Abstract
Background:
The burden of stroke (a leading cause of disability and mortality) in Africa appears to be increasing, but a systematic review of the best available data to support or refute this observation is lacking.
Aim:
To determine the incidence and 1-month case-fatality rates from high-quality studies of stroke epidemiology among Africans.
Summary of review:
We searched and retrieved eligible articles on stroke epidemiology among indigenous Africans in bibliographic databases (MEDLINE, ScienceDirect, Google Scholar, and Cochrane library) using predefined search terms from the earliest records through January 2022. Methodological assessment of eligible studies was conducted using the Newcastle–Ottawa scale. Pooling of incidence and case-fatality rates was performed via generalized linear models (Poisson-Normal random-effects model). Of the 922 articles retrieved, 14 studies were eligible for inclusion. The total number of stroke cases was 2568, with a population denominator (total sample size included in population-based registries or those who agreed to participate in door-to-door community studies) of 3,384,102. The pooled crude incidence rate of stroke per 100,000 persons in Africa was 106.49 (95% confidence interval (CI) = 58.59–193.55), I2 = 99.6%. The point estimate of the crude incidence rate was higher among males, 111.33 (95% CI = 56.31–220.12), I2 = 99.2%, than females, 91.14 (95% CI = 47.09–176.37), I2 = 98.9%. One-month case-fatality rate was 24.45 (95% CI = 16.84–35.50), I2 = 96.8%, with lower estimates among males, 22.68 (95% CI = 18.62–27.63), I2 = 12.9%, than females, 27.57 (95% CI = 21.47–35.40), I2 = 51.6%.
Conclusion:
The burden of stroke in Africa remains very high. However, little is known about the dynamics of stroke epidemiology among Africans due to the dearth of high-quality evidence. Further continent-wide rigorous epidemiological studies and surveillance programs using the World Health Organization STEPwise approach to Surveillance (WHO STEPS) framework are needed.
Keywords: Stroke, epidemiology, incidence, case fatality, Africa, systematic review, meta-analysis
Introduction
Stroke is a principal cause of disability and mortality worldwide,1–3 with significant increases in epidemiological burden in low- and middle-income countries (LMICs).4–6 Recent evidence suggests a rapidly growing burden of stroke in Africa with an annual age-adjusted incidence as high as 316 per 100,000 persons, an age-adjusted prevalence of up to 1460 per 100,000 persons, and a 3-year fatality rate of up to 84%.5 Also, stroke and stroke-related disability accounted for 70% and 80% of all mortality in LMICs between 1970 and 2020.5
The case for the high burden of stroke in Africa is mounting, but large geographical regions of the continent are without high-quality incidence and case-fatality data. Also, the quality of earlier systematic reviews7–9 has been limited by the high heterogeneity across studies and deficiencies in standardized methods of evaluating stroke epidemiology. Many studies on stroke epidemiology among Africans were characterized by low statistical power and poor generalizability across the hugely diverse African population. There are several stroke prevalence studies among Africans. However, they do not provide a clear picture of the African stroke landscape and have limited policy implications and priority settings related to interventions for stroke prevention, surveillance, acute care and rehabilitation among Africans.6 Therefore, an estimate of the burden of stroke using high-quality stroke incidence studies in Africa is important, in the light of newer studies, to advance the understanding of stroke science and care in Africa. Thus, we pooled data from high-quality epidemiological stroke studies to determine the true stroke incidence and 30-day case-fatality rates (CFRs) among Africans.
Methods
This systematic review and meta-analysis were conducted in accordance with the MOOSE (Meta-analysis of Observational Studies in Epidemiology) guidelines10 and reported using the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) framework.11 The protocol was prospectively registered in PROSPERO.12
Search strategy and study selection
The search strategy used “stroke” terms from the Cochrane Stroke Strategy 202013 and an adapted filter14 to search for previously published reports on the epidemiology of stroke among indigenous Africans in MEDLINE (OVID), EMBASE (OVID), AJOL, EBSCO, Google Scholar, Cochrane Library, IMSEAR via Global Index Medicus, Science Citation Index Expanded (SCI-EXPANDED), Social Sciences Citation Index, and Arts & Humanities Citation Index within ISI Web of Science (from the earliest possible record to January 2022). Reference lists of retrieved studies were reviewed for additional studies.
Inclusion criteria
Studies were eligible based on the following criteria: population boundaries defined within Africa, prospective and consecutive recruitment, pre-specified sampling plan, complete community-based case-ascertainment of stroke (with multiple overlapping sources) or non-community-based case-ascertainment (acute hospital-based registry, rehabilitationbased registry), including case series and case-control studies. Studies were included if stroke was confirmed based on a predefined set of criteria, for example, World Health Organization (WHO),15 or clinical criteria (confirmed by imaging, where possible), including cerebral infarction, intracerebral hemorrhage, subarachnoid hemorrhage, or uncertain pathological subtypes with no restrictions on age, sex, degree of impairment post-stroke, or interventions.
Exclusion criteria
Studies were excluded if they were case studies, randomized controlled trials, reviews, epidemiological reports from mixed populations (e.g. stroke and head injury) without specific results for the stroke population, cross-sectional or retrospective recruitment, qualitative assessment only, or adopted convenience sampling. All references were collated using EndNote,16 and duplicates were removed using the EndNote automated function and then manually.
Data collection and analysis
Three independent reviewers (A.P.O., O.A., and S.J.) screened the title or abstract of all citations, two reviewers (S.J. and R.A.) were randomly assigned to evaluate the selected citations, and disagreements were resolved by recourse to a third reviewer (M.H., C.W., and M.O.) to reach a consensus. The article with the most comprehensive dataset was selected when there were multiple articles from the same study population with evidence of overlapping data or identical participant characteristics. The search strategy and selection procedure are detailed in Figure 1.
Figure 1.
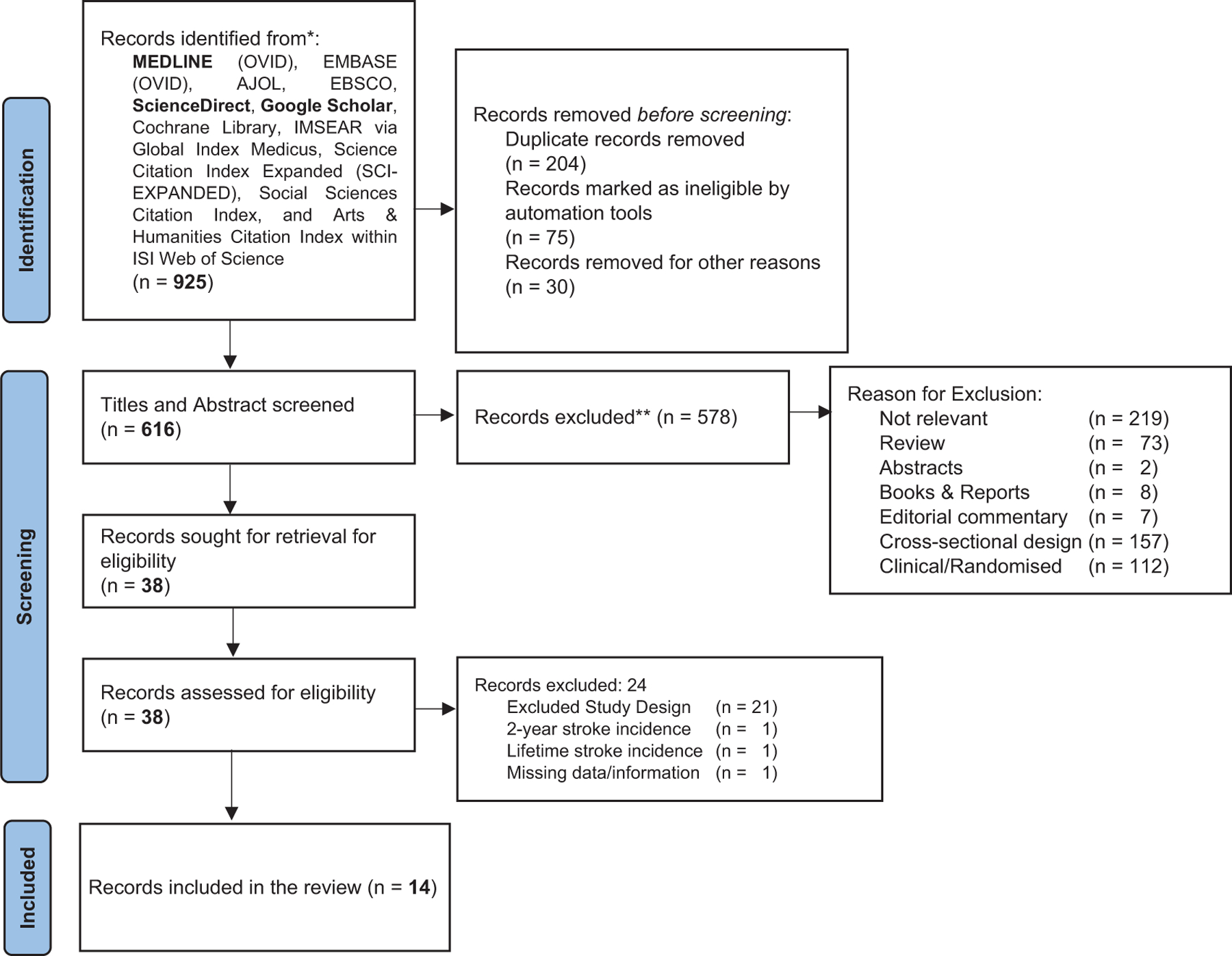
PRISMA flowchart of study selection.
Data extraction, selection, and coding
Data extraction was carried out independently by two reviewers (A.P.O. and O.A.) using a previously designed proforma,15 verified by another reviewer (S.J.). The difference(s) was resolved in an organized discussion in the review team. Extracted data included author, year, study name, sample characteristics (country, city, study period, and design), and epidemiological data (number of stroke cases and subtype, age, crude incidence, 1-month CFR).
Assessment of risk of methodological bias
The Newcastle–Ottawa scale was used to determine the risk of bias (see Supplementary Table 1).
Statistical analysis
Using data reported in the original studies, we (re-)calculated crude incidence and 1-month CFRs along with 95% confidence interval (95% CI). Then, we performed meta-analyses for each outcome fitting a generalized linear model using Poisson-Normal random-effects models. To assess quantitative heterogeneity, we have performed a subgroup analysis by the sex and study setting (community-based or hospital-based) for the overall incidence of stroke and fitted a series of meta-regressions using follow-up lengths as a fixed-effect covariate. We performed a formal homogeneity test and reported the proportion of variability attributable to heterogeneity rather than chance (I2). Statistical analyses were performed using the metafor package of the R software.17
Results
Study characteristics and epidemiological data from included reports
Of 925 records retrieved (Figure 1), 14 reports18–31 from 13 studies across 9 African countries (Table 1) were included. We searched references of studies eligibility during screening and found no additional studies eligible for inclusion. The earliest record was from Benghazi, Libya, published in 1986, and the most recent report was from Akure, Nigeria, published in 2015. More than three-quarters of the studies were conducted in urban areas, with a minimum surveillance period of 6 months. Crude stroke incidence rates were reported in 818–25 reports, and 626–31 of the 10 articles on CFR18,20,22,25–31 reported CFR only (Figure 2, Supplementary Table 2). Six reports were primarily community-based (i.e. recruitment of participants was in a community-based setting),21–25,27 and eight were hospital-based (i.e. recruitment of participants was in a clinical setting).18–20,26,28–31 The total number of recorded strokes was 2568, with a population denominator (total sample included in population-based registries or those who agreed to participate in the door-to-door community studies) of 3,384,102 (see Supplementary Table 2). Five studies reported in-hospital 30-day CFR,20,22,25,28,29 two30,31 reported results from verbal autopsies, and 1013 deaths (out of 3157 stroke events) were recorded within 30 days of stroke onset.
Table 1.
A summary of the characteristics of included studies on stroke epidemiology in Africa.
| Study | Study period | Country | Location | Population type | Study design | Duration of surveillancea | Frequency of surveillance | Population denominator | Female N (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Incidence studies | ||||||||||
| 1 | Ashok et al.18 | November 1983-October 1984 | Libya | Benghazi | Urban | Hospital-based registry | 12 | Continuous* | 518,745 | 251,155 (48.4) |
| 2 | Matenga19 | January–December 1991 | Zimbabwe | Harare | Urban | Hospital-based registry | 12 | Continuous* | 887,768 | NR |
| 3 | Damasceno et al.20 | August 2005-July 2006 | Mozambique | Maputo | Urban | Hospital-based registry | 12 | Continuous* | NR | NR |
| 4 | Walker et al.21 | June 2003-June 2006 | Tanzania | Hai Dar es Salaam | Urban and rural | Community and hospital-based registry | 36 | Continuous* | 159,814 56,517 |
82,242 (51.5) 28,654 (50.7) |
| 5 | Danesi et al.22 | January–December 2007 | Nigeria | Lagos | Urban | Community-based | 12 | Continuous* | 750,000 | 333,000 (44.4) |
| 6 | El-Tallawy et al.23 | July 2009-January 2012 | Egypt | Al Quseir | Urban | Community-based | 30 | Continuous* | 33,285 | NR |
| 7 | Farghaly et al.24 | June 2005-May 2008 | Egypt | Al-Kharga | Urban and rural | Community-based | 36 | Continuous* | 62,583 | 30,418 (48.6) |
| 8 | Okon et al.25 | November 2010-October 2011 | Nigeria | Akure | Urban | Community-based registry | 12 | Continuous* | 491,033 | 245,835 (50.1) |
| Case fatality studies only | ||||||||||
| 9 | Garbusinski et al.26 | February 2000-February 2001 | The Gambia | Banjul | Urban | Hospital-based registry | 12 | Quarterly | NR | NR |
| 10 | Walker et al.27 | June 2003-June 2006 | Tanzania | Hai Dar es Salaam | Urban and rural | Community and hospital-based registry | 36–72 | Post-stroke follow-up until June 2009 | 159,814 | |
| 11 | Gomes et al.28 | August 2005-July 2006 | Mozambique | Maputo | Urban | Hospital-based registry | 12 | Continuous* | NR | NR |
| 12 | Nakibuuka et al.29 | February-August 2014 | Uganda | Kampala | Urban | Hospital-based registry | 6 | Continuous* | NR | NR |
| 13 | Nkoke et al.30 | NR | Cameroon | Yaounde | Urban | Hospital-based registry | 12 | Monthly | NR | NR |
| 14 | Okeng’o et al.31 | January-June 2013 | Tanzania | Dar es Salaam | Urban | Hospital-based registry | 6 | NR | NR | NR |
NR: not reported.
Duration of surveillance in months.
Most of these studies did not report continuous verbatim, but the description in the method depicted so.
Figure 2.
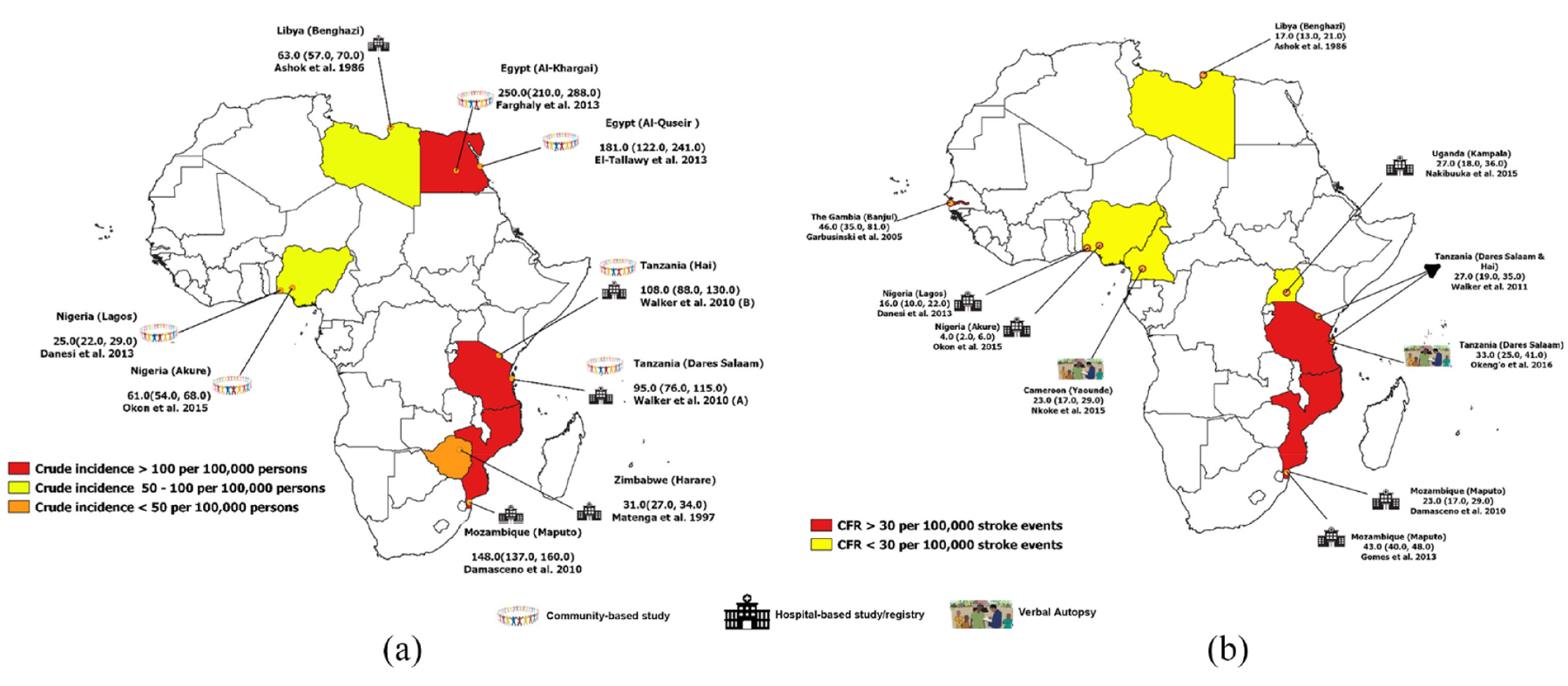
Location of studies assessing the crude incidence (a) and case-fatality rate—CFR (b) of stroke in Africa.
The crude annual incidence rate of stroke among Africans varied widely, from 25 (Danesi et al. in Lagos, Nigeria)22 to ≈250 (Farghaly et al. in Al-Kharga District, Egypt)24 per 100,000 persons. The point estimate of the sex-disaggregated crude incidence rate was generally higher among males, and the age-adjusted incidence rate ranged from 54 (Danesi et al. in Lagos, Nigeria)22 to 316 (Walker et al. in Dar-es-Salaam, Tanzania).21 There was considerable variation in the 1-month CFRs from 4.0 (Okon et al. in Akure, Nigeria)25 to ≈50 (Damasceno et al. in Maputo, Mozambique)20 per 100,000 stroke events.
Crude incidence rate and 30-day CFR of stroke in Africa
The pooled crude incidence rate of stroke (per 100,000 persons) from eight studies was 106.49 (95% CI: 58.59–193.55), I2 = 99.6% (Figure 3). For studies reporting data by sex, the point estimate of the crude incidence rate was higher among males, 111.33 (95% CI: 56.31–220.12), I 2 = 99.2%, than females, 91.14 (95% CI: 47.09–176.37), I2 = 98.9%. Also, meta-regression results revealed that stroke incidence rates increased by 1.17 per 100,000 per person for every month increase in the follow-up period (Supplementary Table 3). When we adjusted for the follow-up period, I2 reduced from 99.6% to 98.3% in the overall pooled analyses. We performed subgroup analyses (Figure 4) and found the pooled point estimate of the crude incidence of stroke was higher among community-based studies, 90.23 (95% CI: 37.03–219.88), I2 = 99.2%, than hospital-based studies, 66.19 (95% CI: 31.91–137.31), I2 = 99.4%, although the CIs were largely overlapping. Furthermore, the pooled CFR of stroke (per 100,000 stroke events) from 10 eligible studies was 24.45 (95% CI: 16.84–35.50), I2 = 96.8% (Figure 5). The point estimate of the CFR was lower among males, 22.68 (95% CI: 18.62–27.63), I2 = 12.9%, than females, 27.57 (95% CI: 21.47–35.40), I2 = 51.6%.
Figure 3.
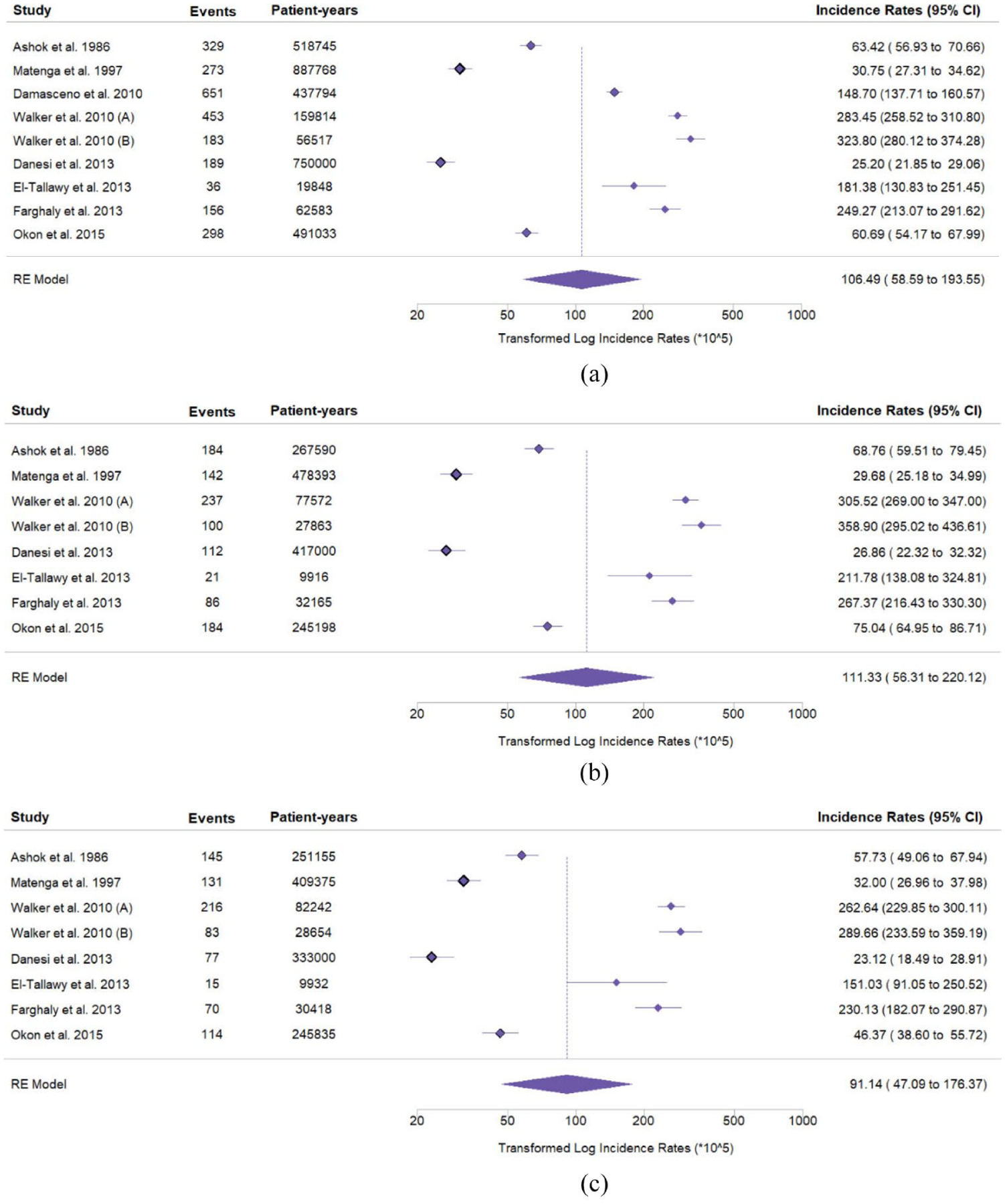
Forest plots on the pooled crude annual incidence of stroke per 100,000 persons in the overall population (a), among males (b) and females (c) in Africa.
Figure 4.
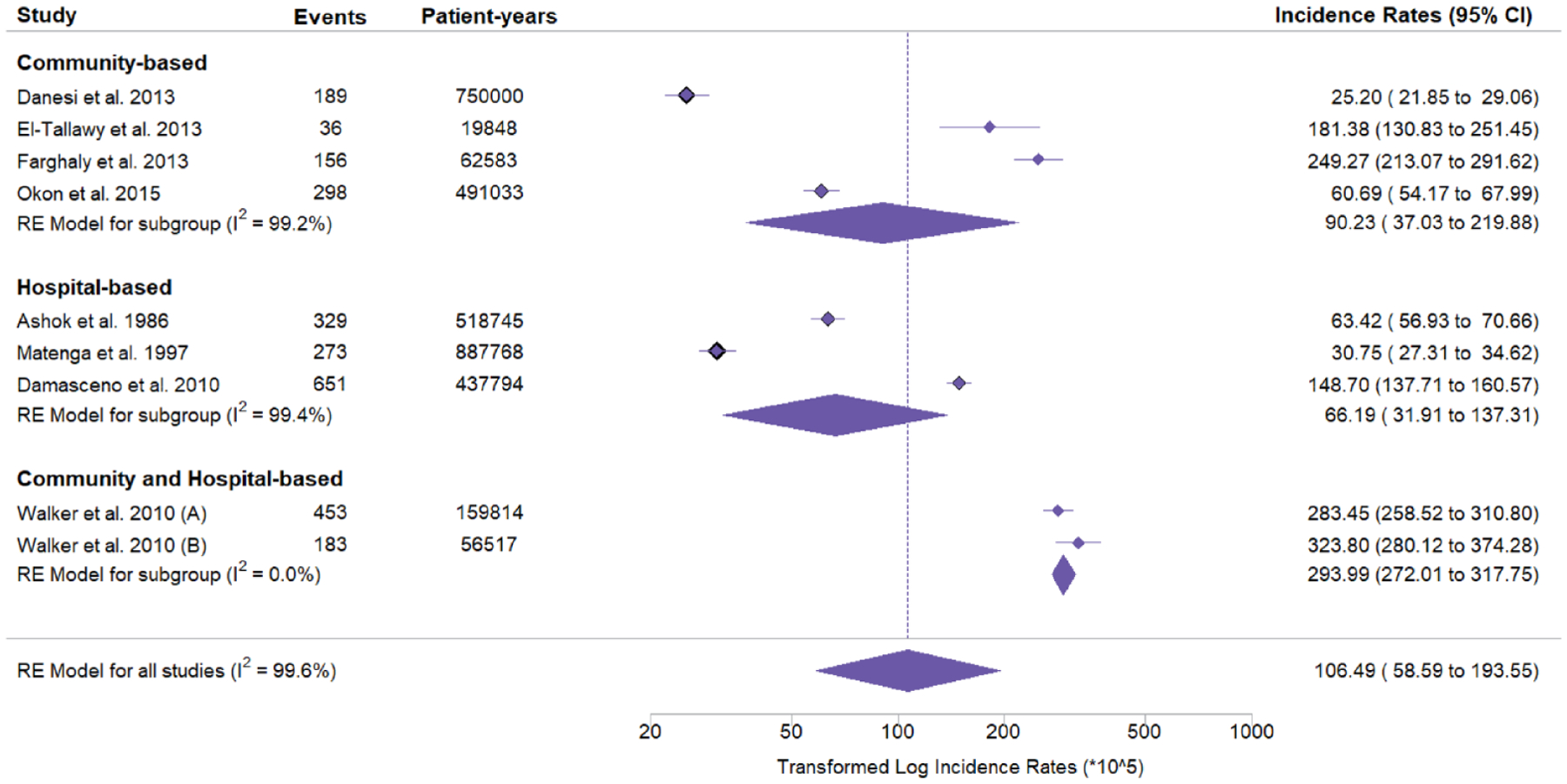
Forest plots on the pooled crude annual incidence rates of stroke per 100,000 persons stratified by study setting (community-based, hospital-based, community-based, and hospital-based).
Figure 5.
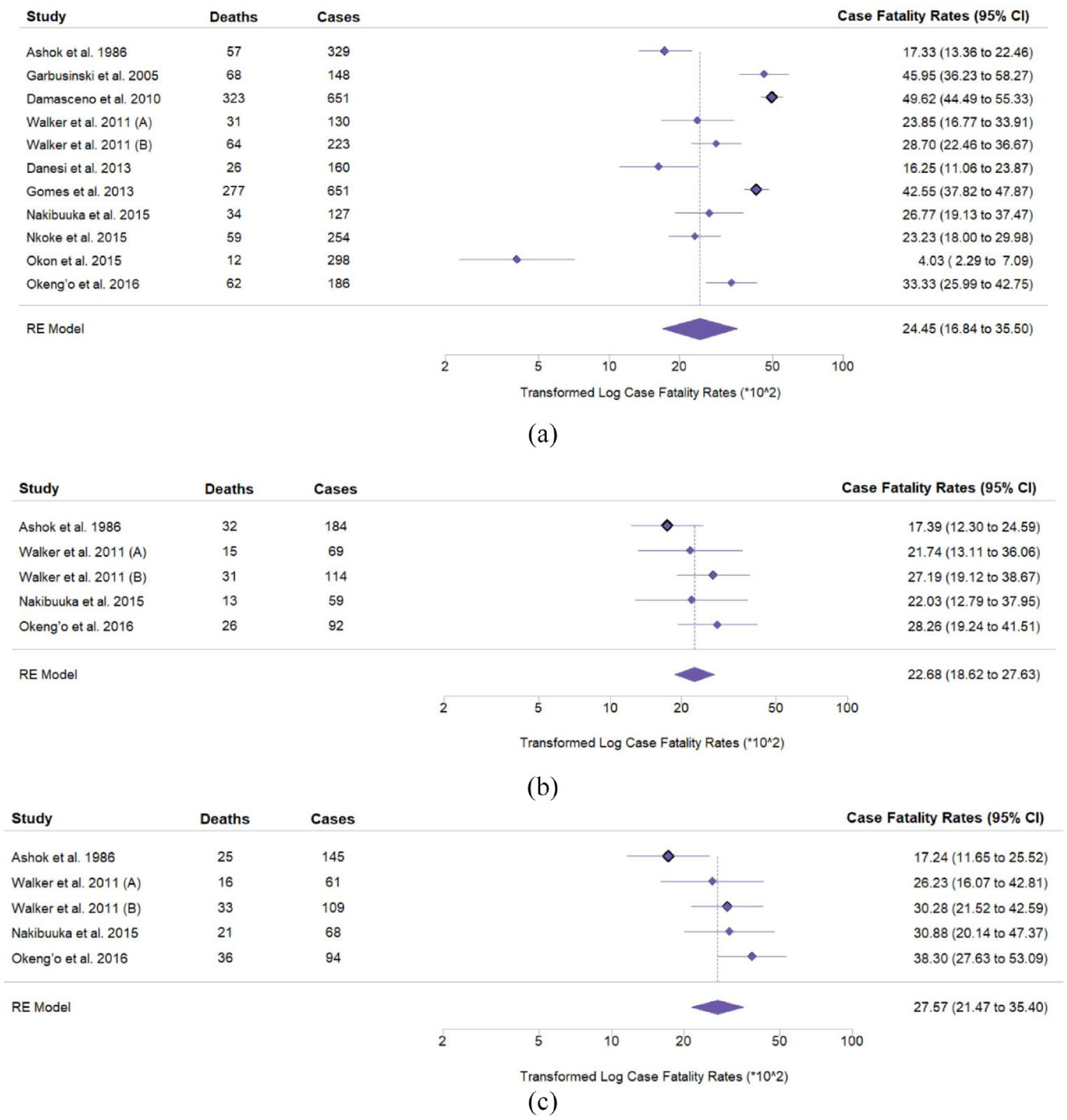
Forest plots on the pooled 30-day case fatality rate of stroke per 100,000 events in the overall population (a), among males (b) and females (c) in Africa.
Methodological assessment of risk of bias
Most studies were rated as having a low risk of bias32,33 (Supplementary Table 1). Most studies defined stroke using the WHO criteria,19–23,28–31 but only two20,28 were primarily guided by the WHO STEPwise approach to Surveillance (WHO STEPS) framework.34
Discussion
This systematic review pooled epidemiological data on stroke incidence rates and CFR from high-quality studies conducted in 13 locations across 10 countries (out of a total of 54 countries) in Africa, leaving most of the world’s second most populous continent short of high-quality data vital for evidence-based decision-making to prevent, track, and manage stroke. The most recent review was conducted about 10 years ago and published in 2013.7 In addition, most reports estimating CFR among Africans20,22,25,28,29,35 primarily used hospital mortality data, limiting the generalizability of the CFR estimates. This limits our ability to track changes in stroke epidemiology and outcome across the countries of Africa and to infer benefit or harm from changes in health policy, investment, or new prevention and treatment strategies. While these findings offer some insights into the epidemiology of stroke in Africa, the heterogeneity of data, from selected populations, within only 10 (of 54) African countries from studies conducted well over 7 years ago limit their usefulness. This review highlights the paucity of available data. However, there are promising prospects for ongoing stroke epidemiological studies in Africa.36
Our meta-analysis revealed that the crude incidence rate of stroke in Africa was ≈106 per 100,000 per year, with a higher point estimate of crude incidence rate among males than females, similar to the Global Burden of Disease (GBD) study for LMICs3 except for China.2,37 This pooled estimate was lower than that reported in a meta-analysis in 20147 and the GBD stroke study3 in sub-Saharan Africa. This observation was comparable to estimates from Asia (116–438 per 100,000 per year)15,38 and the 2022 global stroke fact sheet.39 However, stroke incidence rates appear higher in Europe (219 per 100,000 per year).40 The reasons for these differences, particularly in relation to the modeling-based GBD estimates, are multifaceted41 and might be related to the vast difference in age structure in Europe (with a more aging population) versus Africa.
Furthermore, we found country-level differences in stroke burden in Africa. For example, reports from East and North African countries presented higher estimates compared to those from West Africa. The GBD estimates for East and West Africa were comparable, but reports from North Africa presented higher estimates for stroke burden. Methodological differences in design arising from multifaceted limitations detailed in an earlier report42 might account for these differences. Apart from methodological differences, the differential rates between North and Sub-Saharan Africa are likely attributable to the substructural population and demographic differences between North Africa (which has a higher proportion of older persons—60 years and above) versus sub-Saharan Africa and regional differences in the profile of stroke risk factors.3,5,9 Also, the sparse contribution of African data to the GBD study, poor stroke literacy, diverse socio-cultural barriers and ethnic differences across African countries, and the lack of rigorous community-based and institutional surveillance infrastructure, including neuroimaging for stroke care to promote detection, prognosis, and timely interventions, are additional reasons for these differences.
Pooled CFR revealed that one in every four strokes in Africa is likely to be fatal within the first month. This is similar to a 24% estimate reported in an earlier review.35 Also, our observation is comparable to the 36% global CFR reported in the GBD study3 and India.15 The point estimate of the pooled CFR was comparatively lower among males than females, contrary to observations in other reports.3,15 Several factors account for these differences; the paucity of data and lack of stroke surveillance sites in Africa limit the generalizability of these estimates. Also, timely emergency care (critical to mortality reduction) is grossly deficient in Africa and reduced women’s access to hospital care.43 In addition, there is a significant deficit of well-coordinated and holistic stroke care program(s), including the lack of public awareness, primary prevention, acute management, and post-stroke management, in many African countries.44–46
Some notable studies on stroke epidemiology among Africans47–49 were omitted in this systematic review primarily due to missing details, uncertainties in reporting and other methodological issues previously identified in stroke incidence studies in Africa.42 We intentionally and prospectively limited our review to studies whose design is close to an ideal stroke incidence study in design and rigor.50 While such stringent criteria are necessary for comparing similar studies, they can be problematic in regions like Africa, where limited funding, infrastructure, capacity, and access to diagnostic and time-dependent resources to execute comprehensive stroke epidemiological and surveillance studies effectively make conducting any studies almost impossible. The stroke community must not equate resource constraints with “lesser quality” research. However, this means that understanding is limited regarding the epidemiological dynamics of stroke among Africans.
In the light of the current understanding of stroke presentation in clinical settings among Africans, our findings on stroke epidemiology are likely to be conservative. Future studies should consider recruitment guidelines outlined in the WHO STEPS framework34 to identify stroke cases outside a hospital-based setting, including a range of community-based ascertainment strategies. Also, national and regional population-based stroke registries and surveillance sites (in the context of epidemiological, clinical, and public health studies) across Africa for early treatment, prevention, and management of stroke and other non-communicable diseases (NCDs) are long overdue. The African Stroke Organization promoted these ideals in its current conceptual framework.51
The third goal of the African Union AGENDA 2063 outlined the importance of ensuring healthy livelihoods and well-being for all Africans by 2063.52 Our study aligns with this goal by providing evidence-based data for policy guidelines for Africans to achieve their full potential, free of stroke—a prominent cause of disability and mortality among Africans. Furthermore, our review does offer unique insights into the epidemiology of stroke among Africans. Stroke studies are capital-intensive, and there is a considerable deficit of high-quality studies, even over the 40 years since the first incidence study on stroke in Africa was reported in Ibadan, Nigeria.47 Our study is a clarion call, setting an agenda for a multi-stakeholder approach for health system financing, supportive grants, capacitybuilding, and mobilizing infrastructure for addressing stroke and NCDs among Africans. The current health infrastructure in most African countries delimits local researchers’ efforts to conduct high-quality epidemiological and surveillance studies in a community setting. To that effect, we propose a bolstering of health-system engagement aimed at mobilizing and incentivizing communities to stimulate efforts at reporting stroke and NCDs for early prevention and management. Culturally sensitive interventions including stroke education strategies are also necessary to overcome structural and cultural barriers to stroke surveillance and prevention.
Our findings did not account for the age-standardized incidence rate of stroke. It is important to discern the age group at the highest risk of stroke for prioritizing intervention. Adjusting our estimates for the follow-up period revealed a slight reduction in heterogeneity, yet substantial heterogeneity persisted. The diverse but considerable differences in ethnicity, the year the study was conducted, recruitment strategy, differences in definitions/methods of stroke diagnosis, associated differences in care, age, and follow-up period, to mention a few, likely account for the heterogeneity observed in this systematic review. It is worth noting that this systematic review and meta-analysis aimed not only to provide an overall estimate of stroke incidence and CFR in Africa but also to itemize gaps in data coverage and limitations that could be used to inform future stroke epidemiological studies in Africa. True to our observation, several gaps worth considering when designing future studies were described. Salient details such as a follow-up strategy for most stroke incidence studies were missing, and most studies only reported in-hospital CFR. There is a paucity of epidemiological stroke studies in terms of rigor and quality in Africa. The burden of stroke among Africans is still likely to be predominantly very high. Continent-wide rigorous epidemiological studies and surveillance programs using the WHO STEPS framework are long overdue.
Supplementary Material
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: A.P.O. is a recipient of the Brain Pool Fellowship of the National Research Foundation of Korea (2020H1D3A1A04081265). The National Institutes of Health grants supported the study and investigators; SIREN (U54HG007479), SIBS Genomics (R01NS107900), African Neurobiobank for Precision Stroke Medicine ELSI Project (U01HG010273), SIBS Gen Gen (R01NS107900-02S1), ARISES (R01NS115944-01), H3Africa CVD Supplement (3U24HG00978003S5), CaNVAS (1R01NS114045-01), SSACS (1R13NS11539501A1), and TALENTS (D43TW012030). R.A. and C.W. are supported by a GCRF Networking Grant from the UK Academy of Medical Sciences. R.A. is further supported by the FLAIR fellowship grants FLR/R1/191813 and FCG/R1/201034 funded by the UK Royal Society and the African Academy of Sciences. The funding bodies had no role in the study design, data collection, analysis, interpretation, or writing of this review.
Footnotes
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Supplemental material
Supplemental material for this article is available online.
References
- 1.Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 update: a report from the American Heart Association. Circulation 2018; 137: e67–e492. [DOI] [PubMed] [Google Scholar]
- 2.Kim J, Thayabaranathan T, Donnan GA, et al. Global stroke statistics 2019. Int J Stroke 2020; 15: 819–838. [DOI] [PubMed] [Google Scholar]
- 3.Feigin VL, Stark BA, Johnson CO, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol 2021; 20: 795–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Owolabi MO, Sarfo F, Akinyemi R, et al. Dominant modifiable risk factors for stroke in Ghana and Nigeria (SIREN): a case-control study. Lancet Glob Health 2018; 6: e436–e446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akinyemi RO, Ovbiagele B, Adeniji OA, et al. Stroke in Africa: profile, progress, prospects and priorities. Nat Rev Neurol 2021; 17: 634–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Owolabi MO, Thrift AG, Martins S, et al. The state of stroke services across the globe: report of World Stroke Organization–World Health Organization surveys. Int J Stroke 2021; 16: 889–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adeloye D An estimate of the incidence and prevalence of stroke in Africa: a systematic review and meta-analysis. PLoS ONE 2014; 9: e100724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adeloye D, Ezejimofor M, Auta A, et al. Estimating morbidity due to stroke in Nigeria: a systematic review and meta-analysis. J Neurol Sci 2019; 402: 136–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Owolabi MO, Akarolo-Anthony S, Akinyemi R, et al. The burden of stroke in Africa: a glance at the present and a glimpse into the future. Cardiovasc J Afr 2015; 26: S27–38. doi: 10.5830/CVJA-2015-038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting—Meta-analysis of Observational Studies in Epidemiology (MOOSE) Group. JAMA 2000; 283: 2008–2012. [DOI] [PubMed] [Google Scholar]
- 11.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akinyemi R, Adeniji O, Okekunle A, et al. Epidemiology of stroke in Africa: a systematic review and meta–analysis, of incidence, prevalence, and mortality. PROSPERO 17 February 2022 ed. London: National Institute for Health and Care Research, 2021. [Google Scholar]
- 13.Cheyne J Search strategy for retrieval of references on stroke healthcare in MEDLINE Ovid Edinburgh: College of Medicine and Veterinary Medicine, University of Edinburgh, 2020; Cochrane Stroke Group. [Google Scholar]
- 14.Larney S, Kopinski H, Beckwith CG, et al. Incidence and prevalence of hepatitis C in prisons and other closed settings: results of a systematic review and meta-analysis. Hepatology 2013; 58: 1215–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones SP, Baqai K, Clegg A, et al. Stroke in India: a systematic review of the incidence, prevalence, and case fatality. Int J Stroke 2021; 17: 132–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hupe M EndNote X9. J Electr Res Med Libr 2019; 16: 117–119. [Google Scholar]
- 17.Viechtbauer W Conducting meta-analyses in R with the meta-for package. J Stat Softw 2010; 36: 1–48. [Google Scholar]
- 18.Ashok PP, Radhakrishnan K, Sridharan R and el-Mangoush MA. Incidence and pattern of cerebrovascular diseases in Benghazi, Libya. J Neurol Neurosurg Psychiatry 1986; 49: 519–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matenga J Stroke incidence rates among black residents of Harare-a prospective community-based study. S Afr Med J 1997; 87: 606–609. [PubMed] [Google Scholar]
- 20.Damasceno A, Gomes J, Azevedo A, et al. An epidemiological study of stroke hospitalizations in Maputo, Mozambique. Stroke 2010; 41: 2463–2469. [DOI] [PubMed] [Google Scholar]
- 21.Walker R, Whiting D, Unwin N, et al. Stroke incidence in rural and urban Tanzania: a prospective, community-based study. Lancet Neurol 2010; 9: 786–792. [DOI] [PubMed] [Google Scholar]
- 22.Danesi MA, Okubadejo NU, Ojini FI, et al. Incidence and 30-day case fatality rate of first-ever stroke in urban Nigeria: The prospective community based Epidemiology of Stroke in Lagos (EPISIL) phase II results. J Neurol Sci 2013; 331: 43–47. [DOI] [PubMed] [Google Scholar]
- 23.El-Tallawy HN, Farghaly WM, Shehata GA, et al. Epidemiology of non-fatal cerebrovascular stroke and transient ischemic attacks in Al Quseir, Egypt. Clin Interv Aging 2013; 8: 1547–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farghaly WM, El-Tallawy HN, Shehata GA, et al. Epidemiology of nonfatal stroke and transient ischemic attack in Al-Kharga District, New Valley, Egypt. Neuropsychiatr Dis Treat 2013; 9: 1785–1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Okon M, Adebobola NI, Julius S, et al. Stroke incidence and case fatality rate in an urban population. J Stroke Cerebrovasc Dis 2015; 24: 771–777. [DOI] [PubMed] [Google Scholar]
- 26.Garbusinski JM, van der Sande MA, Bartholome EJ, et al. Stroke presentation and outcome in developing countries. Stroke 2005; 36: 1388–1393. [DOI] [PubMed] [Google Scholar]
- 27.Walker RW, Jusabani A, Aris E, et al. Post-stroke case fatality within an incident population in rural Tanzania. J Neurol Neurosurg Psychiatry 2011; 82: 1001–1005. [DOI] [PubMed] [Google Scholar]
- 28.Gomes J, Damasceno A, Carrilho C, et al. Determinants of early case-fatality among stroke patients in Maputo, Mozambique and impact of in-hospital complications. Int J Stroke 2013; 8: 69–75. [DOI] [PubMed] [Google Scholar]
- 29.Nakibuuka J, Sajatovic M, Nankabirwa J, et al. Early mortality and functional outcome after acute stroke in Uganda: prospective study with 30 day follow-up. Springerplus 2015; 4: 450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nkoke C, Lekoubou A, Balti E, et al. Stroke mortality and its determinants in a resource-limited setting: a prospective cohort study in Yaounde, Cameroon. J Neurol Sci 2015; 358: 113–117. [DOI] [PubMed] [Google Scholar]
- 31.Okeng’o K, Chillo P, Gray WK, Walker RW and Matuja W. Early mortality and associated factors among patients with stroke admitted to a large teaching hospital in Tanzania. J Stroke Cerebrovasc Dis 2017; 26: 871–878. [DOI] [PubMed] [Google Scholar]
- 32.Stang A Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25: 603–605. [DOI] [PubMed] [Google Scholar]
- 33.Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses, http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2021, accessed July 2022).
- 34.World Health Organization. STEPwise approach to NCD risk factor surveillance (STEPS), https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps (2020, accessed 15 July 2022).
- 35.Adoukonou T, Kossi O, Fotso Mefo P, et al. Stroke case fatality in sub-Saharan Africa: systematic review and meta-analysis. Int J Stroke 2021; 16: 902–916. [DOI] [PubMed] [Google Scholar]
- 36.Popoola O, Ovbiagele B, Arulogun O, et al. African rigorous innovative stroke epidemiological surveillance: protocol for a community-based mobile-health study. Neuroepidemiology 2022; 56: 17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang J, Bai L, Shi M, et al. Trends in age of first-ever stroke following increased incidence and life expectancy in a low-income Chinese population. Stroke 2016; 47: 929–935. [DOI] [PubMed] [Google Scholar]
- 38.Turana Y, Tengkawan J, Chia YC, et al. Hypertension and stroke in Asia: a comprehensive review from HOPE Asia. J Clin Hypertens 2021; 23: 513–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Feigin VL, Brainin M, Norrving B, et al. World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke 2022; 17: 18–29. [DOI] [PubMed] [Google Scholar]
- 40.Wafa HA, Wolfe CDA, Emmett E, et al. Burden of stroke in Europe. Stroke 2020; 51: 2418–2427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lanas F and Seron P. Facing the stroke burden worldwide. Lancet Glob Health 2021; 9: e235–e236. [DOI] [PubMed] [Google Scholar]
- 42.Owolabi M, Olowoyo P, Popoola F, et al. The epidemiology of stroke in Africa: a systematic review of existing methods and new approaches. J Clin Hypertens 2018; 20: 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ouma PO, Maina J, Thuranira PN, et al. Access to emergency hospital care provided by the public sector in sub-Saharan Africa in 2015: a geocoded inventory and spatial analysis. Lancet Glob Health 2018; 6: e342–e350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roushdy T, Aref H, Kesraoui S, et al. Stroke services in Africa: What is there and what is needed. Int J Stroke 2022; 17: 972–982. [DOI] [PubMed] [Google Scholar]
- 45.Owolabi MO, Thrift AG, Mahal A, et al. Primary stroke prevention worldwide: translating evidence into action. Lancet Public Health 2022; 7: e74–e85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Okekunle AP, Asowata O, Akpa OM, et al. Dietary patterns associated with stroke among West Africans: a case–control study. Int J Stroke. Epub ahead of print 12 May 2022. DOI: 10.1177/17474930221094933. [DOI] [PubMed] [Google Scholar]
- 47.Osuntokun BO, Bademosi O, Akinkugbe OO, Oyediran AB and Carlisle R. Incidence of stroke in an African City: results from the Stroke Registry at Ibadan, Nigeria, 1973–1975. Stroke 1979; 10: 205–207. [DOI] [PubMed] [Google Scholar]
- 48.Rosman KD. The epidemiology of stroke in an urban black population. Stroke 1986; 17: 667–669. [DOI] [PubMed] [Google Scholar]
- 49.Tekle-Haimanot R, Abebe M, Gebre-Mariam A, et al. Community-based study of neurological disorders in rural central Ethiopia. Neuroepidemiology 1990; 9: 263–277. [DOI] [PubMed] [Google Scholar]
- 50.Investigators WMPP. The World Health Organization MONICA project (monitoring trends and determinants in cardiovascular disease): a major international collaboration. J Clin Epidemiol 1988; 41: 105–114. [DOI] [PubMed] [Google Scholar]
- 51.Akinyemi R, Sarfo F, Abd-Allah F, et al. Conceptual framework for establishing the African Stroke Organization. Int J Stroke 2021; 16: 93–99. doi: 10.1177/1747493019897871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.African Union Commission. Agenda 2063: the AFRICA we want. Addis Ababa, Ethiopia: African Union Commission, 2015. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


