ABSTRACT
BACKGROUND:
The purpose of the study was to compare the functional and radiological results of the conservatively and surgically treated displaced acetabular fractured patients.
METHODS:
The study included 61 patients with a displaced acetabulum fracture over the age of 18, who have been treated conservatively or surgically for acetabular fractures, between 2000 and 2014. Patients were divided into two groups according to their treatment type. Group 1 consisted of conservatively treated 31 between 2000 and 2010 patients and Group 2 consisted of surgically treated 30 patients between 2010 and 2014. The fractures were classified according to Judet and Letournel classification. Clinical evaluation of the patients was conducted according to Modified Merle D’Aubigne Score, SF-36, and Harris Hip Score. Radiological evaluation was evaluated according to Matta’s Radiological Evaluation Criteria. Kolmogorov–Smirnov, t-test, Mann–Whitney U-test, and two Wilcoxon paired sample tests were used for statistical analysis. The significance limit was chosen as p<0.05.
RESULTS:
The mean follow-up time was 10 years for the conservative group and 5.5 years for the surgery group. There was no statistically significant difference in functional scores between both groups (p>0.05), Matta’s radiological staging score was significantly higher in the operated group (p=0.023).
CONCLUSION:
Radiological scores are not directly correlated with the functional capacity. We obtained good radiological and functional scores in the surgical group, operative treatment should be considered when absolute indications are there. The outcome of conservatively managed fractures is not bleak. We think that there is an alternative to surgical treatment in displaced acetabular fractures and that similar functional results can be obtained in selected cases.
Keywords: Acetabulum fracture, conservative treatment, surgical treatment
INTRODUCTION
Acetabular fractures are usually the result of high energy trauma.[1] As in all intra-articular fractures, the aim of treatment is to provide anatomical reduction in a stable manner. Gaining full range of motion and joint function, as soon as possible, should be the expected result of the treatment modality. Due to the complexity of anatomical structures in the surgical field, comorbidities of the patient, and the need of surgical experience of the surgical team, conservative treatment modalities can still be used in displaced acetabular fractures.
The anatomic complexity of the acetabulum and pelvis, along with the difficulty of accurately defining and classifying the fracture pattern, makes treatment decisions even more challenging.[2] Advances in diagnostic tools enable us to define fracture configuration in more detail, and currently, displaced intra-articular fractures should be treated surgically with anatomic reduction and stable fixation.[3,4] We observe good functional and radiological results after surgical treatment of acetabular fractures, but there is limited knowledge about the results of conservatively treated patients and there is a lack of follow-up about the functional capacities of these patients. Magu et al.[5] stated that in the retrospective analysis of patients with displaced acetabular fractures treated conservatively, good radiological and functional results can be obtained in compatible reduction. We observed some conservatively treated displaced acetabular fractured patients with a very high functional capacity although having coxarthrosis, so we wondered how were the results of our conservatively treated patients.
In this study, we aimed to compare the functional and radiological results of surgically or conservatively treated patients with a displaced acetabular fracture, who had mid to long-term follow-ups.
MATERIALS AND METHODS
This is a retrospective study, which was carried out in our university, Department of Orthopedics and Traumatology, with the approval of the Ethics committee. Informed consent form was obtained from all patients to participate in this study. Demographic data (age, gender, comorbidity, etc.) and type of trauma were gathered from the physical examinations and file scans, which performed in our outpatient clinic. The study group included 61 patients over the age of 18, who were conservatively and surgically treated for displaced acetabular fractures, between 2000 and 2014. The inclusion criteria of the study were displaced acetabular fracture with a minimum follow-up of 4 years and patients with pre-operative CT scan. Patients with no regular X-ray follow-up and patients with ipsilateral femoral head and shaft fractures were excluded from the study. A fracture was considered displaced if any of the radiographs including Judet views showed more than 3 mm intra-articular displacement (either a step or widening of fracture).
The archive of our clinic was inspected and two groups were formed. Group 1 consisted of 31 patients, who have been treated conservatively between 2000 and 2010. During those dates, all displaced acetabulum fractures were treated conservatively, for reasons local soft-tissue problem, medical contraindications, patient’s unwillingness for surgery, and limited surgical experience. The inclusion criteria for this group were, patients having full-documented X-rays, full-documented data, and patients who have contact numbers with a continuous follow-up. The number of conservatively treated patients with mid-long-term follow-up fulfilling the inclusion criteria was 31. Therefore, to create a balanced group, 30 patients with mid-long-term follow-up, who have been operated for displaced acetabular fractures which have similar fracture patterns with Group 1, between 2010 and 2014, were included to the second group. Statistical powers of the study were conducted using mean value and standard deviation of the data, in the OpenEpi statistical analysis program. The power effect is over 80% threshold in all parameters in the 95% confidence interval. This calculation ensures that a sufficient number of subjects are enrolled for answering the question of interest (OpenEpi: Open Source Epidemiologic Statistics for Public Health).
Group 1 (Conservative treatment Group): The treatment protocol of non-operative treatment for the displaced acetabular fractures (currently needing reduction and fixation in our daily practice) involved initial closed reduction maneuvers under sedation/anesthesia followed by skeletal Femoral Skeletal supracondylar traction.
Group 2 (Operated Group): Surgical treatment was performed for the fractures with displacement >3 mm, roof arch angle <45°, and intact posterior wall fragment <50%.[6–8] Surgical management was applied by selecting the most appropriate incision, according to the fracture types and pre-operative planning. In the post-operative period, after the removal of the drain, passive hip exercises were begun immediately. After the 3rd week, patients were encouraged to engage in touch-down weight-bearing of the operative side, by considering each patient’s general condition and concomitant injuries. Joint step and gap, <2 mm was regarded as appropriate reduction.
We used Judet and Letournel classification, in our study, hence, for the surgical treatment plan considering the anatomy of the pelvis and the biomechanics of the fracture.[9]
X-rays of the patients were collected from the Picture Archiving and Communication System of our hospital and from the radiology archive of our clinic. All X-rays were scanned and acetabular fractures were classified according to Judet and Letournel classification system. Pre-operative intra-articular displacement of fractures of both groups was measured using Judet X-rays and CT scans (Fig. 1) and post-operative reduction quality was evaluated by Judet X-rays. Radiological and clinical outcomes were graded as excellent, good, fair, and poor. The initial plain radiographs routinely obtained postoperatively were AP, iliac-oblique, and obturator-oblique pelvis radiographs. Post-operative acetabular reduction quality was evaluated according to the method described by Selek et al.[10] and were graded according to the criteria described by Matta.[7,10] A displacement of 1 mm or less was considered as anatomic, 2–3 mm as satisfactory, and >3 mm as poor.[7,10,11] All radiographic measurements were evaluated by two observers with the Sectra Workstation IDS7 program (Sectra AB,Sweden). In the follow-up Judet X-rays, radiological results of both groups were evaluated by Matta’s Radiological Evaluation Criteria.[7,12]
Figure 1.
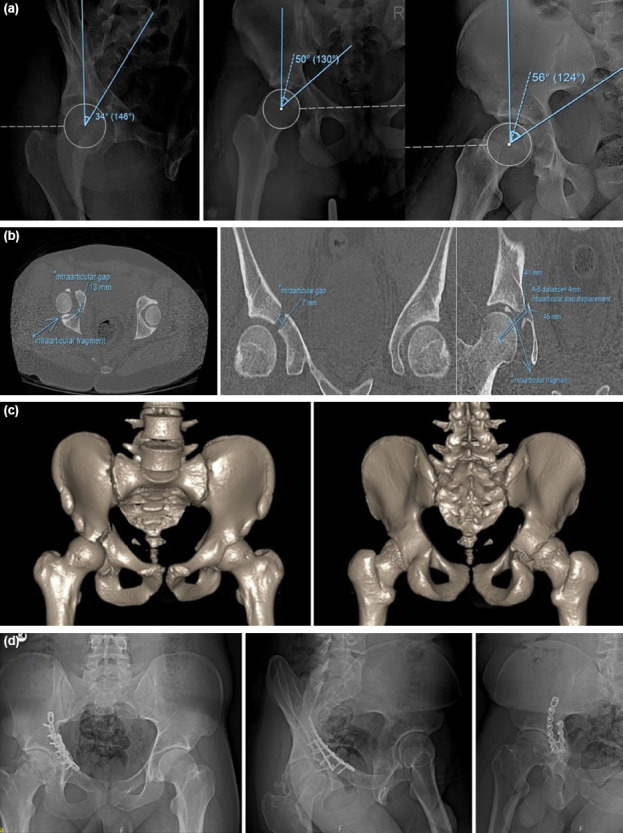
Pre-operative radiological evaluation – 22-year-old male patient who sustained a transvers fracture (a). roof arc angle measurement. (b) Pre-operative evulation of CT-Intra-articular gap and step displacement measurement. (c) Pre-operative pelvic 3-D CT. (d) Post-operative Judet radiographs after 5 year.
Low molecular weight heparin was used for deep vein thrombosis prophylaxis for 6 weeks and no prophylactic measures were applied to prevent heterotopic ossification for both groups.
In the follow-up period, patients were re-called and all their examinations were performed by the authors (E.A, M.E, C.C). Considering the mid-long-term follow-up of all patients in both groups, joint range of motion loss in degrees (loss of flexion, loss of internal rotation, loss of external rotation, and abduction loss) based on the contralateral hip joint of the patients, using a goniometer, were recorded (Fig. 2). Clinical evaluations of the patients were performed according to Modified Merle D’Aubigne criteria, SF-36 and Harris Hip Scoring system.
Figure 2.
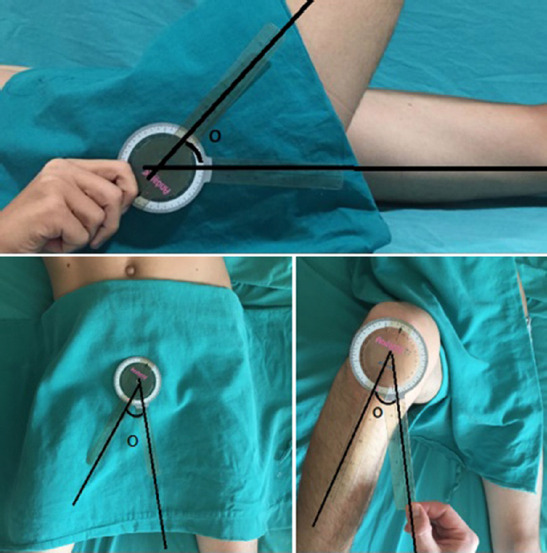
Measurement of hip range of motion.
Statistical evaluation was done using SPSS 19 statistics program with serial number 10240642. The compatibility of the measurable data to the normal distribution is examined with the single-sample Kolmogorov–Smirnov test, after the t-test in the intergroup comparisons for those with normal distribution, t-test in paired series in the group comparisons, Mann–Whitney U-test in the group comparisons for those who do not have a normal distribution, and in the group comparisons, two Wilcoxon paired sample tests were used. For all statistics, the significance limit was chosen as p<0.05.
RESULTS
Demographic data, trauma type, fracture types of both groups according to Judet and Letournel classification, and additional injuries of both groups are listed in Table 1. The average age and gender distribution of the groups were evaluated statistically and there was no significant difference between the groups (p=0.731).
Table 1.
Patient demographics, mechanism of injury, addiotional injuries and types acetabulum of fractures; the study includes 61 patients
| Surgically treated group (n=30) | Conservatively treated group (n=31) | |
|---|---|---|
| Demographics | ||
| Male | 25 | 27 |
| Female | 5 | 4 |
| Average age | 48.93±2.9 | 50.22±2.24 |
| Trauma types | ||
| Traffic accident inside the vehicle (n=31) | 15 | 16 |
| Traffic accident outside the vehicle (n=11) | 8 | 3 |
| Direct trauma (n=6) | 1 | 5 |
| Fall from height (n=13) | 6 | 7 |
| Acetabulum fracture types | ||
| Posterior wall (n=12) | 5 | 7 |
| Posterior column (n=4) | 3 | 1 |
| Anterior Wall (n=–) | – | – |
| Anterior column (n=16) | 8 | 8 |
| Transvers (n=2) | 1 | 1 |
| T-type (n=2) | 1 | 1 |
| Posterior column and posterior wall (n=9) | 5 | 4 |
| Transvers and posterior wall (n=8) | 3 | 5 |
| Anterior column and posterior hemitransverse (n=1) | 1 | – |
| Both column (n=7) | 3 | 4 |
| Additional injuries | ||
| Iliac crest fracture (n=12) | 7 | 5 |
| Sacroiliac dislocation (n=8) | 2 | 6 |
| Spinal fracture (n=5) | 3 | 2 |
| Pubic arm fracture (n=14) | 6 | 8 |
| Pubic diastasis (n=3) | 1 | 2 |
| Acetabulum central or posterior dislocation (n=8) | 4 | 4 |
| Accompanying extremity fracture (n=24) | 16 | 8 |
Four of the conservatively treated patients had fracture dislocation, 12 patients had an unstable fracture in the weight-bearing region and 15 patients had >3 mm displacement in the non-weight-bearing region. In CT sections (axial-coronal-sagittal) of the conservatively treated group, the average fracture displacement in the most displaced sections of the CT was 6.75 mm. Four of the surgically treated patients had fracture dislocation, 14 patients had an unstable fracture in the weight-bearing region, and 12 patients had >3 mm displacement in the non-weight-bearing region. In CT sections (axial-coronal-sagittal) of the surgically treated group, the average fracture displacement in the most displaced sections of the CT was 5,65 mm.
In Group 1 (Conservative), skeletal traction from the supracondylar region of the femur was applied in all of patients; in addition, three patients were applied lateral traction. The average time of skeletal traction was 7.79±3.87 weeks. The average traction weight applied to these cases was 6.69±1.6 kg. The average follow-up period was 10±2.1 years.
In Group 2 (Surgery), all operations were performed by the same surgeon (C.C) on the 5.4±1.15th day averagely (1–16 days) by aiming not to exceed 10 days. The average follow-up period was 5.5±2 years. The approaches applied were as follows: Ilioinguinal approach in eight patients, Kocher–Langenbeck approach in 13 patients, Stoppa approach in three patients, and combined Ilioinguinal and Kocher–Langenbeck in three patients, both Stoppa and Kocher–Langenbeck approach in three patients.
In the early post-operative period, Judet X-rays were evaluated and in the most displaced post-operative X-ray, reduction quality was assessed. Reduction was evaluated as anatomic in 11 patients, satisfactory in 14 patients, and poor in five patients according to the reduction quality evaluation method defined by Matta. In the conservative treatment group, after skeletal traction, reduction was evaluated satisfactory in 14 patients and poor in 17 patients. No patients had anatomical reduction.
According to Judet and Letournel classification, the fracture types were evaluated and compared between the study groups and no significant difference could be observed between both groups (p=0.168) (Table 2).
Table 2.
Categorization of acetabular fractures according to Judet and Letournel classification
| Judet and Letournel classification | Surgically treated group (n=30) | Conservatively treated group (n=31) | p* | p** | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| n | % | n | % | |||
| Elementary fracture (n=33) | ||||||
| JT1 (n=12) | 5 | 16.0 | 7 | 22.5 | 0.168 | 0.527 |
| JT2(n=4) | 3 | 10 | 1 | 3.2 | ||
| JT3 (n=0) | – | – | – | – | ||
| JT4 (n=16) | 8 | 26 | 8 | 25.8 | ||
| JT5 (n=2) | 1 | 3.3 | 1 | 3.2 | ||
| Associated fracture (n=28) | ||||||
| JT6 (n=2) | 1 | 3.3 | 1 | 3.2 | ||
| JT7 (n=9) | 5 | 16.7 | 4 | 12.9 | ||
| JT8 (n=8) | 3 | 10.0 | 5 | 16.6 | ||
| JT9 (n=1) | 1 | 3.3 | – | 0 | ||
| JT10 (n=7) | 3 | 10.0 | 4 | 12.9 | ||
Chi-square test, p<0.05 statistically significant.
All are according to Judet and Letournel classification.
According to elementary and associated fracture classification.
In the evaluation of functional results of both groups, there was no statistically significant difference between the groups (p>0.05), regarding range of motion of the hip joint, Merle D’Aubigne criteria, Harris hip score, and SF-36 functional evaluation scoring after treatment (Table 3).
Table 3.
Evaluation of functional and radiological outcomes of surgical and conservative treatments
| Surgically treated Group (n=30) | Conservatively treated Group (n=31) | p | |
|---|---|---|---|
| Hip joint angle of motion | |||
| Loss of flexion | 8.33±2.35 | 11.61±2.82 | 0.333 |
| Loss of internal rotation | 10.00±2.62 | 9.19±2.54 | 0.960 |
| Loss of external rotation | 7.33±2.19 | 4.51±1.95 | 0.232 |
| Abduction losses | 2.00±1.11 | 1.61±1.14 | 0.410 |
| Functional scoring of hip joint | |||
| SF-36 Mental | 78.00±4.19 | 72.23±5.11 | 0.480 |
| SF-36 Functional | 70.23±2.05 | 68.13±1.67 | 0.292 |
| Harris Hip | 87.13±2.39 | 84.00±3.58 | 0.856 |
| Merle D’Aubigne Score | 16.90±0.27 | 16.32±0.43 | 0.698 |
| Merle D’Aubigne Score, n (%) | |||
| Excellent | 12 (40) | 16 (51.6) | 0.196 |
| Good | 15 (50) | 8 (25.8) | |
| Fair | 3 (10) | 6 (19.3) | |
| Poor | 0 (0) | 1 (3.2) | |
| Radiological scoring (Matta), n (%) | |||
| Excellent | 10 (33.3) | 1 (3.2) | 0.023 |
| Good | 11 (36.6) | 12 (38.7) | |
| Fair | 3 (10.0) | 10 (32.2) | |
| Poor | 6 (20) | 8 (25.8) | |
| Time to put full power to the foot (in weeks) | 11.54±7.55 | 22.6±3.5 | <0.001 |
| Hospitalization period (in days) | 16.2±2.68 | 18.61±4.04 | 0.896 |
In the evaluation of radiological results, Matta’s Radiological Staging scores were compared statistically and there was a significant difference between the groups (p=0.023). It was found that the excellent results in the surgical group were significantly higher than the conservative treatment group, while the poor outcomes were similar in both groups (Table 3).
Mid-long-term follow-up radiographs of some of our patients in both groups (Figs. 3–5).
Figure 3.

A 62-year-old female patient who have acetabulum central dislocation-fracture (a) radiological images before surgical treatment and (b) 7 years after treatment.
Figure 5.
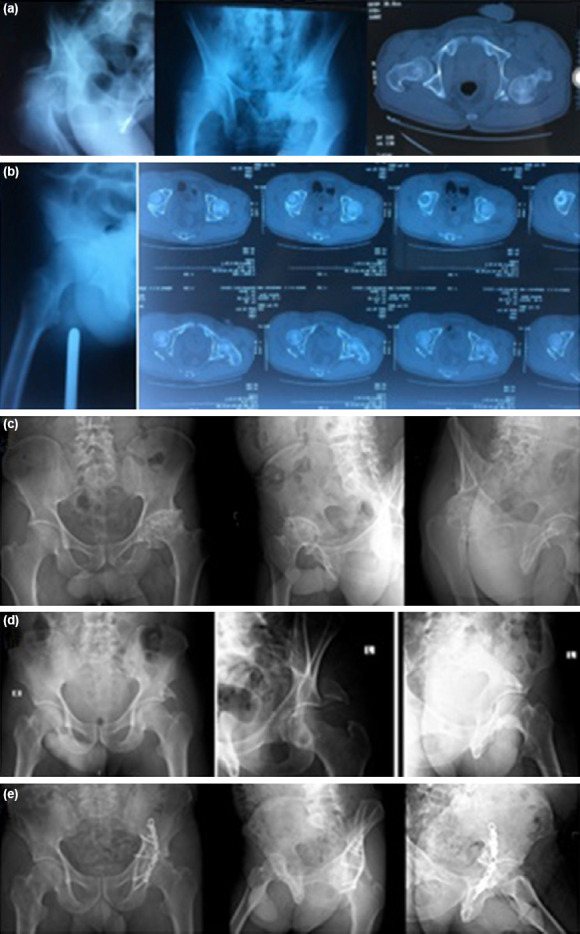
Surgical and conservative treatment results of patients with similar fracture features (a) Pre-operative radiographs – 26-year-old male patient who sustained a dislocation together with posterior wall fracture, (b) post-reduction X-ray and CT images after skeletal traction, (c) results of conservative treatment after 12 years – functional and radiological result – poor result, (d) pre-operative radiographs – 41-year-old male patient who have posterior wall fracture, and (e) results of surgical treatment – after 7 year – functional and radiological result – good result.
Figure 4.
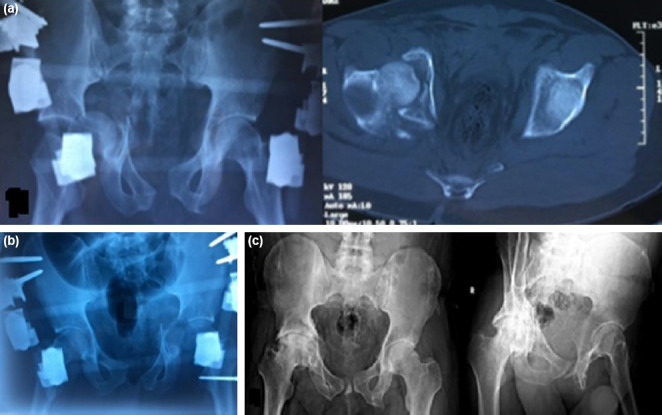
A 26-year-old male patient who have acetabulum central fracture-dislocation. (a) Radiological images before conservative treatment, (b) X-ray image and skeletal traction after reduction, and (c) 11 years after treatment.
The average full weight-bearing time and hospitalization time were compared statistically according to the treatment types and time of full weight-bearing was found longer in the conservative treatment group (p<0.001) and the hospitalization time was similar in both groups (p=0.896) (Table 3).
One patient had Grade – 1 decubitus ulcer due to traction in the cruris region and one patient had pin site infection (External Fixator Pin for accompanying pelvis fracture), in the conservative treatment group. Early surgical site infection was observed in one patient, in the surgical treatment group. No deep venous thrombosis, no neurovascular injury, and no leg-length discrepancy causing functional limitation was observed in both treatment groups.
DISCUSSION
There has been a long-standing debate on the treatment of acetabular fractures. Displaced fractures of the acetabulum are best treated with anatomical reduction and rigid internal fixation,[4] but due to limited surgical experience and medical contraindications, many displaced acetabular fractures have been treated conservatively in the past. There are a few studies reporting long-term outcomes in conservatively treated acetabular fractures.
In a brief exploration of the literature, Sen and Veerappa[13] reported good to excellent results in 56.3% of patients with acetabular fractures who underwent conservative treatment.
Heeg et al.[14] It is concluded that conservative treatment of acetabular fractures can be very successful, even in fractures crossing the weight-bearing dome, provided that congruence is preserved during the period of traction. Magu et al.[5] 71 displaced acetabular fractures (mean age 38.6 years) managed conservatively were retrospectively evaluated and patients with congruent reduction (n=45) had good or excellent functional outcome. Magala et al.[15] stated that in displaced fractures, if the result of surgery is doubtful under various circumstances or if high-risk medical conditions are present in the patient, conservative treatment can be the method of choice with satisfying results. Tipton et al.,[16] in the study’ non-operative management of central fracture-dislocations of the hip’, reported good to excellent functional outcome in 58.4% patients.
Many scoring systems are available in the literature to evaluate hip functional outcomes. Therefore, we think that there is no standard method, in evaluating functional results. We thought that benchmarking with different scores could produce more realistic results. Therefore, we evaluated our patients with Merle D’Aubigne functional evaluation scoring, Harris Hip Scoring and SF-36 scoring systems.
In our study, we achieved 77% good-excellent result, according to the Merle D’Aubigne functional evaluation score, with an average follow-up of 10 years, and we found no significant difference between the surgically treated group statistically. Although there is no significant difference between the functional outcomes in both groups. There are some disadvantages of conservative treatment and these include; lack of early range of motion, long duration of the treatment process, and longer time to full weight-bearing. In our study, in surgically group time to full weight-bearing was 11.54±7.55 weeks, parallel with the literature, whereas in the conservative group, time to full weight-bearing was 22.6±3.5 weeks. Time of full weight-bearing was significantly longer in the conservative group compared to the surgery group (p<0.001). We achieved 90% good-excellent results in the surgical group according to the Merle D’Aubigne functional evaluation score. Kilinc at al.[17] reported 87% excellent or good clinical results, in the modified Stoppa approach applied displaced acetabulum fractured patients, at the end of at least 1-year follow-up. In the study of Aşık et al.[18] including 240 patients with long-term results after surgical treatment, acetabular fractures achieved 80% good and excellent, 5% moderate, and 15% poor results in clinical evaluation with an average follow-up of 11 years. Elmali et al.[19] reported good to excellent results according to clinical evaluation in 71% of 21 patients with acetabular fractures who underwent surgery with an average of 31 months follow-up. In the studies of Kilinc et al.[17] and Elmali et al.,[19] the clinical results were directly related with the reduction quality, statistically.
When we examined our patients by Harris Hip Scoring system, we obtained 63.3%.
(n=18) excellent, 13.3% (n=4) good, 10% (n=3) moderate, and 16.6% (n = 5) poor results in the surgically treated group, while the results were excellent in 64.5% (n=20), good in 12.9% (n=4), and poor in 22.5% (n=7) in the conservative treatment group. When the treatment groups were compared in terms of Harris Hip Scoring system, no significant difference could be found. Regarding the SF-36 scores, there was no statistically significant difference between the two treatment groups. As a result, we obtained similar results with different functional scoring systems.
According to the radiological evaluation criteria of Matta, the rate of excellent results was found 33.3% (n=10) in the surgical group, while the rate of excellent results was found 3.2% (n=1) in the conservative treatment group. We found similar poor outcome rates in both groups. In the statistical comparison of radiological staging scores of Matta, there was a significant difference between the two groups (p=0.023). The excellent results of the surgery group were found to be significantly higher than the conservative treatment group, while the poor outcome was similar in both groups. We correlated the radiological results and functional scores statistically and found no significant difference. This showed us that, poor radiological results does not mean poor functional scores. Although some patients had poor radiological scores, they had a high functional capacity.
There are some advantages and disadvantages of both treatment modalities. Another issue is the complications of acetabular fractures during the treatment period and after the treatment period. Complications of acetabular fractures can be divided into early and late complications.
Venous thromboembolism is the most important cause of mortality and morbidity in the first 24 h. The incidence of pulmonary embolism in patients with acetabular fractures is 2–10% and this is the leading cause of post-operative mortality. Therefore, low molecular weight heparin prophylaxis is highly recommended in all acetabular fractures. Pre-operative and post-operative compression bandaging of the lower extremities is important for mechanical prophylaxis.[13] We applied low molecular weight heparin as medical prophylaxis and compression bandaging as mechanical prophylaxis in both groups. No venous thromboembolism was observed in any patients.
Another important complication is neurologic injuries. Matta et al.[12] found 3.4% nerve injuries in their series, Kınık et al.[20] found 7% iatrogenic nerve damage in their series. Turanlı et al.[21] found this rate as 19.2% after surgery. In our study, the presence of nerve deficits was seen in three cases, two in the surgery group, and one in the conservative treatment group. These deficits were traumatic which occurred during the accident and none of them was iatrogenic and only follow-up, full recovery was achieved.
Although there was no statistically significant difference between the clinical findings, there was a significant difference between radiological findings between both groups. We observed that the clinical findings were good in some patients, although the patient had poor radiological findings. This was interesting and this showed us that radiological scores are not directly correlated with the functional capacity.
Conclusion
Although there is no significant difference between the functional outcomes in both groups statistically, there are some disadvantages of conservative treatment and these include; lack of early range of motion, long duration of the treatment process and longer time to full weight-bearing, and poor radiological scores and to be uncomfortable method. Due to these negativities, it is still controversial that conservative treatment should be the first treatment method in displaced acetabular fractures. In our study, we obtained good radiological and functional scores in the surgical group. Operative treatment should be considered when absolute indications are there. The outcome of conservatively managed fractures is not bleak. We think that there is an alternative to surgical treatment in displaced acetabular fractures and that similar functional results can be obtained in selected cases.
Acknowledgment
The authors thank Dr. Fatma Nesrin Turan for performing the statistical analysis and thanks to our colleagues for their support.
Footnotes
Ethics Committee Approval: This study was approved by the Trakya University Faculty of Medicine Scientific Research Ethics Committee (Date: 19.11.2018, Decision No: 19/26).
Peer-review: Internally peer-reviewed.
Authorship Contributions: Concept: E.A., M.E., C.Ç.; Design: E.A., M.E., C.Ç.; Supervision: E.A., M.E., C.Ç.; Resource: E.A., M.E., C.Ç.; Materials: E.A.; Data: E.A., M.E., C.Ç.; Analysis: E.A., M.E., C.Ç.; Literature search: E.A., C.Ç.; Writing: E.A., M.E., C.Ç.; Critical revision: E.A., C.Ç.
Conflict of Interest: None declared.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Aktuğlu K, Kayaokay K. Surgical complications of Acetabulum fractures. In: Aydoğan NH, editor. Pelvis and Acetabulum fractures. Vol. 2. Ankara: Türkiye Clinics; 2018. pp. 52–9. [Google Scholar]
- 2.Tornetta P. Displaced acetabular fractures:İndications for operative and nonoperative management. J Am Acad Orthop Surg. 2001;9:18–28. doi: 10.5435/00124635-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Giannoudis PV, Grotz MR, Papakostidis C, Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 4.Moed BR, Carr SE, Watson JT. Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am. 2002;84:752–8. doi: 10.2106/00004623-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Magu NK, Rohilla R, Arora S. Conservatively treated acetabular fractures:A retrospective analysis. Indian J Orthop. 2012;46:36–45. doi: 10.4103/0019-5413.91633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Letournel E, Judet R. The kocher-langenbeck approach. In: Reginald AE, editor. Fractures of the Acetabulum. New York: Springer-Verlag; 1993. pp. 364–73. [Google Scholar]
- 7.Matta J. Surgical treatment of acetabulum fractures. In: Browner J, editor. Skeletal Trauma. Vol. 1. New Brunswick: Saunders Company; 2003. pp. 1109–49. [Google Scholar]
- 8.Boudissa M, Ruatti S, Kerschbaumer G, Milaire M, Merloz P, Tonetti J. Part 2:Outcome of acetabular fractures and associated prognostic factors-a ten-year retrospective study of one hundred and fifty six operated cases with open reduction and internal fixation. Int Orthop. 2016;40:2151–6. doi: 10.1007/s00264-015-3070-6. [DOI] [PubMed] [Google Scholar]
- 9.Judet R, Judet J, Letournel E. Fractures of the acetabulum:Classification and surgical approaches for open reduction. J Bone Joint Surg Am. 1964;46:1615–46. [PubMed] [Google Scholar]
- 10.Selek O, Tosun B, Sarlak AY. A new method for reduction quality assessment in acetabular fractures:Acetabular congruency measurement. Hıp Int. 2019;31:435–9. doi: 10.1177/1120700019881620. [DOI] [PubMed] [Google Scholar]
- 11.Matta JM. Acetabular fractures. J Orthop Trauma. 2000;14:377–8. doi: 10.1097/00005131-200006000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Matta JM. Fractures of the acetabulum:Accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78:1632–45. [PubMed] [Google Scholar]
- 13.Sen RK, Veerappa LA. Long-term outcome of conservatively managed displaced acetabular fractures. J Trauma. 2009;67:155–9. doi: 10.1097/TA.0b013e31819db092. [DOI] [PubMed] [Google Scholar]
- 14.Heeg M, Oostvogel HJ, Klasen HJ. Conservative treatment of acetabular fractures:The role of the weight bearing dome and anatomic reduction in the ultimate results. J Trauma. 1987;27:555–9. [PubMed] [Google Scholar]
- 15.Magala M, Popelka V, Božík M, Heger T, Zamborský V, Šimko P. Conservative treatment of acetabular fractures:Epidemiology and medium-term clinical and radiological results. Acta Chir Orthop Traumatol Cech. 2015;82:51–60. [PubMed] [Google Scholar]
- 16.Tipton WW, D'Ambrosia RD, Ryle GP. Non-operative management of central fracture-dislocations of the hip. J Bone Joint Surg Am. 1975;57:888–93. [PubMed] [Google Scholar]
- 17.Kilinc CY, Acan AE, Gultac E, Kilinc RM, Hapa O, Aydogan NH. Treatment results for acetabulum fractures using the modified stoppa approach. Acta Orthop Traumatol Turc. 2019;53:6–14. doi: 10.1016/j.aott.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aşık M, Eralp L, Çetik Ö, Tözün R. Our long-term results in surgically treated acetabular fractures. Acta Orthop Traumatol Turc. 2000;34:245–53. [Google Scholar]
- 19.Elmali N, Ertem K, Inan M, Ayan I, Denizhan Y. Clinical and radiologic results of surgically-treated acetabular fractures. Acta Orthop Traumatol Turc. 2003;37:97–101. [PubMed] [Google Scholar]
- 20.Kınık H, Karakafi A, Mergen E. Surgical treatment of acetabular fractures:Short and midterm results. Acta Orthop Traumatol Turc. 2000;34:254–9. [Google Scholar]
- 21.Turanlı S, Özer H, Yılmaz İ, Doğrul H. Surgical treatment and early results of acetabular fractures. Turk J Arthroplast Arthroscop Surg. 2000;11:1–7. [Google Scholar]


