ABSTRACT
The aim of this retrospective study was to describe the etiology and characteristics of trigeminal nerve injuries referred to a specialized center in Buenos Aires, Argentina. A retrospective analysis was performed of patients referred from February 2016 to January 2020. Age, sex, intervention performed, nerve affected, time elapsed from injury, diagnosis, location, and whether patient had signed informed consent were recorded. A descriptive analysis of the data was made, and 95% confidence intervals were calculated for prevalence. The study sample consisted of 30 subjects (31 nerve injuries), 19 female and 11 male, average age (±SD) 40 ± 17 years. The inferior alveolar nerve was the most frequently injured nerve (74%,) while the lingual nerve accounted for 26%. The most common etiologies were inferior molar extractions (47%), dental implants (20%), and local anesthesia (13%). Other etiologies were autologous mandibular bone grafts for dental implants, removal of cysts associated with the inferior third molar, and endodontic treatment. Dental Institutions at which treatment was provided were found to be significantly associated with patients being warned and asked to sign informed consent (p<0.05), while dentists working at private offices requested fewer consents. The most frequent symptom was paresthesia, and 5 patients suffered spontaneous or evoked pain. Only 2 patients intended to file legal claims. Dentists should be aware of the debilitating effects resulting from trigeminal injuries, the complexity of their resolution and the importance of carefully planning dental procedures to prevent them.
Keywords: trigeminal nerve injuries, trigeminal nerve, mandibular nerve, inferior alveolar nerve, lingual nerve
RESUMEN
El objetivo de este estudio fue describir la etiología y características de las lesiones del nervio trigémino remitidas a un servicio de referencia especializado en Buenos Aires, Argentina. Se realizó un análisis retrospectivo de los pacientes remitidos desde febrero de 2016 a enero de 2020. Se registraron edad, género, intervención recibida, nervio afectado, tiempo transcurrido desde la lesión, diagnóstico, ubicación y firma del consentimiento informado previo a la intervención Se realizó un análisis descriptivo de los datos y se calcularon intervalos de confianza del 95%. La muestra del estudio consistió en 30 sujetos (31 lesiones nerviosas), 19 mujeres y 11 hombres, con una edad promedio (± DE) de 40 ± 17 años. Aproximadamente 3 de cada 4 lesiones correspondieron al nervio alveolar inferior, representando el resto al nervio lingual. Las etiologías más frecuentes fueron la extracción dentaria (47%), los implantes dentales (20%) y la aplicación anestesia local (13%). Otras etiologías fueron la regeneración ósea para la colocación de implantes mandibulares, la extirpación de quistes asociados al tercer molar inferior y el tratamiento endodóntico. Se encontró que el tipo de establecimiento donde se realizó el procedimiento odontológico que generó la lesión, se asoció significativamente con los pacientes a los que se les advirtió y se les pidió que firmen el consentimiento informado (p<0.05); los odontólogos que trabajan en consultorios privados obtienen una menor proporción de consentimientos que los de las instituciones. El síntoma más frecuente fue la parestesia y 5 pacientes sufrieron dolor espontáneo o evocado. Solo 2 pacientes tenían intención de iniciar acciones legales. Teniendo en cuenta que son lesiones potencialmente permanentes, y de resolución compleja, la comunidad odontológica debe realizar especiales esfuerzos para disminuir esta complicación.
Palabras clave: lesión nerviosa, nervio trigémino, nervio mandibular, nervio alveolar inferior, nervio lingual
INTRODUCTION
Sensory deficiencies of the trigeminal nerve manifest as numbness, lack of sensation, increased sensitivity, or even pain, with dental treatment being the most frequent etiology. Altered sensation and pain may interfere with speaking, eating, kissing, shaving, applying makeup, tooth brushing and drinking. Cases of depression, suicidal thoughts, self-biting, dribbling, and retention of food on the chin in public have also been observed 1 , 2 . Trigeminal nerve injuries can be caused by extraction of inferior third molars, dental implant surgery, ostectomy, incision, orthognathic surgery, maxillofacial trauma, surgery for oral pathology, edema and post-surgical infection, and even anesthetic injection 3-6 . The highest prevalence of trigeminal nerve injuries in oral surgery are the terminal branches of the mandibular nerve, the inferior alveolar nerve (IAN) and its mental branch, and the lingual nerve (LN) 7 . LN injury generates the most severe symptoms 8 and may affect the sense of taste 2 . In addition to the patient suffering, the professional becomes emotionally and legally involved. Medical-legal implications are another concern that has increased in recent years, probably due to an increase in dental implant surgery and endodontic therapy 9 .
The aims of this study were to analyze the etiology and characteristics of trigeminal nerve injuries that were referred to an Oral and Maxillofacial Surgery Department in Buenos Aires, Argentina and compare them to reports in the literature.
MATERIALS AND METHODS
A retrospective analysis was conducted of patients referred to the Oral and Maxillofacial Surgery Department of the School of Dentistry of Buenos Aires University, Argentina, from February 2016 to January 2020 .Atotal 3 0 patients with trigeminal nerve injuries were referred during this period. Referrals came mainly from dental and medical healthcare providers in Buenos Aires City and surroundings. Patients provided informed consent authorizing use of information without personal identification. The project was approved by the Ethics Committee of the School of Dentistry of Buenos Aires University (CETICA.FOUBA 002/2021). Clinical and image evaluations were performed. Age, sex, reason for consultation, nerve affected, time elapsed from injury to consultation, type of dental care facility (private office or dental institution where the dental procedure that caused the lesion was performed), description of the intervention, and medication provided were analyzed. Patients were asked whether they had been warned in advance regarding possible complications in the procedure, and whether they had been asked to sign informed consent. Pinprick testing and mapping of the affected zone, thermal stimulation, directional discrimination, two-point discrimination and subjective evaluation by the patient (including pain) were recorded.
Immediate treatment consisted of removal of the etiological agent 10 (1 case); medication only for the first week after injury with corticosteroids (dexamethasone 8 mg per day for 3 days, 4mg per day for 3 days, 1mg per day for 3 days), NSAIDs (ibuprofen 400mg per 8 hours for 21 days) 11-13 (10 cases). Other treatments consisted of low-frequency laser sessions when symptoms did not improve 14 (8 cases), or administration of carbamazepine when symptoms interfered with everyday activities (2 cases). In addition, neurological and psychological consultations were suggested.
The following numerical variables were described: mean, standard deviation (SD), median, minimum (Min), maximum (Max), first quartile (Q1) and third quartile (Q3). Categorical data were described using absolute frequencies (AF) and percentages with 95% confidence intervals (95% CI). The CI95 were estimated using the score method (Newcombe & Merino Soto, 2006). For the comparison of frequencies, Chi-square or Fisher’s exact test were used, with a significance level of 5%. The following software was used: Calc, from Apache OpenOfficeTM v. 4.1.6 (Apache Software Foundation, 2018), Infostat v. 2020 (Di Rienzo et al., 2020) and MedCalc v. 19.2.6 (MedCalc Software bvba, 2020).
For a review of the literature, Medline/PubMed was searched using the terms "trigeminal nerve injury” till August 2021. Articles reporting series of trigeminal nerve injury caused by dental procedures were selected.
RESULTS
Thirty patients were evaluated, 19 female (63%) and 11 male (37%) (ratio 1.7 to 1), average age 40 ± 17 years (median = 37, Q1-Q3 = 26-54). Time from injury to consultation ranged from immediately after the surgery to 3 years (median = 14 days, Q1-Q3 = 6-60; mean ± SD = 115 ± 282).
Injuries were generated at two types of dental care facilities: dental institutions and prívate offices. There were 15 cases from each (50%; 95% CI: 33% to 67%). Nineteen patients had been warned of the possibility of injury (63%; 95% CI: 46% to 78%), while 11 patients had not been warned (37%; 95% CI: 22% to 54%). A significant association was found between type of dental care facility and warning to the patient (Chi-square = 17; df = 1; p<0.05): while only 4 of 15 patients (27%) had been warned at the private offices, all 15 patients (100%) had been warned at the dental institutions. Regarding informed consent, 21 patients had been asked to sign prior to the intervention (70%; 95% CI: 52% to 83%), while 9 patients had not been asked sign (30%; 95% CI: 17% to 48%). A significant association was found between type of dental care facility and being asked to sign informed consent (Fisher’s exact test: p<0.05): while 6 of 15 patients had been asked to sign at the private offices (40%), all 15 patients (100%) had been asked to sign at the dental institutions.
All injuries corresponded to the mandibular branch of the trigeminal nerve. IAN was affected in 22 cases and LN in 7 cases. One patient presented injury of both nerves after the extraction of an impacted mandibular third molar. IAN involvement was found to be significantly more frequent (Chi-square = 7.26; df = 1; p<0.05).
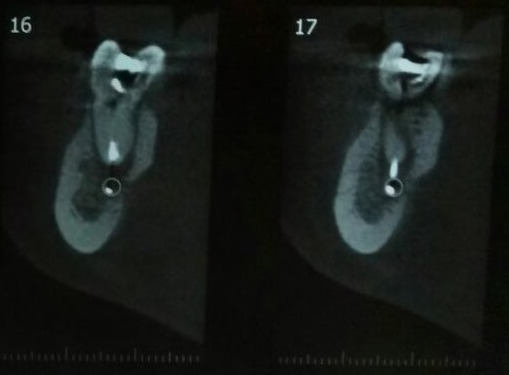
The most frequent cause of nerve injury was tooth extraction, which accounted for almost half the cases ( Table 1 ). All these injuries corresponded to lower molars (11 third molar, 2 second molar, and 1 first molar). In one of the cases of extraction of the lower second molar, a conjunction with another complication occurred: a bisphosphonate-related osteonecrosis of the jaws (zoledronic acid). All LN injuries after extraction (6 cases) corresponded to lower third molar. Fig. 1 shows an example of a case of inferior alveolar nerve injury during extraction of an impacted lower third molar. The second most frequent etiology was mandibular dental implant placement. Four dental implant injuries were by direct trauma ( Fig. 2 ) (1 first molar delayed placement, 1 second premolar delayed placement, 1 first premolar delayed placement, and 1 first premolar immediate placement); and 2 were by indirect trauma ( Fig. 3 ) (1 first molar immediate placement, and 1 second molar delayed placement). One of the cases of nerve injury due to the injection of local anesthesia was caused by a buccal mandibular infiltration in the area of the mental foramen, while the other 3 were caused by the application of the inferior alveolar nerve block technique (Halstead approach) in the IAN (1 case) and LN (2 cases). In addition, 3 nerve injuries after inlay autogenous posterior mandible block graft harvested from the mandibular ramus were recorded, and 2 lesions after the removal of cysts associated with the inferior third molar. There was one injury due to an overextended endodontic treatment in the distal root of an inferior first molar, with a paste containing zinc oxide and iodoform (Klepp Licon D®, Argentina) ( Fig. 4 ).
Table 1. Distribution of cases according to etiology.
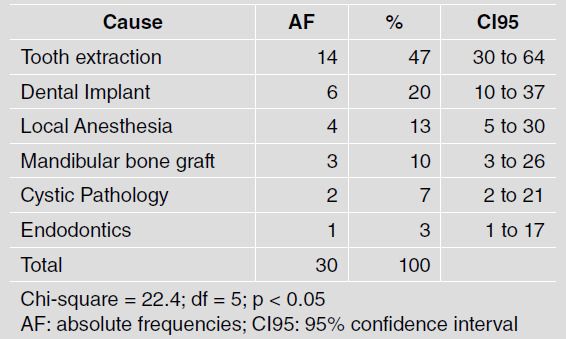
Fig. 1. Female patient, 45 years old, with inferior alveolar nerve injury due to extraction of lower third molar. A. CAT scan prior to extraction (yellow circle marks the lower alveolar canal). B. Clinical photograph showing inferior alveolar nerve.
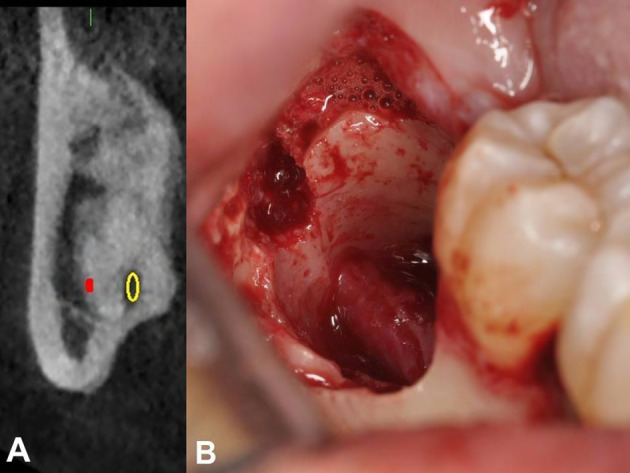
Fig. 2. Male patient, 65 years old, with inferior alveolar nerve injury. Radiograph showing direct trauma generated by the implant (lower first molar) in the inferior alveolar canal.
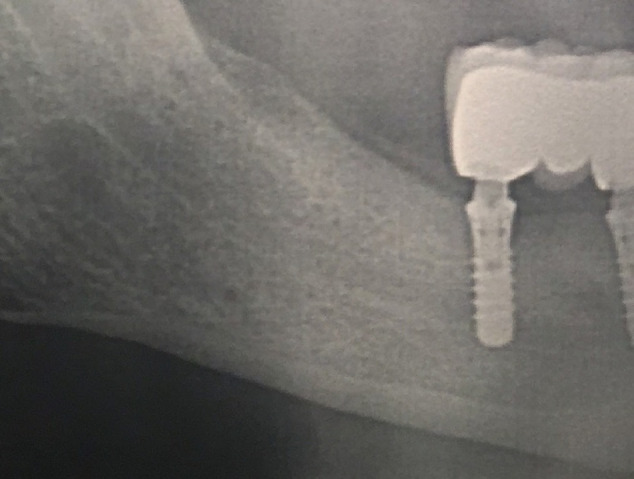
Fig. 3. Female patient, 38years old, with inferior alveolar nerve injury. CAT sean showing the indirect trauma generated by the implant (lowerfirst molar) as a hypodense zone above the inferior alveolar canal.
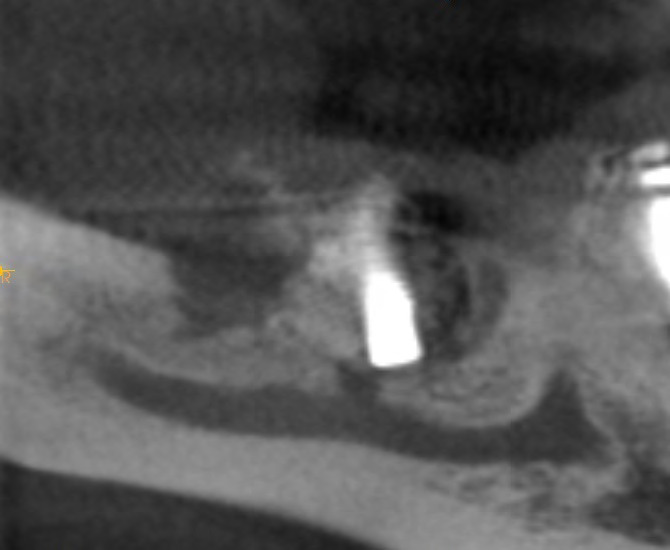
Fig. 4. Female patient, 56 years old, with inferior alveolar nerve injury. CAT sean taken after endodontie treatment, showing presence offilling material within the inferior alveolar canal (distal root of lower first molar).
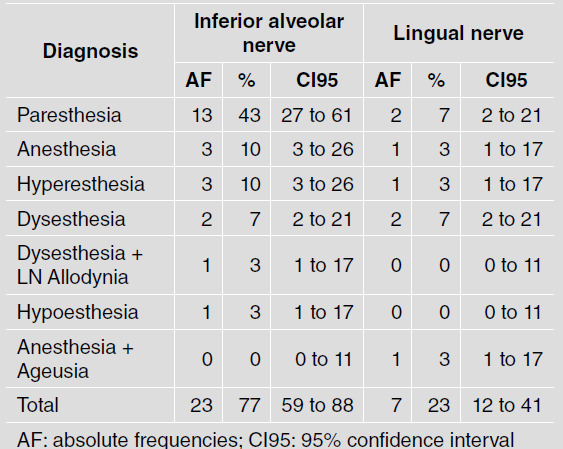
Regarding sensory and gustatory disturbances, the most frequent injury was paresthesia (50%). The second and third most frequent symptoms were anesthesia and dysesthesia, each with 17% of the cases. One LN anesthesia case also referred ageusia. One of dysesthesia cases also presented allodynia of the LN. Hyperesthesia accounted for 13% of the cases, and there was one case of hypoesthesia of the IAN ( Table 2 ).
Table 2. Distribution according to sensory and gustatory lesions.
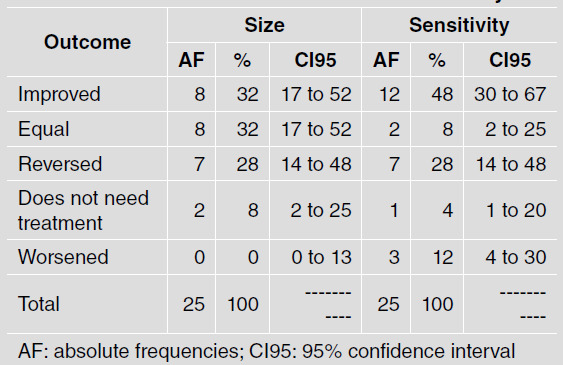
The evolution of nerve injuries was recorded in 25 patients, because 5 patients did not attend the follow-up visits. Twenty-eight percent of the lesions completely reversed in terms of size and sensitivity; while of the remaining 72% of the lesions, 67% improved in sensitivity, and 44% in size. In 3 patients, an unfavorable evolution of sensitivity was observed, with worsening of the symptoms ( Table 3 ). In the group of 10 patients treated with dexamethasone and ibuprofen during the first week after injury, 3 cases achieved total reversal, and 7 had improved symptoms. Of the 15 patients who were prescribed medication, 4 reversed, 5 improved, 3 remained unchanged, and 3 worsened (p>0.05). Only 2 of the 30 patients (female patients, 21 and 26 years old) said they intended to take legal actions for the injury suffered. They both had LN injuries (anesthesia and hyperesthesia) due to inferior third molar extraction (one performed at a prívate office and the other at a dental institution) and considered their personal and professional lives to be affected by the difficulties generated by the injury, mainly in their speech.
Table 3. Distribution according to the evolution of the lesion in relation to size and sensitivity.
The literature review found 8 series reporting nerve injuries caused by dental procedures, including 42 to 1331 cases. The largest of these (1331 cases) is a recent multi-site study conducted in the UK and Belgium 15 ; and the second largest is another European series (Denmark) with 449 cases 8 . Other European studies present 42 to 56 patients 7 , 16 17 ; and studies from USA and Canada report on 73 to 165 cases 2 , 18 19 . No report was found from Latin America.
DISCUSSION
Trigeminal nerve injuries have low prevalence and there are few reports on them. The current study reports the first series from Latin America. Most injuries involved the inferior alveolar nerve and the lingual nerve, with reports of buccal, infraorbital or palatine nerves being rare 2 , 8 16 . Some studies have reported higher prevalence of IAN injuries than LN injuries 2, 15-17 , while others have observed more injuries ofthe LN 8 , 19 . In our series, three out of four injuries were IAN.
There is broad consensus that inferior third molar surgery is the most prevalent cause of trigeminal nerve injuries in dentistry 2 , 8 9 15 16 . In two of the series reported, the IAN Is the nerve most often affected during third molar extraction 2 , 16 , while another series reports more LN injuries 8 . In our series, the distribution was even (50% for each nerve, one patient with both nerves affected). Correct planning of flap design and careful dissection of soft tissues are essential to reduce LN injuries 8 , 20 . Ostectomy has been statistically associated with greater permanent lingual nerve damage than has tooth sectioning 20 . Factors associated with IAN injury include difficult surgery, surgeon’s experience, and proximity to the IAN canal 21 , 22 . If close proximity is confirmed, the risks of temporary and permanent IAN injury are 20% and 1-4% respectively 23 . The patient should be clearly warned of this complication prior to surgery. If the tooth is non-vital, or pathology is associated, careful ostectomy, root sectioning, and tooth removal are recommended. If the tooth is vital and the patient is not compromised, coronectomy of the tooth should be an alternative 24 , 25 .
Reported incidences of implant-related injuries range from 4% to 17% ofthe total nerve injuries 2 , 8 10 . There has been an increase in IAN injuries parallel to the increase in implant surgery 17 . In our series, one out of five injuries occurred during implant placements. Lin et al. 26 reported occurrence of short-term (10 days after implant placement) and long-term incidence (1 year after implant placement) of implant-related IAN injuries of 13% and 3%, respectively, although other authors have reported long-term injuries below 1% 27 , 28 . Nerve injuries associated to dental implant surgery are almost exclusively related to the inferior alveolar nerve, with few reported cases of lingual nerve. When the professional is not sure of placing the implants with a safety zone (> 2 mm) to the mandibular canal, a cone beam computed tomography (CBCT) scan is required to take proper bone measurements. Intra-operative radiographs during implant bed preparation are useful to evaluate the distance to the mandibular canal 29 . Special attention and diagnosis should be ensured for immediate implants in the premolar area because the mental foramen often exits next to the apex of both premolars 11 . Dental implant injuries could be caused by direct (mechanical or chemical), or indirect (hemorrhage or scarring) trauma; professionals should pay special attention to bone density near the inferior alveolar canal 28 . It is important to note that intraoperative pain under mandibular infiltration technique is not an indicator of proximity to the canal. Pain under this technique is associated with surgical time and presence of adjacent teeth 30 . A sudden ‘give’ (feeling of sudden emptiness when drilling the bone tissue) during preparation may be indicative of protrusion through the lingual or buccal plate but may also be associated with perforation of the IAN canal roof. If the professional is not sure of not having intruded into the canal, it is recommended not to place the implant. Moreover, if there is persistent numbness after local anesthesia has worn off, it is recommended to remove the implant before 24-36 hours 10 .
Few patients with inferior IAN injury resulting from major maxillofacial surgery or orthognathic surgery present significant complaints. This may be due to the clear pre-surgical consent and information, along with the significant perceived benefits of the surgery 9 . Two studies 7 , 8 have reported 4 and 15% of this type of injury resulting from orthognathic surgery. In our series, no injury was reported as a result of this procedure.
Any tooth requiring endodontic therapy in close proximity to the IAN canal requires special attention. If the root canal is overprepared and the apex opened, chemical and physical nerve injuries are possible. Current knowledge of endodontic-related nerve injuries relies primarily on single case reports. It has been reported that tooth locations (mandibular molars), types of extruded materials (most report paraformaldehyde-containing sealer) and obturation technique are factors that may affect nerve injury prognosis 12 . Reported IAN injuries after endodontic treatment, account for 1.4 to 6% of total trigeminal nerve injuries 2 , 8 16 ; we found 3% in our series. Early surgical removal of the excess of endodontic material in contact with the nerve provides the best recovery prognosis (before 72 hours) 31 . Apex and/or tooth removal within 24 hours could also be considered 9 . Nerve injuries caused by local anesthetic injection occur in approximately one in every 25,000 to 175,000 inferior alveolar nerve blocks 19 . It is the second reason for nerve injuries in many studies, accounting for 12.3%-17% 2 , 8 16 . The nerve that is usually damaged during IAN block injections is the LN, which accounts for 70-78% 2 , 8 . In our series, 13% of total injuries were caused by anesthesia injections, mainly IAN nerve blocks, also affecting more LN (66%) than IAN (33%). We observed a rare case of IAN injury when buccal infiltrative anesthesia was applied next to the mental foramen to place a clamp for rubber dam isolation during a composite restoration. We observed a rare case of IAN injury when buccal infiltrative anesthesia was applied next to the mental foramen to place a clamp for rubber dam isolation during a composite restoration. Recovery from lesions caused by anesthetic injections has been reported to take place at 8 weeks in 85-94% of cases 32 . Reports of ‘electric shock’ type sensation during IAN block application is not a specific sign of nerve injury 9 . Low injection pressures, and needles with short bevel angles (45°) may produce less damage than long bevel needles (14°) 33 . Higher incidences have been reported when multiple injections, high concentration local anesthetics, and articaine over lidocaine were applied 9 , 20 , though it is not yet conclusive whether articaine is more likely to induce permanent nerve injury 34 . Unexplainably, several studies on nerve injuries in dentistry report a higher incidence in females, with ratios of 3.3 to 1 19 , 2.8 to 1 8 , 2.1 to 1 16 , 1.9 to 1 1 , 1.8 to 1 17 , 1.5 to 1 2 , and 1.4 to 1 15 . Our study also found predominance in females, with a ratio of 1.7 to 1. This is probably only due to the fact that more women than men seek dental care 8 , 12 . There is a wide range of nerve injury clinical symptoms, spanning from minimal anesthesia in a small area to devastating effects on the patient’s quality of life, such as spontaneous pain. Paresthesia is the main symptom in trigeminal injuries, accounting for approximately half of the cases 1 , 8 , as observed in our study. The prevalence of other symptoms is variable, with the most prevalent being anesthesia, hyperesthesia, dysesthesia, and allodynia 1 , 8 . In our series, 5 patients suffered spontaneous or evoked pain and 4 patients had unpleasant increased sensitivity.
In a series of trigeminal nerve injuries from USA, 40% of the patients had filed legal claims against the professionals 19 , and another study reported that 20% of patients filed lawsuits 18 . Other reports have observed that more than half the lawsuits are associated to the lack of pre-operative informed consent for implant surgery, and most are associated to premolar implants 35 . In our series of 30 patients, only 2 patients intended to sue the acting professionals. Ten patients who were not warned of the possibility of injury did not show intentions of making legal claims. This difference may be due to the observed populations having different idiosyncrasies. Professionals should not underestimate the possibility of generating nerve injuries, and should inform the patient of the risks and benefits of the clinical practice. Informed consent prior to any implant surgery is a legal agreement that cannot be ignored 36 . In a series of 30 patients who suffered nerve alterations after implant placement in England, only 46% had been asked to sign the consent and 27% said that they had not been warned of this complication 1 . In our study, a significant difference was observed regarding informed consent depending on the type of dental care facility: professionals in their prívate offices requested fewer informed consents and warned patients less than those who worked at dental institutions.
Trigeminal nerve injury treatment is still controversial, probably due to its low prevalence and the difficulty in designing comparative studies. When nerve injury is confirmed, early removal of the etiological factor, and early administration of oral corticosteroids and NSAIDs are recommended 10-13 . The latter recommendation could not be confirmed in the current study, but further studies using larger samples may be able to clarify this point. Low-level laser therapy and microsurgery have been proposed, although results are controversial 12-14 . Peripheral neuropathy due to diabetes mellitus, alcohol use, hypothyroidism or nutritional deficiency may affect recovery 33 . In a systematic review of the literature on treatment of nerve disorders, it was concluded that clinical trials are still needed to investigate the effectiveness of surgical, pharmacological and physiological treatments 37 . Early referral and treatment appear to be the key factors for better prognosis.
Dentists should be aware of the debilitating effects resulting from trigeminal nerve injuries, the complexity of their resolution and the importance of carefully planning dental procedures to prevent them.
Funding Statement
This study was financially supported by the School of Dentistry of Buenos Aires University. Grant CD 330/19-01
Footnotes
FUNDING This study was financially supported by the School of Dentistry of Buenos Aires University. Grant CD 330/19-01
REFERENCES
- 1.Renton T, Dawood A, Shah A, Searson L, et al. Post-implant neuropathy of the trigeminal nerve. A case series. Br Dent J. 2012;212:E17. doi: 10.1038/sj.bdj.2012.497. [DOI] [PubMed] [Google Scholar]
- 2.Tay AB, Zuniga JR. Clinical characteristics of trigeminal nerve injury referrals to a university centre. Int J Oral Maxillofac Surg. 2007;36:922–927. doi: 10.1016/j.ijom.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 3.Kaleem A, Amailuk P, Hatoum H, Tursun R. The Trigeminal Nerve Injury. Oral Maxillofac Surg Clin North Am. 2020;32:675–687. doi: 10.1016/j.coms.2020.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Pogrel MA. Nerve damage in dentistry. Gen Dent. 2017;65:34–41. [PubMed] [Google Scholar]
- 5.Palma-Carrió C, Balaguer-Martínez J, Peñarrocha-Oltra D, Peñarrocha-Diago M. Irritative and sensory disturbances in oral implantology. Literature review. Med Oral Patol Oral Cir Bucal. 2011;16:e1043–e1046. doi: 10.4317/medoral.17125. [DOI] [PubMed] [Google Scholar]
- 6.Joachim M, Tabib R, Laviv A, Pikovsky A, et al. Trigeminal Neuropathy After Mandibular Fractures: Epidemiology and Neurophysiologic Diagnosis. J Craniofac Surg. 2019;30:1113–1117. doi: 10.1097/SCS.0000000000005215. [DOI] [PubMed] [Google Scholar]
- 7.Agbaje JO, Van de Casteele E, Hiel M, Verbaanderd C, et al. Neuropathy of Trigeminal Nerve Branches After Oral and Maxillofacial Treatment. J Maxillofac Oral Surg. 2016;15:321–327. doi: 10.1007/s12663-015-0843-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hillerup S. Iatrogenic injury to oral branches of the trigeminal nerve: records of 449 cases. Clin Oral Investig. 2007;11:133–142. doi: 10.1007/s00784-006-0089-5. [DOI] [PubMed] [Google Scholar]
- 9.Renton T. Prevention of iatrogenic inferior alveolar nerve injuries in relation to dental procedures. Dent Update. 2010;37:350–360. doi: 10.12968/denu.2010.37.6.350. [DOI] [PubMed] [Google Scholar]
- 10.Khawaja N, Renton T. Case studies on implant removal influencing the resolution of inferior alveolar nerve injury. Br Dent J. 2009;206:365–370. doi: 10.1038/sj.bdj.2009.258. [DOI] [PubMed] [Google Scholar]
- 11.Juodzbalys G, Wang HL, Sabalys G. Injury of the Inferior Alveolar Nerve during Implant Placement: a Literature Review. J Oral Maxillofac Res. 2011;2:e1–20. doi: 10.5037/jomr.2011.2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosen E, Goldberger T, Taschieri S, Del Fabbro M, et al. The Prognosis of Altered Sensation after Extrusion of Root Canal Filling Materials: A Systematic Review of the Literature. J Endod. 2016;42:873–879. doi: 10.1016/j.joen.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 13.Misch CE, Resnik R. Mandibular nerve neurosensory impairment after dental implant surgery: management and protocol. Implant Dent. 2010;19:378–386. doi: 10.1097/ID.0b013e3181effa92. [DOI] [PubMed] [Google Scholar]
- 14.Miloro M, Criddle TR. Does Low-Level Laser Therapy Affect Recovery of Lingual and Inferior Alveolar Nerve Injuries? J Oral Maxillofac Surg. 2018;76:2669–2675. doi: 10.1016/j.joms.2018.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Van der Cruyssen F, Peeters F, Gill T, De Laat A, et al. Signs and symptoms, quality of life and psychosocial data in 1331 post-traumatic trigeminal neuropathy patients seen in two tertiary referral centres in two countries. J Oral Rehabil. 2020;47:1212–1221. doi: 10.1111/joor.13058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klazen Y, Van der Cruyssen F, Vranckx M, et al. Iatrogenic trigeminal post-traumatic neuropathy: a retrospective twoyear cohort study. Int J Oral Maxillofac Surg. 2018;47:789–793. doi: 10.1016/j.ijom.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 17.Deppe H, Mücke T, Wagenpfeil S, Kesting M, et al. Trigeminal nerve injuries after mandibular oral surgery in a university outpatient setting--a retrospective analysis of 1,559 cases. Clin Oral Investig. 2015;19:149–157. doi: 10.1007/s00784-014-1222-5. [DOI] [PubMed] [Google Scholar]
- 18.Caissie R, Goulet J, Fortin M, Morielle D. Iatrogenic paresthesia in the third division of the trigeminal nerve: 12 years of clinical experience. J Can Dent Assoc. 2005;188:185–219. [PubMed] [Google Scholar]
- 19.Pogrel MA, Thamby S. The etiology of altered sensation in the inferior alveolar, lingual, and mental nerves as a result of dental treatment. J Calif Dent Assoc. 1999;27:531,534–538. [PubMed] [Google Scholar]
- 20.Pippi R, Spota A, Santoro M. Prevention of Lingual Nerve Injury in Third Molar Surgery: Literature Review. J Oral Maxillofac Surg. 2017;75:890–900. doi: 10.1016/j.joms.2016.12.040. [DOI] [PubMed] [Google Scholar]
- 21.Kang F, Sah MK, Fei G. Determining the risk relationship associated with inferior alveolar nerve injury following removal of mandibular third molar teeth: A systematic review. J Stomatol Oral Maxillofac Surg. 2020;121:63–69. doi: 10.1016/j.jormas.2019.06.010. [DOI] [PubMed] [Google Scholar]
- 22.Cheung LK, Leung YY, Chow LK, Wong MC, et al. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg. 2010;39:320–326. doi: 10.1016/j.ijom.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 23.Renton T. Oral surgery: part 4. Minimising and managing nerve injuries and other complications. Br Dent J. 2013;215:393–399. doi: 10.1038/sj.bdj.2013.993. [DOI] [PubMed] [Google Scholar]
- 24.Monaco G, D’Ambrosio M, De Santis G, Vignudelli E, et al. Coronectomy: A Surgical Option for Impacted Third Molars in Close Proximity to the Inferior Alveolar Nerve-A 5-Year Follow-Up Study. J Oral Maxillofac Surg. 2019;77:1116–1124. doi: 10.1016/j.joms.2018.12.017. [DOI] [PubMed] [Google Scholar]
- 25.Cervera-Espert J, Pérez-Martínez S, Cervera-Ballester J, Peñarrocha-Oltra D, et al. Coronectomy of impacted mandibular third molars: A meta-analysis and systematic review of the literature. Med Oral Patol Oral Cir Bucal. 2016;21:e505–e513. doi: 10.4317/medoral.21074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin CS, Wu SY, Huang HY, Lai YL. Systematic Review and Meta-Analysis on Incidence of Altered Sensation of Mandibular Implant Surgery. PLoS One. 2016;11:e0154082. doi: 10.1371/journal.pone.0154082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vázquez-Delgado E, Viaplana-Gutiérrez M, Figueiredo R, Renton T, et al. Prevalence of neuropathic pain and sensory alterations after dental implant placement in a universitybased oral surgery department: A retrospective cohort study. Gerodontology. 2018;35:117–122. doi: 10.1111/ger.12326. [DOI] [PubMed] [Google Scholar]
- 28.Scarano A, Sinjari B, Murmura G, Lorusso F. Neurosensory Disturbance of the Inferior Alveolar Nerve After 3025 Implant Placements. Implant Dent. 2017;26:735–743. doi: 10.1097/ID.0000000000000651. [DOI] [PubMed] [Google Scholar]
- 29.Burstein J, Mastin C, Le B. Avoiding injury to the inferior alveolar nerve by routine use of intraoperative radiographs during implant placement. J Oral Implantol. 2008;34:34–38. doi: 10.1563/1548-1336(2008)34[34:AITTIA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 30.Garcia-Blanco M, Gualtieri AF, Puia SA. A randomized controlled trial comparing nerve block and mandibular infiltration techniques in posterior mandible implant surgeries. J Clin Exp Dent. 2018;10:e1003–e1010. doi: 10.4317/jced.54330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Castro R, Guivarc’h M, Foletti JM, Catherine JH, et al. Endodontic-related inferior alveolar nerve injuries: A review and a therapeutic flow chart. J Stomatol Oral Maxillofac Surg. 2018;119:412–418. doi: 10.1016/j.jormas.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 32.Smith MH, Lung KE. Nerve injuries after dental injection: a review of the literature. J Can Dent Assoc. 2006;72:559–564. [PubMed] [Google Scholar]
- 33.Hewson DW, Bedforth NM, Hardman JG. Peripheral nerve injury arising in anaesthesia practice. Anaesthesia. 2018;73(Suppl 1):51–60. doi: 10.1111/anae.14140. [DOI] [PubMed] [Google Scholar]
- 34.Baroni DB, Franz-Montan M, Cogo K, Berto LA, et al. Effect of articaine on mental nerve anterior portion: histological analysis in rats. Acta Odontol Scand. 2013;71:82–87. doi: 10.3109/00016357.2011.654243. [DOI] [PubMed] [Google Scholar]
- 35.Chaushu G, Taicher S, Halamish-Shani T, Givol N. Medicolegal aspects of altered sensation following implant placement in the mandible. Int J Oral Maxillofac Implants. 2002;17:413–415. [PubMed] [Google Scholar]
- 36.Pippi R, Spota A, Santoro M. Medicolegal Considerations Involving Iatrogenic Lingual Nerve Damage. J Oral Maxillofac Surg. 2018;76:1651.e1-1651.e13. doi: 10.1016/j.joms.2018.03.020. [DOI] [PubMed] [Google Scholar]
- 37.Coulthard P, Kushnerev E, Yates JM, Walsh T, et al. Interventions for iatrogenic inferior alveolar and lingual nerve injury. Cochrane Database Syst Rev. 2014;4:CD005293. doi: 10.1002/14651858.CD005293.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]


