Lennings C. Development of the Arabic versions of the impact of events scale-revised and the posttraumatic growth inventory to assess trauma and growth in middle eastern refugees in Australia. Clin Psychol. (2015) 19:131–9. doi: 10.1111/cp.12043 [DOI] [Google Scholar]
- 34.Iranmanesh S, Shamsi A, Dehghan M. Post-traumatic stress symptoms among Iranian parents of children during Cancer treatment. Issues Ment Health Nurs. (2015) 36:279–85. doi: 10.3109/01612840.2014.983622 [DOI] [PubMed] [Google Scholar]
- 35.Brunet A, St-Hilaire A, Jehel L, King S. Validation of a French version of the impact of event scale-revised. Can J Psychiatr. (2003) 48:56–61. doi: 10.1177/070674370304800111 [DOI] [PubMed] [Google Scholar]
- 36.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Int Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.AlHadi AN, AlAteeq DA, Al-Sharif E, Bawazeer HM, Alanazi H, AlShomrani AT, et al. An arabic translation, reliability, and validation of patient health questionnaire in a Saudi sample. Ann General Psychiatry. (2017) 16:32. doi: 10.1186/s12991-017-0155-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dadfar M, Kalibatseva Z, Lester D. Reliability and validity of the Farsi version of the patient health Questionnaire-9 (PHQ-9) with Iranian psychiatric outpatients. Trends Psychiatry Psychother. (2018) 40:144–51. doi: 10.1590/2237-6089-2017-0116 [DOI] [PubMed] [Google Scholar]
- 39.Arthurs E, Steele RJ, Hudson M, Baron M, Thombs BD. Are scores on English and French versions of the PHQ-9 comparable? An assessment of differential item functioning. PLoS One. (2012) 7:e52028. doi: 10.1371/journal.pone.0052028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Int Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 41.Omani-Samani R, Maroufizadeh S, Ghaheri A, Navid B. Generalized anxiety Disorder-7 (GAD-7) in people with infertility: a reliability and validity study. Middle East Fertil Soc J. (2018) 23:446–9. doi: 10.1016/j.mefs.2018.01.013 [DOI] [Google Scholar]
- 42.Micoulaud-Franchi J-A, Lagarde S, Barkate G, Dufournet B, Besancon C, Trébuchon-Da Fonseca A, et al. Rapid detection of generalized anxiety disorder and major depression in epilepsy: validation of the GAD-7 as a complementary tool to the NDDI-E in a French sample. Epilepsy Behav. (2016) 57:211–6. doi: 10.1016/j.yebeh.2016.02.015 [DOI] [PubMed] [Google Scholar]
- 43.Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suleiman KH, Yates BC. Translating the insomnia severity index into Arabic. J Nurs Scholarsh. (2011) 43:49–53. doi: 10.1111/j.1547-5069.2010.01374.x [DOI] [PubMed] [Google Scholar]
- 45.Yazdi Z, Sadeghniiat K, Zohal M, Elmizadeh K. Validity and reliability of the Iranian version of the insomnia severity index. Malays J Med Sci. (2012) 19:31–6. [PMC free article] [PubMed] [Google Scholar]
- 46.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385–96. doi: 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- 47.Almadi T, Cathers I, Hamdan Mansour AM, Chow CM. An Arabic version of the perceived stress scale: translation and validation study. Int J Nurs Stud. (2012) 49:84–9. doi: 10.1016/j.ijnurstu.2011.07.012 [DOI] [PubMed] [Google Scholar]
- 48.Khalili R, Sirati Nir M, Ebadi A, Tavallai A, Habibi M. Validity and reliability of the Cohen 10-item perceived stress scale in patients with chronic headache: Persian version. Asian J Psychiatr. (2017) 26:136–40. doi: 10.1016/j.ajp.2017.01.010 [DOI] [PubMed] [Google Scholar]
- 49.Lesage F-X, Berjot S, Deschamps F. Psychometric properties of the French versions of the perceived stress scale. Int J Occup Med Environ Health. (2012) 25:178–84. doi: 10.2478/S13382-012-0024-8 [DOI] [PubMed] [Google Scholar]
- 50.Weiss DS, Marmar CR. The impact of event scale–revised In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford Press; (1997). 399–411. [Google Scholar]
- 51.Knappe F, Colledge F, Gerber M. Impact of an 8-week exercise and sport intervention on post-traumatic stress disorder symptoms, mental health, and physical fitness among male refugees living in a Greek refugee camp. Int J Environ Res Public Health. (2019) 16:3904. doi: 10.3390/ijerph16203904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. (2019) 394:240–8. doi: 10.1016/S0140-6736(19)30934-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Charlson FJ, Flaxman A, Ferrari AJ, Vos T, Steel Z, Whiteford HA. Post-traumatic stress disorder and major depression in conflict-affected populations: an epidemiological model and predictor analysis. Glob Ment Health (Camb). (2016) 3:e4. doi: 10.1017/gmh.2015.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Grupp F, Piskernik B, Mewes R. Is depression comparable between asylum seekers and native Germans? An investigation of measurement invariance of the PHQ-9. J Affect Disord. (2020) 262:451–8. doi: 10.1016/j.jad.2019.11.055 [DOI] [PubMed] [Google Scholar]
- 55.Murphy D, Ross J, Ashwick R, Armour C, Busuttil W. Exploring optimum cut-off scores to screen for probable posttraumatic stress disorder within a sample of UK treatment-seeking veterans. Eur J Psychotraumatol. (2017) 8:1398001. doi: 10.1080/20008198.2017.1398001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.World Health Organization . Wellbeing measures in primary health care/the DepCare project. Report on a WHO meeting: Stockholm, Sweden, 12–13 February 1998: World Health Organization. Regional Office for Europe (1998).
- 57.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; (2022). [Google Scholar]
- 58.World Health Organization . The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. Geneva: World Health Organization; (1993). [Google Scholar]
- 59.Qi L, Wang G-L, Liu S, Zhang S, Wang H-F. Dissipation-induced topological phase transition and periodic-driving-induced photonic topological state transfer in a small optomechanical lattice. Front Phys. (2021) 16:3045. doi: 10.1007/s11467-020-0983-3 [DOI] [Google Scholar]
- 60.World Health Organization . Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. (2011). Availble at: https://apps.who.int/iris/handle/10665/85839. (Accessed Jan 6, 2023).
- 61.Abbai NS, Nyirenda M, Reddy T, Ramjee G. Good correlation between the Afinion AS100 analyser and the ABX Pentra 400 analyser for the measurement of glycosylated haemoglobin and lipid levels in older adults in Durban, South Africa. S Afr Med J. (2017) 108:50–5. doi: 10.7196/SAMJ.2017.v108i1.12548 [DOI] [PubMed] [Google Scholar]
- 62.Foerster V, Severn M. Point-of-care glycated hemoglobin testing to diagnose type 2 diabetes. Issues Emerg Health Tech. (2016). 156: 1–8. [PubMed] [Google Scholar]
- 63.Kahn R, Buse J, Ferrannini E, Stern M. The metabolic syndrome: time for a critical appraisal. Joint statement from the American Diabetes Association and the European Association for the Study of diabetes. Diabetologia. (2005) 48:1684–99. doi: 10.1007/s00125-005-1876-2 [DOI] [PubMed] [Google Scholar]
- 64.Cavero-Redondo I, Martínez-Vizcaíno V, Álvarez-Bueno C, Agudo-Conde C, Lugones-Sánchez C, García-Ortiz L. Metabolic syndrome including glycated hemoglobin A1c in adults: is it time to change? J Clin Med. (2019). doi: 10.3390/jcm8122090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Eisenmann JC. On the use of a continuous metabolic syndrome score in pediatric research. Cardiovasc Diabetol. (2008) 7:17. doi: 10.1186/1475-2840-7-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Huskisson EC. Measurement of pain. Lancet. (1974) 2:1127–31. doi: 10.1016/s0140-6736(74)90884-8 [DOI] [PubMed] [Google Scholar]
- 67.Carlsson AM. Assessment of chronic pain. I. Aspects of the reliability and validity of the visual analogue scale. Pain. (1983) 16:87–101. doi: 10.1016/0304-3959(83)90088-X [DOI] [PubMed] [Google Scholar]
- 68.Åstrand PO, Rodahl K. Textbook of work physiology: Physiological bases of exercise. Champaign: Human Kinetics; (2003). [Google Scholar]
- 69.Buono MJ, Roby JJ, Micale FG, Sallis JF. Predicting maximal oxygen uptake in children: modification of the Astrand-Ryhming test. Pediatr Exerc Sci. (1989) 1:278–83. [DOI] [PubMed] [Google Scholar]
- 70.Macsween A. The reliability and validity of the Astrand nomogram and linear extrapolation for deriving VO2max from submaximal exercise data. J Sports Med Phys Fitness. (2001) 41:312–7. [PubMed] [Google Scholar]
- 71.American College of Sports Medicine . ACSM’s guidelines for exercise testing and prescription. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; (2010). [Google Scholar]
- 72.Plante TG, LeCaptain SE, McLain HC. Perceived fitness predicts daily coping better than physical activity. J Appl Biobehav Res. (2000) 5:66–79. doi: 10.1111/j.1751-9861.2000.tb00064.x [DOI] [Google Scholar]
- 73.Plante TG, Lantis A, Checa G. The influence of perceived versus aerobic fitness on psychological health and physiological stress responsivity. Int J Stress Manag. (1998) 5:141–56. doi: 10.1023/A:1022936930992 [DOI] [Google Scholar]
- 74.Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, Stein DJ, et al. Posttraumatic stress disorder in the world mental health surveys. Psychol Med. (2017) 47:2260–74. doi: 10.1017/S0033291717000708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Perlis ML, Posner D, Riemann D, Bastien CH, Teel J, Thase M. Insomnia. Lancet. (2022) 400:1047–60. doi: 10.1016/S0140-6736(22)00879-0 [DOI] [PubMed] [Google Scholar]
- 77.Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. (2018) 20:12. doi: 10.1007/s11906-018-0812-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wong MCS, Huang J, Wang J, Chan PSF, Lok V, Chen X, et al. Global, regional and time-trend prevalence of central obesity: a systematic review and meta-analysis of 13.2 million subjects. Eur J Epidemiol. (2020) 35:673–83. doi: 10.1007/s10654-020-00650-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Weisman A, Fazli GS, Johns A, Booth GL. Evolving trends in the epidemiology, risk factors, and prevention of type 2 diabetes: a review. Can J Cardiol. (2018) 34:552–64. doi: 10.1016/j.cjca.2018.03.002 [DOI] [PubMed] [Google Scholar]
- 80.Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. (2020) 16:223–37. doi: 10.1038/s41581-019-0244-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kessler RC, Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, Ormel J, et al. The global burden of mental disorders: an update from the WHO world mental health (WMH) surveys. Epidemiol Psichiatr Soc. (2009) 18:23–33. doi: 10.1017/S1121189X00001421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Long D, Bonsel GJ, Lubetkin EI, Yfantopoulos JN, Janssen MF, Haagsma JA. Health-related quality of life and mental well-being during the COVID-19 pandemic in five countries: a one-year longitudinal study. J Clin Med. (2022). doi: 10.3390/jcm11216467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nissen A, Sengoelge M, Solberg Ø. Post-migration stressors and subjective well-being in adult Syrian refugees resettled in Sweden: a gender perspective. Front Public Health. (2021) 9:717353. doi: 10.3389/fpubh.2021.717353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Blackmore R, Boyle JA, Fazel M, Ranasinha S, Gray KM, Fitzgerald G, et al. The prevalence of mental illness in refugees and asylum seekers: a systematic review and meta-analysis. PLoS Med. (2020) 17:e1003337. doi: 10.1371/journal.pmed.1003337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Henkelmann J-R, de Best S, Deckers C, Jensen K, Shahab M, Elzinga B, et al. Anxiety, depression and post-traumatic stress disorder in refugees resettling in high-income countries: systematic review and meta-analysis. BJPsych Open. (2020) 6:e68. doi: 10.1192/bjo.2020.54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zenner D, Méndez AR, Schillinger S, Val E, Wickramage K. Health and illness in migrants and refugees arriving in Europe: analysis of the electronic personal health record system. J Travel Med. (2022). doi: 10.1093/jtm/taac035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Byrow Y, Pajak R, Specker P, Nickerson A. Perceptions of mental health and perceived barriers to mental health help-seeking amongst refugees: a systematic review. Clin Psychol Rev. (2020) 75:101812. doi: 10.1016/j.cpr.2019.101812 [DOI] [PubMed] [Google Scholar]
- 88.Shishehgar S, Gholizadeh L, DiGiacomo M, Green A, Davidson PM. Health and socio-cultural experiences of refugee women: an integrative review. J Immigr Minor Health. (2017) 19:959–73. doi: 10.1007/s10903-016-0379-1 [DOI] [PubMed] [Google Scholar]
- 89.Steel Z, Silove D, Brooks R, Momartin S, Alzuhairi B, Susljik I. Impact of immigration detention and temporary protection on the mental health of refugees. Br J Psychiatry. (2006) 188:58–64. doi: 10.1192/bjp.bp.104.007864 [DOI] [PubMed] [Google Scholar]
- 90.Uysal B, Yanik M, Tastekne F, Tuzgen E, Altinisik E, Acarturk C. Psychological problems and resilience among Syrian adolescents exposed to war. Eur J Trauma Dissociation. (2022) 6:100258. doi: 10.1016/j.ejtd.2022.100258 [DOI] [Google Scholar]
- 91.Noubiap JJ, Nansseu JR, Lontchi-Yimagou E, Nkeck JR, Nyaga UF, Ngouo AT, et al. Geographic distribution of metabolic syndrome and its components in the general adult population: a meta-analysis of global data from 28 million individuals. Diabetes Res Clin Pract. (2022) 188:109924. doi: 10.1016/j.diabres.2022.109924 [DOI] [PubMed] [Google Scholar]
- 92.van de Wiel W, Castillo-Laborde C, Francisco Urzúa I, Fish M, Scholte WF. Mental health consequences of long-term stays in refugee camps: preliminary evidence from Moria. BMC Public Health. (2021) 21:1290. doi: 10.1186/s12889-021-11301-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hou WK, Liu H, Liang L, Ho J, Kim H, Seong E, et al. Everyday life experiences and mental health among conflict-affected forced migrants: a meta-analysis. J Affect Disord. (2020) 264:50–68. doi: 10.1016/j.jad.2019.11.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lang C, Brand S, Colledge F, Ludyga S, Pühse U, Gerber M. Adolescents' personal beliefs about sufficient physical activity are more closely related to sleep and psychological functioning than self-reported physical activity: a prospective study. J Sport Health Sci. (2019) 8:280–8. doi: 10.1016/j.jshs.2018.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gerber M, Brand S, Holsboer-Trachsler E, Pühse U. Fitness and exercise as correlates of sleep complaints: is it all in our minds? Med Sci Sports Exerc. (2010) 42:893–901. doi: 10.1249/MSS.0b013e3181c0ea8c [DOI] [PubMed] [Google Scholar]
- 96.Backe EL, Bosire EN, Kim AW, Mendenhall E. "thinking too much": a systematic review of the idiom of distress in sub-Saharan Africa. Cult Med Psychiatry. (2021) 45:655–82. doi: 10.1007/s11013-020-09697-z [DOI] [PubMed] [Google Scholar]
- 97.Médecins Sans Frontières . Constructing crisis at Europe's borders: The EU plan to intensify its dangerous hotspot approach on Greek islands. (2021). Available at: https://www.msf.ch/sites/default/files/2021-06/20210610_rep_greece_hotspot.pdf. (Accessed Jan 6, 2023).
- 98.Morres ID, Hatzigeorgiadis A, Stathi A, Comoutos N, Arpin-Cribbie C, Krommidas C, et al. Aerobic exercise for adult patients with major depressive disorder in mental health services: a systematic review and meta-analysis. Depress Anxiety. (2019) 36:39–53. doi: 10.1002/da.22842 [DOI] [PubMed] [Google Scholar]
- 99.Liang M, Pan Y, Zhong T, Zeng Y, Cheng ASK. Effects of aerobic, resistance, and combined exercise on metabolic syndrome parameters and cardiovascular risk factors: a systematic review and network meta-analysis. Rev Cardiovasc Med. (2021) 22:1523–33. doi: 10.31083/j.rcm2204156 [DOI] [PubMed] [Google Scholar]
- 100.Morres ID, Tzouma N-A, Hatzigeorgiadis A, Krommidas C, Kotronis KV, Dafopoulos K, et al. Exercise for perinatal depressive symptoms: a systematic review and meta-analysis of randomized controlled trials in perinatal health services. J Affect Disord. (2022) 298:26–42. doi: 10.1016/j.jad.2021.10.124 [DOI] [PubMed] [Google Scholar]
- 101.Hamilton A, Foster C, Richards J. A systematic review of the mental health impacts of sport and physical activity programmes for adolescents in post-conflict settings. J Sport Dev. (2016) 4:44–59. [Google Scholar]
- 102.Després J-P, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. (2006) 444:881–7. doi: 10.1038/nature05488 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.