Abstract
Objectives:
Cases of severe lower limb injuries that previously were amenable only to amputation can now, in certain circumstances, be managed with reconstruction. The present systematic review and meta-analysis was designed to compare the results of amputation and reconstruction in severe lower extremity injuries.
Methods:
PubMed, EMBASE and Cochrane Central Register of Controlled Trails (CENTRAL) were comprehensively searched for studies comparing amputation and reconstruction for severe lower extremity injuries. The search terms used were the following: “amputation”, “reconstruction”, “salvage”, “lower limb”, “lower extremity”, and “mangled limb”, “mangled extremity”, “mangled foot”. Two investigators screened eligible studies, assessed the risk of bias and extracted the data from each study. Meta-analysis was conducted using the Review Manager Software (RevMan, Version 5.4). The I2 index was used to assess heterogeneity.
Results:
Fifteen studies with 2,732 patients were included. Amputation is associated with lower rehospitalization rates, lower length of stay in the hospital, lower number of operations and additional surgery and fewer cases of infection and osteomyelitis. Limb reconstruction leads to faster return to work and lower rates of depression. The outcomes with respect to function and pain are variable among the studies. Statistically significance was achieved only with regards to rehospitalization and infection rates.
Conclusion:
This meta-analysis suggests that amputation yields better outcomes in variables during the early postoperative period, while reconstruction is associated with improved outcomes in certain long-term parameters. Severe lower limb injuries should be managed on their individual merit. The results of this study may be a useful tool to aid in the decision-making for the treating surgeon. High-quality Randomized Controlled Studies are still required to further our conclusions.
Key Words: Amputation, Lower limb injury, Mangled, Meta-analysis, Reconstruction, Salvage
Introduction
Severe injuries to the lower limb can result in significant morbidity and mortality. The mangled extremity has been historically associated with high amputation rates. More Recent advances in both orthopedic and plastic surgery have led to limb salvage procedures to be potentially undertaken in cases that in the past were considered amenable only to amputation. However, although reconstruction may be technically feasible, it may not be always in the best interest of the patient. The decision between undertaking an amputation and a reconstruction remains challenging with multiple clinical and additional quality of life factors that are unique to every patient, having to be taken into consideration. A number of studies have previously been published reporting the results of amputation and reconstruction after severe lower extremity injury but the results have been conflicting.
The purpose of the present systematic review and meta-analysis is to compare the results of amputation versus reconstruction in severe lower limb injuries in terms of recovery, functional outcome, pain, mental health and complications. These results may provide an additional tool to help in the guidance on the management of these injuries.
Materials and Methods
Search strategy
This systematic review and meta-analysis was conducted in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines.1 We undertook a comprehensive search in PubMed, EMBASE and Cochrane Central Register of Controlled Trails (CENTRAL) from their inception up to July 2022 for Randomized Controlled Trials (RCTs) and two-armed prospective or retrospective studies comparing amputation and reconstruction for severe lower extremity injuries. The search terms used were the following: “amputation”, “reconstruction”, “salvage”, “lower limb”, “lower extremity”, and “mangled limb”, “mangled extremity”, “mangled foot” and “crush injury” with “AND” and “OR” as Boolean terms. Reference lists of the related articles were hand-searched for any additional eligible studies in a further effort not to miss out on any relevant publications. Two independent investigators screened eligible studies. When consensus could not be reached, a third reviewer was consulted to resolve the disagreement.
Eligibility criteria
Articles were included in the meta-analysis based on the following criteria: (1) RCTs and two-armed prospective or retrospective studies comparing amputation and reconstruction for severe lower extremity injuries, (2) studies were designed to compare early amputation vs non-amputation. Exclusion criteria were as follows: (1) other article types (case reports, letters, comments, editorials, reviews, conference abstracts), (2) articles not in English, (3) studies comparing the results of salvage to delayed amputation following limb salvage injury, (4) studies comparing the results of salvage and amputation for lower limb deformity, (5) studies analyzing a subgroup of patients of a study already included in the meta-analysis.
Extraction of the relevant data
Two investigators extracted the data from the eligible studies. To ensure consistency in the extraction of the data from each study, a structured form was used. Information retrieved from each study included author names, year of publication, study design, sample size, patient characteristics (age, gender, civilian/military), injury type, and outcomes.
Quality assessment
Two investigators evaluated the risk of bias of each of the included studies using the ROBINS-I tool for observational studies.2 each of these factors was recorded as low, moderate, serious or critical risk of bias.
Statistical analysis
The meta-analysis was conducted using the Review Manager Software (RevMan, Version 5.4). The results were expressed as odds ratios (ORs) and 95% confidence intervals (CIs). A P-value of less than 0.05 was considered statistically significant. The I2 index was used to assess heterogeneity. A value of I2 of less than 25% was interpreted as homogeneity, and values of 25% to 75% and 75% and more were interpreted as moderate and high heterogeneity respectively. The fixed-effect model was used for homogenous studies and the random-effect model was used when there was heterogeneity. Sensitivity analyses were performed to assess the changes in the overall results by omitting studies.
Results
Search results and study characteristics
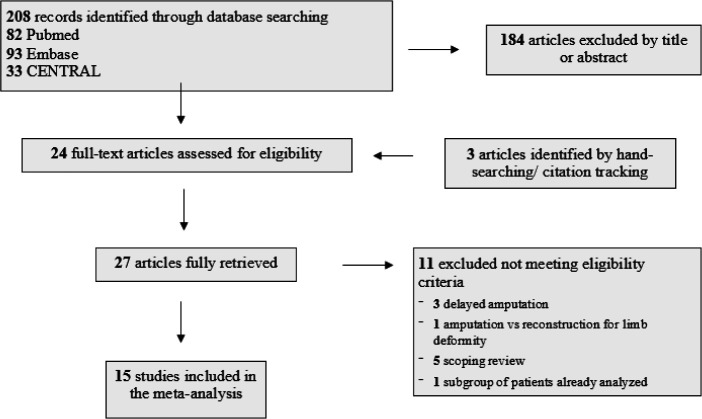
A total of 208 studies were identified from PubMed (n=82), EMBASE (n=93) and CENTRAL (n=33) using the above methodology. After exclusion of the articles that did not meet the eligibility criteria by title or abstract, 24 studies were retrieved for full-article assessment. Three additional studies were identified by citation tracking and hand searching. Nine of the fully-retrieved studies (n=24) were excluded because they did not meet the eligibility criteria. This led to a total of 15 studies from 1993 to 2018 being included in the meta-analysis.3-17 the total number of patients in the included studies was 2,732 (1,326 amputations and 1,406 reconstructions). The literature search and the selection process are summarized in a flow chart in [Figure 1]. The characteristics of the included studies are presented in [Table 1].
Figure 1.
Flow chart summarizing the selection process
Table 1.
Characteristics of the included studies
| Author, year | Study design | Injury type* | Sample size | Gender, males (%) | Mean age (years) |
Patient
Characteristics |
Follow-up (months) (mean/median) | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | R | A | R | A | R | A | R | |||||
| Georgiadis, 1993 | Retrospective | IIIB,C tibial fractures | 18 | 27 | NA | NA | 32 | 33 | Civilian | 44 | 35 | Pain Walking ability Function Employment Gait Range of motion Nottingham Health Profile General Well-Being Schedule Costs |
| Dahl, 1995 | Retrospective | IIIB fractures | 30 | 67 | 80 | 71.7 | 31 | 28 | Civilian | 91 | 108 | Function (Questionnaire) |
| Hertel, 1996 | Retrospective | IIIB,C tibial fractures | 18 | 21 | NA | NA | 22 | 23 | Civilian | 83 | 86 | Function (interview) Hospitalization Costs Employee compensation allowances |
| Dagum, 1999 | Retrospective | IIIB,C lower limb fractures | 9 | 46 | 33.3 | 71.7 | 33 | 37 | Civilian | 60 | Short-Form 36 (SF-36) Western Ontario and McMaster Universities Arthritis Index (WOMAC) |
|
| Hoogendoorn, 2001 | Retrospective | III tibial fractures | 21 | 43 | 76.2 | 76.7 | 44.6 | 39.9 | Civilian | 60 | Guides to the evaluation of permanent impairment Nottingham health profile (NHP) Short-form 36 (SF-36) |
|
| Bosse, 2002 | Prospective | IIIB,C fractures below distal femur Selected IIIA Dyvascular limbs Major soft tissue injuries, IIIB ankle fractures III pilon fractures severe hindfoot/midfoot injuries |
161 | 384 | 63.4 | 75 | 35.2 | 35.8 | Civilian | 24 | Sickness Impact Profile (SIP), Limb Status Complications leading to Rehospitalization Return to work |
|
| Higgins, 2010 | Prospective | IIIB,C fractures Selected IIIA Dyvascular limbs Major soft tissue injuries IIIB ankle fractures III pilon fractures Severe hindfoot/midfoot injuries |
149 | 371 | NA | NA | NA | NA | Civilian | 24 | Sickness impact profile (SIP) Return to work Infection, osteomyelitis |
|
| Doukas, 2013 | Retrospective | IIIB,C fractures Selected IIIA Dyvascular limbs Major soft tissue injuries Severe foot injuries |
126 | 113 | 96.8 | 98.2 | NA | NA | Military | 38.6 | Short Musculoskeletal Function Assessment (SMFA) Paffenbarger Physical Activity Questionnaire Participation in a major role activity Revised Center for Epidemiologic Studies Depression Scale (CESD-R) Military version of the PTSD Checklist Chronic Pain Grade (CPG) scale |
|
| Ellington, 2013 | Prospective | Major soft tissue injuries Severe foot injuries |
58 | 116 | NA | NA | NA | NA | Civilian | 24 | Sickness Impact profile (SIP) Walking speed Time to full weight-bearing Number of rehospitalizations Visual analogue pain scale (VAS) Return to work |
|
| Melcer, 2013 | Retrospective | IIIB,C fractures Selected IIIA Vascular injuries Major soft tissue injuries Severe foot injuries |
587 | 117 | NA | NA | NA | NA | Military | Minimum 24 | Physical complications Psychological diagnoses Health care use |
|
| Demiralp, 2014 | Retrospective | Complex hind foot injuries (land-mine explosions) | 21 | 21 | NA | NA | 38.4 | 38.2 | Civilian | 15.7 | 14.57 | Short-Form 36 (SF-36) Foot and Ankle Disability Index (FADI) Body Image Quality of Life Inventory (BIQLI) Physical complications Psychiatric treatments |
| Edelstein, 2016 | Prospective | Crush injuries to the foot (some extending to the ankle) III fractures |
5 | 16 | 20 | NA | NA | Civilian | Up to 36 | Sickness Impact Profile (SIP) Visual Analogue Scale (VAS) Number of rehospitalizations for secondary surgical procedures |
||
| Ladlow, 2016 | Retrospective | Fractures Nerve damage Extensive soft tissue trauma/ Vascular trauma from blast fragments |
79 | 21 | 98.7 | 95.3 | 38.4 | 38.2 | Military | 30/35** | 22 | 6-minute walk test (6MWT Defense Medical Rehabilitation Centre mobility and activities of daily living scores Depression (Patient Health Questionnaire [PHQ-9]) and general anxiety disorder (General Anxiety Disorder 7-item scale [GAD-7]) Mental health support Pain scores |
| Barla, 2017 | Retrospective | III femoral, tibial and pilon fractures Closed fractures leading to amputation |
20 | 16 | 75 | 68.6 | 47.6 | 37.4 | Civilian | Minimum 12 | Mangled Extremity Severity Score (MESS) Complications Bony union Function |
|
| Fioravanti, 2018 | Retrospective | IIIB,C tibial fractures | 24 | 27 | 95.8 | 92.6 | 43.74 | 42.37 | Civilian | Minimum 24 | Short-Form 36 (SF-36) Primary hospital stay Number of procedures Number of infections Function |
|
A: Amputation, R: Reconstruction
*Gustilo-Anderson Classification for open fractures
** Unilateral/bilateral amputations
NA: Not available
Risk of bias in the included studies
Six of the included studies were found to have a low overall risk for bias based on the ROBINS-I tool. The remaining nine were found to have a moderate risk of bias. In all the included studies the risk of bias in classification of interventions, bias due to deviations from the intended interventions, bias due to missing data, bias in the measurements of outcomes and bias in selection of the reported results was found to be low [Table 2].
| Author, year | Bias due to confounding | Bias in selection of participants into study | Bias in classification of interventions | Bias due to deviations from intended interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of reported result | Overall | |
|---|---|---|---|---|---|---|---|---|---|
| Georgiadis, 1993 | Low risk | Low risk | Low risk | Moderate risk | Low risk | Low risk | Low risk | Moderate risk | |
| Dahl, 1995 | Low risk | Moderate risk | Low risk | Low risk | Low risk | Low risk | Low risk | Moderate risk | |
| Hertel, 1996 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | |
| Dagum, 1999 | Low risk | Moderate risk | Low risk | Low risk | Low risk | Low risk | Low risk | Moderate risk | |
| Hoogendoorn, 2001 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | |
| Bosse, 2002 | Moderate risk | Low risk | Low risk | Low risk | Low risk | Low Risk | Low risk | Moderate risk | |
| Higgins, 2010 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | |
| Doukas, 2013 | Moderate risk | Moderate risk | Low risk | Low risk | Low risk | Low risk | Low risk | Moderate risk | |
| Ellington, 2013 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | |
| Melcer, 2013 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | |
| Demiralp, 2014 | Low risk | Moderate risk | Low risk | Low risk | Low risk | Low risk | Low risk | Moderate risk | |
| Edelstein, 2016 | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | |
| Ladlow, 2016 | Low risk | Moderate risk | Low risk | Low risk | Low risk | Low risk | Low risk | Moderate risk | |
| Barla, 2017 | Low risk | Moderate risk | Low risk | Low risk | Low risk | Low risk | Low risk | Moderate risk | |
| Fioravanti, 2018 | Low risk | Moderate risk | Low risk | Low risk | Low risk | Low risk | Low risk | Moderate risk | |
Results of the meta-analysis
Rehospitalization
The rehospitalization rate was reported in six of the studies,3,8,9,11,12,14 and four of them were included in the quantitative synthesis.3,8,9,11 The meta-analysis revealed statistically significant lower rehospitalizations in the amputees relative to the patients having undergone a reconstruction (odds ratio [OR] 0.56, 95% confidence interval [CI] 0.42-10.75, P<0.0001, and there was no heterogeneity among the included studies (I2=0%) [Figure 2]. In the remaining two studies, Edelstein et al., 14 in line with the results of the meta-analysis, reported a statistically higher number of rehospitalizations in the reconstructed patients, while Melcer et al.12 reported higher rates of use of orthopedic wards and pain clinics in the amputees, but the differences between the groups were not significant.
Figure 2.
Forest plot of rehospitalization rate in amputation versus reconstruction in severe lower limb injury
Number of operations
The number of operations during the initial admission was reported in five of the included studies.3, 5, 7, 13, 16 a meta-analysis could not be conducted due to missing mean or standard deviation values. However, in all of the included studies a lower number of operations was reported in the patients having undergone an amputation relative to the patients having undergone a reconstructive procedure. In two of the studies, 5, 13 the differences were reported to be statistically significant.
Length of stay
The length of stay was reported in five of the included studies.3, 5-7, 17 A meta-analysis could not be conducted due to missing standard deviation values. In all of the included studies the length of stay was longer in patients in the reconstruction group, however, only Fioravanti et al.17 reported statistically significant differences between the groups.
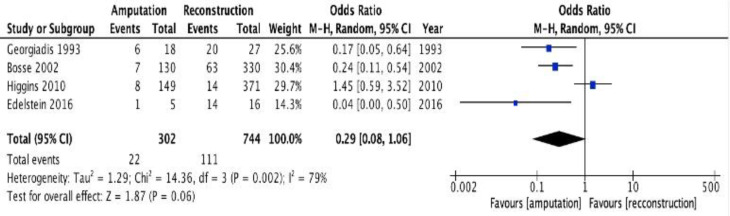
Additional surgery
The number of patients that needed subsequent surgical intervention was reported in four of the included studies.3, 8,9,14 The meta-analysis showed that amputees required less additional surgery compared to the patients in the reconstruction group, but the differences were not statistically significant (odds ratio [OR] 0.29, 95% confidence interval [CI] 0.08-1.06, P=0.06, [Figure 3]) and the heterogeneity was high among the included studies (I2=79%).
Figure 3.
Forest plot of additional surgery in amputation versus reconstruction in severe lower limb injury
Return to work
The number of patients that returned to work after severe lower limb injury was reported in nine of the included studies.3, 4, 6, 8-11, 16, 17 The results of the meta-analysis showed that a higher number of patients returned to work after a reconstructive procedure relative to an amputation, but the differences were not statistically significant (odds ratio [OR] 1.10, 95% confidence interval [CI] 0.89-1.35, P=0.4, [Figure 4]). There was no heterogeneity among the included studies (I2=17%).
Figure 4.
Forest plot of return to work in amputation versus reconstruction in severe lower limb injury
Functional outcome
The functional outcome was reported with different methodological tools in the included studies and therefore a meta-analysis was not performed. Fourteen of the included studies reported functional outcomes. Three of those4, 8, 9 reported similar outcomes in terms of function between patients with an amputation and patients with a reconstruction. Seven of the included studies3, 10, 11, 14-17 showed better functional outcomes in patients having undergone an amputation and four of the included studies5-7, 14 showed better functional outcomes in patients having undergone a reconstruction. Interestingly, all the studies that compared results in the military population showed better functional outcomes with an amputation. The functional outcomes in the included studies are summarized in [Table 3].
Table 3.
Functional outcomes
| Author, year | Functional outcome | Favours |
|---|---|---|
| Georgiadis, 1993 | Significantly longer time to full-weight bear in the reconstruction group More patients in the reconstruction group considered themselves disabled and had problems with performance in recreational and occupational activities |
Amputation |
| Dahl, 1995 | No differences between the groups apart from the complaints for leg swelling which were more in the reconstruction group | Similar results |
| Hertel, 1996 | Compared walking and standing ability, quadriceps muscle wasting, and range of motion between the two groups and found a statistically significant better walking ability in the reconstruction group | Reconstruction |
| Dagum, 1999 | Better results in the reconstruction group in SF-36 and WOMAC scores, but the differences were not statistically significant | Reconstruction |
| Hoogendoorn, 2001 | Lower mean lower extremity impairment in patients having undergone a reconstruction No differences in NHP and SF-36 scores |
Reconstruction |
| Bosse, 2002 | No differences in SIP scores | Similar results |
| Higgins, 2010 | No differences in SIP scores | Similar results |
| Doukas, 2013 | Better results in the amputation group based on the SMFA scores | Amputation |
| Ellington, 2013 | Better results in the amputation group based on the SIP scores Significantly longer time to weight-bear in the reconstruction group |
Amputation |
| Demiralp, 2014 | Significantly better results in the reconstruction group based on the BIQLI scores Better results in the reconstruction group based on the SF-36 scores (not significant) |
Reconstruction |
| Edelstein, 2016 | Better results in the amputation group based on the SIP scores | Amputation |
| Ladlow, 2016 | Patients with a unilateral amputation could walk significantly farther than patients with a reconstruction Patients with a reconstruction could walk significantly farther than patients with bilateral amputation | Amputation |
| Barla, 2017 | Patients with an amputation had a significantly superior walking distance and fewer walking aids | Amputation |
| Fioravanti, 2018 | Walking distance, use of crutches, prolonged standing, climbing easily up and down stairs, running, jumping and return to adapted sports activity significantly better in the amputation group | Amputation |
SF-36: Short-Form 36 (SF-36)
WOMAC: Western Ontario and McMaster Universities Arthritis Index
NHP: Nottingham health profile
SIP: Sickness Impact Profile
SMFA: Short Musculoskeletal Function Assessment
Pain
The severity of pain was reported in five of the included studies.3, 10,11,14,15 A meta-analysis was not performed due to differences among the studies in the methodological tools when reporting this outcome. In the study by Georgiadis et al.3 patients with an amputation and patients with a reconstruction had the same pain scores. Similarly, Ellington et al. and Edelstein et al.11, 14 used the Visual Analogue Scale (VAS) and showed no differences between the groups in terms of pain. On the other hand, Doukas et al.10 reported a lower percentage of patients with pain interfering with their daily activities in the amputation group and Ladlow et al.15 reported that a greater proportion of patients with limb reconstruction reported uncontrolled pain.
Mental health
Four of the included studies reported the number of patients with depression after severe lower limb injury and an amputation or reconstructive procedure.10, 12, 13, 15 the results of the meta-analysis revealed that more patients suffered from depression following an amputation, but the differences were not significant. (Odds ratio [OR] 1.22, 95% confidence interval [CI] 0.65-2.29, P<0.54, [Figure 5]). Moderate heterogeneity was found between the studies (I2=61%).
Figure 5.
Forest plot of depression rate in amputation versus reconstruction in severe lower limb injury
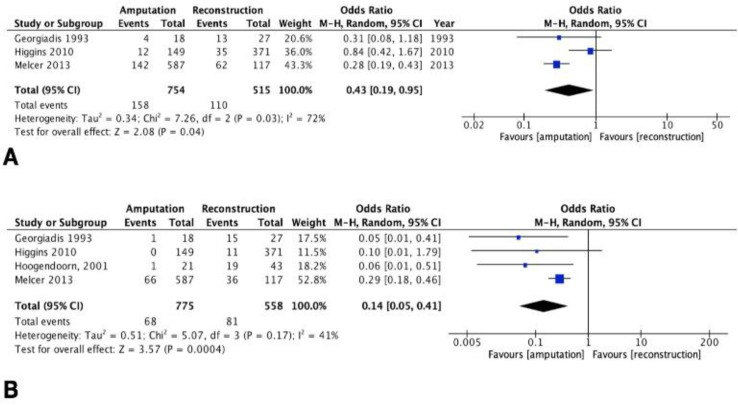
Infection
The rate of infection was reported in three of the included studies3,9,12 and the rate of osteomyelitis in four of the includes studies.3,6,9,12 The meta-analysis showed a statistically significant lower number of infections (odds ratio [OR] 0.43, 95% confidence interval [CI] 0.19-0.95, P=0.04, [Figure 6A]) and a statistically significant lower number of cases of osteomyelitis (odds ratio [OR] 0.14, 95% confidence interval [CI] 0.05-0.41, P=0.0004, [Figure 6B]) in the amputation group and moderate heterogeneity among the studies (I2=72% and I2=41% respectively).
Figure 6.
Forest plot of A. infection rate and B. Cases of osteomyelitis in amputation versus reconstruction in severe lower limb injury
Sensitivity analysis
We conducted a sensitivity analysis by removing each study individually to assess the heterogeneity and robustness of the pooled results. The sensitivity analysis indicated that the results of the meta-analysis for all the outcomes were stable.
Discussion
The main results of this study demonstrate that following a severe lower extremity injury amputation is associated with lower rehospitalization rates, lower length of hospital stay, lower number of operations and additional surgery and fewer cases of infection and osteomyelitis. On the other hand, limb reconstruction leads to a faster return to work and lower rates of depression. The outcomes with respect to function and pain varied between the studies. It should be noted, though, that the results were statistically significant only with regards to rehospitalization and infection rate.
The meta-analysis clearly demonstrates that amputation leads to a faster recovery compared to a reconstructive procedure. Reconstruction of a mangled extremity is a complex process that often requires multiple operations, multiple rehospitalizations and additional surgeries and, as a result, a longer overall length of hospital stay. Interestingly, despite the faster recovery of amputees, this study demonstrated a tendency towards faster return to work and lower risk of adverse mental health outcomes in the long-term in the patients that undergo a reconstruction.
The outcomes in terms of function varied between the included studies. However, the studies in the military population consistently showed improved function following an amputation. It is well established that prosthetic ambulation requires more energy expenditure. Aerobic capacity decreases with age or associated comorbidities and this may be the reason why soldiers, who are in general young and fit, had improved functional outcomes with an amputation. However, the military population is not a representative sample of the entire population, therefore generalizability of these outcomes is not justifiable.
The decision as to whether to attempt to salvage or amputate a severely injured lower limb is always very challenging. This in part is due to the multiple factors that need to be taken into consideration for a life changing injury. Thirty years ago, Johansen and his colleagues developed the Mangled Extremity Severity Score (MESS) as a tool to predict the need for an amputation.18 The MESS tool takes into consideration the skeletal and soft-tissue damage, the limb ischemia, the presence of shock, and the age of the patient. Nevertheless, several studies have subsequently questioned the diagnostic accuracy and the clinical utility of the MESS tool.19-21 most authors since then have advocated a more individualized approach for each patient. This study was designed to compare all the elements that the treating surgeon has to take into account when deciding between a reconstruction and an amputation.
A meta-analysis, by definition, is the quantitative synthesis of separate studies that uses statistical methods to combine the results and draw conclusions. Akula et al. performed a study to compare amputation and reconstruction in severe lower extremity injury.22 However, they only compared functional outcomes from a patient’s perspective and they were also not able to make a quantitative synthesis of the results. Busse et al. systematically reviewed the outcomes between an amputation and a salvage procedure.23 they did not, however, combine their results by using statistical methods. In addition, these studies were performed over a decade ago and since then reconstructive procedures have evolved significantly. To the best of our knowledge, this is the first quantitative synthesis of studies comparing amputation and reconstruction in severe lower limb injury.
The present study has to be seen in light of some limitations. Our results are based on the pooling of observational studies, which introduces selection bias due to the lack of randomization and bias related to measurement of the outcome, since there is no blinding of the participants or the assessors. Unfortunately, there are no Randomized Controlled Trials (RCTs) in the literature comparing reconstruction and amputation for lower extremity injuries and future studies should focus on that. The present meta-analysis includes data from heterogeneous study populations, civilian and military, and with heterogeneous injuries, either tibia or foot injuries or both. Different populations and different injuries may be associated with variable outcomes; therefore, these results should be interpreted with caution.
Conclusion
In conclusion, amputation is associated with a faster recovery in patients with severe lower limb injuries. On the other hand, reconstruction may lead to a faster return to work and may yield improved psychological outcomes. It is inconclusive as to which option leads to better function and less pain. High-quality RCTs are necessary for a more comprehensive evaluation of these treatments and to further our conclusions.
Acknowledgment
Not applicable
Conflict of interest:
None
Funding:
None
References
- 1.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Sterne JA, Hernan MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Georgiadis GM, Behrens FF, Joyce MJ, Earle AS, Simmons AL. Open tibial fractures with severe soft-tissue loss Limb salvage compared with below-the-knee amputation. J Bone Joint Surg Am. 1993;75:1431–1441. doi: 10.2106/00004623-199310000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Dahl B, Andersson AP, Andersen M, Ebskov LB, Reumert T. Functional and social long-term results after free tissue transfer to the lower extremity. Ann Plast Surg. 1995;34:372–375. doi: 10.1097/00000637-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Hertel R, Strebel N, Ganz R. Amputation versus reconstruction in traumatic defects of the leg: outcome and costs. J Orthop Trauma .1996. 10:223–229. doi: 10.1097/00005131-199605000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Dagum AB, Best AK, Schemitsch EH, Mahoney JL, Mahomed MN, Blight KR. Salvage after severe lower-extremity trauma: are the outcomes worth the means? Plast Reconstr Surg. 103: 1212–1220. doi: 10.1097/00006534-199904040-00017. [DOI] [PubMed] [Google Scholar]
- 7.Hoogendoorn JM, van der Werken C. Grade III open tibial fractures: functional outcome and quality of life in amputees versus patients with successful reconstruction. Injury. 2001;32:329–334. doi: 10.1016/s0020-1383(00)00250-3. [DOI] [PubMed] [Google Scholar]
- 8.Bosse MJ, MacKenzie EJ, Kellam JF, et al. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N Engl J Med. 2002;347:1924–1931. doi: 10.1056/NEJMoa012604. [DOI] [PubMed] [Google Scholar]
- 9.Higgins TF, Klatt JB, Beals TC. Lower Extremity Assessment Project (LEAP)--the best available evidence on limb-threatening lower extremity trauma. Orthop Clin North Am .2010;41:233–239. doi: 10.1016/j.ocl.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Doukas WC, Hayda RA, Frisch HM, et al. The Military Extremity Trauma Amputation/Limb Salvage (METALS) study: outcomes of amputation versus limb salvage following major lower-extremity trauma. J Bone Joint Surg Am. 2013;95:138–145. doi: 10.2106/JBJS.K.00734. [DOI] [PubMed] [Google Scholar]
- 11.Ellington JK, Bosse MJ, Castillo RC, MacKenzie EJ. The mangled foot and ankle: results from a 2-year prospective study. J Orthop Trauma. 2013;27:43–48. doi: 10.1097/BOT.0b013e31825121b6. [DOI] [PubMed] [Google Scholar]
- 12.Melcer T, Sechriest VF, Walker J, Galarneau M. A comparison of health outcomes for combat amputee and limb salvage patients injured in Iraq and Afghanistan wars. J Trauma Acute Care Surg, 2013;75(2):S247–54. doi: 10.1097/TA.0b013e318299d95e. [DOI] [PubMed] [Google Scholar]
- 13.Demiralp B, Ege T, Kose O, Yurttas Y, Basbozkurt M. Amputation versus functional reconstruction in the management of complex hind foot injuries caused by land-mine explosions: a long-term retrospective comparison. Eur J Orthop Surg Traumatol. 2014;24:621–626. doi: 10.1007/s00590-013-1345-4. [DOI] [PubMed] [Google Scholar]
- 14.Edelstein DA, Florescu I. Crushing injuries of the foot and ankle, with complex open fractures: result of a prospective study with a 3 year follow-up. J Med Life . 2016;9:255–258. [PMC free article] [PubMed] [Google Scholar]
- 15.Ladlow P, Phillip R, Coppack R, et al. Influence of Immediate and Delayed Lower-Limb Amputation Compared with Lower-Limb Salvage on Functional and Mental Health Outcomes Post-Rehabilitation in the U K Military. J Bone Joint Surg Am. 2016;98:1996–2005. doi: 10.2106/JBJS.15.01210. [DOI] [PubMed] [Google Scholar]
- 16.Barla M, Gavanier B, Mangin M, Parot J, Bauer C, Mainard D. Is amputation a viable treatment option in lower extremity trauma? Orthop Traumatol Surg Res. 2017;103:971–975. doi: 10.1016/j.otsr.2017.05.022. [DOI] [PubMed] [Google Scholar]
- 17.Fioravanti M, Maman P, Curvale G, Rochwerger AA, Mattei JC. Amputation versus conservative treatment in severe open lower-limb fracture: A functional and quality-of-life study. Orthop Traumatol Surg Res. 2018;104:277–281. doi: 10.1016/j.otsr.2017.12.013. [DOI] [PubMed] [Google Scholar]
- 18.Johansen K, Daines M, Howey T, Helfet D, Hansen Jr ST. Objective criteria accurately predict amputation following lower extremity trauma. J Trauma. 1990;30:568–572. doi: 10.1097/00005373-199005000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Bosse MJ, MacKenzie EJ, Kellam JF, et al. A prospective evaluation of the clinical utility of the lower-extremity injury-severity scores. J Bone Joint Surg Am. 2001;83:3–14. doi: 10.2106/00004623-200101000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Schiro GR, Sessa S, Piccioli A, Maccauro G. Primary amputation vs limb salvage in mangled extremity: a systematic review of the current scoring system. BMC Musculoskelet Disord. 2015;16:372 . doi: 10.1186/s12891-015-0832-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loja MN, Sammann A, DuBose J, et al. The mangled extremity score and amputation: Time for a revision. J Trauma Acute Care Surg. 2017;82:518–523. doi: 10.1097/TA.0000000000001339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Akula M, Gella S, Shaw CJ, McShane P, Mohsen AM. A meta-analysis of amputation versus limb salvage in mangled lower limb injuries--the patient perspective. Injury. 2011;42:1194–1197. doi: 10.1016/j.injury.2010.05.003. [DOI] [PubMed] [Google Scholar]
- 23.Busse JW, Jacobs CL, Swiontkowski MF, Bosse J, Bhandari M. Evidence-Based Orthopaedic Trauma Working G Complex limb salvage or early amputation for severe lower-limb injury: a meta-analysis of observational studies. J Orthop Trauma. 2007;21:70–76. doi: 10.1097/BOT.0b013e31802cbc43. [DOI] [PubMed] [Google Scholar]