Abstract
Objective
Assess cancer risks with Janus kinase inhibitors (JAKi) versus biological disease-modifying antirheumatic drugs (bDMARDs) in clinical practice.
Methods
Cohort study of patients with rheumatoid arthritis (RA) or psoriatic arthritis (PsA) initiating treatment with JAKi, tumour necrosis factor inhibitors (TNFi) or other (non-TNFi) bDMARDs 2016–2020 using prospectively collected data from the Swedish Rheumatology Quality Register linked to other registers including the Cancer Register. We estimated incidence rates, and HRs via Cox regression, for all cancers excluding non-melanoma skin cancer (NMSC), and for individual cancer types including NMSC.
Results
We identified 10 447 patients with RA and 4443 patients with PsA who initiated treatment with JAKi, a non-TNFi bDMARD or a TNFi. Median follow-up times in RA were 1.95, 2.83 and 2.49 years, respectively. In RA, based on 38 incident cancers other than NMSC with JAKi vs 213 with TNFi the overall HR was 0.94 (95% CI 0.65 to 1.38). Based on 59 vs 189 incident NMSC, the HR was 1.39 (95% CI 1.01 to 1.91). At 2 or more years since treatment start, the HR for NMSC was 2.12 (95% CI 1.15 to 3.89). In PsA, based on 5 vs 73 incident cancers other than NMSC, and 8 vs 73 incident NMSC, the corresponding HRs were 1.9 (95% CI 0.7 to 5.2) and 2.1 (95% CI 0.8 to 5.3).
Conclusion
In clinical practice, the short-term risk of cancer other than NMSC in individuals initiating treatment with JAKi is not higher than for TNFi, but we found evidence of increased risk for NMSC.
Keywords: Arthritis, Rheumatoid; Epidemiology; Arthritis, Psoriatic; Biological Therapy
WHAT IS ALREADY KNOWN ON THIS TOPIC
Some meta-analyses of trial data and data from the ORAL Surveillance safety phase 3b–4 trial have indicated an elevated risk for non-melanoma skin cancer, and of other types of cancer overall, in patients with rheumatoid arthritis (RA) treated with the Janus kinase inhibitor (JAKi) tofacitinib versus TNFi.
WHAT THIS STUDY ADDS
Our study, based on data on two JAKi (tofacitinib and baricitinib) as used in clinical practice, found no evidence of an increased short-term risk of cancer other than non-melanoma skin cancer in RA. By contrast, the risk of non-melanoma skin cancer may be increased already with short-term use. Furthermore, our study adds information on cancer risk by time since treatment initiation, on the distribution of non-melanoma skin cancer subtypes, in individuals with RA enriched for cardiovascular risk factors, and on the cancer risk in psoriatic arthritis (PsA) patients treated with JAKi. Finally, our study provides information on how these cancer risks with JAKi relate to those with non-TNFi biological disease-modifying antirheumatic drugs and in the general population.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Our study adds evidence to suggest a possible increased risk for non-melanoma skin cancers with JAKi as used in clinical practice for RA and PsA.
Introduction
Patients with rheumatoid arthritis (RA) are at increased risk of cancer overall, mainly due to an increased occurrence of lung cancer and malignant lymphoma.1–3 Increased risks of non-melanoma skin cancer (NMSC) have been reported in patients with RA4 and also in patients with psoriatic arthritis (PsA).5 Studies on cancer risks with biological disease-modifying antirheumatic drugs (bDMARDs) such as tumour necrosis factor inhibitors (TNFi) and other (non-TNFi) bDMARDs have overall been reassuring6–11 but also pointed to signals of potential risk increases, with individual drugs and for individual cancer sites,12 for example, NMSC.8 9 13
For the most recently introduced class of DMARDs, the targeted synthetic DMARDs (tsDMARD) janus kinase inhibitors (JAKi), concerns have been raised that the mechanism of JAK inhibition could increase risk of cancer.14–16 These concerns were recently fueled by the results from the ORAL Surveillance safety trial of tofacitinib versus adalimumab/etanercept, including patients with RA above 50 years of age with at least one cardiovascular (CV) risk factor, in which a 50% relative increased risk of cancers excluding NMSC, and at least an equally large risk increase for NMSC was reported among those treated with JAKi versus TNFi.17 These findings have led regulatory agencies such as the Food and Drug Administration and the European Medicines Agency to issue warnings on cancer risks, extended to the entire class of JAKi drugs, even if it is still uncertain whether any increased cancer risk differ between individual JAKi considering their somewhat different pharmacological properties.
The ORAL surveillance clinical trial encompassed a population enriched with CV risk factors, whose underlying cancer risk may differ from that in clinical practice. It is unclear whether similar increased risks would apply to JAKi as used in younger (<50 years of age) patients with RA, in RA without CV risk factors and in patients treated with JAKi for other inflammatory conditions such as PsA. Further, due to the design of the ORAL Surveillance study, it remains unknown whether the observed higher occurrence of cancer with JAKi than with TNFi reflects an increased risk of cancer with tofacitinib, an unusually low risk of cancer in the TNFi arm or an increased risk of cancer with both drugs but higher for tofacitinib than for TNFi. So far, the cancer safety signals with JAKi have mainly emanated from clinical trials.18–21 Data on cancer risks with JAKi as used in clinical practice are limited to two US studies, neither of which reported any increased cancer risk.22 23
Our primary aim was therefore to estimate incidence rates and HRs of cancer overall, and by type, in patients with RA or PsA treated with JAKi versus TNFi in clinical practice. Moreover, we aimed to compare these rates to those of patients with RA or PsA treated with other bDMARDs than TNFi, and to those in the general population. Finally, we aimed to assess whether the observed rates and HRs of cancer varied with time and when adding a similar CV risk factor enrichment as that in the ORAL surveillance trial.
Subjects and methods
Design and setting
We performed an observational cohort study using prospectively collected individual-level clinical data enriched through linkage to other national Swedish registers, 1 January 2016 to 31 December 2020. In Sweden, most patients with RA are treated by rheumatologists at public hospital-based outpatient clinics; the same applies to patients with PsA treated with DMARDs. Prescription medication is subsidised, and annual patient out-of-pocket costs are capped at €220.
Data sources
We used information from the following national Swedish data sources: The Swedish Rheumatology Quality register (SRQ), the National Patient Register, the Longitudinal Database for Insurance and Labor Market Studies (LISA), the Prescribed Drug Register, the Population and Cause of death register and the National Cancer register. Online supplemental table S1 describes the data sources and the information collected from each of these.
ard-2022-223636supp001.pdf (190.4KB, pdf)
Study population, study period and exposures
We identified all individuals above 18 years of age registered with RA or PsA in SRQ. For each patient, five general population comparator subjects were identified, free from RA/PsA at their index case’s first registration of RA/PsA and matched on age, sex and region of domicile, from the Population register. We used SRQ to identify all treatment initiations among patients with RA or PsA with: (1) TNFi (adalimumab, certolizumab pegol, etanercept, golimumab, infliximab), (2) non-TNFi bDMARD (rituximab, abatacept, tocilizumab, sarilumab) or (3) JAKi (baricitinib, tofacitinib, upadacitinib). All three JAKis were included as a class, baricitinib and tofactinib also as individual drugs (upadacitinib contributed to low number of treatments and zero events as a consequence of its introduction late during the study period). Filgotinib was not included as it was introduced after our study period. To increase statistical precision, we included treatment initiations (TNFi and non-TNFi) from 2016. For JAKi, we included treatment initiations from their market entry in 2017. Because of the new-user design, treatment episodes initiated before or ongoing at the start of the study period were not included (but contributed to the number of previously used b/tsDMARDs), but did not disqualify the same patient from contributing one or more new treatment episodes initiated during the study period. Patients who started one JAKi and later switched to a second (different) JAKi during the study period contributed twice to the JAKi cohort; the same applied for all other treatment episodes with different drugs within the same exposure category. For example, a patient who was on etanercept 2012–2015, abatacept 2017–2019 and baricitinib 2019–2020 contributed once to our non-TNFi group (then with a history of one previous b/tsDMARD) and once to our JAKi group (then with a history of two previous b/tsDMARDs). All study participants who had a history of any previous cancer other than NMSC were excluded from all analyses. No other inclusion/exclusion criteria were employed. Treatment initiations were followed until the first of the specific cancer type under study. Individuals who, during follow-up, developed cancer of another type than the one under study were not censored.
Follow-up
For the RA and PsA cohorts start of follow-up was defined as the date of treatment start with each b/tsDMARDs during the study period. For the general population cohort, start of follow-up was defined as the time point of the first recorded b/tsDMARD treatment start in its index case with RA/PsA during the study period. We used an ever-treated approach, in which each patient in each treatment cohort was followed from every treatment initiation until the occurrence of the outcome, death, emigration from Sweden or end of the study period on 31 December 2020. Treatment interruption of the same molecule shorter than 90 days (+183 days for rituximab) was considered the same treatment episode. No distinction was made between an originator product and its biosimilars.
Outcomes
To identify incident cancers overall and by subtype, we used International Classification of Disease version 10 codes and Systematised Nomenclature of Medicine codes as registered in the Cancer and Cause of death registers (online supplemental table S2). We defined the following cancer outcomes: (1) All cancers other than NMSC (main outcome), (2) NMSC including both basal cell carcinoma (BCC) and squamous cell carcinomas (SCC) (3) prostate, (4) testicular, (5) female breast, (6) all haematopoietic (leukaemias, immunoproliferative, myeloproliferative, lymphoproliferative disease and lymphomas) (7) malignant lymphomas, (8) renal, (9) lung, (10) colorectal, (11) ovarian, (12) cervical (13) urinary tract (bladder, urethra, ureter), (14) central nervous system, (15) uterus, (16) ear-nose-throat, (17) digestive tract (oesophagus, gastric, ileum and jejunum), (18) pancreas, (19) liver-gallbladder cancers and (20) malignant melanoma.
Statistics
For each treatment cohort and for the general population comparator cohort, we presented descriptive statistics, and for each outcome the number of events, and crude incidence rates. We calculated incidence rates standardising to the age and sex distribution in the TNFi cohort. We also fitted Cox proportional hazards models to estimate HRs comparing each treatment cohort (JAKi; overall and separately for tofacitinib and baricitinib, and the non-TNFi bDMARD cohort) to the TNFi cohort, using time since treatment initiation as the time scale. HRs were adjusted for age, sex, line of therapy, comorbidities (see online supplemental table S3), socioeconomic status and RA disease-related factors at treatment start (duration of disease, seropositive status, Disease Activity Score 28 C reactive protein (DAS28CRP), CRP, concomitant drug use (steroid, methotrexate, non-methotrexate csDMARD, prednisolone use, smoking status), with missing categories for those variables (RA disease-related factors, all other variables had negligible missing data) with missing information. Incrementally adjusted models are presented in online supplemental tables S6, S9 and S16, to display the impact of adjustment for specific factors. We only performed comparative analyses (ie, estimated HRs) where the number events in each cohort were ≥5. We used SAS and Stata V.16.1 to perform the analyses.
Additional analyses
We performed several additional analyses. First, we fitted models by time since treatment initiation (≤1, 1–2, ≥2 years) by inclusion of an interaction term and thereby relaxed the proportional hazards assumption. Second, we performed separate analyses by previous use of b/tsDMARDs (0, 1–2, ≥3). Third, we introduced a latency period of 90 days, so that only cancers diagnosed 90 days or later after treatment start would contribute to analyses. Fourth, we restricted the main analysis to a CV-enriched subset of the JAKi, non-TNFi and TNFi cohort (see online supplemental table S4 for definitions of this enrichment). Fifth, we performed a sensitivity analysis using an on-drug approach for all cancers other than NMSC and NMSC, respectively, for patients with RA. Sixth, the study period ended in December 2020 and the COVID pandemic could theoretically affect the results. We; therefore, introduced a sensitivity analysis restricting the follow-up to Feb 2020 (for patients with RA). Finally, in our main analysis, we performed a multiple imputation using chained equations with 30 repetitions for variables with missing information (DAS28CRP, CRP using multinomial logistic regression; disease duration, smoking, civil status and education using logistic regression). Imputation models were adjusted for all covariates included in the analysis model plus the event indicator and the Nelson-Aalen estimate of the cumulative hazard.
Results
During the study period, a total of 10 447 unique individuals with RA without a previous cancer diagnosis started at least one b/tsDMARD. A total of 1967 patients with RA contributed to the JAKi initiator cohort, 3520 to the non-TNFi cohort and 7343 to the TNFi cohort. The total person time at risk in the JAKi, non-TNFi bDMARD and TNFi cohorts was 4022, 11 231 and 21 389 patient years, respectively. The median follow-up times were 1.95, 2.83 and 2.49 years (table 1).
Table 1.
Baseline characteristics of the study cohorts of Swedish patients with RA initiating a b/tsDMARD treatment 2016–2020
| Initiators of tofacitinib | Initiators of baricitinib | Initiators of upadacitinib | Initiators of all JAKis | Initiators of a non-TNFi bDMARD | Initiators of a TNFi | General population Reference cohort |
|
| Observations (treatment initiations) | 377 | 1676 | 90 | 2143 | 4128 | 8580 | |
| Individuals | 377 | 1676 | 90 | 1967 | 3520 | 7343 | 48 318 |
| Age years, median (IQR) | 58 (50–67) | 59 (50–70) | 56 (49–64) | 59 (50–69) | 60 (51–70) | 56 (46–67) | 57 (47–68) |
| Female, % | 83 | 81 | 86 | 82 | 79 | 78 | 78 |
| Median follow-up, years | 2.15 | 1.98 | 0.14 | 1.95 | 2.83 | 2.49 | 2.73 |
| Total person time at risk, years | 799 | 3207 | 15 | 4022 | 11 231 | 21 389 | 130 026 |
| Disease-related | |||||||
| Disease duration years, median (IQR) | 12.9 (7.2–23.9) | 13.2 (6.7–21.9) | 15.6 (7.8–22.1) | 13.2 (6.8–22.3) | 11.2 (4.9–20.0) | 7.1 (2.6–14.7) | |
| Seropositive, % | 76 | 80 | 73 | 79 | 84 | 76 | |
| DAS28CRP, median (IQR) | 4.6 (3.7–5.4) | 4.4 (3.5–5.1) | 4.2 (3.3–5.0) | 4.4 (3.5–5.1) | 4.5 (3.7–5.2) | 4.1 (3.4–4.9) | |
| DAS28CRP missing, % | 45 | 40 | 49 | 41 | 43 | 41 | |
| CRP <5, % | 46 | 47 | 54 | 47 | 40 | 48 | |
| CRP5-9, % | 13 | 18 | 18 | 17 | 18 | 18 | |
| CRP 10–19, % | 13 | 17 | 11 | 16 | 17 | 16 | |
| CRP ≥20, % | 27 | 19 | 18 | 20 | 25 | 18 | |
| CRP missing, % | 34 | 29 | 37 | 30 | 32 | 30 | |
| Smoker, % | 58 | 59 | 60 | 59 | 60 | 57 | |
| Smoking missing, % | 13 | 19 | 20 | 18 | 20 | 28 | |
| 0 previous b/tsDMARDs, % | 9 | 13 | 6 | 12 | 20 | 63 | |
| 1–2 previous b/tsDMARDs, % | 28 | 39 | 34 | 37 | 48 | 31 | |
| 3+previous b/tsDMARDs, % | 63 | 48 | 60 | 51 | 31 | 6 | |
| Treatment related, % | |||||||
| Concomitant methotrexate use, % | 36 | 43 | 39 | 42 | 46 | 63 | 1 |
| Concomitant oral steroid use, % | 68 | 64 | 61 | 64 | 68 | 61 | 2 |
| Prednisolone use (average among users) mg prior 1 year, % | 4.2 (2.7–6.8) | 4.1 (2.1–6.2) | 4.2 (2.1–5.7) | 4.1 (2.1–6.3) | 4.1 (2.7–6.8) | 3.4 (1.4–5.5) | 1.4 (0.7–4.8) |
| Comorbidities (previous 5 years), % | |||||||
| History of diabetes types 1 and 2 | 10 | 10 | 6 | 10 | 11 | 10 | 8 |
| History of ischaemic heart disease | 5 | 5 | 1 | 5 | 6 | 3 | 2 |
| History of hospitalised infections | 13 | 13 | 6 | 12 | 13 | 6 | 3 |
| History of chronic obstructive pulmonary disease | 10 | 8 | 6 | 8 | 10 | 6 | 3 |
| History of kidney failure | 2 | 1 | 1 | 2 | 2 | 1 | 1 |
| History of heart failure | 2 | 2 | 2 | 2 | 3 | 1 | 1 |
| History of stroke | 5 | 5 | 3 | 5 | 6 | 2 | 3 |
| History of VTE | 4 | 3 | 3 | 3 | 3 | 2 | 1 |
| History of joint surgery | 7 | 8 | 3 | 8 | 7 | 5 | 2 |
| History of hypertension | 12 | 15 | 11 | 14 | 16 | 9 | 7 |
| History of NMSC | 1.6 | 1.9 | 3.3 | 1.9 | 1.9 | 1.5 | 1.0 |
| Drug dispensations (previous 6 months), % | |||||||
| Lipid lowering drugs | 15 | 15 | 14 | 15 | 16 | 13 | 14 |
| Other measures of comorbidities/health | |||||||
| Hospital days in the previous year | 5 (1–17) | 5 (2–12) | 5 (3–40) | 5 (2–13) | 7 (3–15) | 4 (2–10) | 5 (2–13) |
| Sick leave in the previous year, % | 17 | 16 | 21 | 16 | 15 | 17 | 7 |
| Disability pension in the previous year, % | 2 | 1 | 0 | 1 | 1 | 1 | 0 |
| Socioeconomics | |||||||
| Education >12 years, % | 29 | 33 | 36 | 33 | 31 | 35 | 38 |
| Married/partner, % | 54 | 51 | 62 | 52 | 51 | 50 | 49 |
b/tsDMARD, biological/targeted synthetic disease-modifying antirheumatic drug; CRP, C reactive protein; DAS28, Disease Activity Score 28; JAKi, Janus kinase inhibitor; NMSC, non-melanoma skin cancer; RA, rheumatoid arthritis; TNFi, tumour necrosis factor inhibitor; VTE, venous thromboembolism.
We similarly included 4443 unique individuals with PsA without a previous cancer diagnosis; 379 contributed to the JAKi cohort, 185 to the non-TNFi cohort and 4186 to the TNFi cohort. The total person time at risk in the JAKi, non-TNFi bDMARD and TNFi cohorts was 585, 418 and 12 623 patient years, respectively. The median follow-up times were 1.52, 2.25 and 2.44 years (online supplemental table S5).
RA: occurrence and relative risk for cancer
Table 2 and figure 1 display number of events, incidence rates and fully adjusted HRs for patients with RA initiating treatment with JAKi, non-TNFi or a TNFi. Based on 38 incident cancers other than NMSC in the JAKi cohort, 141 in the non-TNFi cohort and 213 in the TNFi cohort, the fully adjusted HR for JAKi versus TNFi was 0.94 (95% CI 0.65 to 1.38). The corresponding HR for non-TNFi versus TNFi was 1.12 (95% CI 0.88 to 1.43). For tofacitinib, the fully adjusted HR (vs TNFi) was 1.08 (95% CI 0.52 to 2.24) and 0.92 (95% CI 0.61 to 1.38) for baricitinib (table 2). In the JAKi cohort, there were 7 breast cancers (HR=0.73, 95% CI 0.29 to 1.86, vs TNFi), 6 haematopoietic (HR=1.90, 95% CI 0.70 to 5.16) and 7 lung cancers (HR=1.15, 95% CI 0.57 to 2.32). For all other sites other than NMSC (table 2), there were less than five events observed among the JAKi treated and thus are not presented.
Table 2.
Number of events, person years, crude and standardised incidence rates and HRs, for all cancers other than NMSC, and for cancer sites where at least five incident events were observed in the JAK cohort, in Swedish patients with RA treated with JAKi, non-TNFi bDMARDs or TNFi
| Cohort | Events | Person years, no | Crude incidence rate per 1000 person-years | Standardised incidence rate per 1000 person-years | Fully adjusted HR* |
| All cancers other than NMSC | |||||
| All JAKi | 38 | 3996 | 9.5 | 8.3 | 0.94 (0.65 to 1.38) |
| Tofacitinib | 8 | 793 | 10.1 | 11.2 | 1.08 (0.52 to 2.24) |
| Baricitinib | 30 | 3187 | 9.4 | 8.0 | 0.92 (0.61 to 1.38) |
| Non-TNFi bDMARD† | 141 | 11 051 | 12.8 | 10.5 | 1.12 (0.88 to 1.43) |
| TNFi | 213 | 21 122 | 10.1 | 10.1 | 1.0 (Reference) |
| General population | 1245 | 128 224 | 9.7 | 9.2 | n/a |
| NMSC | |||||
| All JAKi | 59 | 3954 | 14.9 | 12.9 | 1.39 (1.01 to 1.91) |
| Tofacitinib | 11 | 781 | 14.1 | 14.9 | 1.56 (0.83 to 2.92) |
| Baricitinib | 48 | 3157 | 15.2 | 12.5 | 1.37 (0.97 to 1.92) |
| Non-TNFi bDMARD† | 126 | 11 027 | 11.4 | 9.0 | 1.00 (0.78 to 1.28) |
| TNFi | 189 | 21 083 | 9.0 | 9.0 | 1.0 (Reference) |
| General population | 852 | 128 630 | 6.6 | 6.2 | n/a |
| Breast cancer | |||||
| All JAKi | 7 | 4014 | 1.7 | 1.6 | 0.73 (0.29 to 1.86) |
| Tofacitinib | 1 | 797 | 1.3 | – | – |
| Baricitinib | 6 | 3201 | 1.9 | 1.7 | 0.77 (0.29 to 2.06) |
| Non-TNFi bDMARD† | 23 | 11 197 | 2.1 | 1.9 | 0.88 (0.48 to 1.61) |
| TNFi | 42 | 21 328 | 2.0 | 2.0 | 1.0 (Reference) |
| General population | 262 | 129 601 | 2.0 | 2.0 | n/a |
| All haematopoietic | |||||
| All JAKi | 6 | 4018 | 1.5 | 1.5 | 1.90 (0.70 to 5.16) |
| Tofacitinib | 1 | 798 | 1.3 | – | – |
| Baricitinib | 5 | 3203 | 1.6 | 1.6 | 1.96 (0.66 to 5.79) |
| Non-TNFi bDMARD† | 12 | 11 217 | 1.1 | 0.9 | 1.04 (0.48 to 2.25) |
| TNFi | 22 | 21 359 | 1.0 | 1.0 | 1.0 (Reference) |
| General population | 99 | 129 854 | 0.8 | 0.7 | n/a |
| Lung cancer | |||||
| All JAKi | 7 | 4021 | 1.7 | 1.5 | 1.15 (0.57 to 2.32) |
| Tofacitinib | 2 | 798 | 2.5 | – | – |
| Baricitinib | 5 | 3206 | 1.6 | 1.2 | 0.98 (0.44 to 2.23) |
| Non-TNFi bDMARD† | 11 | 11 224 | 1.0 | 0.7 | 0.59 (0.31 to 1.15) |
| TNFi | 30 | 21 368 | 1.4 | 1.4 | 1.0 (Reference) |
| General population | 111 | 129 912 | 0.9 | 0.8 | n/a |
Estimated from Cox proportional hazards models. Standardised incidence rate standardised to the age and sex distribution in the TNFi cohort. – is displayed when too few events (<5) were observed.
*Fully adjusted HR: adjusted for age, sex, line of therapy, for comorbidities, SES, disease-related factors and with missing categories included for those variables with missing information.
†Non-TNFI bDMARD includes rituximab, abatacept, tocilizumab.
bDMARD, biological disease-modifying antirheumatic drug; JAKi, Janus kinas inhibitor; n/a, not available; NMSC, non-melanoma skin cancer; RA, rheumatoid arthritis; SES, socioeconomic status; TNFi, tumour necrosis factor inhibitor.
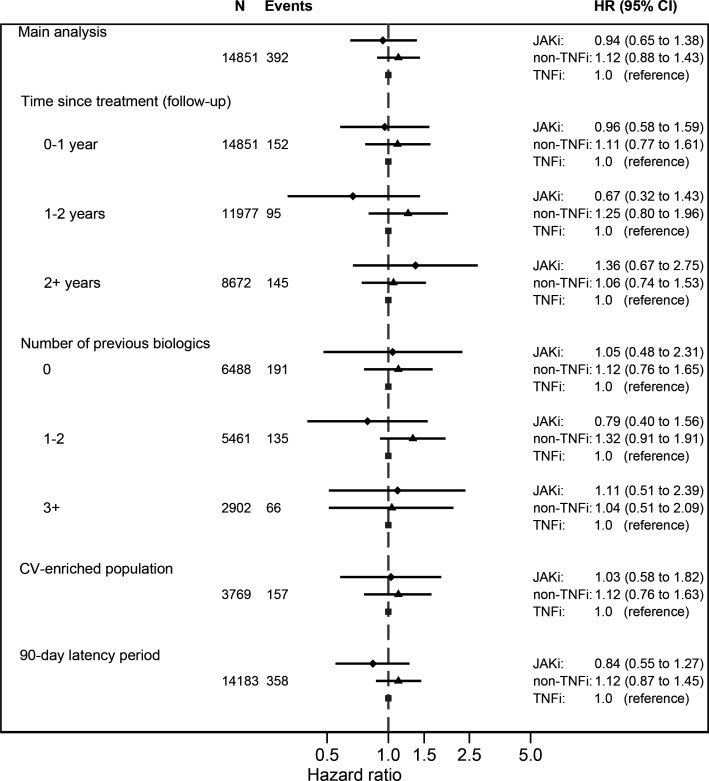
Figure 1.
Hazard ratios with 95% confidence intervals for the outcome all cancers other than non-melanoma skin cancer (overall, and by time since treatment start, number of previous b/tsDMARDs, in a CV enriched population, and using a 90-day latency period) in Swedish patients with RA starting treatment with a JAKi, a TNFi or non-TNFi bDMARD.
We identified 59 incident NMSC events in the JAKi cohort, 126 in the non-TNFi cohort and 189 in the TNFi cohort, which corresponded to fully adjusted HR of 1.39 (95%CI 1.01 to 1.91) for JAKi versus TNFi. The corresponding HR for non-TNFi versus TNFi was 1.00 (95%CI 0.78 to 1.28). The NMSC incidences in the JAKi, TNFi, non-TNFis groups were all higher than in the general population (table 2). The HR of NMSC for tofacitinib (vs TNFi) was 1.56 (95% CI 0.83 to 2.92) and 1.37 (95%CI 0.97 to 1.92) for baricitinib (table 2). These HRs did not vary appreciably between successively adjusted models (online supplemental table S6). The proportion of SCC among all NMSCs was largely similar in the JAKi, TNFi and non-TNFi groups (all of which were higher than in the general population) (online supplemental table S7). The proportion of patients with a history of NMSC (1.5%–1.9%) was largely equal across the treatment cohorts (table 1). Also, the proportion of incident NMSC events that occurred in individuals with a history of NMSC (12%–16%) was largely equal across these cohorts (online supplemental table S8).
Additional analyses
When allowing the effect of treatment to vary across time since treatment initiation, the HR for cancer other than NMSC for JAKi versus TNFi varied from 0.96 (95%CI 0.58 to 1.59) during 0–1 year since treatment start through 1.36 (95% CI 0.67 to 2.75) for 2 or more years since treatment start. For NMSC, the corresponding fully adjusted HRs varied from 1.12 (95% CI 0.70 to 1.78) during the first year since treatment start, to 2.12 (95% CI 1.15 to 3.89) at two or more years since treatment start (table 3), but these variations were not statistically significant (p values for interaction with time were 0.60 and 0.10, respectively). These HRs did not vary appreciably between successively adjusted models (online supplemental table S9).
Table 3.
Number of events, person years, crude and standardised incidence rates of all cancers other than NMSC and NMSC, in patients with RA treated with JAKis, non-TNFi bDMARDs or TNFi, by time since treatment initiation
| Events | Person years, no | Crude incidence rate per 1000 person-years | Standardised incidence rate per 1000 person-years | Fully adjusted HR* | |
| All cancers other than NMSC | |||||
| 0–1 year | |||||
| JAKi | 20 | 1884 | 10.6 | 9.4 | 0.96 (0.58 to 1.59) |
| Non-TNFi | 52 | 3815 | 13.6 | 11.4 | 1.11 (0.77 to 1.61) |
| TNFi | 80 | 7759 | 10.3 | 10.3 | 1.0 (Reference) |
| 1–2 years | |||||
| JAKi | 8 | 1358 | 5.9 | 4.9 | 0.67 (0.32 to 1.43) |
| Non-TNFi | 36 | 3049 | 11.8 | 9.2 | 1.25 (0.80 to 1.96) |
| TNFi | 51 | 6000 | 8.5 | 8.5 | 1.0 (Reference) |
| 2 or more years | |||||
| JAKi | 10 | 754 | 13.2 | 12.2 | 1.36 (0.67 to 2.75) |
| Non-TNFi | 53 | 4187 | 12.7 | 10.7 | 1.06 (0.74 to 1.53) |
| TNFi | 82 | 7363 | 11.1 | 11.1 | 1.0 (Reference) |
| NMSC | |||||
| 0–1 year | |||||
| JAKi | 24 | 1880 | 12.8 | 11.2 | 1.12 (0.70 to 1.78) |
| Non-TNFi | 40 | 3818 | 10.5 | 8.3 | 0.85 (0.57 to 1.26) |
| TNFi | 75 | 7755 | 9.7 | 9.7 | 1.0 (Reference) |
| 1–2 years | |||||
| JAKi | 20 | 1338 | 14.9 | 12.8 | 1.48 (0.87 to 2.51) |
| Non-TNFi | 47 | 3041 | 15.5 | 11.8 | 1.43 (0.95 to 2.15) |
| TNFi | 51 | 5991 | 8.5 | 8.5 | 1.0 (Reference) |
| 2 or more years | |||||
| JAKi | 15 | 735 | 20.4 | 18.3 | 2.12 (1.15 to 3.89) |
| Non-TNFi | 39 | 4168 | 9.4 | 7.3 | 0.86 (0.57 to 1.31) |
| TNFi | 63 | 7338 | 8.6 | 8.6 | 1.0 (Reference) |
Non-TNFI includes; rituximab; abatacept; tocilizumab. All HRs estimated from Cox models including an interaction between time since treatment initiation (0–1, 1–2, 2+ years) and treatment exposure cohort. Standardised incidence rate standardised to the age and sex distribution in the TNFi cohort.
*Fully adjusted HR: adjusted for age, sex, line of therapy, for comorbidities, SES, disease-related factors and with missing categories included for those variables with missing information.
bDMARDs, biological disease-modifying antirheumatic drugs; JAKi, Janus kinase inhibitor; NMSC, non-melanoma skin cancer; RA, rheumatoid arthritis; SES, socioeconomic status; TNFi, tumour necrosis factor inhibitor.
Analyses by the previous number of b/tsDMARDs, and with a 90-day latency period, revealed HRs close to the main analysis (online supplemental tables S10 and S11). Furthermore, the HRs did not vary considerably when changing the main analysis from an ever-exposed model to a on drug model (online supplemental table S12). Also, multiple imputation for missing data and sensitivity analysis for COVID pandemic, respectively, did not appreciably alter the results of the main analysis (online supplemental tables S13 and S14).
In the CV risk-factor enriched subset outlined in online supplemental table S4, there were 17 incident cancers other than NMSC in JAKi cohort (n=543, 27% of the full cohort) and 79 in the TNFi cohort (n=1723, 23% of the full cohort), both corresponding to higher incidences than in the main analysis but a similar fully adjusted HR of 1.03 (95% CI 0.58 to 1.82) (online supplemental table S15). Comparing the 1551 and 6612 individuals in the JAKI and TNFi cohorts, respectively, who did not fulfil the inclusion criteria to the CV-enriched cohort, the adjusted HR was 0.88 (95% CI 0.53 to 1.45).
PsA: Occurrence and relative risk for cancer
There were 5 events of cancer other than NMSC in the JAKi cohort and 73 events in the TNFi cohort resulting in an adjusted HR of 1.88 (95% CI 0.68 to 5.16) for JAKi versus TNFi (table 4). For NMSC, the corresponding HR was 2.05 (95% CI 0.79 to 5.31) based on 8 events in the JAKi cohort and 73 events in the TNFi cohort. These HRs did not vary appreciably between successively adjusted models (online supplemental table S16).
Table 4.
Number of events, crude and standardised incidence rates and HR for all cancers other than NMSC and NMSC, in Swedish patients with PsA treated with JAKi
| Cohort | Events | Crude incidence rate per 1000 person-years | Standardised incidence rate per 1000 person-years | Fully adjusted HR* |
| All cancers other than NMSC | ||||
| JAKi | 5 | 8.6 | 7.3 | 1.88 (0.68 to 5.16) |
| Non-TNFi | 2 | 4.8 | – | – |
| TNFi | 73 | 5.8 | 5.8 | 1.0 (Reference) |
| Gen population | 317 | 5.9 | 6.0 | n/a |
| NMSC | ||||
| JAKi | 8 | 13.9 | 11.7 | 2.05 (0.79 to 5.31) |
| Non-TNFi | 2 | 4.8 | – | – |
| TNFi | 73 | 5.8 | 5.8 | 1.0 (Reference) |
| Gen population | 209 | 3.9 | 3.9 | n/a |
Non-TNFI includes rituximab, abatacept and tocilizumab. Estimated from proportional hazards Cox regression models. Standardised incidence rate standardised to the age- and sex distribution in the TNFi cohort. – is displayed when too few events (<5) were observed.
*Fully adjusted HR: adjusted for age, sex, line of therapy, for comorbidities, SES, disease-related factors and with missing categories included for those variables with missing information.
JAKi, Janus kinas inhibitor; n/a, not available; NMSC, non-melanoma skin cancer; PsA, psoriatic arthritis; SES, socioeconomic status; TNFi, tumour necrosis factor inhibitor.
Discussion
In this nationwide observational study of patients with RA or PsA initiating treatment with a JAKi (tofacitinib or baricitinib), non-TNFi bDMARD or a TNFi, we made several important observations: First, in patients with RA or PsA, the overall risk for cancer other than NMSC was not statistically significantly increased (JAKi vs TNFi) nor were there any clear trends towards increasing relative risks (RRs) by time since treatment start. Second, we found evidence of increased risk for NMSC (for RA) and a potential signal (for PsA) with JAKi, especially in the later follow-up strata although the trend over time was not formally statistically significant. For NMSC, the distributions of SCC and BCC were similar in the JAKi and in the bDMARD cohorts. Third, the risk-increase for NMSC (JAKi vs TNFi) was specific to JAKi and not mirrored by a similar increase for the class of non-TNFi bDMARDs. Fourth, in our RA population, we could not replicate the signal from the ORAL Surveillance trial of an increased risk of lung cancer with JAKi. Fifth, when restricting our analysis to CV risk-factor enriched patients, the incidence of cancer increased (as expected) but the HRs remained the same as in the main analysis (and qualitatively similar to the HR close to one among those without these risk factors).
Signals of cancer risks with JAKi have been documented in (overlapping) meta-analyses of JAKi trials. Wang et al included 20 clinical trials of which seven had information on cancer covering 8982 JAKi treated patients with RA and reported RR of cancer in the JAKi versus comparator arms of 1.68, 95% CI 0.57 to 4.95.24 Maneiro et al reported an OR for cancer other than NMSC in the tofacitinib versus placebo arms of 2.39 (95% CI 0.50 to 11.50).25 Oliviera et al assessed the association between JAKi and NMSC in 23 trials (13 tofacitinib, 4 baricitinib, 1 filgotinib and 7 upadacitinib trials) across indications; RA, psoriasis, inflammatory bowel disease and ankylosing spondylitis, including 26,334 JAKi-treated patients. Across indications, the RR of NMSC with JAKi versus comparator was 1.05 (95% CI 0.47 to 2.35). Oliviera et al also assessed the risk of cancers other than NMSC, in 33 phase 2–3 trials (20 tofacitinib, 5 baricitinib, 1 filgotinib and 7 upadacitinib trials) across the same indications, including 32 131 JAKi exposed patients, an reported an RR with JAKi versus placebo/comparator of 1.39 (95% CI 0.68 to 2.85). When RA was assessed as a separate indication (13 trials), the HR was HR 1.59 (95% CI 0.71 to 3.56).26 Solipuram et al focused on the cancer risk in patients with RA receiving combination therapy with methotrexate and JAKi in 13 randomised controlled trials (6911 patients) and reported that the addition of JAKi to MTX provided no statistically significant increased risk for malignancies excluding NMSC (RR 1.12, 95% CI 0.40 to 3.13) nor for NMSC (RR 1.44, 95% CI 0.36 to 5.76) compared with MTX monotherapy.21
The recent ORAL surveillance trial was a large, randomised, open-label, non-inferiority, postauthorisation and safety end-point trial with a median follow-up of 4.0 years, which included patients with active RA over 50 years of age with a least one CV risk factor. The results included a statistically significant 50% relative higher risk of cancer overall for tofacitinib compared with adalimumab/etanercept, including a signal for lung cancer (HR 2.17, 95% CI 0.95 to 4.93), and also a significantly increased risk of NMSC (HR 1.90, 95% CI 1.04 to 3.47).17 Our results do not offer any immediate support for an increased risk of cancer overall other than NMSC with JAKi (our upper 95% CI bound=1.38), and do not support the signal for lung cancer although precision for the latter estimate was limited. We did not note any major differences in HRs for tofacitinib (vs TNFi) and baricitinib (vs TNFi) although the upper 95% CI bounds in the drug-specific analysis encompassed clinically significant risk increases.
So far, other data on cancer risks with JAKi as used in clinical practice are scare. A US multicentre, observational register study (US Corrona RA registry) included 1999 patients initiating tofacitinib, with mean follow-up of 2.25 years, noted 28 events of malignancies excluding NMSC. They found neither an overall increase in the risk of cancer other than NMSC (HR 1.04, 95% CI 0.68 to 1.61) nor any increased risk of NMSC (HR 1.02, 95% CI 0.69 to 1.50) for tofacitinib versus other bDMARDs.23 Another US study, using claims data from three sources (Optum Clinformatics, IBM MarketScan Research Databases and Medicare) included a total of 83 296 patients with RA but found no increased risk of cancer with tofacitinib (HR 1.01 95% CI 0.83 to 1.22) compared with TNFi, nor any statistically significant increased risk of NMSC (HR 1.15, 95% CI 0.96 to 1.39) (though based on a mean follow-up time of less than 1 year).22
Limitations
Our study has some limitations. The median follow-up time for JAKi was somewhat short (1.95 years) due to their relatively recent introduction on the Swedish market. Also, while we could present results for the combined group of JAKi, drug-specific HRs were less precise, due to relatively few events for each specific JAKi. Furthermore, although we performed analyses restricted to subjects with CV risk factors, these restrictions were not identical to those in the ORAL surveillance study. Further restrictions (to RA disease activity, to concomitant csDMARDs, etc) would have removed the vast majority of all JAKi treated patients (indirectly demonstrating that the ORAL Surveillance trial is not directly comparable to patients in clinical practice). Also, the ORAL surveillance study consisted of patients treated with tofacitinib 5 mg or 10 mg two times per day. In Sweden, only the 5 mg two times per day dosage is used. Nevertheless, when restricting our RA cohort to a CV enriched subgroup the overall cancer risk other than NMSC with JAKi was not statistically significant increased, in this respect in line with the study by Khosrow-Khavar et al.22 There were differences in the characteristics between patients initiating a JAKi and those initiating a TNFi. Although we adjusted for several such factors, we cannot formally rule out residual or unmeasured confounding by indication.
Strengths
Strengths of our study include the use of nationwide, population-based prospective registers with high coverage and validity in which exposure (JAKi/bDMARD treatment) could be assessed independently of outcome (cancer), with a new-user design. This ensured the inclusion of the vast majority of all Swedish RA and PsA patients (without previous cancers) treated with b/tsDMARDs, and a statistical precision to rule out substantially increased overall cancer risks other than NMSC (upper 95% CI=1.38). We were additionally able to assess cancer risks overall and by the most common cancer sites and could study NMSC by type (BCC/SCC) and history, and found limited potential for channelling to or away from JAKi related to a history of NMSC. The inclusion of cohorts treated with non-TNFi bDMARDs, and the general population cohort, allowed us to put the observed rates and HRs with JAKi versus TNFi into context. Our finding of an increased risk of NMSC with JAKi, in a population already at increased risk of skin malignancies, underscores the importance of dermatological vigilance among these patients. In addition, we were able to assess the overall cancer risk, and risks for NMSC, in PsA treated with JAKi, which has not previously been presented.
Conclusion
In conclusion, among individuals with RA or PsA, we found no evidence of an increased short-term risk of all cancers other than NMSC for patients initiating JAKi compared with TNFi, but the risk of NMSC may be increased, at least in patients with RA. Although our results add to the concerns regarding the safety of JAKi with regard to NMSC, a causative biological mechanism remains to be determined and the risks must be viewed in light of the elevated risks for several other comorbidities and adverse outcomes in patients with active RA for whom alternative treatment options may not exist.
Footnotes
Handling editor: Josef S Smolen
Collaborators: The ARTIS Study Group conducts scientific analyses using data from the Swedish Biologics Register ARTIS, run by the Swedish Society for Rheumatology. The following were members of the ARTIS Study Group during study completion: Gerd-Marie Alenius (Department of Public Health and Clinical Medicine/Rheumatology, Umeå University), Eva Baecklund (Department of Medical Sciences, Uppsala University), Katerina Chatzidionysiou (Department of Medicine Solna, Karolinska Institutet), Nils Feltelius (Swedish Medical Products Agency, Department of Public Health and Caring Sciences, Uppsala University), Helena Forsblad-d’Elia (Department of Rheumatology and Inflammation Research, Sahlgrenska Academy, University of Gothenburg), Alf Kastbom (Department of Biomedical and Clinical Sciences, Linköping University), Lars Klareskog (Department of Medicine Solna, Karolinska Institutet), Ann Knight (Department of Medical Sciences, Uppsala University), Elisabet Lindqvist (Department of Clinical Sciences, Rheumatology, Lund University, Skåne University Hospital), Ulf Lindström (Department of Rheumatology and Inflammation Research, Sahlgrenska Academy, University of Gothenburg), Lotta Ljung (Department of Medicine Solna, Karolinska Institutet), Carl Turesson (Rheumatology, Department of Clinical Sciences, Malmö, Lund University), Christopher Sjöwall (Department of Biomedical and Clinical Sciences, Linköping University), and Johan Askling (Department of Medicine Solna, Karolinska Institutet).We also would like to thank all Swedish RA patients and rheumatologists for entering data into the Swedish Rheumatology Quality Register.
Contributors: VH is guarantor and accepts full responsibility for the work and/or the conduct of the study, had access to the data and controlled the decision to publish.VH, HB, KH, TF and JA had full access to all the data in the study and participated in the design of the study. HB and VH conducted the statistical analyses. All authors participated in designing the analyses and in the interpretation of the results. All authors contributed to the drafting of the manuscript.
Funding: This work was supported by funding from the Karolinska Institute Region Stockholm funds (ALF), the Swedish Research Council, the Swedish Cancer Society and the Swedish HeartLung Foundation. TF was supported by the Swedish Research Council (2021-01418).
Disclaimer: Funders had no impact on the design or interpretation of the study or its results.
Competing interests: VH and KH have no competing interests to declare. JA has had or have research agreements with Abbvie, Astra-Zeneca, BMS, Eli Lilly, MSD, Pfizer, Roche, Samsung Bioepis, Sanofi, and UCB, mainly in the context of safety monitoring of biologics via ARTIS/Swedish Biologics Register. TF and HB are partly employed by the ARTIS project.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
Collaborators: behalf of the ARTIS group, Gerd-Marie Ahlenius, Eva Baecklund, Katerina Chatzidionysiou, Nils Feltelius, Helena Forsblad-d’Elia, Alf Kastbom, Lars Klareskog, Elisabet Lindqvist, Ulf Lindström, Carl Turesson, Christopher Sjöwall, and Johan Askling
Data availability statement
The data in this study is part of a linkage between registers performed by Karolinska Institutet. Further sharing of the data is limited due to legal restrictions.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was approved by the Swedish Ethics Review Authority 2015-1844-31.
References
- 1. Zintzaras E, Voulgarelis M, Moutsopoulos HM. The risk of lymphoma development in autoimmune diseases: a meta-analysis. Arch Intern Med 2005;165:2337–44. 10.1001/archinte.165.20.2337 [DOI] [PubMed] [Google Scholar]
- 2. Lopez-Olivo MA, Tayar JH, Martinez-Lopez JA, et al. Risk of malignancies in patients with rheumatoid arthritis treated with biologic therapy: a meta-analysis. JAMA 2012;308:898–908. 10.1001/2012.jama.10857 [DOI] [PubMed] [Google Scholar]
- 3. Wu X, Peng H, Wen Y, et al. Rheumatoid arthritis and risk of lung cancer: meta-analysis and mendelian randomization study. Semin Arthritis Rheum 2021;51:565–75. 10.1016/j.semarthrit.2021.03.015 [DOI] [PubMed] [Google Scholar]
- 4. Chakravarty EF, Michaud K, Wolfe F. Skin cancer, rheumatoid arthritis, and tumor necrosis factor inhibitors. J Rheumatol 2005;32:2130–5. [PubMed] [Google Scholar]
- 5. Egeberg A, Thyssen JP, Gislason GH, et al. Skin cancer in patients with psoriasis. J Eur Acad Dermatol Venereol 2016;30:1349–53. 10.1111/jdv.13619 [DOI] [PubMed] [Google Scholar]
- 6. Strangfeld A, Hierse F, Rau R, et al. Risk of incident or recurrent malignancies among patients with rheumatoid arthritis exposed to biologic therapy in the German biologics register rabbit. Arthritis Res Ther 2010;12:R5. 10.1186/ar2904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Aaltonen KJ, Joensuu JT, Virkki L, et al. Rates of serious infections and malignancies among patients with rheumatoid arthritis receiving either tumor necrosis factor inhibitor or rituximab therapy. J Rheumatol 2015;42:372–8. 10.3899/jrheum.140853 [DOI] [PubMed] [Google Scholar]
- 8. Askling J, Fored CM, Brandt L, et al. Risks of solid cancers in patients with rheumatoid arthritis and after treatment with tumour necrosis factor antagonists. Ann Rheum Dis 2005;64:1421–6. 10.1136/ard.2004.033993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dreyer L, Mellemkjær L, Andersen AR, et al. Incidences of overall and site specific cancers in TNFα inhibitor treated patients with rheumatoid arthritis and other arthritides-a follow-up study from the DANBIO registry. Ann Rheum Dis 2013;72:79–82. 10.1136/annrheumdis-2012-201969 [DOI] [PubMed] [Google Scholar]
- 10. van Vollenhoven RF, Fleischmann RM, Furst DE, et al. Longterm safety of rituximab: final report of the rheumatoid arthritis global clinical trial program over 11 years. J Rheumatol 2015;42:1761–6. 10.3899/jrheum.150051 [DOI] [PubMed] [Google Scholar]
- 11. Slimani S, Lukas C, Combe B, et al. Rituximab in rheumatoid arthritis and the risk of malignancies: report from a french cohort. Joint Bone Spine 2011;78:484–7. 10.1016/j.jbspin.2010.11.012 [DOI] [PubMed] [Google Scholar]
- 12. Huss V, Bower H, Wadström H, et al. Short- and longer-term cancer risks with biologic and targeted synthetic disease-modifying antirheumatic drugs as used against rheumatoid arthritis in clinical practice. Rheumatology (Oxford) 2022;61:1810–8. 10.1093/rheumatology/keab570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wadström H, Frisell T, Askling J, et al. Malignant neoplasms in patients with rheumatoid arthritis treated with tumor necrosis factor inhibitors, tocilizumab, abatacept, or rituximab in clinical practice: a nationwide cohort study from Sweden. JAMA Intern Med 2017;177:1605–12. 10.1001/jamainternmed.2017.4332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hodge JA, Kawabata TT, Krishnaswami S, et al. The mechanism of action of tofacitinib-an oral Janus kinase inhibitor for the treatment of rheumatoid arthritis. Clin Exp Rheumatol 2016;34:318–28. [PubMed] [Google Scholar]
- 15. van Vollenhoven R, Lee EB, Strengholt S, et al. Evaluation of the short-, mid-, and long-term effects of tofacitinib on lymphocytes in patients with rheumatoid arthritis. Arthritis Rheumatol 2019;71:685–95. 10.1002/art.40780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ghoreschi K, Jesson MI, Li X, et al. Modulation of innate and adaptive immune responses by tofacitinib (CP-690,550). J Immunol 2011;186:4234–43. 10.4049/jimmunol.1003668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ytterberg SR, Bhatt DL, Mikuls TR, et al. Cardiovascular and cancer risk with tofacitinib in rheumatoid arthritis. N Engl J Med 2022;386:316–26. 10.1056/NEJMoa2109927 [DOI] [PubMed] [Google Scholar]
- 18. Curtis JR, Lee EB, Kaplan IV, et al. Tofacitinib, an oral Janus kinase inhibitor: analysis of malignancies across the rheumatoid arthritis clinical development programme. Ann Rheum Dis 2016;75:831–41. 10.1136/annrheumdis-2014-205847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mariette X, Chen C, Biswas P, et al. Lymphoma in the tofacitinib rheumatoid arthritis clinical development program. Arthritis Care Res (Hoboken) 2018;70:685–94. 10.1002/acr.23421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cohen SB, Tanaka Y, Mariette X, et al. Long-term safety of tofacitinib for the treatment of rheumatoid arthritis up to 8.5 years: integrated analysis of data from the global clinical trials. Ann Rheum Dis 2017;76:1253–62. 10.1136/annrheumdis-2016-210457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Solipuram V, Mohan A, Patel R, et al. Effect of Janus kinase inhibitors and methotrexate combination on malignancy in patients with rheumatoid arthritis: a systematic review and meta-analysis of randomized controlled trials. Auto Immun Highlights 2021;12:8. 10.1186/s13317-021-00153-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Khosrow-Khavar F, Desai RJ, Lee H, et al. Tofacitinib and risk of malignancy: results from the safety of tofacitinib in routine care patients with rheumatoid arthritis (STAR-RA) study. Arthritis Rheumatol 2022;74:1648–59. 10.1002/art.42250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Kremer JM, Bingham CO, Cappelli LC, et al. Postapproval comparative safety study of tofacitinib and biological disease-modifying antirheumatic drugs: 5-year results from a united states-based rheumatoid arthritis registry. ACR Open Rheumatol 2021;3:173–84. 10.1002/acr2.11232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang F, Sun L, Wang S, et al. Efficacy and safety of tofacitinib, baricitinib, and upadacitinib for rheumatoid arthritis: a systematic review and meta-analysis. Mayo Clin Proc 2020;95:1404–19. 10.1016/j.mayocp.2020.01.039 [DOI] [PubMed] [Google Scholar]
- 25. Maneiro JR, Souto A, Gomez-Reino JJ. Risks of malignancies related to tofacitinib and biological drugs in rheumatoid arthritis: systematic review, meta-analysis, and network meta-analysis. Semin Arthritis Rheum 2017;47:149–56. 10.1016/j.semarthrit.2017.02.007 [DOI] [PubMed] [Google Scholar]
- 26. Olivera PA, Lasa JS, Bonovas S, et al. Safety of janus kinase inhibitors in patients with inflammatory bowel diseases or other immune-mediated diseases: a systematic review and meta-analysis. Gastroenterology 2020;158:1554–73. 10.1053/j.gastro.2020.01.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
ard-2022-223636supp001.pdf (190.4KB, pdf)
Data Availability Statement
The data in this study is part of a linkage between registers performed by Karolinska Institutet. Further sharing of the data is limited due to legal restrictions.