Abstract
Objective
Evaluate the effectiveness of systematically delivered evidence-based home safety promotion for improving child home safety practices.
Design
Controlled before-and-after study.
Setting
Nine electoral wards in Nottingham, UK.
Participants
361 families with children aged 2–7 months at recruitment living in four intervention wards with high health, education and social need; and 401 in five matched control wards.
Intervention
Evidence-based home safety promotion delivered by health visiting teams, family mentors and children’s centres including 24 monthly safety messages; home safety activity sessions; quarterly ‘safety weeks’; home safety checklists.
Outcomes
Primary: composite measure comprising having a working smoke alarm, storing poisons out of reach and having a stairgate. Secondary: other home safety practices; medically attended injuries. Parents completed questionnaires at 12 and 24 months after recruitment plus optional three monthly injury questionnaires.
Results
At 24 months there was no significant difference between groups in the primary outcome (55.8% vs 48.8%; OR 1.58, 95% CI 0.98 to 2.55) or medically attended injury rates (incidence rate ratio 0.89, 95% CI 0.51 to 1.56), but intervention families were more likely to store poisons safely (OR 1.81, 95% CI 1.06 to 3.07), have a fire escape plan (OR 1.81, 95% CI 1.06 to 3.08), use a fireguard or have no fire (OR 3.17, 95% CI 1.63 to 6.16) and perform more safety practices (β 0.46, 95% CI 0.13 to 0.79).
Conclusions
Systematic evidence-based home safety promotion in areas with substantial need increases adoption of some safety practices. Funders should consider commissioning evidence-based multicomponent child home safety interventions.
Trial registration number
ISRCTN31210493.
Keywords: home, child, education, public health
WHAT IS ALREADY KNOWN ON THIS TOPIC
Injuries that occur in the home contribute substantially to morbidity and mortality experienced by preschool children; there are steep social gradients in childhood home injuries, with children from disadvantaged families being at greater risk.
Multicomponent interventions have been shown to improve child home safety but are not consistently implemented.
WHAT THIS STUDY ADDS
A multicomponent preschool child home safety intervention led to significantly more families storing poisons safely, having fire escape plans and adopting more home safety practices.
Multiple imputation, but not complete case analysis, showed the intervention to significantly increase the primary outcome (working smoke alarm; safe poison storage; having a stairgate) at 24 months’ follow-up.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Funders should consider commissioning evidence-based multicomponent preschool child home safety interventions; large-scale evaluations are needed to investigate their impact on injury occurrence.
Introduction
Unintentional injuries are responsible for substantial morbidity and mortality in children aged 0–5 years, resulting in an annual average of 370 000 emergency department attendances, 40 000 hospital admissions and 55 deaths in England in 2012–2016.1 Childhood injuries disproportionately affect disadvantaged families or those living in deprived areas.2–6 Other risk factors include male gender, living in a single-parent household, having a younger mother and a larger number of siblings.2–5 Most injuries to preschool children occur in the home and are preventable1; the most common avoidable causes for medical attendance are falls, accidental or suspected accidental poisonings and scalds.1 Such injuries can lead to severe and long-lasting physical and psychological effects7 and may adversely impact families.8
Child injury risk can be reduced through home modifications and undertaking a range of safety practices; providing education and supplying and fitting some safety equipment improves home safety9 and can reduce injury-related hospital admissions.10 The practices associated with the best evidence for child injury risk reduction (and whose uptake is improved through educational intervention) are: having a fitted and working smoke alarm; storing household poisons (cleaning products and medications) out of children’s reach; and having a stairgate (also known as a safety gate) on stairs.4 9 11–14 The impact of other safety practices on reducing injuries is less clear, although evidence indicates that educational interventions can improve uptake of a range of safety practices.9
In England and Wales the National Institute for Health and Care Excellence (NICE) recommends that health and social care services provide safety advice and consider assessing home safety or providing safety equipment to families whose children are at increased risk of injury.15 However, despite evidence that such interventions improve safety practices,9 they are not implemented consistently or systematically.16
This study aimed to assess the effectiveness of systematically delivered evidence-based home safety promotion with the aim of improving child home safety practices for families with high levels of health, educational and social need, living in urban areas.17
Methods
Design
A non-randomised controlled before-and-after design was used for intervention evaluation. The intervention was delivered in four electoral areas (‘wards’) in Nottingham City (which consists of 20 wards), UK. These wards had been chosen, prior to this study being designed, by the Small Steps Big Changes (SSBC) programme, which works towards giving all children the best possible start in life and is funded by The National Lottery Community Fund ‘A Better Start’ programme.18 The wards were chosen due to having high levels of health, education and social need; and large numbers of children younger than 5 years. Comparisons were made between families living in these wards and those living in five matched control wards who received usual care. Control and intervention wards were matched first by rate of emergency department injury presentation by 0–5 year-olds,19 second by income deprivation affecting children and, third, by minimising health visitor service case load overlap. Five matched control wards were selected, rather than four, due to intervention wards being larger than control wards; hence, one of the intervention wards was matched to two control wards.
Participants
Participants were parents or carers of children aged 2–7 months at recruitment. Eligible participants were identified using a community healthcare database and were sent postal participation invitations. The study was also promoted verbally by primary care workers and through posters and social media. Multiple participant retention strategies were used (online supplemental material S1).
ip-2022-044745supp001.pdf (111.4KB, pdf)
There were three participant cohorts. Cohort 1 was recruited in September 2017, cohort 2 in March 2018 and cohort 3 in September 2018.
Intervention
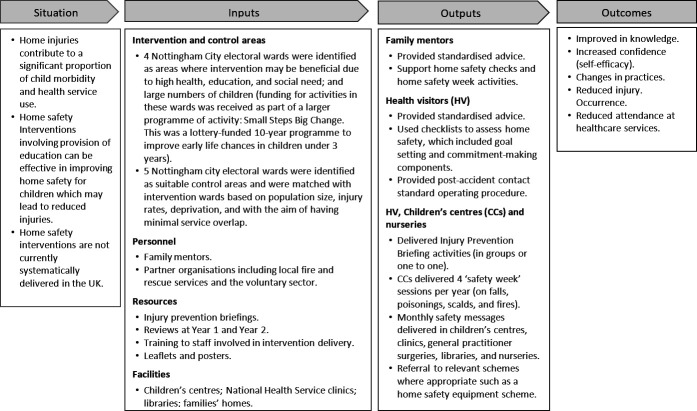
The intervention, called Stay One Step Ahead (SOSA), was delivered as part of the SSBC programme. SOSA was coproduced by parents, researchers and practitioners and was based on the NICE principles of behaviour change for individual-level interventions.20 SOSA had multiple evidence-based9 21 components: 24 unique monthly safety messages distributed using flyers, quizzes and posters; home safety activities for families; home safety checklists for health visiting teams for 9–12 and 24–30 months’ child health reviews; eight activities included in a structured manual for use by family mentors (community members with experience of parenting), completed with parents during home visits from birth to 3 years; and educational ‘safety weeks’ for families delivered four times per year by children’s centre staff. These ‘safety weeks’ included information on how best to reduce risk from four common causes of childhood injuries: poisons, scalds, fires and falls.1 Health visiting teams, children’s centre staff and family mentors received training on delivering the intervention. Families living in control areas received usual care, which involved child health reviews at 9–12 months and 24–30 months from health visiting teams (but without the SOSA home safety checklists being used), but no family mentor service, monthly safety messages or ‘safety weeks’. See figure 1 for logic model.
Figure 1.
Logic model for the Stay One Step Ahead intervention.
Questionnaires
All data were from parent-reported questionnaires (see online supplemental material S1 for strategies to improve completion rates and online supplemental material S2 for how questionnaire items related to outcomes). Home safety outcome measures were reported at recruitment (baseline), and 12 and 24-month follow-up. Additionally, families could opt to report injury data at three monthly intervals. Questionnaires were in English, and interpretation services were provided for phone completion where required. Families were thanked for questionnaire completion with gift vouchers.
Outcomes
The primary outcome was a binary composite measure reflecting whether families performed all three practices associated with the best evidence for child injury risk reduction: having a working smoke alarm, storing poisons out of reach (at adult eye level or above or locked away) and either having a stairgate or no stairs at home. It was measured using questionnaires at baseline and at 12 and 24-month follow-up. Secondary outcomes were parent-reported medically attended child injuries and health services to which the child presented, and adoption of the following additional safety practices: not leaving their child alone in the bath in the past week, using a fireguard (or not having a home fire), keeping blind cords out of the reach of children, having safety catches on any windows, having a fire escape plan and always accompanying their child outside. We included families without stairs in our primary outcome analysis. As children in these families were not exposed to the risk of stairway falls, we treated them as families who had a safety gate on stairs. Excluding these families from the analysis would have reduced study power as the composite primary outcome measure required data on all three safety practices. We treated those with no fires in the same way that we treated those with no stairs to be consistent across analyses.
Post hoc analysis investigated the number of safety practices performed. For all outcomes, at each follow-up time point, we compared differences between families living in intervention and control areas, adjusting for the baseline value of the outcome.
Statistical analysis
All non-injury outcomes were binary and are described as proportions; medically attended injuries and associated health service presentations are presented as rates per 100 participant-years. All primary and secondary outcomes were analysed using multilevel regression with family observations at level 1, and wards in which the families lived at level 2 to control for clustering at ward level and family-level and area-level covariates.22
Logistic regression was used to assess safety practice adoption, including the primary outcome, at 12 and 24-month follow-up comparing families in the intervention wards with control families. Poisson regression or negative binomial regression (if likelihood ratio tests indicated overdispersion) was used to assess injury and associated health service presentation rates over 0–12 month and 13–24 months’ follow-up. Linear regression was used for post hoc analysis of total number of adopted safety practices.
All models included a fixed effect term indicating the relevant pair or trio of matched wards to account for homogeneity within matched areas. Where the relevant outcome was measured at baseline (the only secondary safety practice outcome measured at baseline was supervised bathing due to the age of children at recruitment) models also controlled for this; for the Poisson models, this was the event rate in the 3 months prior to baseline. All models were also adjusted for variables which differed significantly between the groups at baseline (assessed using Wilcoxon rank-sum or χ2 tests as appropriate), which significantly predicted the outcome, or which altered the regression coefficient for the intervention by at least 10% at 12 or 24-month follow-up. Where models failed to converge, the matched ward term was removed.
In additional analyses, multiple imputation using chained equations was conducted to impute values for missing data at 12 and 24-month follow-up in all participants who completed the baseline questionnaire. Fifty data sets were generated and results for analysis of all primary and secondary outcomes were pooled. All analyses were conducted using STATA V.17 (Stata Statistical Software, Stata, Texas, USA).
Sample size
It was assumed, based on previous research,23 that 54% of control ward homes would have the primary outcome. To achieve 80% power with a two-tailed significance level of 5%, a sample of 237 families in the intervention group and 237 in the control group would be required to detect a 13% difference between groups for the primary outcome. The sample size was not inflated to account for clustering as the intraclass correlation coefficient for electoral ward-level smoke alarm ownership was previously found to be <0.00001,24 hence the design effect is effectively 1. Population estimates indicated there to be 1047 children aged under 1 year in intervention wards and 909 in control wards. Attrition rates of up to 60% were anticipated25; the recruitment target, therefore, was 400 families from intervention and 400 from control wards.
Patient and public involvement
The SOSA intervention was coproduced with parents from Nottingham City. These ‘Parent Champions’ were parents of young children, residents of the intervention wards and part of the SSBC programme. They contributed to developing parent recruitment and retention strategies, designing data collection tools, study oversight and dissemination.
Results
Baseline data were collected from 361 (25% of 1447 invited) intervention and 401 control families (29% of 1394 invited); 237 (65.7%) intervention and 298 (74.3%) control families completed the 12-month questionnaire, and 233 (64.5%) intervention and 298 (74.3%) control families completed the 24-month questionnaire (see figure 2). Table 1 displays both groups’ baseline characteristics. Intervention families were significantly larger, had younger mothers and were more likely to be single-adult households and live in areas of higher material deprivation according to the Index of Multiple Deprivation (IMD).26 Families who did not respond to the 12-month or 24-month questionnaire, in comparison to those who responded, were significantly larger, included younger mothers and were more likely to be single-adult households, live in areas of higher IMD and live in an intervention rather than control ward (online supplemental material S3).
Figure 2.
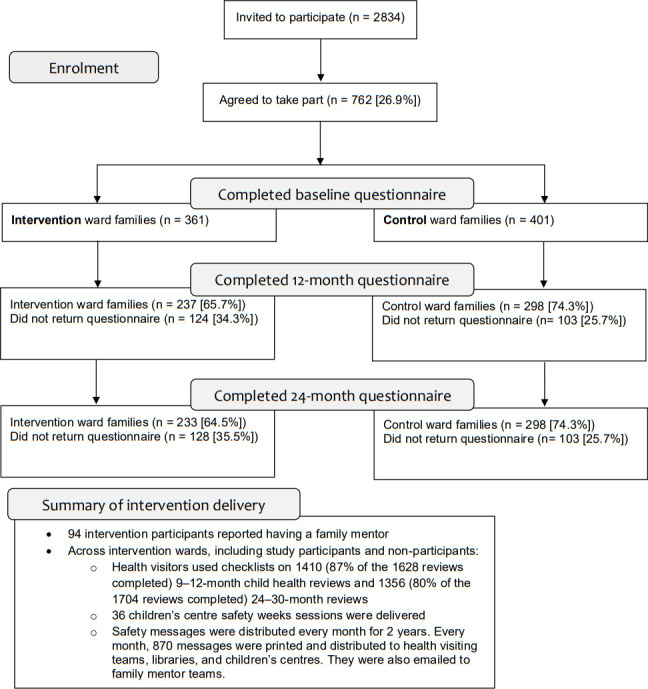
Participant flow diagram.
Table 1.
Baseline characteristics for families in intervention and control groups
| Variable | Control group (n=401) | Intervention group (n=361) | P value | ||
| Median* | IQR | Median* | IQR | ||
| Child age (months) | 4.6 [4] | 3.1–6.0 | 4.6 [7] | 3.1–6.2 | 0.90 |
| Child gender (% male) | 191 (48.2%) [5] | 181 (50.4%) [2] | 0.55 | ||
| Number of children (under 16) living in household | 2 [2] | 1–2 | 2 [3] | 1–3 | 0.047 |
| Maternal age at birth of first child | 27 [34] | 21–31 | 25 [19] | 20–29 | 0.001 |
| Proportion of families with one adult per household | 61 (15.3%) [3] | 96 (26.7%) [1] | 0.001 | ||
| Index of Multiple Deprivation (IMD) 2019 | 34.3 [6] | 24.7–40.5 | 52.69 [9] | 45.9–57.3 | 0.001 |
| Distance to the nearest emergency department (km)† | 4.86 [2] | 3.74–5.78 | 4.24 [6] | 3.74–6.10 | 0.074 |
[ ] denotes missing values.
*Unless otherwise specified.
†Direct distances (not road distances) from participants’ home postcodes to the nearest emergency department were calculated using https://www.doogal.co.uk/DrivingDistances.php
Primary outcome: having a working smoke alarm, storing poisons out of reach and having a stairgate
There was no significant effect of the intervention on the primary outcome at 12 months (OR 0.98, 95% CI 0.61 to 1.56, p=0.92) or 24 months (OR 1.58, 95% CI 0.98 to 2.55, p=0.06). However, a significantly greater proportion of intervention than control families stored poisons out of reach at 24 months (OR 1.81, 95% CI 1.06 to 3.07, p=0.029).
Additional home safety practices
Families in intervention wards were significantly more likely to have a fire escape plan than families living in control wards at both 12 months (OR 1.78, 95% CI 1.08 to 2.95, p=0.025) and 24 months (OR 1.81, 95% CI 1.06 to 3.08, p=0.030). Families in intervention wards were also more likely to use a fireguard or not have a fire at both 12 months (OR 3.04, 95% CI 1.57 to 5.89, p=0.001) and 24 months (OR 3.17, 95% CI 1.63 to 6.16, p=0.001). There was no significant difference between intervention and control groups for other individual safety practices, but for most practices, more intervention families reported the safety practice than control families (see table 2).
Table 2.
Primary and secondary outcomes at baseline and 12 and 24 months for intervention and control groups
| Measure | Measurement time point | Control group Baseline n=401 12 months n=298 24 months n=298 |
Intervention group Baseline n=361 12 months n=237 24 months n=233 |
Primary analysis | Multiple imputation analysis (control group n=401; intervention group n=361) | ||
| Adjusted* OR (95% CI)† | P value | Adjusted* OR (95% CI)† | P value | ||||
| Primary outcome measure | |||||||
| Families with primary outcome measure (having a working smoke alarm, storing poisons out of reach and having a stairgate or no stairs). |
Baseline | 117 (29.3%) [2] | 112 (31.1%) [1] | 1.00 (0.67 to 1.51) | 0.98 | 0.96 (0.65 to 1.43) | 0.85 |
| 12 months | 170 (57.1%) [0] | 132 (56.4%) [3] | 0.98 (0.61 to 1.56) | 0.92 | 1.25 (0.79 to 1.96) | 0.34 | |
| 24 months | 144 (48.8%) [3] | 130 (55.8%) [0] | 1.58 (0.98 to 2.55) | 0.060 | 1.75 (1.12 to 2.73) | 0.014 | |
| Working smoke alarm | Baseline | 375 (94.0%) [2] | 329 (91.4%) [1] | 0.85 (0.38 to 1.88) | 0.69 | 0.83 (0.40 to 1.74) | 0.63 |
| 12 months | 279 (93.6%) [0] | 215 (91.9%) [3] | 0.67 (0.28 to 1.57) | 0.35 | 0.88 (0.36 to 2.17) | 0.79 | |
| 24 months | 283 (95.9%) [3] | 218 (93.6%) [0] | 0.83 (0.28 to 2.46) | 0.73 | 1.20 (0.45 to 3.18) | 0.72 | |
| Storing poisons out of reach | Baseline | 203 (51.0%) [3] | 201 (56.0%) [2] | 0.89 (0.60 to 1.30) | 0.53‡ | 0.86 (0.60 to 1.25) | 0.44 |
| 12 months | 190 (63.8%) [0] | 159 (68.0%) [3] | 1.13 (0.69 to 1.86) | 0.63 | 1.45 (0.88 to 2.41) | 0.15 | |
| 24 months | 198 (67.1%) [3] | 170 (73.3%) [1] | 1.81 (1.06 to 3.07) | 0.029 | 1.82 (1.13 to 2.93) | 0.015 | |
| Has a stairgate or no stairs | Baseline | 210 (52.9%) [4] | 198 (55.0%) [1] | 1.37 (0.93 to 2.01) | 0.11 | 1.29 (0.90 to 1.87) | 0.17 |
| 12 months | 262 (87.9%) [0] | 202 (86.3%) [3] | 0.84 (0.40 to 1.76) | 0.65 | 1.13 (0.58 to 2.20) | 0.73 | |
| 24 months | 222 (75.3%) [3] | 177 (77.3%) [4] | 1.17 (0.66 to 2.11) | 0.59 | 1.38 (0.78 to 2.42) | 0.26 | |
| Secondary outcome measures | |||||||
| Supervised bathing | Baseline | 387 (98.7%) [9] | 351 (98.0%) [3] | 0.33 (0.06 to 2.01) | 0.23 | 0.63 (0.15 to 2.70) | 0.53 |
| 12 months | 278 (93.6%) [1] | 223 (94.9%) [2] | 1.18 (0.44 to 3.13) | 0.75 | 0.94 (0.39 to 2.34) | 0.91 | |
| 24 months | 266 (91.1%) [6] | 217 (96.0%) [7] | 1.85 (0.72 to 4.79) | 0.20 | 1.51 (0.66 to 3.47) | 0.33 | |
| Using a fireguard or not having a home fire | 12 months | 233 (78.5%) [1] | 203 (87.1%) [4] | 3.04 (1.57 to 5.89) | 0.001 | 2.98 (1.61 to 5.53) | 0.001 |
| 24 months | 235 (80.2%) [5] | 192 (85.3%) [8] | 3.17 (1.63 to 6.16) | 0.001 | 3.06 (1.60 to 5.85) | 0.001 | |
| Blind cords out of reach | 12 months | 244 (82.2%) [1] | 202 (86.3%) [3] | 1.03 (0.55 to 1.92) | 0.93 | 1.06 (0.59 to 1.93) | 0.84 |
| 24 months | 251 (86.0%) [6] | 201 (89.0%) [7] | 0.72 (0.36 to 1.44) | 0.35 | 0.76 (0.40 to 1.43) | 0.40 | |
| Safety catches on any windows | 12 months | 159 (53.5%) [1] | 159 (68.0%) [3] | 1.29 (0.80 to 2.09) | 0.30 | 1.33 (0.84 to 2.13) | 0.21 |
| 24 months | 174 (59.2%) [4] | 148 (65.5%) [7] | 0.78 (0.48 to 1.27) | 0.32 | 0.76 (0.47 to 1.22) | 0.25 | |
| Fire escape plan | 12 months | 184 (62.0%) [1] | 181 (76.7%) [1] | 1.78 (1.08 to 2.95) | 0.025 | 1.81 (1.10 to 2.94) | 0.020 |
| 24 months | 196 (67.1%) [6] | 174 (77.0%) [7] | 1.81 (1.06 to 3.08) | 0.030 | 1.72 (1.06 to 2.78) | 0.029 | |
| Outdoor supervision | 24 months | 203 (73.0%) [20] | 169 (79.9%) [21] | 1.30 (0.73 to 2.31) | 0.37 | 1.28 (0.76 to 2.14) | 0.35 |
| Post hoc analysis: mean (± standard deviation) total number of home safety practices adopted and adjusted difference between means | |||||||
| Total number of home safety practices adopted | Baseline (max 4) | 2.97±0.79 [51] | 3.01±0.83 [32] | 0.01 (−0.14 to 0.15) | 0.92 | 0.00 (-0.20 to 0.19) | 0.97‡ |
| 12 months (max 8) | 6.15±1.37 [36] | 6.62±1.21 [24] | 0.34 (0.06 to 0.63) | 0.019 | 0.39 (0.13 to 0.65) | 0.004 | |
| 24 months (max 9) | 6.92±1.44 [57] | 7.37±1.39 [34] | 0.46 (0.13 to 0.79) | 0.006 | 0.42 (0.12 to 0.71) | 0.005 | |
[ ] denotes missing values.
*The model controlled for: number of siblings under the age of 16 years; maternal age at the time of birth of the first child; the Index of Multiple Deprivation (IMD) of the home postcode, whether the family lived in a single-adult household; the corresponding baseline variable (where collected) for each outcome; and the matched wards factor.
†The control group was the reference group.
‡Model did not converge. ‘Matched wards’ factor removed, and the model converged.
Total number of safety practices
The total number of home safety practices, including both those comprising the primary outcome and the additional practices (maximum eight at 12-months and nine at 24 months), was significantly higher for intervention than control families at both 12 months (β 0.34, 95% 0.06 to 0.63, p=0.019) and 24 months (β 0.46, 95% CI 0.13 to 0.79, p=0.006) (see table 3).
Table 3.
Parent-reported medically attended injury and injury-associated health service presentation rates (per 100 person-years) for intervention and control groups
| Measure | Measurement time point | Control group rate per 100 person-years (n events) Baseline n=393 12 months n=349 24 months n=312 |
Intervention group rate per 100 person-years (n events) Baseline n=354 12 months n=286 24 months n=260 |
Primary analysis | Multiple imputation analysis | ||
| Adjusted* incidence rate ratio (95% CI) | P value | Adjusted* incidence rate ratio (95% CI) | P value | ||||
| Medically attended injury | Baseline† | 10.2 (10) | 13.6 (12) | 1.31 (0.26 to 6.62) | 0.74‡ | 1.14 (0.33 to 3.87) | 0.84 |
| Year 1 | 23.7 (66) | 27.3 (57) | 0.89 (0.51 to 1.56) | 0.68 | 1.05 (0.64 to 1.70) | 0.86‡ | |
| Year 2 | 32.0 (84) | 31.5 (59) | 0.98 (0.57 to 1.70) | 0.95 | Not applicable | ** | |
| Family doctor presentations due to injury | Baseline† | 3.1 (3) | 9.0 (8) | 4.85 (0.46 to 50.79) | 0.19 | 7.70 (0.88 to 676.70) | 0.37 |
| Year 1 | 5.0 (14) | 9.1 (19) | 1.13 (0.36 to 3.54) | 0.83 | 1.22 (0.45 to 3.30) | 0.70‡ | |
| Year 2 | 5.7 (15) | 5.3 (10) | 1.01 (0.31 to 3.25) | 0.99 | 1.13 (0.45 to 2.85) | 0.80 | |
| Urgent care or walk-in centre presentations due to injury | Baseline† | 0.0 (0) | 1.1 (1) | Not applicable§ | 0.99‡¶ | Not applicable§ | ** |
| Year 1 | 2.5 (7) | 3.8 (8) | 1.69 (0.23 to 12.41) | 0.61 | Not applicable | ** | |
| Year 2 | 4.6 (12) | 3.2 (6) | 0.60 (0.19 to 1.96) | 0.40¶ | 0.56 (0.20 to 1.55) | 0.26¶ | |
| Emergency department presentations due to injury | Baseline† | 9.2 (9) | 14.7 (13) | 0.63 (0.08 to 5.32) | 0.67 | 0.62 (0.15 to 2.56) | 0.51 |
| Year 1 | 15.1 (42) | 14.4 (30) | 0.97 (0.52 to 1.81) | 0.94¶ | Not applicable | ** | |
| Year 2 | 22.5 (59) | 23.5 (44) | 0.97 (0.50 to 1.91) | 0.94 | 0.92 (0.54 to 1.57) | 0.77‡ | |
| Hospital admissions due to injury | Baseline† | 1.0 (1) | 2.3 (2) | 0.55 (0.00 to 509.0) | 0.87 | Not applicable | ** |
| Year 1 | 1.4 (4) | 0.5 (1) | Not applicable§ | ** | Not applicable | ** | |
| Year 2 | 2.3 (6) | 1.1 (2) | 0.01 (0.0001 to 1.06) | 0.053¶ | 0.09 (0.01 to 1.43) | 0.088¶ | |
Completion of each three monthly follow-up injury questionnaire represented 0.25 years of data. For year 1, for example, any participant could contribute 0.25, 0.50, 0.75 or 1.0 years of injury follow-up data.
*The adjusted model controlled for: number of siblings under the age of 16 years; maternal age at the time of birth of the first child; the Index of Multiple Deprivation (IMD) of the home postcode, whether the family lived in a single-adult household; the corresponding baseline variable (where collected); and the matched wards factor.
†Baseline rates were based on the number of events that were reported to have occurred in the 3 months prior to the intervention.
‡The model did not initially converge so the ‘Matched wards’ factor was removed to enable convergence.
§The ratio of events is 0:1 and the upper 95% CI cannot be defined.
¶A Poisson model was used.
**Model did not converge following removal of matched wards.
Medically attended injury occurrence
There was no significant difference in medically attended injury rates between the two groups in year 1 (incidence rate ratio (IRR) 0.89, 95% CI 0.51 to 1.56, p=0.68) or year 2 (IRR 0.98, 95% CI 0.57 to 1.70, p=0.95), and there was no difference in associated presentations to health services (table 3).
Multiple imputation analysis
The multiple imputation analysis (MIA) found intervention families were significantly more likely to report the primary outcome than control families at 24 months (OR 1.75, 95% CI 1.12 to 2.73, p=0.014). All other non-significant complete case analysis findings remained non-significant, and all significant findings in the complete case analysis remained significant, in the MIA.
Discussion
We found that significantly more intervention families stored household poisons out of reach at 24 months, had fire escape plans and either used fireguards or did not have fires at 12 and 24 months; but there was no significant difference in the primary home safety outcome (had a working smoke alarm, stored poisons out of reach and had either a stairgate or no stairs at home), other safety practices or the rate of medically attended injuries. Post hoc analysis found that intervention families undertook more safety practices than control families at 12 and 24 months. MIA found more intervention families had the primary outcome at 24 months.
The study recruitment rate was reasonable (27% of those invited) and retention rates were higher than the 60%25 predicted (figure 1), despite some data collection occurring during the SARS-CoV-2 pandemic. Study retention may have been facilitated by Parent Champion involvement in the design of the intervention27 and Parent Champion-informed multiple retention strategies. A further study strength is the intervention being evidence based9 21 and adhering to recommended behaviour change principles.20
Outcomes were parent reported and therefore may have been affected by performance bias, although we have no evidence that this differed between groups. We specifically asked families if they had a plan for how to get out of the house if there is a fire, but it is possible that some families mistook knowledge of how to escape for having an escape plan. However, there is no reason to believe that this would have occurred differentially in the intervention and control groups. Additionally, attrition was greater in the intervention than control group (figure 1), which was unsurprising given that intervention group families were more socioeconomically disadvantaged.28 We found some differences in baseline characteristics between responders and non-responders to follow-up questionnaires. However, our MIA accounted for missing data, finding similar results to the complete case analysis, but also finding a significant effect on the primary outcome favouring intervention families. The SARS-CoV-2 pandemic affected intervention delivery as health visiting teams and family mentors stopped most home visits (including most routine child health reviews) and children’s centres stopped delivering safety weeks from March 2020. As services adapted to the requirements of the pandemic, some child health reviews were conducted remotely, but delivery of the home safety checklists remotely is likely to have differed from those undertaken during home visits where the home environment could also be observed. Additionally, participants became more likely to submit data using email than post during national ‘lockdown’ periods, which may have affected response rates.29
Our findings of intervention group families being more likely to store poisons safely, have a fire escape plan and conduct more safety practices are consistent with previous evaluations of educational interventions.9 30–33 The prevalence of working smoke alarms and stairgates was not affected by the intervention. Studies describing interventions successfully promoting these practices have involved provision of, or improving access to, safety equipment alongside educational approaches.34–38 When the current study was planned, a safety equipment scheme was operating in the study wards, and it was anticipated that the intervention would increase referrals to the scheme. However, funding for the scheme ceased prior to the study starting, terminating this key source of free safety equipment.
Baseline smoke alarm prevalence in our study was higher than expected at 92%. When we designed the study in 2014, 88% of households in England had a working smoke alarm (https://www.gov.uk/government/statistics/fire-prevention-and-protection-statistics-england-april-2020-to-march-2021/fire-prevention-and-protection-statistics-england-april-2020-to-march-2021). Previous research had found large inequalities in smoke alarm ownership with prevalence being at least 9% lower for families receiving means-tested benefits, living in rented accommodation or single-parent households, with younger mothers or from ethnic minority groups.39 Given the area-level deprivation of study intervention wards, and lack of contemporaneous smoke alarm ownership data for the study population, it was not unreasonable at the time of study design to expect to achieve a demonstrable increase in smoke alarm ownership. However, legislative changes enacted after design of the study (https://www.legislation.gov.uk/uksi/2015/1693/) mandating smoke alarm installation in rented accommodation are likely to have contributed to the higher-than-expected smoke alarm prevalence.
It is always difficult to disentangle the key components in multicomponent interventions, and this is true of the SOSA intervention. It is possible that some components were more effective than others. However, it is also possible that it is the package of components, rather than individual components, that produced the observed effect. Indeed, there is evidence that home safety interventions with more components can be more effective than those with fewer.38
It is unsurprising that our complete case analysis found no significant effect of the intervention on injury rates as it was not powered to do so. This is consistent with findings of previous systematic reviews,9 40 which highlight the challenge of assessing intervention impact on injury rates because of the large sample sizes required.
Conclusion
Systematic evidence-based home safety promotion for families with high levels of need improves some safety practices and total number of safety practices. Funders should consider commissioning evidence-based multicomponent child home safety interventions. Funders should also consider commissioning safety equipment schemes alongside multicomponent interventions because the most effective home safety interventions are those that provide access to free or low-cost safety equipment in addition to educational approaches. This is especially relevant for disadvantaged families who may struggle to prioritise purchasing equipment. Further large-scale evaluations are required to explore the effect of multicomponent interventions on injury occurrence.
Acknowledgments
We would like to thank the Small Steps Big Changes Parent Champions (a team of parent volunteers) for their invaluable input into this project and the parents and practitioners who participated in the project
Footnotes
Contributors: EO, DK, MCW, MH, MJ and CC obtained funding for the study and designed the main study methods and data collection tools. EO, DK, CC and MJT planned and conducted the data analysis. CT prepared documentation for the ethics committee. CT, TP and RC collected the data. MJT, EO, DK, CC, MH and MCW drafted the manuscript with revisions additionally from MJ, RC, CT and TP. EO is the guarantor for the study.
Funding: This project was supported by funding from the Small Steps Big Changes, part of The National Lottery Community Fund A Better Start programme.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by the East Midlands Leicester Central Research Ethics Committee (reference: 17/EM/0240). Participants gave informed consent to participate in the study before taking part.
References
- 1. Public Health England; Royal Society for the Prevention of Accidents; Child Accident Prevention Trust . Reducing unintentional injuries in and around the home among children under five years [Internet]. 2018. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/696646/Unintentional_injuries_under_fives_in_home.pdf
- 2. McClure R, Kegler S, Davey T, et al. Contextual determinants of childhood injury: a systematic review of studies with multilevel analytic methods. Am J Public Health 2015;105:e37–43. 10.2105/AJPH.2015.302883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Orton E, Kendrick D, West J, et al. Independent risk factors for injury in pre-school children: three population-based nested case-control studies using routine primary care data. PLoS One 2012;7:e35193. 10.1371/journal.pone.0035193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kendrick D, Mulvaney C, Burton P, et al. Relationships between child, family and neighbourhood characteristics and childhood injury: a cohort study. Soc Sci Med 2005;61:1905–15. 10.1016/j.socscimed.2005.04.003 [DOI] [PubMed] [Google Scholar]
- 5. Mytton J, Towner E, Brussoni M, et al. Unintentional injuries in school-aged children and adolescents: lessons from a systematic review of cohort studies. Inj Prev 2009;15:111–24. 10.1136/ip.2008.019471 [DOI] [PubMed] [Google Scholar]
- 6. Edwards P, Roberts I, Green J, et al. Deaths from injury in children and employment status in family: analysis of trends in class specific death rates. BMJ 2006;333:119. 10.1136/bmj.38875.757488.4F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bell N, Kruse S, Simons RK, et al. A spatial analysis of functional outcomes and quality of life outcomes after pediatric injury. Inj Epidemiol 2014;1:16. 10.1186/s40621-014-0016-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Brown FL, Whittingham K, Sofronoff K, et al. Parenting a child with a traumatic brain injury: experiences of parents and health professionals. Brain Inj 2013;27:1570–82. 10.3109/02699052.2013.841996 [DOI] [PubMed] [Google Scholar]
- 9. Kendrick D, Young B, Mason-Jones AJ, et al. Home safety education and provision of safety equipment for injury prevention. Cochrane Database Syst Rev 2012;2012:CD005014. 10.1002/14651858.CD005014.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hill T, Coupland C, Kendrick D, et al. Impact of the National home safety equipment scheme “ safe at home ” on hospital admissions for unintentional injury in children under 5: a controlled interrupted time series analysis. J Epidemiol Community Health 2022;76:53–9. 10.1136/jech-2021-216613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Runyan CW, Bangdiwala SI, Linzer MA, et al. Risk factors for fatal residential fires. N Engl J Med 1992;327:859–63. 10.1056/NEJM199209173271207 [DOI] [PubMed] [Google Scholar]
- 12. Marshall SW, Runyan CW, Bangdiwala SI, et al. Fatal residential fires: who dies and who survives? JAMA 1998;279:1633–7. 10.1001/jama.279.20.1633 [DOI] [PubMed] [Google Scholar]
- 13. Kendrick D, Zou K, Ablewhite J, et al. Risk and protective factors for falls on stairs in young children: multicentre case-control study. Arch Dis Child 2016;101:909–16. 10.1136/archdischild-2015-308486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kendrick D, Majsak-Newman G, Benford P, et al. Poison prevention practices and medically attended poisoning in young children: multicentre case-control study. Inj Prev 2017;23:93–101. 10.1136/injuryprev-2015-041828 [DOI] [PubMed] [Google Scholar]
- 15. National Institute for Health and Care Excellence . Unintentional injuries in the home: interventions for under 15s [Internet]. 2010. Available: https://www.nice.org.uk/guidance/ph30/chapter/1-Recommendations
- 16. Watson MC, Mulvaney C, Timblin C, et al. Missed opportunities to keep children safe? national survey of injury prevention activities of children’s centres. Health Education Journal 2016;75:833–42. 10.1177/0017896916629816 [DOI] [Google Scholar]
- 17. Orton E, Watson MC, Hayes M, et al. Evaluation of the effectiveness, implementation and cost-effectiveness of the stay one step ahead home safety promotion intervention for pre-school children: a study protocol. Inj Prev 2020;26:573–80. 10.1136/injuryprev-2020-043877 [DOI] [PubMed] [Google Scholar]
- 18. CityCare . Building healthier communities [Internet]. 2021. Available: https://www.nottinghamcitycare.nhs.uk/our-services/small-steps-big-changes
- 19. Quilty S, Kendrick D, Watson M, et al. Avoidable injuries in children and young people [Internet]. n.d. Available: https://www.nottinghaminsight.org.uk/themes/health-and-wellbeing/joint-strategic-needs-assessment/children-and-young-people/avoidable-injuries-in-children-and-young-people-2015/
- 20. National Institute for Health and Care Excellence . Behaviour change: general approaches public health guideline [PH6] [Internet]. n.d. Available: https://www.nice.org.uk/guidance/ph6
- 21. Swart L, van Niekerk A, Seedat M, et al. Paraprofessional home visitation program to prevent childhood unintentional injuries in low-income communities: a cluster randomized controlled trial. Inj Prev 2008;14:164–9. 10.1136/ip.2007.016832 [DOI] [PubMed] [Google Scholar]
- 22. Sommet N, Morselli D. Keep calm and learn multilevel logistic modeling: a simplified three-step procedure using stata, R, mPLUS, and SPSS. International Review of Social Psychology 2017;30:203–18. 10.5334/irsp.90 [DOI] [Google Scholar]
- 23. Kendrick D, Marsh P, Fielding K, et al. Preventing injuries in children: cluster randomised controlled trial in primary care. BMJ 1999;318:980–3. 10.1136/bmj.318.7189.980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. DiGuiseppi C, Roberts I, Wade A, et al. Incidence of fires and related injuries after giving out free smoke alarms: cluster randomised controlled trial. BMJ 2002;325:995. 10.1136/bmj.325.7371.995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hindmarch P, Hawkins A, McColl E, et al. Recruitment and retention strategies and the examination of attrition bias in a randomised controlled trial in children’s centres serving families in disadvantaged areas of england. Trials 2015;16:79. 10.1186/s13063-015-0578-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. National Statistics . English indices of deprivation [Internet]. 2019. Available: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019
- 27. Pizzo E, Doyle C, Matthews R, et al. Patient and public involvement: how much do we spend and what are the benefits? Health Expect 2015;18:1918–26. 10.1111/hex.12204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bonevski B, Randell M, Paul C, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Med Res Methodol 2014;14:42. 10.1186/1471-2288-14-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mitchell EJ, Ahmed K, Breeman S, et al. It is unprecedented: trial management during the COVID-19 pandemic and beyond. Trials 2020;21:784. 10.1186/s13063-020-04711-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hwang V, Duchossois GP, Garcia-Espana JF, et al. Impact of a community based fire prevention intervention on fire safety knowledge and behavior in elementary school children. Inj Prev 2006;12:344–6. 10.1136/ip.2005.011197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Petridou E, Tolma E, Dessypris N, et al. A controlled evaluation of a community injury prevention project in two Greek islands. Int J Epidemiol 1997;26:173–9. 10.1093/ije/26.1.173 [DOI] [PubMed] [Google Scholar]
- 32. Wang Y, Gielen AC, Magder LS, et al. A randomised safety promotion intervention trial among low-income families with toddlers. Inj Prev 2018;24:41–7. 10.1136/injuryprev-2016-042178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Achana FA, Sutton AJ, Kendrick D, et al. The effectiveness of different interventions to promote poison prevention behaviours in households with children: a network meta-analysis. PLoS One 2015;10:e0121122. 10.1371/journal.pone.0121122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Phelan KJ, Khoury J, Xu Y, et al. A randomized controlled trial of home injury hazard reduction: the home injury study. Arch Pediatr Adolesc Med 2011;165:339–45. 10.1001/archpediatrics.2011.29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Watson M, Kendrick D, Coupland C, et al. Providing child safety equipment to prevent injuries: randomised controlled trial. BMJ 2005;330:178. 10.1136/bmj.38309.664444.8F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hendrickson SG. Reaching an underserved population with a randomly assigned home safety intervention. Inj Prev 2005;11:313–7. 10.1136/ip.2004.007229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sangvai S, Cipriani L, Colborn DK, et al. Studying injury prevention: practices, problems, and pitfalls in implementation. Clin Pediatr (Phila) 2007;46:228–35. 10.1177/0009922806293861 [DOI] [PubMed] [Google Scholar]
- 38. Kendrick D, Ablewhite J, Achana F, et al. Keeping children safe: a multicentre programme of research to increase the evidence base for preventing unintentional injuries in the home in the under-fives. Programme Grants Appl Res 2017;5:1–834. 10.3310/pgfar05140 [DOI] [PubMed] [Google Scholar]
- 39. Kendrick D, Mulvaney C, Watson M. Does targeting injury prevention towards families in disadvantaged areas reduce inequalities in safety practices? Health Educ Res 2009;24:32–41. 10.1093/her/cym083 [DOI] [PubMed] [Google Scholar]
- 40. Turner S, Arthur G, Lyons RA, et al. Modification of the home environment for the reduction of injuries. Cochrane Database Syst Rev 2011;2011:CD003600. 10.1002/14651858.CD003600.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ip-2022-044745supp001.pdf (111.4KB, pdf)
Data Availability Statement
No data are available.