Abstract
Objectives
To investigate associations between leisure-time physical activity (LPA) and injurious falls in older women and explore modification of associations by physical function and frailty.
Methods
Women born during 1946–51 from the Australian Longitudinal Study on Women’s Health, injurious falls (self-reported fall with injury and/or medical attention) and self-reported weekly LPA (duration and type). We undertook cross-sectional and prospective analyses using data from 2016 [n = 8,171, mean (SD) age 68 (1)] and 2019 surveys (n = 7,057). Associations were quantified using directed acyclic graph-informed logistic regression and effect modification examined using product terms.
Results
Participation in LPA as recommended by World Health Organization (150–300 min/week) was associated with lower odds of injurious falls in cross-sectional (adjusted Odds Ratio (OR) 0.74, 95% CI 0.61–0.90) and prospective analyses (OR 0.75, 95% CI 0.60–0.94). Compared with those who reported no LPA, cross-sectionally, odds of injurious falls were lower in those who reported brisk walking (OR 0.77, 95% CI 0.67–0.89) and vigorous LPA (OR 0.86, 95% CI 0.75–1.00). No significant association was found between different types of LPA and injurious falls prospectively. Only cross-sectionally, physical function limitation and frailty modified the association between LPA and injurious falls, with tendencies for more injurious falls with more activity in those with physical limitation or frailty, and fewer injurious falls with more activity among those without physical function limitation or frailty.
Conclusion
Participation in recommended levels of LPA was associated with lower odds of injurious falls. Caution is required when promoting general physical activity among people with physical limitation or frailty.
Keywords: accidental falls, directed acyclic graph, older adults, physical activity, older people
Key Points
Participation in World Health Organization (WHO) guideline recommended level of physical activity was associated with fewer injurious falls in older women.
Physical function limitation and frailty modified the association between leisure-time physical activity and injurious falls.
Leisure-time physical activity was associated with fewer injurious falls in those without physical function limitation or frailty.
There are tendencies for more injurious falls with more activity in those with physical limitation or frailty.
Caution is warranted in the promotion of leisure-time physical activity among women with physical limitation or frailty.
Introduction
There is an increasing trend of hospitalisation for fall-related injuries among people aged 65+, with three-quarters of all injury-related hospitalisations resulting from a fall [1]. The consequences of injurious falls can be detrimental leading to additional care for rehabilitation, dependency in activities of daily living, activity avoidance, and decline in physical function [1–3].
Promoting physical activity (PA) has been one of the global actions for ageing well [4]. According to the World Health Organization (WHO), older adults are recommended to undertake 150–300 min of moderate-intensity PA per week [5, 6]. Structured exercise reduces falls and fall-related injuries in community-dwelling people aged 60+ [7, 8]. However, the availability of and adherence to structured exercise programmes is sub-optimal [9]. Greater participation in leisure-time physical activity (LPA) among older adults would bring many health benefits but LPA’s association with injurious falls is not well understood.
Inconsistent associations between overall PA and falls and injurious falls have been reported [10–14]. One systematic review of prospective cohort studies found inconclusive associations between PA levels and falls [13]. In contrast, another systematic review of both cross-sectional and prospective cohort studies showed PA was associated with a lower risk of falls and injurious falls [14]. These inconsistent findings may be explained by the heterogeneity among the included studies, including duration and frequency of follow-up (e.g. weekly versus yearly), and the method of falls data collection (e.g. falls calendar versus delayed recall). Variable analyses methods may contribute to inconsistent findings as some studies have used cross-sectional analysis examining the association between PA and falls at one specific timepoint while others have undertaken prospective analysis examining PA at baseline and falls at the follow-up. Findings are incomparable as studies have been performed in different cohorts of different ages with different functional capacities. Moreover, frailty and physical function are associated with both LPA and injurious falls [15, 16]. Insufficient evidence was available to determine whether the relationship between PA and injurious falls varies by different levels of physical function or mobility limitation [17]. Although previously using data from 1999 and 2002 surveys of the Australian Longitudinal Study on Women’s Health (ALSWH), no prospective association between no or very low LPA and injurious falls was evident, prospective associations were evident between at least moderate to vigorous LPA and reduced falls; in this study, there was no consideration of the impact of frailty and physical function limitation on the associations [10]. Thus, using a prospective and cross-sectional data from the ALSWH cohort, we aimed to
examine the associations between different amounts and types of LPA and injurious falls; and
assess whether physical function limitation or frailty modifies the association between different types of LPA and injurious falls.
Method
Data source
The ALSWH is an ongoing population-based study which began in 1996 with three samples of women born within the years 1921–26, 1946–51 and 1973–78 (initial response rate 37–40, 53–56 and 41–42%, respectively), randomly selected from Medicare, the national health insurance database [18–20]. Rural and remote areas were intentionally oversampled to ensure good representation of these women [18]. Participants responded to follow-up surveys in 1998 and then every three years thereafter. To understand the cross-sectional associations between LPA and injurious falls among women of older age, our study used data from the 1946–51 cohort (n = 13,714; aged 45–50 years at baseline) who returned 2016 survey (n = 8,622, aged 65–70 years). Prospective associations were examined by using LPA at the 2016 survey and injurious falls at the 2019 survey.
Exposure: amount and types of LPA
LPA was measured using a validated version of the Active Australia National Physical Activity survey [21]. Participants self-reported frequency and total duration of LPA in the past week including (i) walking briskly (for recreation or exercise or to get from place to place); (ii) moderate leisure activity (e.g. social tennis, moderate exercise classes, recreational swimming); and (iii) vigorous leisure activity that makes one breathe harder or puff and pant (e.g. aerobics, vigorous cycling, running, swimming).
Amount of LPA per week was the sum of total duration of walking briskly, moderate and vigorous LPA, and was categorised into: zero, 1 to <150, 150 to <300 and ≥ 300 min. The 150- and 300-min cut-off were used according to WHO’s recommended targeted duration of moderate-intensity activity [6]. In 2019 survey, participants additionally reported involvement of strength or toning activities. Participating in the abovementioned LPA and any LPA were dichotomised (yes/no). LPA involvement were considered if the participants had a non-zero response to either the frequency and/or total duration of the corresponding activity.
Outcome: injurious falls
Participants’ responses were dichotomised (yes/no) based on the self-reported response to the two questions: in the last 12 months whether (i) been injured from a fall and (ii) needed to seek medical attention for an injury from a fall. Participants who gave a positive response to either question were considered as people who had injurious falls. Participants who had reported a fall to the ground without a positive response to the abovementioned questions were considered as people with non-injurious falls. The type of injury was not recorded in the surveys.
Frailty
Frailty was assessed by the five components: fatigue, resistance, ambulation, illness and loss of weight [22]. Participants were classified as frail if more than two positive responses were recorded out of the five components (Supplementary Table 1) [23]. This approach has previously been validated in the ALSWH 1946–51 cohort [24].
Physical function limitation
Participants were classified as having physical function limitation if they reported limitation in climbing one flight of stairs and/or walking 100 m, which is commonly defined in cohort studies in assessing physical function [25, 26].
Potential covariates
Potential confounders were identified using expert knowledge and the literature, and incorporated into a directed acyclic graph (DAG) before performing any analysis using DAGitty, version 3.0 (Supplementary Figure 1) [27]. Supplementary Information 1 shows the statistical procedures in selecting a minimum sufficient set of variables for confounding the exposure-outcome relationship. These variables include age, highest education completed, ability to manage income, Accessibility Remoteness Index of Australia scale (ARIA+) [28] and housing type.
Statistical analysis
Univariate and multivariable logistic models [29] were used to examine relationship between different amounts and types of LPA and injurious falls cross-sectionally (2016 survey) and prospectively (LPA at 2016 survey; injurious falls at 2019 survey). Multivariable models included the covariates identified from the minimally sufficient adjustment set. Effect modifications were examined for physical function limitation and frailty on the association between any and different types of LPA and injurious falls. To establish the consistency of the findings between surveys, additional analyses were performed to examine the cross-sectional association between LPA and injurious falls in 2019 survey. Statistical analyses were undertaken using SAS v9.4 (x64), SAS Institute, Inc., Cary, NC. P-values were considered statistically significant at P < 0.05.
Results
Of those eligible for 2016 survey (n = 10,716), 8,622 participants (80.5%) who returned the survey were eligible for inclusion in the analyses. Women with missing exposure (n = 126), outcome (n = 89), physical function limitation (n = 39) and covariates (n = 197) were excluded (Figure 1). The final analytical sample size was 8,171 for cross-sectional and 7,057 for prospective analyses (Figure 1). Table 1 presents the characteristics of the included women (mean age (SD) 68 (1)).
Figure 1.
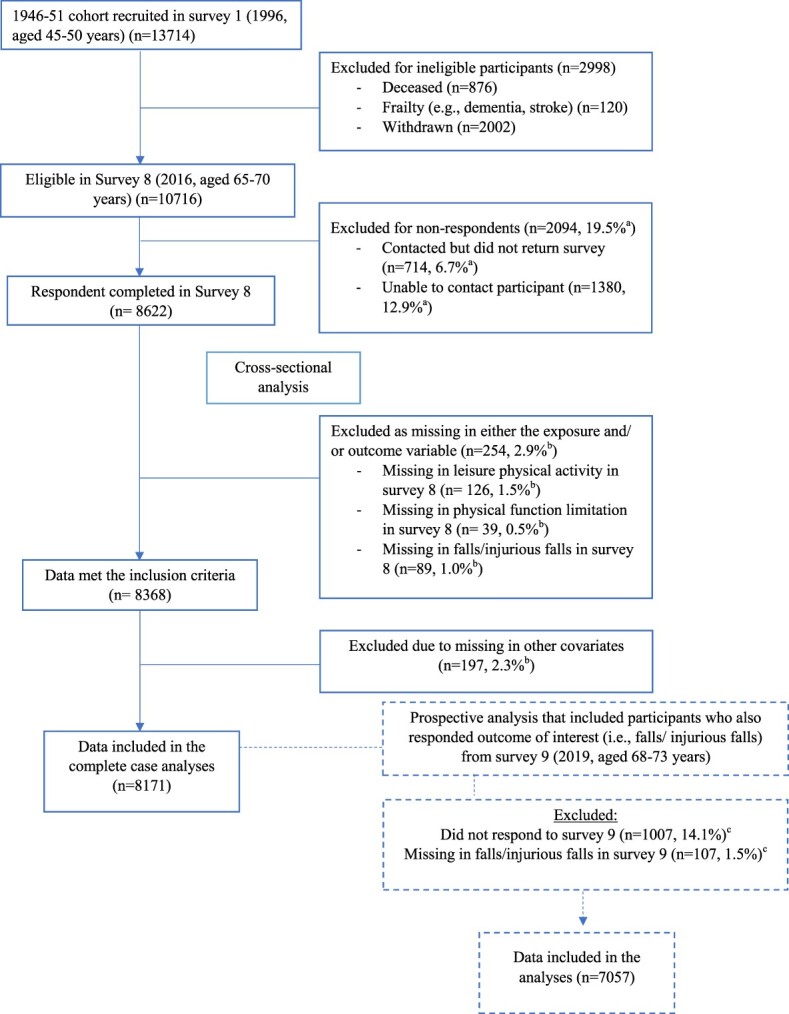
Sample selection flowchart. aThe percentage was calculated based on the number of participants eligible in survey 8 (2016) (n = 10,716). bThe percentage was calculated based on the number of participants completed survey 8 (n = 8,622). cThe percentage was calculated based on the number of participants responded to both survey 8 and survey 9 (2019) (n = 7,164).
Table 1.
Characteristics of participants (1946–51 born cohort) overall and by level of frailty and limitation in physical function in 2016 survey in the Australian Longitudinal Study on Women’s Health
| Total | Fraila | Non-frail | Limitation in physical functionb | No limitation in physical function | |
|---|---|---|---|---|---|
| (n = 8,171) | (n = 912) | (n = 7,259) | (n = 2,040) | (n = 6,131) | |
| Age, years, mean (SD) | 68 (1) | 68 (1) | 68 (1) | 68 (1) | 68 (1) |
| Location (ARIA+), n (%) | |||||
| Majorities of Australia | 3,209 (39) | 320 (35) | 2,889 (40) | 768 (38) | 2,441 (40) |
| Inner regional of Australia | 3,306 (40) | 362 (40) | 2,944 (41) | 793 (39) | 2,513 (41) |
| Regional (Outer regional, remote and very remote Australia) | 1,656 (20) | 230 (25) | 1,426 (20) | 479 (23) | 1,177 (19) |
| Housing arrangement, n (%) | |||||
| House/unit/apartment/villa/townhouse | 7,764 (95) | 836 (92) | 6,928 (95) | 1,894 (93) | 5,870 (96) |
| Caravan/mobile home/retirement village/hostel/residential aged care | 407 (5) | 76 (8) | 331 (5) | 146 (7) | 261 (4) |
| Education, n (%) | |||||
| No formal education | 1,020 (12) | 186 (20) | 834 (11) | 404 (20) | 616 (10) |
| School or intermediate certificate | 2,003 (25) | 249 (27) | 1,754 (24) | 555 (27) | 1,448 (24) |
| Higher school or leaving certificate | 1,575 (19) | 164 (18) | 1,411 (19) | 398 (20) | 1,177 (19) |
| University degrees of above | 1,731 (21) | 113 (12) | 1,618 (22) | 266 (13) | 1,465 (24) |
| Others | 1,842 (23) | 200 (22) | 1,642 (23) | 417 (20) | 1,425 (23) |
| Ability to manage income, n (%) | |||||
| Impossible | 125 (2) | 47 (5) | 78 (1) | 59 (3) | 66 (1) |
| Difficult always | 615 (8) | 177 (19) | 438 (6) | 307 (15) | 308 (5) |
| Difficult sometimes | 1,658 (20) | 253 (28) | 1,405 (19) | 523 (26) | 1,135 (19) |
| Not too bad | 3,974 (49) | 346 (38) | 3,628 (50) | 904 (44) | 3,070 (50) |
| Easy | 1799 (22) | 89 (10) | 1710 (24) | 247 (12) | 1,552 (25) |
| Frailty b , n (%) | |||||
| Fatiguec | 3,802 (47) | 892 (98) | 2,910 (40) | 1,606 (79) | 2,196 (36) |
| Resistancec | 1,943 (24) | 871 (96) | 1,072 (15) | 1,943 (96) | 0 (0) |
| Ambulationc | 885 (11) | 724 (80) | 161 (2) | 885 (44) | 0 (0) |
| Illness ≥ 5 conditions | 305 (4) | 213 (23) | 92 (1) | 199 (10) | 106 (2) |
| Loss of weight ≥ 5%c | 1,098 (15) | 282 (36) | 816 (13) | 296 (17) | 802 (15) |
| Fall reported in the last survey c,d , n (%) | 2,137 (26) | 392 (43) | 1745 (24) | 772 (38) | 1,365 (22) |
| Leisure physical activity participation, n (%) | |||||
| No leisure physical activity | 1,442 (18) | 473 (52) | 969 (13) | 815 (40) | 627 (10) |
| Any leisure physical activity | 6,729 (82) | 439 (48) | 6,290 (87) | 1,225 (60) | 5,504 (90) |
Data presented in mean (SD) unless specified; ARIA+, Accessibility Remoteness Index of Australia; FRAIL, Fatigue, Resistance, Ambulation, Illness, Loss of weight.
aWomen were classified as frail if more than two positive responses were recorded out of the five components
bWomen had limitation in physical function if they responded ‘limited a lot’ or ‘limited a little’ in climbing one flight of stairs and/ or walking 100 m.
cMissing data in body mass index (n = 380), fatigue (n = 26), resistance (n = 42), ambulation (n = 34), loss of weight (n = 1,007), history of falls (n = 26)
dFall reported in the last survey was first retrieved from survey 7 (2013). To minimise missing information, if participants did not respond to falls questions in survey 7 (2013), previous survey 6 (2010) was used. If there were still any missing information about previous falls, survey 5 (2007) and survey 4 (2004) were both used using the same procedure as described.
Associations between LPA and injurious falls
Overall, 26% of the women (n = 2,137) reported a fall in the previous 12 months at 2016 survey, and more than half (55%) of these were injurious falls (n = 1,177).
Results from cross-sectional analyses
Primary cross-sectional analyses in 2016 showed various amounts and types of LPA participation were associated with lower odds of injurious falls, except borderline significance for moderate-vigorous LPA (OR 0.86, 95% CI 0.73–1.01) (Table 2), compared with no LPA. After adjusting for potential confounders, the associations between different amounts of LPA and injurious falls remained, with the lowest odds among women with ≥300 min of LPA (OR 0.63, 95% CI 0.53–0.75) (Table 2). Lower odds of injurious falls were found for those involved in any LPA, brisk walking and vigorous LPA, with borderline significance in moderate LPA (OR 0.89, 95% CI 0.78–1.01), compared with no LPA (Table 2). Additional cross-sectional analyses in 2019 survey (n = 7,540, Supplementary Figure 2) showed broadly similar results with lower odds of injurious falls in various amounts and types of LPA (Supplementary Table 2). Strength or toning exercise in 2019 was associated with lower odds of injurious falls (OR 0.84, 95% CI 0.73–0.97), with similar association after adjusting for potential confounders (Table 2).
Table 2.
Association between different amount and types of leisure physical activity and cross-sectional (2016 survey, n = 8,171) and prospective (2019 survey, n = 7,057) injurious falls in the 1946–51 born women of the Australian Longitudinal Study on Women’s Health
| Cross-sectional analysisa | Prospective analysisb | |||||||
|---|---|---|---|---|---|---|---|---|
| People who had non-injurious fallsc n = 6,994 |
People who had injurious falls n = 1,177 |
Odds of injurious falls OR (95% CI) |
Adjusted odds of injurious falls (95% CI)d | People who had non-injurious fallsc n = 6,048 |
People who had injurious falls n = 1,009 |
Odds of injurious falls (95% CI) |
Adjusted Odds of injurious falls (95% CI)d |
|
| A) Duration of total leisure physical (LPA) activity in the past week, n (%) | ||||||||
| No physical activity | 1,161 (17) | 281 (24) | Ref. | Ref. | 929 (15) | 189 (19) | Ref. | Ref |
| 1 to <150 min | 1,278 (18) | 233 (20) | 0.75 (0.62–0.91) | 0.80 (0.66–0.97) | 1,190 (20) | 196 (19) | 0.88 (0.70–1.09) | 0.91 (0.73–1.13) |
| 150 to <300 min | 1,394 (17) | 227 (19) | 0.67 (0.56–0.82) | 0.74 (0.61–0.90) | 1,261 (21) | 181 (18) | 0.71 (0.57–0.88) | 0.75 (0.60–0.94) |
| ≥ 300 min | 3,161 (45) | 436 (37) | 0.57 (0.48–0.67) | 0.63 (0.53–0.75) | 2,758 (46) | 443 (44) | 0.79 (0.66–0.95) | 0.84 (0.70–1.02) |
| B) Any leisure physical activity participation, n (%) | ||||||||
| None reported | 1,161 (17) | 281 (24) | Ref. | Ref. | 929 (15) | 189 (19) | Ref. | Ref. |
| Some reported | 5,833 (83) | 896 (76) | 0.64 (0.55–0.74) | 0.70 (0.60–0.81) | 5,119 (85) | 820 (81) | 0.79 (0.66–0.94) | 0.83 (0.70–1.00) |
| C) Physical activity that included walking briskly, n (%) | ||||||||
| No brisk walking reported | 1,460 (21) | 321 (27) | Ref. | Ref. | 1,208 (20) | 229 (23) | Ref. | Ref |
| Some brisk walking reported | 5,534 (79) | 856 (73) | 0.70 (0.61–0.81) | 0.77 (0.67–0.89) | 4,840 (80) | 780 (77) | 0.85 (0.72–1.00) | 0.90 (0.76–1.06) |
| D) Physical activity that included moderate leisure activity, n (%) | ||||||||
| No moderate activity reported | 3,911 (56) | 708 (60) | Ref. | Ref. | 3,319 (55) | 559 (55) | Ref. | Ref. |
| Some moderate activity reported | 3,083 (44) | 469 (40) | 0.84 (0.74–0.95) | 0.89 (0.78–1.01) | 2,729 (45) | 450 (45) | 0.98 (0.86–1.12) | 1.00 (0.88–1.15) |
| E) Physical activity that included vigorous leisure activity, n (%) | ||||||||
| No vigorous activity reported | 4,999 (71) | 886 (75) | Ref. | Ref. | 4,276 (71) | 741 (73) | Ref. | Ref. |
| Some vigorous activity reported | 1995 (29) | 291 (25) | 0.82 (0.71–0.95) | 0.86 (0.75–1.00) | 1,772 (29) | 268 (27) | 0.87 (0.75–1.01) | 0.89 (0.77–1.04) |
| F) Physical activity that included moderate-vigorous leisure activity, n (%) | ||||||||
| No moderate-vigorous activity reported | 5,535 (79) | 960 (82) | Ref. | Ref. | 4,745 (78) | 804 (80) | Ref. | Ref. |
| Some moderate-vigorous activity reported | 1,459 (21) | 217 (18) | 0.86 (0.73–1.01) | 0.90 (0.77–1.06) | 1,303 (22) | 205 (20) | 0.93 (0.79–1.10) | 0.95 (0.80–1.12) |
| G) Physical activity that included strength or toning activity d , n (%) | ||||||||
| No strength or toning reported (n = 5,196) | 4,399 (63) | 797 (72) | Ref. | Ref. | N/A | |||
| Some strength or toning reported (n = 2,344) | 2,033 (29) | 311 (28) | 0.84 (0.73–0.97) | 0.87 (0.75–1.00) | ||||
Association between leisure physical activity and injurious falls were calculated using logistic regression and presented in odds ratio (OR) and 95% confidence intervals (95% CI).
N/A = not applicable
Leisure physical activity was used as exposure and injurious falls was used as an outcome.
aCross-sectional analyses refer to the use of exposure and outcome in 2016 survey (when aged 65–70 years).
bProspective analyses refer to the use of exposure in 2016 survey and outcome in 2019 survey (when aged 68–73 years).
cWomen who did not have any fall or women who had falls and without injuries.
dTo understand the relationship of all types of LPA and injurious falls, the cross-sectional analysis of strength or toning activity (such as lifting weights, pull-ups, push-ups, sit-ups, yoga, pilates) and injurious falls was performed using 2019 survey (when aged 68–74 years) as the strength or toning activity was first included in 2019.
eAdjusted for age, Accessibility Remoteness Index of Australia (ARIA+), housing arrangement, education and ability to manage income.
Results from prospective analyses
At the 2019 survey, 1,009 of the 7,057 women reported injurious falls. Compared with no LPA as reported in 2016, participation in 150 to <300 and ≥ 300 min of LPA were both associated with lower odds of injurious falls in 2019 (Table 2). After adjusting for potential confounders, only those with 150 to <300 min of LPA had lower odds of prospective injurious falls (OR 0.75, 95% CI 0.60–0.94), with borderline significance in those with ≥300 min of LPA (OR 0.84, 95% CI 0.70–1.02), compared with no LPA (Table 2). For the different types of LPA, those with any LPA and brisk walking had lower odds of injurious falls; however, only any LPA remained significant after adjusting for potential confounders (OR 0.83, 95% CI 0.70–1.00) (Table 2). No association was found between moderate and moderate-vigorous LPA and subsequent injurious falls. Vigorous LPA had a borderline association with subsequent injurious falls (OR 0.87 95% CI 0.75–1.01), and similar association was found after adjusting for potential confounders (Table 2).
Effect modification of physical function limitation and frailty
Eleven percent (n = 912) of women were classified as frail and 25% (n = 2,040) had physical function limitations (Table 1). Compared with the non-frail women, a smaller proportion of frail women participated in LPA (87% vs 48%, P < 0.001). Compared with those without physical function limitations, fewer women with physical function limitations participated in LPA (90% vs 60%, P < 0.001).
Both physical function limitation and frailty modified the associations between any and different types of LPA and injurious falls cross-sectionally (all P-values for interaction≤0.05, Figure 2). Cross-sectionally, women with physical function limitation or frailty who participated in any LPA had higher odds of injurious falls compared with those without physical function limitation or frailty, before and after adjusting for potential confounders (Figure 2). Additional analyses showed physical function limitation and frailty modified the cross-sectional associations between any LPA and brisk walking and injurious falls in 2019 survey (Supplementary Figure 3). No effect modification of physical function limitation and frailty were found prospectively (all P-values for interaction>0.05, Supplementary Figure 4).
Figure 2.
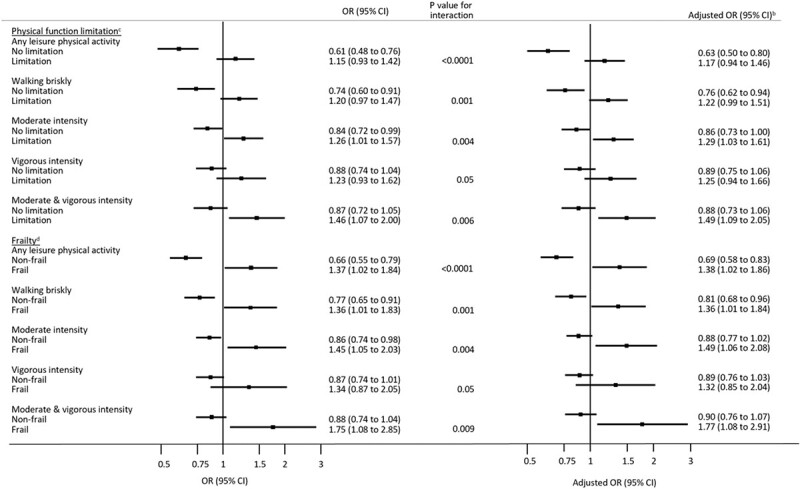
Effect modifications of physical function limitation and frailty on the cross-sectional associationsa between any leisure physical activity and the different types of leisure physical activity and injurious falls in 2016 survey in the 1946–51 born women of the Australian Longitudinal Study on Women’s Health. aCross-sectional association between leisure physical activity and injurious falls were calculated using logistic regression and presented in odds ratios (OR) and 95% confidence intervals (95% CI). Cross-sectional analysis refers to the use of exposure (i.e. leisure physical activity) and outcome (i.e. injurious falls) in 2016 survey (when aged 65–70 years). bAdjusted ORs were presented after adjusting for age, Accessibility Remoteness Index of Australia scale (ARIA+), housing arrangement, education and ability to manage income. cParticipants had a physical function limitation if they responded “limited a lot’ or ‘limited a little’ in their ability to climb one flight of stairs or walk 100 m. dWomen were frail if FRAIL score was greater than 2 points.
Discussion
Our study investigated the association between different amounts and types of LPA and injurious falls. LPA participation was associated with reduced risk of injurious falls in cross-sectional and prospective analyses. Physical function limitation or frailty modified the associations between LPA and injurious falls cross-sectionally, but not prospectively.
Our study showed participation in 150–300 min of LPA, as is recommended by WHO, was associated with less risk of injurious falls cross-sectionally (26% less) and prospectively (25% less), after adjusting for potential confounders. Cross-sectionally, the lowest risk of injurious falls (37% less) was found in women with ≥300 min of LPA, suggesting a dose–response relationship. Exercise dose is an important variable in falls prevention [30] and a previous systematic review demonstrated higher amount of PA was associated with fewer falls [31]. Prospectively, a potential U-shaped association between LPA and injurious falls was observed, with the lowest risk of subsequent injurious falls found among those with 150 to <300 min of LPA. Previous studies reported the U-shaped associations between LPA and falls regardless of injuries with contradictory findings [11, 12]. A cohort study of community-dwelling Chinese older adults (mean age 83 years, n = 671) found an increase in falls among those who were inactive or highly active, compared with those who were moderately active [11]. However, another cohort study in the Netherlands (mean age 75 years, n = 1,337) did not find such U-shaped relationship between PA and falls [12]. In addition, while in agreement with our findings, a previous ALSWH study found associations between moderate and vigorous LPA and lower odds of injurious falls, no associations were reported between no/very low/low LPA and injurious falls three years later in older women of another generation (i.e. 1921–26 born cohort) [10]. The different definitions of PA may lead to different findings. In the previous ALSWH study, PA was grouped into five categories (i.e. none/very low, low, moderate, high and very high) based on weekly frequency and intensity of LPA participation [10], whereas LPA in our study was considered based on the total amount of PA performed in minutes in the past week. Another possible explanation could be the variation in health status between birth cohorts. Differences in health profile between cohorts in the ALSWH have been reported [32].
Any LPA, brisk walking, vigorous LPA and strength or toning activity were all associated with a lower risk of injurious falls cross-sectionally after adjusting for potential confounders. Similarly, a recent cross-sectional study in China showed protection for falls among both men and women who participated in aerobics, resistance or leisure-sports activity [33]. Our findings extend the understanding of the association between the different intensities of LPA and injurious falls. Meanwhile, we found no association between the different types of LPA and subsequent injurious falls. These findings suggest that PA dose is possibly more important in prospective injurious falls prevention than the type of PA. The lack of association between walking and prospective injurious falls were previously reported [34]. Most previous studies only account for the amount or type of PA and injurious falls in either cross-sectional or prospective analyses and rarely considered the amount and type of PA in both analyses within the same cohort [13, 14].
Physical function limitation and frailty modified the associations between LPA and injurious falls when measured at the same timepoint. For women without physical function limitation or frailty, LPA participation were associated with a lower risk of injurious falls, suggesting a protective mechanism. On the contrary, among women with physical function limitation or frailty, LPA participation were associated with higher risk of injurious falls, suggesting the potential injurious falls risk when participating in LPA. Those with physical function limitation or frailty may be more susceptible to falls and injuries when falls occur due to lower muscle mass and weakness [35]. Lower limbs weakness is a predictor of falls and fall-related injuries in older adults [36, 37]. In our study, the relationship between LPA and injurious falls measured 3 years later did not differ by physical function limitation and frailty. A previous population-based cohort study of men in the United Kingdom (mean age 71–91 years, n = 3,137) found that the association between PA and falls 1 year later differed by the presence of mobility limitation, with reduced falls with increasing activity among men with mobility limitation and increased falls among men without mobility limitation [38], which is in contrast to our findings. Another cohort study of German men and women (≥65 years, n = 1,214) showed an increase in activity was associated with more falls, particularly among those with slower walking speed (<0.8 m/s) [39]. Our findings should be analysed with caution because of loss to follow-up and fluctuating LPA (as shown previously among ALSWH women [40]), physical function and other confounders. Of note, trials have demonstrated the benefits of structured exercise or supervised home-based programmes on falls among older adults at high risk of falls [8] and with signs of frailty and physical function limitation [41].
Strengths and limitations
The main strength of our study is the large longitudinal population-based sample of Australian women [18], which allows for more precise estimates of the associations between different amounts and types of LPA and injurious falls, particularly in women with physical function limitations and frailty. An added value of our study is the use of DAG to identify confounding variables, which reduces the potential sources of bias in an exposure-outcome relationship, including overadjustment bias.
As with all observational studies, it is possible that respondents who continued the survey were healthier than those who had dropped out (dropout rate of 19.5% in 2016 survey), suggesting survival bias [42]. The women who withdrew were more likely to have poorer physical health [42]. However, 28% women reported falls in our study, which is similar to the proportion of falls for people aged 65+ years reported worldwide [43]. There is a possibility of reverse causation in cross-sectional analyses, that is, women not falling as much may be more active or women with physical function limitation or frailty are less likely to participate in LPA. However, we also evaluated the prospective association between LPA and subsequent injurious falls. Another limitation is self-reported LPA that does not account for incidental activities, which could increase exposure to risk of falls and/or injurious falls, particularly among people with impaired gait and balance [44]. Self-reported LPA and injurious falls are prone to recall bias. However, recall of past week PA has acceptable psychometric properties [45] and our study had similar fall prevalence as the prevalence worldwide [43]. Furthermore, LPA participation changes in different phases of life and changes in LPA levels may have different associations with falls [46, 47]. Although all efforts was made to ensure the representativeness of the sample in the ALSWH, the sample was of higher education qualification and with English speaking background [48], which may limit the generalisability to others with non-English speaking background and of lower socioeconomic status. Finally, our findings may not be generalised to men.
Clinical implications
Guideline recommended levels of LPA participation was associated with fewer injurious falls in older women. Clinicians should be cautious when promoting LPA among people with physical function limitations or frailty, and these people may need specific exercise programmes. There is evidence from trials that structured exercise that challenges balance (with the optional addition of strength training) can prevent falls in people assessed as being at an increased risk [49]. The role of exercise in preventing falls in people with frailty is less clear but systematic review evidence indicates that exercise targeting mobility can enhance mobility and function in people with frailty [50].
Conclusion
Compared with those without any LPA, participation in LPA as recommended by WHO was associated with lower risk of injurious falls cross-sectionally and prospectively. Brisk walking and vigorous LPA were both associated with less risk of injurious falls cross-sectionally. No association was found between the different types of LPA and injurious falls prospectively. Both physical function limitation and frailty modified the cross-sectional association between different types of LPA and injurious falls with tendencies for more injurious falls with more activities among those with physical function limitation or frailty, and protection of injurious falls among those without physical function limitation or frailty.
Supplementary Material
Acknowledgements
The research on which this paper is based was conducted as part of the Australian Longitudinal Study on Women’s Health by the University of Queensland and the University of Newcastle. We are grateful to the Australian Government Department of Health and Aged Care for funding and to the women who provided the survey data.
Contributor Information
Wing S Kwok, Institute for Musculoskeletal Health, The University of Sydney and Sydney Local Health District, Sydney, Australia; School of Public Health, Faculty of Medicine and Health, The University of Sydney, , Australia.
Xenia Dolja-Gore, School of Medicine and Public Health, The University of Newcastle, , Australia.
Saman Khalatbari-Soltani, School of Public Health, Faculty of Medicine and Health, The University of Sydney, , Australia; ARC Centre of Excellence in Population Aging Research (CEPAR), The University of Sydney, Sydney, Australia.
Julie Byles, School of Medicine and Public Health, The University of Newcastle, , Australia.
Juliana S Oliveira, Institute for Musculoskeletal Health, The University of Sydney and Sydney Local Health District, Sydney, Australia; School of Public Health, Faculty of Medicine and Health, The University of Sydney, , Australia.
Marina B Pinheiro, Institute for Musculoskeletal Health, The University of Sydney and Sydney Local Health District, Sydney, Australia; School of Public Health, Faculty of Medicine and Health, The University of Sydney, , Australia.
Vasi Naganathan, Concord Clinical School, Faculty of Medicine and Health, The University of Sydney, Sydney, Australia; Centre for Education and Research on Ageing, Department of Geriatric Medicine, Concord Repatriation General Hospital, Sydney, Australia.
Anne Tiedemann, Institute for Musculoskeletal Health, The University of Sydney and Sydney Local Health District, Sydney, Australia; School of Public Health, Faculty of Medicine and Health, The University of Sydney, , Australia.
Catherine Sherrington, Institute for Musculoskeletal Health, The University of Sydney and Sydney Local Health District, Sydney, Australia; School of Public Health, Faculty of Medicine and Health, The University of Sydney, , Australia.
Declaration of Conflicts of Interest
None.
Declaration of Sources of Funding
WK was supported by the National Health and Medical Research Council Center of Research Excellence Prevention of Falls injuries; the funders had no role in the study design, data collection and analysis, decision to publish or preparation of this paper. SKS was supported by the Australian Research Council Centre of Excellence in Population Aging Research (project no. CE170100005); the funders had no role in study design, data collection and analysis, decision to publish or preparation of this paper. MBP is supported by a research fellowship from the National Health and Medical Research Council (NHMRC), Australia; the funders had no role in study design, data collection and analysis, decision to publish or preparation of this paper.
Ethical Approval
The ALSWH survey has ongoing ethical approval from the Human Research Ethics Committees (HRECs) of the Universities of Newcastle and Queensland (approval numbers H-076-0795 and 2004000224, respectively).
Data Availability Statement
The data that support the findings of this study are available from the Australian Longitudinal Study on Women’s Health (ALSWH). Data in the current study was used following approvals and data sharing agreements and therefore, data is not publicly available.
References
- 1. Australian Institute of Health and Welfare . Trends in Hospitalised Injury Due to Falls in Older People 2007–08 to 2016–17. Injury research and statistics series no. 126. Cat. no. INJCAT 206. Canberra: AIHW, 2019. [Google Scholar]
- 2. Close JCT, Lord SR, Antonova Eet al. . Older people presenting to the emergency department after a fall: a population with substantial recurrent healthcare use. Emerg Med J 2012; 29: 742–7. [DOI] [PubMed] [Google Scholar]
- 3. Yardley L, Smith H. A prospective study of the relationship between feared consequences of falling and avoidance of activity in community-living older people. Gerontologist 2002; 42: 17–23. [DOI] [PubMed] [Google Scholar]
- 4. World Health Organization . Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. Geneva: World Health Organization, 2018. [Google Scholar]
- 5. Bauman A, Merom D, Bull FC, Buchner DM, Fiatarone Singh MA. Updating the evidence for physical activity: summative reviews of the epidemiological evidence, prevalence, and interventions to promote “active aging”. Gerontologist 2016; 56 (Suppl 2): S268–80. [DOI] [PubMed] [Google Scholar]
- 6. Bull FC, Al-Ansari SS, Biddle Set al. . World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med 2020; 54: 1451–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. El-Khoury F, Cassou B, Charles M-A, Dargent-Molina P. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ 2013; 347: f6234. 10.1136/bmj.f6234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sherrington C, Fairhall NJ, Wallbank GKet al. . Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev 2019; 2019: CD012424–4. 10.1002/14651858.CD012424.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ng CACM, Fairhall N, Wallbank G, Tiedemann A, Michaleff ZA, Sherrington C. Exercise for falls prevention in community-dwelling older adults: trial and participant characteristics, interventions and bias in clinical trials from a systematic review. BMJ Open Sport Exerc Med 2019; 5: e000663–3. 10.1136/bmjsem-2019-000663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Heesch KC, Byles JE, Brown WJ. Prospective association between physical activity and falls in community-dwelling older women. J Epidemiol Commun health (1979) 2008; 62: 421–6. [DOI] [PubMed] [Google Scholar]
- 11. Lu Z, Lam FMH, Leung JCS, Kwok TCY. The U-shaped relationship between levels of Bouted activity and fall incidence in community-dwelling older adults: a prospective cohort study. J Gerontol A 2020; 75: e145–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Peeters GMEE, Schoor NM, Pluijm SMF, Deeg DJH, Lips P. Is there a U-shaped association between physical activity and falling in older persons? Osteoporosis Int 2010; 21: 1189–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Soares WJS, Lopes AD, Nogueira E, Candido V, de Moraes SA, Perracini MR. Physical activity level and risk of falling in community-dwelling older adults: systematic review and meta-analysis. J Aging Phys Act 2018; 27: 34–43. [DOI] [PubMed] [Google Scholar]
- 14. Thibaud M, Bloch F, Tournoux-Facon Cet al. . Impact of physical activity and sedentary behaviour on fall risks in older people: a systematic review and meta-analysis of observational studies. Eur Rev Aging Phys Act 2012; 9: 5–15. [Google Scholar]
- 15. Assen MALM, Helmink JHM, Gobbens RJJ. Associations between lifestyle factors and multidimensional frailty: a cross-sectional study among community-dwelling older people. BMC Geriatr 2022; 22: 7. 10.1186/s12877-021-02704-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Giné-Garriga MPPT, Roqué-Fíguls MMD, Coll-Planas LMD, Sitjà-Rabert MPPT, Salvà AMD. Physical exercise interventions for improving performance-based measures of physical function in community-dwelling, frail older adults: a systematic review and meta-analysis. Arch Phys Med Rehabil 2014; 95: 753–769.e3. [DOI] [PubMed] [Google Scholar]
- 17. Dipietro L, Campbell WW, Buchner DMet al. . Physical activity, injurious falls, and physical function in aging: an umbrella review. Med Sci Sports Exerc 2019; 51: 1303–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Brown WJ, Bryson L, Byles JEet al. . Women’s Health Australia: recruitment for a National Longitudinal Cohort Study. Women Health 1999; 28: 23–40. [DOI] [PubMed] [Google Scholar]
- 19. Lee C, Dobson AJ, Brown WJet al. . Cohort profile: the Australian Longitudinal Study on Women’s Health. Int J Epidemiol 2005; 34: 987–91. [DOI] [PubMed] [Google Scholar]
- 20. Australian Longitudinal Study on Women's Helath . https://alswh.org.au/ (2020, date last accessed).
- 21. Brown WJ, Burton NW, Marshall AL, Miller YD. Reliability and validity of a modified self-administered version of the active Australia physical activity survey in a sample of mid-age women. Aust N Z J Public Health 2008; 32: 535–41. [DOI] [PubMed] [Google Scholar]
- 22. Kan GAMD, Rolland YMMD, Morley JE, Vellas B. Morley JEMBB, Vellas BMD; frailty: toward a clinical definition. J Am Med Dir Assoc 2008; 9: 71–2. [DOI] [PubMed] [Google Scholar]
- 23. EYz H, Lam SC. Review of frailty measurement of older people: evaluation of the conceptualization, included domains, psychometric properties, and applicability. Aging Med 2021; 4: 272–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Susanto M, Hubbard RE, Gardiner PA. Validity and responsiveness of the FRAIL scale in middle-aged women. J Am Med Dir Assoc 2018; 19: 65–9. [DOI] [PubMed] [Google Scholar]
- 25. Mendonça N, Hengeveld LM, Visser Met al. . Low protein intake, physical activity, and physical function in European and North American community-dwelling older adults: a pooled analysis of four longitudinal aging cohorts. Am J Clin Nutr 2021; 114: 29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tomey KM, Sowers MR. Assessment of physical functioning: a conceptual model encompassing environmental factors and individual compensation strategies. Phys Ther 2009; 89: 705–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Textor J, Zander B, Gilthorpe MS, Liskiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package `dagitty'. Int J Epidemiol 2016; 45: 1887–94. [DOI] [PubMed] [Google Scholar]
- 28. Australian Bureau of Statistics . Australian Statistical Geography Standard (ASGS). vol. 5. Remoteness Structure. Canberra, Australia: Commonwealth of Australia, 2016. [Google Scholar]
- 29. Wright RE; Logistic regression . Reading and Understanding Multivariate Statistics. Washington, DC: American Psychological Association, 1995; 217–44. [Google Scholar]
- 30. Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JCT. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc 2008; 56: 2234–43. [DOI] [PubMed] [Google Scholar]
- 31. Ramsey KA, Meskers CGM, Maier AB. Every step counts: synthesising reviews associating objectively measured physical activity and sedentary behaviour with clinical outcomes in community-dwelling older adults. Lancet Healthy Longevity 2021; 2: e764–72. [DOI] [PubMed] [Google Scholar]
- 32. Mishra GBI, Byrnes E, Cavenagh Det al. . Health and Wellbeing of Women in Midlife: Findings from the Australian Longitudinal Study on Women’s Health. Report prepared for the Australian Government Department of Health. Newcastle: ALSWH, 2022. https://alswh.org.au/post-outcomes/2022-major-report-health-and-wellbeing-of-women-in-midlife/.
- 33. Figueiredo JA, Lopes CS, Vale WSet al. . Association between types of leisure-time physical activity and falls in the older adults: a population-based study. Sport Sci Health 2022; 18: 689–97. [Google Scholar]
- 34. Iinattiniemi S, Jokelainen J, Luukinen H. Exercise and risk of injurious fall in home-dwelling elderly. Int J Circumpolar Health 2008; 67: 235–44. [DOI] [PubMed] [Google Scholar]
- 35. Reid KF, Naumova EN, Carabello RJ, Phillips EM, Fielding RA. Lower extremity muscle mass predicts functional performance in mobility-limited elders. J Nutr Health Aging 2008; 12: 493–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc 2004; 52: 1121–9. [DOI] [PubMed] [Google Scholar]
- 37. Suey SYY, Reijnierse EM, Pham VKet al. . Sarcopenia and its association with falls and fractures in older adults: a systematic review and meta-analysis. J Cachexia Sarcopenia Muscle 2019; 10: 485–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Jefferis BJ, Merom D, Sartini Cet al. . Physical activity and falls in older men: the critical role of mobility limitations. Med Sci Sports Exerc 2015; 47: 2119–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Klenk J, Kerse N, Rapp Ket al. . Physical activity and different concepts of fall risk estimation in older people--results of the ActiFE-Ulm study. PloS One 2015; 10: e0129098–8. 10.1371/journal.pone.0129098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Leigh L, Byles JE, Mishra GD. Change in physical function among women as they age: findings from the Australian Longitudinal Study on Women's Health. Qual Life Res 2017; 26: 981–91. [DOI] [PubMed] [Google Scholar]
- 41. Suikkanen S, Soukkio P, Aartolahti Eet al. . Effect of 12-month supervised, home-based physical exercise on functioning among persons with signs of frailty: a randomized controlled trial. Arch Phys Med Rehabil 2021; 102: 2283–90. 10.1016/j.apmr.2021.06.017. [DOI] [PubMed] [Google Scholar]
- 42. Young AF, Powers JR, Bell SL. Attrition in longitudinal studies: who do you lose? Aust N Z J Public Health 2006; 30: 353–61. [DOI] [PubMed] [Google Scholar]
- 43. World Health Organization . WHO Global Report on Falls Prevention in Older Age. Geneva, Switzerland: WHO Press, 2007. https://www.who.int/publications/i/item/9789241563536.
- 44. Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas 2013; 75: 51–61. [DOI] [PubMed] [Google Scholar]
- 45. Brown WJ, Trost SG, Bauman A, Mummery K, Owen N. Test-retest reliability of four physical activity measures used in population surveys. J Sci Med Sport 2004; 7: 205–15. [DOI] [PubMed] [Google Scholar]
- 46. Brown WJ, Heesch KC, Miller YD. Life events and changing physical activity patterns in women at different life stages. Ann Behav Med 2009; 37: 294–305. [DOI] [PubMed] [Google Scholar]
- 47. Hirvensalo M, Lintunen T. Life-course perspective for physical activity and sports participation. Eur Rev Aging Phys Act 2011; 8: 13–22. [Google Scholar]
- 48. Powers JR. Comparison of the Australian Longitudinal Study on Women’s Health Cohorts with Women of the Same Age in the 2001 Census. Technical Report. Newcastle: ALSWH, 2004. [Google Scholar]
- 49. Sherrington C, Fairhall N, Kwok Wet al. . Evidence on physical activity and falls prevention for people aged 65+ years: systematic review to inform the WHO guidelines on physical activity and sedentary behaviour. The international journal of behavioral nutrition and physical activity 2020; 17: 144–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Treacy D, Hassett L, Schurr Ket al. . Mobility training for increasing mobility and functioning in older people with frailty. Cochrane Database Syst Rev 2022; 2022: CD010494. 10.1002/14651858.CD010494.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the Australian Longitudinal Study on Women’s Health (ALSWH). Data in the current study was used following approvals and data sharing agreements and therefore, data is not publicly available.


