Abstract
Objectives
To compare hearing outcome and surgical complications between endoscopic classic and reversal stapedotomies.
Patients and methods
A prospective single blinded randomized clinical study carried out on 60 patients with otosclerosis who were randomized into two groups; each containing 30 patients. Patients in group 1 underwent endoscopic classic stapedotomy. Patients in group 2 underwent endoscopic reversal stapedotomy. Both groups were compared as regards hearing outcome and surgical complications.
Results
The difference in the hearing outcome between the two groups was statistically non-significant. Post-operative closure of the air bone gap (ABG) within 10 dB was attained in 76.67% and 80% of patients in groups 1 and 2, respectively. The differences in the surgical complications between the two studied groups were statistically non-significant.
Conclusion
Endoscopic classic and reversal stapedotomies are comparable to each other as regards hearing outcome and surgical complications. The authors recommend further studies with relatively larger sample size.
Keywords: Stapedotomy, Endoscopic, Classic, Reversal
Introduction
Otosclerosis is a remodeling disorder of the otic capsule where foci of resorbed bone were present, associated with newly formed bone, together with vascular proliferation [1]. Progressive hearing loss is the main presentation and stapes surgery; either stapedectomy or stapedotomy; is the primary treatment [2, 3]. Although some authors observed similar results with both methods (stapedectomy and stapedotomy), the current tendency is to replace stapedectomy with stapedotomy due to greater air bone gap (ABG) closure in high frequencies together with higher speech discrimination scores after surgery [4–6]. The order of the surgical steps during stapes surgery is another crucial factor. Accordingly, two techniques can be performed: classic and reversal techniques. The classic technique starts with removal of the stapes superstructure, followed by perforation of the stapes footplate, and ends with insertion of the Teflon piston. The reversal technique; on the other hand; begins with footplate perforation, then insertion of the Teflon piston, and ends with removal of the superstructure [7]. Throughout the literatures, many studies were conducted to compare classic and reversal stapedotomies. However, all these studies were carried out using the microscope. As far as we know, our current study is the first in the literatures that compared such two techniques endoscopically.
Patients and methods
This study was a prospective single blinded randomized clinical study carried out between September 2021 and September 2022. Approval from Institutional ethics committee was obtained (code: MS.21.11.1758). The study was conducted among 60 patients with clinical evidence of otosclerosis who were randomly divided into two equal groups (each containing 30 patients) using computer generated block randomization. Patients in group 1 underwent endoscopic classic stapedotomy while patients in group 2; on the other hand; underwent endoscopic reversal stapedotomy.
All involved patients had clinically evidenced otosclerosis including gradual progressive diminution of hearing with intact tympanic membrane, an audiogram showing ABG > 20 dB at the frequencies of 0.5, 1, 2 and 3 kHz together with absent stapedial reflex. Revision cases, cases with obliterative type of otosclerosis, and cases with facial nerve dehiscence were all excluded. Since narrow footplate is a contraindication for reversal stapedotomy, we also excluded all cases with narrow footplate to make the whole patients amenable for both classic and reversal stapedotomies. We defined narrow footplate as a footplate that could not accommodate a 0.7 mm manual perforator.
A 0° endoscope, 17 cm length and 4 mm diameter (Karl Storz, Germany) which was coupled to a high-definition (HD) camera head connected with a monitor (Karl Storz, Germany) were used. All surgeries were performed under local anesthesia (2% lidocaine with 1:50,000 epinephrine). The surgery began with 4 quadrant injection of the local anesthetic solution. Incision of the skin of the external ear canal was performed followed by tympano-meatal flap elevation towards the tympanic annulus. Entry to the middle ear was then carried out by raising of the tympanic annulus out of its sulcus. Curettage of the posterosuperior canal wall was carried out till the following structures were fully exposed: the stapes footplate, the facial nerve, the stapedial tendon and the pyramid. The ossicular chain mobility was then assessed to confirm the true diagnosis of otosclerosis. Measurement of the size of footplate was then done by using a 0.7 mm manual perforator. Cases where the footplate could not accommodate the 0.7 mm perforator were excluded because this would be a narrow footplate which is a contraindication for reversal stapedotomy.
Group 1
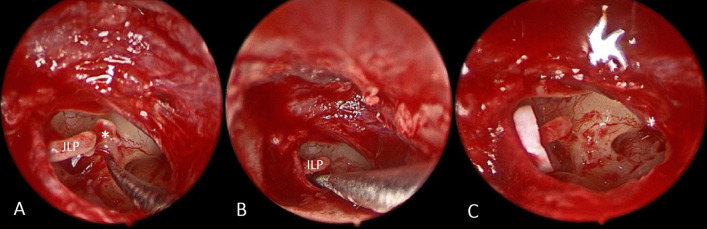
Classic stapedotomy was done starting by removal of the stapes superstructure (Fig. 1A). Using 0.7 mm manual perforator, perforation of the stapes footplate was then performed (Fig. 1B). The perforation was done under vision in alternating clockwise and counterclockwise rotatory movement and without pushing. A Teflon piston (0.6 mm in diameter) was inserted and fixed to the incus long process (Fig. 1C). The tympano-meatal flap was then repositioned and supported with small pieces of Gelfoam®.
Fig. 1.
Steps of endoscopic classic stapedotomy: A Removal of stapes superstructure. B Perforation of the stapes footplate. C Insertion of the Teflon piston. (*Stapes superstructure, ILP incus long process)
Group 2
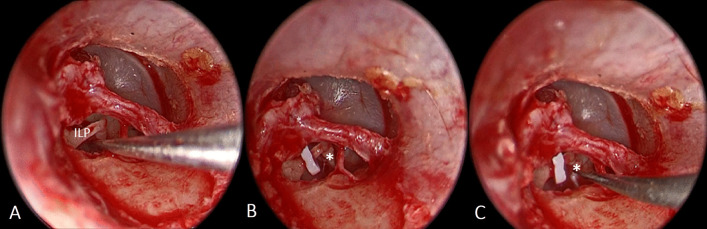
Reversal stapedotomy was performed which began by perforation of the footplate (Fig. 2A) using a 0.7 mm manual perforator under vision in alternating clockwise and counterclockwise rotatory movement and without pushing. This was followed by insertion of 0.6 mm in diameter Teflon piston (Fig. 2B). Finally, removal of the stapes superstructure was done (Fig. 2C). The tympano-meatal flap was then repositioned and supported with small pieces of Gelfoam®.
Fig. 2.
Steps of endoscopic reversal stapedotomy: A Perforation of the stapes footplate. B Insertion of the Teflon piston. C Removal of stapes superstructure. (*Stapes superstructure, ILP incus long process)
Follow-up
The initial scheduled visit for follow-up was carried out 1 week after surgery where the covering gauze was removed, and antibiotic ear drops were prescribed for 1 week. Audiological assessment was done 3 months after surgery in line with the guidelines of the American Academy of Otolaryngology- Head and Neck Surgery Committee on Hearing and Equilibrium. Pre- and post-operative air conduction (AC) thresholds and bone conduction (BC) thresholds were estimated at the frequencies 0.5, 1, 2, and 3 kHz. To calculate the 3 kHz results, the results for 2 and 4 kHz had to be averaged. The air bone gap (ABG) was estimated by calculating the difference between AC and BC thresholds [8].
Data collection and statistical analysis
Pre- and post-operative data were collected, tabulated, and analyzed. The data were presented in the form of mean ± standard deviation (SD). Analysis was done using SPSS for Windows version 28. statistical software program (Statistical Package for Social Sciences = SPSS Inc., Chicago, IL, USA). The paired t test was used for comparison of the pre-operative with the post-operative results. The chi-square test was utilized to compare the results of the two groups. A statistically significant result was considered when P value was < 0.05.
Results
Sixty patients were involved in this study. Group 1 comprised 30 patients: 19 females (63.33%) and 11 males (36.67%). Their mean age ± SD was 41.43 ± 10.76 years. Group 2 consisted of 30 patients: 21 females (70%) and 9 males (30%). Their mean age ± SD was 44.33 ± 8.14 years. Statistically non-significant differences in both sex and age between the two groups were found (P values for differences in sex and age between the two groups were 0.49 and 0.16 respectively).
Table 1 shows the pre- and post-operative hearing results in groups 1 and 2. The mean pre-operative AC thresholds in groups 1 and 2 were 56.21 ± 11.51 and 52.00 ± 10.47, respectively. Such difference was statistically non-significant (P value 0.14). The mean post-operative AC thresholds in groups 1 and 2 were 30.35 ± 14.22 and 27.82 ± 12.25 respectively, with statistically non-significant difference (P value 0.47). In both groups, statistically significant reductions in post-operative AC thresholds in comparison to the pre-operative values were reported (P value < 0.001 in both groups). The mean pre-operative BC thresholds in groups 1 and 2 were 23.54 ± 7.34 and 22.32 ± 4.73, respectively. Such difference was statistically non-significant (P value 0.43). The mean post-operative BC thresholds in groups 1 and 2 were 21.50 ± 12.27 and 20.17 ± 9.87 respectively, with statistically non-significant difference (P value 0.66). In both groups, no statistically significant differences between pre-operative and post-operative BC thresholds were reported (P values for groups 1 and 2 were 0.36 and 0.16, respectively). The mean pre-operative ABG thresholds in groups 1 and 2 were 32.67 ± 7.33 and 29.68 ± 8.40, respectively. Such difference was statistically non-significant (P value 0.15). The mean post-operative ABG thresholds in groups 1 and 2 were 8.92 ± 5.28 and 7.61 ± 5.52 respectively, with statistically non-significant difference (P value 0.29). In both groups, statistically significant reductions in post-operative ABG thresholds in comparison to the pre-operative values were reported (P value < 0.001 in both groups). The mean pre-operative speech reception thresholds (SRTs) in groups 1 and 2 were 55.67 ± 9.80 and 51.83 ± 6.88, respectively. Such difference was statistically non-significant (P value 0.08). The mean post-operative SRTs in groups 1 and 2 were 29.50 ± 12.82 and 24.83 ± 11.56 respectively, with statistically non-significant difference (P value 0.14). In both groups, statistically significant reductions in post-operative SRTs in comparison to the pre-operative values were reported (P value < 0.001 in both groups). The mean pre-operative speech discrimination scores (SDSs) in groups 1 and 2 were 95.73 ± 7.12 and 97.47 ± 3.28, respectively. Such difference was statistically non-significant (P value 0.26). The mean post-operative SDSs in groups 1 and 2 were 96.13 ± 7.08 and 97.67 ± 3.16 respectively, with statistically non-significant difference (P value 0.31). In both groups, no statistically significant differences between pre-operative and post-operative SDSs were reported (P values in groups 1 and 2 were 0.08 and 0.18, respectively).
Table 1.
Comparison between groups 1 and 2 as regard mean AC, BC, ABG, SRT and SDS
| Group 1 | Group 2 | P value | |
|---|---|---|---|
| AC threshold (mean ± SD) | |||
| Preoperative | 56.21 ± 11.51 | 52.00 ± 10.47 | 0.14 |
| Postoperative | 30.35 ± 14.22 | 27.82 ± 12.25 | 0.47 |
| P value | < 0.001 | < 0.001 | |
| BC threshold (mean ± SD) | |||
| Preoperative | 23.54 ± 7.34 | 22.32 ± 4.73 | 0.43 |
| Postoperative | 21.50 ± 12.27 | 20.17 ± 9.87 | 0.66 |
| P value | 0.36 | 0.16 | |
| ABG (mean ± SD) | |||
| Preoperative | 32.67 ± 7.33 | 29.68 ± 8.40 | 0.15 |
| Postoperative | 8.92 ± 5.28 | 7.61 ± 5.52 | 0.29 |
| P value | < 0.001 | < 0.001 | |
| SRT (mean ± SD) | |||
| Preoperative | 55.67 ± 9.80 | 51.83 ± 6.88 | 0.08 |
| Postoperative | 29.50 ± 12.82 | 24.83 ± 11.56 | 0.14 |
| P value | < 0.001 | < 0.001 | |
| SDS (mean ± SD) | |||
| Preoperative | 95.73 ± 7.12 | 97.47 ± 3.28 | 0.26 |
| Postoperative | 96.13 ± 7.08 | 97.67 ± 3.16 | 0.31 |
| P value | 0.08 | 0.18 |
Post-operative closure of the ABG within 10 dB was attained in 23 cases in group 1 (76.67%) and in 24 cases in group 2 (80%). Such difference was statistically non-significant (P value 0.77).
Table 2 shows the incidence of complications among both groups. Neither sensory neural hearing loss nor floating footplate were reported in the two groups. A tear in the tympanic membrane occurred in only 1 case in group 1 while in group 2, no tears were encountered. Such difference in the incidence of the tears in the tympanic membrane was statistically non-significant (P value 0.33). Incus subluxation occurred in 2 cases in group 1 (6.66%) and 1 case in group 2 (3.33%) with statistically non-significant difference (P value 0.33). Vertigo was encountered in 6 cases (20.00%) in group 1 and in 4 cases (13.33%) in group 2 with statistically non-significant difference (P value 0.16). Taste disturbance reported in 6 cases (20.00%) in group 1 and in 3 cases (10.00%) in group 2 with statistically non-significant difference (P value 0.08).
Table 2.
Difference in complications between the 2 groups:
| Group 1 | Group 2 | P value | |
|---|---|---|---|
| Sensory neural hearing loss | 0 (0%) | 0 (0%) | – |
| Floating footplate | 0 (0%) | 0 (0%) | – |
| Tympanic membrane tear | 1 (3.33%) | 0 (0%) | 0.33 |
| Incus subluxation | 2 (6.66%) | 1 (3.33%) | 0.33 |
| Vertigo | 6 (20.00%) | 4 (13.33%) | 0.16 |
| Taste disturbance | 6 (20.00%) | 3 (10.00%) | 0.08 |
Discussion
Surgical techniques for treatment of otosclerosis have been improved, updated, or adjusted over time to lower intraoperative and post-operative problems and boost overall effectiveness [9]. The order of surgical steps had been a matter of debate. Early cases were treated with classic stapedotomy, where the stapes superstructure was first removed, the footplate was then perforated, and lastly the prosthesis was fixed to the incus. Fisch provided a different sequence of the surgical steps where he first performed perforation of the stapes footplate, then removed the stapes superstructure and finally inserted the prosthesis. Then he shifted towards a whole reversal of the classic stapedotomy steps where he started by perforation of the stapes footplate, then inserted the prosthesis and in the end removed the stapes superstructure [7].
Not only the order of surgical steps was debatable but also the surgical tool, whether to use the microscope or the endoscope. Different studies compared microscopic with endoscopic stapedotomy. Although hearing outcome and post-operative complications were comparable, the endoscope gives a very important advantage which is the excellent visualization [10–14].
The utilization of endoscope in stapes surgery has many advantages. The wide angle of view offered by endoscope allows better exposure of both stapes and its footplate. In addition, it facilitates detection of any anatomical variations or pathological changes. Moreover, it allows confirmation of the proper insertion of the prosthesis [15, 16]. Despite these advantages, endoscope also has many disadvantages. One of these disadvantages is the single-handed surgery as the other hand is occupied the endoscope. In addition, endoscope appeared to enhance exposure not necessarily visualization. Moreover, the incidence of perforation of the tympanic membrane during flap elevation; using the endoscope; was high. Furthermore, the incidence of chorda tympani injury with subsequent dysgeusia was high when the endoscope was used in stapes surgery [17]. As in every modern surgical technique, endoscopic stapes surgery has a learning curve that should be overcome. Such learning curve is longer for endoscopic than microscopic ear surgery [18–20] making it the main cause that dampen most otologists from starting endoscopic stapedotomy [20]. In addition, the depth of perception is reduced when the endoscope is used. Such problem can be overcome by changing the viewpoint while moving the endoscope and the surgical instruments in the field. In addition, the progress in the learning curve converts this problem into a minor one [18, 21].
Throughout the literatures, many studies were conducted to compare classic and reversal stapedotomies. All these studies were performed using the microscope. To our knowledge, our current study is the first in the literatures that compared classic and reversal stapedotomies using the endoscope.
In our study, statistically significant reductions in post-operative AC thresholds, ABGs and SRTs were obtained in both groups indicating that both techniques were effective in management of associated hearing loss. When both groups were compared, no statistically significant differences in post-operative AC thresholds, ABGs or SRTs were found. Moreover, closure of the ABG within 10 dB was attained in 76.67% and 80% of cases in groups 1 and 2 respectively, with statistically non- significant difference. All these findings suggested that endoscopic classic and reversal techniques were comparable as regards hearing outcome. Such finding was in agreement with the previously published studies [22–27].
Sensorineural hearing loss is relatively uncommon complication [28]. It is believed to occur due injury of the inner ear either during perforation or during insertion of the prosthesis. When the technical fault is ruled out, other causes are conceivable including reparative granuloma, labyrinthitis, and perilymph fistula [29].
During stapes surgery, small perforations of the tympanic membrane are usually closed with fascial graft at the end of the surgery with excellent result. Injury of the chorda tympani typically occurs during curettage or during its mobilization to expose the oval window. Such complication was estimated to occur in about 3% of cases in the literatures [30, 31]. House proposed that division of the chorda tympani; in comparison to stretching and manipulation; gives milder symptoms [32]. Mahendran et al., on the contrary, did not agree with these results. They evaluated the impacts of cutting and manipulation of the chorda tympani and presumed that whenever possible, the chorda tympani would be preserved since its cutting ends in significantly worse symptoms than its manipulation [31].
In our study, no sensory neural hearing loss was encountered in any of the cases of both groups. In addition, no statistically significant differences were reported between the two groups as regards post-operative vertigo and taste disturbance. All these findings were comparable to the previously published studies [22–27].
Floating footplate is one of the major complications that may be encountered during stapes surgery. In this condition, the footplate is accidently mobilized and may be pushed into the vestibule. Such complication may occur when the footplate is pushed too strong with manual perforator or even with microdrill. To avoid this complication, perforation should be done before removal of the stapes superstructure (as in reversal stapedotomy). Such support provided by the stapes superstructure will prevent footplate mobilization during perforation. Another method of prevention of such complication was the utilization of CO2 laser in the perforation, which enables the surgeon to create a perforation in the footplate without pushing on the footplate [33]. Accordingly, it is unsurprising to find in the literatures that reversal stapedotomy or the utilization of CO2 laser are the best ways to prevent such complication [22–27]. In our study, on the other hand, we did not encounter floating footplate in any of the cases of both groups. This was because alternating clockwise and counterclockwise rotatory movement without pushing will perforate rather than push the footplate. In addition, the excellent visualization provided by the endoscope allowed us to see and feel the perforation making it controlled perforation. On the hand, during microscopic stapedotomy we usually feel the perforation more than we see it except after its creation, so the perforation is usually uncontrolled with liability for pushing that may result in floating footplate. Accordingly, we can say that endoscopic stapedotomy together with alternating clockwise and counterclockwise rotatory perforation without pushing can prevent floating footplate.
Incus subluxation was another complication that may be encountered during stapes surgery. It was reported to occur if removal of stapes superstructure was done before insertion of the prosthesis. Thus, it is also unsurprising to encounter such complication in classic stapedotomy than in reversal type [15, 16, 18, 19, 21, 22]. In our study, on the other hand, no significant difference in the incidence of incus subluxation was reported between the two groups. This may indicate that the utilization of the endoscope may reduce the incidence of incus subluxation during classic stapedotomy. This may be explained by the fact that better visualization (offered by the endoscope) allows smooth insertion of the prosthesis without excessive manipulation that may cause incus subluxation. Such finding gives an advantage for the endoscope over the microscope during stapes surgery.
Since this study; to our knowledge; is the first randomized controlled trial that compared classic and reversal stapedotomy techniques endoscopically, the authors are encouraging further studies with relatively larger sample size.
Conclusion
Endoscopic classic and reversal stapedotomies are comparable to each other as regards hearing outcome and surgical complications. The authors recommend further studies with relatively larger sample size.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
All authors declare that they had no conflicts of interest.
Research involving human participants and/or animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants involved in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Quesnel AM, Ishai R, McKenna MJ. Otosclerosis: temporal bone pathology. Otolaryngol Clin North Am. 2018;51:291–303. doi: 10.1016/j.otc.2017.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Yeh CF, Wang MC, Chu CH, Shiao AS. Predictors of hearing outcomes after stapes surgery in otosclerosis. Acta Otolaryngol. 2019;139:1058–1062. doi: 10.1080/00016489.2019.1648866. [DOI] [PubMed] [Google Scholar]
- 3.Foster MF, Backous DD. Clinical evaluation of the patient with otosclerosis. Otolaryngol Clin North Am. 2018;51:319–326. doi: 10.1016/j.otc.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 4.House HP, Hansen MR, Dakhail A, House JW. Stapedectomy versus stapedotomy: comparison of results with long-term follow-up. Laryngoscope. 2002;112:2046–2050. doi: 10.1097/00005537-200211000-00025. [DOI] [PubMed] [Google Scholar]
- 5.Kürsten R, Schneider B, Zrunek M. Long-term results after stapedectomy versus stapedotomy. Am J Otol. 1994;15:804–806. [PubMed] [Google Scholar]
- 6.Kos MI, Montandon PB, Guyot JP. Short-and long-term results of stapedotomy and stapedectomy with a Teflon-wire piston prosthesis. Ann Otol Rhinol Laryngol. 2001;110:907–911. doi: 10.1177/000348940111001003. [DOI] [PubMed] [Google Scholar]
- 7.Fisch U. Stapedotomy versus stapedectomy. Am J Otol. 1982;4:112–117. [PubMed] [Google Scholar]
- 8.Gurgel RK, Jackler RK, Dobie RA, Popelka GR. A new standardized format for reporting hearing outcome in clinical trials. Otolaryngol Head Neck Surg. 2012;147:803–807. doi: 10.1177/0194599812458401. [DOI] [PubMed] [Google Scholar]
- 9.Hashemi B, Bozorgi H, Sehat M. A review on reversal stapedotomy outcome and associated factors. Oper Tech Otolayngol Head Neck Surg. 2020;31:e47–e52. doi: 10.1016/j.otot.2020.08.001. [DOI] [Google Scholar]
- 10.Surmelioglu O, Ozdemir S, Tarkan O, Tuncer U, Dagkiran M, Cetik F. Endoscopic versus microscopic stapes surgery. Auris Nasus Larynx. 2017;44:253–257. doi: 10.1016/j.anl.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Sproat R, Yiannakis C, Iyer A. Endoscopic stapes surgery: a comparison with microscopic surgery. Otol Neurotol. 2017;38:662–666. doi: 10.1097/MAO.0000000000001371. [DOI] [PubMed] [Google Scholar]
- 12.Kojima H, Komori M, Chikazawa S, Yaguchi Y, Yamamoto K, Chujo K, Moriyama H. Comparison between endoscopic and microscopic stapes surgery. Laryngoscope. 2014;124:266–271. doi: 10.1002/lary.24144. [DOI] [PubMed] [Google Scholar]
- 13.Koukkoullis A, Tóth I, Gede N, Szakács Z, Hegyi P, Varga G, Révész P. Endoscopic versus microscopic stapes surgery outcomes: a meta-analysis and systematic review. Laryngoscope. 2020;130:2019–2027. doi: 10.1002/lary.28353. [DOI] [PubMed] [Google Scholar]
- 14.Moneir W, Abd El-fattah AM, Mahmoud E, Elshaer M. Endoscopic stapedotomy: merits and demerits. J Otol. 2018;13:97–100. doi: 10.1016/j.joto.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hunter JB, Rivas A. Outcomes following endoscopic stapes surgery. Otolaryngol Clin North Am. 2016;49:1215–1225. doi: 10.1016/j.otc.2016.05.012. [DOI] [PubMed] [Google Scholar]
- 16.Júnior JFN, Martins MJB, Aguiar CV, Pinheiro AI. Fully endoscopic stapes surgery (stapedotomy): technique and preliminary results. Braz J Otorhinolaryngol. 2011;77:721–727. doi: 10.1590/S1808-86942011000600008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hoskison EE, Harrop E, Jufas N, Kong JH, Patel NP, Saxby AJ. Endoscopic stapedotomy: a systematic review. Otol Neurotol. 2021;42:e1638–e1643. doi: 10.1097/MAO.0000000000003242. [DOI] [PubMed] [Google Scholar]
- 18.Hunter JB, O’Connell BP, Rivas A. Endoscopic techniques in tympanoplasty and stapes surgery. Curr Opin Otolaryngol Head Neck Surg. 2016;24:388–394. doi: 10.1097/MOO.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 19.Iannella G, Magliulo G. Endoscopic versus microscopic approach in stapes surgery: are operative times and learning curve important for making the choice? Otol Neurotol. 2016;37:1350–1357. doi: 10.1097/MAO.0000000000001186. [DOI] [PubMed] [Google Scholar]
- 20.Bartel R, Sanz JJ, Clemente I, Simonetti G, Viscacillas G, Palomino L, Lao X. Endoscopic stapes surgery outcomes and complication rates: a systematic review. Eur Arch Otorhinolaryngol. 2021;278:2673–2679. doi: 10.1007/s00405-020-06388-8. [DOI] [PubMed] [Google Scholar]
- 21.Fernandez IJ, Bonali M, Ghirelli M, Presutti L. Limits in endoscopic ear surgery. HNO. 2021;69:803–810. doi: 10.1007/s00106-021-01051-y. [DOI] [PubMed] [Google Scholar]
- 22.Fiorino F, Barbieri F. Reversal of the steps stapedotomy technique with early removal of the posterior crus: early post-operative results: how we do it. Clin Otolaryngol. 2008;33:359–362. doi: 10.1111/j.1749-4486.2008.01707.x. [DOI] [PubMed] [Google Scholar]
- 23.Szymański M, Gołabek W, Morshed K, Siwiec H. The influence of the sequence of surgical steps on complications rate in stapedotomy. Otol Neurotol. 2007;28:152–156. doi: 10.1097/01.mao.0000247815.23948.89. [DOI] [PubMed] [Google Scholar]
- 24.Lang EE, Waheed K, Colreavy M, Burns H. A retrospective review of stapes surgery following introduction of ‘reversal of the steps’ technique. Clin Otolaryngol Allied Sci. 2004;29:571–573. doi: 10.1111/j.1365-2273.2004.00863.x. [DOI] [PubMed] [Google Scholar]
- 25.Arsović NA, Babić BB, Djukić VB, Mikić BM, Milovanović AP, Panović BM, Ugrinović AB. Preliminary results of applying the inverse stapedotomy. Acta Chir Iugosl. 2009;56:23–27. doi: 10.2298/aci0903023a. [DOI] [PubMed] [Google Scholar]
- 26.Huang H, Wu P, Xu M, Ge R. The effect of reversal steps stapedotomy on the treatment of otosclerosis. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2011;25:1022–1024. [PubMed] [Google Scholar]
- 27.Freni F, Mannella VK, Cammaroto G, Azielli C, Cappuccio C, Galletti F. Classic and reversal steps stapedotomy performed with CO2 laser: a comparative analysis. Eur Arch Otorhinolaryngol. 2014;271:981–986. doi: 10.1007/s00405-013-2500-6. [DOI] [PubMed] [Google Scholar]
- 28.Häusler R. Fortschritte in der Stapeschirurgie. Laryngorhinootologie. 2000;79:S95–S139. doi: 10.1055/s-2000-15920. [DOI] [Google Scholar]
- 29.Rangheard AS, Marsot-Dupuch K, Mark AS, Meyer B, Tubiana JM. Post-operative complications in otospongiosis: usefulness of MR imaging. AJNR Am J Neuroradiol. 2001;22:1171–1178. [PMC free article] [PubMed] [Google Scholar]
- 30.Lescanne E, Moriniere S, Gohler C, Manceau A, Beutter P, Robier A. Retrospective case study of carbon dioxide laser stapedotomy with lens-based and mirror-based micromanipulators. J Laryngol Otol. 2003;117:256–260. doi: 10.1258/00222150360600832. [DOI] [PubMed] [Google Scholar]
- 31.Mahendran S, Hogg R, Robinson JM. To divide or manipulate the chorda tympani in stapedotomy. Eur Arch Otorhinolaryngol. 2005;262:482–487. doi: 10.1007/s00405-004-0854-5. [DOI] [PubMed] [Google Scholar]
- 32.House HP. Early and late complications of stapes surgery. Arch Otolaryngol. 1963;78:606–613. doi: 10.1001/archotol.1963.00750020618022. [DOI] [PubMed] [Google Scholar]
- 33.Beatty TW, Haberkamp TJ, Khafagy YW, Bresemann JA. Stapedectomy training with the carbon dioxide laser. Laryngoscope. 1997;107:1441–1444. doi: 10.1097/00005537-199711000-00004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.