Abstract
Introduction
Remote consultation has potential benefits in increasing patient pathway efficiency and has been found to reduce costs and carbon emissions. Previous studies of remote consultation in ear, nose and throat (ENT) practice have reported mixed results and used relatively small sample sizes. The aim of this article is to study the impact of remote telephone consultation on ENT clinic outcomes and pathway efficiency, compared with in-person review, within new and follow-up patient cohorts and subspeciality, where previous studies demonstrate mixed and inconclusive results.
Methods
This was a comparison of remote clinic appointment outcomes over a 2-month period from a single ENT referral centre (426) with an equivalent data set of face-to-face clinic appointments over a similar time frame (1,533). Statistical analysis included chi-squared test for clinic outcomes and two-sample t-squared test for mean hand-off between both cohorts (p < 0.05).
Results
For new referrals, remote consultation was associated with statistically significantly greater rates of follow-up (p < 0.00001), investigation (p = 0.00251) and hand-off (p < 0.00013) than patients seen face-to-face – particularly where presenting with head and neck symptoms. For follow-up patients, remote consultation had similar rates of investigation (p = 0.11071) or further follow-up (p = 0.08) and mean hand-off (p < 0.11764) to those seen face-to-face.
Conclusions
Remote consultation in ENT could become the norm for follow-up patients, but should be used with caution in the initial consultation of new patients.
Keywords: Remote consultation, Efficiency, Follow-up, Hand-off, ENT
Introduction
Remote consultation is gaining interest as an alternative to face-to-face (F2F) clinics and has become increasingly incorporated into ear, nose and throat (ENT) practice, particularly to reduce risk of viral transmission during the COVID-19 pandemic.1,2 Authoritative bodies such as the General Medical Council and Royal College of Surgeons of England have supported the use of remote consultation as an alternative to F2F clinics during this time.3,4 In addition to the use of telephone, software such as encrypted video-conferencing platforms and other, asynchronous consultation systems have benefitted from rapid development and incorporation in mainstream use.
Previous reports of remote consultation within ENT have varied and included initial or follow-up consultation, use in rhinology, otology or head and neck, and utilised telephone, video or other platforms for data capture.1 Reported outcome measures have also been variable, and not always examined the key question of patient pathway efficiency. Reported advantages of remote assessment include financial benefits to patient and provider, reduced negative environmental impact and increased convenience for patients, particularly by mitigating travel for the frail, infirm or those with dependents.5,6 As we emerge from the pandemic, this will be increasingly important: remote consultation has potential to increase efficiency and save time and cost for patient and provider, but lack of physical examination and opportunity to perform procedures such as nasendoscopy or otoscopy may limit applicability.1
Here, we report the first large-scale comparative effectiveness study to directly compare the outcomes of patient pathways for remote and F2F ENT outpatient consultations, from a single ENT department. Outcomes of interest specifically include comparative follow-up and discharge rates, investigation rates and patient hand-off rates. We also include subset analyses of new vs follow-up consultation, and by subspecialty of the presenting complaint to identify any effect of these two variables on clinic outcome.
Methods
Objectives
This comparative effectiveness study set out to directly compare the outcomes of patient pathways for remote and F2F ENT outpatient consultations, from a single ENT department. The objective of this study was to ascertain whether remote telephone consultation was associated with similar or increased patient pathway efficiency, compared with F2F consultation – where efficiency related to fewer subsequent follow-up appointments and referral for further investigation.
Furthermore, we aimed to identify whether pre-existing follow-up status (new referral vs patient already under follow-up) and subspeciality of appointment (head and neck, otology, rhinology) had any significant impact on stated outcome measures.
Data sources and cohort selection
We extracted data for two cohorts, remote patient consultation (prospective intervention) and F2F consultation (retrospective control).
Following the first lockdown of the COVID-19 pandemic within the United Kingdom, our department adopted remote consultation for all new and follow-up ENT outpatient consultations at our hospital trust. For two months between Monday 8 June 2020 and Friday 4 August 2020, outcomes for every adult patient scheduled for remote consultation were prospectively recorded. All remote consultations were undertaken within the department by telephone, by a consultant or specialist trainee in ENT, or an experienced general practitioner with special interest.
Our control cohort comprised all adult ENT consultations for a comparable period one year earlier, between Monday 10 June 2019 and Friday 2 August 2019, when clinics were run solely F2F (and using essentially the same team). No remote consultation occurred during this period. Historical control data were extracted from administrative outpatient clinic records, accessed through the hospital central information unit, which were then verified against patient medical records.
Exclusion criteria
Surveillance of head and neck cancer continued to be delivered via F2F consultations throughout the COVID-19 pandemic owing to the need for physical examination and/or scope. This cohort was therefore excluded from data collection. The same group was also excluded from the control cohort.
Data collection was limited to adult consultation only with exclusion of any paediatric patient encounters.
Outcome measurement
We analysed administrative database records as well as electronic clinic letters to verify or ascertain clinical pathways for each patient, and recorded outcomes of each consultation as either discharged or followed-up. For those followed-up, further outcome measures were also recorded – such as referral for investigation (eg imaging), to allied speciality or for surgery. Outcomes between the remote and F2F consultation cohorts were compared using the chi-squared test, with significance at p < 0.05.
The same analysis was undertaken for subgroups, specifically between patients having a new (first) consultation and those having follow-up consultation, as well as comparison between subspeciality (assigned as per predominant symptoms to otology, rhinology or head and neck).
Finally, we evaluated the overall efficiency of the patient pathway using hand-off (the number of times the patient and their data was transferred between parties during discrete patient encounters), where the lower the hand-off, the greater the efficiency.7 The initial consultation scored one point, and if the patient was discharged no further points were scored. If a follow-up appointment was arranged (either with ENT or referral to another specialty) or the patient was listed for surgery, one additional point was scored each. If the patient was also sent for investigation a further point was scored (resulting in maximum hand-off using our scoring system of five). Mean hand-off for both cohorts of remote and F2F consultation were compared using a two-sample t-squared test with significance at p < 0.05.
Managing bias
Classification and measurement bias of recorded outcomes was minimised by clearly defining outcomes prior to the study and verifying administrative outpatient records with patient medical records. Selection bias was minimised by having limited exclusion criteria that were applied identically across both cohorts as well as prospective recording of outcomes with the remote consultation cohort.
Results
Within the prospective, remote consultation cohort, 698 consultations were carried out between 8 June 2020 and 4 August 2020, of which 272 were excluded because they were delivered F2F as part of head and neck cancer surveillance, leaving 426 for analysis. Of the control, F2F consultation cohort, 1,658 consultations took place between 10 June 2019 and 2 August 2019, of which 125 were excluded as part of head and neck cancer surveillance, leaving 1,533 for analysis. Where patients were sent for investigation, this was most often imaging including computed tomography, magnetic resonance imaging, ultrasound or contrast swallow, and less often hearing, balance or allergy tests.
Table 1 shows outcomes for remote and F2F consultations for new and follow-up patients. In the remote consultation cohort, there was a higher proportion of new patients (272/426 = 64% vs 743/1,533 = 48%, p < 0.0001). For new consultations, remote telephone assessment was more likely to lead to follow-up (82% vs 54%, p < 0.00001) and/or investigation (37% vs 27%, p = 0.00251) and less likely to lead to listing for surgery (1% vs 10%, p < 0.00001). We found no evidence that patients already under follow-up were more or less likely to be followed-up further (58% vs 66%, p = 0.08521) or have more investigations (13% vs 9%, p = 0.11071). Where patients having remote consultation were scheduled for F2F follow-up, common reasons cited were need for physical examination, to perform procedures such as otoscopy or nasendoscopy, need to discuss surgery and for patient reassurance.
Table 1 .
Outcomes for remote and face-to-face (F2F) consultations for new and follow-up patients
| Outcome | All consultations | New consultations | Follow-up consultations | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Remote | F2F | p-value | Remote | F2F | p-value | Remote | F2F | p-value | |
| Follow-up | 72% (312) | 60% (924) | 0.00001 | 82% (222) | 54% (405) | 0.00001 | 58% (90) | 66% (519) | 0.08521 |
| + Surgery | 2% (10) | 10% (155) | 0.00001 | 1% (3) | 10% (74) | 0.00001 | 5% (7) | 10% (81) | 0.02584 |
| + Investigation | 28% (121) | 18% (273) | 0.00001 | 37% (101) | 27% (203) | 0.00251 | 13% (20) | 9% (70) | 0.11071 |
| Discharged | 27% (114) | 40% (609) | 0.00001 | 18% (50) | 46% (338) | 0.00001 | 42% (64) | 34% (271) | 0.08521 |
| Total | 426 | 1,533 | 272 | 743 | 154 | 790 | |||
Table 2 shows outcomes for remote and F2F consultations by subspecialty of predominant patient symptoms. In the remote consultation cohort, there was a higher proportion of patients with head and neck-related symptoms (308/426 = 72% vs 560/1,533 = 36%, p < 0.00001). Patients with head and neck symptoms were more likely to be followed-up (78% vs 53%, p < 0.00001) and investigated (32% vs 21%, p < 0.00024) and less likely to be listed for surgery (1% vs 12%, p < 0.00001) when seen remotely rather than F2F. We found no evidence of difference in outcomes for remote vs F2F consultation for patients with otology or rhinology symptoms, but sample sizes in the remote consultation cohort for this particular question were small, so these findings should be treated with caution.
Table 2 .
Outcomes for remote and face-to-face (F2F) consultations by subspecialty
| Outcome | Otology symptoms | Rhinology symptoms | Head and neck symptoms | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Remote | F2F | p-value | Remote | F2F | p-value | Remote | F2F | p-value | |
| Follow-up | 63% (40) | 65% (416) | 0.67765 | 59% (32) | 62% (208) | 0.67203 | 78% (240) | 53% (299) | 0.00001 |
| + Surgery | 6% (4) | 7% (43) | 0.88365 | 6% (3) | 14% (47) | 0.08310 | 1% (3) | 12% (67) | 0.00001 |
| + Investigation | 17% (11) | 14% (91) | 0.52341 | 20% (11) | 19% (65) | 0.87587 | 32% (99) | 21% (117) | 0.00024 |
| Discharged | 38% (24) | 35% (223) | 0.67765 | 41% (22) | 38% (126) | 0.67203 | 22% (68) | 47% (261) | 0.00001 |
| Total | 64 | 639 | 54 | 334 | 308 | 560 | |||
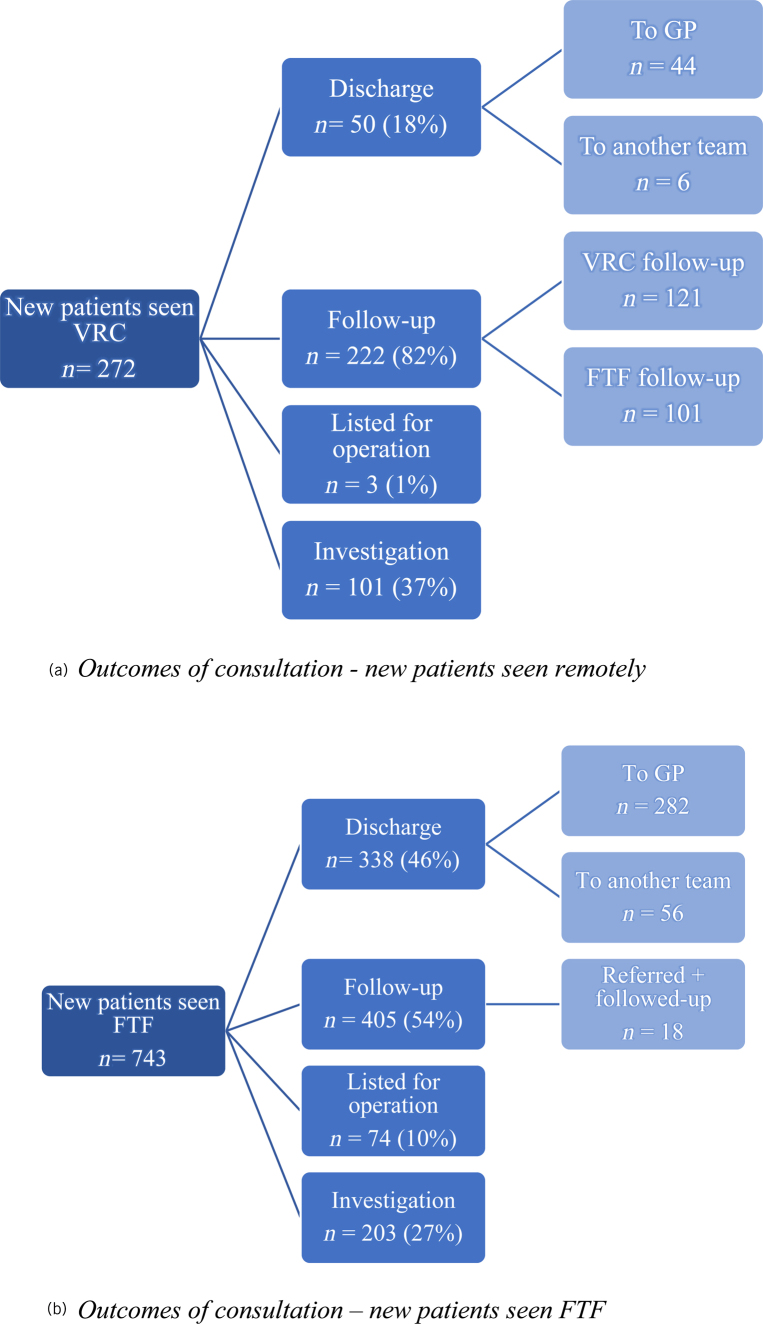
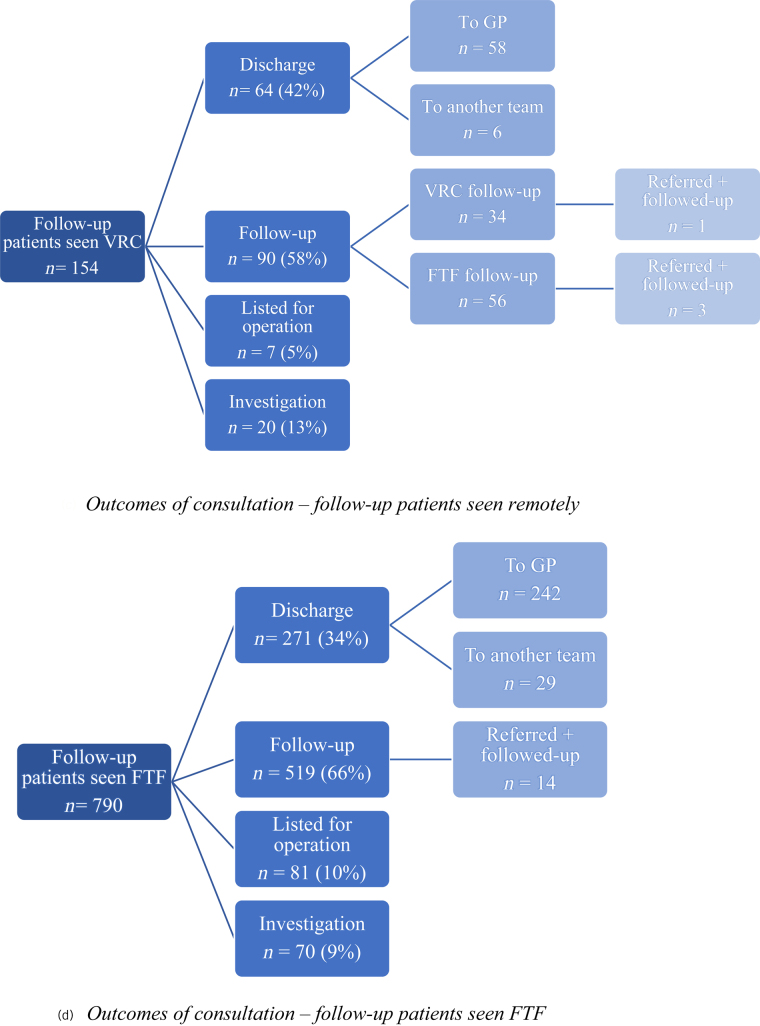
Figure 1 and Table 3 show outcomes of consultation and hand-off in each cohort. For new patients mean hand-off was higher at 2.2 for those seen remotely and 2.0 for those seen F2F (10% more hand-off if seen remotely; p < 0.00013). For follow-up patients in both the remote and F2F cohorts there was no significant difference, with mean hand-off 1.8 and 1.9 respectively (p < 0.11764).
Figure 1 .
Outcomes of consultation for (a) new patients seen remotely, (b) new patients seen face-to-face (F2F), (c) follow-up patients seen remotely and (d) follow-up patients seen F2F. GP = general practitioner; VRC = virtual remote clinic
Table 3 .
Hand-off outcomes of remote and face-to-face consultations for new and follow-up patients
| Hand-off point | Virtual remote clinic | Face-to-face | ||
|---|---|---|---|---|
| New | Follow-up | New | Follow-up | |
| Initial consultation | 272 | 154 | 743 | 790 |
| Follow-up consultation | 222 | 90 | 405 | 519 |
| Investigation | 101 | 20 | 203 | 70 |
| Surgery | 3 | 7 | 74 | 81 |
| Referral to another team | 10 | 10 | 74 | 43 |
| Total hand-off | 608 | 281 | 1,499 | 1,503 |
| Mean hand-off | 2.2 | 1.8 | 2.0 | 1.9 |
Figure 1 .
Continued.
Discussion
Our previous review suggests remote consultation in ENT holds promise for enhancing patient pathway efficiency, as well as saving time, cost and carbon emissions.1 However, we cautioned that previous studies showed large variation in outcomes and often with small sample sizes. Furthermore, few studies directly compared remote with F2F consultation or studied differences in outcomes of initial with follow-up consultation.
In the second quarter of 2020, the COVID-19 pandemic required our unit to adopt remote telephone consultation for almost all our patients, affording opportunity to evaluate this approach. It is noteworthy that the pandemic also reduced our capacity, with ∼70% fewer (remote) appointments scheduled during 2020 compared with the same period of (F2F) consultations in 2019. This may reflect the sudden drop in referrals from primary care, the redirection of resources such as money and manpower away from outpatient clinics and greater referral scrutiny within the department.
Our key finding is that new patients assessed remotely were significantly more likely to be followed-up and investigated than new patients seen in-person, as also reflected in a mean hand-off of 2.2 compared with 2.0 for those seen F2F. A higher hand-off number represents an increased potential for delay.7 Thus, for new patients, remote consultation may associate with less-efficient patient pathways. For follow-up patients, we found no difference in patient pathways (except listing for surgery). Overall, our findings suggest that, as a general rule, remote consultation in ENT is appropriate (and possibly preferable) for patients already under follow-up but should be used with more caution for new patients.
Our findings are supported by other studies that report new patients seen remotely have high rates of follow-up consultation of between 13% and 72%.8-13 Reasons for this wide range underpin the actuality of ENT as a speciality of facial cavities, where physical examination is consequently difficult to perform remotely. Furthermore, clinician concerns of missed or misdiagnosis, reluctance to discharge patients without physical examination, unease at listing for operation without in-person counselling and patient health-seeking behaviours are all commonly quoted factors in the literature.8-13 Nevertheless, we should continue to explore where remote consultation for new patients can be appropriate: for example, we have shown remote consultation to be effective and associated with high satisfaction in adults referred with recurrent sore throat for consideration of tonsillectomy.14
Previous studies also support our statement that remote consultation is more appropriate for follow-up patients (particularly postoperatively),15-18 with 1.5%–45% of such consultations requiring further review.1 In such patients, diagnosis is often established, and appointments may focus on response to treatment or discussing results, without a need for physical examination. However, further study is advisable to evaluate other patient pathway efficiency metrics in relation to this cohort of patients to assess the value of remote consultation in follow-up. As well as lead time and touch time, this could also include cost efficiency analysis and patient or provider satisfaction.
Study limitations
There are limits to our study findings and their generalisability. In subgroup analyses, some groups were small: in particular those seen remotely for follow-up or those seen remotely with predominant otology and rhinology symptoms, which increases risk of type II error. Furthermore, the team conducting consultations in both cohorts, although essentially the same, was composed of a mixture of levels of experience. This may have had an impact on individual clinic outcomes although we were unable to measure this because we did not have access to the relevant data.
The effect of the COVID-19 pandemic cannot be discounted, which could influence patient health-seeking behaviour or clinical decision making, and the smaller volume of patients seen remotely during the pandemic may be imperfectly matched to the larger historical F2F cohort. Recommendations for further study would be to analyse similar data sets for virtual clinics in a non-COVID-19 setting.
Although we reported remote consultation using telephone, our data may not apply to platforms such as video, text or email, or where clinical data such as images may be available to support diagnosis or management. The impact of remote consultation methods on clinic outcomes where image transfer is used in particular would be an important point of further study. Finally, we did not evaluate other metrics of the patient pathway such as lead time (referral to assessment/treatment time), touch time (duration of consultation) or environmental impacts such as carbon footprint, because we did not have access to relevant data.
Conclusion
Remote telephone consultation appears appropriate for follow-up of patients in ENT but should be used with more caution for new patients, where it associates with higher rates of follow-up and investigation, and lower patient pathway efficiency. Further study is advised outside a COVID-19 setting, of other methods of remote consultation and of its impact on other patient pathway metrics in order to broaden its application.
Acknowledgements
The assistance provided by all departmental consultants and GP with special interest in recording data on remote consultations is greatly appreciated.
Author contributions
TG acquired and analysed the data as well as drafting and revising the manuscript. MB supervised and revised the manuscript. Both authors have approved the manuscript for submission and agree to be accountable for the work presented.
Data availability statement
The data that supports the findings of this study are available from the corresponding author upon reasonable request.
References
- 1.Gupta T, Gkiousias V, Bhutta M. A systematic review of outcomes of remote consultation in ENT. Clin Otolaryngol 2021; 46: 699–719. [DOI] [PubMed] [Google Scholar]
- 2.Tysome J, Bhutta M. COVID-19: protecting our ENT workforce. Clin Otolaryngol 2020; 45: 311–312. [DOI] [PubMed] [Google Scholar]
- 3.Prasad A, Carey R, Rajasekaran K. Head and neck virtual medicine in a pandemic era: lessons from COVID -19. Head Neck 2020; 42: 1308–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Royal College of Surgeons. COVID-19: Good Practice For Surgeons And Surgical Teams. London: Royal College of Surgeons; 2020. [Google Scholar]
- 5.Garritano F, Goldenberg D. Successful telemedicine programs in otolaryngology. Otolaryngol Clin North Am 2011; 44: 1259–1274. [DOI] [PubMed] [Google Scholar]
- 6.Jacups S, Kinchin I, McConnon K. Ear, nose, and throat surgical access for remote living Indigenous children: what is the least costly model? J Eval Clin Pract 2018; 24: 1330–1338. [DOI] [PubMed] [Google Scholar]
- 7.NHS Institute for Innovation and Improvement. Improvement Leaders’ Guide: Process Mapping, Analysis And Redesign. Coventry: NHS Institute for Innovation and Improvement; 2017, 17–18. [Google Scholar]
- 8.Mandavia R, Lapa T, Smith M, Bhutta M. A cross-sectional evaluation of the validity of a smartphone otoscopy device in screening for ear disease in Nepal. Clin Otolaryngol 2017; 43: 31–38. [DOI] [PubMed] [Google Scholar]
- 9.Smith A, Dowthwaite S, Agnew J, Wootton R. Concordance between real-time telemedicine assessments and face-to-face consultations in paediatric otolaryngology. Med J Aust 2008; 188: 457–460. [DOI] [PubMed] [Google Scholar]
- 10.Moumoulidis I, Mani N, Patel H, Leong P. A novel use of photo messaging in the assessment of nasal fractures. J Telemed Telecare 2007; 13: 387–390. [DOI] [PubMed] [Google Scholar]
- 11.Sclafani A, Heneghan C, Stern J. Teleconsultation in otolaryngology: live versus “store- and-forward” consultations. Otolaryngol Head Neck Surg 1997; 117: 53–53. [DOI] [PubMed] [Google Scholar]
- 12.Heneghan C, Sclafani A, Stern J, Ginsburg J. Telemedicine applications in otoloryngology. IEEE Eng Med Biol Mag 1999; 18: 53–62, 79. [DOI] [PubMed] [Google Scholar]
- 13.Mughal Z, Iniowuari D, Clark M. Telephone triage is effective in identifying nasal fractures that require manipulation. Clin Otolaryngol 2021; 46: 682–686. [DOI] [PubMed] [Google Scholar]
- 14.Gupta T, Bowles P, Bhutta MF. Effectiveness, perceptions and environmental benefits of remote consultation for adults referred with recurrent tonsillitis. Ann R Coll Surg Eng 2022. [In press]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Urquhart A, Antoniotti N, Berg R. Telemedicine-An efficient and cost-effective approach in parathyroid surgery. Laryngoscope 2011; 121: 1422–1425. [DOI] [PubMed] [Google Scholar]
- 16.Jones D, Yoon M, Licameli G. Effectiveness of postoperative follow-up telephone interviews for patients who underwent adenotonsillectomy. Arch Otolaryngol –Head Neck Surg 2007; 133: 1091. [DOI] [PubMed] [Google Scholar]
- 17.Alemi A, Seth R, Heaton Cet al. Comparison of video and in-person free flap assessment following head and neck free tissue transfer. Otolaryngol–Head Neck Surg 2017; 156: 1035–1040. [DOI] [PubMed] [Google Scholar]
- 18.Rosbe K, Jones D, Jalisi S, Bray M. Efficacy of postoperative follow-up telephone calls for patients Who underwent adenotonsillectomy. Arch Otolaryngol–Head Neck Surg 2000; 126: 718. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that supports the findings of this study are available from the corresponding author upon reasonable request.