Abstract
Objectives
This paper examines the health, work, and financial experiences of older adults with disabling conditions during the COVID-19 pandemic. It also explores the role of county- and state-level conditions in these experiences.
Methods
Using data from the 2020 Health and Retirement Study, we estimated regression models to assess differences in outcomes between those with and without disabling conditions and by race/ethnicity. We used multilevel modeling to assess whether and how county or state factors might be associated with the differences in these effects.
Results
Older adults with disabilities were more likely to report experiencing financial hardships, delaying health care, and experiencing effects on work than those without disabilities; these differences are heighted between race and ethnicity. Older adults with disabilities were more likely to live in counties with greater social vulnerability.
Discussion
This work underscores the importance of developing a robust, disability-inclusive public health response that protects older adults.
Keywords: disability, chronic conditions, epidemiology
Introduction and Background
The impacts of the COVID-19 pandemic have been experienced unequally across both geography and the social structure of the United States. In particular, older adults, historically marginalized racial groups, and people living in communities with low resources have been among those hardest hit by the myriad health and economic effects of the pandemic. This study examines the experiences of older adults with disabling conditions during the COVID-19 pandemic. It descriptively documents negative health, work, and financial experiences of older adults by disability status, focusing on its intersection with race and ethnicity. It also explores the role of contextual factors affecting health and economic conditions using county- and state-level data.
Older Americans have been disproportionately impacted by the COVID-19 pandemic. According to the Centers for Disease Control and Prevention, more than 81% of COVID-19 deaths have been among people older than 65 (as of August 2021), and the number of deaths in that age group is 80 times higher than the number of deaths among those ages 18–29 (CDC, 2021). Likewise, historically marginalized racial and ethnic groups, particularly non-Hispanic Black adults, have had higher rates of infection, hospitalization, and death compared with non-Hispanic White adults ( Kirby, 2020; Oppel et al., 2020; Price-Haywood et al., 2020). Observations of a disparate racial and ethnic burden of COVID-19 have been broadly documented across geographical regions (Polyakova et al., 2021).
Evidence suggests that preexisting vulnerabilities in the social environments in which people live exacerbate the risks of COVID infection. For example, counties with larger non-White populations experienced higher rates of COVID-19 deaths and hospitalizations (Schnake-Mahl & Bilal, 2021). In addition, people with disabilities who are non-White or live in households with incomes below the poverty level are significantly overrepresented in counties with higher COVID-19 incidence compared with other people with disabilities (Chakraborty, 2021). Similarly, emerging evidence suggests socioeconomic characteristics of counties are associated with both the severity and the transmission of COVID-19 infection (Andersen et al., 2021; Baum & Henry, 2020; Hatef et al., 2020).
Despite growing evidence about inequities in vulnerability across sociodemographic groups, surprisingly little is known about the experiences people with disabilities have had with COVID-19. Their risk factors include being more likely to have an underlying health problem (Dixon-Ibarra & Horner-Johnson, 2014; Stevens et al., 2014), live in a congregate care setting (McConkey et al., 2016), and rely on assistance with personal care and routine preventative measures (Armitage & Nellums, 2020).
Emerging evidence on this topic has been grim. A study of nearly 65 million patients across 547 health care centers in the United States found the mortality rate of people with intellectual and developmental disabilities was nearly eight times higher than the general population (Gleason et al., 2021). A similar study of more than two million health care patients in Canada found people with physical disabilities were more likely to die of COVID-19 than those without a disability, even after adjusting for a number of socioeconomic factors. A systematic review of the impacts of COVID-19 on people with physical disabilities suggests that the pandemic is associated with daily functioning—resulting in diminished access to health care, mood changes, and lower levels of physical activity (Lebrasseur et al., 2021).
These disparities in COVID outcomes have underscored the social and structural inequities that influence health and well-being, including the role of intersectionality. Originally introduced by Kimberle Crenshaw as a way to help explain the legal oppression of Black women (Crenshaw, 1989), intersectionality has developed as a theory suggesting that multiple and coexisting dimensions of marginalization or inequality, such as race, age, gender, or disability status, might have overlapping and cumulative effects beyond the sum of their individual parts. In other words, people at the intersection of more than one identity that has been disproportionately impacted by COVID might be particularly vulnerable to adverse outcomes (Bowleg 2020; Elnaiem 2020; Walubita et al., 2021). For example, emerging evidence indicates that older Black and Hispanic adults are more likely than their White counterparts to report food and housing insecurity and difficulty paying household expenses during the pandemic (Lopez, Rainie, and Budiman, 2020).
In particular, evidence shows that people with disabilities who are older, people of color, or both, might be particularly vulnerable to negative impacts of COVID-19. Already, racial differences in disability prevalence exist: Native American persons have the highest rate of disability (3 in 10), followed by Black persons (1 in 4), White persons (1 in 4), Native Hawaiians/Pacific Islander and Hispanic persons (1 in 6), and Asian persons (1 in 10) (Courtney-Long et al., 2017). These existing disparities motivate the potential for important intersectional difference in the impacts of COVID-19 for people with disabilities of different racial identities, hence motivating the research inquiries in this article.
COVID-19, Disability, Race, or Ethnicity, and Disparities in Work, Financial Security, and Health Care
Moreover, the virus’s impact on older adults with disabilities might go beyond a higher risk for serious infection and include limited access to care for all health conditions, financial implications, and effects on employment. Given the nature of the infection and the social mitigation strategies put into place for containment, COVID-19 can be considered a “social disease” (Trout & Kleinman, 2020), as it impacts social and economic domains of everyday life in addition to individual health. For older adults with disabilities, the impacts of COVID-19 might exacerbate existing differences in health care, employment, and financial security.
Even before the pandemic led to economic losses and a reduction in the U.S. workforce, the unemployment rates of people with disabilities were higher than those of people without a disability (Jashinky et al., 2021; BLS 2021). The effects of the pandemic on the labor market have amplified this concern. Between March and August 2020, employment of people with disabilities declined by 20%, compared with a 14% decline for those without a disability (BLS 2020a; 2020b).
The COVID-19 pandemic also dealt a unique shock to older workers (Davis, 2021). Roughly 3.7 million workers age 55 and older became unemployed between March and April 2020. By October 2021, the employment-population ratio of workers 55 and older was down 2.2% points from February 2020. Quinby et al. (2021) found that among workers age 55 and older, the likelihood of leaving work over the course of a year rose by 7.6% points, a 50% increase over the pre-pandemic rate.
The disruption of financial resources (job loss, unpaid leave, decreased household income, and economic hardship) for older adults with during a crisis can result in reduced access to other resources, such as food and preventive health care services (Abrams et al., 2021; Choi et al., 2022; Gauthier et al., 2021; Morris, 2022). For example, emerging evidence indicates that older Black and Hispanic adults are more likely than their White counterparts to report food and housing insecurity and difficulty paying household expenses during the pandemic (Lopez et al., 2020).
In light of this evidence, and the gaps therein, we sought to understand the COVID-19 pandemic’s effects on health, work, and financial experiences using nationally representative data for adults aged 50 and older with disabling conditions. We compared differences in outcomes between adults with and without disabling conditions. We emphasized intersectionality with racial and ethnic identity by examining differences across and within races and ethnicities. Finally, we examined the extent to which contextual factors are correlated with outcomes. Given the unique ways in which people with disabilities might interact physically and socially with their community, the role of contextual factors in COVID-related outcomes might be particularly important for people with disabilities.
Data and Methods
Data Sources
This study was based on data from the Health and Retirement Study (HRS). The HRS is a longitudinal survey that collects data on health, work, retirement, income, and other related topics from a nationally representative sample of the U.S. population age 50 and older (Sonnega et al., 2014). In 2020, the HRS included a module that asked about the effects of the COVID-19 pandemic on older adults’ ability to access health care, their finances, and their labor force participation (Health and Retirement Study 2021). We also used the 2018 RAND-HRS Longitudinal File, a cross-wave HRS file that has been cleaned and streamlined to track each HRS respondent from 1992 to 2018. 1 Finally, for our area-level analysis, we used the HRS Cross-Wave Geographic Information (Detail) Restricted Data file, which contains geographical data for each HRS respondent through 2018. We linked this file to the 2020 HRS file to determine the county and state of residence for each respondent in our sample.
For our area-level analysis, we drew from a number of publicly available data sources to characterize aspects of potential COVID vulnerability. We describe the measures further in Table 1 and in the Supplemental Materials.
Table 1.
List of Area-Level Contextual Data.
| Area-level factor | Source | Time Period | Definition | |
|---|---|---|---|---|
| COVID-19 risk and vulnerability | ||||
| Cases per 100,000 | COVID Act now | March 2020–May 2021 | This measure represents the average number of COVID-19 cases in a given county per 100,000 people. A higher number implies that COVID-19 was more prevalent in that county than others. We calculated monthly means by averaging daily data on cases per 100,000 people for each month. We then averaged the monthly means to get a mean cases per 100,000 metric across our time period | |
| Pandemic vulnerability index (PVI) score | PVI | March 2020–May 2021 | This measure aggregates components of pandemic vulnerability to create a PVI score of 0–1. Scores closer to 1 imply higher vulnerability to COVID-19. We used the PVI score for the first day of each month as the month-specific PVI. We then averaged the score across all months to get a mean PVI score across our time period | |
| Socioeconomic characteristics | ||||
| Social vulnerability index score | Agency for healthcare research and quality | 2018 | Ranks factors such as socioeconomic status, housing, transportation, and racial breakdown of a county to index its vulnerability to natural disasters and other emergencies. Values range from 0 to 1, where values closer to 1 imply higher social vulnerability | |
| Racial segregation, white versus non-white | County health rankings | 2015–2019 | This measure indexes the degree to which white and non-white residents are geographically segregated from one another within a county. Values range from 0 to 100, where values closer to 100 imply a higher level of segregation | |
| Medical infrastructure and health care access | ||||
| Hospital bed capacity | PVI subscore | June 2020 | This is a measure of the number of hospital beds divided by the population of the county. Values range from 0 to 1, with values closer to 1 implying that the county has a higher hospital capacity. We used the PVI hospital bed capacity subscore for the first day of each month as the month-specific capacity. We then averaged the score across all months to get a mean hospital bed capacity across our time period | |
| Years of potential life lost, all races | County health rankings | 2017–2019 | Age-adjusted rate of potential life lost from deaths of people under age 75 per 100,000 people in a given county. A higher value suggests a higher rate of premature death | |
| Employment opportunities and income | ||||
| Unemployment rate, all races | American community survey | 2016–2020 | This measure is the percentage of the population older than 16 who are unemployed. Values range from 0 to 100; values closer to 100 imply a higher rate of unemployment | |
| Percentage of people receiving government assistance | American community survey | 2016–2020 | This measure is the percentage of the total population in a county who receive cash public assistance or participate in the supplemental nutrition assistance program | |
| Governance | ||||
| Republican control of state | National conference of state legislature | 2020 | These data detail partisan composition of a state based on (1) the majority political party in control of the state legislature and (2) the party affiliation of the governor. States are defined as republican, democrat, or divided if the legislative and governor parties are different. We code 1 for republican and 0 otherwise | |
Sample
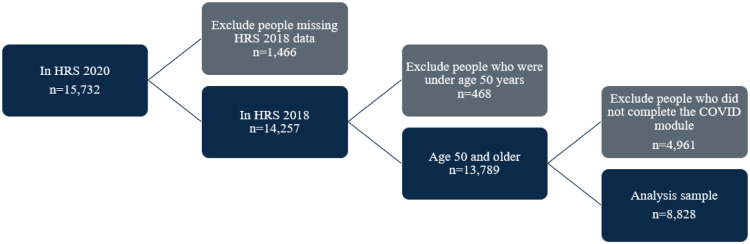
Our final sample included 8828 participants from the 2020 HRS. 2 Of these, 3155 participants were surveyed as part of the early-release sample. 3 Figure 1 displays the sample restrictions. We excluded from our analysis any participant who we could not match to the 2018 RAND file, because we use these data in our modeling to define respondent race, disabling condition, and covariates. 4 We also excluded participants younger than 50 because they did not meet our definition of older adult. Finally, we limited our sample to respondents who completed the COVID-19 module.
Figure 1.
Sample size and restrictions.
COVID Outcome Measures
We focused on three primary outcomes related to COVID-19: (1) health care delays, (2) financial hardship, and (3) effects on work. For each domain, we examined self-reported measures of whether the respondent experienced that outcome.
For health care delays, respondents were asked, “Since March 2020, was there any time when you needed medical or dental care, but delayed getting it, or did not get it at all?” Respondents who answered yes were asked to select why their care was delayed and what type of care was delayed. Respondents were also asked whether they thought they ever had COVID-19. They were then asked whether they had ever been tested for COVID-19. Those who answered yes were asked for their test results.
To assess financial hardship, respondents were first asked whether their income increased, decreased, or stayed the same. They were then asked to select the types of financial hardships they had experienced, such as missing a rent payment or being unable to pay a medical bill.
To assess work effects, respondents were asked, “Was your work affected because of the coronavirus pandemic?” Respondents who answered yes were asked whether they had to stop working entirely. If they were still working, they were asked whether they experienced effects, such as changes in hours and switching to remote work. Respondents could also indicate that they were not working at the time of the pandemic.
Definitions of Disability
For our primary analysis, we defined “disabling condition” as the presence of difficulty with an activity of daily living (ADL) or an instrumental activity of daily living (IADL). We examined whether respondents ever reported having difficulties with one or more ADL or IADL in any wave of the HRS through 2018. Recognizing that the term “disability” may encompass a broader spectrum of physical and mental functions, including self-identification, legal status, and chronic illnesses (Mauldin & Brown, 2021), we also considered four alternative measures of self-reported disability status: (1) the presence of a work-limiting condition when the 2018 HRS survey was fielded, (2) receipt of Supplemental Security Income (SSI) or Disability Insurance (DI) benefits in any wave of the HRS through 2018, (3) the presence of two or more chronic health conditions, and (4) the presence of five or more chronic health conditions. Because the sample population includes adults age 50 and older, many respondents were not working or were retired by 2018, regardless of disability status; measures (1) and (2) limit the pool of people who could meet the definition of “disability” to working-age older adults. Our measure using ADLs and IADLs reflects disability status among people of all ages or work statuses in our sample. This approach of combining ADLs and IADLs is often used to measure functional disability for older adults (Spector & Fleishman, 1998; Millán-Calenti et al., 2010; Gobbens, 2018; Wang et al. 2020). Results for the alternative measures of disability were qualitatively similar and can be found in the Supplemental Materials (Tables S9–S10).
Other Individual-Level Measures
We considered four mutually exclusive categories of race and ethnicity: (1) non-Hispanic White, (2) non-Hispanic Black, (3) non-Hispanic other race, and (4) Hispanic. Our other covariates included gender, birth year, education, marital status, HRS cohort, and number of long-term health conditions. 5
Area-Level Measures
We considered nine area-level contextual factors (Table 1). These factors were in five domains: (1) COVID-risk and vulnerability; (2) socioeconomic characteristics; (3) medical infrastructure and health care access; (4) employment opportunities and income; and (5) governance. We chose these domains based on the Healthy People 2030 domains of social determinants of health, adapted to be more specific to the needs and circumstances of people with disabilities as well as the emerging literature on specific domains salient to COVID-19 (Healthy People 2030). Eight of our measures are reported at the county level; governance is collected at the state level. Where possible, we chose data for contextual factors in the most recent year prior to the beginning of the COVID-19 pandemic in 2020. This was in order to capture the usual contextual environments of our respondents and so not to confound changes in social context due to COVID-19. (The exception to this was the domain of COVID risk and vulnerability, which we could only capture after the onset of the pandemic.) We linked these data to the individual-level HRS data through the county and state FIPS code available in the HRS Cross-Wave Geographic Information file.
Weights
Our primary results are regression-adjusted for race and ethnicity, disability status, and personal characteristics. They are unweighted. The weights for the full HRS 2020 sample had not been released at the time of our analysis. Because the HRS weights are based primarily on descriptive characteristics similar to the characteristics we adjusted for, our regression-adjusted results would be very similar to the results from a weighted analysis (Heeringa et al., 2017). Although we do not have weights for the full sample, the HRS released preliminary weights for the nationally representative early-release sample. We applied these weights in sensitivity analyses. Results remain unchanged with the addition of weights.
Methods
Individual-Level Analysis
We present descriptive statistics summarizing self-reported COVID-19 effects on work, financial issues, receipt of first round of stimulus payment, and health experiences for older adults by race or ethnicity and disabling conditions. We first compared the characteristics of our sample by disabling condition and race or ethnicity, using t-tests for binary and continuous outcomes and Chi-squared tests for categorical outcomes (we focus discussion on differences by disabling condition). We then estimated logistic regression and linear regression models to assess the differences in outcomes between those with and without disabling conditions, controlling for personal characteristics. We estimated models among all older adults and separately within each race or ethnicity category. We conducted a variety of sensitivity analyses to determine how our results would change if we altered our chosen disability definition, weights, or covariates.
Area-Level Analysis
We first compared the area-level contextual factors of our sample by race or ethnicity and disabling condition. We used t-tests to compare characteristics of older adults with and without disabling conditions. We then used multilevel modeling techniques to assess whether contextual factors might be associated with the differences between self-reported COVID-19 effects among those with disabling conditions and those without disabling conditions and by race and ethnicity. We focused our area-level analysis on the three primary COVID-19-related outcomes in our previous analysis: (1) health care delays, (2) financial hardship, and (3) effects on work. We used the full analytical sample in which geocoded information was available and standardized all area-level factors and control variables.
To test the potential association of area-level factors with individual COVID-19 experience, we employed three models. Our first model was an unadjusted multilevel model with a random slope for county. Our second model built on this first model by adjusting for the same individual-level control variables used in previous analysis. Finally, our third model added interaction terms between the county- or state-level factor and race and disability status. The addition of the interaction terms enabled us to ascertain whether area-level factors are associated with individual COVID outcomes differently for individuals of different racial and ethnic identities and for adults with or without disabling conditions.
For each of our three COVID outcomes, we ran a separate set of multilevel models testing each of our nine area-level measures separately. As such, we ran 27 multilevel models for each outcome: three models for each of the eight county-level factors, and three models for the state-level measure. This resulted in a total of 81 models. All models are unweighted because the HRS does not produce weights for the geocoded subsample that are nationally representative. Models using the four alternative definitions of disability are available upon request; model results are very similar across all disability definitions.
Results
Almost 40% of older adults in our sample required assistance with an ADL or IADL (Table 2). On average, respondents had 2.3 health conditions out of the eight conditions we examined. Hispanic and Black respondents had higher rates of disability and were also younger, on average, than White respondents. White respondents were the oldest on average and were least likely to be working. The differences in distributions of each of these characteristics across race and ethnicity were statistically significant.
Table 2.
Characteristics of Older Adults by Race, Ethnicity, and Disabling Condition (ADLs or IADLs).
| All Older Adults | Disabling Condition | No Disabling Condition | T-test a | Non-Hispanic White | Non-Hispanic Black | Hispanic or Latino | Non-Hispanic other | Chi-Square a | |
|---|---|---|---|---|---|---|---|---|---|
| Unweighted number | 8828 | 3497 | 5331 | 4781 | 2010 | 1553 | 428 | ||
| Percentage | 100.0 | 39.6 | 60.4 | 54.7 | 22.8 | 4.9 | 17.6 | ||
| ADL/IADL | 39.6 | – | – | – | 35.7 | 44.6 | 38.8 | 46.2 | ### |
| Work-limiting condition | 39.8 | – | – | – | 40.9 | 41.1 | 36.7 | 36.0 | ### |
| SSI/DI receipt | 13.0 | – | – | – | 9.1 | 22.7 | 12.9 | 12.5 | ### |
| Female | 59.6 | 62.1 | 58.0 | *** | 58.7 | 63.4 | 56.3 | 59.2 | ### |
| Age (mean) | 66.7 | 69.0 | 65.1 | *** | 69.1 | 64.0 | 62.0 | 64.1 | ### |
| Married or partnered | 60.4 | 51.5 | 66.2 | *** | 64.1 | 45.9 | 63.4 | 65.9 | ### |
| Years of education (mean) | 12.9 | 12.1 | 13.5 | *** | 13.7 | 12.9 | 13.6 | 10.3 | ### |
| Number of health conditions (mean) | 2.3 | 3.1 | 1.8 | *** | 2.3 | 2.4 | 2.1 | 2.1 | ### |
| Working for pay in 2020 | 35.2 | 18.3 | 46.2 | *** | 31.8 | 37.4 | 46.5 | 38.5 | ### |
at test significance at p < 0.05 is shown in each applicable row using *. Chi-square significance is shown using #. * Indicates p < .10, ** indicates p < .05, and *** indicates p < .01. Blank columns indicate a p-value that is not significant at the p < .10 level. We use an F-test for continuous variables rather than a Chi-square test.
ADL = activity of daily living; DI = Disability insurance; IADL = instrumental activity of daily living; SSI = Supplemental Security income
What Were the Negative Health, Work, and Financial Experiences of Older Adults with Disabilities?
COVID Testing
About 4% of older adults with disabilities reported that they had received a positive COVID diagnosis, compared with 3% of those without disabilities (Table 3). A higher share of older adults with disabling conditions reported that they had been tested for COVID (35 vs. 30%).
Table 3.
Self-Reported Health, Work, and Financial Experiences During the COVID-19 Pandemic by Disabling Condition and Race or Ethnicity.
| All Older Adults | ADL or IADL | No ADL or IADL | T-test a | Non-Hispanic White | Non-Hispanic Black | Hispanic or Latino | Non-Hispanic other | Chi-Square a | |
|---|---|---|---|---|---|---|---|---|---|
| Unweighted number | 8828 | 3497 | 5331 | 4781 | 2010 | 1553 | 428 | ||
| Health outcomes (%) | |||||||||
| Ever received a COVID diagnosis | ### | ### | |||||||
| Yes | 3.5 | 4.0 | 3.2 | 2.6 | 3.3 | 6.2 | 5.6 | ||
| Probably yes | 0.6 | 0.5 | 0.6 | 0.8 | 1.7 | 1.3 | 2.6 | ||
| Probably no | 0.7 | 0.8 | 0.6 | 0.9 | 0.6 | 1.6 | 3.7 | ||
| No | 95.3 | 94.7 | 95.6 | 95.7 | 95.9 | 93.3 | 92.4 | ||
| Ever tested | 32.3 | 35.1 | 30.4 | *** | 27.4 | 40.6 | 35.7 | 33.6 | ### |
| If tested, any positive results | 9.9 | 10.0 | 9.8 | 8.0 | 8.3 | 16.4 | 14.4 | ### | |
| If positive diagnosis, | 15.5 | 16.8 | 14.8 | 11.1 | 23.9 | 21.0 | – | ### | |
| hospitalization | |||||||||
| Delayed any type of health care | 30.7 | 36.3 | 27.2 | *** | 31.1 | 30.5 | 28.8 | 33.7 | ### |
| Delayed surgery | 13.1 | 15.9 | 10.5 | *** | 13.7 | 12.5 | 12.1 | 13.9 | ### |
| Delayed doctor visit | 57.2 | 58.5 | 56.2 | 56.2 | 55.2 | 62.9 | 56.2 | ### | |
| Delayed filling a prescription | 7.3 | 9.4 | 5.2 | *** | 5.0 | 9.6 | 11.9 | 10.3 | ### |
| Delayed dental care | 72.2 | 70.8 | 73.6 | 74.0 | 67.9 | 71.0 | 76.8 | ### | |
| Delayed other health care | 22.7 | 27.2 | 19.0 | *** | 22.6 | 19.4 | 26.3 | 26.8 | ### |
| Reasons for delaying care | |||||||||
| Could not afford it | 14.5 | 17.3 | 11.8 | *** | 12.0 | 19.4 | 14.5 | 19.0 | ### |
| Could not get an appointment | 15.7 | 16.8 | 14.8 | 15.6 | 15.4 | 16.1 | 16.2 | ||
| The clinic/hospital/doctor’s office canceled, closed, or suggested rescheduling | 51.8 | 47.1 | 55.6 | *** | 55.1 | 49.3 | 44.8 | 50.7 | ### |
| Decided it could wait | 33.3 | 30.6 | 35.4 | ** | 35.7 | 28.4 | 32.2 | 36.6 | ### |
| Was afraid to go | 23.9 | 23.9 | 23.9 | 21.7 | 24.4 | 30.6 | 24.2 | ### | |
| Work outcomes (%) | |||||||||
| Work affected because of the pandemic | ### | ### | |||||||
| Yes | 28.7 | 24.1 | 30.9 | 26.3 | 29.5 | 32.3 | 37.9 | ||
| No | 45.6 | 44.5 | 46.4 | 47.5 | 47.8 | 38.6 | 39.0 | ||
| Not working when pandemic started | 25.7 | 30.3 | 22.1 | 26.2 | 22.7 | 29.3 | 24.3 | ||
| Work affected because of the pandemic (among those working) | 38.6 | 35.5 | 40.0 | *** | 35.6 | 38.2 | 45.6 | 49.1 | ### |
| Stopped work entirely | 43.6 | 51.4 | 41.1 | *** | 34.5 | 52.7 | 58.7 | 35.5 | ### |
| Reason for work ending | |||||||||
| Lost job/laid off permanently | 14.0 | 16.5 | 13.0 | 12.6 | 16.4 | 14.2 | 23.1 | ||
| Furloughed/laid off temporarily | 48.8 | 42.9 | 51.5 | 50.0 | 49.8 | 46.5 | 46.0 | ||
| Quit | 6.1 | 6.7 | 5.8 | 3.7 | 6.9 | 9.0 | 17.4 | # | |
| Changed work days or hours | 27.8 | 29.2 | 27.4 | 24.5 | 28.8 | 35.8 | 33.7 | ### | |
| Work became more risky or dangerous | 20.8 | 25.2 | 19.7 | * | 17.8 | 27.9 | 23.0 | 26.0 | |
| Work became harder | 21.4 | 25.6 | 20.5 | * | 22.2 | 21.5 | 17.3 | 24.5 | |
| Switched to working remotely | 46.5 | 43.0 | 47.3 | 50.8 | 43.8 | 33.0 | 55.8 | ### | |
| Other changes | 34.2 | 30.1 | 35.2 | 34.8 | 30.1 | 37.6 | 33.7 | ### | |
| Financial outcomes (%) | |||||||||
| Missed rent or mortgage payments | 5.5 | 7.6 | 4.2 | *** | 1.9 | 10.3 | 9.3 | 8.1 | ### |
| Missed credit card or other debt payments | 6.7 | 9.3 | 5.1 | *** | 3.5 | 11.6 | 9.1 | 10.6 | ### |
| Missed other payments (such as utilities or insurance) | 7.1 | 10.3 | 5.0 | *** | 2.9 | 14.5 | 9.7 | 8.8 | ### |
| Could not pay medical bills | 6.2 | 8.7 | 4.4 | *** | 3.8 | 9.8 | 8.0 | 9.6 | ### |
| Didn’t have enough money to buy food | 8.9 | 13.1 | 5.9 | *** | 4.6 | 12.7 | 16.3 | 11.6 | ### |
| Had trouble buying food even though had money | 16.0 | 19.7 | 13.4 | *** | 13.9 | 17.4 | 19.4 | 18.5 | ### |
| No hardship | 68.6 | 60.5 | 74.0 | *** | 76.3 | 60.1 | 58.7 | 60.0 | ### |
| Other material hardship | 6.9 | 9.0 | 5.5 | *** | 6.0 | 8.1 | 7.7 | 9.2 | ### |
| Income changed because of the pandemic | ### | ### | |||||||
| Income went up | 5.1 | 5.1 | 5.2 | 5.0 | 5.9 | 4.6 | 6.0 | ||
| Income went down | 17.8 | 18.7 | 17.2 | 13.3 | 17.6 | 29.3 | 26.0 | ||
| About the same | 77.1 | 76.2 | 77.6 | 81.7 | 76.7 | 66.1 | 68.4 | ||
| Received stimulus payment in late 2020/early 2021 | 80.3 | 79.7 | 80.8 | 81.5 | 78.7 | 79.9 | 76.7 | ### | |
at test significance is shown in each applicable row using *. For categorical variables, Chi-square significance is shown in the variable heading row. Chi-square significance is shown using #. * Indicates p < .10, ** indicates p < .05, and *** indicates p < .01. Blank columns indicate a p-value that is not significant at the p < .10 level. We use an F-test for continuous variables rather than a Chi-square test
ADL = activity of daily living; IADL = instrumental activity of daily living
Health Care Delays
More people with disabilities reported delaying needed medical or dental care (36 vs. 27%). Respondents who delayed receiving needed health care were asked what type of care they delayed and could indicate multiple responses. There were differences in many of the types of care delayed between those with and without disabilities and in all of the types of care delayed by race and ethnicity. More older adults with disabilities delayed surgeries (16 vs. 11%), filling prescriptions (9 vs. 5%), or other health care (27 vs. 19%).
Reasons for Delaying Care
Older adults with disabilities were more likely than those without disabilities to report that they delayed care because they could not afford it (17 vs. 12%), and less likely to report that the doctor’s office canceled their care (47 vs. 56%) or that they decided to wait (31 vs. 35%). Hispanic or Latino older adults were most likely to report delaying a doctor visit (63%).
Stopping Work
About one-quarter (24%) of older adults with disabilities reported that their work was affected during the pandemic, and 30% were not working when the pandemic started (compared with 31 and 22% of older adults without disabilities). Even among those working, a smaller share of older adults with disabilities reported effects on their work (35 vs. 40%). Among those whose work was affected, about half of people with disabilities reported that they stopped work entirely (51 vs. 41%).
Other Work Effects
Among those whose work was affected, but who did not stop working, there were few differences between older adults with and without disabilities who reported switching to remote work or changing their work days or hours. More older adults with disabilities reported that their work became more risky or dangerous (25 vs. 20%) or their work became harder (26 vs. 21%).
Financial Hardships
Respondents were asked which types of financial hardships they experienced since the start of the pandemic. Older adults with disabilities were more likely to experience financial hardships (39 vs. 26%). For each hardship, older adults with disabilities were more likely to report hardships than older adults without disabilities. More people with disabilities compared with those without disabilities reported not having enough money to buy food (13 vs. 6%) and having trouble buying food even if they had the money (20 vs. 13%). Similarly, more older adults with disabilities reported missing credit card or other debt payments (9 vs. 5%), missing other payments (10 vs. 5%), or other material hardships (9 vs. 6%), or missing rent or mortgage payments (8 vs. 4%).
Income and Stimulus Payment
Most older adults with disabilities reported that their income stayed the same (76%), but 19% reported their income declined, and 5% reported their income increased. Most older adults reported that they received a stimulus payment (80%); there were no differences by disability.
What Was the Role of Intersectional Identities on These Outcomes?
We examined COVID outcomes both by disability within racial and ethnic categories and by race and ethnicity among those with disabilities to understand the intersectionality of these characteristics among Americans age 50 and older. Although many patterns of health, work, and financial impacts were similar, intersectional findings emerged in several areas:
COVID Testing
Although fewer White older adults were tested or diagnosed with COVID overall (Table 3), White older adults with disabilities were more likely to receive a COVID diagnoses or to be tested than those without disabilities (Table 4).
Table 4.
Self-Reported Health, Work, and Financial Experiences During the COVID-19 Pandemic by Disabling Condition Within Race or Ethnicity.
| Non-Hispanic White | Non-Hispanic Black | Hispanic or Latino | Non-Hispanic other | Chi-Square b | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ADL or IADL | No ADL or IADL | T-test a | ADL or IADL | No ADL or IADL | T-test a | ADL or IADL | No ADL or IADL | T-test a | ADL or IADL | No ADL or IADL | T-test a | ||
| Unweighted number | 1705 | 3076 | 897 | 1113 | 717 | 836 | 166 | 262 | |||||
| Health outcomes (%) | |||||||||||||
| Ever received a COVID diagnosis | ### | ## | # | ### | |||||||||
| Yes | 3.5 | 2.2 | 3.3 | 3.3 | 6.4 | 6.0 | 4.6 | 6.6 | |||||
| Probably yes | 0.9 | 0.8 | 2.2 | 1.4 | – | 1.9 | – | 3.6 | |||||
| Probably no | 1.2 | 0.7 | 0.6 | 0.6 | 3.6 | – | – | 5.5 | |||||
| No | 94.4 | 96.3 | 95.8 | 96.0 | 92.9 | 93.7 | 95.6 | 89.3 | |||||
| Ever tested | 30.4 | 25.7 | *** | 42.3 | 39.3 | 37.7 | 34.0 | 38.4 | 30.6 | ### | |||
| If tested, any positive results | 8.7 | 7.6 | 8.2 | 8.4 | 16.1 | 16.7 | 10.7 | 18.2 | ## | ||||
| If positive diagnosis, hospitalization | 13.6 | 8.7 | 17.4 | 29.3 | 16.9 | 25.7 | – | – | |||||
| Delayed any type of | 37.6 | 27.7 | *** | 34.4 | 27.5 | *** | 34.3 | 24.2 | *** | 43.2 | 28.2 | *** | ### |
| Health care | |||||||||||||
| Delayed surgery | 16.7 | 11.3 | *** | 16.3 | 7.9 | *** | 14.5 | 9.7 | 9.8 | 21.8 | |||
| Delayed doctor visit | 56.3 | 56.2 | 55.0 | 55.3 | 65.9 | 59.5 | 70.4 | 44.0 | ** | ||||
| Delayed filling a prescription | 6.7 | 3.6 | ** | 9.5 | 9.7 | 17.1 | 5.7 | *** | 14.9 | 6.5 | ### | ||
| Delayed dental care | 71.9 | 75.6 | 71.8 | 70.0 | 79.1 | 74.1 | ### | ||||||
| Delayed other health care | 25.7 | 20.4 | ** | 65.8 | 70.1 | 31.1 | 20.7 | ** | 31.4 | 22.3 | ### | ||
| Reasons for delaying care | |||||||||||||
| Could not afford it | 15.3 | 9.1 | *** | 20.3 | 18.3 | 16.7 | 12.0 | 20.5 | 17.3 | ### | |||
| Could not get an appointment | 19.3 | 13.3 | *** | 12.5 | 18.7 | * | 16.3 | 15.8 | 17.4 | 15.2 | |||
| The clinic/hospital/doctor’s office canceled, closed, or suggested rescheduling | 50.9 | 57.9 | ** | 42.9 | 55.6 | *** | 42.4 | 47.6 | 51.8 | 49.9 | |||
| Decided it could wait | 32.5 | 37.7 | * | 26.0 | 30.7 | 30.8 | 33.7 | 33.5 | 39.1 | ## | |||
| Was afraid to go | 22.0 | 21.5 | 28.1 | 20.9 | * | 25.0 | 37.4 | *** | 25.6 | 23.4 | ## | ||
| Work outcomes (%) | |||||||||||||
| Work affected because of the pandemic | ### | ### | ### | ### | ### | ||||||||
| Yes | 21.3 | 28.2 | 23.6 | 33.2 | 29.3 | 34.3 | ** | 36.1 | 38.7 | ||||
| No | 46.6 | 48.1 | 48.0 | 47.7 | 36.4 | 40.5 | 36.0 | 40.9 | |||||
| Not working when | 30.3 | 23.4 | 27.2 | 18.0 | 33.9 | 24.4 | *** | 29.0 | 20.7 | ||||
| Pandemic started | |||||||||||||
| Work affected because of the pandemic (among those working) | 31.5 | 37.1 | *** | 32.9 | 41.1 | *** | 45.5 | 45.7 | 50.8 | 48.3 | ### | ||
| Stopped work entirely | 41.4 | 32.7 | ** | 61.7 | 49.6 | ** | 63.9 | 56.5 | 31.8 | 37.0 | ### | ||
| Reason for work ending | |||||||||||||
| Lost job/laid off permanently | 13.3 | 12.4 | 17.1 | 16.1 | 20.0 | 10.9 | 6.7 | 34.5 | |||||
| Furloughed/laid off temporarily | 42.5 | 52.7 | 45.0 | 52.1 | 44.1 | 47.9 | 44.0 | 46.7 | |||||
| Quit | 3.6 | 3.7 | 7.9 | 6.3 | 7.7 | 1.0 | 38.9 | 8.9 | |||||
| Changed work days or hours | 26.5 | 24.1 | 40.1 | 26.4 | * | 30.2 | 37.7 | 16.1 | 39.4 | * | |||
| Work became more risky or dangerous | 20.7 | 17.2 | 28.7 | 27.7 | 27.4 | 21.4 | 27.5 | 25.6 | |||||
| Work became harder | 27.3 | 21.3 | 36.5 | 18.4 | ** | 22.0 | 16.0 | 10.2 | 29.7 | * | |||
| Switched to working remotely | 49.6 | 51.0 | 23.0 | 48.2 | *** | 47.8 | 28.5 | ** | 49.4 | 57.7 | ### | ||
| Other changes | 29.3 | 36.0 | 31.5 | 29.7 | 25.4 | 41.6 | * | 37.7 | 32.4 | # | |||
| Financial outcomes (%) | |||||||||||||
| Missed rent or mortgage payments | 3.0 | 1.3 | *** | 12.6 | 8.7 | ** | 12.7 | 7.1 | *** | 7.0 | 8.8 | ### | |
| Missed credit card or other debt payments | 5.6 | 2.2 | *** | 14.3 | 9.6 | *** | 11.8 | 7.4 | *** | 11.7 | 9.9 | ### | |
| Missed other payments (such as utilities or insurance) | 4.7 | 1.9 | *** | 18.8 | 11.1 | *** | 13.6 | 7.1 | *** | 11.9 | 6.5 | * | ### |
| Could not pay medical bills | 5.7 | 2.5 | *** | 13.1 | 7.2 | *** | 9.7 | 6.5 | ** | 13.4 | 6.7 | * | ### |
| Didn’t have enough money to buy food | 7.0 | 3.0 | *** | 18.4 | 8.2 | *** | 22.3 | 11.4 | *** | 13.7 | 9.9 | ### | |
| Had trouble buying food even though had money | 18.1 | 11.4 | *** | 21.1 | 14.4 | *** | 22.7 | 16.6 | *** | 17.5 | 19.2 | ### | |
| No hardship | 68.4 | 80.8 | *** | 52.5 | 66.1 | *** | 50.7 | 65.3 | *** | 55.0 | 62.9 | ### | |
| Other material hardship | 7.8 | 4.9 | *** | 10.5 | 6.2 | *** | 9.7 | 6.1 | ** | 11.4 | 7.6 | ### | |
| Income changed because of the pandemic | ### | ### | ### | ### | ### | ||||||||
| Income went up | 4.9 | 5.1 | 5.8 | 5.9 | 4.6 | 4.4 | 6.9 | 5.6 | |||||
| Income went down | 14.9 | 12.7 | 17.8 | 17.7 | 28.0 | 30.4 | 31.3 | 23.3 | |||||
| About the same | 80.3 | 82.3 | 77.1 | 76.5 | 67.2 | 65.3 | 62.3 | 71.5 | |||||
| Received stimulus payment in late 2020/early 2021 | 81.5 | 81.5 | 77.7 | 80.0 | 80.2 | 79.5 | 70.7 | 79.8 | ### | ||||
at test significance is shown in each applicable row using *. For categorical variables, Chi-square significance is shown in the variable heading row. Chi-square significance is shown using #. * Indicates p < .10, ** indicates p < .05, and *** indicates p < .01. Blank columns indicate a p-value that is not significant at the p < .10 level. We use an F-test for continuous variables rather than a Chi-square test
bChi-square value is across race or ethnicity, conditional on having one or more difficulties with ADLs or IADLs.
ADL = activity of daily living; IADL = instrumental activity of daily living
Health Care Delays
Within each race and ethnicity group, disabled older adults were more likely to delay health care. The difference was largest for older adults of another race, among whom 43% of those with disabilities delayed health care compared with 28% of those without disabilities. Among those with disabilities, there were also statistically significant differences across race and ethnicity. We compared the same 43% of older adults of another race with a disability who delayed health care to 38% of White older adults with a disability and 35% of older adults with disabilities who were Black or Hispanic or Latino.
Delaying Prescriptions
Many of the same patterns in types of health care delays by disability persisted or were exacerbated when we consider separate racial and ethnic groups. For example, 17% of Hispanic or Latino older adults with a disabling condition reported delaying prescriptions compared with 6% of those without disabilities. Among all older adults, the difference by disability was 4% points.
Stopping Work
Among those whose work was affected, there were differences in those who stopped working by disability and exacerbations by race or ethnicity. For example, 62% of Black older adults with disabilities reported stopping work, compared with 44% of all older adults, 52% of older adults with disabilities of any race, and 53% of Black older adults regardless of disability status.
Moving to Remote Work
Among all older adults whose work was affected, there was no difference by disability in those who moved to remote work (Table 3). However, Hispanic or Latino older adults with disabilities were more likely to move to remote work compared with those without disabilities (48 vs. 28%; Table 4). Conversely, Black older adults with disabilities were less likely to move to remote work compared with those without disabilities (23 vs. 48%).
Financial Hardships
The differences in older adults’ financial hardships by disability status persisted across White, Black, and Hispanic or Latino older adults. Some of the largest differences were in having enough money to buy food. Twenty-two percent of Hispanic or Latino older adults with disabilities did not have enough money to buy food, compared with 11% without disabilities. For Black older adults, 18% with disabilities did not have enough money to buy food compared with 8% without disabilities. There were similar patterns of older adults reporting that they had trouble buying food even if they had the money.
Stimulus Payments
There were no differences in stimulus receipt by disability, overall or within racial and ethnic groups. There were some differences by race or ethnicity (Table 3) that persisted among those with disabling conditions. Seventy-one percent of disabled older adults of another race received the stimulus payment (Table 4), compared with about 80% of disabled older adults who were Black (78%), Hispanic or Latino (80%), or White (81%).
Role of Contextual and Social Factors
Next, we focus on contextual factors associated with COVID-19 experiences, using the nine area-level measures described above. Table 5 describes differences in county characteristics between older adults with and without disabling condition, across our whole sample and within racial and ethnic categories. We found statistically significant differences in county-level characteristics for people with and without disabilities, across the full sample and within racial and ethnic categories. Across the full sample, adults with disabling conditions were more likely to live in counties characterized by higher levels of COVID vulnerability, lower levels of economic opportunity and health care access, and higher levels of socioeconomic vulnerability, as measured by our county-level factors. Specifically, adults with disabling conditions were more highly concentrated in counties with a higher average case counts, higher scores on the Pandemic Vulnerability and Social Vulnerability Indexes, more years of potential life lost (YPLL), and higher rates of unemployment and populations receiving government assistance. This pattern also remained consistent within race and ethnicity. When examining differences within the subgroup of respondents with disabling conditions, the observed racialized patterns persisted. Older adults with disabilities who are non-White were more clustered in counties with less favorable county characteristics, relative to people with disabilities who identify as non-Hispanic White.
Table 5.
Contextual Factors of Counties in Which Older Adults Lived by Race or Ethnicity, and Disabling Condition.
| All Older Adults | Non-Hispanic White | |||||||
|---|---|---|---|---|---|---|---|---|
| All older adults | ADL or IADL | No ADL or IADL | T-test a | All Non-Hispanic White | ADL or IADL | No ADL or IADL | T-test a | |
| Mean weighted county-level value for HRS respondents a | ||||||||
| COVID-19 risk and vulnerability | ||||||||
| Case counts (per 100,000) | 21.7 | 22.1 | 21.4 | *** | 21.5 | 21.9 | 21.2 | *** |
| Pandemic vulnerability index | 0.5 | 0.5 | 0.5 | *** | 0.5 | 0.5 | 0.5 | *** |
| Socioeconomic characteristics | ||||||||
| Social vulnerability index | .51 | .54 | .50 | *** | 0.5 | 0.5 | 0.5 | *** |
| Residential racial segregation | 33.9 | 33.7 | 34.0 | 34.1 | 33.9 | 34.1 | ||
| Medical infrastructure and health care access | ||||||||
| Hospital beds capacity | 0.4 | 0.4 | 0.4 | 0.4 | 0.4 | 0.4 | ||
| Years of potential life lost | 7760.5 | 8105.5 | 7502.2 | *** | 7644.5 | 7946.3 | 7438.3 | *** |
| Employment opportunities and income | ||||||||
| Unemployment | 5.4 | 5.4 | 5.3 | ** | 5.2 | 5.3 | 5.2 | ** |
| Percentage receiving government assistance | 12.3 | 12.7 | 12.0 | *** | 11.9 | 12.3 | 11.6 | *** |
| Number of observations | 8616 | 3408 | 5208 | 4678 | 1664 | 3014 | ||
aMeans of county-level variables are weighted to adjust for different proportions of HRS respondents across counties. A simple inverse-probability weight was created to account for county clustering across the entire sample and again for each racial/ethnic subgroup.
ADL = activity of daily living; HRS = Health and retirement Study; IADL = instrumental activity of daily living
Are Contextual Factors Associated with COVID Outcomes for People with Disabling Conditions?
Next, we examined the association of contextual factors on individual experiences with financial hardship, delaying health care, and whether one’s work was affected. The intraclass coefficient for the unadjusted model of financial hardship with county measures is .07, suggesting that clustering at the county level can explain 7% of the individual-level variation in financial hardship. However, the ICC for work being affected is .0388 and the ICC for delaying health care is .0046. These small values suggest that there might not be clustering of work effects and health care delays at the county level.
We found only two significant county-level factors on the likelihood of declaring financial hardship because of COVID-19: (1) Years of Potential Life Lost (Table 6) and (2) state political party affiliation (Table 7). We did, however, observe statistically significant positive associations with financial hardship for both disability and with race or ethnicity across all models for all county-level factors, suggesting that an individual’s disability status and race or ethnicity remain positive predictors of financial hardship due to COVID-19 even after accounting for contextual factors. Results for all models estimating associations of area-level factors with financial hardship, health care, and work can be found in the Supplemental Materials (Tables S1–S8).
Table 6.
Association Between Area-Level Years of Potential Life Lost and Self-Reported Health, Work, and Financial Experiences During the COVID-19 Pandemic.
| Years of Potential Life Lost (YPLL) | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Finance | Health Care Delays | Work | ||||||||||||||||
| Model 0 | Model 1 | Model 2 | Model 0 | Model 1 | Model 2 | Model 0 | Model 1 | Model 2 | ||||||||||
| YPPL | 1.08 | *** | 1.05 | * | 1.13 | *** | 0.9 | *** | 0.9 | ** | 0.9 | *** | 0.8 | *** | 0.9 | *** | 0.9 | * |
| Disability | 1.95 | *** | 1.90 | *** | 1.90 | *** | 1.4 | *** | 1.6 | *** | 1.6 | *** | 0.4 | *** | 0.7 | *** | 0.7 | *** |
| Race | ||||||||||||||||||
| Black | 2.00 | *** | 1.49 | *** | 1.53 | *** | 1.0 | 0.8 | *** | 0.8 | *** | 1.3 | *** | 0.9 | 0.9 | |||
| Other | 2.14 | *** | 1.61 | *** | 1.59 | *** | 1.1 | 0.9 | 0.8 | 1.5 | *** | 0.8 | 0.8 | |||||
| Hispanic | 2.25 | *** | 1.69 | *** | 1.66 | *** | 0.8 | *** | 0.7 | *** | 0.8 | ** | 1.4 | *** | 1.1 | 1.1 | ||
| YPPL* Disability |
N/A | N/A | 1.0 | N/A | N/A | 1.0 | N/A | N/A | 0.9 | ** | ||||||||
| YPPL*Black | N/A | N/A | 0.9 | ** | N/A | N/A | 1.1 | N/A | N/A | 1.1 | ||||||||
| YPPL*Other | N/A | N/A | 0.8 | * | N/A | N/A | 1.0 | N/A | N/A | 1.0 | ||||||||
| YPPL* Hispanic | N/A | N/A | 0.9 | N/A | N/A | 1.3 | ** | N/A | N/A | 0.9 | ||||||||
| Individual covariates | Yes | Yes | Yes | Yes | Yes | Yes | ||||||||||||
| Interaction terms | Yes | Yes | Yes | |||||||||||||||
| N | 8473 | 8456 | 8456 | 8475 | 8457 | 8457 | 8503 | 8477 | 8477 | |||||||||
| Number of counties | 772 | 769 | 769 | 770 | 767 | 767 | 772 | 768 | 768 | |||||||||
| AIC | 10,034.2 | 9677.9 | 9678.8 | 10,394.5 | 10,023.9 | 10,024.7 | 9710.2 | 8309.4 | 8311.0 | |||||||||
| BIC | 10,083.5 | 9846.9 | 9876.0 | 10,443.8 | 10,185.9 | 10,214.8 | 9759.6 | 8471.4 | 8501.2 | |||||||||
Notes: * Indicates p < .10, ** indicates p < .05, and *** indicates p < .01. N/A = not applicable
Table 7.
Association Between Political Party of State and Self-Reported Health, Work, and Financial Experiences During COVID-19 Pandemic.
| Republican Control of State (RCS) | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Finance | Health Care Delays | Work | ||||||||||||||||
| Model 0 | Model 1 | Model 2 | Model 0 | Model 1 | Model 2 | Model 0 | Model 1 | Model 2 | ||||||||||
| RCS | 1.2 | ** | 1.2 | ** | 1.2 | ** | 0.8 | *** | 0.8 | *** | 0.7 | *** | 0.9 | ** | 1.0 | 0.9 | ||
| Disability | 1.9 | *** | 1.9 | *** | 2.0 | *** | 1.4 | *** | 1.6 | *** | 1.6 | *** | 0.4 | *** | 0.7 | *** | 0.7 | *** |
| Race | ||||||||||||||||||
| Black | 2.1 | *** | 1.5 | *** | 1.5 | *** | 0.9 | 0.8 | *** | 0.7 | *** | 1.3 | *** | 0.9 | 0.9 | |||
| Other | 2.1 | *** | 1.6 | *** | 1.5 | *** | 1.1 | 0.9 | 0.8 | 1.6 | *** | 0.8 | 0.9 | |||||
| Hispanic | 2.2 | *** | 1.6 | *** | 1.7 | *** | 0.8 | ** | 0.8 | *** | 0.7 | *** | 1.4 | *** | 1.1 | 1.0 | ||
| RCS* Disability | N/A | N/A | 0.9 | N/A | N/A | 1.0 | N/A | N/A | 1.0 | |||||||||
| RCS*Black | N/A | N/A | 1.0 | N/A | N/A | 1.2 | * | N/A | N/A | 1.2 | ||||||||
| RCS*Other | N/A | N/A | 1.1 | N/A | N/A | 1.2 | N/A | N/A | 0.9 | |||||||||
| RCS*Hispanic | N/A | N/A | 1.0 | N/A | N/A | 1.5 | *** | N/A | N/A | 1.3 | ||||||||
| Individual covariates | Yes | Yes | Yes | Yes | Yes | Yes | ||||||||||||
| Interaction terms | Yes | Yes | Yes | |||||||||||||||
| N | 8416 | 8400 | 8400 | 8419 | 8402 | 8402 | 8447 | 8422 | 8422 | |||||||||
| Number of states | 47 | 47 | 47 | 47 | 47 | 47 | 47 | 47 | 47 | |||||||||
| AIC | 9999.8 | 9635.1 | 9640.9 | 10,322.0 | 9955.6 | 9956.7 | 9727.4 | 8269.2 | 8274.4 | |||||||||
| BIC | 10,049.1 | 9804.0 | 9837.9 | 10,364.2 | 10,117.4 | 10,153.8 | 9776.7 | 8431.1 | 8464.4 | |||||||||
Notes: * Indicates p < .10, ** indicates p < .05, and *** indicates p < .01. N/A = not applicable.
Focusing on the set of models with statistically significant relationships, we first describe the set of models examining the role of YPLL. YPLL measures premature mortality in a county by counting the years of life lost before age 75, thus focusing on preventable deaths. This measure captures elements associated with social determinants of health and area-level health behaviors such as smoking and accidents. The main effects on YPLL, disability, and race or ethnicity are all greater than one and statistically significant. There is a statistically significant association for the interaction between YPLL and both non-Hispanic Black persons and persons of non-Hispanic other races.
Focusing on the state-level model of political party (Table 7), we found that older adults were more likely to report a financial hardship in a state with a republican-controlled government (OR = 1.2). As with the county-level models, the main effects on disability and race or ethnicity remain positive and statistically significant. In addition, we observed an association between delayed health care and political party wherein individuals in republican-controlled states are less likely to report delaying health care (OR = .7).
We do not see a consistent pattern of association between county-level contextual factors and individual experiences with delayed health care or work being affected.
Discussion
We found evidence of negative COVID-19 effects on health, work, and financial experiences for older adults with disabilities. This group was more negatively impacted on several measures compared with those without disabilities. In addition, we found evidence of intersectionality: older adults with disabilities who were Black or Hispanic often had disparate impacts compared with either those without disabilities or White older adults with disabilities.
Most notably, older adults with disabilities were more likely to report experiencing financial hardships than older adults without disabilities and these differences were exacerbated especially among Black and Hispanic or Latino older adults. Overall, about one-third of older adults reported financial hardships since the start of the pandemic. Although there was no difference by disabling condition in the receipt of stimulus payments, older adults with disabling conditions were more likely to experience each of the financial hardships examined. There were also large differences at the intersection of race or ethnicity and disabling condition; for example, 49% of Hispanic or Latino older adults with disabilities reported financial hardships, compared with 19% of White older adults without disabilities and 32% of those with disabilities.
Older adults with disabilities also reported negative impacts on health care delays and work. They were also more likely than older adults without disabilities to report delaying many types of health care, such as surgeries and prescriptions, since March 2020. Among older adults whose work was impacted by the pandemic, more older adults with disabilities reported stopping work than older adults without disabilities, and fewer moved to remote work.
Although few contextual factors were associated with these negative COVID outcomes, we found evidence that contextual factors mattered. First, there were important differences in county-level characteristics for people with and without disabilities, across the full sample and within race or ethnicity. Moreover, older adults with disabilities who are Hispanic, Black, or another race other than White tend to live in counties that performed poorly on measures of several county-level factors relative to people with disabilities who identify as non-Hispanic White. We did not see a consistent pattern of association between county-level contextual factors and individual experiences with delayed health care or work being affected. For financial outcomes, only YPLL and political party are significant and in the expected direction. These findings reveal that people with disabilities tend to be more highly concentrated in areas that are more susceptible to COVID and other socioeconomic inequalities. However, these contexts do not appear to influence their COVID outcomes beyond respondents’ individual identities and experiences.
The data and findings have two key limitations. First, the negative COVID experiences are self-reported and subject to potential biases. For example, because the survey was fielded over about a year, some respondents were answering questions about the impacts of COVID very early during shutdowns while others had a longer period of time to experience negative impacts. Thus, early respondents might not yet have experienced the negative effects that they would eventually experience, and later respondents might have forgotten or misreported experiences from nearly a year earlier. However, the timing of interviews is plausibly random with respect to whether someone has a disabling condition (measured in 2018) and with respect to their race or ethnicity. Second, we cannot determine a causal link between disability, race, or ethnicity on pandemic-related outcomes. Some questions were phrased to inquire about the “effects” of COVID-19, while others focused on experiences since March 2020. However, it is likely that older adults with disabilities had more financial hardships, barriers to health care, and difficulty accessing work before the pandemic. Indeed, there is a great deal of literature documenting many such difficulties. This study thus provides descriptive evidence of the disparities experienced in approximately the first year of the pandemic, but causation cannot be determined.
The findings highlight key takeaways. First, the pandemic had disparate impacts on older adults and people with disabilities, especially those who were Black and Hispanic, and the vulnerability of this community suggests future public health events might impact them similarly. Resources could be put into understanding particular needs to better support the well-being of people with disabilities. These results are intended to provide a descriptive overview of the myriad impacts the pandemic has had on people with disabilities; future work can and should attempt to better elucidate the mechanisms that may be contributing to these disparities.
Second, these findings underscore the importance of using an intersectionality approach to understanding disparities in outcomes within and across populations. Consistent with intersectionality theory (Crenshaw, 1989), we find that older adults with intersecting identities of disability and historically marginalized race or ethnicity were more likely to have been negatively impacted by the pandemic. Indeed, our results support the notion that multiple and coexisting dimensions of marginalization or inequality, in this case race, ethnicity, and disability status, may have overlapping and cumulative effects beyond the sum of their individual parts. When considering impacts separately by race or ethnicity, or by disability, the extent of hardships experienced at the intersection of these identities is hidden; the finding that more people with multiple marginalized identities faced difficulties highlights that continued study of this intersection should lead to policies better aimed at alleviating hardship. Due to the small sample, we were unable to examine subpopulations by type (mental or physical) or timing of disability (such as those with newly acquired disability), but future research with an intersectionality lens might seek to identify groups with more vulnerabilities in need of stronger policy responses.
Finally, policies mitigating financial impacts could be universally beneficial. Financial impacts were widespread across every demographic group, despite pandemic-specific policies enacted to provide financial support. For example, although most older adults received a stimulus payment, about a third still experienced financial hardships. Likewise, even though eligibility for the Supplemental Nutrition Assistance Program was extended, 13% of older adults with disabilities and 22% of Hispanic older adults with disabilities reported not having enough money to buy food. Especially for older adults who have reached retirement age, additional financial support might be necessary to mitigate hardships.
We invite future research to expand upon this work and to continue to explore the effects of the pandemic on people with disabilities through an intersectionality lens. While this manuscript gives a sense of the impacts of the pandemic that older adults with disabilities experienced, we hope it lays the foundation for future work that considers the potential mechanisms that may explain why people with disabilities had more negative experiences than people without disabilities, and why the differences were larger for older adults with disabilities who were Black or Hispanic. Potential mechanisms may include access to services, characteristics of employment, and household-level characteristics.
Supplemental Material
Supplemental Material for Racial Disparities in COVID-19 Experiences Among Older Adults With Disabling Conditions by Marisa Shenk, Bernadette Hicks, Ana Quiñones, and Amal Harrati in Journal of Aging and Health.
Notes
We merged the 2020 HRS data to the RAND files using the household and respondent identification numbers.
The 2020 HRS was fielded between March 2020 and June 2021 and included 15,732 participants. The COVID-19 module was added in May 2020. Between June 11, 2020 and October 2020, a random 25% subset of the HRS sample was surveyed with the COVID-19 module. From September 2020 to May 2021, another random 25% subset of the HRS sample was surveyed with the COVID-19 module. In January 2022, the data from the 2020 HRS was released without weights.
The early-release sample is a random 25% subset of the HRS sample that was surveyed with the COVID-19 module. The data from this nationally representative subsample was released in November 2020 with preliminary weights. We used this early-release sample and its corresponding weights as part of our sensitivity analysis.
We could not match 1466 participants to the HRS 2018 data. These participants might have been newly added to the HRS (such as a new spouse of an existing participant) or included in prior years but did not complete the 2018 survey. We excluded these participants because we measured disability and work status through 2018 for everyone in the analysis. We measured these variables through 2018 rather than 2020 because of the potential relationship between COVID and disability and work in 2020. For example, respondents could have developed disabling conditions because of COVID, and we can’t disentangle that effect. Our estimates are therefore likely undercounting the share of people with disabilities, which could make our effect sizes appear smaller than the actual differences in COVID impacts between people with and without these disabling conditions.
This measure comes from the RAND file. The eight long-term health conditions included high blood pressure, diabetes, cancer, lung disease, heart disease, stroke, psychiatric problems, and arthritis.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study is supported by U.S. Social Security Administration
Supplemental Material: Supplemental Material for this article is available online.
ORCID iD
Amal Harrati https://orcid.org/0000-0002-3940-725X
References
- Abrams D., Lalot F., Hogg M. A. (2021). Intergroup and intragroup dimensions of COVID-19: A social identity perspective on social fragmentation and unity. Group Processes & Intergroup Relations, 24(2), 201–209. 10.1177/1368430220983440 [DOI] [Google Scholar]
- Andersen L. M., Harden S. R., Sugg M. M., Runkle J. D., Lundquist T. E. (2021). Analyzing the spatial determinants of local Covid-19 transmission in the United States. Science of the Total Environment, 754(10144), 142396. 10.1016/j.scitotenv.2020.142396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage R., Nellums L. B. (2020). The COVID-19 response must be disability inclusive. Atlantic monthly group. 2021. The COVID racial data tracker. The Lancet Public Health, 5(5), e257. Accessed June 17, 2020.https://covidtracking.com/race [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum C. F., Henry M. (2020). Socioeconomic factors influencing the spatial spread of COVID-19 in the United States. Miguel, Socioeconomic Factors Influencing the Spatial Spread of COVID-19 in the United States. (May 29, 2020) https://ssrn.com/abstract=3614877. or. 10.2139/ssrn.3614877 [DOI] [Google Scholar]
- Bowleg L. (2020). We’re not all in this together: On COVID-19, intersectionality, and structural inequality. American journal of public health, 110(7), 917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics (2020. a). Labor force statistics from the current population survey: Supplemental data measuring the effects of the coronavirus (COVID-19) pandemic on the labor market. https://www.bls.gov/cps/effects-of-the-coronavirus-COVID-19-pandemic.htm#highlights_Oct_2020
- Bureau of Labor Statistics (2020. b). Persons with a disability: Labor force characteristics—2019. https://www.bls.gov/news.release/archives/disabl_02262020.htm
- Bureau of Labor Statistics (2021). Persons with a disability: Labor force characteristics—2020. https://www.bls.gov/news.release/disabl.nr0.htm [Google Scholar]
- Centers for Disease Control and Prevention (Cdc) (2021). COVID-19 recommendations for older adults. (Accessed August 2022).https://www.cdc.gov/aging/covid19/covid19-older-adults.html
- Chakraborty J. (2021). Social inequities in the distribution of COVID-19: An intra-categorical analysis of people with disabilities in the US. Disability and Health Journal, 14(1), 101007. 10.1016/j.dhjo.2020.101007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi S. L., Carr D., Namkung E. H. (2022). Physical disability and older adults’ perceived food and economic insecurity during the COVID-19 pandemic. The Journals of Gerontology: Series B, 77(7), e123–e133. 10.1093/geronb/gbab162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtney-Long E. A., Romano S. D., Carroll D. D., Fox M. H. (2017). Socioeconomic factors at the intersection of race and ethnicity influencing health risks for people with disabilities. Journal of Racial and Ethnic Health Disparities, 4, 213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K. (1989). Demarginalizing the intersection of race and sex: A black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics (p. 139). u. Chi. Legal f. [Google Scholar]
- Davis O. (2021) Employment and retirement among older workers during the COVID-19 pandemic. Schwartz Center for Economic Policy Analysis and Department of Economics, The New School for Social Research, Working Paper Series. 6, 1–36 [Google Scholar]
- Dixon-Ibarra A., Horner-Johnson W. (2014). Peer reviewed: Disability status as an antecedent to chronic conditions: National health interview survey, 2006–2012. Preventing Chronic Disease. 11(2014), E15. 10.5888/pcd11.130251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauthier G. R., Smith J. A., García C., Garcia M. A., Thomas P. A. (2021). Exacerbating inequalities: Social networks, racial/ethnic disparities, and the COVID-19 pandemic in the United States. The Journals of Gerontology: Series B, 76(3), e88–e92. 10.1093/geronb/gbaa117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gleason J., Ross W., Fossi A., Blonsky H., Tobias J., Stephens M. (2021). The devastating impact of Covid-19 on individuals with intellectual disabilities in the United States. NEJM Catalyst Innovations in Care Delivery, 2(2), 1–2. 10.1056/CAT.21.0051 [DOI] [Google Scholar]
- Gobbens R. J. (2018). Associations of ADL and IADL disability with physical and mental dimensions of quality of life in people aged 75 years and older. PeerJ, 6(e5425), e5425. 10.7717/peerj.5425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elnaiem A. D. (2021). Intersectionality in the time of COVID-19: dispatches from a contact tracer. American journal of public health, 111(1), 93–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatef E., Chang H. Y., Kitchen C., Weiner J. P., Kharrazi H. (2020). Assessing the impact of neighborhood socioeconomic characteristics on COVID-19 prevalence across seven states in the United States. Frontiers in Public Health, 8, 571808. 10.3389/fpubh.2020.571808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Retirement Study . (2021). 2020 HRS COVID-19 project, early version 1.0. https://hrsdata.isr.umich.edu/sites/default/files/documentation/data-descriptions/1613082944/2020COVID_DD_Feb2021.pdf
- Healthy People 2030 . U.S. Department of health and human services, office of disease prevention and health promotion. Retrieved [date graphic was accessed], from:https://health.gov/healthypeople/objectives-and-data/social-determinants-health. Last accessed June 28, 2023
- Heeringa S. G., West B. T., Berglund P. A. (2017). Applied survey data analysis. chapman and hall/CRC. [Google Scholar]
- Jashinsky T. L., King C. L., Kwiat N. M., Henry B. L., Lockett‐Glover A. (2021). Disability and COVID‐19: Impact on workers, intersectionality with race, and inclusion strategies. The Career Development Quarterly, 69(4), 313–325. 10.1002/cdq.12276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby T. (2020). Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities. The Lancet Respiratory Medicine, 8(6), 547–548. 10.1016/S2213-2600(20)30228-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebrasseur A., Fortin-Bédard N., Lettre J., Bussières E. L., Best K., Boucher N., Routhier F. (2021). Impact of COVID-19 on people with physical disabilities: A rapid review. Disability and Health Journal, 14(1), 101014. 10.1016/j.dhjo.2020.101014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez M. H., Rainie L., Budiman A. (2020). Financial and health impacts of COVID-19 vary widely by race and ethnicity. [Google Scholar]
- Mauldin L., Brown R. L. (2021). Missing pieces: Engaging sociology of disability in medical sociology. Journal of Health and Social Behavior, 62(4), 477–492. 10.1177/00221465211019358 [DOI] [PubMed] [Google Scholar]
- McConkey R., Keogh F., Bunting B., Garcia Iriarte E., Watson S. F. (2016). Relocating people with intellectual disability to new accommodation and support settings: Contrasts between personalized arrangements and group home placements. Journal of Intellectual Disabilities, 20(2), 109–120. 10.1177/1744629515624639 [DOI] [PubMed] [Google Scholar]
- Millán-Calenti J. C., Tubío J., Pita-Fernández S., González-Abraldes I., Lorenzo T., Fernández-Arruty T., Maseda A. (2010). Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Archives of Gerontology and Geriatrics, 50(3), 306–310. 10.1016/j.archger.2009.04.017 [DOI] [PubMed] [Google Scholar]
- Morris Z. A. (2022). Understanding the increased financial hardship experienced by older adults with disabilities during the COVID-19 pandemic. Center for Retirement Research at Boston College. Working Paper 2022-9. [Google Scholar]
- Oppel R. A., Robert Gebeloff K. K., Rebecc L., Wright W., Smith M. (2020). The fullest look yet at the racial inequity of coronavirus. The New York Times. Accessed February 18, 2022.https://www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html [Google Scholar]
- Polyakova M., Udalova V., Kocks G., Genadek K., Finlay K., Finkelstein A. N. (2021). Racial Disparities in Excess All-Cause Mortality during the Early COVID-19 Pandemic Varied Substantially across States: Study examines the geographic variation in excess all-cause mortality by race to better understand the impact of the COVID-19 pandemic. Health Affairs, 40(2), 307–316. 10.1377/hlthaff.2020.02142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price-Haywood E. G., Burton J., Fort D., Seoane L. (2020). Hospitalization and mortality among black patients and white patients with Covid-19. New England Journal of Medicine, 382(26), 2534–2543. 10.1056/NEJMsa2011686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinby L., Rutledge M. S., Wettstein G. (2021). How has COVID-19 affected the labor force participation of older workers? Center for Retirement Research at Boston College, CRR WP 2021-13. [Google Scholar]
- Schnake-Mahl A. S., Bilal U. (2021). Person, place, time and COVID-19 inequities. American Journal of Epidemiology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnega A., Faul J. D., Ofstedal M. B., Langa K. M., Phillips J. W., Weir D. R. (2014). Cohort profile: The health and retirement study (HRS). International Journal of Epidemiology, 43(2), 576–585. 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spector W. D., Fleishman J. A. (1998). Combining activities of daily living with instrumental activities of daily living to measure functional disability. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 53(1), S46–S57. https://doi.otg/10.1093/geronb/53b.1.s46 [DOI] [PubMed] [Google Scholar]
- Stevens A., Courtney-Long E., Gillespie C., Armour B. S. (2014). Peer reviewed: Hypertension among US adults by disability status and type, national health and nutrition examination survey, 2001–2010. Preventing Chronic Disease, 11(8), E139. 10.5888/pcd11.140162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trout L. J., Kleinman A. (2020). Covid-19 requires a social medicine response. Frontiers in Sociology, 5, 579991. 10.3389/fsoc.2020.579991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walubita T., Beccia A., Boama-Nyarko E., Goulding M., Herbert C., Kloppenburg J., Mabry G., Masters G., McCullers A., Forrester S. (2021). Aging and COVID-19 in minority populations: A perfect storm. Current Epidemiology Reports, 8, 63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D. X., Yao J., Zirek Y., Reijnierse E. M., Maier A. B. (2020). Muscle mass, strength, and physical performance predicting activities of daily living: A meta‐analysis. Journal of Cachexia, Sarcopenia and Muscle, 11(1), 3–25. 10.1002/jcsm.12502 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Racial Disparities in COVID-19 Experiences Among Older Adults With Disabling Conditions by Marisa Shenk, Bernadette Hicks, Ana Quiñones, and Amal Harrati in Journal of Aging and Health.