Abstract
Background:
The Park Rx study is a prospective, randomized controlled trial implemented within a federally qualified health center serving a low-income population in Washington, DC.
Design and setting:
The 5-year randomized controlled trial will recruit 500 children, ages 6–16 to be randomized to receive either a park prescription (Park Rx) during routine clinical visits (intervention arm) or care as usual (control arm).
Intervention:
Park prescriptions promote both physical activity and exposure to nature. The prescription includes a place (i.e., park), an activity, a frequency, and a duration. Compared to usual care, we expect children receiving a park prescription will have greater physical activity levels and improved physical and mental health outcomes.
Implications:
The results of the Park Rx trial will demonstrate the efficacy of the intervention and whether it will increase time spent in nature-rich areas (i.e., parks); have any biological impacts on health, including reducing hypercholesterolemia, hypertriglyceridemia, HbA1c, body mass index (BMI), and impact mental health, including stress and cognitive functioning.
Trial Registration:
ClinicalTrials.gov identifier: NCT04114734. Registered on October 3, 2019.
Keywords: Physical activity, Nature, Children, Outdoor play, Mental health, Nature prescription, Park prescription
1. Introduction: Rationale for the Park Rx trial
1.1. Health benefits of physical activity, outdoor activity, and nature exposure
Regular physical activity provides multiple health benefits [1] including reduced risk of cardiovascular disease, hypertension, hyperlipidemia and Type 2 diabetes, colon cancer, osteoporosis, depression, and other chronic diseases. Physical activity increases lean body mass and contributes to the control of body weight. In addition, physical activity increases bone mass, reduces sleep disorders, and improves psychological well-being among adults and children [2-4]. Time spent outdoors is associated with increased physical activity among children [5] and lower chronic disease rates in a population-based sample of working age American adults in the National Health and Nutrition Examination Survey (NHANES) for 2009–2012 [6]. Although most of the benefits of physical activity have been documented in adult populations, research suggests that habitual physical activity also benefits children, not only to support motor skills, healthy muscle development and bone growth [7], but also to reduce the risk of cardiovascular disease [8], obesity [9], hypertension [10] and hyperlipidemia [11]. Yet participation in physical activity declines among U.S. youth as they age [12].
While physical activity alone has benefits, physical activity outdoors may have additional positive effects beyond the well-recognized cardiovascular benefits, including reductions of psychological stress, blood pressure, heart rate and cortisol and improved cognitive function [13-15]. Recent studies have investigated the role of spending time outdoors in nature, not only on stress, but also on cognitive skills, including a variety of constructs associated with learning, self-control and attention [15-19]. There is growing evidence suggesting that children who spend more time in green space have better cognitive functioning [20], fewer behavioral problems and lower rates of hyperactivity than children who don't play outdoors [21]. There is some evidence that contact with nature is a factor that can ameliorate ADHD [22], lower blood pressure, and improve cognitive functions [23,24]. Nevertheless, some studies show no impact for adults [25,26] and others that used accelerometry to measure the impact of nature exposure on physical activity in children showed increases in light physical activity, but no changes in moderate-to-vigorous physical activity [27,28]. Systematic reviews of nature and health outcomes for both children and adults are mixed, indicating a need for stronger designs [29-31]. A recent systematic review of 108 studies that evaluated nature and physical activity among children showed that 66% had positive associations [32].
1.2. Promoting physical activity, outdoor activity, and nature exposure among children in the U.S
Because patterns of physical activity (outdoor and indoor) are often established in childhood and persist over time, it is important to establish routine physical activity habits as early as possible [33]. However, the transition from childhood to adolescence is associated with a 34% decline in physical activity in girls [34]. Lower rates of leisure physical activity among low-income groups likely contribute to health disparities that are ultimately manifested in disproportionate rates of chronic diseases [35,36].
In the US an estimated 40% of children live in poverty or near the poverty level [37]. Low-income children have lower levels of achievement, worse health, and more behavioral and emotional problems than children who are more advantaged [37,38]. The sources of these disparities are many and include lower levels of cognitive stimulation and higher levels of stress [37,38]. Both physical activity and exposure to nature have been associated with stress reduction and better cognitive functioning [15-19,39]. That low-income populations spend less of their leisure time in physical activity and less time in outdoor settings than higher income populations, and use parks at a lower frequency than higher income groups [40] may, in part, explain health and achievement disparities.
Public parks provide free physical activity opportunities, potentially more attractive than indoor physical activity. Neighborhood parks are designed for moderate-to-vigorous physical activity (MVPA) and are the preferred site of leisure time physical activity in many communities, particularly among minority and disadvantaged groups that cannot afford to join health clubs or may not have access to them [41]. Both youth and seniors are more physically active when outdoors [42,43]. Adolescents are more likely to engage in physical activity, and achieve their highest physical activity levels outdoors [44]. Most localities maintain parks, and most Americans in urban communities have a park within a half-mile radius of their homes [45]. However, neighborhood parks in communities across the US are generally underutilized and provide limited programming that supports moderate-to-vigorous physical activity (MVPA), particularly in low- income neighborhoods [46]. The National Study of Neighborhood Parks found that every 10% increase in neighborhood poverty level was associated with 20% fewer visitors in local playgrounds [47]. From the population health perspective, neighborhood parks have the potential to support much more leisure-time physical activity than what they currently do. Park prescriptions were developed to encourage patients to engage in more physical activity and spend time outdoors in natural settings.
1.3. Study design
1.3.1. Overview of the intervention
A park prescription is a formal clinical recommendation to be active outdoors. During routine primary care visits for well child care and chronic care follow up, providers engage the participant in brief dialogue to ask questions of the participant/family regarding where they feel safe and comfortable outside (most often a park), what they enjoy doing outside (an activity), how many times per week and on which days they can commit to an activity (frequency), and for how many minutes or hours (duration). Providers are trained to ask about safety, comfort, interests, and schedules. In this way, the prescription becomes a consensus between the family and the provider to ensure the plan is feasible and allows parental support, but is also flexible to allow, when appropriate, other family members or acquaintances to chaperone, or older children to fill the prescription on their own. This brief physician intervention affords a unique opportunity for the provider to use their medical expertise to maximize therapeutic potential, safely. While using the parkrxamerica.org platform, the provider creates a park prescription which must include a park or other nature-rich environment, an activity, a frequency, and a duration of time (i.e., walk your dog with your sister at Garrison Park, every day, for 30 min).
Providers use the park prescription platform, known as Park Rx America, which is a searchable park database (aka park formulary) that allows health providers to search for parks by address, landmarks and park amenities. Using the same platform, the provider sends the participant an electronic reminder (SMS text or email), commensurate with the frequency of the prescription (e.g., every day). The provider then reminds the participant and family to check their text/email, to answer 1–2 research questions, and log every time they fill their park prescription. Providers then document the park prescription in the electronic health record by pasting the exact prescription from the platform back into the electronic health record in the treatment section of the participant's note, corresponding to an ICD 10 diagnostic code. This entire process takes on average 2–3 min of provider time, and is done in lieu of more general advice about the importance of exercising or moving more.
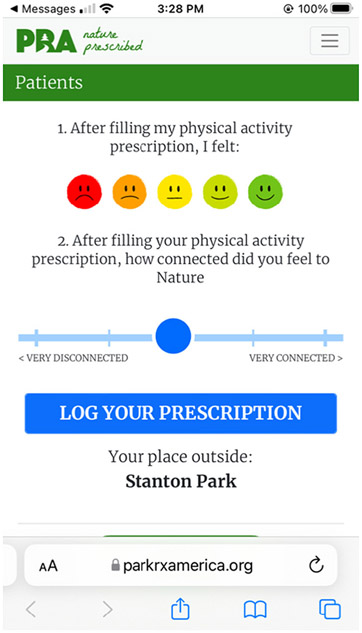
The prescription is provided both verbally and patients are given a printed prescription. In addition, patients are sent a reminder by text or email, showing which park was prescribed. (See Fig. 1) The reminder asks participants to log that they filled their prescription on ParkRxAmerica.org either during or after their park visit, after they answer questions about mood and nature connectedness. They can only log 1 park prescription per day. The Park Rx America platform records when the park was prescribed, which parks were prescribed, who prescribed the park, and when the patient logs a visit to the park.
Fig. 1.
SMS/text message reminder from ParkRxAmerica.org
Depending on the complexity of chronic disease and other clinical considerations of each participant, the provider then schedules a follow up appointment, generally with a maximum interval of three months, between one visit and the next. Every time the participant returns for a follow-up routine visit, the provider uses a unique park prescription code (found in the previous clinical note) to review how many times the previous park prescription was filled through their individualized parkrxamerica.org account. After weighing the success and barriers of the previous park prescription in the context of the participant's medical conditions, the provider re-engages the participant by asking questions of safety, comfort, activity and commitments to frequency and duration, in order to generate a new unique park prescription. This process repeats itself approximately every three months for the duration of study enrollment (24 months).
Given the onset of COVID-19 epidemic and restrictions on movement, with provider and patient hesitancy in issuing and filling park prescriptions respectively, we trained and encouraged providers to issue nature prescriptions, which can be customized to a place other than a park and where physical activity is possible. Henceforth, “park prescription” and “nature prescription” will be used interchangeably.
1.3.2. Experimental design
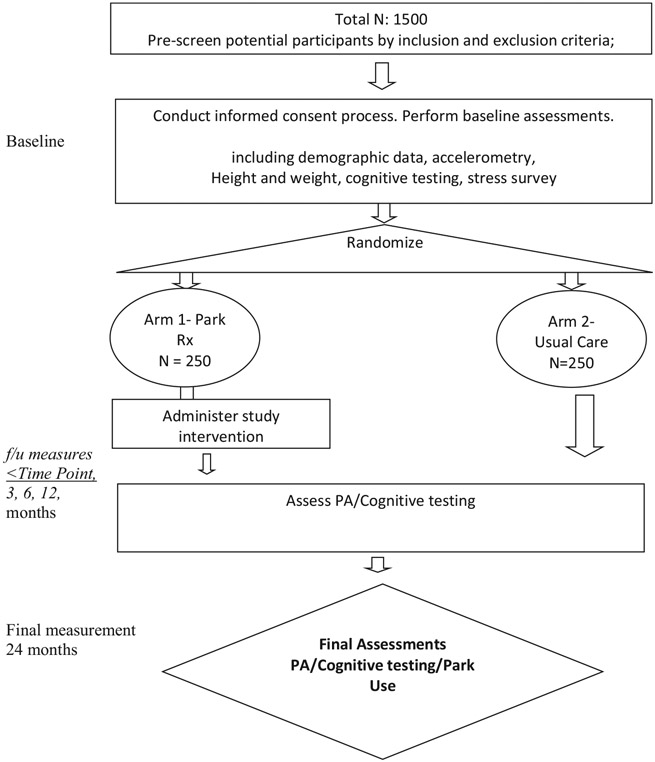
This study is a longitudinal, two-arm, randomized controlled trial. (See Fig. 2) The intervention arm (250 participants) is receiving routine medical attention, including a park prescription, at regular intervals (ranging from every 1 to 3 months). The control arm (250 participants) is receiving only routine medical attention. Each enrolled participant will take a baseline measurement before any intervention takes place. Scheduled follow-up times are at 3, 6, 12, and 24 months after the baseline. Enrolled patients will be blocked by gender, age group and health status jointly. Age groups are defined as ages 6–9 and ages 10–16. Health status groups are defined as 1) having overweight/obesity only and no other conditions, or 2) at least one chronic condition (e.g., high triglycerides/cholesterol/pre-diabetes, Type2 diabetes, ADHD). A patient with chronic conditions may or may not be overweight/obese. This yields a total of eight blocks (gender by age group by health condition). Within each block, we will use a sequence of random numbers to assign participants into the two study conditions.
Fig. 2.
Flow diagram.
1.3.3. Eligibility criteria
An eligible individual must meet all of the following criteria: 1) Informed assent and parental informed consent to participate in the study; 2) Stated willingness to comply with all study procedures and availability for the duration of the study; 3) Pediatric patients ages ≥6 and ≤ 16 with one or more diagnoses of chronic conditions that usually require two or more routine health care provider visits per year; 4) One or more eligible diagnoses (ADHD, Overweight or obesity, hypertriglyceridemia or hypercholesterolemia, pre-diabetes and Type 2 diabetes); 5) Having not already received a prior nature prescription; and 6) Likely to live in the Washington DC area in the next 2 years.
Exclusion criteria include: 1) Individuals who have previously been given a park prescription; 2) Activity restrictions that limit one's ability to engage in intense physical activity; 3) Individuals with a sibling already enrolled.
1.3.4. Recruitment and adjustments due to SARS-COV-2
The commencement of study participant recruitment (March 2020) coincided with some of the earliest pandemic lock-down mandates. Given the closing of clinics where we had intended to conduct in-person recruitment, we had to change to a remote recruitment protocol. Bilingual Spanish-English research assistants are responsible for recruitment. Based on age and eligibility criteria, a list of eligible patients was developed. Initially, a letter was sent to all eligible patients informing them that they may receive a call about the study. Research assistants called eligible families, explained the study details, the need to wear an accelerometer for one week at each of the study visits (baseline, 3, 6, 12 and 24 months) and the $40 incentive offered at measurement. Patients who consent are randomized to one of the two study arms. All materials are available in English and Spanish. Baseline measures, including surveys and accelerometry, are collected before participants are randomized.
1.3.5. Process evaluation
Providers are observed at least one time during a patient visit. Observers document how closely the providers followed the protocol, including the documentation of prescribing a place for outdoor physical activity, a frequency and duration. Table 1 lists the specific items documented.
Table 1.
Items in the process evaluation.
| 1 | Did the provider prescribe review previous prescription in PRA platform? |
| 2 | Did the provider prescribe time outdoors? |
| 3 | Did the prescription include a location (e.g., park)? |
| 4 | Did the prescription include an activity (e.g., play basketball)? |
| 5 | Did the prescription include frequency (e.g., once a week)? |
| 6 | Did the prescription include duration (e.g., 30 min per visit)? |
| 7 | Did the provider ask parent/child permission to send a reminder? |
| 8 | Did the provider send a reminder to parent/child by email or text? |
| 9 | Did the reminder include frequency? (e.g., days of week)? |
| 10 | Did the reminder include duration? (e.g., 1 week, 1 mo)? |
| 11 | Did the provider ask the parent/child to open their email or text? |
| 12 | Did the provider ask the parent/child to click on the embedded link? |
| 13 | Did the provider remind parent/child to consent and agree to terms and conditions? |
| 14 | Did the provider remind the parent/child to log every prescription? |
| 15 | Did the provider document the prescription in the child's medical record? |
| 16 | Did the provider print and sign the prescription? |
| 14 | Did the provider avoid using the phrase park/nature prescription? |
After the observation, feedback is provided with the intent to improve and standardize the nature prescription, the reminder, and documentation in the electronic health record. In addition to the online training and observations, every park prescription is tracked and followed by the study team, to ensure adherence to the study protocol. We will be able to report the percentage participation in the study as well as the percentage that fills the prescription as ordered.
1.3.6. Data collection protocol
Once enrolled participants are given an accelerometer (GT3X) to wear for 7 days on their waist. Caregivers do not need to keep a log of the wear time, as this is automatically captured by the accelerometer. Because in-person visits were not possible and the mail was unreliable, deliveries and pickups were scheduled with a driver. Surveys assessing behavior, including self-reported park visits, stress, cognition and use of electronic media are conducted over the phone.
1.3.7. Participant discontinuation from the study
Study participants are free to withdraw from participation in the study at any time upon request. The reason for participant discontinuation or withdrawal from the study is recorded on a Case Report Form (CRF). A participant is considered lost to follow-up if he or she fails to return for 4 subsequent scheduled visits and study staff are unable to contact the participant after at least 5 attempts.
1.3.8. Primary outcome measures
The first primary outcome is accelerometer-measured moderate-tovigorous physical activity (MVPA) as measured by Actigraph GT3x accelerometers. In the literature MVPA cutpoints for children have varied between 500 and 3200 counts per minute [48,49] while others use agespecific cutpoints [12]. We chose 3000 counts/per minute as the cutpoint to initially evaluate the data, but given that our outcome will be the difference between baseline and follow-up this choice will not have a major effect on the intervention outcome. Ultimately we will also analyze the data using the Freedson cutpoints recommended by age group [48]. Although we are striving to have participant wear the accelerometers for 1 week during all waking hours, we will analyze all data with over 400 min of wear time/day, and compare this to results with more rigorous wear time of at least 4 days and 10 h per day. In the literature, the minimum requirement for wear time varies between 8 and 12 h per day for 3–4 days [50,51]. We chose the minimum requirement of 8 h for 3 days of the week, which reduces the need for re-wears, and does not appear to alter data quality [50,51].
The second primary outcome is self-reported park use. In addition to collecting data from the Park Rx America's platform in which participants report their park use as filling the prescription, we ask participants to self-report their park use at every measurement visit. We also ask participants in the control group to answer the same questions about park use at their interim visits. We ask participants to report how often they visit any parks in the last week and month, how long they stayed, and what their primary activity was at the park. Questions about park use and frequency have been previously validated [52].
1.3.9. Secondary outcome measures
Secondary outcomes include BMI/BMI percentile extracted from the electronic health record and a set of biomarkers (cholesterol, triglycerides, and HbA1c). We are using the Perceived Stress Score (PSS 10) which is a validated scale with a 5-option Likert responses for adults and youth with a junior high education [53,54]. We are using the PSS-C (Perceived Stress Scale for Children), for children with less than a junior high education [55].
Given the ongoing restrictions on in-person research activity within Unity Health Care Inc.'s health center sites and the need for remote recruitment, cognition is now being captured by the PROMIS Pediatric Short Form v1.0 - Cognitive Function 7a and the PROMIS Parent Proxy Short Form v1.0 - Cognitive Function 7a questions from the NIH Toolbox [56]. If the participant is between 8 and 16 years old, both the parent and the child complete the PROMIS questions. If the participant is ≥6 but <8, only the parent is asked the PROMIS questions.
2. Specific aims
Aim 1- To test whether park prescriptions will increase park visits and accelerometry-measured physical activity among children, Hypothesis: Children prescribed park prescriptions will visit parks more frequently and accrue more weekly MVPA than similar children not prescribed park prescriptions.
Aim 2- To identify any biological impacts of park prescriptions on health, including impact on hypercholesterolemia, hypertriglyceridemia, HbA1C, overweight and obesity, for those patients with relevant diagnoses. Hypothesis: Children prescribed park prescriptions will have more favorable improvements in biomarkers than similar children who do not get the park prescriptions.
Aim 3- To explore impacts on mental health, including stress and measures of cognitive functioning. Hypothesis: Children prescribed park prescriptions will have more favorable improvements in stress and cognitive functioning than similar children who do not get the park prescriptions. Study hypotheses under Aims 1 to 3 will be tested by a set of repeated-measure regression models.
Aim 4- To determine whether there are age and gender differences in adherence to and impact of park prescriptions. Under this aim we address age group differences as well as sex as a biological variable.
2.1. Statistical analysis plan
We propose to implement intent-to-treat (ITT) analysis under all aims, where the treatment condition is based on randomized assignment rather than actual compliance (e.g., whether a patient will visit a park). We anticipate a low- to moderate-level of attrition in study participants (an attrition is defined as lacking all follow-up measurements) given the financial incentive and retention efforts, as well as the intervention being concurrent with their routine medical visits. Unless patients change providers or they intentionally drop out, we will be able to assess outcomes in their electronic health records. Since all predictors are measured at baseline, we will be able to apply the standard missing at random (MAR) assumption to account for missing data in the outcome by properly conditioning on covariates which are correlated with the propensity for attrition. In the case of high correlation between (some) covariates and missingness, we will do weighting adjustment in all statistical analyses, where weights are the conditional probability of observing a data point given the predictors. Statistical models will be fitted by quasi-likelihood where the classic likelihood is weighted to adjust for the propensity of observing the data point. We will fit longitudinal regression models and test the treatment effects for each follow-up wave separately. Aims 1 to 3 will be based on the same model equation with different distributional specifications for the corresponding outcome measures. Aim 4 will expand the model to subgroup analyses by gender and age groups. Analysis under all aims will be expanded to test potential moderations, including effect moderation by neighborhood-level variables (park quality, size, local population density, local poverty level) and individual-level variables. Due to the limited sample size and the relatively large number of moderators, we will test only one moderator a time to examine the marginal moderating relationship. All analyses will be performed using SAS 9.4.
2.2. Power analysis
Our plan is to recruit 500 participants allowing for a 20% drop-out rate over time. Under the regular setting of power > 0.80 and two-sided p-value<.05 we can detect a standardized effect size of 0.28 times SD of an outcome and 0.40 times SD for a subgroup analysis with a half of the total sample size. Our preliminary data from the first 78 participants suggest that the SD of daily MVPA time is 14.6 min and varies between 9 and 18 min by subgroups. The detectable effect sizes are translated to 4.1 min overall and 2.5 to 5 min by subgroups.
For reference, the sample mean of the baseline outcome is 10.7 min/person*day for all MVPA.
3. Discussion
3.1. Contextual barriers
The National Capital Region, including Washington DC, and parts of Maryland and Virginia, all experienced varying degrees of lockdown, with restrictions placed on public gatherings, especially in public places, including parks at the beginning of our study. In addition, mask mandates were also passed, in an effort to further decrease the person-toperson transmission of COVID-19. Especially during the first half of 2020, our study team observed both a hesitancy in providers' willingness to prescribe parks, and in participant families' comfort level with spending time outdoors, especially in parks. Early on in the lockdown, this meant that participants in the intervention arm might be limited to a backyard, a patio, a balcony or open window overlooking green space, or even a neighborhood sidewalk lined with trees.
As the vast majority of our study participants transitioned from in-person to online learning in March 2020, schools were struggling to create online curricula to meet every student's needs, with a focus on equity. It is unclear to us, at this time, how this change from in-person to online learning, and the paucity or absence of physical education, which for most students in the National Capital Region, lasted from March 2020 through June 2021, will impact our study results. In particular, it is unclear how this sudden and dramatic change in the daily life of a student, might impact each participant's ability and probability of filling their park prescription.
The increase in racial unrest, fueled by police brutality, in the summer of 2020, presented another potential barrier for our study participants to spend time outdoors time in public spaces. Nearly all our participants are BIPOC (black, indigenous, people of color), and would be at higher risk of experiencing a negative encounter with lawenforcement, when compared to White counterparts. In addition to being BIPOC (black indigenous people of color), many of our participants are immigrants, and/or whose parents/guardians are foreignborn. 2020 was an election year, with a concomitant rise in antiimmigrant sentiment, and in racially-motivated crime.
On January 6, 2021, another unusual event occurred in Washington DC, at the United States Capitol Building, an insurrection. For people living in Washington DC, freedom of movement was again restricted, and shortly after the insurrection, a barbed wire fence perimeter was erected around the perimeter of the US Capitol Grounds, which remained in place for more than two months. The US Capitol Grounds is a 58-acre park and an accredited arboretum. For many people living near the US Capitol, the Capitol Grounds fill an important public health need, access to green space. The insurrection and subsequent restricted access to the US Capitol Grounds, undoubtedly impacted movement of people through one of Washington, DC's largest parks.
Another barrier was the sudden transition from in-person visits to telemedicine visits. March 2021 was beginning of incorporating telemedicine visits into provider schedules, at Unity Health Care Inc. The practice of telemedicine at Unity was new to both patients and providers. Not all visit types lent themselves well to the format of telemedicine. Most of the study participants are low-income, and live in crowded housing, which adds another layer of difficulty to safeguarding patient privacy. Unreliable Wi-Fi and shared indoor spaces present a challenge to both providers and patients. With regard to the intervention, it was initially not unusual for providers to shed doubt as to the feasibility of issuing a park prescription in such less-than-ideal environments. Fortunately, Park Rx America's nature prescribing platform was designed to be used both in-person and for virtual visits. However, the absence of face-to-face interaction with participant families, during telemedicine visits, resulted in difficulty in providers' confirming participants' receipt of the park prescription reminder text or email.
Because our study team had no face-face contact with participants, we could not hand them accelerometers or the incentive gift cards. We found the mail to be unreliable and encountered many problems with mailboxes broken into and mail stolen. We therefore hired a driver to deliver and retrieve the accelerometers, and sent the gift cards electronically. Because gifts cards were delivered electronically, some families had trouble redeeming them. This has resulted in frequent complaints from participating families, and some have withdrawn because of their frustration with redeeming gift cards.
Lastly, we should note that our study team's physical presence was and continues to be largely absent at Unity Health Care Inc.'s nine community health centers, except on a few occasions when supplies and incentives for providers and clinic staff are dropped off. As we quickly transitioned from an in-person study team to a virtual one, we noticed insufficient time to do the work of recruitment, enrollment, and measurements (both surveys and accelerometry). In an effort to accommodate for the absence of our study team presence, we regularly send communications electronically (texts, emails, eClinicalWorks messages) to keep the line of communication open with providers.
3.2. Implications
Overall, we have made a variety of accommodations, outlined above, to address the barriers and limitations imposed on us by COVID-19 pandemic, racial unrest, and an insurrection. The findings from this study will reflect real-world conditions and will elucidate the impact of park prescriptions on a low-income population. Because the times have been so unusual, there is a risk that the findings may not be generalizable to other settings and populations.
Acknowledgements
This work was supported by the National Heart Lung and Blood Institute, # RO1HL147574.
Footnotes
Declaration of Competing Interest
Dr. Robert Zarr is founder and medical director of Park Rx America, a non-profit organization that developed and maintains parkrxamerica.org (website and nature prescribing platform) which is used as the intervention tool in this clinical trial.
Data availability
Data will be made available on request.
References
- [1].U.S. Department of Health and Human Services, Physical Activity and Health: A Report of the Surgeon General, U.S. Department of Health and Human Services, Atlanta, 1996. [Google Scholar]
- [2].USDHHS, The Surgeon General's Vision for a Healthy and Fit Nation. http://www.surgeongeneral.gov/priorities/healthy-fit-nation/obesityvision2010.pdf, 2010. [PubMed]
- [3].USDHHS, Physical Activity Guidelines for Americans, 2nd ed., 2018. https://health.gov/sites/default/files/2019-09/Physical_Activity_Guidelines_2nd_edition.pdf. [Google Scholar]
- [4].Sothern MS, Loftin M, Suskind RM, Udall JN, Blecker U, The health benefits of physical activity in children and adolescents: implications for chronic disease prevention, Eur. J. Pediatr 158 (4) (1999) 271–274. [DOI] [PubMed] [Google Scholar]
- [5].McKenzie TL, Sallis JF, Nader PR, et al. , BEACHES: an observational system for assessing children’s eating and physical activity behaviors and associated events, J. Appl. Behav. Anal 24 (1) (1991) 141–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Beyer KMM, Szabo A, Hoormann K, Stolley M, Time spent outdoors, activity levels, and chronic disease among American adults, J. Behav. Med 41 (4) (2018) 494–503, 10.1007/s10865-018-9911-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Loprinzi PD, Cardinal BJ, Loprinzi KL, Lee H, Benefits and environmental determinants of physical activity in children and adolescents, Obes. Facts 5 (4) (2012) 597–610. [DOI] [PubMed] [Google Scholar]
- [8].Rowland TW, The role of physical activity and fitness in children in the prevention of adult cardiovascular disease, Prog. Pediatr. Cardiol 12 (2) (2001) 199–203. [DOI] [PubMed] [Google Scholar]
- [9].Hager RL, Tucker LA, Seljaas GT, Aerobic fitness, blood lipids, and body fat in children, Am. J. Public Health 85 (12) (1995) 1702–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Hagberg JM, Goldring D, Ehsani AA, et al. , Effect of exercise training on the blood pressure and hemodynamic features of hypertensive adolescents, Am. J. Cardiol 52 (7) (1983) 763–768. [DOI] [PubMed] [Google Scholar]
- [11].Tolfrey K, Jones AM, Campbell IG, The effect of aerobic exercise training on the lipid-lipoprotein profile of children and adolescents, Sports Med. 29 (2) (2000) 99–112. [DOI] [PubMed] [Google Scholar]
- [12].Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M, Physical activity in the United States measured by accelerometer, Med. Sci. Sports Exerc 40 (1) (2008) 181–188. [DOI] [PubMed] [Google Scholar]
- [13].Richardson EA, Pearce J, Mitchell R, Kingham S, Role of physical activity in the relationship between urban green space and health, Public Health 127 (4) (2013) 318–324. [DOI] [PubMed] [Google Scholar]
- [14].Francis J, Wood LJ, Knuiman M, Giles-Corti B, Quality or quantity? Exploring the relationship between public open space attributes and mental health in Perth, Western Australia, Soc. Sci. Med 74 (10) (2012) 1570–1577. [DOI] [PubMed] [Google Scholar]
- [15].Stigsdotter UK, Ekholm O, Schipperijn J, Toftager M, Kamper-Jorgensen F, Randrup TB, Health promoting outdoor environments–associations between green space, and health, health-related quality of life and stress based on a Danish national representative survey, Scand. J. Public Health 38 (4) (2010) 411–417. [DOI] [PubMed] [Google Scholar]
- [16].Beyer KM, Kaltenbach A, Szabo A, Bogar S, Nieto FJ, Malecki KM, Exposure to neighborhood green space and mental health: evidence from the survey of the health of Wisconsin, Int. J. Environ. Res. Public Health 11 (3) (2014) 3453–3472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Kondo MC, Jacoby SF, South EC, Does spending time outdoors reduce stress? A review of real-time stress response to outdoor environments, Health Place 51 (2018) 136–150. [DOI] [PubMed] [Google Scholar]
- [18].Ward Thompson C, Aspinall P, Roe J, Robertson L, Miller D, Mitigating stress and supporting health in deprived urban communities: the importance of green space and the social environment, Int. J. Environ. Res. Public Health 13 (4) (2016) 440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Louv R, Last Child in the Woods: Saving Our Children From Nature-Deficit Disorder, Algonquin Books, Chapel Hill, NC, 2005. [Google Scholar]
- [20].Schutte AR, Torquati JC, Beattie HL, Impact of urban nature on executive functioning in early ann middle childhood, Environ. Behav 49 (1) (2017) 3–30. [Google Scholar]
- [21].Flouri E, Midouhas E, Joshi H, The role of urban neighborhood green space in children’s emotional and behavioral resilience, Jl Environ. Psych 40 (2014) 179–186. [Google Scholar]
- [22].McCormick R, Does access to green space impact the mental well-being of children: a systematic review, J. Pediatr. Nurs 37 (2017) 3–7. [DOI] [PubMed] [Google Scholar]
- [23].Bowler DE, Buyung-Ali LM, Knight TM, Pullin AS, A systematic review of evidence for the added benefits to health of exposure to natural environments, BMC Public Health 10 (1) (2010) 456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Christiana RW, Battista RA, James JJ, Bergman SM, Pediatrician prescriptions for outdoor physical activity among children: a pilot study, Prev. Med. Rep 5 (2017) 100–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Annerstedt M, Ostergren PO, Bjork J, Grahn P, Skarback E, Wahrborg P, Green qualities in the neighbourhood and mental health - results from a longitudinal cohort study in Southern Sweden, BMC Public Health 12 (2012) 337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].de Vries S, van Dillen SM, Groenewegen PP, Spreeuwenberg P, Streetscape greenery and health: stress, social cohesion and physical activity as mediators, Soc. Sci. Med 94 (2013) 26–33. [DOI] [PubMed] [Google Scholar]
- [27].Bolling M, Mygind E, Mygind L, Bentsen P, Elsborg P, The association between education outside the classroom and physical activity: differences attributable to the type of space? Children (Basel). 8 (6) (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Trapasso E, Knowles Z, Boddy L, Newson L, Sayers J, Austin C, Exploring gender differences within Forest schools as a physical activity intervention, Children (Basel). 5 (10) (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kabisch N, van den Bosch M, Lafortezza R, The health benefits of nature-based solutions to urbanization challenges for children and the elderly - a systematic review, Environ. Res 159 (2017) 362–373. [DOI] [PubMed] [Google Scholar]
- [30].Kondo MC, Fluehr JM, McKeon T, Branas CC, Urban green space and its impact on human health, Int. J. Environ. Res. Public Health 15 (3) (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Mnich C, Weyland S, Jekauc D, Schipperijn J, Psychosocial and physiological health outcomes of green exercise in children and adolescents-a systematic review, Int. J. Environ. Res. Public Health 16 (21) (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Fyfe-Johnson AL, Hazlehurst MF, Perrins SP, et al. , Nature and Children’s health: a systematic review, Pediatrics 148 (4) (2021). [DOI] [PubMed] [Google Scholar]
- [33].Jose KA, Blizzard L, Dwyer T, McKercher C, Venn AJ, Childhood and adolescent predictors of leisure time physical activity during the transition from adolescence to adulthood: a population based cohort study, Int. J. Behav. Nutr. Phys. Activity 8 (2011) 54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Kimm SY, Glynn NW, Kriska AM, et al. , Longitudinal changes in physical activity in a biracial cohort during adolescence, Med. Sci. Sports Exerc 32 (8) (2000) 1445–1454. [DOI] [PubMed] [Google Scholar]
- [35].Poitras VJ, Gray CE, Borghese MM, et al. , Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth, Appl. Physiol. Nutr. Metab 41 (6 Suppl 3) (2016) S197–S239. [DOI] [PubMed] [Google Scholar]
- [36].Bauman A, Merom D, Bull FC, Buchner DM, Fiatarone Singh MA, Updating the evidence for physical activity: summative reviews of the epidemiological evidence, prevalence, and interventions to promote “active aging”, The Gerontologist 56 (Suppl. 2) (2016) S268–S280. [DOI] [PubMed] [Google Scholar]
- [37].Johnson SB, Riis JL, Noble KG, State of the art review: poverty and the developing brain, Pediatrics. 137 (4) (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Shankar P, Chung R, Frank DA, Association of Food Insecurity with Children’s Behavioral, emotional, and academic outcomes: a systematic review, J. Dev. Behav. Pediatrics 38 (2) (2017) 135–150. [DOI] [PubMed] [Google Scholar]
- [39].Alvarez-Bueno C, Pesce C, Cavero-Redondo I, Sanchez-Lopez M, Garrido-Miguel M, Martinez-Vizcaino V, Academic achievement and physical activity: a meta-analysis, Pediatrics. 140 (6) (2017). [DOI] [PubMed] [Google Scholar]
- [40].BLS, American Time Use Survey. https://www.bls.gov/tus/home.htm, 2017.
- [41].Cohen DA, McKenzie TL, Sehgal A, Williamson S, Golinelli D, Lurie N, Contribution of public parks to physical activity, Am. J. Public Health 97 (3) (2007) 509–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Kerr J, Sallis JF, Saelens BE, et al. , Outdoor physical activity and self rated health in older adults living in two regions of the U.S, Int. J. Behav. Nutr. Phys. Activity 9 (2012) 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Wheeler BW, Cooper AR, Page AS, Jago R, Greenspace and children’s physical activity: a GPS/GIS analysis of the PEACH project, Prev. Med 51 (2) (2010) 148–152. [DOI] [PubMed] [Google Scholar]
- [44].Oreskovic NM, Perrin JM, Robinson AI, et al. , Adolescents’ use of the built environment for physical activity, BMC Public Health 15 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].TPL, City Parks Facts Report. https://www.tpl.org/2017-city-park-facts#sm.0008i9q5fqemfqt10qj1bxlxy4but 2018, TPL, Washington, DC, . [Google Scholar]
- [46].Cohen DA, Setodji C, Evenson KR, et al. , How much observation is enough? Refining the administration of SOPARC, Jl Phys. Activity Health 8 (8) (2011) 1117–1123, 10.1123/jpah.8.8.1117 (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Cohen DA, Playgrounds and Physical Activity: The National Study of Neighborhood Parks. 9th Biennial Childhood Obesity Conference; May, 2017, 2017 (San Diego). [Google Scholar]
- [48].Freedson P, Pober D, Janz KF, Calibration of accelerometer output for children, Med. Sci. Sports Exerc 37 (11 Suppl) (2005) S523–S530. [DOI] [PubMed] [Google Scholar]
- [49].Puyau MR, Adolph AL, Vohra FA, Butte NF, Validation and calibration of physical activity monitors in children, Obes. Res 10 (3) (2002) 150–157. [DOI] [PubMed] [Google Scholar]
- [50].Cohen DA, Han B, Kraus L, Young DR, The contribution of the built environment to physical activity among Young women, Environ. Behav 51 (7) (2018) 811–827. [Google Scholar]
- [51].Chinapaw MJ, de Niet M, Verloigne M, De Bourdeaudhuij I, Brug J, Altenburg TM, From sedentary time to sedentary patterns: accelerometer data reduction decisions in youth, PLoS One 9 (11) (2014), e111205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Evenson KR, Wen F, Golinelli D, Rodriguez DA, Cohen DA, Measurement properties of a park use questionnaire, Environ. Behav 45 (4) (2013) 526–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Cohen S, Kamarck T, Mermelstein R, A global measure of perceived stress, J. Health Soc. Behav 24 (1983) 385–396. [PubMed] [Google Scholar]
- [54].Lee E-H, Review of the psychometric evidence of the perceived stress scale, Asian Nursing Res. 6 (4) (2012) 121–127. [DOI] [PubMed] [Google Scholar]
- [55].White B, The Perceived Stress Scale for Children: A Pilot Study in a Sample of 153 Children vol 2, 2014. [Google Scholar]
- [56].NorthwesternUniversity, Health Measures. https://www.healthmeasures.net/search-view-measures?task=Search.search, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.