Abstract
Racial and ethnic disparities in COVID-19 incidence are pronounced in underserved U.S./Mexico border communities. Working and living environments in these communities can lead to increased risk of COVID-19 infection and transmission, and this increased risk is exacerbated by lack of access to testing. As part of designing a community and culturally tailored COVID-19 testing program, we surveyed community members in the San Ysidro border region. The purpose of our study was to characterize knowledge, attitudes, and beliefs of prenatal patients, prenatal caregivers, and pediatric caregivers at a Federally Qualified Health Center (FHQC) in the San Ysidro region regarding perceived risk of COVID-19 infection and access to testing. A cross-sectional survey was used to collect information on experiences accessing COVID-19 testing and perceived risk of COVID-19 infection within San Ysidro between December 29, 2020 and April 2, 2021. A total of 179 surveys were analyzed. Most participants identified as female (85%) and as Mexican/Mexican American (75%). Over half (56%) were between the age of 25 and 34 years old. Perceived Risk: 37% reported moderate to high risk of COVID-19 infection, whereas 50% reported their risk low to none. Testing Experience: Approximately 68% reported previously being tested for COVID-19. Among those tested, 97% reported having very easy or easy access to testing. Reasons for not testing included limited appointment availability, cost, not feeling sick, and concern about risk of infection while at a testing facility. This study is an important first step to understand the COVID-19 risk perceptions and testing access among patients and community members living near the U.S./Mexico border in San Ysidro, California.
Keywords: COVID-19, U.S./Mexico border, Access, Risk perception, Testing strategies, Disease burden
In a US/Mexico border community with one of the highest rates of COVID-19 in San Diego County, half of the individuals surveyed reported their perceived risk of acquiring COVID-19 infection as low to none.
Implications.
Practice: Needs assessments to describe the knowledge, attitudes, and health beliefs of U.S./Mexico border communities are vital in the development and implementation of COVID-19 testing programs.
Policy: Policymakers who want to reduce the morbidity and mortality among Black, Indigenous, and People of Color communities affected by COVID-19 must consider cultural factors that influence COVID-19 preventative behavior among the U.S./Mexico border.
Research: Future research should be aimed at identifying community and culture specific barriers to COVID-19 testing and the development of effective strategies for increasing access to testing in border regions of the U.S.
INTRODUCTION
The United States (U.S.) continues to lead the world with the largest number of infections and deaths due to the Coronavirus Disease 2019 (COVID-19), with more than 79 million infections and approximately 1 million deaths between January 2020 and June 2022 [1]. Racial and ethnic disparities in COVID-19 incidence have been observed during the pandemic specifically among underserved Latino, Black, Indigenous, and People of Color (BIPOC) communities. More than half, (64%) of COVID-19 cases are among Latino and Black individuals, even though these groups comprise about a third of the total U.S. population [2]. These groups also see a higher number of hospitalizations and deaths in the U.S. compared to non-Hispanic individuals [3–5]. These disparities are often compounded by social and contextual factors such as lower access to healthcare and higher rates of poverty [5–7]. Further, Latino and BIPOC communities are also overrepresented in essential industries (e.g., caregivers in nursing homes, transportation, food service, and hospitality) heightening their risk of infection and transmission [8–11]. These occupational hazards are intensified for those in the hospitality industry as only 55% of these essential workers have access to paid sick leave [12]. Communities with higher racial and ethnic minority populations also experience higher housing density, more housing insecurity, and live in multigenerational households, which prevents physical distancing thereby increasing the risk of COVID-19 infection and transmission [13–15]. These factors are more prevalent among U.S./Mexico border communities.
San Ysidro is one such border region that has experienced high rates of health comorbidities linked to poor COVID-19 outcomes. The district of San Ysidro, adjacent to the U.S./Mexico border in the southernmost part of the city of San Diego, is one of the busiest international border crossing facilities in the world with an estimated 70,000 vehicles and 20,000 pedestrians crossing each day [16, 17]. It is one of the poorest districts in the county of San Diego where 32% of household incomes are less than $29,999 per year [18]. San Ysidro is home to a young, culturally, and linguistically diverse population of 26,082 residents of which 82.6% are Latino [18]. It also has the largest number of pre- and middle school children in San Diego with 1/3 of the population under 18 years of age [18]. While a relatively young community, San Ysidro has been disproportionately impacted by COVID-19, with the highest incidence of COVID-19 cases, approximately 35% more than any district in County of San Diego [19]. The response to the pandemic in San Ysidro has been hampered by multiple factors, including the physical distance from major testing centers and the initial shortage of COVID-19 testing coupled with long turnaround times for results. Furthermore, a large fraction of San Ysidro households consists of multigenerational families living together making this community particularly vulnerable to high rates of COVID-19 transmission and morbidity and underscoring the need for ample testing geared toward families with children.
While there are community-wide concerns for access to testing across San Ysidro, there is a unique need to address access to testing for prenatal and pediatric populations [20, 21]. There is reported increase in COVID-19 related mortality and morbidity among pregnant women, and pregnant women and children are considered high risk for contracting infectious disease during outbreaks [20, 22, 23]. In line with this, pregnant women also perceive themselves to be more vulnerable to the COVID-19 pandemic [24]. Despite being considered a high-risk population, prenatal women have been universally excluded from clinical trials [25–27], leaving regular COVID-19 testing as the primary prevention method for these communities. Yet information and access to testing have historically been lacking and patients have reported not knowing about COVID-19 prevention resources and continue to look for and receive information via social media sites [28]. Thus, there is a need to provide timely, accurate, and culturally appropriate information coupled with increased access to COVID-19 testing in these populations. We partnered with a Federally Qualified Health Center (FQHC), which continued regular prenatal and pediatric care during the pandemic that created an excellent opportunity to engage families in our COVID-19 needs assessment in an otherwise hard-to-reach population.
We also engaged multiple stakeholders consisting of community members, community health center partners, and academic research partners to evaluate the needs for a community-driven COVID-19 testing program for the San Ysidro community. Based on initial discussions, these stakeholders reported limited access to culturally tailored messaging including Spanish materials, difficulty finding testing sites, transportation issues, and language barriers. As part of the initial phase of this research, we conducted a needs assessment among prenatal patients and prenatal and pediatric caregivers at the FQHC in the San Ysidro border region during the COVID-19 pandemic to better understand COVID-19-related knowledge, attitudes, and health beliefs. This paper describes survey findings from the needs assessment in order to understand how these factors can facilitate or serve as barriers to the co-creation of a culturally tailored COVID-19 testing program.
METHODS
A cross-sectional survey was used to collect information on demographics, experiences accessing COVID-19 testing at a FQHC in San Ysidro, and barriers to COVID-19 testing within the San Ysidro community. These data were drawn from a larger study called, Community-driven Optimization of COVID-19 testing to Reach and Engage underserved Areas for Testing Equity (CO-CREATE). CO-CREATE is a two-year study funded through the National Institutes of Health Rapid Acceleration of Diagnostics for Underserved Population initiative. For more information about this study, please see Stadnick et al. [29]. Survey items were drawn from the NIH-funded Community Engagement Alliance (CEAL) Against COVID-19 Common Survey (version 1) developed by the National Needs Assessment and Evaluation Working Group for the CEAL Initiative [30]. The survey was available in both English and Spanish.
The study sample was recruited from a patient population from the FQHC along with their caregivers or familial supporters. Participants were recruited into three cohorts and categorized based on self-endorsement of the role that best described them. Cohort 1 was defined as patients that were at least 13 years old and either currently pregnant or had delivered within 6 months of survey completion. Cohort 2 was individuals at least 18 years old who were supporters or caregivers of pre-/post-natal patients. Cohort 3 was individuals 18 years and older who were supporters or caregivers of pediatric patients. All study procedures were approved by the University of California, San Diego Institutional Review Board and all participants provided electronic or verbal consent at the start of the survey.
Survey recruitment and administration occurred between December 29, 2020 and April 2, 2021. Four primary recruitment methods were used. The initial recruitment method was initiated by a phone call to a sample of patients provided by the FQHC who met all the Cohort 1 inclusion criteria. These individuals were FQHC patients ages 18 years or older who received care at the women’s health clinic, had at least one clinic visit within the past year at the FQHC, and were reported as pregnant in their health records in the last year; if the individual was currently pregnant, the age requirement was 13 years or older. We note that in California, according to California Family Code § 6925, “A minor may consent to medical care related to the prevention or treatment of pregnancy.” Therefore, pregnant women between the ages of 13 and 17 years old were eligible for enrollment and able to independently consent to participation. During the recruitment calls, trained clinical research staff provided information about the study, reviewed the consent procedures, and obtained verbal consent for those interested in participating. Phone calls and survey administration were offered in Spanish or English, based on the participant’s language preference. If the participant was unable to complete the survey during the call, a link to the electronic version of the survey was sent via email or text message in the participant’s preferred language. The second recruitment strategy was undertaken in person at the FQHC by clinical research staff which included those who met Cohort 1, Cohort 2, and Cohort 3 inclusion criteria. Participants had the option to complete the survey onsite via email or text message. Further recruitment strategies included posting and distributing study flyers at the FQHC and encouraging participants and non-participants to invite other community members that met the inclusion criteria to complete the survey via email, phone, or in person. Upon completion of the survey, participants received a $25 gift card incentive.
Statistical analysis
Data collected were described using frequencies and presented graphically with cumulative bar charts, including missing data. Categorical data were compared across cohort and sex using Person’s chi-square. Data were analyzed using STATA 17 (College Station, TX, U.S.). To enable collaborative analysis of survey results within the project team, we also used Survey Analysis via Visual Exploration (SuAVE) [31]. The SuAVE Co-Create applications were generated directly from REDCap [32] (where the survey responses were managed), using a Python script. The SuAVE platform enables online visual analysis of survey data, using bar charts, cross-tabs, and other animated data views, and additional statistical analysis using Jupyter notebooks. Users can explore and compare distributions of responses in different user-defined cohorts, zoom in to individual cases and outliers and zoom out to view the larger picture. They can also save and annotate data view snapshots and share them with the project team. Furthermore, the SuAVE platform made it possible to share data with other interested researchers [33] (after personally identifiable information has been redacted).
RESULTS
As total of 204 surveys were administered, 22 participants did not provide consent to share their survey data, and 3 surveys were determined to be duplicates, leaving 179 surveys for analysis. We reported the results first by demographics and living situation followed by self-reported perception of COVID-19 risk, perceptions of COVID-19 exposure and severity, and testing experience.
Demographics and living situation
Out of the 179 participants, 84 (47%) identified as a FQHC prenatal patient (Cohort 1), 33 (18%) identified as a friend or family member of a prenatal patient (Cohort 2), and 62 (35%) identified as a family member or caregiver of a pediatric patient (Cohort 3). Approximately half (47%) of the participants indicated that they lived in San Ysidro and 153 participants (85%) identified as female. Most of the respondents classified themselves as Mexican/Mexican American or American/Chicano 134 (75%). Most participants were less than 35 years of age, with over half (56%) reporting their age between 25 and 34 years old, and (20%) between 18 and 24 years. Additional demographic details, including race, level of education, and employment status, are reported by cohort in Table 1.
Table 1.
Sample demographics, stratified by cohort, for participants who completed the survey between December 2020 and April 2021 (n = 179)
| Cohort 1: Prenatal Patient | Cohort 2: Prenatal Supporter | Cohort 3: Pediatric Supporter | Total | |
|---|---|---|---|---|
| Sample Characteristics | n = 84, (%)* | n = 33, (%) | n = 62, (%) | n = 179, (%) |
| Live in San Ysidro | ||||
| Yes | 47 (56) | 15 (45) | 23 (37) | 85 (48) |
| No | 31 (37) | 16 (48) | 34 (55) | 81 (45) |
| Prefer not to answer | 2 (2) | 1 (3) | 3 (5) | 6 (3) |
| Missing | 4 (5) | 1 (3) | 2 (3) | 7 (4) |
| Sex | ||||
| Female | 80 (95) | 22 (67) | 51 (82) | 153 (85) |
| Male | 0 (0) | 10 (30) | 10 (16) | 20 (11) |
| Prefer not to answer | 0 (0) | 0 (0) | 1 (2) | 1 (1) |
| Missing | 4 (5) | 1 (3) | 0 (0) | 5 (3) |
| Age | ||||
| 13–17 | 2 (2) | 0 (0) | 2 (3) | 4 (2) |
| 18–24 | 15 (18) | 8 (24) | 12 (19) | 35 (20) |
| 25–34 | 55 (65) | 16 (48) | 26 (42) | 97 (54) |
| 35–44 | 8 (10) | 2 (6) | 15 (24) | 25 (14) |
| 45–64 | 0 (0) | 5 (15) | 6 (10) | 11 (6) |
| 65–74 | 0 (0) | 1 (3) | 1 (2) | 2 (1) |
| Missing | 4 (5) | 1 (3) | 0 (0) | 5 (3) |
| Hispanic origin | ||||
| Not of Hispanic, Latino, or Spanish origin | 3 (4) | 0 (0) | 3 (5) | 6 (3) |
| Mexican, Mexican American, Chicano | 58 (69) | 26 (79) | 50 (81) | 134 (75) |
| Puerto Rican | 0 (0) | 0 (0) | 3 (5) | 3 (2) |
| Another Hispanic, Latino, or Spanish origin | 10 (12) | 3 (9) | 2 (3) | 15 (8) |
| Prefer not to answer | 7 (8) | 3 (9) | 4 (6) | 14 (8) |
| Missing | 6 (7) | 1 (3) | 0 (0) | 7 (4) |
| Race | ||||
| American Indian or Alaska Native | 1 (1) | 0 (0) | 1 (2) | 2 (1) |
| Filipino | 1 (1) | 0 (0) | 0 (0) | 1 (1) |
| Korean | 0 (0) | 0 (0) | 1 (2) | 1 (1) |
| Native Hawaiian | 1 (1) | 0 (0) | 0 (0) | 1 (1) |
| White | 39 (46) | 15 (45) | 31 (50) | 85 (47) |
| Prefer not to answer | 40 (48) | 11 (33) | 14 (23) | 45 (25) |
| Other | 14 (17) | 8 (24) | 14 (23) | 36 (20) |
| Education | ||||
| Less than high school | 11 (13) | 6 (18) | 9 (15) | 26 (15) |
| Some high school | 16 (19) | 5 (15) | 11 (17) | 32 (18) |
| High school graduate or equivalent | 27 (32) | 6 (18) | 20 (32) | 53 (30) |
| Some college | 11 (13) | 7 (21) | 10 (16) | 28 (16) |
| Associate degree | 2 (2) | 0 (0) | 4 (6) | 6 (3) |
| Bachelor’s degree | 10 (12) | 7 (21) | 5 (8) | 22 (12) |
| Graduate degree | 0 (0) | 1 (3) | 0 (0) | 1 (1) |
| Prefer not to answer | 3 (4) | 0 (0) | 3 (5) | 6 (3) |
| Missing | 4 (5) | 1 (3) | 0 (0) | 5 (3) |
| Employment | ||||
| Full time | 16 (19) | 8 (24) | 17 (27) | 41 (23) |
| Part time | 7 (8) | 6 (18) | 6 (10) | 19 (11) |
| Disabled | 3 (4) | 3 (9) | 2 (3) | 8 (4) |
| Not employed or looking for work | 23 (27) | 1 (3) | 18 (29) | 42 (23) |
| Not employed and looking for work | 20 (24) | 12 (36) | 16 (26) | 48 (27) |
| Other | 10 (12) | 2 (6) | 1 (2) | 13 (7) |
| Missing | 5 (6) | 1 (3) | 2 (3) | 8 (4) |
* Percent rounded to nearest whole number.
A majority, 112 (65%) of participants, reported living in a household with children under the age of 18. Third-four percent of respondents (61 respondents) reported adults in the home that were considered essential workers and 9 of those individuals were first responders or health care workers that worked in facilities treating COVID-19. Table 2 displays participants living situations stratified by cohort. There was no statistical difference across these groups.
Table 2.
COVID-19 living situation, stratified by cohort, for participants who completed the survey between December 2020 and April 2021 (n = 179)
| Cohort 1: Prenatal Patient | Cohort 2: Prenatal Supporter | Cohort 3: Pediatric Supporter | Total | |
|---|---|---|---|---|
| Sample Characteristics | n=84, (%)* | n=33, (%) | n=62, (%) | n=179, (%) |
| Living situation over the past month | ||||
| In a household with other people including children < 18 years old | 53 (63) | 15 (45) | 44 (71) | 112 (63) |
| Alone in home | 12 (14) | 7 (21) | 6 (10) | 25 (14) |
| In a household with other adults, but no children under 18 years old | 8 (10) | 9 (27) | 1 (2) | 18 (10) |
| Temporarily staying with a relative or friend | 5 (6) | 1 (3) | 4 (6) | 10 (6) |
| Other/missing | 6 (7) | 1 (3) | 7 (11) | 14 (8) |
| Additional adults ≥18 living in house | ||||
| 0 | 5 (6) | 2 (6) | 2 (3) | 9 (5) |
| 1 | 24 (29) | 12 (36) | 25 (40) | 61 (34) |
| 2 | 25 (30) | 9 (27) | 16 (26) | 50 (28) |
| 3 | 14 (17) | 8 (24) | 10 (16) | 32 (18) |
| 4–5 | 7 (8) | 1 (3) | 3 (5) | 11 (6) |
| > 6 | 2 (2) | 0 (0) | 0 (0) | 2 (1) |
| Missing | 7 (8) | 1 (3) | 4 (6) | 14 (8) |
| Children <18 living in house | ||||
| 0 | 5 (6) | 11 (33) | 1 (2) | 17 (10) |
| 1 | 22 (26) | 7 (21) | 12 (19) | 41 (23) |
| 2 | 25 (30) | 10 (30) | 25 (40) | 60 (34) |
| 3 | 18 (21) | 2 (6) | 13 (21) | 33 (18) |
| 5-Apr | 6 (7) | 0 (0) | 6 (10) | 12 (7) |
| > 6 | 3 (4) | 0 (0) | 0 (0) | 3 (2) |
| Missing | 5 (6) | 3 (9) | 5 (8) | 13 (7) |
| Adults working in essential industries | 30 (36) | 11(33) | 20 (32) | 61 (34) |
| First responder/healthcare provider/worker in facility treating COVID-19 | 3 (4) | 3 (9) | 3 (5) | 9 (5) |
* Percent rounded to nearest whole number.
Perceived COVID-19 risk attitudes
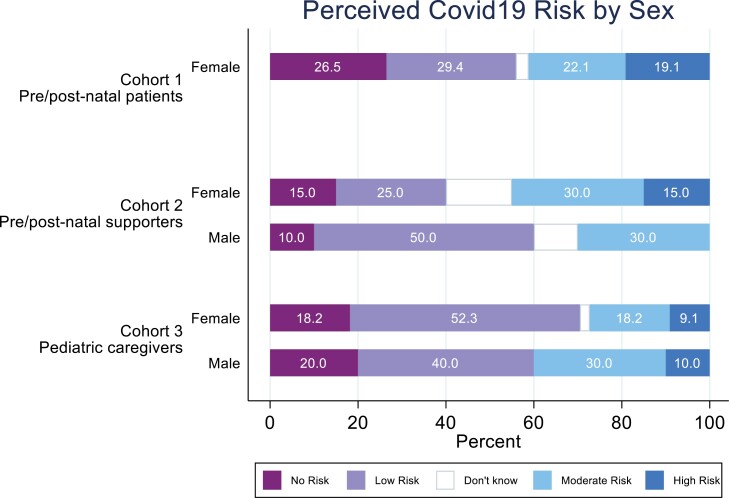
Survey respondents were asked to report their perceived risk of becoming infected with COVID-19 along with risk of disease severity. Overall, 37% (67 respondents) rated their risk of acquiring COVID-19 as moderate to high. Fifty percent (90 respondents) rated their risk of getting COVID-19 as low to none. There was no statistically significant relationship between risk perception and cohort (Pearson chi = 4.1; p = 0.13). See Fig. 1.
Fig 1.
Perceived COVID-19 risk by sex and cohort among survey participants between December 29, 2020 and April 2, 2021 within a Federally Qualified Health Center in San Ysidro (n = 179).
When asked, “I know what actions to take to prevent myself and my family from becoming infected with COVID-19,” 55 prenatal patients (65%) strongly agreed while only 8 (10%) strongly disagreed. Among prenatal supporters 17 (52%) strongly agreed while only 1 (3%) strongly disagreed. Among pediatric supporters 36 (58%) strongly agreed while 5 (8%) strongly disagreed.
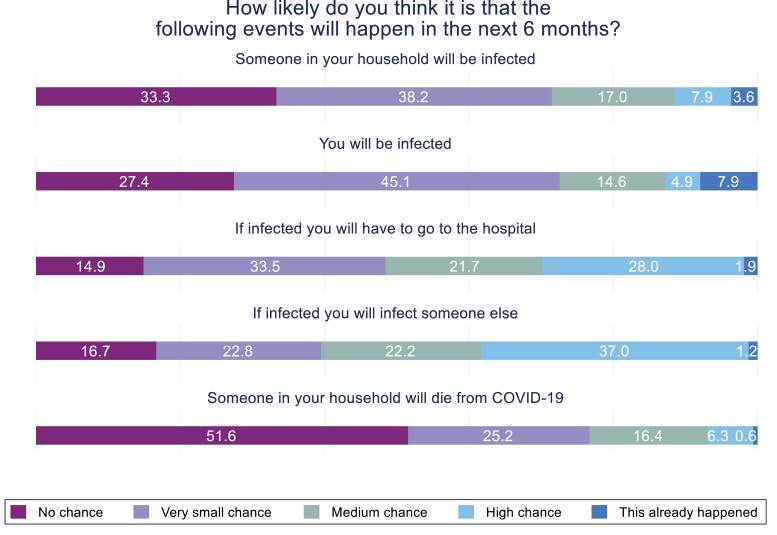
When asked how likely in the next six months participants thought they would become infected with COVID-19, 13 individuals (7%) indicated that they had already been infected with COVID-19. Six respondents (3%) indicated that someone in their household had already been infected with COVID-19, three (1.7%) reported that they had already been hospitalized with COVID-19, and one (0.6%) respondent indicated that a person from their household had already died from COVID-19.
Excluding the individuals who reported a COVID-19 infection, hospitalization, or death, respondents indicated their perceived likelihood of risk and/or complication from a COVID-19 infection within the next six months (Fig. 2). About 18% (36 respondents) thought that there was a medium to high chance they would be infected with COVID-19; 23% (41 respondents) thought that there was a medium to high chance someone in their household would be infected; 45% (80 respondents) thought that if they got COVID-19, there was a medium to high chance that they would have to go to the hospital; 54% (96 respondents) thought that if they acquired COVID-19, then there was a medium to high chance they would infect someone else, and 20% (36 respondents) thought there was a medium to high chance that someone in their household would die from COVID-19. There were no statistically significant differences in perception of future risk by cohort.
Fig 2.
Perception of future risk and/or complication from a COVID-19 infection among survey participants between December 29, 2020 and April 2, 2021 within a Federally Qualified Health Center in San Ysidro (n = 179).
COVID-19 testing experiences
Approximately 68% (121 respondents) indicated that they had previously been tested for COVID-19. Among tested individuals, 29 respondents (24%) indicated that they had previously tested positive for COVID-19. Among the group reported having been tested, 117 (97%) reported having very easy or easy access to testing for COVID-19 and 118 (98%) reported the testing experience as easy or very easy. About 43% (n = 52) of those tested had been tested once, 33% had been tested 2 times, and 24% had been tested 3 or more times. About 15 individuals (12.5%) reported having been tested at the FQHC. A majority (83%) of tested individuals reported receiving their results within 3 days.
Five individuals indicated that they had tried to be tested for COVID-19 and had been unable to get a test. They listed the following three reasons for not obtaining a test: “I haven’t felt sick,” “I wasn’t able to get an appointment for when I needed it,” and “I was worried about not being able to pay.” When asked why they might not get tested for COVID-19, 65 participants (36%) indicated that they were worried about being infected with COVID-19 upon visiting a testing facility.
Discussion
Findings from a community and clinic assessment survey of 179 adults living near the U.S./Mexico border were reported for sociodemographic characteristics, perceived COVID-19 risk, infection, and testing access. Although results for three cohorts (pre/post-natal patients; caregivers for pre/post-natal patients; and caregivers for pediatric patients) living in or near the San Ysidro region were evaluated separately, findings were generally consistent across the cohorts. Overall, the sample was predominantly female, Latino, young (less than 35 years of age), living in households with multiple adults and children, unemployed, and with educational attainment at or less than some college. This is largely consistent with the demographic trends in the San Ysidro region [34, 35] with the exceptions of the employment status. These differences are likely due to the clinic-based recruitment of the original sample and the recruitment methods favoring those who are more likely to have an interest in and availability to participate in a research survey.
In our sample, 65% of participants indicated that they had adequate knowledge on COVID-19 prevention measures, which is consistent with the global literature. For example, Nwafor et al. (2020) reported that 60% of pregnant women were knowledgeable of preventative measures [36] and Naqvi et al. (2022) reported 56.8% of pregnant women reported knew three or more preventative measures [37]. It is possible that our population indicated slightly higher rates of knowledge given the FQHCs COVID-19 prevention messaging posted throughout the clinics along with the widely disseminated COVID-19 prevention campaigns in the U.S. Less than 55% of participants reported that there was a medium to high likelihood that they would acquire COVID-19, infect others, or suffer serious side effects from infection, including hospitalization or death. This is in line with earlier studies that identified low COVID-19 threat perception among Black and Hispanic populations living in the U.S. [14, 15]. One possible explanation that may have influenced the results is the timing of the survey and surrounding public health events, as this survey was administered during the first anniversary of the start of the pandemic, and shortly after vaccines started to become available.
We were particularly interested in the COVID-19 testing experiences of this border community to inform our efforts to co-create a culturally responsive testing program. Among the 179 total survey respondents, most reported that they had been tested for COVID-19, with 29 (16%) receiving a positive test result. Only a subset of participants reported being tested at the local FQHC, though it is unclear which other testing sites this sample accessed for their testing needs. With regard to the testing experience, among those who had accessed a test, almost all participants described their testing experience as easy and most received their results in three days. The reported ease and relatively fast turnaround of results are contradictory to the recent literature and media reports in which the U.S. has seen large testing inequities among communities of color, including a significant lack of access to testing and challenges with the return of results [38–40]. It is possible, however, that this population may have had referrals for testing through their prenatal and/or pediatric medical visits that could potentially explain this ease in access to testing.
Although few participants reported access challenges such as the inability to obtain a testing appointment, our survey findings did offer valuable insights regarding testing perceptions. Our sample expressed economic concerns regarding the perceived need to pay for testing [10] as well as refusing testing because they were asymptomatic. These findings are like Cervantez et al. (2021), who identified “misinformation and disbelief” as well as “worry about health care costs” as subthemes in their analysis of the experiences of Latino adults who had been discharged from hospitalization due to COVID-19. The most frequently reported reason for not getting tested was concern about COVID-19 exposure.
This study had both strengths and limitations. A primary strength was that this was a unique and typically under-included sample (i.e., individuals, many of whom were pregnant, living near the U.S./Mexico border) in health services research. Another strength is the focus of important and not well-studied perceptions of COVID-19 testing and risk. Limitations included the cross-sectional, self-report nature of the survey that may lead to social desirability and other reporting biases, as well as the moderate sample size which limited statistical power to conduct sub-group analyses. It was beyond the scope of our study to collect data on and report the accuracy of COVID-19 prevention knowledge nor the practice of those preventative behaviors. We also did not have concurrent testing data to validate the infection rate and were not able to report on vaccination status. In addition, the timing of our survey may have skewed the results. The FDA issued Emergency Use Authorizations for the use of COVID-19 vaccines on persons ages 18 and older between December 2020 and February 2021 and announced the availability of vaccines to all person’s ages 16 and older April 19, 2021 [41]. Our surveys were administered amid this development with global perspectives of COVID-19 risk likely decreasing as the general public (e.g., those not in health care, school or childcare settings) was soon eligible for vaccination.
This limitation is potentially borne out in the high rates of endorsement that participants know what preventive behaviors to take to mitigate COVID-19 infection and the low levels of COVID-19 threat perceptions. Related research with Latino participants has not only reported similar trends in COVID-19 risk perception but also limited engagement in COVID-19 preventive behaviors [14].
Results from this study have important implications at multiple levels. At the local level, these data were triangulated with a Theory of Change [29] process completed by a Community and Scientific Advisory Board that consisted of FQHC providers, administrators, public health researchers, and promoters to identify targeted implementation strategies to inform the co-creation of the COVID-19 testing program [29]. The triangulated results directly informed the iterative design of the RADx Underserved Populations (RADx-UP) testing program, CO-CREATE, which continues to offer no-cost, walk-up testing at the FQHC. At the policy level, these results can help guide the design and implementation of culturally tailored testing strategies that can be translated beyond this border community. Our study was an important first step in understanding the COVID-19 experiences and risk perceptions of patients and community members living near the U.S./Mexico border in San Ysidro, California. These initial findings ignited a series of additional research questions that informed the development of our survey for the testing phase of the study where we assess COVID-19 preventative behaviors, vaccine hesitancy, vaccine status, as well as community and cultural barriers to testing and vaccination.
CONCLUSION
Since the start of the COVID-19 pandemic in early 2020, there have been over 1 million COVID-19 related deaths and these deaths have disproportionately affected BIPOC communities [1, 2]. COVID-19 testing strategies that fail to incorporate culturally competent methods to reach traditionally underserved communities will lead to persistent transmission and increased infection rates, and further compound well-established health care and outcome disparities. Our study aimed to characterize the knowledge, attitudes, and beliefs of prenatal patients, and prenatal and pediatric caregivers regarding perceived risk of COVID-19 infection and access to testing. These results were triangulated with a Theory of Change process completed by a Community and Scientific Advisory Board and informed the design and co-creation of a culturally tailored COVID-19 testing program in the U.S./Mexico Border region. Future research should aim to identify community and culture specific barriers to COVID-19 testing and the development of effective and sustainable strategies for increasing equitable access to testing in border regions of the U.S.
ACKNOWLEDGEMENTS
The authors would like to extend their gratitude for the time and wisdom shared by the CO-CREATE Community Advisory Board members.
Contributor Information
Linda Salgin, San Ysidro Health, San Diego, CA, USA; San Diego State University/University of California San Diego Joint Doctoral Program in Public Health, San Diego, CA, USA.
Lawrence O Ayers, University of California, San Diego Department of Obstetrics, Gynecology, and Reproductive Sciences, San Diego, CA, USA.
Maria-Linda Burola, University of California, San Diego Department of Obstetrics, Gynecology, and Reproductive Sciences, San Diego, CA, USA.
Anne-Marie Engler, University of California, San Diego Department of Obstetrics, Gynecology, and Reproductive Sciences, San Diego, CA, USA.
Alexis Osuna, San Ysidro Health, San Diego, CA, USA.
Luis Gay, San Ysidro Health, San Diego, CA, USA.
Kelli Cain, University of California, San Diego, Herbert Wertheim School of Public Health and Human Longevity Science, San Diego, CA, USA.
Nicole Stadnick, University of California San Diego, Department of Psychiatry, San Diego, CA, USA; University of California, San Diego Altman Clinical and Translational Research Institute Dissemination and Implementation Science Center, San Diego, CA, USA; Child and Adolescent Services Research Center, San Diego, CA, USA.
Borsika Rabin, University of California, San Diego, Herbert Wertheim School of Public Health and Human Longevity Science, San Diego, CA, USA; University of California, San Diego Altman Clinical and Translational Research Institute Dissemination and Implementation Science Center, San Diego, CA, USA.
Ilya Zaslavsky, University of California San Diego, Spatial Information Systems Lab, San Diego Supercomputer Center, San Diego, CA, USA.
Louise C Laurent, University of California, San Diego Department of Obstetrics, Gynecology, and Reproductive Sciences, San Diego, CA, USA.
Robert Tukey, University of California San Diego, Department of Chemistry and Biochemistry, San Diego, CA, USA.
Marva Seifert, University of California San Diego, Division of Pulmonary and Critical Care Medicine, San Diego, CA, USA.
FUNDING
This work was funded by the National Institutes of Health: P42 ES010337-19S2 RADx-UP Supplement (Laurent, Tukey); K23 MH110602 (Stadnick); R34 MH120190 (Stadnick), and the UC San Diego ACTRI Dissemination and Implementation Science Center (Rabin, Stadnick).
COMPLIANCE WITH ETHICAL STANDARDS
Conflict of interest: This research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Human rights: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Welfare of animals: This article does not contain any studies with animals performed by any of the authors.
TRANSPARENCY STATEMENTS
Study Registration: This study has not been formally registered.
Analytic Plan Registration: This analysis plan was not formally pre-registered.
Availability of Data: De-identified data from this study are not available in a public archive. De-identified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author.
Availability of Analytic Code: Analytic code used to conduct the analyses presented in this study is not available in a public archive. They may be available by emailing the corresponding author.
Availability of Materials: Materials used to conduct the study are not publicly available.
Perceived COVID-19 Risk and Testing Experiences in the San Ysidro US/Mexico Border Region
References
- 1. Centers for Disease Control and Prevention. (2021). COVID data tracker. https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendscases
- 2. Thakur N, Lovinsky-Desir S, Bime C, Wisnivesky JP, Celedón JC.. The structural and social determinants of the racial/ethnic disparities in the U.S. COVID-19 pandemic what’s our role? Am J Respir Crit Care Med. 2020;202(7):943–949. doi: 10.1164/rccm.202005-1523PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Price-Haywood EG, Burton J, Fort D, Seoane L.. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382(26):2534–2543. doi: 10.1056/NEJMsa2011686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rodriguez F, Solomon N, de Lemos JA, et al. Racial and ethnic differences in presentation and outcomes for patients hospitalized with COVID-19: findings from the American heart association’s COVID-19 cardiovascular disease registry. Circulation. 2021;143(24):2332–2342. doi: 10.1161/CIRCULATIONAHA.120.052278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Webb Hooper M, Nápoles AM, Pérez-Stable EJ.. COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466–2467. 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kaiser Family Foundation. (2018). Poverty rate by race/ethnicity. https://www.kff.org/other/state-indicator/poverty-rate-by-raceethnicity/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
- 7. Moore JT, Pilkington W, Kumar D. Diseases with health disparities as drivers of COVID-19 outcome. J Cell Mol Med. 2020;24(19):11038–11045. doi: 10.1111/jcmm.15599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Calo WA, Murray A, Francis E, Bermudez M, Kraschnewski J.. Reaching the hispanic community about COVID-19 through existing chronic disease prevention programs. Prev Chronic Dis. 2020;17:200165. doi: 10.5888/pcd17.200165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cervantes L, Martin M, Frank MG, et al. . Experiences of latinx individuals hospitalized for COVID-19: a qualitative study. JAMA Network Open. 2021;4(3):e210684–e210684. doi: 10.1001/jamanetworkopen.2021.0684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Laurencin CT. Addressing justified vaccine hesitancy in the black community. J Racial Ethn Health Disparities. 2021;8(3):543–546. doi: 10.1007/s40615-021-01025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rentsch CT, Kidwai-Khan F, Tate JP, et al. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: a nationwide cohort study. PLoS Med. 2020;17(9):e1003379. doi: 10.1371/journal.pmed.1003379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sönmez S, Apostolopoulos Y, Lemke MK, Hsieh Y-CJ.. Understanding the effects of COVID-19 on the health and safety of immigrant hospitality workers in the United States Tourism Manage Persp. 2020;35:100717. doi: 10.1016/j.tmp.2020.100717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Karout L, Serwat A, El Mais H, Kassab M, Khalid F, Ruiz Mercedes B.. COVID-19 prevalence, risk perceptions, and preventive behavior in asymptomatic Latino population: a cross-sectional study. Cureus. 2020;12(9):e10707–e10707. doi: 10.7759/cureus.10707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Khunti K, Platt L, Routen A, Abbasi K. (2020). Covid-19 and ethnic minorities: an urgent agenda for overdue action. The government’s report falls seriously short on commitment. Available at doi:10.1136/bmj.m2503
- 15. Pareek M, Bangash MN, Pareek N, et al. . Ethnicity and COVID-19: an urgent public health research priority. Lancet (London, England). 2020;395(10234):1421–1422. doi: 10.1016/S0140-6736(20)30922-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Meneses Gutiérrez MM. Mexico-US local transborder micro-business methods resisting border travel restrictions in 2020. Latino Studies. 2021;19:400–404. doi: 10.1057/s41276-021-00330-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. United States General Service Administration. (2021). San Ysidro land port of entry. https://www.gsa.gov/about-us/regions/welcome-to-the-pacific-rim-region-9/land-ports-of-entry/san-ysidro-land-port-of-entry
- 18. SANDAG. (2020). Data surfer. https://datasurfer.sandag.org/dataoverview
- 19. San Diego Health and Human Services Agence. (2020). County of San Diego Coronavirus Disease 2019 (COVID-19) Summary of Cases by Zip Code of Residence. https://www.sandiegocounty.gov/content/dam/sdc/hhsa/programs/phs/Epidemiology/COVID-19%20Summary%20of%20Cases%20by%20Zip%20Code.pdf
- 20. Mor G, Cardenas I, Abrahams V, Guller S.. Inflammation and pregnancy: the role of the immune system at the implantation site. Ann N Y Acad Sci. 2011;1221(1):80–87. doi: 10.1111/j.1749-6632.2010.05938.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vora KS, Sundararajan A, Saiyed S, Dhama K, Natesan S.. Impact of COVID-19 on women and children and the need for a gendered approach in vaccine development. Human Vaccine Immunother. 2020;16(12):2932–2937. doi: 10.1080/21645515.2020.1826249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Durankuş F, Aksu E.. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J Maternal-Fetal Neonatal Med. 2022; 35(2):205–211. doi: 10.1080/14767058.2020.1763946. [DOI] [PubMed] [Google Scholar]
- 23. Metz TD, Clifton RG, Hughes BL.. Association of SARS-CoV-2 infection with serious maternal morbidity and mortality from obstetric complications. JAMA. 2022; 327(8):748–759. doi: 10.1001/jama.2022.1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhang Y, Ma ZF.. Psychological responses and lifestyle changes among pregnant women with respect to the early stages of COVID-19 pandemic. Int J Soc Psychiatry. 2021; 67(4):344–350. doi: 10.1177/0020764020952116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Craig AM, Hughes BL, Swamy GK. Coronavirus disease 2019 vaccines in pregnancy. American Journal of Obstetrics & Gynecology MFM. 2021;3(2):100295. doi: 10.1016/j.ajogmf.2020.100295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Skjefte M, Ngirbabul M, Akeju O, et al. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol. 021;36(2):197–211. doi: 10.1007/s10654-021-00728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wastnedge EAN, Reynolds RM, van Boeckel SR.. Pregnancy and COVID-19. Physiol Rev. 2021;101(1):303–318. doi: 10.1152/physrev.00024.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Corbett GA, Milne SJ, Hehir MP, Lindow SW, O’connell MP.. Health anxiety and behavioural changes of pregnant women during the COVID-19 pandemic. Eur J Obstet Gynecol Reprod Biol. 2020;249:96–97. doi: 10.1016/j.ejogrb.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stadnick NA, Ma KLC, Oswald W, et al. Cocreating a theory of change to advance COVID-19 testing and vaccine uptake i n underserved communities. Health Services Res. 2021;57:1–9. doi: 10.1111/1475-6773.13910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Community Engagement Alliance (CEAL) Against COVID-19 disparities | community engagement alliance. (n.d.). https://covid19community.nih.gov/. Accessibility verified May 1, 2022.
- 31. Zaslavsky I, Burton M, Levy T. (2017). A new approach to online visual analysis and sharing of archaeological surveys and image collections (pp. 133–150). doi: 10.1007/978-3-319-65370-9_7 [DOI]
- 32. REDCap. 2004. https://www.project-redcap.org/. Accessibility verified March 7, 2022.
- 33. SuAVE: Survey Analysis via Visual Exploration. (2015). Accessibility verified February 27, 2022. https://suave.sdsc.edu/
- 34. City-Data. (n.d.). San Ysidro neighborhood in San Ysidro, California (CA), 92173. http://www.city-data.com/neighborhood/San-Ysidro-San-Ysidro-CA.html. Accessibility verified January 10, 2022.
- 35. Point 2 Homes. (n.d.). San Ysidro,CA Household Income, Population & Demographics. . Retrieved January 10, 2022
- 36. Nwafor JI, Aniukwu JK, Anozie BO, Ikeotuonye AC, Okedo-Alex IN.. Pregnant women’s knowledge and practice of preventive measures against COVID-19 in a low-resource African setting. Int J Gynec Obstetr. 2020;150(1):121–123. doi: 10.1002/ijgo.13186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Naqvi F, Naqvi S, Billah SM, et al. Knowledge, attitude and practices of pregnant women related to COVID-19 infection: a cross-sectional survey in seven countries from the Global Network for Women’s and Children’s Health. BJOG:Int J Obst Gynaec. 2022;129(8):1289–1297. doi: 10.1111/1471-0528.17122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Garcini LM, Pham TT, Ambriz AM, Lill S, Tsevat J.. COVID-19 diagnostic testing among underserved Latino communities: Barriers and facilitators. Health Soc Care Community. 2022;30(5):e1907–e1916. doi: 10.1111/hsc.13621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Gray DM, Anyane-Yeboa A, Balzora S, Issaka RB, May FP.. COVID-19 and the other pandemic: populations made vulnerable by systemic inequity. Nature Reviews Gastroenterology & Hepatology. 2020;17(9):520–522. doi: 10.1038/s41575-020-0330-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. National Institutes of Health. (n.d.). NIH to assess and expand COVID-19 testing for underserved communities. https://www.nih.gov/news-events/news-releases/nih-assess-expand-covid-19-testing-underserved-communities. Accessibility verified January 10, 2022.
- 41. U.S. Food and Drug Administration. COVID-19 Vaccines Approved or Authorized for Emergency Use. https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines. Accessed November 3, 2022.