ABSTRACT
BACKGROUND:
Pertrochanteric fractures are serious health problem with an ever-increasing prevalence in elderly population. Potential post-operative intensive care need leads to delays in the timing of surgery due to the referral of patients to better equipped hospitals as well as the inability to arrange a reserved intensive care bed. The purpose of this study is to investigate whether pre-operative neutrophil-lymphocyte ratio (NLR) has predictive value in terms of post-operative intensive care need in geriatric patients who underwent surgery following pertrochanteric fractures.
METHODS:
A total of 535 patients aged 65 years and above with hip fractures who presented to the emergency service between 2017 and 2020 were retrospectively screened. Out of 535 patients, 317 patients who met the inclusion and exclusion criteria were included in the study. The screened patient population was divided into two groups as those followed in the post-operative intensive care unit (ICU) and those followed in the orthopedic ward.
RESULTS:
There were 190 patients (59.9%) who were followed in the orthopedic ward postoperatively and 127 (40.1%) patients followed in the ICU postoperatively. While the mean pre-operative NLR value of all patients was 6.57, the mean pre-operative NLR of the patients who were followed up postoperatively in the orthopedic ward was 5.85, and the mean NLR of those who were followed up in the ICU was 7.65. It was found that the admission NLR values of the ICU group patients were significantly higher compared to those of the orthopedic ward group (p<0.001) and also the cutoff value of NLR was calculated as 6.14.
CONCLUSION:
We believe that this objective, simple, cost-effective, and rapid marker can be used in combination with other parameters to predict ICU need to prevent surgical delays due to the lack of a reserved intensive care bed in the ASA 3 geriatric patient group with pertrochanteric fractures, whose intensive care need cannot be clarified, thereby reducing mortality and morbidity.
Keywords: Intensive care, neutrophil-lymphocyte ratio, pertrochanteric fracture
INTRODUCTION
Hip fractures are a serious health problem with an ever-increasing prevalence in the elderly population. Around 110,000 cases are detected annually in the world, and it is estimated to increase to 2.6 million cases per year in 2025 and 4.5 million cases per year in 2050.[1] In the literature, 1-year mortality following hip fractures ranges from 8.4% to 36%.[2] With advanced age, physiological changes in organ functions and its associated comorbidities lead to post-operative complications.[3] The most important causes of mortality are myocardial infarction, cardiac failure, pneumonia, and pulmonary embolism regardless of the shape of the fracture and the treatment method.[4] In the literature, laboratory findings such as high potassium level, low hemoglobin and albumin, CRP elevation, and neutrophil-lymphocyte ratio (NLR) have been investigated for their role in predicting mortality, and significant results have been obtained.[5–8]
While white blood cell count is considered a well-defined inflammatory and/or stress indicator, NLR, which is calculated by dividing the absolute neutrophil count by the absolute number of lymphocytes, has been proposed as a novel indicator of inflammatory response.[9] A high correlation has been found between NLR and acute coronary syndrome, non-ST myocardial infarctions, ischemic and hemorrhagic strokes, pulmonary embolism, bullous pemphigoid, and various types of cancer.[10–12]
Although there are studies in the literature investigating the relationship between NLR and mortality following hip fracture surgery,[4,13] femoral neck and pertrochanteric fractures are discussed together under the title of hip fractures in most of the studies, and different surgical methods are evaluated together in terms of their mortality and morbidity. In addition, these studies have generally focused on mortality.[14,15] To the best of our knowledge, there is no study focusing on the need for post-operative intensive care in this patient group.
Potential post-operative intensive care need leads to delays in the timing of surgery due to the referral of patients to better equipped hospitals as well as the inability to arrange a reserved intensive care bed. In these patients whose surgical timing is delayed, mortality, decubitus ulcers due to immobilization and the incidence of post-operative pneumonia increases.[16] Preoperatively, predicting the need for intensive care using a simple and valid method may be beneficial in preventing time losses which increase mortality and morbidity.
The purpose of this retrospective study is to investigate whether preoperative NLR has a predictive value in terms of post-operative intensive care need in geriatric patients who underwent proximal femoral nail procedure following pertrochanteric fractures. No other planned study in a similar population has been identified in the literature.
MATERIALS AND METHODS
A total of 535 patients aged 65 years and above with hip fractures who presented to the emergency service of Necmettin Erbakan University Meram Faculty of Medicine between 2017 and 2020 were retrospectively screened. Exclusion criteria included acute infection, use of immunosuppressants, multitrauma, open fracture, pathological fracture, and previous surgical history from the same hip, pre-operative hemogram <10 mg/dL, surgery time >2 h, and open reduction. In addition, the study included patients over 65 years of age with an American Society of Anesthesiologists (ASA) score of 3 who were operated within a period of 48 h and who underwent proximal femoral nail procedure with closed reduction under regional anesthesia to create a homogeneous group.
The age, gender, ASA score, and pre-operative NLR values of the patients were determined retrospectively by reviewing the hospital records. The same anesthesiology team, who evaluated the patients in the pre-operative period, decided the patients’ need for intensive care based on their intraoperative hemodynamic parameters. The hemodynamic parameters used in the decision-making process were blood oxygen pressure, oxygen saturation, mean blood pressure, and the patient’s state of consciousness. The screened patient population was divided into two groups as those followed in the post-operative intensive care unit (ICU) and those followed in the orthopedic ward. The patients followed in the orthopedic ward were assigned as the control group, and the patients followed in the ICU were assigned as the study group (Fig. 1).
Figure 1.

Study design.
All patients with pertrochanteric femur fractures were treated with proximal femoral nail procedure after closed reduction in the lateral decubitus position under regional anesthesia. Surgical infection prophylaxis with 1 g cefazolin was administered to all patients 1 h before the surgery. For thromboembolism prophylaxis, a single daily dose of enoxaparin sodium 0.4–0.6 ml (based on weight) was administered to each patient from the day of admission to the first post-operative month. In addition, patients were advised to use antiembolism stockings and mobilized by applying partial weight from the 1st post-operative day.
Routine complete blood count biochemistry, bleeding panel, and viral serological tests were performed using venous blood samples collected at the time of initial admission. NLR values were calculated by dividing the neutrophil count in venous blood collected in the pre-operative period by the lymphocyte count.
The study protocol was approved by the Necmettin Erbakan University Maram Faculty of Medicine institutional review board. A written informed consent was obtained from each patient before surgery. The study was conducted in accordance with the principles of the Declaration of Helsinki.
The results were analyzed statistically using SPSS 22 (IBM Corp., Armonk, NY, USA) software. Mean values were expressed as mean±standard deviation. The statistical distribution of the N/L ratio between the groups was determined using the Mann-Whitney U-test. P<0.05 was considered statistically significant. The ROC curve was utilized in assessing whether the NLR could be used as a marker in predicting the need for ICU care.
RESULTS
Out of 535 patients, 317 patients who met the inclusion and exclusion criteria were included in the study. Among the 317 patients, 148 were male (46.7%) and 169 (53.3%) were female. Mean age of the patients was 81.2 years (65–104). There were 190 patients (59.9%) who were followed in the orthopedic ward postoperatively and 127 (40.1%) patients followed in the ICU postoperatively. Twenty-five (7.8%) patients died during the early post-operative period (Table 1). While the mean pre-operative NLR value of all patients was 6.57, the mean pre-operative NLR of the patients who were followed up postoperatively in the orthopedic ward was 5.85, and the mean NLR of those who were followed up in the ICU was 7.65 (Table 2). It was found that the admission NLR values of the ICU group patients were significantly higher compared to those of the orthopedic ward group (p<0.001). While no mechanical complications were observed in any of the patients in the post-operative control radiographs of the patients during their hospitalization, superficial wound infection was observed in 17 patients and uncomplicated deep vein thrombosis in six patients. 25 patients died due to serious post-operative complications such as massive pulmonary embolism, myocardial infarct, and aspiration pneumonia. The NLR of the 25 patients who died during the early post-operative period was 8.1. However, mortality rate could not be statistically compared with NLR as our in-hospital mortality number was very low. In addition, it was found that NLR showed a statistically significant positive correlation with age (Fig. 2). In the ROC analysis performed to investigate whether the NLR could be used as a predictive marker for need of post-operative ICU admission, area under the curve was 0.655 (p<0.001; lower bound: 0.593, upper bound: 0.716), and cutoff value of NLR was calculated as 6.14. The sensitivity and the specificity of this value for ICU admission were 62.2% and 62.1%, respectively (Fig. 3).
Table 1.
Demographic data of study group
| Variables | Case (ICU admission) (n=127) | Control (Orthopaedic ward) (n=190) | p |
|---|---|---|---|
|
|
|
||
| Mean±SD | Mean±SD | ||
| Age (years) | 82.79±7.96 | 80.05±7.98 | 0.002 |
| Sex, n (%) | |||
| Male | 60 (47) | 88 (46) | |
| Female | 67 (43) | 102 (44) | |
| Neutrophil-lymphocyte ratio | 7.6549±3.50320 | 5.8464±3.10122 | <0.001 |
ICU: Intensive care unit.
Table 2.
The neutrophil-to-lymphocyte ratio of study group
| Group | n | Median | Minimum | Maximum | Mean | Standard deviation |
|---|---|---|---|---|---|---|
| Case (ICU admission) | 127 | 7.4600 | 1.0400 | 15.4000 | 7.6549 | 3.50320 |
| Control (Orthopaedic ward) | 190 | 5.1300 | 1.0400 | 16.2000 | 5.8464 | 3.10122 |
| Total | 317 | 5.9800 | 1.0400 | 16.2000 | 6.5709 | 3.38135 |
ICU: Intensive care unit.
Figure 2.

Distribution of the patients who need to ICU and those who did not, according to their age and neutrophil-to-lymphocyte ratios (NLR).
Figure 3.
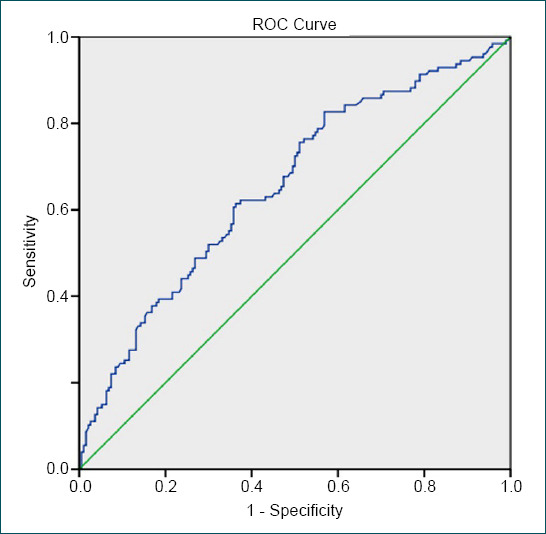
ROC analysis of post-operative ICU admission and NLR (area under the curve: 0.655 (p<0.001; lower bound: 0.593, upper bound: 0.716), cutoff value of NLR=6.14. (Sensitivity: 62.2%, specificity 62.1).
DISCUSSION
The most important result of this study is that there is a statistically significant relationship between the pre-operative NLR value and post-operative intensive care need. Although there are many studies in the literature focusing on mortality in patients with hip fractures, there are no studies on parameters that can predict the need of post-operative ICU care in these patients. Surgeries for patients who are predicted to require intensive care are sometimes delayed due to the lack of a reserved intensive care bed; however, they are followed up in the ward in the post-operative period due to stable pre-operative hemodynamic parameters. Especially in periods when the use of intensive care beds is too intense due to pandemics such as the COVID-19, the lack of a reserved intensive care bed in the orthogeriatric patient group often leads to delays in the surgical timing. In a study by Cha et al.,[17] it was shown that three-quarters of the delays in the timing of surgery were caused due to factors related to the hospital, not the patient. This results in increased patient mortality, various complications, loss of time, inefficient use of hospital beds, and unnecessary referral of patients to higher-level hospitals. The significance of our study is that it is the first study which shows that NLR can be used as a predictor of the patients who will need intensive care.
ASA scoring is the most valid scoring system proven and accepted in determining the general health status of patients who undergo surgical procedures. It has been shown in the literature that the ASA score has a serious relationship with mortality following hip fractures.[18] While patients with ASA score of 4 are more likely to need intensive care, there is often uncertainty about intensive care need in patients with ASA score of 3 due to their age. Therefore, only patients with an ASA score of 3 were included in our study. We think that the ability of NLR to predict intensive care need in the patient population in our study can be beneficial both in preventing patients who will have to wait unnecessarily for a reserved intensive care bed and in determining patients at risk who will likely need post-operative intensive care support despite an ASA score of 3, and facilitate in taking additional precautions accordingly.
As a side result of our study, the positive correlation of NLR with increasing age has been reported previously by Li et al.[19] in healthy population. In fact, Pillay et al.[20] suggested that the frequency of chronic diseases and malignancies that increase with age may be due to the decrease in cytotoxic T lymphocytes fighting tumor cells despite the increased number of neutrophils, which increase the inflammation level of the body.
Mortality is highest in the first 30 days following hip fracture surgeries. In the literature, early mortality ranges from 3.5% to 13.3%.[4,13] In our study, in-hospital early mortality was 7.8% (25 patients), which was consistent with the literature. Forget et al.[14] were the first to describe NLR as a new risk factor for mortality in patients with hip fractures. However, in their study, it was reported that the NLR value >5 on the 5th post-operative day was closely associated with mortality rather than the preoperative NLR value. Fisher et al.[15] found that pre-operative NLR values were associated with post-operative myocardial infarction, high inflammatory response, and in-hospital mortality in the orthogeriatric patient group. In our study, mortality rate could not be statistically compared with NLR as our in-hospital mortality number was very low. Furthermore, Temiz and Ersözlü[21] found that post-operative NLR value ≥4.7 increased the risk of 1-year mortality in patients with hip fracture. Özbek et al.[8] investigated NLR and mortality in pertrochanteric orthogeriatric population and determined that the cutoff value was 5.25 for mortality. In their studies, need for intensive care and its duration were also reported; however, there was no statistical comparison between NLR and intensive care need. Both the small number of patients and the evaluation of ASA 3 and ASA 4 patients together prevent such a comparison.
Different results have been achieved in several studies which examined the relationship between general and regional anesthesia and mortality following hip fractures, and there are international, multicenter, prospective, randomized, and controlled studies (IHOPE, REGAIN) which are still ongoing.[22,23] Since most of the patients operated in our study were elderly patients with multiple comorbid diseases and decreased respiratory capacity, regional anesthesia was used in most of the cases by the anesthesia department. To create a homogeneous group in our study, patients who were operated with only regional anesthesia were included, and those who received general anesthesia were excluded from the study.
In the literature, although there are conflicting results in terms of the time of surgery for hip fractures and its relationship with mortality, the meta-analyses of these studies have definitely shown that mortality rate increases as a result of various complications in patients waiting for more than 48 h.[16,24,25] To eliminate this factor, our study excluded patients who could not be operated in 48 h due to patient and hospital conditions. It is reported that in many countries with highly developed healthcare systems, elderly patients with hip fractures are operated at least 24 h after their admission to the emergency service.[26] A study conducted in France in 2010 has demonstrated that 47–60% of patients are operated after 48 h, a rate close to that observed in the UK (49%).[27] The rate of patients who undergo surgery after 48 h exceeds 13%, even in the protocols which accept hip fractures in the elderly as an indication for emergency surgeries.[28] These delays may be explained by many reasons including pre-operative medical evaluations, optimization of patients’ pre-operative cardiovascular and pulmonary problems, access to the operating room, and the absence of a reserved intensive care bed. By predicting the need for intensive care, it may be possible to decrease morbidity (pressure sores, pulmonary, and urinary problems caused by immobilization) and mortality as a result of preventing at least some of the delays.
The first limitation of our study is that it is a single-center and retrospective study. In addition, although all patients were operated using the same surgical technique, operations were performed by different surgeons. Although the two groups with and without intensive care need were homogenized in terms of factors such as ASA, age, fracture type, surgical technique, and the duration of surgery, it cannot be claimed that all factors likely to affect NLR were excluded from the study. For example, patients with acute infection were not included in our study, however, malignancies not diagnosed yet, the duration and degree of chronic diseases, and the possible effects of the drugs on the NLR were not investigated. In addition, only in-hospital early mortality was examined in our study; however, parameters, such as long-term mortality and function and quality of life indices, were not evaluated. Although, it was found that NLR showed a statistically significant correlation with post-operative intensive care need, the sensitivity and specificity of the cutoff value obtained were not very high (cutoff value of NLR: 6.14. Sensitivity: 62.2%, and specificity: 62.1%). Therefore, we think that this value can be used in combination with other parameters associated with intensive care need, although not alone.
Despite all the limitations of our study, it has been demonstrated that pre-operative NLR is a significant marker that can predict post-operative ICU need. Using this objective, simple, cost-efficient, and fast marker, we believe that unnecessary surgical delays can be reduced due to the lack of reserved ICU beds for orthogeriatric ASA 3 patients with pertrochanteric fractures, for whom intensive care need is unclear, and thus increased mortality and morbidity rates resulting from these delays can be prevented.
Footnotes
Ethics Committee Approval: This study was approved by the Necmettin Erbakan University Faculty of Medicine Clinical Research Ethics Committee (Date: 06.09.2014, Decision No: 29111).
Peer-review: Internally peer-reviewed.
Authorship Contributions: Concept: A.F.K., T.S.Ç.; Design: A.F.K., T.S.Ç.; Supervision: A.F.K., T.S.Ç.; Resource: A.F.K., T.S.Ç.; Materials: A.F.K., T.S.Ç.; Data: T.S.Ç.; Analysis: T.S.Ç.; Literature search: A.F.K.; Writing: A.F.K.; Critical revision: A.F.K., T.S.Ç.
Conflict of Interest: None declared.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Sterling RS. Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res. 2011;469:1913–8. doi: 10.1007/s11999-010-1736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abrahamsen B, Van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture:A systematic epidemiological review. Osteoporos Int. 2009;20:1633–50. doi: 10.1007/s00198-009-0920-3. [DOI] [PubMed] [Google Scholar]
- 3.Partridge JS, Harari D, Martin FC, Dhesi JK. The impact of pre-operative comprehensive geriatric assessment on postoperative outcomes in older patients undergoing scheduled surgery:A systematic review. Anaesthesia. 2014;69:8–16. doi: 10.1111/anae.12494. [DOI] [PubMed] [Google Scholar]
- 4.Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery:A systematic review and meta-analysis. Injury. 2012;43:676–85. doi: 10.1016/j.injury.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 5.Mosfeldt M, Pedersen OB, Riis T, Worm HO, Mark SV, Jørgensen HL, et al. Value of routine blood tests for prediction of mortality risk in hip fracture patients. Acta Orthop. 2012;83:31–5. doi: 10.3109/17453674.2011.652883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forasassi C, Golmard JL, Pautas E, Piette F, Myara I, Raynaud-Simon A. Inflammation and disability as risk factors for mortality in elderly acute care patients. Arch Gerontol Geriatr. 2009;48:406–10. doi: 10.1016/j.archger.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 7.Forget P, Dillien P, Engel H, Cornu O, De Kock M, Yombi JC. Use of the neutrophil-to-lymphocyte ratio as a component of a score to predict postoperative mortality after surgery for hip fracture in elderly subjects. BMC Res Notes. 2016;9:284. doi: 10.1186/s13104-016-2089-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Özbek EA, Ayanoğlu T, Olçar HA, Yalvaç ES. Is the preoperative neutrophil-to-lymphocyte ratio a predictive value for postoperative mortality in orthogeriatric patients who underwent proximal femoral nail surgery for pertrochanteric fractures? Ulus Travma Acil Cerrahi Derg. 2020;26:607–12. doi: 10.14744/tjtes.2020.57375. [DOI] [PubMed] [Google Scholar]
- 9.Soylu K, Gedikli Ö, Ekşi A, Avcıoğlu Y, Soylu Aİ, Yüksel S, et al. Neutrophil-to-lymphocyte ratio for the assessment of hospital mortality in patients with acute pulmonary embolism. Arch Med Sci. 2016;12:95–100. doi: 10.5114/aoms.2016.57585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang F, Hu S, Ding Y, Ju X, Wang L, Lu Q, et al. Neutrophil-to-lymphocyte ratio and 30-Day mortality in patients with acute ıntracerebral hemorrhage. J Stroke Cerebrovasc Dis. 2016;25:182–7. doi: 10.1016/j.jstrokecerebrovasdis.2015.09.013. [DOI] [PubMed] [Google Scholar]
- 11.Wasilewski J, Pyka Ł, Hawranek M, Osadnik T, Kurek A, Skrzypek M, et al. Prognostic value of neutrophil-to-lymphocyte ratio in predicting long-term mortality in patients with ischemic and nonischemic heart failure. Pol Arch Med Wewn. 2016;126:166–73. doi: 10.20452/pamw.3316. [DOI] [PubMed] [Google Scholar]
- 12.Ozer I, Balevi S, Ataseven A. Can neutrophil/lymphocyte ratio be used as a marker in the diagnosis of bullous pemphigoid? Selcuk Med J. 2018;34:65–9. [Google Scholar]
- 13.Carretta E, Bochicchio V, Rucci P, Fabbri G, Laus M. Hip fracture:Effectiveness of early surgery to prevent 30-day mortality. Int Orthop. 2011;35:419–24. doi: 10.1007/s00264-010-1004-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Forget P, Moreau N, Engel H, Cornu O, Boland B, De Kock M, et al. The neutrophil-to-lymphocyte ratio (NLR) after surgery for hip fracture (HF) Arch Gerontol Geriatr. 2015;60:366–71. doi: 10.1016/j.archger.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 15.Fisher A, Srikusalanukul W, Fisher L, Smith P. The neutrophil to lymphocyte ratio on admission and short-term outcomes in orthogeriatric patients. Int J Med Sci. 2016;13:588–602. doi: 10.7150/ijms.15445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klestil T, Röder C, Stotter C, Winkler B, Nehrer S, Lutz M, et al. Impact of timing of surgery in elderly hip fracture patients:A systematic review and meta-analysis. Sci Rep. 2018;8:13933. doi: 10.1038/s41598-018-32098-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cha YH, Ha YC, Yoo JI, Min YS, Lee YK, Koo KH. Effect of causes of surgical delay on early and late mortality in patients with proximal hip fracture. Arch Orthop Trauma Surg. 2017;137:625–30. doi: 10.1007/s00402-017-2674-2. [DOI] [PubMed] [Google Scholar]
- 18.Nkanang B, Parker M, Parker E, Griffiths R. Perioperative mortality for patients with a hip fracture. Injury. 2017;48:2180–3. doi: 10.1016/j.injury.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 19.Li J, Chen Q, Luo X, Hong J, Pan K, Lin X, et al. Neutrophil-to-lymphocyte ratio positively correlates to age in healthy population. J Clin Lab Anal. 2015;29:437–43. doi: 10.1002/jcla.21791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pillay J, Kamp VM, Van Hoffen E, Visser T, Tak T, Lammers JW, et al. A subset of neutrophils in human systemic inflammation inhibits T cell responses through Mac-1. J Clin Invest. 2012;122:327–36. doi: 10.1172/JCI57990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Temiz A, Ersözlü S. Admission neutrophil-to-lymphocyte ratio and postoperative mortality in elderly patients with hip fracture. Ulus Travma Acil Cerrahi Derg. 2019;25:71–4. doi: 10.5505/tjtes.2018.94572. [DOI] [PubMed] [Google Scholar]
- 22.Kowark A, Adam C, Ahrens J, Bajbouj M, Bollheimer C, Borowski M, et al. Improve hip fracture outcome in the elderly patient (iHOPE):A study protocol for a pragmatic, multicentre randomised controlled trial to test the efficacy of spinal versus general anaesthesia. BMJ Open. 2018;8:e023609. doi: 10.1136/bmjopen-2018-023609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neuman MD, Ellenberg SS, Sieber FE, Magaziner JS, Feng R, Carson JL, et al. REGAIN Investigators. Regional versus General Anesthesia for Promoting Independence after Hip Fracture (REGAIN):Protocol for a pragmatic, international multicentre trial. BMJ Open. 2016;6:e013473. doi: 10.1136/bmjopen-2016-013473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shiga T, Wajima Z, Ohe Y. Is operative delay associated with increased mortality of hip fracture patients?Systematic review, meta-analysis, and meta-regression. Can J Anaesth. 2008;55:146–54. doi: 10.1007/BF03016088. [DOI] [PubMed] [Google Scholar]
- 25.Moja L, Piatti A, Pecoraro V, Ricci C, Virgili G, Salanti G, et al. Timing matters in hip fracture surgery:Patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS One. 2012;7:e46175. doi: 10.1371/journal.pone.0046175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hip Fracture Accelerated Surgical Treatment and Care Track (HIP ATTACK) Investigators. Accelerated care versus standard care among patients with hip fracture:The hıp attack pilot trial. CMAJ. 2014;186:E52–60. doi: 10.1503/cmaj.130901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.White SM, Griffiths R, Holloway J, Shannon A. Anaesthesia for proximal femoral fracture in the UK:First report from the NHS Hip Fracture Anaesthesia Network. Anaesthesia. 2010;65:243–8. doi: 10.1111/j.1365-2044.2009.06208.x. [DOI] [PubMed] [Google Scholar]
- 28.Boddaert J, Cohen-Bittan J, Khiami F, Le Manach Y, Raux M, Beinis JY, et al. Postoperative admission to a dedicated geriatric unit decreases mortality in elderly patients with hip fracture. PLoS One. 2014;9:e83795. doi: 10.1371/journal.pone.0083795. [DOI] [PMC free article] [PubMed] [Google Scholar]


