Abstract
Background:
Disaster events adversely affect the health of millions of individuals each year. They create exposure to physical, chemical, biological, and psychosocial hazards while simultaneously exploiting community and individual-level vulnerabilities that allow such exposures to exert harm. Since 2013, the National Institute of Environmental Health Sciences (NIEHS) has led the development of the Disaster Research Response (DR2) program and infrastructure; however, research exploring the nature and effects of disasters on human health is lacking. One reason for this research gap is the challenge of developing and deploying cost-effective sensors for exposure assessment during disaster events.
Objectives:
The objective of this commentary is to synergize the consensus findings and recommendations from a panel of experts on sensor science in support of DR2.
Methods:
The NIEHS convened the workshop, “Getting Smart about Sensors for Disaster Response Research” on 28 and 29 July 2021 to discuss current gaps and recommendations for moving the field forward. The workshop invited full discussion from multiple viewpoints, with the goal of identifying recommendations and opportunities for further development of this area of research. The panel of experts included leaders in engineering, epidemiology, social and physical sciences, and community engagement, many of whom had firsthand experience with DR2.
Discussion:
The primary finding of this workshop is that exposure science in support of DR2 is severely lacking. We highlight unique barriers to DR2, such as the need for time-sensitive exposure data, the chaos and logistical challenges that ensue from a disaster event, and the lack of a robust market for sensor technologies in support of environmental health science. We highlight a need for sensor technologies that are more scalable, reliable, and versatile than those currently available to the research community. We also recommend that the environmental health community renew efforts in support of DR2 facilitation, collaboration, and preparedness. https://doi.org/10.1289/EHP12270
Introduction
Disasters are on the rise around the world.1 Notwithstanding the loss of housing and infrastructure, events such as hurricanes, floods, and wildland fires frequently expose individuals to chemical, biological, and physical hazards that create both acute and chronic health risks.2,3 Disasters, by their nature, exacerbate the underlying physical and social vulnerabilities of communities, which only broadens a disaster’s ill effects on human health.4
Flooding, for example, may release and disperse myriad chemicals (e.g., pesticides, metals, and persistent organic pollutants) from soil, storm- or wastewater overflows, building materials, or stored wastes. Lingering effects of floods also include mold accumulation, contamination of food and drinking water by pathogens, and the stress induced by loss of housing and infrastructure.3,5 Wildfires emit high levels of combustion byproducts, including fine particulate matter (PM), volatile organic compounds (VOCs), and reactive/toxic gases.6,7 When released to the upper atmosphere, these pollutants can travel thousands of miles, exposing large proportions of the population.6 The rising trend of fires crossing the wildland–urban interface raises new public health concerns about population exposure to the burning of synthetic building materials8—a largely uncharacterized mixture of hazardous chemicals. Chemical spills from industrial accidents, including fires at chemical plants and spills that penetrate local water resources, create conditions that can spread toxicants both near and far, with lasting effects and prolonged community exposure.9 Although the immediate actions of local and national first responders, health officials, and residents are to protect the health and safety of affected individuals, the cascading health and safety risks to exposed populations are often not considered in the days, months, and years following the event.9 Thus, we know woefully little about short- and long-term health effects from disasters, and we remain poorly positioned to use our experiences to prepare individuals, communities, and the public health system for potential future events.10
Recognizing the health burden posed by disaster-related exposures, the National Institute of Environmental Health Sciences (NIEHS) led the development of the Disaster Research Response (DR2) program and infrastructure, established by the National Institutes of Health (NIH) in 2013.10 Since its inception, the DR2 program has spearheaded U.S. efforts and has worked with global partners to improve capacity for timely environmental health research in the wake of disasters and public health emergencies.
Despite these investments, there is a lack of research exploring the nature and effects of disasters on human health, especially population-based epidemiological studies with high-quality exposure assessment.10 We contend that one reason for this gap is the challenge of developing and deploying cost-effective sensors for accurate detection and monitoring of contaminant release and exposure during disaster events. For the purpose of this discussion, we define “sensor” in this context as a device that can detect or measure a physical property (e.g., quantifying the concentration of one or more pollutants in an environmental or biological medium). Such sensors are not only necessary for research but also for identifying and preventing health risks during response and cleanup efforts.11 This need is amplified by the fact that disasters are increasing in frequency and magnitude globally,1 becoming more complex, and will require enhanced preparation strategies. Current sensor technologies have provided some measures of the chemicals and other health hazards related to disasters.11,12 However, challenges remain in monitoring and characterizing the complexity of chemical mixtures in air, water, and soil related to disaster events that will continue to pose risks to human health. The objective of this commentary is to identify potential knowledge gaps, along with opportunities for research and development related to sensor science in support of DR2.
To prepare the scientific community to address these challenges, NIEHS convened the workshop, “Getting Smart about Sensors for Disaster Response Research” 28–29 July 2021 to discuss current gaps and recommendations for moving the field forward. The workshop invited full discussion from multiple viewpoints with the goal of identifying recommendations and opportunities for further development of this area of research. The panel of experts included leaders in engineering, epidemiology, social and physical sciences, and community engagement, many of whom had firsthand experience with conducting research in the context of events such as wildfires, floods, and industrial accidents.
Because this workshop was designed to support the NIEHS mission of advancing public and environmental health sciences, topics of discussion were focused on sensor technologies for quantifying exposures to environmental stressors from disasters, in addition to sensors for quantifying the resultant acute and chronic health effects of these stressors. Emphasis was also placed on understanding exposure and health risks for community members vs. an explicit focus on response and recovery workers, with the acknowledgment that exposure and health research is lacking for both groups of affected individuals. Although the workshop organizers recognized the importance of immediate injury risks from the disaster itself (e.g., physical injury from floods, storms, wildfire, etc.) and the health impacts on first responders, these research areas fall more directly under the mission of U.S. Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health (CDC/NIOSH) and were not an emphasis at this workshop.
The Need for Improved Sensor Science in DR2: A Case Scenario
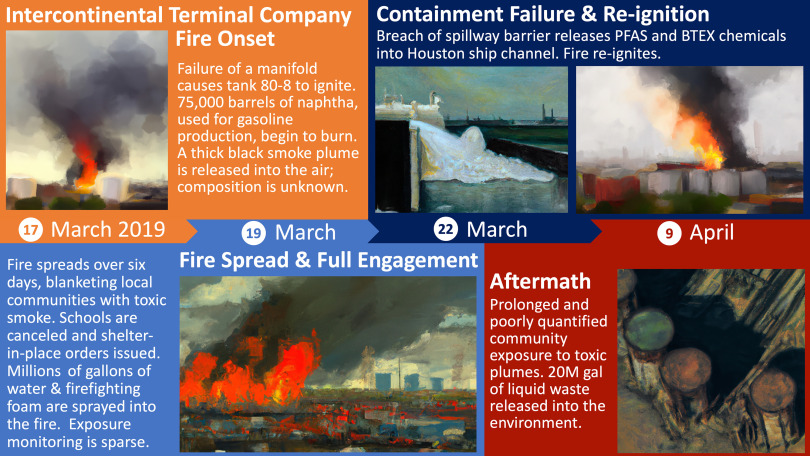
The need for improved sensor science for DR2 becomes clear when reviewing lessons learned. For example, a fire (and subsequent chemical spill) occurred in 2019 at the Intercontinental Terminals Company, LLC (ITC), a petrochemical storage facility in Deer Park, Texas (Figure 1).13 This industrial disaster blanketed surrounding communities with acrid black smoke—the result of naphtha tanks burning out of control—and spilled benzene, toluene, ethylbenzene, and xylene (BTEX)-related chemicals and per- and polyfluoroalkyl substances (PFAS) (the latter a by-product of fire-retardant foam used to combat the fire) into local groundwater and the Houston Ship Channel.14,15 Emissions and exposure monitoring were initially haphazard and uncoordinated. As reported by news agencies, the air and water quality monitoring response was “chaotic,” poorly integrated, and subject to delays in the release of information.16,17 As a result, exposure assessment for the surrounding communities was incomplete. Unfortunately, a lack of comprehensive exposure monitoring typifies most disaster events, because researchers often struggle to conduct postdisaster exposure monitoring in coordination with public health agencies, community members, local government, and responders,18 which severely limits the ability to conduct human health risk assessment or surveillance.
Figure 1.
The 2019 ITC disaster typifies the need for improved sensor technology for emissions and exposure monitoring related to DR2. Image depictions were created by the authors with the assistance of DALL·E 2. Note: DR2, Disaster Research Response; ITC, Intercontinental Terminals Company, LLC.
Attendees of the 2021 workshop concluded that, ideally, exposure monitoring that was sensitive and specific to VOCs and PFAS in the air and water surrounding the community should have commenced within hours of the event onset, at multiple locations (e.g., fence line, upstream/downstream, indoor/outdoor, community/residential) surrounding the site. Such monitoring is necessary not only to inform disaster response and risk management in the immediate aftermath of a disaster but could also support research on acute and chronic health impacts and could inform future disaster response efforts by providing information on contaminant dispersion/exposure in a community setting. For the ITC fire, because both volatilization and combustion of VOCs occurred simultaneously,19 workshop attendees concluded that real-time, continuous monitoring was needed for dozens of toxic compounds [e.g., BTEX, naphtha compounds, aldehydes, polycyclic aromatic hydrocarbons, PM with aerodynamic diameter less than or equal to () and black carbon]. Such monitoring technology is expensive and challenging to deploy rapidly (within hours of an event) and at scale.2,9,20 Further, even if such technology were available, we are not aware of a standard “playbook” for community exposure monitoring that is tailored to specific disaster events.
Discussion
The primary goal of the DR2 program is to understand how disasters impact human health. To achieve that goal, we believe that advancements in sensor technologies, both for exposure and health outcome assessment, are needed. We also see these advances as a necessary component of hypothesis-driven research that focuses on causality and quantification of exposure–response relationships. Without quantifiable exposure–response data, we contend that our society will struggle to manage the health burden from disaster-related pollution exposure, which is expected to rise under a changing global climate.1 The discussion and recommendations that follow represent the authors’ opinions and the consensus findings from the 2021 DR2 Workshop.
Current Sensor Technologies Are Limited in Their Ability to Support DR2
Rigorous and systematic measurement of environmental exposures and health outcomes in the aftermath of disasters present major limitations to the conduct of DR2.20 In traditional occupational or environmental epidemiology, researchers dedicate substantial time and resources to ensure that exposures and outcomes are measured using well-validated devices, assays, or assessments. The nature of disaster research, however, requires rapid deployment of devices capable of measuring exposures and outcomes, often by end users with limited or no training and resources. Standard reference instruments for exposure assessment (i.e., validated, “gold standard” instruments that provide reliable data) tend to be expensive and cumbersome (bulky and heavy, requiring line power and air-conditioned enclosures); they also require a skilled technician to set up and operate. Taken together, these limitations complicate the utility and feasibility of fielding standard reference instruments in the immediate wake of a disaster, meaning that critical windows of exposure are often missed.
For health research, including epidemiology and health risk communication, sensor technology offers an opportunity to identify initial health events (e.g., inflammation, irritation, symptom onset, etc.) otherwise not captured in administrative databases used for retrospective analysis. Identifying such health events contemporaneously may provide insight into pathways that link exposure to disease, in addition to shedding light on dose–response and time-to-event outcomes. Understanding the link between exposure and subacute health outcomes is particularly important to health risk communication, with the objective of informing and engaging the public on adopting behavioral changes that could protect their health. In the absence of such knowledge, public motivation to adopt health protective behaviors is often hindered by low perceptions of risk and health outcomes that may be distant and rare.21 To date, most health outcome data in the field of DR2 is limited to health care encounters [e.g., hospitalizations, emergency department (ED) visits],20 mortality, or survey-based research22 to capture both physical and mental health outcomes with a long time between the exposure and the initial health event. Sensors for noninvasive, subacute biomarkers are therefore a key priority for improving health outcomes during disasters. Validated, commercially available sensors are emerging. Examples of established technologies include wearable devices for electrocardiogram data,23 blood pressure24,25 and blood-oxygen partial pressure,26 and blood glucose27—all of which can be coupled to smartphone systems for data visualization, storage, and transmission. There is also growing interest in research and development of wearable, point-of-care biosensors that leverage advances in microelectromechanics and microfluidics.28 Although these emerging biosensor technologies show promise, they have yet to be widely used in support of DR2.
The burgeoning availability of low-cost sensors capable of monitoring environmental exposures, paired with mobile health devices and smartphones, may be one potential solution to this challenge. These devices offer several advantages to traditional occupational or environmental exposure methods, including their scalability, price, and usability with limited training. Disaster research following wildfire exposures offers a relevant example where sensor technology may be employed to measure smoke exposures and pulmonary outcomes. In traditional air pollution epidemiological studies, measuring PM is conducted using stationary monitors, often with filter-based, time-integrated active sampling. This approach involves substantial costs, time, and resources and is not suitable to the rapidly changing locations and exposures associated with wildfires. In this scenario, low-cost, mobile air sensors may be provided to firefighters and residents and either worn or placed on their vehicles or in their homes. When paired with GPS location data these devices can measure exposure in real-time (e.g., 1-s resolution) enabling researchers to identify specific times and locations of exposures that lead to unhealthy exposures in population and occupational settings. However, low-cost sensors are limited in the agents/hazards they can detect,29 and they can be prone to measurement error/interferences or are not adequately calibrated or validated for the application of interest.30,31
The collection of health-outcome data is similarly difficult. For example, traditional assessments of respiratory outcomes tend to be time and resource intensive (e.g., spirometry conducted by trained technicians), which can limit sample size, or imprecise and prone to bias (e.g., collection of symptom data via questionnaires). Smartphone-based questionnaires,32–34 ecological momentary assessment (EMA) of symptoms,35,36 and handheld spirometers are examples of alternative approaches more suitable to the needs of disaster response research. Smartphone-based questionnaires and EMA methods enable investigators to rapidly “push” notifications and questionnaires to affected individuals, particularly when existing institutional review board (IRB) protocols are in place to enable electronic consent. Providing handheld spirometers to responders and affected residents requires limited training, and data may be collected, stored, and transmitted by smartphones.
Technology Transfer and Commercialization Are Key Steps for Sensor Development, but Unique Barriers Exist for DR2
The advent of smartphones and related consumer electronics (the “Internet of Things”) has resulted in a wave of commercially available sensor technologies that have been leveraged for scientific research.37 Examples include microelectronic sensors for temperature, light and electromagnetic intensity, pressure, acceleration, location, and image data. The availability of sensors in the commercial market generally works to support more rigorous, reliable, and (more democratized) on-demand use. Commercialization of sensors, however, is not uniform, and barriers exist for the development and use of sensors for DR2. The unfortunate reality is that although sensor technologies for DR2 exposure and health research are desired, there may not be a strong enough market for them to succeed commercially.
One key program that supports scientific innovation in the United States is the federal Small Business Innovation Research (SBIR) program, including support by a range of federal agencies for the development of sensors for detecting a range of environmental pollutants and conditions affecting water and air quality (https://www.sbir.gov/Sensor-technology-for-the-21st-century).
Although the SBIR and Small Business Technology Transfer Research (STTR) programs provide seed funding for research and development of these technologies, small businesses face challenges in securing additional investment during the commercialization and scale-up phase. In the absence of regulatory statutes that prescribe regular monitoring at scale (e.g., ambient , household radon, carbon monoxide, total coliform bacteria), markets for exposure assessment technologies and venture capital or other investments can be limited. To meet the needs for the growing DR2 community of practice, the cost of measurement technologies developed in the SBIR/STTR programs will need to be affordable for research teams. Scale-up efforts and additional investments in production efficiency can be key to lowering costs for products entering the market.
Although investments in scale-up efforts typically fall to venture capital and private equity firms, the market for exposure measurements related to environmental research is often too small to attract serious attention, because large venture capital investments tend to pursue exit valuations of more than USD $50 million.38 In practice, only a few chemical/physical hazards have such large domestic markets, as previously described (e.g., ambient ,39 etc.). However, many existing and emerging exposure hazards experienced during a disaster do not have monitoring networks promulgated by law (e.g., isocyanates; PFAS; BTEX; engineered nanomaterials, etc.), meaning that commercial sales potential is insufficient to support private-sector investment. This reality drives up the cost of measurement technologies, which can stifle both research and commercialization efforts. For example, our experience has led us to conclude that real-time analyzers for multiple VOCs such as BTEX that are accurate, sensitive, and compound-specific tend to cost more than USD $100,000 each. These market challenges are exacerbated within the biomonitoring space. Although the biomedical device market is a USD $400 billion industry,40 there is a considerably smaller market for environmental exposure monitoring, partly owing to our opinion that most investments for health care focus on treating disease, not preventing it. As a result, exposure biomonitoring technologies also face an uphill climb.
An Opportunity Exists to Leverage Emergent Data into DR2
We believe the value of DR2 exposure data can be enhanced by combining it with emergent (and nonstandard) data that are ubiquitous but currently underused. Broadly, these include but are not limited to data from cell phones, social media, and Internet of Things (“found” data) devices; data collected by low-cost sensor networks (“planned” data); existing public or privately owned databases that can be repurposed (“repurposed” data); and data associated with a particular disaster event such as administrative data and claims (“event” data). When well organized, these nontraditional data can be leveraged to understand the threat of a disaster, provide background information about the nature and social environment before and after a disaster, and inform the behavior and health effects of impacted populations. For example, after Hurricane Maria, geotagged tweets in Puerto Rico were used to understand population movement patterns after the disaster.41 Geocoded tweets also provide a way to record the user’s travel history, space, and activity, which, otherwise, are difficult to collect. The increasing number of low-cost sensor networks built through crowdsourcing and community research initiatives present a resource of “planned” data for DR2. Data collected by PurpleAir sensor networks not only have been used for estimating concentration (ambient and indoor) during normal and wildfire days but can potentially serve as a sentinel network for detecting a distant wildfire event.42,43 Sentinel networks for environmental health hazards, such as the PurpleAir network, are rare; however, when available, they have been leveraged to produce impactful DR2.44 In lieu of such sentinel networks, however, there are numerous existing place-based measurements, such as satellite remote sensing data, community measures, and census data that can be leveraged for assessing both baseline environment before a disaster and exposure during and post disaster. It has been increasingly recognized that combining and fusing these different data streams () is critical for improved exposure prediction and more comprehensive assessment.45
Although these nonstandard data present enormous opportunities for DR2, there are inherent challenges because of the nature of the data. Many of these data reside in the private sector and are proprietary. Responsible parties may be reluctant to share (such as the compensation claims associated with a disaster). The data are often created for various reasons, are poorly organized, and may exhibit significant implicit and explicit biases.46,47 The research community is often unaware of data sources and platforms, or the data requires specialized skills for access and use. In addition, because the quality and format of these nontraditional data vary broadly, there are likely to be challenges and issues in curating, harmonizing, and systematic assessment. These challenges may also stem from the nonexistent or unclear context, methodology, and or agreement on vocabulary (i.e., lack of metadata). So, there is a clear need to verify the quality of data, curate, minimize interferences/bias, and harmonize, thereby improving the ability to evaluate, interpret, and make meaningful predictions or outcomes. Each of these tasks could have their own challenges and limitations. In addition, we believe these approaches need to be planned with a careful consideration of ethical issues, with clear transparency, and with a focus on a broader adoption of standards, so meaningful data can be obtained through these nontraditional resources.
Beyond Sensors, There Are Challenges and Barriers Associated with “Disaster Research Preparedness” in the Context of DR2
Regardless of the available technology, there are administrative, logistical, and technical challenges to conducting DR2.10 In addition to sensor deployment, DR2 poses time-sensitive challenges to researchers who need to have personnel, IRB materials, and study designs in place for an event of unknown timing, duration, and location. Unexpected challenges may arise when the logistical needs of a research project (e.g., access to site locations, interfacing with local agencies and first responders) must occur alongside response/recovery efforts in the immediate wake of a disaster event. Collecting data from individuals in disaster-impacted communities can also place psychological or other burdens on those involved. It is not surprising, then, that most of the existing literature on post-disaster research consists of case studies with relatively small sample sizes.
Although partnerships among researchers, practitioners, and communities can support an integrated and effective disaster response, no sustained mechanism has been available to support these efforts between disasters. In response to this need,48 the NIEHS DR2 Network program10,49 has developed guidance on disaster research ethics, compiled a searchable database of disaster research protocols and tools, and established a DR2 community of practice. From this program arose the NIH Rapid Acquisition of Pre- and Post-Incident Disaster Data (RAPIDD) protocol tool.50 Although the NIEHS DR2 program has made steady progress since its inception, much remains to be done to support improved disaster health research.
Sensor Science for DR2 is a Prime Opportunity for Public Health Partnerships
We contend that research conducted in the wake of a disaster necessitates a community-based approach, because sentinel networks for monitoring environmental exposure and/or health data are lacking and unlikely to evolve soon. Just as collaboration, communication, and interdisciplinary teaming are required to mount an effective public health response to a disaster, so also do these needs apply to research—including sensor and exposure science. We also believe that research teams will require leadership and expertise that span social, environmental, physical, and data sciences. Our experience has shown us that the creation and efficacy of such teams require time and effort; such teams are not likely to succeed unless they are formed, practiced, and poised in anticipation of a future event. The DR2 community should therefore look to improve on existing models, like influenza surveillance networks, to facilitate the concept of transdisciplinary research in support of DR2.
A particular challenge will be to establish, in advance, public–private–community partnerships that bring together the capabilities of many groups to enable improved tracking of exposures and illnesses following disaster events. The formation of such partnerships would not only facilitate research but could also enhance response and recovery efforts through sample collection, timely access to areas or populations, training of workers and citizen scientists, and communication/education of affected stakeholders on hazards and exposure risks. The involvement of community groups is vital to sustain effective partnerships, to build trust, and to facilitate bidirectional communication of information before, during, and after disasters.51 Community groups may also support exposure monitoring via sensor deployment and/or related data gathering efforts. Training and education in environmental health hazards in the wake of a disaster can aid recovery and help maintain engagement in the interdisaster period. Academic institutions can also preapprove IRB protocols before disasters to enable rapid emergency response. Such protocols, modeled on the NIEHS RAPIDD, can be customized and rapidly modified for review at the time of a disaster.
The NIEHS currently supports projects related to disaster research for characterizing initial exposure, collecting environmental and biological samples, and collecting human health and exposure through a Time-Sensitive R21 grant program. The NIEHS, in partnership with other NIH institutes also oversees the Human Health Exposure Analysis Resource,52 which provides resources to support targeted and untargeted exposure analyses of biological samples as well as environmental samples that could be leveraged to build DR2 capacity. The NIEHS Environmental Health Sciences Core Centers (EHSCC) program funds institutional infrastructure to support environmental health sciences,53,54 and many of these centers have begun to support disaster-related capacity development and investigations.55–57
The demonstrated leadership of the National Science Foundation in supporting time-sensitive investigations and the development of disaster research infrastructure provides a good model for support of DR2. The NSF-supported Natural Hazards Engineering Research Infrastructure (NHERI) is a “shared-use, nationally distributed network that provides key infrastructure for the natural hazards engineering and social science community.”58 The network includes a coordinating office, experimental facilities, an instrumentation facility, a convergence science hub, and topical or discipline-oriented post-event reconnaissance and research teams.59 These teams are funded to develop systems, processes, and networks of trained researchers to conduct reconnaissance and collect time-sensitive, perishable data following extreme events60 and have pre-positioned resources to deploy teams to collect perishable data without NSF advance approval, which then become available to the larger research community.
Collaboration among the NIEHS, the NSF, and other federal agencies can also support additional data-collection opportunities through supplements to these groups, including through the RAPID grant program, which permits program officers to release funds for time-sensitive research.61 Similarly, the NIH could consider funding research teams and coordination centers to facilitate infrastructure and capacity development and integration with existing NHERI capabilities, including through partnership with the NSF. We believe that leveraging these types of resources with programs supported by other federal agencies will be important for developing the infrastructure needed for disaster response research.
Recommendations and Research Needs
We present three overarching needs for sensor technology development in support of disaster response and research: scalability, reliability, and versatility. These priorities are outlined in Table 1 and represent the consensus opinions of authors and the 2021 workshop attendees. We also provide a list of parallel needs in support of the DR2 research community in Table 2.
Table 1.
Sensor research and development needs for DR2.
| Need | Description |
|---|---|
| Scalable | Supporting large sample sizes and/or population-based epidemiological studies |
| Easy to deploy in the field with minimal training | |
| Low burden to the user | |
| Low cost per sample to the researcher (including collection and analysis) | |
| Reliable | Unbiased, precise, agent- or outcome-specific measurement |
| Well-characterized and independently validated (in field) | |
| Versatile | Rapidly deployable |
| Wearable (or at least portable) | |
| Multianalyte measurement, space- and time-resolved |
Note: DR2, Disaster Research Response.
Table 2.
Research community needs for DR2.
| Need | Description |
|---|---|
| Facilitation | Internal team building: |
| External team building: | |
| Data integration | Management, integration, and analysis of “found,” “planned,” “repurposed,” and “event” data |
| Guidance on common data elements to facilitate data harmonization and utility | |
| Preparedness | Rapid, streamlined study design: data collection, sampling logistics, and IRB are preapproved and ready in advance |
| Flexible funding mechanisms to facilitate rapid deployment and data collection efforts for ephemeral data |
Note: DR2, Disaster Research Response; IRB, institutional review board.
Scalability means that sensors must enable sample sizes (and study designs) that support causal-inference62,63 and the establishment of exposure–response relationships with adequate confidence; without such capability, we contend that research is likely to stagnate and/or produce limited impact. What is “adequate” for sample size varies according to the study design and research question, but, as highlighted by Bongers et al.,20 many disaster events lack the exposure assessment necessary to make meaningful health-effect associations. To be scalable in the context of DR2, a sensor must have an acceptable cost-per-sample ratio and be easy to deploy, likely with minimal user training. Many DR2 applications require sensor deployments by nonscientists; thus, consideration must be given to the training of community members, with access to training in multiple formats (e.g., handouts, mobile apps, SMS instructions, online videos, etc.) and in multiple languages. For this priority, the research community should establish metrics that define a cost-per-unit basis that considers overall budget, sample size, data quality, and required personnel time/effort. The challenge of scalability is especially difficult when considering that assessment of exposures and health outcomes at the individual level is desired but rarely achieved.20
Reliability speaks to the collective performance of the sensor itself (i.e., its analytic figures of merit). To be useful, a sensor must have acceptable performance metrics such as precision, specificity, sensitivity, bias, linearity, shelf life, and battery life. Although “acceptable performance” can take on different meanings, given the study design and research question(s), both the U.S. Environmental Protection Agency (U.S. EPA)64 and NIOSH65 have published guidelines for sensors and sampling methods that provide performance benchmarks for designers and manufacturers to consider. A reliable sensor will have been validated, first in the lab and then in the field, against standard reference methods so that these performance metrics can be estimated under real-world settings. We believe that a robust and independent validation (i.e., conducted, peer reviewed, and published by groups that did not design/manufacture the technology) is often the key step that engenders acceptance of sensor technology by the larger research community.
In the age of the Internet of Things,66 sensor capabilities must also include data logging, transmission, storage, and quality assurance. Thus, software development should accompany sensor development to process, analyze, and report back data captured from the sensor. All data capabilities would need to have sufficient quality assurance and quality-control measures to ensure that data are reliable; these procedures would likely require a collective effort to develop and establish standard practices for collecting high-quality data.
A versatile sensor for DR2 research is one that can be deployed rapidly while providing a measure of cumulative exposure (or other relevant dose metric) for multiple hazards/stressors/outcomes. Versatility also relates to quantifying spatial and temporal heterogeneity of exposures and health outcomes. For example, in the case of the ITC Fire, a need existed to quantify air concentrations of dozens of different VOC species at many locations across Deer Park and within minutes of the event, given the rapidly changing nature of the fire and the complex air dispersion patterns67 that can occur in an urban environment. Having continuous measures (i.e., real-time sensors) and geo-referenced data is therefore a key advantage. We note, however, that in the absence of real-time data, any exposure data are valuable, and that timeliness and scalability (i.e., obtaining adequate sample size) are paramount concerns. For health outcome research, an estimate of cumulative exposure,68 assigned at the individual level20 is key, as is knowledge of a latency period (i.e., knowing the expected timing between exposure and disease onset).
We recognize that sensors and their capabilities must be fit for purpose: The environmental hazards created by disasters vary widely and may contain a mixture of biological, chemical, physical, and psychological stressors.2,11 It is unlikely that the research community would be able to develop one instrument that has sufficient utility for all disaster scenarios. We also recognize that the field of disaster research is broad; the data needs for disaster health science are distinct from that of disaster preparedness and disaster response. We envision an iterative process among researchers in this area wherein research needs at multiple levels can be identified and appropriate sensor technology can be developed or adapted to address current limitations in our understanding, moving toward the goals of prevention, protection, and resilience.
We highlight needs of the DR2 research community that go beyond sensor technology in Table 2. We believe these research needs align with the mission of the NIEHS, for which an opportunity exists to provide continued leadership.
Facilitation needs relate to communication and collaboration between researchers, affected communities, responders, and state/federal agencies. Disasters are often chaotic events, and the logistical challenges of conducting research in the wake of a disaster are numerous. The authors recognize that disaster research must be subservient to disaster response; however, we also recognize that to learn from, prepare for, and become more resilient to disasters, we must do a better job of studying the environmental health risks that ensue from disasters.
An opportunity also exists to improve data integration in support of DR2. This need speaks to the collection, management, and analysis of myriad forms of data and metadata on exposure and health surrounding a disaster. We live in an unprecedented age of information, and the authors believe there are many forms of pre- and post-event data that could be found (e.g., historic, electronic records), planned (e.g., insurance claims), and/or repurposed (e.g., social media) to support the needs of the DR2 community.
Finally, the need to improve preparedness is clear. The authors have observed repeated disaster events that come and go with a lack of quantitative exposure assessment for the affected communities. Although we applaud the NIEHS time-sensitive R21 program in providing necessary funding for the environmental health sciences, we believe that further improvements and innovations are needed. For instance, the NSF has the Rapid Response Research (RAPID) proposal type. This type of proposal is used when “there is a severe urgency with regard to availability of, or access to, data, facilities, or specialized equipment, including quick-response research on natural or anthropogenic disasters and similar unanticipated events.”61 We suggest that a corresponding mechanism within the NIH should be explored. As concluded during the workshop, the time-sensitive nature of DR2 requires quantitative and comprehensive exposure data within hours of a disaster onset; such data are rarely captured.
Conclusions
The workshop was an effort to integrate the experiences of scientists and community engagement experts in disaster situations to produce a practical set of recommendations to devise new or improved sensors that will allow measurement of serious exposure and prediction of health risk. The consensus was that these goals could be reached by addressing the following needs:
- Engage with communities.
- Emphasize those at increased risk from disasters.
- Work to achieve multiple levels of preparedness.
- Create stakeholder buy-in to participate in surveillance, monitoring, and communication.
- Focus on timely disclosures of results/findings to participants and community leaders.
- Produce sensors that can:
- near-continuously estimate personal exposure
- estimate body burden of exposure
- be available for rapid deployment
- produce baseline measures where possible
- have cost effectiveness and allow for distribution and use—where appropriate—by the public, or with minimal technical assistance.
Improve communication coordination and effectively return data to researchers, local public health officials, and the public.
Implement long-term follow-up studies and reporting on exposure and health risk.
In closing, we believe the need for improved sensor science in the field of DR2 is great and expected to grow in the coming century.69 Without a sustained commitment to technology development and discovery, in addition to increased facilitation of transdisciplinary research, disasters are likely to exert continued harm to human health, especially among the many susceptible and vulnerable members of our society. The February 2023 train derailment in East Palestine, Ohio, that released vinyl chloride, benzene, and their combustion byproducts to the air, soil, and waterways surrounding the community70 is an acute reminder of the need for improved and coordinated DR2 and the need for the deployment of rapid environmental assessment tools.
Acknowledgments
Special thanks go to A. Miller, whose leadership and vision helped establish the DR2 concept and program. The authors also wish to acknowledge the valuable contributions made by additional attendees of the 2021 NIEHS workshop: D. Abramson, D. Balshaw, E. Symanski, E. Craft, J. Wartman, J. Thornburg, M. McCoy, M. Landis, S. Henderson, T. Dye, and T. Swager.
The research described in this article has been reviewed by the Center for Public Health and Environmental Assessment, U.S. EPA, and approved for publication. Approval does not signify that the contents necessarily reflect the views and policies of the agency, nor does the mention of trade names of commercial products constitute endorsement or recommendation for use.
References
- 1.Djalante R. 2019. Key assessments from the IPCC special report on global warming of 1.5°C and the implications for the Sendai framework for disaster risk reduction. Prog Disaster Sci 1:100001, 10.1016/j.pdisas.2019.100001. [DOI] [Google Scholar]
- 2.Young S, Balluz L, Malilay J. 2004. Natural and technologic hazardous material releases during and after natural disasters: a review. Sci Total Environ 322(1–3):3–20, PMID: , 10.1016/S0048-9697(03)00446-7. [DOI] [PubMed] [Google Scholar]
- 3.Noji EK. 1997. The Nature of Disaster: General Characteristics and Public Health Effects. Oxford, UK: Oxford University Press. [Google Scholar]
- 4.Chmutina K, von Meding J. 2019. A dilemma of language: “natural disasters” in academic literature. Int J Disaster Risk Sci 10(3):283–292, 10.1007/s13753-019-00232-2. [DOI] [Google Scholar]
- 5.Erickson TB, Brooks J, Nilles EJ, Pham PN, Vinck P. 2019. Environmental health effects attributed to toxic and infectious agents following hurricanes, cyclones, flash floods and major hydrometeorological events. J Toxicol Environ Health B Crit Rev 22(5–6):157–171, PMID: , 10.1080/10937404.2019.1654422. [DOI] [PubMed] [Google Scholar]
- 6.Jaffe DA, O’Neill SM, Larkin NK, Holder AL, Peterson DL, Halofsky JE, et al. 2020. Wildfire and prescribed burning impacts on air quality in the United States. J Air Waste Manag Assoc 70(6):583–615, PMID: , 10.1080/10962247.2020.1749731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Permar W, Wang Q, Selimovic V, Wielgasz C, Yokelson RJ, Hornbrook RS, et al. 2021. Emissions of trace organic gases from western U.S. wildfires based on WE-CAN aircraft measurements. J Geophys Res Atmos 126(11):e2020JD033838, 10.1029/2020JD033838. [DOI] [Google Scholar]
- 8.NASEM (National Academies of Sciences, Engineering & Medicine). 2020. Implications of the California Wildfires for Health, Communities, and Preparedness: Proceedings of a Workshop. Washington, DC: National Academies Press. [Google Scholar]
- 9.Shareefdeen Z, Bhojwani J. 2022. Hazardous Waste Management: Advances in Chemical and Industrial Waste Treatment and Technologies 27-56. New York, NY: Springer. [Google Scholar]
- 10.Miller A, Yeskey K, Garantziotis S, Arnesen S, Bennett A, O’Fallon L, et al. 2016. Integrating health research into disaster response: the new NIH Disaster Research Response Program. Int J Environ Res Public Health 13(7):676, PMID: , 10.3390/ijerph13070676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lucchini RG, Hashim D, Acquilla S, Basanets A, Bertazzi PA, Bushmanov A, et al. 2017. A comparative assessment of major international disasters: the need for exposure assessment, systematic emergency preparedness, and lifetime health care. BMC Public Health 17(1):1–12, 10.1186/s12889-016-3939-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindell MK, Prater C, Perry RW. 2006. Wiley Pathways Introduction to Emergency Management. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- 13.Harris County Fire Marshall’s Office, Bureau of Alcohol, Tobacco, Firearms, and Explosives. 2019. Final Report: Intercontinental Terminals Company Tank Farm Fire. La Porte, TX: Harris County Fire Marshall’s Office. [Google Scholar]
- 14.Jang S, McDonald TJ, Bhandari S, Rusyn I, Chiu WA. 2021. Spatial and temporal distribution of surface water contaminants in the Houston Ship Channel after the Intercontinental Terminal Company fire. J Expo Sci Environ Epidemiol 31(5):887–899, PMID: , 10.1038/s41370-021-00343-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Texas Commission on Environmental Quality. 2020. Intercontinental Terminals Company Fire Response 2019 After Action Review Report. https://www.tceq.texas.gov/assets/public/response/smoke/air/final-ITCFire-AAR-01.07.2020.pdf [accessed 27 June 2023].
- 16.Douglas E, Martinez A, Covington C. 2023. Toxic benzene lingered for weeks after shelter-in-place warnings ended following 2019 Houston-area chemical fire. The Texas Tribune, online edition. April 27, 2023. https://www.texastribune.org/2023/04/27/texas-chemical-plant-fire-itc-deer-park-benzene/ [accessed 27 June 2023]. [Google Scholar]
- 17.Foxhall E. 2020. Harris County, Houston aim to fix air monitoring that ‘seemed like chaos’ during the ITC fire. The Houston Chronicle, online edition. October 14, 2020. https://www.houstonchronicle.com/news/houston-texas/environment/article/Harris-County-Houston-fix-air-monitoring-ITC-fire-15645881.php [accessed 27 June 2023]. [Google Scholar]
- 18.NASEM. 2020. Evidence-Based Practice for Public Health Emergency Preparedness and Response. Report No. 0309670411. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- 19.U.S. CSB (U.S. Chemical Safety Board). 2019. Storage Tank Fire at Intercontinental Terminals Company, LLC (ITC) Terminal: Deer Park, Texas. Washington, DC: U.S. Chemical Safety and Hazard Investigation Board. [Google Scholar]
- 20.Bongers S, Janssen NAH, Reiss B, Grievink L, Lebret E, Kromhout H, et al. 2008. Challenges of exposure assessment for health studies in the aftermath of chemical incidents and disasters. J Expo Sci Environ Epidemiol 18(4):341–359, PMID: , 10.1038/jes.2008.23. [DOI] [PubMed] [Google Scholar]
- 21.Rappold AG, Hano MC, Prince S, Wei L, Huang SM, Baghdikian C, et al. 2019. Smoke sense initiative leverages citizen science to address the growing wildfire‐related public health problem. GeoHealth 3(12):443–457, PMID: , 10.1029/2019GH000199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laffon B, Pásaro E, Valdiglesias V. 2016. Effects of exposure to oil spills on human health: updated review. J Toxicol Environ Health B Crit Rev 19(3–4):105–128, PMID: , 10.1080/10937404.2016.1168730. [DOI] [PubMed] [Google Scholar]
- 23.Cole-Hunter T, Dhingra R, Fedak KM, Good N, L’Orange C, Luckasen G, et al. 2021. Short-term differences in cardiac function following controlled exposure to cookstove air pollution: the Subclinical Tests on Volunteers Exposed to Smoke (STOVES) study. Environ Int 146:106254, PMID: , 10.1016/j.envint.2020.106254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim J, Chou E‐F, Le J, Wong S, Chu M, Khine M, et al. 2019. Soft wearable pressure sensors for beat‐to‐beat blood pressure monitoring. Adv Healthcare Mater 8(13):1900109, PMID: , 10.1002/adhm.201900109. [DOI] [PubMed] [Google Scholar]
- 25.Kario K. 2020. Management of hypertension in the digital era: small wearable monitoring devices for remote blood pressure monitoring. Hypertension 76(3):640–650, PMID: , 10.1161/HYPERTENSIONAHA.120.14742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soon S, Svavarsdottir H, Downey C, Jayne DG. 2020. Wearable devices for remote vital signs monitoring in the outpatient setting: an overview of the field. BMJ Innov 6(2):55–71, 10.1136/bmjinnov-2019-000354. [DOI] [Google Scholar]
- 27.Kim J, Campbell AS, Wang J. 2018. Wearable non-invasive epidermal glucose sensors: a review. Talanta 177:163–170, PMID: , 10.1016/j.talanta.2017.08.077. [DOI] [PubMed] [Google Scholar]
- 28.Purohit B, Kumar A, Mahato K, Chandra P. 2020. Smartphone-assisted personalized diagnostic devices and wearable sensors. Curr Opin Biomed Eng 13:42–50, 10.1016/j.cobme.2019.08.015. [DOI] [Google Scholar]
- 29.Kumar P, Morawska L, Martani C, Biskos G, Neophytou M, Di Sabatino S, et al. 2015. The rise of low-cost sensing for managing air pollution in cities. Environ Int 75:199–205, PMID: , 10.1016/j.envint.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 30.Castell N, Dauge FR, Schneider P, Vogt M, Lerner U, Fishbain B, et al. 2017. Can commercial low-cost sensor platforms contribute to air quality monitoring and exposure estimates? Environ Int 99:293–302, PMID: , 10.1016/j.envint.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 31.Kruse P. 2018. Review on water quality sensors. J Phys D: Appl Phys 51(20):203002, 10.1088/1361-6463/aabb93. [DOI] [Google Scholar]
- 32.Melin J, Bonn SE, Pendrill L, Lagerros YT. 2020. A questionnaire for assessing user satisfaction with mobile health apps: development using Rasch measurement theory. JMIR mHealth Uhealth 8(5):e15909, PMID: , 10.2196/15909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marcano Belisario JS, Jamsek J, Huckvale K, O’Donoghue J, Morrison CP, Car J, et al. 2015. Comparison of self‐administered survey questionnaire responses collected using mobile apps versus other methods. Cochrane Database Syst Rev 2015(7):MR000042, PMID: , 10.1002/14651858.MR000042.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roberts H, Helbich M. 2021. Multiple environmental exposures along daily mobility paths and depressive symptoms: a smartphone-based tracking study. Environ Int 156:106635, PMID: , 10.1016/j.envint.2021.106635. [DOI] [PubMed] [Google Scholar]
- 35.Beute F, de Kort YAW. 2018. The natural context of wellbeing: ecological momentary assessment of the influence of nature and daylight on affect and stress for individuals with depression levels varying from none to clinical. Health Place 49:7–18, PMID: , 10.1016/j.healthplace.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 36.Moskowitz DS, Young SN. 2006. Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. J Psychiatry Neurosci 31(1):13–20, PMID: . [PMC free article] [PubMed] [Google Scholar]
- 37.Cressey D. 2017. The DIY electronics transforming research. Nature 544(7648):125–126, PMID: , 10.1038/544125a. [DOI] [PubMed] [Google Scholar]
- 38.Davila A, Foster G, Gupta M. 2003. Venture capital financing and the growth of startup firms. J Bus Venturing 18(6):689–708, 10.1016/S0883-9026(02)00127-1. [DOI] [Google Scholar]
- 39.MarketsandMarkets. 2022. Particulate Matter Monitoring Market. https://www.marketsandmarkets.com/Market-Reports/particulate-matter-monitoring-market-153413567.html [accessed 27 June 2023].
- 40.Statistica. 2021. Statista Health Market Outlook - Segment Report. https://www.statista.com/study/107264/medical-devices-report/ [accessed 27 June 2023].
- 41.Martín Y, Cutter SL, Li Z, Emrich CT, Mitchell JT. 2020. Using geotagged tweets to track population movements to and from Puerto Rico after Hurricane Maria. Popul Environ 42(1):4–27, 10.1007/s11111-020-00338-6. [DOI] [Google Scholar]
- 42.Lu Y, Giuliano G, Habre R. 2021. Estimating hourly PM2.5 concentrations at the neighborhood scale using a low-cost air sensor network: a Los Angeles case study. Environ Res 195:110653, PMID: , 10.1016/j.envres.2020.110653. [DOI] [PubMed] [Google Scholar]
- 43.Liang Y, Sengupta D, Campmier MJ, Lunderberg DM, Apte JS, Goldstein AH, et al. 2021. Wildfire smoke impacts on indoor air quality assessed using crowdsourced data in California. Proc Natl Acad Sci USA 118(36): PMID: , 10.1073/pnas.2106478118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nance E, King D, Wright B, Bullard RD. 2016. Ambient air concentrations exceeded health-based standards for fine particulate matter and benzene during the Deepwater Horizon oil spill. J Air Waste Manag Assoc 66(2):224–236, PMID: , 10.1080/10962247.2015.1114044. [DOI] [PubMed] [Google Scholar]
- 45.Xue T, Zheng Y, Geng G, Xiao Q, Meng X, Wang M, et al. 2020. Estimating spatiotemporal variation in ambient ozone exposure during 2013–2017 using a data-fusion model. Environ Sci Technol 54(23):14877–14888, PMID: , 10.1021/acs.est.0c03098. [DOI] [PubMed] [Google Scholar]
- 46.Harford T. 2014. Big data: a big mistake? Significance 11(5):14–19, PMID: , 10.1111/j.1740-9713.2014.00778.x.30366833 [DOI] [Google Scholar]
- 47.Olteanu A, Castillo C, Diaz F, Kıcıman E. 2019. Social data: biases, methodological pitfalls, and ethical boundaries. Front Big Data 2:13, PMID: , 10.3389/fdata.2019.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lurie N, Manolio T, Patterson AP, Collins F, Frieden T. 2013. Research as a part of public health emergency response. N Engl J Med 368(13):1251–1255, PMID: , 10.1056/NEJMsb1209510. [DOI] [PubMed] [Google Scholar]
- 49.NIEHS (National Institute of Environmental Health Sciences). 2022. Disaster Research Response (DR2) Program. https://www.niehs.nih.gov/research/programs/disaster/index.cfm [accessed 27 June 2023].
- 50.Garantziotis S. 2015. Rapid Acquisition of Pre- and Post-Incident Disaster Data Study. https://www.niehs.nih.gov/research/programs/disaster/assets/docs/rapidd_study_508.pdf [accessed 27 June 2023].
- 51.Svendsen ER, Runkle JR, Dhara VR, Lin S, Naboka M, Mousseau TA, et al. 2012. Epidemiologic methods lessons learned from environmental public health disasters: Chernobyl, the World Trade Center, Bhopal, and Graniteville, South Carolina. Int J Environ Res Public Health 9(8):2894–2909, PMID: , 10.3390/ijerph9082894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.NIH (National Institutes of Health). 2023. Human Health Exposure Analysis Resource. https://hhearprogram.org/ [accessed 27 June 2023].
- 53.NIEHS. Environmental Health Sciences Core Centers. 2022. https://www.niehs.nih.gov/research/supported/centers/core/index.cfm [accessed 27 June 2023].
- 54.Errett NA, Haynes EN, Wyland N, Everhart A, Pendergrast C, Parker EA, et al. 2019. Assessing the national capacity for disaster research response (DR2) within the NIEHS Environmental Health Sciences Core Centers. Environ Health 18(1):61, PMID: , 10.1186/s12940-019-0498-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Quist AJL, Rohlman DS, Kwok RK, Stewart PA, Stenzel MR, Blair A, et al. 2019. Deepwater Horizon oil spill exposures and neurobehavioral function in Gulf study participants. Environ Res 179(pt B):108834, PMID: , 10.1016/j.envres.2019.108834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sullivan J, Croisant S, Howarth M, Rowe GT, Fernando H, Phillips-Savoy A, et al. 2018. Building and maintaining a citizen science network with fishermen and fishing communities post Deepwater Horizon oil disaster using a CBPR approach. New Solut 28(3):416–447, PMID: , 10.1177/1048291118795156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.White-Newsome JL, McCormick S, Sampson N, Buxton MA, O’Neill MS, Gronlund CJ, et al. 2014. Strategies to reduce the harmful effects of extreme heat events: a four-city study. Int J Environ Res Public Health 11(2):1960–1988, PMID: , 10.3390/ijerph110201960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chowdhury A, Conte J, Masters F, Ramirez J, Ricles J. 2021. Editorial: Natural Hazards Engineering Research Infrastructure (NHERI): mitigating the impact of natural hazards on civil infrastructure and communities. Front Built Environ 7, 10.3389/fbuil.2021.708450. [DOI] [Google Scholar]
- 59.Berman JW, Wartman J, Olsen M, Irish JL, Miles SB, Tanner T, et al. 2020. Natural hazards reconnaissance with the NHERI RAPID facility. Front Built Environ 6, 10.3389/fbuil.2020.573067. [DOI] [Google Scholar]
- 60.Kijewski-Correa T, Roueche DB, Mosalam KM, Prevatt DO, Robertson I. 2021. StEER: a community-centered approach to assessing the performance of the built environment after natural hazard events. Front Built Environ 7, 10.3389/fbuil.2021.636197. [DOI] [Google Scholar]
- 61.National Science Foundation. 2021. Proposal Award and Procedures Guide. Alexandria, VA: National Science Foundation. [Google Scholar]
- 62.Carone M, Dominici F, Sheppard L. 2020. In pursuit of evidence in air pollution epidemiology: the role of causally driven data science. Epidemiology 31(1):1–6, PMID: , 10.1097/EDE.0000000000001090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dominici F, Zigler C. 2017. Best practices for gauging evidence of causality in air pollution epidemiology. Am J Epidemiol 186(12):1303–1309, PMID: , 10.1093/aje/kwx307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Williams R, Kilaru V, Snyder E, Kaufman A, Dye T, Rutter A, et al. 2014. Air Sensor Guidebook. EPA/600/R-14/159 (NTIS PB2015-100610). Washington, DC: US Environmental Protection Agency. [Google Scholar]
- 65.Atzori L, Iera A, Morabito G. 2017. Understanding the internet of things: definition, potentials, and societal role of a fast evolving paradigm. Ad Hoc Networks 56:122–140, 10.1016/j.adhoc.2016.12.004. [DOI] [Google Scholar]
- 66.Wikipedia. 2022. Internet of things. https://en.wikipedia.org/wiki/Internet_of_things [accessed 27 June 2023].
- 67.Truong SCH, Lee M-I, Kim G, Kim D, Park J-H, Choi S-D, et al. 2016. Accidental benzene release risk assessment in an urban area using an atmospheric dispersion model. Atmos Environ 144:146–159, 10.1016/j.atmosenv.2016.08.075. [DOI] [Google Scholar]
- 68.Savitz DA, Engel LS. 2010. Lessons for study of the health effects of oil spills. Ann Intern Med 153(8):540–541, PMID: , 10.7326/0003-4819-153-8-201010190-00276. [DOI] [PubMed] [Google Scholar]
- 69.Bhola V, Hertelendy A, Hart A, Adnan SB, Ciottone G. 2023. Escalating costs of Billion-Dollar disasters in the US: climate change necessitates disaster risk reduction. The Journal of Climate Change and Health 10:100201, 10.1016/j.joclim.2022.100201. [DOI] [Google Scholar]
- 70.U.S. Environmental Protection Agency. 2023. Unilateral Administrative Order for Removal Actions. CERCLA Docket No. V-W-23-C-004. 42 U.S.C. § 9606(a). U.S. EPA Regions 3 and 5. https://www.epa.gov/system/files/documents/2023-03/Unilateral%20Administrative%20Order%20for%20Removal%20Action-First%20Amendment%20-%2020230327.pdf [accessed 27 June 2023].