Abstract
Background
The optimal revascularization strategy in patients with left main coronary artery (LMCA) disease in the emergency setting is still controversial. Thus, we aimed to compare the outcomes of percutaneous coronary interventions (PCI) vs. coronary artery bypass grafting (CABG) in patients with and without emergent LMCA disease.
Methods
This retrospective cohort study included 2138 patients recruited from 14 centers between 2015 and 2019. We compared patients with emergent LMCA revascularization who underwent PCI (n = 264) to patients who underwent CABG (n = 196) and patients with non-emergent LMCA revascularization with PCI (n = 958) to those who underwent CABG (n = 720). The study outcomes were in-hospital and follow-up all-cause mortality and major adverse cardiovascular and cerebrovascular events (MACCE).
Results
Emergency PCI patients were older and had a significantly higher prevalence of chronic kidney disease, lower ejection fraction, and higher EuroSCORE than CABG patients. CABG patients had significantly higher SYNTAX scores, multivessel disease, and ostial lesions. In patients presenting with arrest, PCI had significantly lower MACCE (P = 0.017) and in-hospital mortality (P = 0.016) than CABG. In non-emergent revascularization, PCI was associated with lower MACCE in patients with low (P = 0.015) and intermediate (P < 0.001) EuroSCORE. PCI was associated with lower MACCE in patients with low (P = 0.002) and intermediate (P = 0.008) SYNTAX scores. In non-emergent revascularization, PCI was associated with reduced hospital mortality in patients with intermediate (P = 0.001) and high (P = 0.002) EuroSCORE compared to CABG. PCI was associated with lower hospital mortality in patients with low (P = 0.031) and intermediate (P = 0.001) SYNTAX scores. At a median follow-up time of 20 months (IQR: 10–37), emergency PCI had lower MACCE compared to CABG [HR: 0.30 (95% CI 0.14–0.66), P < 0.003], with no significant difference in all-cause mortality between emergency PCI and CABG [HR: 1.18 (95% CI 0.23–6.08), P = 0.845].
Conclusions
PCI could be advantageous over CABG in revascularizing LMCA disease in emergencies. PCI could be preferred for revascularization of non-emergent LMCA in patients with intermediate EuroSCORE and low and intermediate SYNTAX scores.
Keywords: Emergency PCI, Emergency CABG, ULMCA, Outcomes, Gulf
Background
Left main coronary artery (LMCA) disease represents a highly morbid condition with a poor prognosis if not revascularized [1]. Furthermore, infarction related to LMCA disease is associated with a high myocardial jeopardy score and extensive ischemia to multiple large coronary territories. It, therefore, carries an increased risk of complications, including left ventricular (LV) systolic dysfunction, cardiogenic shock, and death [2]. Historically, revascularization with coronary artery bypass grafting (CABG) has been the gold standard for LMCA disease in stable coronary artery disease (CAD). With current stent technology and guideline-based acute coronary syndrome (ACS) management, percutaneous coronary intervention (PCI) revascularization for the left-main disease is now considered non-inferior to CABG in patients with stable CAD and low to intermediate SYNTAX scores [2, 3]. Published reports indicated that patients undergoing PCI revascularization for unprotected LMCA disease are increasing, and CABG procedures are decreasing [4].
The number of patients with LMCA disease and high anatomical complexity included in randomized controlled trials is low because they are usually excluded [5]. Consequently, the risk estimates and confidence intervals are imprecise; however, they suggest a trend toward better survival with CABG [3]. There is a paucity of data to guide left-main revascularization in emergency presentations, including cardiac arrest and cardiogenic shock complicating acute myocardial infarction. The optimal revascularization strategies in emergent and non-emergent LMCA revascularization have not been thoroughly evaluated. Considering this gap in the evidence, we conducted this study to analyze the outcomes of reperfusion strategies (PCI versus CABG) for emergent and non-emergent LMCA disease.
Methods
Study design, patient population
The Gulf left-main registry contains data about LMCA revascularization with either PCI or CABG from 14 cardiac centers in the Gulf Area [6, 7]. Patients were recruited from January 2015 to December 2019. A total of 2657 patients with significant LMCA disease were identified. The registry included 2138 patients with unprotected left-main coronary artery (ULMCA) disease; 460 had emergent, and 1678 had non-emergent revascularization. We compared patients with emergent LMCA disease who had PCI (n = 264) to CABG patients (n = 196) and patients with non-emergent LMCA who had PCI (n = 958) to those who had CABG (n = 720). We excluded patients with previous LMCA PCI (n = 37), Unprotected LMCA treated medically (n = 193), concomitant valvular or aortic surgery (n = 115), and those with protected LMCA disease with patent grafts (n = 174).
Definitions
The emergent LMCA revascularization group included all ST-elevation myocardial infarction (STEMI) cases and high-risk non-ST-elevation acute coronary syndrome (NSTE-ACS). High-risk NSTE-ACS included patients in cardiac arrest and/or cardiogenic shock. The non-emergent LMCA revascularization group included all remaining patients who underwent LMCA revascularization.
Significant LMCA disease was defined as luminal stenosis greater than 50%.
Unprotected LMCA disease was defined as LMCA disease without previous bypass grafts to either the left anterior descending (LAD) or circumflex coronary artery.
Preprocedural patient risk stratification was performed using the European System for Cardiac Operative Risk Evaluation (EuroSCORE II) [8]. The EuroSCORE II is divided into three categories [low score (0–2), medium (3–5) and high (≥ 6)].
The SYNTAX score was used to score the angiographic lesions [9]. The SYNTAX score was divided into three groups [low score (≤ 22), intermediate (23–32), and high (> 33)].
Medina classification was used for LM bifurcation lesions [10].
Bleeding events were defined according to the International Society of Thrombosis and Hemostasis (ISTH) Scientific and Standardization Committee's (SSC) statement [11, 12].
Clinical assessment and clinical follow-up
The data pertaining to the patient's demographics, presentation, medications at the time of discharge, and in-patient and follow-up outcomes were analyzed in both emergent and non-emergent LMCA revascularization procedures. Clinical outcomes included hospital and follow-up all-cause mortality and major adverse cardiac and cerebrovascular events (MACCEs). MACCEs included the composite endpoint of myocardial infarction (MI), cerebrovascular events, target lesion revascularization, target vessel revascularization, and cardiac or noncardiac mortality. The mechanism by which follow-up events were recorded was based either on ICD coding diagnosis or on clinical description based on clinical diagnosis by admitting physicians in the electronic health record (EHR).
Ethical approval
This study was approved by the Institutional Review Board of King Faisal Specialist Hospital and Research Center in Riyadh (12-November 2020—RAC # 2201226: Gulf-LM Registry) and was carried out per local guidelines and ethical guidelines of the Declaration of Helsinki [13]. The IRB waived informed consent for this study due to its retrospective and observational nature and the absence of any patient-identifying information.
Statistical analysis
Stata 17 (Stata Corp- College Station- TX- USA) was used for all analyses. Quantitative data were evaluated for normality distribution using the Shapiro‒Wilk test, and normally distributed variables were compared using the Student t-test and presented as the mean and standard deviation. Skewed quantitative data were expressed as the median (interquartile range) and compared with the Wilcoxon test. Qualitative data were expressed as numbers and percentages and compared with the Chi-squared or Fisher's exact test if the expected frequency was less than five. The distribution of time-to-event outcomes (MACCE and survival) was plotted using Kaplan‒Meier curves and compared with the log-rank test. Multivariable logistic regression analysis was used to evaluate factors associated with hospital MACCE and mortality in both emergent and non-emergent LMCA revascularization separately. Data were grouped into four models; baseline data, presentations, EuroSCORE, and SYNTAX score. Univariable logistic regression analysis was performed, and all variables were included in a stepwise forward selection regression model. Significant variables were retained in the final model. The interaction between PCI/CABG and presentation, EuroSCORE, or SYNTAX score was evaluated. The odds ratio and its 95% confidence interval, and P-values were reported. Collinearity was tested with the variance inflation factor (VIF), and all variables included in the model had VIF < 1.5. Multivariable Cox regression analysis was used to evaluate factors associated with the time-to-event outcomes (MACCE and survival). Stepwise forward selection was used, and a P < 0.05 was used to retain the variables in the final model. The model contained all patients with emergent and non-emergent LMCA revascularization, and the interaction between emergent/non-emergent revascularization and the technique (PCI vs. CABG) was evaluated in the final model. All preoperative and angiographic variables were included. The hazard ratio and its 95% confidence interval and P-value were reported. A P-value of less than 0.05 was considered statistically significant.
Results
Preprocedural and procedural technique and lesion characteristics
In the emergent LMCA revascularization group, patients who underwent PCI were older and had a significantly higher prevalence of chronic kidney disease than those who underwent CABG. Peripheral arterial disease was more common in patients with non-emergent PCI than non-emergent CABG. The EuroSCORE II was significantly higher in patients with PCI than those with CABG (Table 1).
Table 1.
Comparison of the baseline demographics between patients who had emergency left main (LM) and non-emergency LM revascularization
| Overall, n = 2138 | Emergent LM revascularization n = 460 (21.5%) | P-Value | Non-emergent LM revascularization n = 1678 (78.5%) | P Value | |||
|---|---|---|---|---|---|---|---|
| PCI (n = 264) | CABG (n = 196) | PCI (n = 958) | CABG (n = 720) | ||||
| Baseline characteristics | |||||||
| Age (years), median (IQR) | 64 (57–70) | 63 (56–72) | 60 (54- 68) | 0.004 | 66 (60–72) | 62 (55–69) | < 0.001 |
| Body mass index (kg/m2), median (IQR) | 28 (25- 32) | 28 (25–31) | 28 (25–30) | 0.269 | 29 (26–33) | 28 (25–31) | < 0.001 |
| Gender (male), n (%) | 1678 (78.5%) | 202 (76.52%) | 170 (86.73%) | 0.006 | 692 (7223%) | 614 (85.28%) | < 0.001 |
| Smoker, n (%) | 849 (39.7%) | 85 (32.20%) | 83 (42.35%) | 0.025 | 394 (41.13%) | 287 (39.86%) | 0.601 |
| Diabetes mellitus, n (%) | 1468 (68.7%) | 185 (70.08%) | 139 (70.92%) | 0.845 | 619 (64.61%) | 525 (72.92%) | < 0.001 |
| Hypertension, n (%) | 1495 (70.4%) | 173 (65.78%) | 122 (62.24%) | 0.434 | 686 (72.67%) | 514 (71.39%) | 0.564 |
| Dyslipidemia, n (%) | 1463 (69.0%) | 179 (68.06%) | 125 (63.78%) | 0.337 | 642 (68.15%) | 517 (71.81%) | 0.108 |
| Congestive heart failure, n (%) | 261 (12.2%) | 44 (16.67%) | 23 (11.73%) | 0.138 | 152 (15.87%) | 42 (5.83%) | < 0.001 |
| Peripheral arterial disease, n (%) | 246 (11.5%) | 28 (10.61%) | 20 (10.20%) | 0.889 | 156 (16.28%) | 42 (5.83%) | < 0.001 |
| Cerebral vascular accident, n (%) | 222 (10.4%) | 30 (11.36%) | 11 (5.61%) | 0.032 | 149 (15.55%) | 32 (4.44%) | < 0.001 |
| Chronic kidney disease, n (%) | 437 (20.4%) | 62 (23.48%) | 29 (14.80%) | 0.021 | 254 (26.51%) | 92 (12.78%) | < 0.001 |
| Atrial fibrillation, n (%) | 183 (8.6%) | 27 (10.23%) | 12 (6.12%) | 0.118 | 127 (13.26%) | 17 (2.36%) | < 0.001 |
| Previous myocardial infarction, n (%) | 613 (28.7%) | 84 (31.82%) | 60 (30.61%) | 0.783 | 334 (34.86%) | 135 (18.75%) | < 0.001 |
| EuroSCORE, median (IQR) | 2.9 (1.26–4.56) | 3.9 (2.01–7) | 2.45 (1.27–5) | < 0.001 | 1.75 (1.04–3.65) | 3.65 (1.6–4.65) | < 0.001 |
CABG: coronary artery bypass graft surgery, PCI: percutaneous coronary intervention, EuroSCORE score: European system for cardiac operative risk evaluation, IQR: interquartile range
Eighteen patients (1%) presented with cardiac arrest (50% ventricular fibrillation), 82 (3.8%) with cardiogenic shock, and 52 (2.4%) with both. Ninety-five percent of cardiac arrests occurred in-hospital, and 95% of cardiogenic shocks occurred pre-revascularization. More patients in cardiogenic shock and cardiac arrest had PCI. Three hundred eighty-nine patients (84.6%) presented with STEMI; 81 (21%) were in cardiogenic shock and cardiac arrest. Seventy-one (15.4%) patients presented with high-risk (arrest and shock) non-ST-elevation acute coronary syndrome (NSTE-ACS). While more patients with STEMI underwent CABG, more patients presenting with NSTE-ACS underwent PCI. Patients who underwent PCI had significantly lower left ventricular ejection fractions than those who underwent CABG (Table 2). The most frequently observed anatomical pattern was Medina 1,1,1 lesion (35.5%), followed by 1,1,0 (18.8%). Patients who underwent CABG had significantly higher SYNTAX scores, multivessel disease, and ostial lesions. However, PCI patients had significantly lower SYNTAX scores and more isolated LMCA disease or LMCA with either single or double-vessel disease and distal bifurcation lesions (Table 3).
Table 2.
Comparison of the hospital presentation between patients who had emergency left main (LM) vs. non-emergency LM revascularization
| Overall, n = 2138 | Emergent LM revascularization n = 460 (21.5%) | P-Value | Non-emergent LM revascularization n = 1678 (78.5%) | P Value | |||
|---|---|---|---|---|---|---|---|
| PCI (n = 264) | CABG (n = 196) | PCI (n = 958) | CABG (n = 720) | ||||
| Hospital presentation | |||||||
| Cardiac arrest, n (%) | 18 (1%) | 7 (2.65%) | 11 (5.61%) | 0.105 | NA | NA | NA |
| Types, n (%) | |||||||
| Ventricular fibrillation | 9 (50%) | 2 (28.57%) | 7 (63.64%) | 0.335 | NA | NA | NA |
| Pulseless electrical activity | 6 (33.3%) | 3 (42.86%) | 3 (27.27%) | 0.627 | NA | NA | NA |
| Asystole | 3 (16%) | 2 (28.57%) | 1 (9.09%) | 0.528 | NA | NA | NA |
| Location, n (%) | |||||||
| Out of hospital cardiac arrest (OHCA) | 1 (5.5%) | 1 (14.29%) | 0 | 0.389 | NA | NA | NA |
| In-hospital cardiac arrest (IHCA) | 17 (94.5%) | 6 (85.71%) | 11 (100%) | 0.389 | NA | NA | NA |
| Timing, n (%) | |||||||
| Pre coronary angiography | 18 (100%) | 7 (100%) | 11 (100%) | > 0.99 | NA | NA | NA |
| Post coronary angiography | 0 (0%) | 0 | 0 | > 0.99 | NA | NA | NA |
| Cardiogenic shock and cardiac arrest, n (%) | 52 (2.4%) | 44 (16.67%) | 8 (4.08%) | < 0.001 | |||
| Timing, n (%) | |||||||
| Pre coronary angiography | 47 (90.4%) | 43 (97.73%) | 4 (50%) | 0.001 | NA | NA | NA |
| Post coronary angiography | 5 (9.6%) | 1 (2.27%) | 4 (50%) | 0.001 | NA | NA | NA |
| Cardiogenic shock, n (%) | 82 (3.8%) | 57 (21.59%) | 25 (12.76%) | 0.014 | NA | NA | NA |
| Timing, n (%) | |||||||
| Pre coronary angiography | 78 (95%) | 57 (100%) | 21 (84%) | 0.007 | NA | NA | NA |
| Post coronary angiography | 4 (5%) | 0 | 4 (16%) | 0.007 | NA | NA | NA |
| Coronary presentation, n (%) | |||||||
| ST-elevation myocardial infarction | 389 (18.2%) | 214 (81.06%) | 175 (89.29%) | 0.016 | NA | NA | NA |
| Non-ST-elevation acute coronary syndrome | 1084 (50.7%) | 50 (18.93%) | 21 (10.71%) | 0.034 | 578 (60.33%) | 435 (60.41%) | 0.868 |
| Stable coronary artery disease | 273 (12.77%) | NA | NA | NA | 137 (14.32%) | 136 (18.89%) | 0.012 |
| Silent ischemia/others | 380 (17.78%) | NA | NA | NA | 234 (24.45%) | 146 (20.28%) | 0.043 |
| Left ventricular ejection fraction, mean (SD) | 44.8 ± 11.6 | 40 (35–45) | 50 (40–55) | < 0.001 | 45 (35–55) | 50 (40–55) | < 0.001 |
| LVEF ≤ 40%, n (%) | 578 (27.0%) | 98 (37.12%) | 33 (16.84%) | < 0.001 | 291 (30.38%) | 156 (21.67%) | < 0.001 |
| LVEF 41–49%, n (%) | 618 (28.91%) | 101 (38.26%) | 48 (24.49%) | 0.002 | 286 (29.85%) | 183 (25.42%) | 0.045 |
| LVEF ≥ 50%, n (%) | 942 (44.1%) | 65 (24.62%) | 115 (58.67%) | < 0.001 | 381 (39.77%) | 381 (52.92%) | < 0.001 |
| Creatinine clearance (ml/min), mean (SD) | 76.2 ± 24.2 | 90 (62–90) | 83 (65–90) | 0.016 | 90 (53–93) | 83 (70–90) | 0.002 |
| Hemoglobin (g/L), median (IQR) | 13.4 (12–14.6) | 13.4 (12.2–14.6) | 13 (11.5–14.5) | 0.012 | 13.6 (12.3–14.9) | 13.2 (11.7–14.3) | < 0.001 |
SD: standard deviation, CABG: coronary artery bypass graft surgery, PCI: percutaneous coronary intervention,, IQR: interquartile range, LVEF: left ventricular ejection fraction
Table 3.
Comparison of the angiographic and procedural data between patients who had emergency left main (LM) vs. non-emergency LM revascularization
| Overall, n = 2138 | Emergent LM revascularization n = 460 (21.5%) | P-Value | Non-emergent LM revascularization n = 1678 (78.5%) | P Value | |||
|---|---|---|---|---|---|---|---|
| PCI (n = 264) | CABG (n = 196) | PCI (n = 958) | CABG (n = 720) | ||||
| Angiographic characteristics | |||||||
| Medina classification, n (%) | < 0.001 | < 0.001 | |||||
| 1,1,1 | 760 (35.5%) | 74 (28.03%) | 62 (31.63%) | 0.402 | 356 (37.16%) | 268 (37.22%) | 0.979 |
| 1,0,1 | 162 (7.6%) | 11 (4.17%) | 28 (14.29%) | < 0.001 | 37 (3.86%) | 86 (11.94%) | < 0.001 |
| 0,1,1 | 393 (18.4%) | 79 (29.92%) | 45 (22.96%) | 0.096 | 153 (15.97%) | 116 (16.11%) | 0.938 |
| 1,1,0 | 402 (18.8%) | 60 (22.73%) | 11 (5.61%) | < 0.001 | 250 (26.10%) | 81 (11.25%) | < 0.001 |
| 1,0,0 | 202 (9.4%) | 20 (7.58%) | 23 (11.73%) | 0.130 | 96 (10.02%) | 81 (11.25%) | 0.417 |
| 0,1,0 | 160 (7.5%) | 11 (4.17%) | 19 (9.69%) | 0.016 | 45 (4.70%) | 85 (11.81%) | < 0.001 |
| 0,0,1 | 59 (2.7%) | 9 (3.41%) | 8 (4.08%) | 0.689 | 21 (2.19%) | 21 (2.92%) | 0.347 |
| Lesion characteristics | |||||||
| Isolated left main disease, n (%) | 138 (6.5%) | 22 (8.3%) | 12 (6.1%) | < 0.001 | 81 (8.5%) | 23 (3.2%) | < 0.001 |
| LM + (triple-vessel disease), n (%) | 1202 (56.2%) | 98 (37.1%) | 124 (63.3%) | < 0.001 | 481 (50.2%) | 499 (69.3%) | < 0.001 |
| LM + (LAD and LCx), n (%) | 327 (15.3%) | 50 (18.9%) | 27 (13.8%) | < 0.001 | 138 (14.4%) | 112 (15.6%) | < 0.001 |
| LM + [RCA and (LAD or LCx)], n (%) | 139 (6.5%) | 20 (7.6%) | 25 (12.8%) | < 0.001 | 44 (4.6%) | 50 (6.9%) | < 0.001 |
| LM + LAD, n (%) | 287 (13.4%) | 63 (23.9%) | 8 (4.1%) | < 0.001 | 188 (19.6%) | 28 (3.9%) | < 0.001 |
| LM + LCx, n (%) | 35 (1.6%) | 10 (3.8%) | 0 (0.0%) | < 0.001 | 20 (2.1%) | 5 (0.7%) | < 0.001 |
| LM + RCA, n (%) | 10 (0.5%) | 1 (0.4%) | 0 (0.0%) | 0.99 | 6 (0.6%) | 3 (0.4%) | 0.740 |
| SYNTAX score | < 0.001 | < 0.001 | |||||
| Low (≤ 22), n (%) | 430 (20.2%) | 81 (30.68%) | 18 (9.18%) | < 0.001 | 223 (23.30%) | 108 (15.17%) | < 0.001 |
| Intermediate (23–32), n (%) | 1107 (52.0%) | 104 (39.39%) | 83 (42.35%) | 0.524 | 577 (60.29%) | 343 (48.17%) | < 0.001 |
| High (≥ 33), n (%) | 592 (27.8%) | 79 (29.92%) | 95 (48.47%) | < 0.001 | 157 (16.41%) | 261 (36.66%) | < 0.001 |
| SYNTAX score, median (IQR) | 28 (24–33) | 28 (22–33) | 32 (25–37) | < 0.001 | 28 (23–32) | 29 (25–35) | < 0.001 |
| Lesion location | |||||||
| Ostial/shaft only, n (%) | 536 (25.1%) | 51 (19.32%) | 59 (30.10%) | 0.007 | 184 (19.21%) | 242 (33.61%) | < 0.001 |
| Distal bifurcation, n (%) | 1602 (74.9%) | 213 (80.68%) | 137 (69.90%) | 0.007 | 774 (80.79%) | 478 (66.39%) | < 0.001 |
| Procedure | |||||||
| Intra-aortic ballon pump, n (%) | 200 (9.4%) | 62 (23.48%) | 52 (26.53%) | 0.454 | 36 (3.76%) | 50 (6.94%) | 0.003 |
| Impella, n (%) | 14 (0.7%) | 6 (2.27%) | 1 (0.51%) | 0.247 | 6 (0.63%) | 1 (0.14%) | 0.250 |
CABG: coronary artery bypass graft surgery, PCI: percutaneous coronary intervention, LM: left main, LAD: left anterior descending, LCX: left circumflex, RCA: right coronary, SYNTAX: The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery, IQR: interquartile range
Procedural technique
All PCIs were performed using second-generation DESs (drug-eluting stents). The most common type of stent used was the XIENCE family (Abbott Vascular- Santa Clara, CA, USA) of everolimus-eluting coronary stent systems (65%). The most common PCI approach in emergency LMCA revascularization patients was the planned 2-stent strategy (80%). The most frequently performed type of CABG in emergency LMCA revascularization was conventional CABG (on-pump), accounting for 85% of patients. The left internal mammary artery was used in 98%, double mammary arteries in 5%, and radial conduits in 1% of cases, whereas 99% of patients received venous grafts.
Discharge and follow-up medications
In emergent LMCA revascularization, patients who underwent PCI were more frequently discharged on P2Y12, beta-blockers, statins, and ACEi/ARBs (angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers). No difference was seen in either type of revascularization strategy concerning aspirin (ASA) on discharge (Table 4). A similar pattern was observed at follow-up for P2Y12 inhibitors and ACEi/ARBs. ASA was more common in CABG patients than PCI patients (p = 0.032). No difference was observed between PCI and CABG patients concerning beta-blockers or statin prescriptions at discharge (Table 4).
Table 4.
Comparison of the medications during discharge and follow-up between patients who had emergency left main (LM) vs. non-emergency LM revascularization
| Overall, n = 2138 | Emergent LM revascularization n = 460 (21.5%) | P-Value | Non-emergent LM revascularization n = 1678 (78.5%) | P Value | |||
|---|---|---|---|---|---|---|---|
| PCI (n = 264) | CABG (n = 196) | PCI (n = 958) | CABG (n = 720) | ||||
| Discharge medications | |||||||
| ASA, n (%) | 2010 (99.10%) | 222 (99.55%) | 166 (97.65%) | 0.095 | 946 (99.58%) | 676 (98.69%) | 0.045 |
| P2Y12 inhibitors, n (%) | 1833 (90.40%) | 223 (100%) | 129 (75.88%) | < 0.001 | 946 (99.58%) | 535 (78.10%) | < 0.001 |
| Beta blocker, n (%) | 1914 (94.40%) | 216 (96.86%) | 146 (85.88%) | < 0.001 | 915 (96.32%) | 637 (92.99%) | 0.003 |
| Statin, n (%) | 1934 (95.40%) | 214 (95.96%) | 139 (81.76%) | < 0.001 | 947 (99.68%) | 634 (92.55%) | < 0.001 |
| ACE inhibitors or ARB, n (%) | 1516 (74.80%) | 202 (90.58%) | 86 (50.59%) | < 0.001 | 847 (89.16%) | 381 (55.62%) | < 0.001 |
| Medications during follow-up | |||||||
| ASA, n (%) | 1713 (97.10%) | 174 (96.67%) | 135 (100%) | 0.032 | 859 (97.50%) | 545 (95.78%) | 0.068 |
| P2Y12 inhibitors, n (%) | 1129 (64.00%) | 140 (77.78%) | 83 (61.48%) | 0.002 | 638 (72.42%) | 268 (47.10%) | < 0.001 |
| Beta blocker, n (%) | 1674 (94.80%) | 171 (95.00%) | 129 (95.56%) | 0.819 | 838 (95.12%) | 536 (94.20%) | 0.443 |
| Statin, n (%) | 1727 (97.80%) | 174 (96.67%) | 130 (96.30%) | 0.859 | 873 (99.09%) | 550 (96.66%) | 0.001 |
| ACE inhibitors or ARB, n (%) | 1332 (75.50%) | 159 (88.33%) | 71 (52.59%) | < 0.001 | 765 (86.83%) | 337 (59.23%) | < 0.001 |
ASA: aspirin, ACE: angiotensin-converting enzyme, ARB: angiotensin II receptor blocker, CABG: coronary artery bypass grafting, PCI: percutaneous coronary intervention
In-hospital events
Univariable analysis was used to compare hospital events between PCI and CABG in patients with emergent and non-emergent revascularization. The emergent LMCA revascularization group had higher cardiac mortality (59/460, 12.8%) and total mortality (66/460, 14.35%) without a significant difference between PCI and CABG patients. There was no significant difference between PCI and CABG patients concerning MACCEs. The non-emergent LMCA revascularization group had lower cardiac mortality (22/1678, 1.3%) and total mortality (39/1678, 2.3%). CABG patients reported a higher mortality rate than PCI patients. MACCE and noncardiac mortality were significantly higher in CABG patients than PCI patients. In both the emergent and non-emergent LMCA revascularization groups, hospital stay was significantly longer in CABG patients (Table 5).
Table 5.
Comparison of the hospital and follow-up events between patients who had emergency left main (LM) and non-emergency LM revascularization
| Overall, n = 2138 | Emergent LM revascularization n = 460 (21.5%) | P-Value | Non-emergent LM revascularization n = 1678 (78.5%) | P Value | |||
|---|---|---|---|---|---|---|---|
| PCI (n = 264) | CABG (n = 196) | PCI (n = 958) | CABG (n = 720) | ||||
| In-hospital events | |||||||
| Cardiac death, n (%) | 81 (3.8%) | 36 (13.64%) | 23 (11.73%) | 0.546 | 3 (0.31%) | 19 (2.64%) | < 0.001 |
| Non-cardiac death, n (%) | 24 (1.1%) | 4 (1.52%) | 3 (1.53%) | > 0.99 | 3 (0.31%) | 14 (1.94%) | 0.001 |
| Myocardial infarction, n (%) | 73 (3.4%) | 15 (5.68%) | 20 (10.20%) | 0.070 | 3 (0.31%) | 35 (4.86%) | < 0.001 |
| Target lesion revascularization, n (%) | 11 (0.5%) | 3 (1.14%) | 1 (0.51%) | 0.640 | 2 (0.21%) | 5 (0.69%) | 0.147 |
| Target vessel revascularization, n (%) | 15 (0.7%) | 5 (1.89%) | 0 | 0.075 | 2 (0.21%) | 8 (1.11%) | 0.023 |
| Cerebrovascular events, n (%) | 48 (2.2%) | 12 (4.55%) | 13 (6.63%) | 0.329 | 7 (0.73%) | 16 (2.22%) | 0.009 |
| MACCE, n (%) | 125 (5.8%) | 38 (14.39%) | 28 (14.29%) | 0.974 | 16 (1.67%) | 43 (5.97%) | < 0.001 |
| Congestive heart failure, n (%) | 89 (4.2%) | 17 (6.44%) | 32 (16.33%) | 0.001 | 32 (3.34%) | 8 (1.11%) | 0.003 |
| Major bleeding, n (%) | 313 (14.6%) | 39 (14.77%) | 34 (17.35%) | 0.455 | 125 (13.06%) | 115 (15.97%) | 0.092 |
| Minor bleeding, n (%) | 157 (7.3%) | 17 (6.44%) | 18 (9.18%) | 0.272 | 50 (5.22%) | 72 (10%) | < 0.001 |
| Total mortality, n (%) | 105 (4.9%) | 40 (15.15%) | 26 (13.27%) | 0.568 | 6 (0.63%) | 33 (4.58%) | < 0.001 |
| Duration of hospital stay, median (IQR) (Days) | 7 (3–12) | 5 (3–9) | 13 (9–17) | < 0.001 | 3 (0–5) | 11 (8–15) | < 0.001 |
| Follow-up events | |||||||
| Cardiac death, n (%) | 14 (0.7%) | 5 (2.59%) | 2 (1.23%) | 0.889 | 3 (0.33%) | 4 (0.60%) | 0.524 |
| Non-cardiac death, n (%) | 25 (1.3%) | 2 (1.04%) | 0 | 0.237 | 10 (1.09%) | 13 (1.94%) | 0.043 |
| Myocardial infarction, n (%) | 50 (2.6%) | 3 (1.63%) | 10 (6.29%) | 0.005 | 21 (2.33%) | 16 (2.41%) | 0.665 |
| Target lesion revascularization, n (%) | 52 (2.72%) | 8 (4.35%) | 8 (5.03%) | 0.371 | 27 (2.99%) | 9 (1.35%) | 0.141 |
| Target vessel revascularization, n (%) | 57 (2.98%) | 4 (2.17%) | 8 (5.03%) | 0.046 | 27 (2.99%) | 18 (2.71%) | 0.936 |
| Cerebrovascular events, n (%) | 29 (1.64%) | 4 (2.22%) | 4 (2.96%) | 0.636 | 11 (1.25%) | 10 (1.76%) | 0.465 |
| MACCE, n (%) | 108 (6.1%) | 15 (8.33%) | 16 (11.85%) | 0.099 | 48 (5.45%) | 29 (5.09%) | 0.955 |
| Congestive heart failure, n (%) | 415 (19.4%) | 83 (31.44%) | 24 (12.24%) | 0.008 | 212 (22.13%) | 96 (13.33%) | < 0.001 |
| Major bleeding, n (%) | 7 (0.4%) | 0 | 0 | 5 (0.57%) | 2 (0.35%) | 0.614 | |
| Minor bleeding, n (%) | 31 (1.76%) | 5 (2.78%) | 4 (2.96%) | 0.685 | 11 (1.25%) | 11 (1.93%) | 0.322 |
| Total mortality, n (%) | 39 (2.0%) | 7 (3.63%) | 2 (1.23%) | 0.470 | 13 (1.41%) | 17 (2.54%) | 0.036 |
| Median follow-up time (IQR) (months) | 20 (10–37) | 20 (13–31) | 12 (3–33) | 0.002 | 21 (12–39) | 19 (9–37) | 0.009 |
CABG: coronary artery bypass grafting, IQR: interquartile range, MACCE: major adverse cardiovascular and cerebrovascular events, PCI: percutaneous coronary intervention
Follow-up events
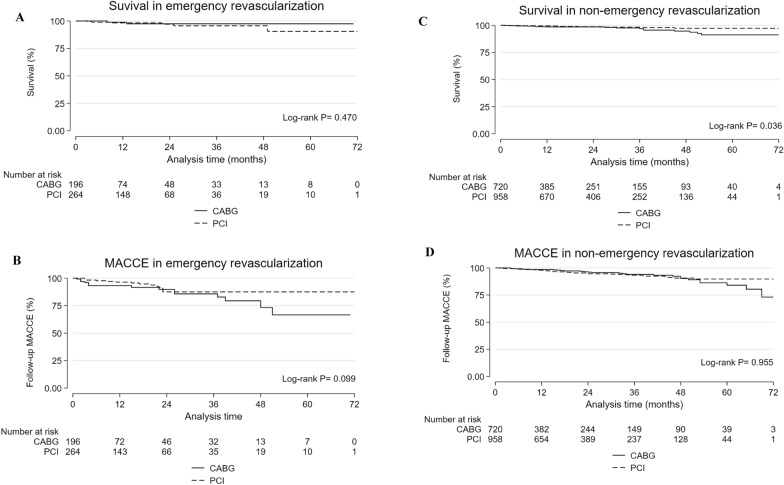
The median follow-up time was 20 months (IQR: 10–37 months). Those with emergent LMCA revascularization had a cardiac mortality of 7/460 (1.5%) and a total mortality of 9/460 (1.96%), without a significant difference between PCI and CABG. MACCEs were reported in 31/460 (6.74%) patients, with no significant difference between PCI and CABG. Follow-up myocardial infarction and target vessel revascularization were significantly higher in patients who underwent CABG than in those who underwent PCI. Congestive heart failure was significantly higher in PCI patients than in CABG patients. The non-emergent LMCA revascularization patients had a total mortality of 30/1678 (1.79%), noncardiac (1.37%), and cardiac (0.42%). The total mortality was significantly higher in CABG patients than in PCI patients. MACCE was reported in 77/1678 (4.6%) patients, with no significant difference between PCI and CABG (Table 5). Kaplan‒Meier curves showed no significant difference between CABG and PCI patients in emergent LMCA revascularization regarding all-cause mortality and MACCE (Figs. 1A, B). Kaplan‒Meier curves showed significantly higher all-cause mortality in non-emergent LMCA revascularization patients who underwent CABG, with no significant difference in MACCE between CABG and PCI (Figs. 1C, D).
Fig. 1.
Total mortality and major adverse cardiovascular and cerebrovascular events (MACCE) in patients with emergent and non-emergent left main revascularization (PCI and CABG), at a median follow-up time of 20 months (IQR: 10-372). Total mortality A and C; MACCE B and D; percutaneous coronary intervention (PCI) (long dash); coronary artery bypass grafting (CABG) (solid line)
Multivariable analysis
Several models were constructed to adjust for risk factors for hospital MACCE and mortality in emergent and non-emergent LMCA revascularization. In patients with emergent LMCA revascularization, MACCE was significantly higher in patients with high EuroSCORE, whether they underwent PCI [OR: 5.13 (95% CI 1.98–13.34); P = 0.001] or CABG [OR: 4.35 (95% CI 1.51–12.57); P = 0.007] compared to patients with low EuroSCORE. However, there was no difference in MACCE according to the revascularization technique after adjusting for EuroSCORE [OR: 0.79 (95% CI 0.45–1.38); P = 0.409]. Different revascularization methods did not significantly affect MACCE in different SYNTAX score categories. In patients presenting with arrest, both PCI [7.64 (3.37–17.35); P < 0.001] and CABG [45.81 (11.29- 185.82); P < 0.001] were associated with significantly higher MACCE compared to other presentations. Additionally, PCI had significantly lower MACCE in patients with arrest than CABG [0.46 (0.24- 0.87); P = 0.017] (Table 6).
Table 6.
Univariable and multivariable analysis for factors associated with hospital MACCE in emergency and non-emergency left main revascularization
| Hospital MACCE | Univariable | Multivariable | ||
|---|---|---|---|---|
| Emergency revascularization | OR (95% CI) | P | OR (95% CI) | P |
| Baseline characteristics | ||||
| Male | 1.90 (1.05–3.44) | 0.033 | – | – |
| Age | 1.02 (0.99–1.04) | 0.111 | – | – |
| Body mass index | 0.99 (0.93–1.04) | 0.642 | – | – |
| Smoking | 0.85 (0.49–1.47) | 0.561 | – | – |
| Diabetes mellitus | 0.96 (0.54–1.69) | 0.887 | – | – |
| Dyslipidemia | 1.02 (0.59–1.78) | 0.936 | – | – |
| Hypertension | 1.89 (1.03–3.44) | 0.038 | – | – |
| Previous myocardial infarction | 1.77 (1.04–3.01) | 0.037 | – | – |
| Chronic kidney disease | 3.57 (2.04–6.24) | < 0.001 | 2.99 (1.62–5.50) | < 0.001 |
| Peripheral arterial disease | 3.22 (1.63–6.33) | 0.001 | 2.45 (1.17–5.13) | 0.017 |
| Cerebrovascular accident | 2.09 (0.97–4.50) | 0.059 | – | – |
| Congestive heart failure | 3.88 (2.13–7.06) | < 0.001 | 2.67 (1.37–5.19) | 0.004 |
| Atrial fibrillation | 1.92 (0.85–4.24) | 0.109 | – | – |
| Ejection fraction category | 1.03 (0.74–1.41) | 0.874 | – | – |
| PCI vs. CABG | 1.01 (0.60–1.71) | 0.974 | – | – |
| EuroSCORE | ||||
| EuroSCORE | 1.08 (1.04–1.10) | < 0.001 | 2.69 (1.82–3.97) | < 0.001 |
| PCI vs. CABG | 1.01 (0.60–1.71) | 0.974 | 0.79 (0.45–1.38) | 0.409 |
| Presentation | ||||
| Arrest | 4.72 (2.63–8.50) | < 0.001 | 2.16 (1.11–4.22) | 0.024 |
| Shock | 8.73 (4.87–15.64) | < 0.001 | 8.69 (4.47–16.92) | < 0.001 |
| STEMI | 0.26 (0.14–0.67) | < 0.001 | – | – |
| NSTEMI | 0.24 (0.13–0.44) | < 0.001 | – | – |
| PCI vs. CABG | 1.01 (0.60–1.71) | 0.974 | 0.46 (0.24–0.87) | 0.017 |
| SYNTAX score | ||||
| SYNTAX score | 1.02 (0.99–1.04) | 0.158 | 1.38 (0.95–1.99) | 0.091 |
| PCI vs. CABG | 1.01 (0.60–1.71) | 0.974 | 1.14 (0.66–1.96) | 0.641 |
| Non–emergency revascularization | ||||
| Baseline characteristics | ||||
| Male | 1.20 (0.66–2.19) | 0.542 | – | – |
| Age | 1.01 (0.98–1.03) | 0.553 | – | – |
| Body mass index | 0.97 (0.92–1.02) | 0.232 | – | – |
| Smoking | 0.93 (0.55–1.59) | 0.796 | – | – |
| Diabetes mellitus | 1.16 (0.65–2.05) | 0.618 | – | – |
| Dyslipidemia | 2.79 (1.31–5.93) | 0.008 | 2.36 (1.22–5.57) | 0.013 |
| Hypertension | 1.68 (0.86–3.27) | 0.127 | – | – |
| Previous myocardial infarction | 1.23 (0.71–2.15) | 0.461 | – | – |
| Chronic kidney disease | 1.33 (0.73–2.42) | 0.350 | – | – |
| Peripheral arterial disease | 1.01 (0.45–2.25) | 0.989 | – | – |
| Cerebrovascular accident | 0.59 (0.21–1.65) | 0.317 | – | – |
| Congestive heart failure | 1.59 (0.79–3.19) | 0.192 | 2.36 (1.10–5.04) | 0.027 |
| Atrial fibrillation | – | – | – | – |
| Ejection fraction category | 0.80 (0.59–1.08) | 0.148 | – | – |
| PCI vs. CABG | 0.27 (0.15–0.48) | < 0.001 | 0.30 (0.16–0.56) | < 0.001 |
| EuroSCORE | ||||
| EuroSCORE | 1.06 (1.02–1.12) | 0.005 | 1.07 (1.03–1.11) | 0.001 |
| PCI vs. CABG | 0.27 (0.15–0.48) | < 0.001 | 0.25 (0.14–0.45) | < 0.001 |
| Presentation | ||||
| Arrest | – | – | – | – |
| Shock | – | – | – | – |
| STEMI | – | – | – | – |
| NSTEMI | 0.62 (0.35–1.11) | 0.107 | – | – |
| PCI vs. CABG | 0.27 (0.15–0.48) | < 0.001 | – | – |
| SYNTAX score | ||||
| SYNTAX score | 1.02 (0.99–1.05) | 0.117 | 1.17 (0.79–1.73) | 0.444 |
| PCI vs. CABG | 0.27 (0.15–0.48) | < 0.001 | 0.27 (0.15–0.50) | < 0.001 |
MACCE: major adverse cardiovascular and cerebrovascular events, CABG: coronary artery bypass graft surgery, PCI: percutaneous coronary intervention, EuroSCORE score: European system for cardiac operative risk evaluation, STEMI: ST–segment elevation myocardial infarction; NSTEMI: non-ST-segment elevation myocardial infarction, OR: odds ratio, CI: confidence interval
In emergent LMCA revascularization, hospital all-cause mortality was significantly higher with PCI [36.78 (4.86–278.48); P < 0.001] and CABG [42.13 (5.35–331.75); P < 0.001] in patients with high EuroSCORE compared to low EuroSCORE. While there was no difference between both approaches after adjusting for EuroSCORE [0.87 (0.49–1.56); P = 0.647]. There was no interaction between PCI/CABG and SYNTAX score categories for their effect on hospital all-cause mortality. Mortality was significantly higher in patients presented with arrest and had CABG [133.09 (28.63- 618.50); P < 0.001] or PCI [4.81 (2.09–11.08); P < 0.001]; however, PCI was associated with lower mortality compared to CABG [0.43 (0.22–0.85); P 0.016] (Table 7).
Table 7.
Univariable and multivariable analysis for factors associated with hospital mortality in emergency and non-emergency left main revascularization
| Hospital mortality | Univariable | Multivariable | ||
|---|---|---|---|---|
| Emergency revascularization | OR (95% CI) | P | OR (95% CI) | P |
| Baseline characteristics | ||||
| Male | 1.90 (1.05–3.45) | 0.033 | – | – |
| Age | 1.04 (1.01–1.06) | 0.005 | 1.04 (1.01–1.07) | 0.007 |
| Body mass index | 0.95 (0.89–1.01) | 0.108 | 0.93 (0.87–0.99) | 0.038 |
| Smoking | 0.56 (0.31–1.01) | 0.052 | – | – |
| Diabetes mellitus | 0.88 (0.50–1.54) | 0.665 | – | – |
| Dyslipidemia | 1.43 (0.80–2.55) | 0.230 | – | – |
| Hypertension | 2.54 (1.34–4.82) | 0.004 | 2.91 (1.38–6.16) | 0.005 |
| Previous myocardial infarction | 1.52 (0.89–2.61) | 0.127 | – | – |
| Chronic kidney disease | 1.81 (1.001–3.36) | 0.05 | – | – |
| Peripheral arterial disease | 1.93 (0.93–4.01) | 0.078 | – | – |
| Cerebrovascular accident | 2.09 (0.97–4.50) | 0.059 | – | – |
| Congestive heart failure | 2.91 (1.58–5.38) | 0.001 | 3.03 (1.50–6.14) | 0.002 |
| Atrial fibrillation | 1.62 (071–3.69) | 0.255 | – | – |
| Ejection fraction category | 1.43 (1.02–2.00) | 0.036 | 2.68 (1.47–4.89) | 0.001 |
| PCI vs. CABG | 1.17 (0.69–1.99) | 0.568 | – | – |
| EuroSCORE | ||||
| EuroSCORE | 1.09 (1.06–1.13) | < 0.001 | 4.45 (2.83–7.01) | < 0.001 |
| PCI vs. CABG | 1.17 (0.69–1.99) | 0.568 | 0.87 (0.49–1.56) | 0.647 |
| Presentation | ||||
| Arrest | 10.57 (5.84–19.20) | < 0.001 | 5.40 (2.77–10.56) | < 0.001 |
| Shock | 11.53 (6.25–21.27) | < 0.001 | 9.07 (4.47 (18.42) | < 0.001 |
| STEMI | 0.20 (0.11–0.36) | < 0.001 | – | – |
| NSTEMI | 0.21 (0.12–0.39) | < 0.001 | – | – |
| PCI vs. CABG | 1.17 (0.69–1.99) | 0.568 | 0.43 (0.22–0.85) | 0.016 |
| SYNTAX score | ||||
| SYNTAX score | 1.01 (0.98–1.04) | 0.044 | 1.36 (0.94–1.97) | 0.099 |
| PCI vs. CABG | 1.17 (0.69–1.99) | 0.568 | 1.31 (0.76–2.28) | 0.331 |
| Non–emergency revascularization | ||||
| Baseline characteristics | ||||
| Male | 0.90 (0.411–1.98) | 0.800 | – | – |
| Age | 1.02 (0.99–1.06) | 0.168 | 1.04 (1.003–1.08) | 0.031 |
| Body mass index | 0.96 (0.90–1.03) | 0.287 | – | – |
| Smoking | 0.64 (0.32–1.28) | 0.209 | – | – |
| Diabetes mellitus | 1.57 (0.74–3.33) | 0.241 | – | – |
| Dyslipidemia | 3.88 (1.37–10.99) | 0.011 | 3.56 (1.24–10.22) | 0.018 |
| Hypertension | 1.79 (0.78–4.08) | 0.167 | – | – |
| Previous myocardial infarction | 1.01 (0.50–2.05) | 0.973 | – | – |
| Chronic kidney disease | 2.77 (1.45–5.30) | 0.002 | 3.74 (1.83–7.62) | < 0.001 |
| Peripheral arterial disease | 1.37 (0.57–3.31) | 0.485 | – | – |
| Cerebrovascular accident | 0.44 (0.11–1.84) | 0.262 | – | – |
| Congestive heart failure | 2.01 (0.91–4.45) | 0.083 | – | – |
| Atrial fibrillation | 0.57 (0.14–2.39) | 0.441 | – | – |
| Ejection fraction category | 1.07 (0.72–1.57) | 0.743 | – | – |
| PCI vs. CABG | 0.13 (0.05–0.32) | < 0.001 | 0.100 (0.04–0.25) | < 0.001 |
| EuroSCORE | ||||
| EuroSCORE | 1.12 (1.08–1.17) | < 0.001 | 1.13 (1.08–1.18) | < 0.001 |
| PCI vs. CABG | 0.13 (0.05–0.32) | < 0.001 | 0.11 (0.04–0.27) | < 0.001 |
| Presentation | ||||
| Arrest | – | – | – | – |
| Shock | – | – | – | – |
| STEMI | – | – | – | – |
| NSTEMI | 0.53 (0.26–1.10) | 0.089 | – | – |
| PCI vs. CABG | 0.13 (0.05–0.32) | < 0.001 | 0.13 (0.05–0.32) | < 0.001 |
| SYNTAX score | ||||
| SYNTAX score | 1.05 (1.01–1.08) | 0.005 | 1.38 (0.84–2.25) | 0.201 |
| PCI vs. CABG | 0.13 (0.05–0.32) | < 0.001 | 0.14 (0.06–0.36) | < 0.001 |
CABG: coronary artery bypass graft surgery, PCI: percutaneous coronary intervention, EuroSCORE score: European system for cardiac operative risk evaluation, STEMI: ST–segment elevation myocardial infarction; NSTEMI: non-ST-segment elevation myocardial infarction, OR: odds ratio, CI: confidence interval
In non-emergent revascularization, PCI was associated with lower MACCE in patients with low [0.16 (0.04–0.70); P = 0.015] and intermediate [0.20 (0.09–0.48); P < 0.001] EuroSCORE compared to CABG in patients with the same EuroSCORE category. PCI was associated with lower MACCE in patients with low [0.09 (0.02–0.41); P = 0.002] and intermediate [0.30 (0.13–0.73); P = 0.008] SYNTAX scores compared to CABG with the same SYNTAX score category (Table 6).
In non-emergent revascularization, PCI was associated with reduced hospital mortality in patients with intermediate [0.12 (0.03–0.43); P = 0.001] and high [0.13 (0.03–0.47); P = 0.002] EuroSCORE compared to CABG with the same EuroSCORE category. PCI was associated with lower hospital mortality in patients with low [0.09 (0.01–0.89); P = 0.031] and intermediate [0.09 (0.02–0.39); P = 0.001] SYNTAX scores compared to CABG with the same SYNTAX score category (Table 7).
Multivariable Cox regression analysis revealed that factors that increased the follow-up MACCE were female sex, cardiac arrest, cardiogenic shock at presentation, low left ventricular ejection fraction, hypertension, and low body mass index. Emergent PCI had a lower rate of follow-up MACCE compared to CABG [HR: 0.30 (95% CI 0.14–0.66), P < 0.003], with no difference between elective CABG and PCI [HR: 0.79 (95% CI 0.47–1.31), P = 0.355]. Factors associated with follow-up mortality were age, hypertension, peripheral arterial disease, and high EuroSCORE II. There was no difference in follow-up mortality between emergency PCI and CABG [HR: 1.18 (95% CI 0.23- 6.08), P = 0.845]. However, elective PCI was associated with lower follow-up mortality than CABG [HR: 0.35 (95% CI 0.16–0.76), P = 0.008] (Table 8).
Table 8.
Multivariable Cox regression analysis for factors affecting follow-up MACCE and all-cause mortality
| HR (95% CI) | P | |
|---|---|---|
| Follow-up MACCE | ||
| Female | 2.47 (1.58–3.87) | < 0.001 |
| Arrest | 2.82 (1.06–7.49) | 0.038 |
| Ejection fraction | 0.97 (0.95–0.98) | < 0.001 |
| Hypertension | 2.04 (1.16–3.58) | 0.013 |
| Body mass index | 0.95 (0.91–0.99) | 0.020 |
| Group | ||
| Elective PCI vs. CABG | 0.79 (0.47–1.31) | 0.355 |
| Emergency PCI vs. CABG | 0.30 (0.14–0.66) | 0.003 |
| Follow-up all-cause mortality | ||
| Age | 1.04 (1.004–1.07) | 0.027 |
| Hypertension | 5.32 (1.26–22.45) | 0.023 |
| Peripheral arterial disease | 2.91 (1.30–6.53) | 0.010 |
| EuroSCORE | 1.07 (1.04–1.11) | < 0.001 |
| Group | ||
| Elective PCI vs. CABG | 0.35 (0.16–0.76) | 0.008 |
| Emergency PCI vs. CABG | 1.18 (0.23–6.08) | 0.845 |
MACCE: major adverse cardiovascular and cerebrovascular events, CABG: coronary artery bypass graft surgery, PCI: percutaneous coronary intervention, EuroSCORE score: European system for cardiac operative risk evaluation, HR: hazard ratio
Discussion
Several studies addressing revascularization of the LMCA disease focused on patients with chronic coronary artery disease; however, around 7% of patients with LMCA disease present with acute coronary syndrome [14]. Those patients are usually excluded from clinical studies; therefore, it is essential to evaluate the optimal revascularization strategy for LMCA disease in both elective and emergency situations [15]. The Gulf Left-Main Study investigated emergent LMCA revascularization and compared the outcomes of PCI versus CABG. The study found that PCI was associated with lower hospital MACCE and hospital all-cause mortality compared to CABG in patients presented with arrest or shock; however, there was no advantage of PCI vs. CABG in emergency revascularization if stratified by EuroSCORE or SYNTAX score. Additionally, PCI had lower follow-up MACCE compared to CABG in emergent LMCA revascularization within a 20-month follow-up period. PCI was more advantageous than CABG in non-emergency situations, especially in patients with low and intermediate EuroSCORE and SYNTAX scores. Despite being associated with high mortality, revascularization in the acute phase has been shown to improve prognosis [16].
The baseline characteristics differed between groups. The EuroSCORE II was significantly higher in patients with PCI compared to CABG in patients who had emergency revascularization, and there was a greater number of patients with left ventricular ejection fraction (LVEF) of less than 40% in the PCI group in emergency and non-emergency revascularization. However, EuroSCORE was higher in CABG patients with non-emergent revascularization than in PCI. Of patients who required LMCA revascularization, 21.5% were identified as needing revascularization emergently. The study also found that the incidence of LMCA being the culprit lesion in patients with acute myocardial infarction was 5%, which is consistent with a previous report [17, 18].
In a meta-analysis of 977 patients from 13 different studies, the thirty-day mortality was 15% post-emergent LMCA PCI, comparable to the data for the PCI group in this study [19]. In patients who required emergent LMCA revascularization using CABG, the estimated death rate was reported to be 19%, which is higher than the rate of 11.7% in this study, indicating a trend toward percutaneous revascularization for high-risk patients and considering surgical options only for lower-risk selected patients [20]. The choice of revascularization strategy is largely affected by the clinical status of the patients. Urgent revascularization with either PCI or CABG is essential in clinically unstable patients to improve survival [21]. Practically, PCI is more convenient in emergencies. We found that PCI had survival benefits and lower hospital and follow-up MACCE in patients with shock or cardiac arrest. The outcomes of emergency revascularization were affected by patients' characteristics rather than the revascularization technique, except in critically ill patients with either arrest or shock. Optimizing patients before PCI and the early use of mechanical circulatory support in those patients might improve the outcomes of emergency revascularization [22]. In this study, PCI was more advantageous for revascularizing non-emergent LMCA disease, especially in patients with low and intermediate risk stratification using EuroSCORE and SYNTAX scores.
Once discharged, the reported mortality in this study was low (1.23–2.59% CABG vs. PCI, respectively) compared to published reports of 10.5% mortality at one year with emergent PCI of LMCA lesions [23]. This study is the largest series to date to assess revascularization in patients requiring emergent LMCA intervention. This demonstrates that PCI was associated with better in-hospital and follow-up outcomes than CABG, especially in patients presented in critically ill conditions. This supports PCI as the intervention of choice for hemodynamically unstable patients in the setting of myocardial infarction. However, the study had some limitations, including its retrospective, nonrandomized design and the potential influence of unmeasured factors, such as the surgeons' experience and the volumes of the procedures at participating centers. Therefore, future randomized trials on this subset of patients are highly recommended to continue to define optimal revascularization strategies.
Conclusions
Emergent LMCA revascularization is associated with high in-hospital mortality and morbidity. Nevertheless, patients who survive to discharge have a much better prognosis. PCI could be advantageous over CABG in revascularizing LMCA disease in emergencies. PCI could be preferred for revascularization of non-emergent LMCA in patients with intermediate EuroSCORE and low and intermediate SYNTAX scores.
Acknowledgements
The authors would like to thank all the nurses and cardiac catheterization technologists who helped in collecting the data from all the participating centers.
Abbreviations
- LMCA
Left-main coronary artery
- PCI
Percutaneous coronary intervention
- CABG
Coronary artery bypass graft surgery
- MACCE
Major adverse cardiovascular and cerebrovascular events
- EuroSCORE score
European system for cardiac operative risk evaluation
- CABG
Coronary artery bypass grafting
- MACCE
Major adverse cardiovascular and cerebrovascular events
- OR
Odds ratio
- CI
Confidence interval
- IQR
Interquartile range
- HR
Hazard ratio
- LV
Left ventricle
- CAD
Coronary artery disease
- EHR
Electronic health record
- VIF
Variance inflation factor
- EuroSCORE score
European system for cardiac operative risk evaluation
- NSTE-ACS
Non-ST Elevation Acute Coronary Syndrome
- SYNTAX
The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery
- DES
Drug eluting stent
- ACE
Angiotensin-converting enzyme
- ARB
Angiotensin II receptor blocker
- ASA
Aspirin
Author contributions
AD, AA, SRD, AZ, ASH, WA, NY, AA, MA, BA, AE, AAA, AJ, KZA, RA, AHA, TA, SH, ZD, WR, HMK, MAG, HA, NH, YE, ES, JA, MAQ, WQ, MNA, AMI, AE, AA, MJN, TH, MB, AFH, IAMA, MMM, OA, MR, AAG, AMS, HAN, A.M., FA, SA, MK, RTB, AA, IA, AL: study design, development, data collection. AD, SRD, AZ, AAA, AL: produced the initial draft of the manuscript. AAA: statistical analysis including figures, tables and interpretation of data. AD, AAA, AL: reviewed the manuscript and provided critical revision and final editing.
Funding
The authors have no funding sources to disclose.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of King Faisal Specialist Hospital and Research Center in Riyadh (12 November 2020—RAC # 2201226: Gulf-LM Registry) and was carried out per the local guidelines and ethical guidelines of the Declaration of Helsinki.
Informed consent
The IRB waived informed consent for this study due to its retrospective and observational nature and the absence of any patient-identifying information.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gaudino M, Farkouh ME, Stone GW. Left main revascularization: an evidence-based reconciliation. Eur Heart J. 2022;43(25):2421–2424. doi: 10.1093/eurheartj/ehac216. [DOI] [PubMed] [Google Scholar]
- 2.Mavromatis K, Sandesara PB. Complete revascularization in left main disease: is it important? JACC Asia. 2023;3:75–77. doi: 10.1016/j.jacasi.2022.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2018;40(2):87–165. doi: 10.1093/eurheartj/ehy394. [DOI] [Google Scholar]
- 4.Huang HW, Brent BN, Shaw RE. Trends in percutaneous versus surgical revascularization of unprotected left main coronary stenosis in the drug-eluting stent era: a report from the American college of cardiology-national cardiovascular data registry (ACC-NCDR) Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv. 2006;68(6):867–872. doi: 10.1002/ccd.20886. [DOI] [PubMed] [Google Scholar]
- 5.Tam DY, Fang J, Rocha RV, Rao SV, Dzavik V, Lawton J, et al. Real-world examination of revascularization strategies for left main coronary disease in ontario. Canada JACC Cardiovasc Interv. 2023;16(3):277–288. doi: 10.1016/j.jcin.2022.10.016. [DOI] [PubMed] [Google Scholar]
- 6.Daoulah A, Alasmari A, Hersi AS, Alshehri M, Al GT, Abuelatta R, et al. Percutaneous coronary intervention Vs coronary artery bypass surgery for unprotected left main coronary disease: G-LM registry. Curr Probl Cardiol. 2022;47(10):101002. doi: 10.1016/j.cpcardiol.2021.101002. [DOI] [PubMed] [Google Scholar]
- 7.Daoulah A, Abozenah M, Alshehri M, Hersi AS, Yousif N, Al GT, et al. Unprotected left main revascularization in the setting of non-coronary atherosclerosis: gulf left main registry. Curr Probl Cardiol. 2023;48(1):101424. doi: 10.1016/j.cpcardiol.2022.101424. [DOI] [PubMed] [Google Scholar]
- 8.Nashef SAM, Roques F, Sharples LD, Nilsson J, Smith C, Goldstone AR, et al. EuroSCORE II†. Eur J Cardio-Thoracic Surg. 2012;41(4):734–745. doi: 10.1093/ejcts/ezs043. [DOI] [PubMed] [Google Scholar]
- 9.Ong ATL, Serruys PW, Mohr FW, Morice M-C, Kappetein AP, Holmes DRJ, et al. The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study: design, rationale, and run-in phase. Am Heart J. 2006;151(6):1194–1204. doi: 10.1016/j.ahj.2005.07.017. [DOI] [PubMed] [Google Scholar]
- 10.Medina A, Suárez de Lezo J, Pan M. A new classification of coronary bifurcation lesions. Rev Esp Cardiol. 2006;59:183. doi: 10.1157/13084649. [DOI] [PubMed] [Google Scholar]
- 11.Schulman S, Angerås U, Bergqvist D, Eriksson B, Lassen MR, Fisher W. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. J Thromb Haemost. 2010;8(1):202–204. doi: 10.1111/j.1538-7836.2009.03678.x. [DOI] [PubMed] [Google Scholar]
- 12.Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(4):692–694. doi: 10.1111/j.1538-7836.2005.01204.x. [DOI] [PubMed] [Google Scholar]
- 13.Ballantyne A, Eriksson S. Research ethics revised: the new CIOMS guidelines and the world medical association declaration of helsinki in context. Bioethics. 2019;33:310–311. doi: 10.1111/bioe.12581. [DOI] [PubMed] [Google Scholar]
- 14.Abdelmalak HD, Omar HR, Mangar D, Camporesi EM. Unprotected left main coronary stenting as alternative therapy to coronary bypass surgery in high surgical risk acute coronary syndrome patients. Ther Adv Cardiovasc Dis. 2013;7(4):214–223. doi: 10.1177/1753944713488637. [DOI] [PubMed] [Google Scholar]
- 15.Tam DY, Bakaeen F, Feldman DN, Kolh P, Lanza GA, Ruel M, et al. Modality selection for the revascularization of left main disease. Can J Cardiol. 2019;35(8):983–992. doi: 10.1016/j.cjca.2018.12.017. [DOI] [PubMed] [Google Scholar]
- 16.Beijk MAM, Palacios-Rubio J, Grundeken MJD, Kalkman DN, De Winter RJ. Clinical outcomes after percutaneous coronary intervention for cardiogenic shock secondary to total occlusive unprotected left main coronary artery lesion-related acute myocardial infarction. J Clin Med. 2023 doi: 10.3390/jcm12041311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baek JY, Seo SM, Park H-J, Kim PJ, Park MW, Koh YS, et al. Clinical outcomes and predictors of unprotected left main stem culprit lesions in patients with acute ST segment elevation myocardial infarction. Catheter Cardiovasc Interv Off J Soc Card Angiogr Interv. 2014;83(7):E243–E250. doi: 10.1002/ccd.23420. [DOI] [PubMed] [Google Scholar]
- 18.Cheng C-I, Wu C-J, Fang C-Y, Youssef AA, Chen C-J, Chen S-M, et al. Feasibility and safety of transradial stenting for unprotected left main coronary artery stenoses. Circ J. 2007;71(6):855–861. doi: 10.1253/circj.71.855. [DOI] [PubMed] [Google Scholar]
- 19.Vis MM, Beijk MA, Grundeken MJ, Baan JJ, Koch KT, Wykrzykowska JJ, et al. A systematic review and meta-analysis on primary percutaneous coronary intervention of an unprotected left main coronary artery culprit lesion in the setting of acute myocardial infarction. JACC Cardiovasc Interv. 2013;6(4):317–324. doi: 10.1016/j.jcin.2012.10.020. [DOI] [PubMed] [Google Scholar]
- 20.Nagaoka H, Ohnuki M, Hirooka K, Shimoyama T. Emergency coronary artery bypass grafting for left main coronary artery disease. Kyobu Geka. 1999;52(8 Suppl):634–638. [PubMed] [Google Scholar]
- 21.Hochman JS, Sleeper LA, Webb JG, Sanborn TA, White HD, Talley JD, et al. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK investigators. Should we emergently revascularize occluded coronaries for cardiogenic shock. N Engl J Med. 1999;341(9):625–634. doi: 10.1056/NEJM199908263410901. [DOI] [PubMed] [Google Scholar]
- 22.Fernando SM, Price S, Mathew R, Slutsky AS, Combes A, Brodie D. Mechanical circulatory support in the treatment of cardiogenic shock. Curr Opin Crit Care. 2022;28(4):434–441. doi: 10.1097/MCC.0000000000000956. [DOI] [PubMed] [Google Scholar]
- 23.Pappalardo A, Mamas MA, Imola F, Ramazzotti V, Manzoli A, Prati F, et al. Percutaneous coronary intervention of unprotected left main coronary artery disease as culprit lesion in patients with acute myocardial infarction. JACC Cardiovasc Interv. 2011;4(6):618–626. doi: 10.1016/j.jcin.2011.02.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.