Abstract
Video Abstract
OBJECTIVES
Adverse childhood experiences (ACEs) can drive poor adult mental and physical health, but the impact of early life protective factors should not be overlooked. Positive childhood experiences (PCEs) measures quantify protective factors, but evidence is lacking on their link to health conditions independent of ACEs in nationally representative studies. This study examines associations between composite PCE score and adult health, adjusting for ACEs.
METHODS
The most recent 2017 wave of the Panel Study of Income Dynamics, a nationally representative study and its 2014 Childhood Retrospective Circumstances supplement (n = 7496) collected adult health outcomes, PCEs, and ACEs. Multivariable logistic regression assessed associations between PCE score and adult self-rated health or condition diagnosis, with and without ACEs adjustment. Cox proportional hazards models examined relationships between PCEs, ACEs, and annual risk of diagnosis.
RESULTS
Adults with 5 to 6 PCEs had 75% (95% confidence interval [CI], 0.58–0.93) of the risk of fair/poor overall health and 74% of the risk of any psychiatric diagnosis (CI, 0.59–0.89) compared with those with 0 to 2 PCEs, independent of ACEs. In survival analysis models accounting for PCEs and ACEs, reporting 5 to 6 PCEs was associated with a 16% lower annual hazard of developing any adult psychiatric or physical condition (hazard ratio, 0.84; CI, 0.75–0.94); reporting 3+ ACEs was associated with a 42% higher annual hazard (CI, 1.27–1.59).
CONCLUSIONS
PCEs were independently associated with lower risks of fair or poor adult health, adult mental health problems, and developing any physical or mental health condition at any given age after adjusting for ACEs.
What’s Known on This Subject:
Adverse childhood experiences (ACEs) have been linked to worse adult health outcomes. Positive childhood experiences (PCEs) likely protect against adult health risks, but evidence is lacking on how ACEs and PCEs jointly influence adult health outcomes, especially in nationally representative studies.
What This Study Adds:
Independent of ACEs, PCEs are associated with better self-reported adult health and lower risk of mental and physical conditions, especially among those with fewer ACEs. Higher PCE scores are also associated with lower annual risk of adult disease diagnosis.
Adverse childhood experiences (ACEs) are stressful and potentially traumatic events and family challenges occurring before adulthood.1 Ample evidence links ACEs to increased risk of common adult diseases, including heart disease, lung disease, and cancer.2–8 Medical professional organizations, health systems, and a growing number of policymakers are recognizing that ACEs drive excess morbidity and mortality at a population level.9–13 Yet the ACEs framework has been critiqued for focusing on risks without accounting for protective childhood experiences and resilience factors that may promote health and buffer long-term health effects of early adversity.14–17
Published evidence suggests positive childhood experiences (PCEs), characterized by the Centers for Disease Control and Prevention as “safe, stable, nurturing relationships and environments” before adulthood, are linked to better adult health.18–29 Common PCE domains, including positive parent–child relationships, social engagement in school, and neighborhood social cohesion, have been linked to better adult self-reported well-being, mental health, and overall health.22–27,30–34 However, these studies have been limited by analytic models omitting ACEs or other measures of early adversity, nonnationally representative samples, examination of single PCE domains rather than composite scores, and an underemphasis on physical health, focusing instead largely on mental health. Recent studies examining the association between PCEs and adult health outcomes after accounting for ACEs have found that PCEs are associated with lower risk of poor adolescent and adult mental health and greater adult flourishing.33,35,36 However, whether PCE scores are associated with adult health conditions and annual risk of diagnosis independent of ACEs has not been explored in a national sample, and no large studies have provided evidence on whether ACEs and PCEs interact in their effects on adult health outcomes.
Thus, in this study, using a nationally representative population-based survey, we examine whether PCEs are associated with overall adult health status and risk of mental and/or physical health conditions cumulatively throughout adulthood, as well as annually in any given year of adulthood, with and without ACEs and ACE-by-PCE interactions.37
Methods
Study Sample
We used data from the 2017 wave of the Panel Study of Income Dynamics’ (PSID’s, https://psidonline.isr.umich.edu/) main survey, the world’s longest-running national longitudinal household panel survey begun in 1968, which interviewed adult participants and, if eligible, their spouse or partner for information on health status, health conditions, education, income, health insurance, family structure, and demographic characteristics.37 Additionally, ACEs and PCEs were retrospectively assessed via the Childhood Retrospective Circumstances Study (CRCS) supplement, which collected data from eligible English-speaking adults who had participated in the previous 2013 main survey, well before the 2017 PSID health outcomes were collected.38 Eight thousand and seventy-two individuals completed the CRCS via Web-based or mailed survey between May 2014 and January 2015, for an unweighted response rate of 62% (weighted response rate 67%), similar to Web-based supplements in other national panel studies.38 Of those CRCS participants, 7496 (93%) had complete data.
Independent Variable
Positive Childhood Experiences (PCEs) Score
The PCEs composite score was constructed with CRCS survey items selected for their similarity to the previously published Benevolent Childhood Experiences Scale and the Children and Youth Resilience Measure scales created to measure childhood experiences associated with improved mental health outcomes (Supplemental Table 4).33,39,40 The CRCS survey retrospectively assessed positive childhood experiences in domains including their (1) comfort confiding in at least 1 parent about things that were bothering them, (2) perception that at east 1 parent understood their problems, (3) rating of their relationship with their parents, (4) happiness at school, (5) comfort with friends, and (6) perception of their neighbors’ helpfulness. Each item was first dichotomized, then summed and binned into categories (0–2, 3–4, or 5–6 PCEs) for an overall PCE score (Supplemental Table 10) with a similar distribution of scores similar to Bethell et al.33
Adverse Childhood Experiences
Our previously published ACE score41,42 used CRCS data to construct binary indicators of each of the following before age 18 years: parent mental illness, parent substance use disorder, parent intimate partner violence, parental divorce or separation, deceased or absent parent, physical abuse, sexual abuse, emotional abuse, and neglect. These were summed and binned into 3 dose-related categories (0, 1–2, and 3 or more ACEs) similar to previous studies.43,44
Outcomes: Mental and Physical Health
Fair or Poor Self-Reported Health Status
Participants rated their or their spouse/partner’s health as “excellent,” “very good,” “good,” “fair,” or “poor,” which was dichotomized to fair/poor versus excellent/very good/good.45
Health Conditions
Mental health diagnoses were measured as self-report of a physician or other clinician telling the respondent they had a diagnosis of (1) any psychiatric problem, (2) depression, or (3) anxiety (Supplemental Table 5).
Physical health diagnoses were similarly measured as report of a diagnosis of hypertension, diabetes, coronary heart disease or heart failure, heart attack, stroke, lung disease, asthma, cancer, and/or arthritis. These diagnoses were also combined into a composite indicator of any physical condition.
Age at Diagnosis
We used participants’ report of their age at the time of diagnosis. We also constructed a composite age at first diagnosis of any physical health condition, using the earliest age at diagnosis for the following conditions: hypertension, diabetes, coronary heart disease, stroke, heart attack, lung disease, arthritis, cancer, and asthma (if diagnosed in adulthood). Similarly, we constructed a composite age at first diagnosis of any physical or psychiatric health condition, using the earliest age at diagnosis of any condition (Supplemental Table 6).
Statistical Analysis
Health Condition Diagnosis
We used doubly robust inverse probability-weighted regression-adjusted models with covariate adjustment to measure the association between PCE score and adult health outcomes.46 The logistic regression model estimated the predicted risk of developing each condition for 0 to 2, 3 to 4, and 5 to 6 PCE groups, using propensity weights according to predicted probabilities of being in a particular PCE score category on the basis of age, sex, race/ethnicity, education, household income (as a percentage of federal poverty level), and health insurance (including uninsured, employer-sponsored, privately purchased, Medicare/Medigap/supplemental, Medicaid, and veterans and other government coverage). The nonlinear combinations of estimators command was used postestimation (Stata, nonlinear combinations of estimators) to convert odds ratios to relative risk ratios.47 We added the 3-category ACE score to control for ACEs, along with the covariates used for propensity weights listed above.
All models were weighted to accommodate the complex survey design, achieve population representation, and adjust for nonresponse using the CRCS survey base weights in both the propensity score and outcome models.48 All estimates employed survey-robust standard errors.
Interaction Between PCEs and ACEs
Multivariable logistic regression models with a PCE-by-ACE interaction term were used to examine how associations between PCEs and adult health outcomes varied according to an individual’s ACE burden, while also controlling for sociodemographic covariates listed above. The probability of the outcome at each PCE-by-ACE combination was estimated using the delta method (Stata, margins program), followed by calculation of absolute risk increases compared with the 0 ACEs/5 to 6 PCEs reference group.
Survival Analysis: Annual Diagnosis Risk
Survival analyses with Cox proportional hazards regression models were used to examine the relationships between PCE score and annual risk of diagnosis at a given age for 3 outcomes: any condition, any psychiatric condition, and any physical condition. We dichotomized each outcome into whether an individual reported a diagnosis at the time of the survey, using their age at diagnosis as the “time to event.” To focus on adult-onset conditions, we left-censored individuals who reported childhood diagnoses at 18 years old. Individuals who had not reported a diagnosis at the time of survey were censored using their age. We also controlled for age, sex, race/ethnicity, education, health insurance, income, and ACE count.
Sensitivity Analyses
Logistic regression models, without inverse probability-weighted regression-adjusted models, (generalized linear models [Stata, generalized linear models family (binomial) link (log)]) results matched the results from our primary approach, which was opted for because of greater ease of model convergence and estimating relative risks. ACEs were incorporated for models of outcomes with sufficient sample size to satisfy the treatment overlap assumption. Other models varied covariate specifications for parental education, marital status, and income. Another alternate model used adult health outcomes from the 2013 PSID wave. All these alternate models gave substantially similar results.
Analyses were carried out in 2019 to 2021 using Stata, version 15 (StataCorp). The University of California, Los Angeles, institutional review board approved this study.
Results
The study sample included 7496 adults (Table 1), of which 3841 (51.5%), 2467 (32.3%), and 118 (16.3%) reported 5 to 6 PCEs, 3 to 4, and 0 to 2 PCEs, respectively. Those with more PCEs were more often older, non-Hispanic white, and married, and had employer-sponsored or Medicare insurance, higher income, and more years of education.
TABLE 1.
Survey-Weighted Study Population Characteristics, Overall and by Number of PCEs
| Total | PCEs | P | |||
|---|---|---|---|---|---|
| 5–6 PCEs | 3–4 PCEs | 0–2 PCEs | |||
| Sample size, n (%) | 7496 | 3841 (51.5) | 2467 (32.3) | 1188 (16.3) | — |
| Age, mean (SE) | 53.2 (0.23) | 55.0 (0.33) | 51.4 (0.40) | 51.1 (0.57) | <.0001 |
| Sex, female, % | 52.9 | 53.1 | 48.2 | 61.6 | <.0001 |
| Race, % | .0003 | ||||
| White | 79.6 | 80.9 | 78.7 | 77.2 | |
| Hispanic | 6.1 | 4.5 | 7.6 | 8.5 | |
| Black | 11.3 | 11.6 | 11.2 | 10.7 | |
| Asian American/Pacific Islander | 1.9 | 1.8 | 1.5 | 2.6 | |
| Other | 1.1 | 1.2 | 1.0 | 1.0 | |
| Education, % | .0001 | ||||
| Less than high school | 9.2 | 7.6 | 9.9 | 12.6 | |
| High school | 24.9 | 24.0 | 26.2 | 25.0 | |
| Any college/vocational school | 66.0 | 68.4 | 63.9 | 62.4 | |
| Income, FPL, % | <.0001 | ||||
| <100% | 6.8 | 5.0 | 7.7 | 10.5 | |
| 100%–199% | 12.5 | 11.3 | 13.7 | 13.6 | |
| 200%–299% | 14.6 | 14.1 | 15.1 | 15.3 | |
| 300%–399% | 13.9 | 14.3 | 14.5 | 11.6 | |
| >400% | 52.3 | 55.3 | 49.1 | 49.1 | |
| Health insurance, % | <.0001 | ||||
| Employer-sponsored | 53.6 | 53.7 | 54.4 | 51.6 | |
| Privately purchased | 7.6 | 7.7 | 7.2 | 8.0 | |
| Medicare | 23.5 | 26.3 | 20.6 | 20.2 | |
| Medicaid | 6.2 | 4.6 | 7.1 | 9.6 | |
| VA/Tricare | 2.8 | 2.7 | 2.9 | 3.0 | |
| Other insurance | 0.2 | 0.1 | 0.3 | 0.0 | |
| Uninsured | 6.2 | 4.9 | 7.6 | 7.5 | |
| No. of ACEs, % | <.0001 | ||||
| 0 | 33.4 | 44.7 | 25.6 | 11.1 | |
| 1–2 | 45.6 | 44.1 | 49.5 | 42.5 | |
| 3+ | 21.0 | 11.2 | 24.9 | 46.4 | |
FPL, federal poverty level; VA, US Department of Veterans Affairs. —, not applicable.
PCEs, ACEs, and Adult Health Outcomes
Compared with those who reported 0 to 2 PCEs (Table 2, Supplemental Table 11), adults with 5 to 6 PCEs had a 34.6% lower risk of fair/poor self-rated health (adjusted risk ratio [aRR], 0.65; confidence interval [CI], 0.54–0.76), which was dampened to 24.6% (aRR, 0.75; CI, 0.58–0.93) after adjusting for ACEs.
TABLE 2.
Association Between PCE Score and Adult Self-Reported Health and Physical and Psychiatric Condition, Relative Risk (95% Confidence Interval)
| Outcome | Model Specification for Childhood Experiences | PCEs, aRR (95% CI) | ACEs, aRR (95% CI) | Model Specification for Childhood Experiences | ||||
|---|---|---|---|---|---|---|---|---|
| 5–6 PCEs | 3–4 PCEs | 0–2 PCEs (Ref) | 0 ACEs (Ref) | 1–2 ACEs | 3+ ACEs | |||
| Fair or poor health | PCEs only | 0.65*** | 0.87 | 1.00 | 1.00 | 1.40*** | 1.74*** | ACEs only |
| (0.55–0.76) | (0.72–1.02) | (1.14–1.67) | (1.39–2.09) | |||||
| ACEs + PCEs | 0.75* | 0.94 | 1.00 | 1.00 | 1.34*** | 1.69*** | ACEs + PCEs | |
| (0.58–0.93) | (0.71–1.16) | (1.06–1.61) | (1.29–2.08) | |||||
| Any psychiatric or physical condition | PCEs only | 0.90*** | 0.96 | 1.00 | 1.00 | 1.12*** | 1.25*** | ACEs only |
| (0.86–0.95) | (0.90–1.01) | (1.06–1.17) | (1.18–1.32) | |||||
| ACEs + PCEs | 0.92* | 0.93 | 1.00 | 1.00 | 1.08*** | 1.21*** | ACEs + PCEs | |
| (0.86–0.99) | (0.87–1.00) | (1.03–1.14) | (1.14–1.29) | |||||
| Any psychiatric condition | PCEs only | 0.57*** | 0.78** | 1.00 | — | 1.63*** | 2.38*** | ACEs only |
| (0.47–0.66) | (0.65–0.91) | (1.33–1.94) | (1.91–2.85) | |||||
| ACEs + PCEs | 0.74** | 0.90 | 1.00 | 1.00 | 1.50*** | 1.90*** | ACEs + PCEs | |
| (0.59–0.89) | (0.71–1.08) | (1.12–1.81) | (1.48–2.31) | |||||
| Any physical condition | PCEs only | 0.94* | 0.99 | 1.00 | — | 1.10*** | 1.22*** | ACEs only |
| (0.88–0.99) | (0.9–1.05) | (1.04–1.16) | (1.15–1.29) | |||||
| ACEs + PCEs | 0.93 | 0.96 | 1.00 | 1.00 | 1.07* | 1.21*** | ACEs + PCEs | |
| (0.87–1.00) | (0.89–1.03) | (1.00–1.13) | (1.13–1.29) | |||||
Results from main analytic model shown are relative risks, with 95% confidence intervals, from postestimation using inverse probability weighting with regression adjustment (Stata tefffects inverse probability-weighted regression-adjusted models, pomean; postestimation using nonlinear combinations of estimators). Covariates in the treatment model included continuous age, sex, a 5-category race/ethnicity measure, educational attainment, health insurance, and income as measured by percentage of federal poverty level. Survey weights were included in both the treatment and outcome model to accommodate the PSID’s complex survey design. Statistical significance at the 5% level is indicated:
P < .05;
P < .01;
P < .001. Ref, reference group.
Higher PCE count was associated with a lower risk of having of any psychiatric or physical condition (Table 2) after adjusting for sociodemographic characteristics. Compared with 0 to 2 PCEs, those reporting 5 to 6 PCEs had a 9.8% lower risk of reporting any condition (aRR, 0.90; CI, 0.86–0.95) and a 7.7% lower risk after adjusting for ACEs (aRR, 0.92; CI, 0.86–0.99).
When examined separately, those reporting 3 to 4 and 5 to 6 PCEs had 21.8% and 43.2% lower risk of any psychiatric diagnosis, respectively, compared with 0 to 2 PCEs. In adjusted models including both PCEs and ACEs, adults with 5 to 6 PCEs had a 26.2% reduction in risk of any psychiatric condition (aRR, 0.74; CI, 0.59–0.89), and a 37.3% reduction in depression risk (aRR, 0.63; CI, 0.44–0.81).
A higher PCE score (Table 2) was associated with a small reduction in the risk of any physical condition (5–6 PCEs: aRR, 0.94; CI, 0.88–0.99), which was not significant after controlling for ACEs (aRR, 0.93; CI, 0.87–1.00). When examined individually, higher PCE scores were associated with lower risks of developing asthma (5–6 PCEs: aRR, 0.75, CI, 0.61–0.88) which remained significant after controlling for ACEs (aRR, 0.76, CI: 0.59–0.94). There were otherwise no statistically significant associations between PCE score and the risk of other individual conditions examined (Supplemental Table 9).
Interaction Between PCEs and ACEs Measures and Adult Health Outcomes
In our interaction analyses, the PCE–ACE interaction term was statistically significant for both having any physical or psychiatric condition and having any physical condition (Fig 1, Supplemental Table 7), indicating that the strength of association between PCEs and these outcomes varied according to ACE count. Specifically, among those who reported 0 ACEs, reporting 3 to 4 PCEs and 0 to 2 PCEs were associated with an absolute increase of 5.2 (CI, 1.9–13.8) and 15.2 percentage points (95% CI, 8.3–27.7), respectively, of reporting any physical or psychiatric diagnosis, compared with the risk among those reporting 5 to 6 PCEs. In contrast, among those with 3+ ACEs, the change in absolute risk of reporting any physical or psychiatric condition did not differ significantly as PCE count increased (11.7% [CI 7.0–19.6] among those with 5–6 PCEs versus 18.0% [CI 13.5–24.0] for those with 3–4 PCEs or 15.7% [CI 11.2–22.1] for those with 0–2 PCEs). Similarly, the strength of association between PCEs and having any psychiatric condition did not vary by ACE burden (Supplemental Table 7).
FIGURE 1.
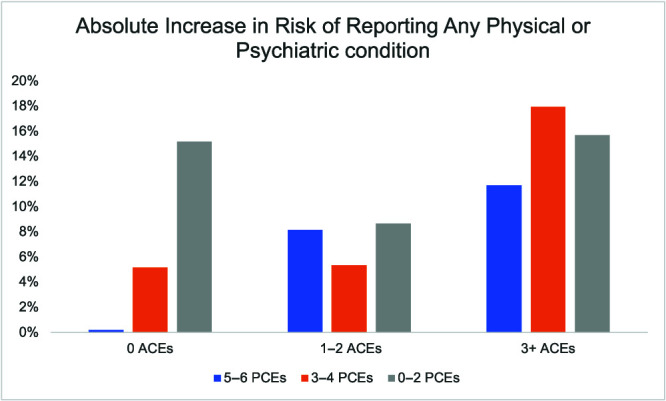
Absolute increase in risk of reporting any physical or psychiatric condition across ACEs and PCEs score (reference group: 5–6 PCEs/0 ACEs). Results from main analytic model shown are absolute risk increases from models with PCEs and ACEs scores interacted. Covariates in the treatment model included continuous age, sex, a 5-category race/ethnicity measure, educational attainment, health insurance, and income as measured by percentage of federal poverty level. Survey weights were included in both the treatment and outcome model to accommodate the PSID’s complex survey design.
Survival Analysis Using Age at Diagnosis: PCEs and ACEs
In unadjusted analyses, higher PCE scores were associated with lower likelihoods of being diagnosed with each of the following during a given year of adulthood: any psychiatric condition, any physical condition, and any psychiatric or physical condition (Table 3, Supplemental Table 8).
TABLE 3.
Hazard Ratios of Reporting Any Psychiatric Condition, Any Physical Condition, or Either during Adulthood by PCE Score and ACE Score
| PCEs Score, HR (95% CI) | ACEs Score, HR (95% CI) | |||||
|---|---|---|---|---|---|---|
| 5–6 PCEs | 3–4 PCEs | 0–2 PCEs | 0 ACEs | 1–2 ACEs | 3+ ACEs | |
| Any physical condition | ||||||
| PCE only (unadjusted) | 0.79*** | 0.94 | 1.00 | — | — | — |
| (0.70–0.88) | (0.83–1.06) | |||||
| PCEs (adjusted) | 0.84** | 0.93 | 1.00 | 1.00 | 1.18*** (1.08–1.29) | 1.54*** (1.38–1.72) |
| (0.75–0.94) | (0.83–1.05) | |||||
| PCEs + ACEs (adjusted) | 0.92 | 0.99 | 1.00 | 1.00 | 1.10* | 1.35*** |
| (0.80–1.04) | (0.87–1.13) | (1.00–1.20) | (1.20–1.52) | |||
| Any psychiatric condition | ||||||
| PCE only (unadjusted) | 0.73** | 0.83 | 1.00 | — | — | — |
| (0.58–0.92) | (0.66–1.03) | |||||
| PCE only (adjusted) | 0.84 | 0.94 | 1.00 | — | — | — |
| (0.67–1.05) | (0.76–1.17) | |||||
| PCEs + ACEs (adjusted) | 0.99 | 0.99 | 1.00 | 1.00 | 1.12 | 1.47** |
| (0.77–1.27) | (0.79–1.25) | (0.89–1.42) | (1.14–1.90) | |||
| Any psychiatric or physical condition | ||||||
| PCE only (unadjusted) | 0.72*** | 0.87* | 1.00 | — | — | — |
| (0.65–0.80) | (0.78–0.98) | |||||
| PCE OR ACE only (adjusted) | 0.78*** | 0.87* | 1.00 | — | — | — |
| (0.70–0.87) | (0.78–0.97) | (1.08–1.29) | (1.38–1.72) | |||
| PCEs + ACEs (adjusted) | 0.85** | 0.91 | 1.00 | 1.00 | 1.15*** | 1.42*** |
| (0.75–0.95) | (0.80–1.02) | (1.05–1.26) | (1.26–1.56) | |||
Results shown are the HRs, using survey-weighted Cox proportional hazards regression models. Covariates in the treatment model included continuous age, sex, a 5-category race/ethnicity measure, educational attainment, health insurance, and income as measured by percentage of federal poverty level. Statistical significance is indicated at the 5% level:
P < .05;
P < .01;
P < .001. —, not applicable.
After adjusting for sociodemographic characteristics, reporting 5 to 6 PCEs remained associated with lower annual hazard of being diagnosed with any physical condition (hazard ratio [HR], 0.84; CI, 0.75–0.94) and any psychiatric or physical condition (HR, 0.78; CI, 0.70–0.87). The association between PCEs and age at diagnosis of any psychiatric condition was not statistically significant.
Upon controlling for ACEs, the hazard for reporting being diagnosed with any psychiatric or physical condition was lower (HR, 0.85; CI, 0.75–0.95) among those reporting 5 to 6 PCEs, but upon condition of subtype disaggregation, the associations between PCE score and the risk of developing any psychiatric condition or any physical condition were no longer statistically significant.
In contrast, reporting 3 or more ACEs was associated with a 35.1% greater hazard of reporting developing any physical condition (CI 1.200–1.521), 47.2% greater hazard of developing any psychiatric condition (CI 1.139–1.903), and a 41.5% greater hazard of developing any physical or psychiatric condition (CI 1.271–1.593) in a given year.
Discussion
This is the first nationally representative study to demonstrate the relationship between PCEs and adult mental and physical health outcomes while accounting for ACEs. It is the first study to show that PCEs are not only independently associated with improved health status and reduced overall mental or physical health condition risk but also that the strength of this association varies with (ie, is statistically moderated by) an individual’s ACE score and strongest when the burden of ACEs was small. When looking at mental and physical condition diagnoses separately, this study showed a dose-dependent relationship between PCEs and risk of psychiatric conditions after controlling for ACEs. Higher PCE scores were associated with a lower annual hazard of diagnosis in adulthood of a mental or physical health condition, even after controlling for ACEs, consistent with later onset and later diagnosis.
Our study adds to the body of literature linking greater PCEs to better mental health during adulthood. Although the magnitude of the relationship between higher PCE score and lower risk of mental illness does decrease after controlling for ACE burden, the association persists. One proposed mechanism that could explain this is the “stress-buffering” hypothesis that individuals exposed to PCEs are more resilient to health challenges and this can potentially counter the effects of ACEs.49,50 Our finding that PCEs may be protective against poor adult self-reported health and mental health while controlling for ACEs is certainly consistent with this model, but we did not observe greater protective effects in those with greater ACE burden. Instead, our results suggest that PCEs offer mental health protective effects that largely operate independent of ACE burden, with a smaller additional impact at the margins through PCEs’ moderating effects on ACE health associations.33,34 This is in contrast to the findings from Bethell et al that those with the highest ACE burden experienced greater reductions from increased PCE scores in their risk of depression and poor mental health. There are many potential explanations for these different findings, including differences in how the outcomes were defined (clinician diagnoses that included anxiety in our study versus inclusion of a self-assessment of more poor than good mental health days without including anxiety by Bethell et al) and differences in study sample population (nationally representative versus Wisconsin adults).
The strength of relationship between adult physical health outcomes and PCE score differed depending on an individual’s ACE burden in our study. Although greater PCEs were associated with a slight reduction in the risk of any physical diagnosis, this was not significant after controlling for ACEs overall. However, after allowing for this association to vary across different ACE counts, PCEs were most consistently associated with a reduction in the risk of having any diagnosis (physical or psychiatric) and any physical diagnosis among those with fewer ACEs.
Our study was not sufficiently powered to find significant relationships between PCEs and individual conditions, such as diabetes and cardiovascular disease. However, when these conditions were combined into a composite measure, there was a trend toward lower hazards and thus older age at diagnosis among those with more PCEs. Thus, it is possible that any differences in specific disease prevalence across PCE groups may not have had enough time or sample to manifest. Though we lacked statistical power to see a significant effect for many individual disease diagnoses, we did find that higher PCE score was associated with older age at diagnosis specifically for any physical diagnosis. This suggests that, assuming that age at diagnosis is a proxy for age at onset, higher PCE score may protect individuals exposed to ACEs from early onset of these physical illnesses. In contrast, we did not find an association between PCEs, ACEs, and age at diagnosis for any psychiatric diagnosis during adulthood, possibly because psychiatric conditions tend to develop during the late teenage years and early adulthood and, as such, there may be very little accumulation during later adulthood where our study had greatest resolution.
Our findings suggest that PCEs play a role in enhancing health resilience, promoting healthy outcomes while also protecting from poor mental and physical health conditions.16,51,52 Previous studies have identified that positive parent–child relationships, school engagement, and neighborhood support, individual domains reflected in our composite PCE score, are critical resilience factors.53,54 Just as ACEs can represent threats to the development of caregiving relationships, increasing an individual’s allostatic load and increasing their risk of disease throughout their life course,55,56 our study of PCEs suggests that social cohesion and supportive relationships can be protective. Indeed, other studies have found lower levels of epigenetic aging and lower biomarkers associated with chronic illness among adults who reported positive childhood social relationships, even in the setting of childhood adversity, across multiple life stages.57–59 Future research should continue to examine the relationship between PCEs, ACEs, and adult health outcomes to guide the development of public health interventions that engage individuals, their families, and their communities to promote relational health.21,60
Our study used retrospective recall of ACEs and PCEs. To ameliorate potential recall bias, we used PCE and ACE measures that were reported 5 years before the reported health outcomes. Further, as in any observational study, unmeasured confounders, like many of our measured sociodemographic characteristics vary by PCE level, could have affected our findings, though we used doubly robust models to minimize confounding. The associations found cannot be interpreted as causative. Additionally, we used age at diagnosis as a proxy for age at onset of health condition; this may overestimate age at onset, particularly among those with poor access to health care.
Conclusions
This is the first national study to find an association between a composite PCE score and adult mental and physical health outcomes. Overall, our results suggest a dose-dependent buffering relationship between PCE score and risk of poor adult overall health and mental health conditions that persists after controlling for ACEs, and the relationship between PCEs and lower risks of any physical and mental health conditions varies by ACE burden. Interventions that promote PCEs may improve health across the life course.
Supplementary Material
Glossary
- ACE
adverse childhood experience
- aRR
adjusted risk ratio
- CI
confidence interval
- CRCS
Childhood Retrospective Circumstances Study
- HR
hazard ratio
- PCE
positive childhood experience
- PSID
Panel Study of Income Dynamics
Footnotes
Drs Huang and Schickedanz conceptualized and designed the study, obtained and maintained access to the data, performed the statistical analyses, and drafted the initial manuscript; Dr Halfon reviewed and revised the analytic approach and critically reviewed and revised the manuscript; Dr Sastry contributed substantially to the initial study design, reviewed and revised the analytic approach, and critically reviewed and revised the manuscript; Dr Chung contributed integrally to the study design, and reviewed and revised the analyses and initial manuscript; and all authors approved the manuscript as submitted and agree to be accountable for all aspects of the work.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2023-061264.
FUNDING: Dr Schickedanz was funded for this work by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development #K23HD099308 and Health Resources and Services Administration of the US Department of Health and Human Services award #UA6MC32492, the Life Course Intervention Research Network. Drs Halfon, Sastry, and Chung have indicated they have no financial disclosures relevant to this article to disclose. The collection of Panel Study of Income Dynamics data used in this study by the University of Michigan Institute for Social Research was partly supported by the National Institutes of Health under grant #R01 HD069609 and #R01 AG040213, and the National Science Foundation under award #SES 1157698 and #1623684. The funders had no role in the design or conduct of this study.
CONFLICT OF INTEREST DISCLOSURES: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1. Liu RS, Aiello AE, Mensah FK, et al. Socioeconomic status in childhood and C reactive protein in adulthood: a systematic review and meta-analysis. J Epidemiol Community Health. 2017;71(8):817–826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356–e366 [DOI] [PubMed] [Google Scholar]
- 3. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258 [DOI] [PubMed] [Google Scholar]
- 4. Brown DW, Anda RF, Tiemeier H, et al. Adverse childhood experiences and the risk of premature mortality. Am J Prev Med. 2009;37(5):389–396 [DOI] [PubMed] [Google Scholar]
- 5. Felitti VJ, Anda R. The Relationship of Adverse Childhood Experiences to Adult Medical Disease, Psychiatric Disorders, and Sexual Behavior: Implications for Healthcare. In The Impact of Early Life Trauma on Health and Disease: The Hidden Epidemic (pp.77–87). Cambridge, UK: Cambridge University Press; 2010 [Google Scholar]
- 6. Hayashi Y, Okamoto Y, Takagaki K, et al. Direct and indirect influences of childhood abuse on depression symptoms in patients with major depressive disorder. BMC Psychiatry. 2015;15:244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Anda RF, Brown DW, Dube SR, Bremner JD, Felitti VJ, Giles WH. Adverse childhood experiences and chronic obstructive pulmonary disease in adults. Am J Prev Med. 2008;34(5):396–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brown DW, Anda RF, Felitti VJ, et al. Adverse childhood experiences are associated with the risk of lung cancer: a prospective cohort study. BMC Public Health. 2010;10:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. American Psychological Association . Resolution on psychological issues related to child abuse and neglect. Available at: https://www.apa.org/about/policy/child-abuse-neglect. Accessed May 4, 2020
- 10. Suglia SF, Koenen KC, Boynton-Jarrett R, et al. American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Functional Genomics and Translational Biology; Council on Cardiovascular and Stroke Nursing; and Council on Quality of Care and Outcomes Research . Childhood and adolescent adversity and cardiometabolic outcomes: a scientific statement from the American Heart Association. Circulation. 2018;137(5):e15–e28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. American Heart Association . Screening for adverse childhood experiences (ACEs) and referral pathways position statement of the American Heart Association. Available at: https://www.heart.org/-/media/Files/About-Us/Policy-Research/Policy-Positions/Social-Determinants-of-Health/ACES--Screening-and-Referral-Pathways.pdf. Accessed May 4, 2020.
- 12. Lopez MA, Wong SL, Raphael JL. Health policies to address adverse childhood experiences: taking a whole child approach. Pediatr Res. 2020;88(1):8–10 [DOI] [PubMed] [Google Scholar]
- 13. Shonkoff JP, Garner AS. Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics . The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e246 [DOI] [PubMed] [Google Scholar]
- 14. Ellis WR, Dietz WH. A new framework for addressing adverse childhood and community experiences: the building community resilience model. Acad Pediatr. 2017;17(7S):S86–S93 [DOI] [PubMed] [Google Scholar]
- 15. Sege RD, Harper Browne C. Responding to ACEs with HOPE: health outcomes from positive experiences. Acad Pediatr. 2017;17(7S):S79–S85 [DOI] [PubMed] [Google Scholar]
- 16. Liu SR, Kia-Keating M, Nylund-Gibson K, Barnett ML. Co-occurring youth profiles of adverse childhood experiences and protective factors: associations with health, resilience, and racial disparities. Am J Community Psychol. 2020;65(1-2):173–186 [DOI] [PubMed] [Google Scholar]
- 17. Halfon N, Hochstein M. Life course health development: an integrated framework for developing health, policy, and research. Milbank Q. 2002;80(3):433–479, iii [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Centers for Disease Control and Prevention . Essentials for childhood: creating safe, stable, nurturing relationships and environments for all children. Available at: https://www.cdc.gov/violenceprevention/pdf/essentials-for-childhood-framework508.pdf. Accessed May 4, 2020.
- 19. Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a meta-analysis. J Adolesc Health. 2013;53(4 Suppl):S32–S38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kosterman R, Mason WA, Haggerty KP, Hawkins JD, Spoth R, Redmond C. Positive childhood experiences and positive adult functioning: prosocial continuity and the role of adolescent substance use. J Adolesc Health. 2011;49(2):180–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Garner A, Yogman M. Committee on Psychosocial Aspects of Child and Family Health, Section on Developmental and Behavioral Pediatrics, Council on Early Childhood . Preventing childhood toxic stress: Partnering with families and communities to promote relational health. Pediatrics. 2021;148(2):e2021052582. [DOI] [PubMed] [Google Scholar]
- 22. Vartanian TP, Houser L. The effects of childhood neighborhood conditions on self-reports of adult health. J Health Soc Behav. 2010;51(3):291–306 [DOI] [PubMed] [Google Scholar]
- 23. Abbott-Chapman J, Martin K, Ollington N, Venn A, Dwyer T, Gall S. The longitudinal association of childhood school engagement with adult educational and occupational achievement: findings from an Australian national study. Br Educ Res J. 2014;40(1):102–120 [Google Scholar]
- 24. Huppert FA, Abbott RA, Ploubidis GB, Richards M, Kuh D. Parental practices predict psychological well-being in midlife: life-course associations among women in the 1946 British birth cohort. Psychol Med. 2010;40(9):1507–1518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chen Y, Kubzansky LD, VanderWeele TJ. Parental warmth and flourishing in mid-life. Soc Sci Med. 2019;220:65–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Khaleque A. Perceived parental warmth, and children’s psychological adjustment, and personality dispositions: a meta-analysis. J Child Fam Stud. 2013;22(2):297–306 [Google Scholar]
- 27. Abbott-Chapman J, Gall S, Ollington N, Martin K, Dwyer T, Venn A. The association between childhood school engagement and attainment and adult education and health outcomes: preliminary findings from an interdisciplinary research project using longitudinal Australian cohort data. AARE International Research Conference. Hobart, Tasmania, Australia: 2012 [Google Scholar]
- 28. Skodol AE, Bender DS, Pagano ME, et al. Positive childhood experiences: resilience and recovery from personality disorder in early adulthood. J Clin Psychiatry. 2007;68(7):1102–1108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Crandall A, Miller JR, Cheung A, et al. ACEs and counter-ACEs: how positive and negative childhood experiences influence adult health. Child Abuse Negl. 2019;96:104089. [DOI] [PubMed] [Google Scholar]
- 30. Bellis MA, Hardcastle K, Ford K, et al. Does continuous trusted adult support in childhood impart life-course resilience against adverse childhood experiences–a retrospective study on adult health-harming behaviors and mental well-being. BMC Psychiatry. 2017;17(1):110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hillis SD, Anda RF, Dube SR, et al. The protective effect of family strengths in childhood against adolescent pregnancy and its long-term psychosocial consequences. Perm J. 2010;14(3):18–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chung EK, Mathew L, Elo IT, Coyne JC, Culhane JF. Depressive symptoms in disadvantaged women receiving prenatal care: the influence of adverse and positive childhood experiences. Ambul Pediatr. 2008;8(2):109–116 [DOI] [PubMed] [Google Scholar]
- 33. Bethell C, Jones J, Gombojav N, Linkenbach J, Sege R. Positive childhood experiences and adult mental and relational health in a statewide sample: associations across adverse childhood experiences levels. JAMA Pediatr. 2019;173(11):e193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Easterlin MC, Chung PJ, Leng M, Dudovitz R. Association of team sports participation with long-term mental health outcomes among individuals exposed to adverse childhood experiences. JAMA Pediatr. 2019;173(7):681–688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Whitaker RC, Dearth-Wesley T, Herman AN. Childhood family connection and adult flourishing: associations across levels of childhood adversity. Acad Pediatr. 2021;21(8):1380–1387 [DOI] [PubMed] [Google Scholar]
- 36. Guo S, O’Connor M, Mensah F, et al. Measuring positive childhood experiences: testing the structural and predictive validity of the Health Outcomes From Positive Experiences (HOPE) Framework. Acad Pediatr. 2022;22(6):942–951 [DOI] [PubMed] [Google Scholar]
- 37. Institute for Social Research . Panel Study of Income Dynamics. Available at: https://psidonline.isr.umich.edu/. Accessed April 30, 2020
- 38. PSID . PSID Main Interview User Manual: release 2013. Available at: http://psidonline.isr.umich.edu/data/Documentation/UserGuide2011.pdf. Accessed May 4, 2020
- 39. Narayan AJ, Rivera LM, Bernstein RE, Harris WW, Lieberman AF. Positive childhood experiences predict less psychopathology and stress in pregnant women with childhood adversity: A pilot study of the benevolent childhood experiences (BCEs) scale. Child Abuse Negl. 2018;78:19–30 [DOI] [PubMed] [Google Scholar]
- 40. Liebenberg L, Ungar M, LeBlanc JC. The CYRM-12: a brief measure of resilience. Can J Public Health. 2013;104(2):e131–e135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Schickedanz AB, Escarce JJ, Halfon N, Sastry N, Chung PJ. Adverse childhood experiences and household out-of-pocket health care costs. Am J Prev Med. 2019;56(5):698–707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Schickedanz A, Halfon N, Sastry N, Chung PJ. Parents’ adverse childhood experiences and their children’s behavioral health problems. Pediatrics. 2018;142(2):e20180023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Bethell C, Gombojav N, Solloway M, Wissow L. Adverse childhood experiences, resilience and mindfulness-based approaches: common denominator issues for children with emotional, mental, or behavioral problems. Child Adolesc Psychiatr Clin N Am. 2016;25(2):139–156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bright MA, Knapp C, Hinojosa MS, Alford S, Bonner B. The comorbidity of physical, mental, and developmental conditions associated with childhood adversity: a population-based study. Matern Child Health J. 2016;20(4):843–853 [DOI] [PubMed] [Google Scholar]
- 45. Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self-rated health status as a health measure: the predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J Clin Epidemiol. 1997;50(5):517–528 [DOI] [PubMed] [Google Scholar]
- 46. Wooldridge JM. The MIT Press . Econometric analysis of cross section and panel data. Available at: https://books.google.com/books?hl=en&lr=&id=hSs3AgAAQBAJ&oi=fnd&pg=PP1&dq=Econometric+Analysis+of+Cross+Section+and+Panel+Data.+2nd+ed.+Cambridge,+MA:+MIT+Press.&ots=VXUTkBT1No&sig=1jmdfY9d6h0w0BHJYknTW7e-_4E#v=onepage&q=Econometric. Accessed July 5, 2020
- 47. StataCorp . Nlcom–nonlinear combinations of estimators. Available at: www.stata-press.com/data/r13/regress. Accessed May 4, 2020
- 48. Ridgeway G, Kovalchik SA, Griffin BA, Kabeto MU. Propensity score analysis with survey weighted data. J Causal Inference. 2015;3(2):237–249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Cheong EV, Sinnott C, Dahly D, Kearney PM. Adverse childhood experiences (ACEs) and later-life depression: perceived social support as a potential protective factor. BMJ Open. 2017;7(9):e013228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cohen S. Social relationships and health. Am Psychol. 2004;59(8):676–684 [DOI] [PubMed] [Google Scholar]
- 51. Beutel ME, Tibubos AN, Klein EM, et al. Childhood adversities and distress–the role of resilience in a representative sample. PLoS One. 2017;12(3):e0173826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lau SYZ, Guerra RO, Barbosa JFS, Phillips SP. Impact of resilience on health in older adults: a cross-sectional analysis from the International Mobility in Aging Study (IMIAS). BMJ Open. 2018;8(11):e023779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Collishaw S, Pickles A, Messer J, Rutter M, Shearer C, Maughan B. Resilience to adult psychopathology following childhood maltreatment: evidence from a community sample. Child Abuse Negl. 2007;31(3):211–229 [DOI] [PubMed] [Google Scholar]
- 54. Masten AS, Barnes AJ. Resilience in children: developmental perspectives. Children (Basel). 2018;5(7):98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Gruenewald TL, Karlamangla AS, Hu P, et al. History of socioeconomic disadvantage and allostatic load in later life. Soc Sci Med. 2012;74(1):75–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. McEwen BS. Stressed or stressed out: what is the difference? J Psychiatry Neurosci. 2005;30(5):315–318 [PMC free article] [PubMed] [Google Scholar]
- 57. Carroll JE, Gruenewald TL, Taylor SE, Janicki-Deverts D, Matthews KA, Seeman TE. Childhood abuse, parental warmth, and adult multisystem biological risk in the Coronary Artery Risk Development in Young Adults study. Proc Natl Acad Sci USA. 2013;110(42):17149–17153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Brody GH, Miller GE, Yu T, Beach SRH, Chen E. Supportive family environments ameliorate the link between racial discrimination and epigenetic aging: a replication across 2 longitudinal cohorts. Psychol Sci. 2016;27(4):530–541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Yang YC, Boen C, Gerken K, Li T, Schorpp K, Harris KM. Social relationships and physiological determinants of longevity across the human life span. Proc Natl Acad Sci USA. 2016;113(3):578–583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, Harvey SB. Road to resilience: a systematic review and meta-analysis of resilience training programs and interventions. BMJ Open. 2018;8(6):e017858. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


