Abstract
Objectives
To analyse the differences in hypertensive complications according to continuity of care (COC) and medication adherence in patients with hypertension.
Design
A national population-based retrospective cohort study.
Setting
Secondary data analysis using National insurance claims data at all levels of hospitals in South Korea.
Participants
A total of 102 519 patients diagnosed with hypertension were included in this study.
Primary outcome measures
The levels of COC and medication adherence were estimated within the initial 2 years of the follow-up period, and the incidence of medical complications was estimated within the subsequent 16 years. We used the level of COC to measure COC and the medication possession ratio (MPR) to measure medication adherence.
Results
The average level of COC in the hypertension group was 0.8112. The average proportion of the MPR in the hypertension group was 73.3%. COC in patients with hypertension showed varying results: the low COC group had a 1.14-fold increased risk of medical complications compared with the high COC group. In terms of the level of MPR in patients with hypertension, the 0%–19% MPR group had a 1.5-fold risk of medical complications relative to the 80%–100% MPR group.
Conclusions
In patients with hypertension, high COC and medication adherence for the first 2 years of diagnosis can help prevent medical complications and promote patients’ health. Therefore, effective strategies to improve COC and medication adherence are required. Future research should include some factors that may affect the incidence of hypertensive complications, such as familial aggregation, and hazard stratification by the level of blood pressure, which were not considered in this study. Therefore, there may be residual confounding and still room for improvement.
Keywords: ambulatory care-sensitive conditions, continuity of care, hypertension, medication adherence, retrospective cohort
STRENGTHS AND LIMITATIONS OF THIS STUDY
The study had a long follow-up period (18 years) and included over 100 000 participants, which are regarded as indicators of relatively higher reliability and validity in cohort studies according to the European Society of Cardiology.
The used database contained data on health service use of over 50 000 000 Korean citizens’ (99.7% of whole population), indicating that it was nationally representative.
Hypertension (International Classification of Disease-11 code: I.10) was selected from the Ambulatory Care-Sensitive Conditions list in the Agency of Health Research and Quality standard and hypertensive complications were selected according to the definitions from World Health Organization and the advice from specialists in internal medicine.
Owing to the retrospective nature of the study, the possibility of bias, including misclassification bias, may not be excluded.
Some factors that may affect the incidence of hypertensive complications, such as familial aggregation, and hazard stratification by the level of blood pressure were not considered.
Introduction
Hypertension is one of the most important health issues worldwide.1 In terms of the global prevalence of hypertension, almost 1.4 billion people, which is almost 20% of the world population, have hypertension.2 In an evaluation of all risk factors by the World Health Organization (WHO) and the Global Burden of Disease Study, hypertension ranked first as a contributor to the burden of disease at 20%, with a contribution greater than that of obesity.3 Hypertension progresses in approximately 50%, 33% and 10%–15% of cases caused by coronary artery disease or heart disease, stroke and renal disease, respectively.1 It is closely related to ischaemic heart disease, which is the leading cause of death worldwide.4
Hypertension is also classified as an Ambulatory Care-Sensitive Condition (ACSCs), which means that early diagnosis and intervention are beneficial in preventing the medical complications that may result in death, hospitalisation and major medical costs.5 ACSCs have been classified by the Agency of Health Research and Quality (AHRQ), and 16 diseases selected by the AHRQ can be prevented from progressing if they are treated effectively in a timely manner by providing prevention and medical services.6 By treating and managing these conditions early, hospitalisation due to aggravation or complications of the disease can be reduced.6 Early intervention in an outpatient setting slows the onset and progression of the disease7 and prevents avoidable hospitalisation.5 8
ACSCs are representative indicators for evaluating the accessibility and quality of primary care, which plays a pivotal role in ‘early intervention’.9 To assess the management of ACSCs in medical institutions, including primary care, continuity of care (COC) and medication possession ratio (MPR) are the most important indicators of measurement tools. COC refers to a continuous relationship and consultation between a patient and physician, and the MPR refers to the compliance rate of medications as prescribed by a physician. Therefore, these two measurements are broadly used for the evaluation of the ACSCs management.
Several studies have focused on hypertension, COC and medication adherence.10–12 However, the study design of previous studies was limited by the setting, and the small number of patients included.10–12 This study used the National Health Insurance Service (NHIS) database, in which over 50 million patients are registered.13 Patient data include physician visit information and the prescription data for each visit.13 As national health insurance is mandatory for every citizen in South Korea, the reliability of the data is high and data are representative of the population on a national level.13
The objective of this study was to analyse the effect of providing timely and effective ambulatory care to patients with early hypertension on preventing the occurrence of medical complications using COC and the MPR as indicators of effective care. The secondary objective was to assess the outcomes of hypertension according to the level of hospital at which patients were treated.
Methods
This national, population-based, retrospective cohort study investigated the incidence of hypertension from 1 January 2002 to 31 December 2019 among the general population in South Korea. We analysed the secondary data using national insurance claims data at all levels of hospitals in South Korea. Unlike previous studies on the risk of complications according to the COC and medication adherence, this study examined the time variance, including the time from the first visit to initial 2 years of the medical institution, and limited the patient’s age (>30 years).14
Inclusion and exclusion of participants
This study used the data of 1.4 million individuals from the NHIS database from 2002 to 2019 selected using stratified sampling.13 The NHIS database, which includes the medical records of more than 50 million people, is stratified by sex and age group (18 strata).13 To maintain representativeness, sampling was performed according to the demographic characteristics and income deciles in South Korea.13 In addition, these cohort data were linked to the national health check-up database, including data of over 66% of the general population (over 33 million) in South Korea. Furthermore, information on the cause of death was provided by linkage to death data from the National Statistical Office.15 16
After excluding patients with missing data for any of the key variables, data on the medical claims of 102 519 patients with hypertension (International Classification of Disease code: I.10) were extracted from the NHIS database, covering the 2002–2019 period, and included in the analysis. No patients were lost to follow-up because all medical records were registered through the electronic medical record system and tracked in accordance with the ‘National Health Insurance Act’ established by the Korean government.
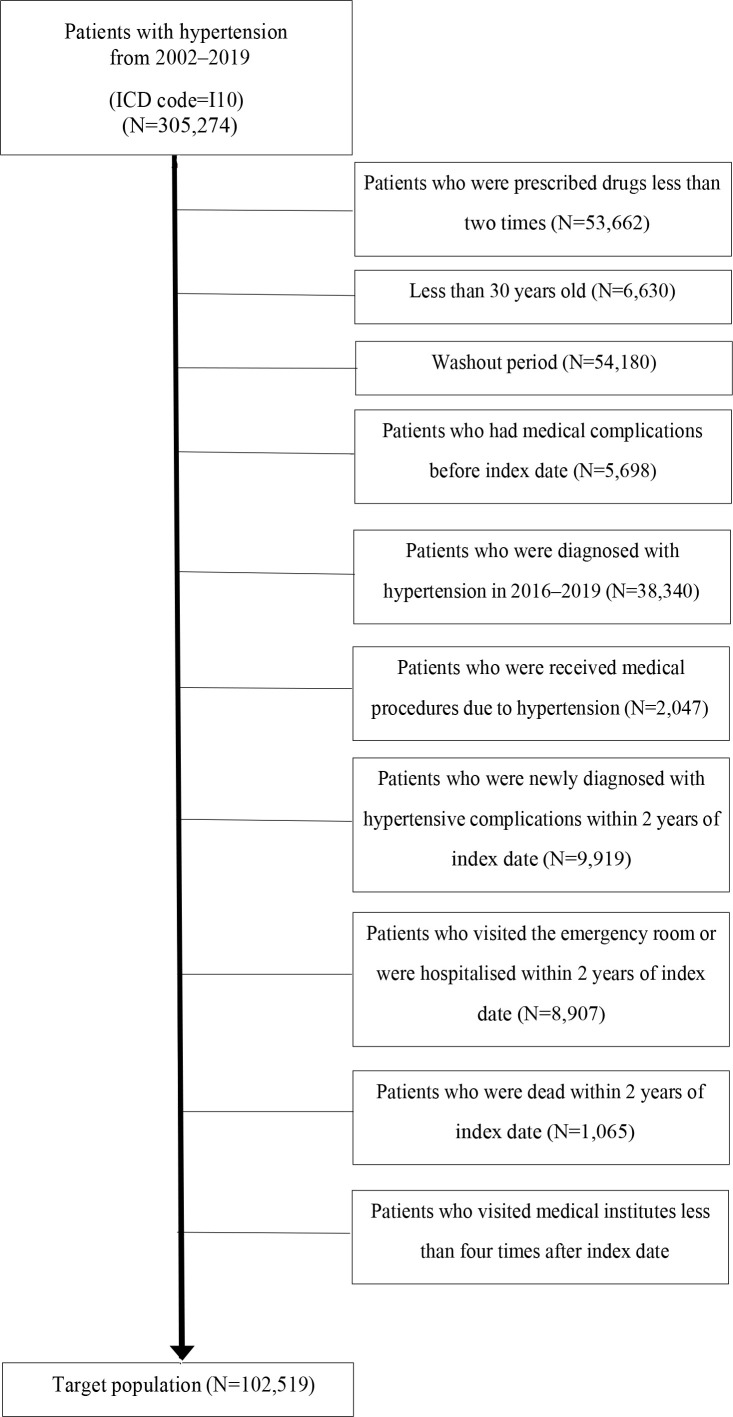
To avoid bias, we excluded patients who were prescribed drugs less than twice (n=53 662) to enable proper measurement of the MPR; patients aged <30 years (n=6630) to exclude low-risk patients; patients who visited medical institutions in 2002 and 2003 (n=54 180) as an wash-out period; patients with medical complications (n=5698) to prevent contamination of results on the incidence of complications; those who were diagnosed with hypertension from 2016 to 2019 (n=38 340) to maintain the baseline characteristics of the target population; patients who had taken related drugs or undergone related procedures or surgeries according to the AHRQ guidelines on ACSCs (n=2047); those who had visited the medical institution before the index date due to hypertension (n=9919), or who visited the emergency room or were hospitalised within 2 years of the index date according to the AHRQ guidelines on ACSCs research (n=8907) to avoid unequal baseline characteristics; those who died within 2 years of the index date (n=1065) for the wash-out period of mortality and severity; and patients who visited medical institutions less than four times after the index date (n=22 308) to enable proper measurement of COC. After these exclusions, retrospective data of 102 519 patients (out of 1.4 million members of the general population of South Korea) were included in the analysis (figure 1).
Figure 1.
Flow diagram of the study population. ICD, International Classification of Disease.
Measurements
COC was defined as ‘continuance of care by a healthcare provider to meet a patient’s medical needs providing high-quality and harmonised care’.17 Additionally, with a good level of continuous care provided by the physicians, the hospitalisation rate, prevalence and the number of medical visits are reduced.18 Methods for measuring COC include the COC, Usual Provider of Care index, Most Frequent Primary Care and the Modified Continuity Index.19 We used COC as an indicator.
Shortell identified four core factors required for COC.20 First, the data should be of individuals. Second, analysed data should be distinguished and compared when individuals visit different medical institutions and providers. Third, COC should reflect the total number of visits for care. Finally, appropriate referral patterns should also be considered.21 South Korea has a fee-for-service system without a proper referral system.21
COC measures COC on a scale of 0–1, based on all visits to medical institutions. It weighs both the frequency of visits to each provider and the dispersion of visits between providers. If every visit for medical services to one provider, the COC index will be 1. The formula is:
N=total number of ambulatory care.
=number of visits to provider
M=total number of provider.
The major drawback of this method is that it is not applicable if there are fewer than four visits.14 This is not an ultimate threshold of COC, but is used in practice.
Medication adherence refers to the degree of compliance with medications prescribed by a physician. Accurate tracking of prescription data is essential for analysing medication adherence as well as effectively predicting healthcare costs and utilisation.14 To measure medication adherence, the MPR and proportion of days covered are usually used for analysis.12 The formula for MPR is:
The MPR is usually estimated using prescription data. For example, prescription data were provided with the defined daily dose. An MPR value of 100% means complete medication adherence.
The major limitation of MPR estimation is that it is based on retrospective data review, and patients may have received unrecorded medication. However, owing to the Korean pharmaceutical information system, unrecorded prescriptions cannot occur in NHIS data.12 Another limitation of the MPR method is sharing medicine between family members. However, sharing of medication is likely to be minimal, because each medical appointment is scheduled according to the number of days of medication prescribed in South Korea. The major strength of the MPR method is that by researching diseases containing data on changeable parameters, such as blood pressure, HbA1c, fasting blood glucose, researchers can closely estimate patient health status based on the drugs that they are prescribed. We received professional advice from specialists in internal medicine and cardiology for the selection of antihypertensive drugs and its list (online supplemental table 1).
bmjopen-2023-073404supp001.pdf (389KB, pdf)
Medical complications of hypertension—coronary artery disease, vascular complications, cerebrovascular disease, heart disease and hypertensive nephropathy—were selected based on WHO documentation.1 The WHO documentation also includes cognitive impairment as a type of hypertensive complication,1 but as data on mental examination were unavailable, we were unable to include cognitive impairment as a complication in our study.
Statistical analysis
Explanatory variables influencing COC, MPR and the occurrence of complications in patients with hypertension included sex, age, insurance type, income, outpatient status, COC, MPR level of the patient, number of visits, number of providers, main medical institution and comorbidities. Patients without values for any of these variables were excluded. Subgroup analysis was performed for primary care visits to assess the efficiency of the healthcare system in South Korea. The statistical significance of differences between the groups was assessed using Student’s t-test and analysis of variance. P values<0.05 were regarded as statistically significant. The Kruskal-Wallis test and Wilcoxon rank-sum test were used to compare continuous variables that were not normally distributed, and Fisher’s exact test was used to compare categorical variables between the groups.
Insurance type is divided into two categories: health insurance beneficiaries and medical aid recipients. The national health insurance system in South Korea enables medical aid recipients to obtain free health services because it is based on the lowest level of household income. Income was divided into 10 categories as described in online supplemental table 2.
COC was divided into two categories: high (COC index=1) and low (COC index <1). Most COC-related research in South Korea uses this standard because the overall levels of COC in South Korea are high compared with those in other countries. According to Organisation for Economic Cooperation and Development (OECD) statistics on healthcare utilisation, South Korea has a threefold higher outpatient and inpatient medical care use than the OECD average.22 In this study, the mean COC index was 0.8112, confirming the high level of COC in South Korea. In previous studies, the MPR has generally been divided into three categories (>80%, 50%–80% and <50% of MPR) or two categories (>60% and <60% of MPR).23 24 However, we decided to use five categories (excellent: 80%–100%, good: 60%–80%, normal: 40%–60%, bad: 20%–40% and very bad: 0%–20%) to enable more detailed analysis of the MPR. Outpatient status, number of visits, number of providers and main medical institution are required factors for calculating the COC level.
The term ‘comorbidity’ indicates that patients or participants have different diseases that can affect the results of the study. Comorbidities are sometimes confused with complications, but comorbidities differ from complications because they do not occur as a result of the target disease. Defining comorbidities plays a pivotal role in risk adjustment because confounding can occur if the results are not adjusted for comorbidities.
In this study, we selected diabetes and dyslipidaemia as comorbidities, which are cofactors of cardiovascular disease, cerebrovascular disease and hypertensive nephropathy.25–27 These two types of disease could affect the incidence of hypertensive complications.
Categorical variables associated with the level of COC (low vs high) were compared using the χ2 test. A comparison of complications according to the COC and MPR was performed using Kaplan-Meier survival curves and log-rank tests. The differences in medical complications according to COC and MPR were examined. The Cox proportional hazards model was used to compare the risk. HRs and 95% CIs were estimated using multivariable Cox proportional hazards regression.
The study has been prepared in accordance with the STRengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines. This study was conducted in accordance with the Declaration of Helsinki.
Patient and public involvement
We did not involve patients and public in this study because it was a retrospective study using data from the NHIS database.
Results
The average COC level in the hypertension group was 0.8112. The average MPR in the hypertension group was 73.3%.
General characteristics of patients with hypertension
The patient characteristics are shown in online supplemental table 1. Of the patients, 51 522 (50.3%) were male and 50 997 (49.7%) were female. The over 80-year age group was the largest age group (27.0%), followed by the 70−79 years (21.5%) and 60–69 years (18.1%) age groups. The vast majority of patients (94.0%) were covered by national health insurance. The largest income categories were the 9th–10th decile (27.0%), followed by the 7th–8th decile (21.5%) and the 5th–6th decile (18.1%). The most common outpatient visit categories were 7–9 visits (29.7%), followed by 10–12 visits (29.5%) and ≥13 visits (25.0%). Of the patients, 50.9% visited only one provider and 31.0% visited two providers. The majority of patients visited clinics (70.8%). The most common comorbidities were dyslipidaemia (49.8%) and diabetes (28.7%). Approximately half the patients (50.9%) had a high level of COC. The majority of patients (55.5%) had an excellent MPR. The most frequent years of diagnosis were 2004 (10.1%), 2005 (12.1%) and 2006 (10.1%).
Risk of complications of hypertension according to the COC and MPR level
Compared with the high COC group, participants in the low COC group had a significantly higher risk of complications (HR 1.14, 95% CI 1.10 to 1.17) (table 1).
Table 1.
Risk of complications of hypertension according to the COC level
| COC level | No of patients | No of events | IR per 1000 PYR | HR* (95% CI) | P value |
| High | 52 179 | 7143 | 15.4 | Ref | |
| Low | 50 340 | 8142 | 17.7 | 1.14 (1.10 to 1.17)† | <0.001 |
*Adjusted for sex, age, insurance type, income, number of visits, number of providers, level of hospital and comorbidities
†p<0.001.
COC, continuity of care; IR, incidence rate; PYR, person-years at risk.
Compared with the excellent MPR group, the risk of developing hypertensive complications was significantly higher in the good, normal, bad and very bad MPR groups (table 2).
Table 2.
Risk of hypertensive complications according to the MPR level
| MPR level | No of patients | No of events | IR per 1000 PYR | HR* (95% CI) | P value |
| Excellent | 56 939 | 7143 | 14.1 | Ref | |
| Good | 16 012 | 2695 | 17.9 | 1.24 (1.18 to 1.29)† | <0.001 |
| Normal | 11 808 | 2146 | 19.5 | 1.36 (1.29 to 1.42)† | <0.001 |
| Bad | 9996 | 1834 | 20.3 | 1.42 (1.35 to 1.50)† | <0.001 |
| Very bad | 7764 | 1467 | 21.4 | 1.50 (1.42 to 1.59)† | <0.001 |
*Adjusted for sex, age, insurance type, income, number of visits, number of providers, level of hospital and Comorbidities
†p<0.001.
IR, incidence rate; MPR, medication possession ratio; PYR, person-years at risk.
Risk of specific types of hypertension complication according to the COC and MPR levels
Kaplan-Meier survival curves showing the time until complications occurred according to the COC and MPR are shown in online supplemental figures 1 and 2, respectively. The risks of developing coronary artery disease, vascular complications, cerebrovascular disease, heart disease and hypertensive nephropathy according to each COC and MPR level are shown in tables 3 and 4, respectively. Patients with diabetes and high cholesterol had a higher incidence of hypertensive complications than patients without diabetes and high cholesterol, respectively.
Table 3.
Risk of medical complications of hypertension according to the COC level
| Complication | Parameter | COC level | |
| High | Low | ||
| CAD | Events (N) | 2117 | 2350 |
| IR per 1000 PYR | 4.4 | 4.9 | |
| HR* (95% CI) | Ref | 1.10 (1.03 to 1.16)† | |
| P value | – | 0.002 | |
| Vascular complications | Events (N) | 412 | 451 |
| IR per 1000 PYR | 0.8 | 0.9 | |
| HR* (95% CI) | Ref | 1.07 (0.94 to 1.23) | |
| P value | – | 0.302 | |
| Cerebrovascular disease | Events (N) | 3639 | 4178 |
| IR per 1000 PYR | 7.6 | 8.7 | |
| HR* (95% CI) | Ref | 1.14 (1.09 to 1.19)‡ | |
| P value | – | <0.001 | |
| Heart disease | Events (N) | 2602 | 2951 |
| IR per 1000 PYR | 5.4 | 6.1 | |
| HR* (95% CI) | Ref | 1.11 (1.06 to 1.17)‡ | |
| P value | – | <0.001 | |
| Hypertensive nephropathy | Events (N) | 716 | 768 |
| IR per 1000 PYR | 1.5 | 1.6 | |
| HR* (95% CI) | Ref | 1.05 (0.95 to 1.16) | |
| P value | – | 0.367 | |
*Adjusted for sex, age, insurance type, income, number of visits, number of providers, level of hospital and comorbidities
†p<0.01
‡p<0.001
CAD, coronary artery disease; COC, continuity of care; IR, incidence rate; N, Number; PYR, person-years at risk.
Table 4.
Risk of medical complications of hypertension according to the MPR level
| Complication | Parameter | MPR level | ||||
| Excellent | Good | Normal | Bad | Very bad | ||
| CAD | Events (N) | 2081 | 811 | 635 | 535 | 405 |
| IR per 1000 PYR | 4 | 5.1 | 5.5 | 5.6 | 5.5 | |
| HR* (95% CI) | Ref | 1.26 (1.16 to 1.37)§ | 1.35 (1.23 to 1.47)§ | 1.38 (1.26 to 1.52)§ | 1.38 (1.24 to 1.53)§ | |
| P value | – | <0.001 | <0.001 | <0.001 | <0.001 | |
| Vascular complications | Events (N) | 393 | 154 | 120 | 107 | 89 |
| IR per 1000 PYR | 0.7 | 1 | 1 | 1.1 | 1.2 | |
| HR* (95% CI) | Ref | 1.25 (1.04 to 1.51)† | 1.33 (1.08 to 1.63)‡ |
1.45 (1.17 to 1.79)§ | 1.59 (1.26 to 2.00)§ | |
| P value | – | 0.018 | 0.007 | 0.001 | <0.001 | |
| Cerebrovascular disease | Events (N) | 3613 | 1312 | 1120 | 997 | 775 |
| IR per 1000 PYR | 6.9 | 8.4 | 9.8 | 10.6 | 10.8 | |
| HR* (95% CI) | Ref | 1.18 (1.11 to 1.26) § | 1.38 (1.29 to 1.47) § | 1.51 (1.41 to 1.62) § | 1.54 (1.43 to 1.67) § | |
| P value | – | <0.001 | <0.001 | <0.001 | <0.001 | |
| Heart disease | Events (N) | 2585 | 981 | 788 | 659 | 540 |
| IR per 1000 PYR | 4.9 | 6.2 | 6.8 | 6.9 | 7.4 | |
| HR* (95% CI) | Ref | 1.21 (1.13 to 1.30)§ | 1.33 (1.23 to 1.44)§ | 1.36 (1.25 to 1.48)§ | 1.47 (1.34 to 1.62)§ | |
| P value | – | <0.001 | <0.001 | <0.001 | <0.001 | |
| Hypertensive nephropathy | Events (N) | 633 | 278 | 232 | 194 | 147 |
| IR per 1000 PYR | 1.2 | 1.7 | 2 | 2 | 2 | |
| HR* (95% CI) | Ref | 1.39 (1.21 to 1.60)§ | 1.58 (1.36 to 1.84)§ | 1.62 (1.38 to 1.90)§ | 1.62 (1.35 to 1.94)§ | |
| P value | – | <0.001 | <0.001 | <0.001 | <0.001 | |
*Adjusted for sex, age, insurance type, income, number of visits, number of providers, level of hospital and comorbidities
†p<.05
‡p<.01
§p<0.001
CAD, coronary artery disease; MPR, medication possession ratio; N, Number; PYR, person-years at risk.
The risk of coronary artery disease was significantly higher in the low than in the high COC group (HR 1.10, 95% CI 1.03 to 1.16) (table 3). Compared with the excellent MPR group, the risk of coronary artery disease was significantly higher in the good, normal, bad and very bad MPR groups (table 4).
The risk of vascular complications did not differ significantly according to the COC level (table 3). Compared with the excellent MPR group, the risk of vascular complications was significantly higher in the good, normal, bad and very bad MPR groups (table 4).
The risk of cerebrovascular disease was significantly higher in the low continuity group than the high COC group (HR 1.14, 95% CI 1.09 to 1.19) (table 3). Compared with the excellent MPR group, the risk of cerebrovascular disease was significantly higher in the good, normal, bad and very bad MPR groups (table 4).
The risk of heart disease was significantly higher in the low COC than in the high COC group (HR 1.11, 95% CI 1.06 to 1.17) (table 3). Compared with the excellent MPR group, the risk of heart disease was significantly higher in the good, normal, bad and very bad MPR groups (table 4).
The risk of hypertensive nephropathy did not differ significantly according to the COC level (table 3). Compared with the excellent MPR group, the risk of hypertensive nephropathy was significantly higher in the good, normal, bad and very bad MPR groups (table 4).
Subgroup analysis of risk of medical complications according to the COC and MPR levels in primary care clinics
A subgroup analysis of the risk of medical complications according to the COC level and MPR in patients with hypertension attending primary care clinics showed that the risk of developing complications was significantly higher in the low than in the high COC group (HR 1.16, 95% CI 1.12 to 1.21). Compared with the excellent MPR group, the risk of developing hypertensive complications was significantly higher in the good, normal, bad and very bad MPR groups. Compared with patients who had 4–6 visits, the risk of developing medical complications was significantly lower in patients with 7–9, 10–12 or ≥13 visits (online supplemental table 3).
Discussion
In this study, we analysed the differences in hypertensive complications according to COC and medication adherence in patients with hypertension. The study highlights the fact that COC and MPR were associated with the occurrence of complications caused by hypertension. Overall, for patients with hypertension in the low as compared with the high COC group, the risk of complications was significantly higher. In this study, the order of establishing health policies related to COC, MPR can increase the response and lower the risk of long-term complications within the first 2 years of diagnosis of hypertension. Similarly, the risk of developing coronary artery disease, cerebrovascular disease and heart disease was greater in the low as compared with the high COC group. Regarding overall medication adherence, in comparison to the excellent MPR group (80%–100%), the good (60%–79%), normal (40%–59%), bad (20%–39%) and very bad groups (0%–19%) were at significantly higher risk of developing hypertensive complications, such as coronary artery disease, vascular complications, cerebrovascular disease, heart disease and hypertensive nephropathy.
Other COC and MPR studies have found that patients with low medication adherence are more likely to result in progress to inpatient or mortality (HR 1.24, 95% CI 1.18 to 1.29). The differences were attributed to the type of antihypertensive medication, follow-up period and the differences in the definition of medication adherence. We overcame these limitations because of the 18-year follow-up period.
Another MPR study showed that low medication adherence is more likely to result in progress to inpatient or mortality (HR 1.57, 95% CI 1.40 to 1.76). This result is similar to that of our study.28
Other COC and MPR studies focused on hypertension and diabetes, and found that for hypertension, low COC medication adherence is more likely to result in progress to death in hospitalised patients (HR 1.66, 95% CI 1.55 to 1.77; HR 1.14, 95% CI 1.08 to 1.20, respectively). Low COC and medication adherence are more likely to result in progress to hospitalisation or death among outpatients (HR 1.67, 95% CI 1.47 to 1.90). The differences were attributed to the fact that the incidence of hypertensive complications was not among their outcomes, and the reason for hospitalisation varied, potentially causing the overestimation of the results.
This study had several strengths. First, the study obtained population representativeness because we utilised NHIS data and the subscription of national health insurance is legally mandatory (covering approximately 99.7%) in South Korea. Second, the disease was selected from AHRQ standards of ACSCs and hypertensive complications were selected according to the definitions from WHO.1 Third, there is a standard in ACSCs related to hypertension (no cardiac procedures included), which is often omitted in previous studies, and this is the first attempt at a long-term (18-year) analysis of ACSCs (hypertension) with a clearer definition of patients and its incidence rate of complications.
However, this study also had several limitations. First, as only the COC and medication adherence in the initial 2 years were measured, follow-up after 2 years was not reflected in the effects of changes in care. Second, the risk of complications or blood pressure level was not analysed in this study. Third, whether other underlying diseases or external factors may affect the results, such as familial aggregation, the levels of blood pressure and overprescription of drugs, of this study could not be fully excluded. Fourth, owing to the retrospective nature of this observational study, misclassification or recall bias may impact the validity of this study. Finally, this study can be elevated to mortality or factor study. The case–control or prospective cohort study to elucidate the association between COC, MPR levels and the mortality of patients with hypertensive complications with its characteristics.
There are several policies for the management of ACSCs worldwide. For example, there are policies for diabetes, cervical cancer and asthma in Australia and policies for depression, cancer and asthma in the UK and USA; it is possible to provide primary care in a timely manner and manage chronic diseases more efficiently by including more diseases subject to chronic disease management in the ACSCs.29 Therefore, a follow-up study on the differences in the risk of complications according to changes in care should be conducted in the future.
This study sheds light on the association between COC and medication adherence and the incidence of hypertensive complications, such as coronary artery disease and heart disease. The continuous management of blood pressure can be beneficial to prevent hypertensive complications among patients with hypertension. The implication should be based on subgroup analysis (online supplemental table 3). Visiting primary care facilities is adequately beneficial to patients with hypertension. Therefore, the Korean government should establish health policies related to chronic diseases that need management with a view to long-term care. Moreover, because of its unique structure (lack of a gatekeeper system (referral system)), the healthcare system of South Korea is facing a financial shortage. Future studies should compare the cost-effectiveness of care provided by different types of medical institutions, such as general hospitals and clinics.
bmjopen-2023-073404supp002.pdf (56.3KB, pdf)
Supplementary Material
Acknowledgments
We thank Editage (www.editage.co.kr) for English language editing.
Footnotes
Contributors: Conceptualisation: DK, methodology: DK, software: DK, data curation: DK, writing—original draft preparation: JC, visualisation: JC, investigation: DK and JC, supervision: JC, validation: JC, writing—reviewing and editing: DK and JC, Guarantor: JC.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request Raw data were generated by the National Health Insurance Service. Derived data supporting the findings of this study are available from the corresponding author, JC, on request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants but ethics approval for the study was obtained from the Institutional Review Board at Korea University (IRB document no. KUIRB-2021-0333-01). Informed consent was not required due to the retrospective nature of the study. Participants gave informed consent to participate in the study before taking part.
References
- 1.World Health Organisation . Hypertension. Available: https://www.who.int/health-topics/hypertension#tab=tab_1 [Accessed 27 Nov 2022].
- 2.World health Organisation . More than 700 million people with untreated hypertension. Available: https://www.who.int/news/item/25-08-2021-more-than-700-million-people-with-untreated-hypertension [Accessed 27 Nov 2022].
- 3.Forouzanfar MH, Liu P, Roth GA, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA 2017;317:165–82. 10.1001/jama.2016.19043 [DOI] [PubMed] [Google Scholar]
- 4.Liu J, Bu X, Wei L, et al. Global burden of cardiovascular diseases attributable to hypertension in young adults from 1990 to 2019. J Hypertens 2021;39:2488–96. 10.1097/HJH.0000000000002958 [DOI] [PubMed] [Google Scholar]
- 5.Ansari Z. The concept and usefulness of ambulatory care sensitive conditions as indicators of quality and access to primary health care. Aust J Prim Health 2007;13:91. 10.1071/PY07043 [DOI] [Google Scholar]
- 6.Lin W, Huang I-C, Wang S-L, et al. Continuity of diabetes care is associated with Avoidable hospitalizations: evidence from Taiwan's national health insurance scheme. Int J Qual Health Care 2010;22:3–8. 10.1093/intqhc/mzp059 [DOI] [PubMed] [Google Scholar]
- 7.Billings J, Zeitel L, Lukomnik J, et al. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993;12:162–73. 10.1377/hlthaff.12.1.162 [DOI] [PubMed] [Google Scholar]
- 8.Gao J, Moran E, Li Y-F, et al. Predicting potentially Avoidable hospitalizations. Med Care 2014;52:164–71. 10.1097/MLR.0000000000000041 [DOI] [PubMed] [Google Scholar]
- 9.Laditka JN, Laditka SB, Mastanduno MP. Hospital utilization for ambulatory care sensitive conditions: health outcome disparities associated with race and Ethnicity. Soc Sci Med 2003;57:1429–41. 10.1016/s0277-9536(02)00539-7 [DOI] [PubMed] [Google Scholar]
- 10.Shin S, Song H, Oh S-K, et al. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertens Res 2013;36:1000–5. 10.1038/hr.2013.85 [DOI] [PubMed] [Google Scholar]
- 11.Nam Y, Cho K, Kang H, et al. Greater continuity of care reduces hospital admissions in patients with hypertension: an analysis of nationwide health insurance data in Korea, 2011-2013. Health Policy 2016;120:604–11. 10.1016/j.healthpol.2016.04.012 [DOI] [PubMed] [Google Scholar]
- 12.Gygli N, Zúñiga F, Simon M. Regional variation of potentially Avoidable Hospitalisations in Switzerland: an observational study. BMC Health Serv Res 2021;21:849. 10.1186/s12913-021-06876-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National health insurance service . National health insurance data sharing service. Available: https://nhiss.nhis.or.kr/bd/ab/bdaba012eng.do [Accessed 27 Nov 2022].
- 14.Christakis DA, Wright JA, Koepsell TD, et al. Is greater continuity of care associated with less emergency Department utilization? Pediatrics 1999;103:738–42. 10.1542/peds.103.4.738 [DOI] [PubMed] [Google Scholar]
- 15.Korea S. Statistics Korea – cause of death. Available: https://kostat.go.kr/portal/eng/index.action [Accessed 2 Dec 2022].
- 16.KOSIS. KOSIS: life table. KOSIS . Published December, Available: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B42&conn_path=I2 [Accessed 25 Dec 2023].
- 17.Citro R, Ghosh S, Churgin PG. A fundamental metric for continuity of care: modeling and performance evaluation. IEEE Trans Inf Technol Biomed 1997;1:189–204. 10.1109/4233.654862 [DOI] [PubMed] [Google Scholar]
- 18.Tom J, Tseng C, Davis J, et al. Missed well-child care visits, low continuity of care, and risk of ambulatory care-sensitive hospitalizations in young children. Arch Pediatr Adolesc Med 2010;164:1052–8. 10.1001/archpediatrics.2010.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hong JS, Kim JY, Kang HC. Continuity of ambulatory care among adult patients for type 2 diabetes and its associated factors in Korea. Korean Journal of Health Policy and Administration 2009;19:51–70. 10.4332/KJHPA.2009.19.2.051 [DOI] [Google Scholar]
- 20.Shortell SM. Continuity of medical care: conceptualization and measurement. Med Care 1976;14:377–91. 10.1097/00005650-197605000-00001 [DOI] [PubMed] [Google Scholar]
- 21.Bice TW, Boxerman SB. A quantitative measure of continuity of care. Med Care 1977;15:347–9. 10.1097/00005650-197704000-00010 [DOI] [PubMed] [Google Scholar]
- 22.Statistics office, Korea. The number of outpatient visit in Korea. Available: https://www.index.go.kr/unify/idx-info.do?idxCd=4240 [Accessed 10 Apr 2023].
- 23.Pittman DG, Chen W, Bowlin SJ, et al. Adherence to Statins, subsequent Healthcare costs, and cardiovascular hospitalizations. Am J Cardiol 2011;107:1662–6. 10.1016/j.amjcard.2011.01.052 [DOI] [PubMed] [Google Scholar]
- 24.Han E, Suh D-C, Lee S-M, et al. The impact of medication adherence on health outcomes for chronic metabolic diseases: a retrospective cohort study. Res Social Adm Pharm 2014;10:e87–98. 10.1016/j.sapharm.2014.02.001 [DOI] [PubMed] [Google Scholar]
- 25.World health organization. cardiovascular diseases (Cvds). World health organization. Available: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) [Accessed 27 May 2023].
- 26.Lee H-Y, Shin J, Kim G-H, et al. Korean society of hypertension guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens 2019;25:20. 10.1186/s40885-019-0124-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burnier M, Damianaki A. Hypertension as cardiovascular risk factor in chronic kidney disease. Circ Res 2023;132:1050–63. 10.1161/CIRCRESAHA.122.321762 [DOI] [PubMed] [Google Scholar]
- 28.Shin S, Song H, Oh SK, et al. Effect of antihypertensive medication adherence on hospitalization for cardiovascular disease and mortality in hypertensive patients. Hypertens Res 2013;36:1000–5. 10.1038/hr.2013.85 [DOI] [PubMed] [Google Scholar]
- 29.Santos R, Rice N, Gravelle H. Patterns of emergency admissions for ambulatory care sensitive conditions: a spatial cross-sectional analysis of observational data. BMJ Open 2020;10:e039910. 10.1136/bmjopen-2020-039910 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-073404supp001.pdf (389KB, pdf)
bmjopen-2023-073404supp002.pdf (56.3KB, pdf)
Data Availability Statement
Data are available on reasonable request Raw data were generated by the National Health Insurance Service. Derived data supporting the findings of this study are available from the corresponding author, JC, on request.