Abstract
Rift Valley fever virus (RVFV) is an emerging arboviral pathogen that causes disease in both livestock and humans. Severe disease manifestations of Rift Valley fever (RVF) in humans include hemorrhagic fever, ocular disease, and encephalitis. This review describes the current understanding of the pathogenesis of RVF encephalitis. While some data from human studies exist, the development of several animal models has accelerated studies of the neuropathogenesis of RVFV. We review current animal models and discuss what they have taught us about RVFV encephalitis. We briefly describe alternative models that have been used to study other neurotropic arboviruses and how these models may help contribute to our understanding RVFV encephalitis. We conclude with some unanswered questions and future directions.
Keywords: Rift Valley fever, viral encephalitis, arbovirus, bunyavirus, aerosol, rat, monkey, African green monkey
INTRODUCTION
Rift Valley fever (RVF) is an emerging arboviral disease that affects livestock and humans in Africa, the western Indian Ocean, and the Middle East. RVF disease was first described in 1931 after sudden mortality in lambs occurred on a farm in the Rift Valley region of Kenya (1). The causative agent, eventually identified and named Rift Valley fever virus (RVFV), has contributed to outbreaks in livestock and humans in the years since with increasing frequency due to climate change (2).
RVFV is a member of the Bunyavirales order, Phenuiviridae family, of negative-sense RNA viruses. RVFV contains three genome segments: The large (L) segment encodes the viral RNA-dependent RNA polymerase (RdRp), the medium (M) segment encodes the surface glycoproteins Gn and Gc along with nonstructural protein NSm, and the small (S) segment encodes the nucleoprotein N and the nonstructural NSs protein (Figure 1) (3). The virus enters cells by receptor-mediated endocytosis, and uncoating of the virion occurs via pH-dependent fusion in the late endosome. The 3 ribonucleocapsids (RNPs) containing the negative-sense genome segments associated with nucleoprotein then undergo transcription into messenger RNA (mRNA) catalyzed by the virus-encoded RdRp. L and S segment mRNAs are translated using free ribosomes, but mRNA from the M segment is translated by endoplasmic reticulum (ER) membrane-bound ribosomes. Replication of (−) genomes to (+) antigenomes and back to (−) genomes is also catalyzed by the RdRp in the cytoplasm of the cell. Newly synthesized RNP segments accumulate at the Golgi where they interact with the cytoplasmic tail of the Gn glycoprotein. Newly assembled virions bud into the lumen of the Golgi, followed by transport to the cell surface in Golgi vesicles and release from the cell.
Figure 1.
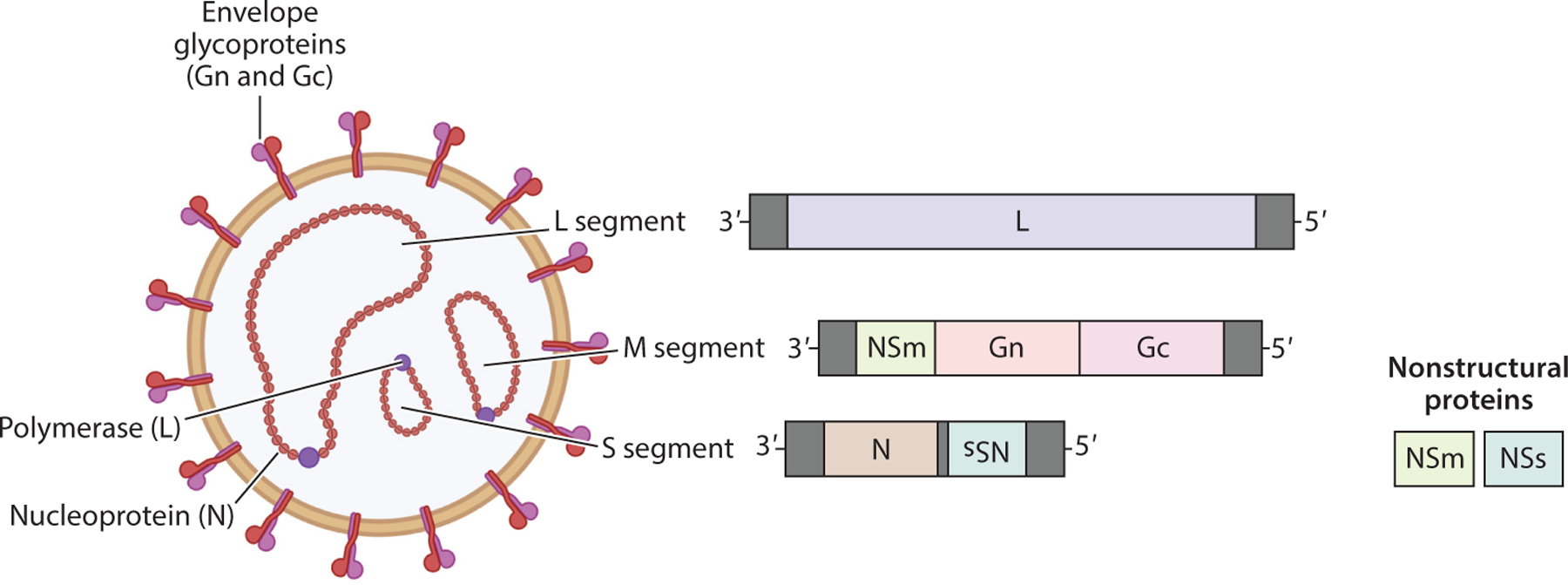
Structure and genome organization of Rift Valley fever virus (RVFV). The envelope glycoproteins Gn and Gc form heterodimers on the virion surface embedded within the lipid bilayer envelope. Within the virion, the three genome segments (L, large; M, medium; and S, small) are complexed with nucleoprotein to form individual ribonucleocapsids. Complementary base pairs on the 3’and 5’ends of each segment result in circularized nucleocapsids, and the viral polymerase (L) protein associates with nucleocapsids to catalyze transcription upon infection of a cell. RVFV does not contain a matrix protein. Two nonstructural proteins, NSm and NSs, are encoded on the M and S segments, respectively. For RVFV, NSm is encoded 3’of Gn and Gc. NSs is encoded in an ambisense orientation on the S segment. Figure adapted from images created with BioRender.com.
As an arbovirus, RVFV is spread by several mosquito species that contribute to viral transmission in the enzootic cycle among sylvatic animals and in the epizootic transmission cycle among domestic livestock and people (4). Mosquitoes of the Aedes and Culex genera are thought to be the primary vectors. Wild animal reservoir(s) such as bats, rodents, or other mammals (gazelles, warthogs, wildebeest, and impala, among others) likely play a role in maintenance and transmission; however, details of RVF circulation in reservoir species remain unknown. Increased rainfall and environmental conditions can promote spread of RVFV into Culex mosquitoes and infection of livestock, which display high viremia and severe disease.
RVFV infection of domesticated livestock, which includes sheep, cattle, goats, and camels, commonly results in severe disease where the primary target organ is the liver (5, 6). In ewes, outbreaks of RVFV infection cause large abortion storms, in which up to 100% of fetuses of pregnant animals are lost (7, 8). Human infection occurs by several means: inhalation or exposure of mucous membranes to viral particles following the handling of sick or deceased livestock, consumption of raw animal products, or mosquito bites (9–11).
RVF in humans is often self-limiting; the probability of asymptomatic infection ranges from 90% to 98% (12). Symptoms of acute disease include headaches, body aches, and fever that lasts 3–5 days (13). For some, these acute symptoms can last for a week or more (13, 14). However, 8–10% of symptomatic RVF cases progress to severe disease, which includes hemorrhagic fever, ocular disease, and encephalitis (15–17). No human-to-human transmission of RVFV has been reported.
RVFV is an emerging virus with regular outbreaks and expanding range. Enhanced understanding of the more severe manifestations of RVFV infection is required to develop mitigation and therapeutic strategies. This review describes what is known about one of the more severe outcomes of RVFV infection, neurological disease (meningoencephalitis). We first describe natural disease outcomes in humans followed by the current status of experimental animal models of RVFV encephalitis. Additionally, we briefly describe alternative models of viral encephalitis being employed to study neurological disease and how these models may be applied to the study of RVFV encephalitis.
EPIDEMIOLOGY
In the past few decades, RVFV appears to be reemerging more frequently, with some regions of eastern Africa experiencing outbreaks of RVF every 4 years (12, 18). A systemic analysis of case reports and seroprevalence studies found that RVFV has been documented in all five African regions encompassing 80% of all African countries (12). The emergence of RVF in the Arabian Peninsula in the early 2000s likely occurred due to the import of infected mosquitos or livestock during trade across the Red Sea (19). Livestock studies show a wide range of RVFV seroprevalence, from less than 1% to nearly 50% in cattle, goats, and camels, and up to 90% of sheep, depending on locality, bioclimatic region, season, breed of animal, and age of animal (20–24). RVFV continues to spread to parts of Africa where it was not previously detected, and introduction of disease into other countries remains a potential threat (12, 25, 26).
Human cases following epizootic outbreaks can range from hundreds to thousands, with case fatalities between 1% and 30% in symptomatic patients reporting to healthcare authorities (15, 17, 27). Human infection most often occurs following outbreaks in livestock (28–30). Incidence of RVFV infection may be underestimated or misdiagnosed unless adjacent to a known livestock outbreak due to the nonspecific symptoms of disease and similarity to cocirculating pathogens (31). RVFV overlaps with other endemic viral diseases with similar disease manifestations, including Lassa fever and West Nile virus (WNV), potentially complicating diagnoses and treatment of cases (32).
HUMAN CASES OF RIFT VALLEY FEVER PRESENTING WITH NEUROLOGICAL DISEASE
In humans infected with RVFV, a range of clinical disease manifestations can be present in individual patients, many of which involve the central nervous system (CNS). This variety of clinical manifestations makes it difficult to define suspected RVF cases. Incidences of complicated RVFV can be categorized into groups based on symptomology (Table 1). General neurologic manifestations have been observed in up to 17% of cases during some outbreaks (11). In 2000 in Saudi Arabia, 53% of patients who displayed CNS involvement died (11). During acute infection, headaches, neck stiffness, retro-orbital pain, and delirium are among the most common neurological symptoms. However, some patients have a delayed onset of meningoencephalitis that ranges from 5 to 60 days following initial symptoms (13, 15). Delayed-onset complications can include vertigo, disorientation, and hallucinations (13). Vision loss and other ocular manifestations occur at an alarming rate, even in the absence of other serious complications, and are considered a neurological outcome of RVF. During the Saudi Arabian outbreak, 15% of hospitalized patients with severe RVF disease had ocular disease consisting primarily of retinitis and retinal hemorrhage (33). More than 100 outpatients (i.e., patients with otherwise mild illness) reported to healthcare facilities specifically with vision-related complaints including a high rate of anterior uveitis. Chorioretinal scarring was the most frequent long-term effect, and some individuals never regained full vision. Comorbidities such as human immunodeficiency virus and malaria may worsen neurologic symptoms (34). Despite the occurrence of neurologic complications during RVF, there is still little understanding of the mechanisms involved in RVFV pathogenesis in the CNS.
Table 1.
Potential clinical classifications of Rift Valley fever disease and their corresponding neurological features
| Disease outcome | Primary clinical feature(s) | Neurological features |
|---|---|---|
| Acute disease (uncomplicated) | Fever, chills, nausea, vomiting, diarrhea, abdominal pain, body aches, headache | Not applicable |
| Severe hemorrhagic fever disease with concomitant neurological involvement | Jaundice, rash, vomiting blood, blood in urine/stool, nosebleed, conjunctival hemorrhage | Headache, neck stiffness, retro-orbital pain, hypersalivation, teeth grinding, confusion, stupor, coma |
| Acute disease with concomitant neurological signs | Acute disease | Neck stiffness, retro-orbital pain, hypersalivation, teeth grinding, confusion |
| Acute disease followed by delayed-onset neurological disease | Acute disease | Recurring headache, confusion, neck stiffness, disorientation, vertigo, hallucination |
| Ocular disease | Acute disease | Vision loss, scotomas, retinal lesions, retinitis, retinal hemorrhage, uveitis |
LABORATORY ANIMAL MODELS OF RIFT VALLEY FEVER VIRUS ENCEPHALITIS
Because neurological manifestations are an outcome of severe RVF in humans, and because autopsy samples from natural human infections are rare, animal models are required to understand neuropathogenesis and clinical outcomes. Several animal models have been developed to specifically study neurologic disease effects in a controlled experimental environment (Table 2). This review focuses on brain involvement and outcomes in animal models of RVFV.
Table 2.
Laboratory animal models of Rift Valley fever neurologic disease
| Species/Strain | Rift Valley fever virus strain; route of infection | Neurological manifestation(s) | Reference(s) |
|---|---|---|---|
| Mice | |||
| C57BL/6J | RVFV-DelNSs; IN | Early-onset neurologic signs, development of meningoencephalitis | 35 |
| BALB/c | ZH501; SC | Delayed-onset encephalitis in mice surviving acute liver disease | 36 |
| ZH501; AERO | Earlier neuroinvasion in AERO-infected mice compared to SC infection | 37 | |
| ZH501; IC | Rapid development of neurologic symptoms including paralysis and convulsions | 38 | |
| STAT-1 knockout | MP-12; IN | Cage circling, head pressing | 39 |
| Rats | |||
| Lewis (LEW/SsNhsd) | ZH501; AERO | Circling or rolling in cage, head tilt, unsteady gait | 40,41 |
| August-Copenhagen-Irish (ACI/SegHsd) | ZH501; AERO | Circling or rolling in cage, head tilt, unsteady gait | 40 |
| Nonhuman primates | |||
| African green monkey (Chlorocebus aethiops) | ZH501; AERO | Fever, drooling, ataxia, horizontal nystagmus, head pressing, seizures | 42,43 |
| Marmoset (Callithrix jacchus) | ZH501; AERO | Biphasic fever, ataxia, tremors, seizures | 42,44 |
| ZH501; SC, IN | Late-onset encephalitis in SC inoculation; lethal encephalitis in all IN-inoculated animals | 44 | |
| Other | |||
| Ferret (Mustela purotius furo) | ZH501; ID, IN | Fever, head tilt (ID), ataxia, seizures/tremors, hind-limb weakness (IN) | 45 |
| Gerbil (Meriones unguiculatus) | ZH501; SC, IC | Hind-limb paralysis; focal necrotizing encephalitis observed by IHC | 46 |
Abbreviations: AERO, aerosol; IC, intracranial; ID, intradermal; IHC, immunohistochemistry; IN, intranasal; SC, subcutaneous.
Rodent Models
Mice are the most common animals used for studies of RVFV pathogenesis due to their extraordinary sensitivity to lethal disease. Unlike most other viruses within the Bunyavirales order, wild-type strains of RVFV cause lethal disease in immunocompetent mice of all ages and strains (36, 47–49). The LD50 (lethal dose 50) is 1 plaque-forming unit (pfu) administered by most tested routes (subcutaneous, intranasal, aerosol, or intraperitoneal), and the average survival time in most mouse strains is 3–5 days. MBT/Pas mice succumb more quickly [2–4 days post-inoculation (dpi)], while BALB/c mice succumb a few days later (6–8 dpi) (48). Consistent across mouse strains, virus strains, and infection routes is that mice perish due to severe hepatic necrosis, with rampant viral titers in the liver and extraordinary elevations of liver enzymes. The sensitivity to hepatic infection is suspected to be due to the inability of the mouse innate antiviral response to limit viral replication. In BALB/c mice, infection with wild-type RVFV most often leads to lethal disease from hepatitis. However, mice that clear infection from visceral organs succumb to late-onset encephalitis (36, 50). In BALB/c mice inoculated via aerosolization of viral particles, viral encephalitis occurs one day earlier than in mice infected via subcutaneous injection (37). A study of inbred mouse strains (C57BL/6J, 129S1/SvlmJ, NOD/ShiLtJ, A/J, and NZO/HILtJ) demonstrated that infection with even a single virion of wild-type RVFV via footpad injection resulted in severe acute hepatitis as the primary outcome. In three animals that survived acute infection, virus was cleared from the liver but encephalitis developed and led to death (47). Given the inconsistent development of encephalitis in mice, it has been difficult to experimentally study viral encephalitis using these animals. An exception to this general rule has been the use of an attenuated RVFV strain lacking the interfernon (IFN)-antagonist NSs protein (RVFV-DelNSs). When administered intranasally, but not subcutaneously, RVFV-DelNSs-infected C57BL/6J mice develop lethal encephalitis in 7–9 days (35). Additional studies using RVFV-DelNSs have shown that cellular immunity is largely responsible for preventing late-onset encephalitis in subcutaneously infected mice (35, 45, 51, 52). Studies using the Collaborative Cross mouse resource identified several mouse strains that develop lethal neurological disease after footpad inoculation, which would allow more detailed studies of pathogenesis to be conducted using an immunocompetent mouse background (53).
Rats are susceptible to RVFV infection and display a wider spectrum of disease manifestations and outcomes compared with mice (54). Some rat strains succumb quickly to hepatic disease (Wistar-Furth, Brown Norway), while others are much more resistant to disease and death (Lewis, Buffalo, F344) (54, 55). A genetic basis for the disparate disease outcome in rats exists but has not been ascribed to specific genes (56, 57). Aerosol exposure is a reliable inoculation route for inducing encephalitis in most rat strains. August-Copenhagen-Irish and Lewis rats are resistant to disease after subcutaneous inoculation of RVFV, but these animals develop reproducibly lethal encephalitis after aerosol exposure (40). RVFV has been found in the eye of some rat strains infected with RVFV (58), suggesting that ocular disease can be studied using these animals (59).
Given the stark contrast in clinical outcomes displayed following subcutaneous and aerosol inoculation of Lewis rats (survival and lethal encephalitis, respectively), Lewis rats have been used for more detailed studies of the pathologic events during RVF encephalitis (Figure 2). Lewis rats succumb to encephalitis 7–8 days after aerosol inoculation with RVFV (ZH501 strain; LD50 ~ 120 pfu) (40). After aerosol exposure, cells of the olfactory epithelium are extensively infected, followed by infection of cells across the cribriform plate and subsequent invasion of the olfactory bulb by 2 dpi (60). Microglia become activated during the initial infection of the brain, as the virus replicates to high levels. RVFV spreads from the olfactory bulb through the brain (61). Due to high levels of virus replication, integrity of the brain structure, in particular the glomerular layer of the olfactory bulb and the vascular integrity of the cortex, is compromised after 5 dpi (60, 61). At the time of brain vasculature deterioration (~5 dpi), immune cells (macrophages and neutrophils) flood the vasculature and parenchyma. Activated microglia, infiltrating macrophages, and neutrophils are infected with RVFV based on flow cytometry and immunofluorescence analysis (41). Histological hallmarks of RVFV encephalitis include vasculitis, meningitis, and neuronal apoptosis (58). The chemokines MMP-9, MCP-1, Gro/KC, MIP-1α, MIP-3α, IL-1α, and IL-1β are elevated first in serum at 3–5 dpi and then are found in high levels in the brain after 5 dpi (41, 58). In contrast, Lewis rats infected subcutaneously develop transient viremia and display moderate levels of viral replication in the liver and spleen (2–5 dpi) and mildly elevated cytokines, such as tumor necrosis factor (TNF)-α, in the serum. While viral RNA can be detected at low levels in the brain of subcutaneous-inoculated rats, viral RNA levels do not increase dramatically, as observed in aerosol-inoculated animals. Taken together, studies of Lewis rats infected with RVFV indicate that high levels of virus replication in the brain after aerosol inoculation cause structural and vascular disintegration, promoting rampant inflammation at end-stage disease. Therapeutic interventions for RVF encephalitis will need to consider how to limit viral entry into the brain, and once there, will need to limit both virus replication and inflammation to protect from lethal disease.
Figure 2.

Current model of neuropathogenesis of Rift Valley fever (RVF) in Lewis rats: timing of clinical and virological events after exposure of Lewis rats to Rift Valley fever virus (RVFV). Events above the timeline (orange background) are those documented in studies of Lewis rats inoculated by subcutaneous (SC) injection, which represents sublethal infection. Events below the timeline (red background) are from animals with lethal neurological disease resulting from aerosol exposure. Events in the periphery are depicted in green, while events in the brain are depicted in blue. (Top) After SC infection [lethal dose 50 (LD50) > 105 plaque-forming unit (pfu)], rats develop viremia from 1 to 4 days post-inoculation (dpi), during which time the virus replicates in the liver and spleen. Transient lymphopenia occurs along with increases in cytokines in the serum. Low levels of viral RNA can be detected in the brain. However, increases in virus levels in the brain over time are not observed. Modestly increased numbers of T cells are observed in the brain at 6 dpi. Rats display no observable signs of illness. (Bottom) After aerosol exposure, the disease course from time of exposure to euthanasia due to severe disease is 7–8 days (LD50 = 120 pfu). Cells within the olfactory epithelium become heavily infected, and the virus invades the brain by crossing the cribriform plate into the olfactory bulb. RVFV then replicates to high levels in the neurons of the olfactory bulb and spreads through the cortex and into the cerebellum. Around 5–6 dpi, vascular integrity of the brain is compromised, and immune cells invade from the periphery. These cells consist primarily of macrophages and neutrophils. These cells, along with activated microglia, are infected with RVFV. Inflammatory cytokines are expressed in the brain at high levels during end-stage disease. Death of neurons and disruption of cell architecture of the brain leads to tissue destruction and severe pathology. During this time, the animals develop observable signs of illness, including weight loss, fever, and neurological manifestations (head tilt, circling in cage).
Nonhuman Primate Models
While nonhuman primates (NHPs) can be infected with RVFV, they are far less susceptible to disease than are rodents and, as such, are more similar to humans in that most disease is mild. In rhesus monkeys inoculated intravenously, intramuscularly, or subcutaneously with RVFV, ~20%develop signs of hemorrhagic fever and ~40% show mild signs of disease such as fever, rash, or vomiting, while the remaining show no clinical disease (62–64). In most infected animals, transient viremia coincides with fever. Rhesus and cynomolgus macaques exposed to aerosols containing RVFV develop transient viremia, fever, and decreased appetite (42, 44, 65). Lack of reproducible severe disease in these species makes it difficult to study viral pathogenesis and efficacy of countermeasures using these animals.
Reproducible lethal disease has been documented in common marmosets exposed to RVFV via intravenous, subcutaneous, and intranasal routes, which lead to both hemorrhagic fever and delayed-onset encephalitis (44). Marmosets inoculated intranasally display 100% mortality with neurological signs 8–11 dpi (44). Both marmosets and old-world African green monkeys (AGMs) are susceptible to neurological disease after aerosol RVFV infection, while cynomolgus and rhesus macaques develop mild febrile illness (42). Beginning 8–10 dpi, both marmosets and AGMs develop symptoms of neurologic disease, including drooling, ataxia, head pressing, and seizures, and the animals succumb 10–12 dpi (42). At end-stage disease, AGMs contain infectious virus only in CNS tissues, while marmosets contain virus in the CNS and abdominal viscera. High numbers of granulocytes predominate in complete blood count analyses at end-stage disease in both monkey models. Infectious virus and viral RNA are found within the eyes, although no pathologic changes in the eye have been documented. Fever is a dominant characteristic in both species, with pyrexia being biphasic in marmosets and monophasic in AGMs. Widespread lesions in the brain with moderate numbers of inflammatory cells (lymphocytes and neutrophils) occur in marmosets and AGMs. Neuronal necrosis and neuronophagia (phagocytosis of degenerate and necrotic neurons) are also commonly observed. There is intense multifocal positive staining of neurons for RVFV antigen by immunohistochemistry. The reproducible encephalitic disease in both marmosets and AGMs makes them useful for studies of neuropathogenic mechanisms.
A more in-depth immunological analysis of AGM compared lethal and sublethal infections (43). AGMs that survive aerosol exposure to RVFV mount an early IFN and cytokine response, along with increased numbers of CD4+ and CD8+ T cells and activation markers. In contrast, AGMs that succumb to neurologic disease have an absent IFN response and no increase in T cell numbers or activation markers; instead they have increased caspase-3 expression in CD8+ T cells. Similar to the situation in RVFV-infected rats, the brains of encephalitic AGMs contain high levels of MCP-1, MIP, IL-6, and IL-8 at end-stage disease. The current model of RVFV neuropathogenesis in AGMs is shown in Figure 3. Collectively, the AGM model highlights the importance of an early innate response and induction of cellular immunity as key predictors of survival (43, 52).
Figure 3.
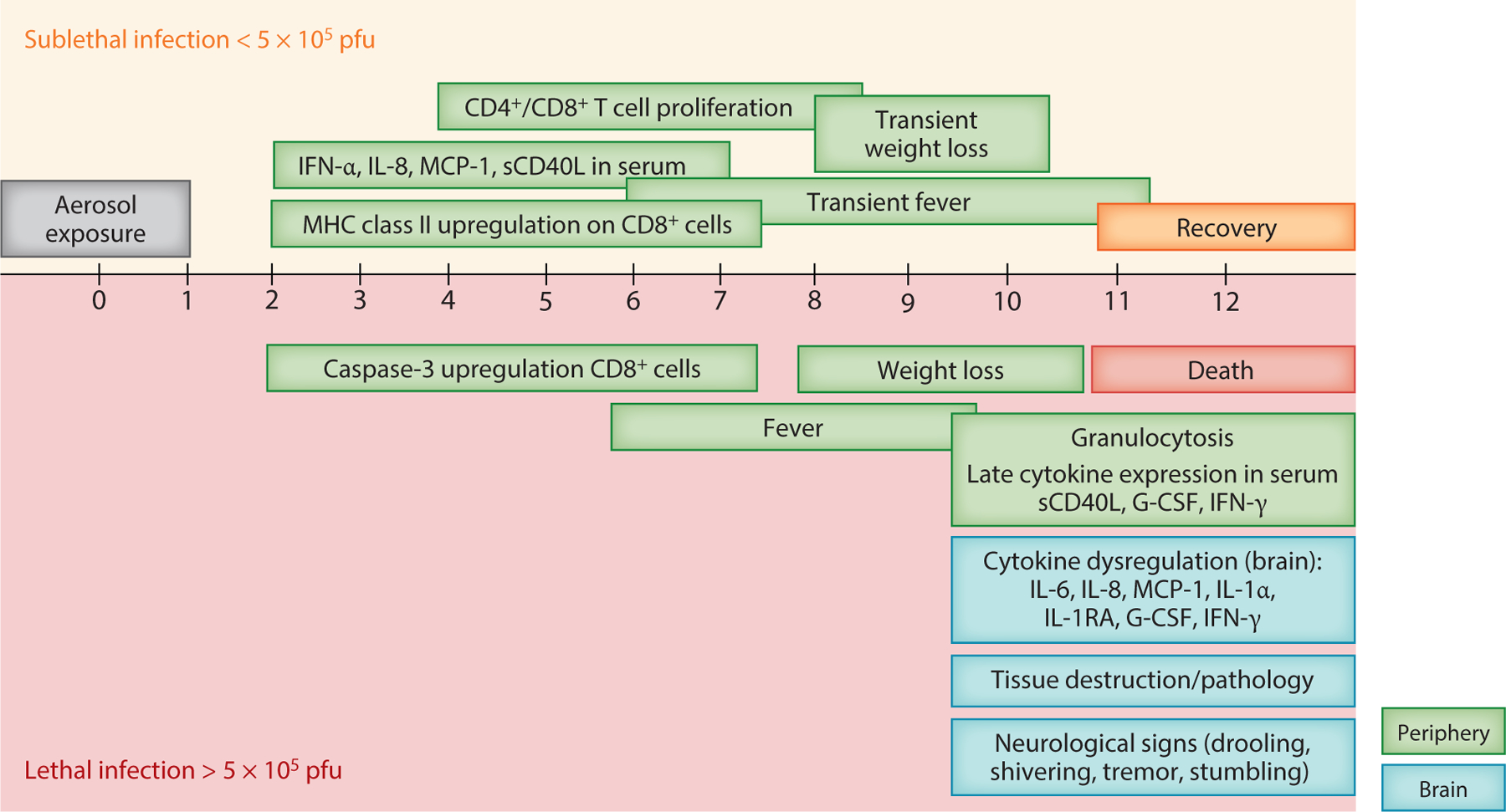
Current model of neuropathogenesis of Rift Valley fever (RVF) in African green monkeys (AGMs): timing of clinical and virological events after aerosol exposure to RVFV. The lethal dose 50 (LD50) of RVFV in AGMs is 5 ×105 plaque-forming unit (pfu). Events above the timeline (orange background) are those documented in RVFV-infected AGMs that survive aerosol infection; events below the timeline (red background) are from animals with lethal neurological disease. Events in the periphery are depicted in green, while events in the brain are depicted in blue. The disease course from time of exposure to euthanasia due to severe disease in AGMs is 9–12 days. (Top) In animals that survive infection, an early cytokine response is detectable in the serum. There is an increase in major histocompatibility complex (MHC) class II expression by CD8+ T cells as early as 2 days post-inoculation (dpi), followed by an increase in both CD4+ and CD8+ T cell numbers beginning at 4 dpi. Surviving AGMs may develop transient fever and weight loss, but these animals recover by 10–12 dpi. (Bottom) In lethally infected animals, there is an absence of an early cytokine response and immune activation in the peripheral blood. Instead, CD8+ T cells express activated forms of caspase-3. AGMs develop severe fever beginning at ~ 6 dpi, followed by weight loss and neurological manifestations (excess salivation, tremors, and stumbling). High numbers of granulocytes in the blood are detectable at ~10 dpi and are a hallmark of severe disease. AGMs reach euthanasia criteria between 9 and 12 dpi and have high levels of inflammatory cytokines, viral titers, and severe pathology in the brain.
Other Animal Models
Gerbils exposed to RVFV subcutaneously display dose- and age-dependent development of encephalitis, with up to 100% mortality in young gerbils with little liver disease (46). However, when a low dose (50 pfu) of RVFV is administered intracranially, all animals, regardless of age, succumb to lethal encephalitis at 7 dpi. Ferrets are susceptible to RVF encephalitis. Exposure of ferrets to RVFV by high-dose intranasal inoculation results in lethal febrile disease with clinical and pathological manifestations of encephalitis by 8–11 dpi (66). Inflammation occurs in the brain and the choroid of the eye. Elevations of liver enzymes (ALT, AST) are observed in lethally infected ferrets. Thus, ferrets may serve as an attractive large animal alternative to NHPs for studies of RVFV pathogenesis, which are more expensive and difficult to acquire.
COMMON PATHOLOGICAL OBSERVATIONS
Human brain tissue from autopsied RVFV cases is not often available, but histological samples were obtained during outbreaks in South Africa (1974), Saudi Arabia (2000), and Kenya (2006) (6, 67). Histology of human brain lesions reveals focal necrosis alongside infiltration of lymphocytes and macrophages with perivascular cuffing (67). Encephalitis also has been documented in RVF cases in individuals with hemorrhagic fever, suggesting brain involvement in this severe form of RVF (68). Common in rat, ferret, and NHP models of RVFV neurologic disease are high titers of virus within the brain itself, likely contributing directly to death of neurons, inflammatory responses (such as MCP-1, Gro/KC/IL-8, IL-6, IL-1α, IL-1RA, G-CSF), and infiltration of macrophages and neutrophils, which are seen in all animal models. Primary histological features in animal models of neurologic disease are perivascular cuffing (inflammatory cells around blood vessels within the brain), meningitis (leukocytic cells within the meninges), encephalitis (lymphocytes, macrophages, neutrophils within the brain parenchyma), and neuronal necrosis or apoptosis. All animal models that manifest neurologic disease also contain virus within the eye, an aspect of RVF pathogenesis that has remained unexplored.
CELL CULTURE AND ALTERNATIVE MODELS OF VIRAL ENCEPHALITIS
Several brain-derived cell lines are highly susceptible to RVFV infection in vitro. Viral replication of the attenuated MP-12 RVFV stain is most efficient in brain cell lines derived from North American livestock and wildlife compared with cell lines derived from kidney and lung (69). The human neuroblastoma cell line SH-SY5Y and microglia cell line HMC3 as well as rat microglia cell line HAPI support high levels of viral replication following infection with the wild-type ZH501 RVFV strain (41). In addition to immortalized cell lines, RVFV replicates in primary cultures of rat neurons and glial cells (70, 71). These studies highlight the in vitro susceptibility of CNS cells to RVFV infection.
While animal models are exceedingly useful in studies of viral pathogenesis, 2D and 3D cell models can be informative. These include brain organoids and ex vivo tissue-culture models. Brain organoids are 3D in vitro culture systems that mimic the organizational and developmental processes of the brain (72). Induced-pluripotent stem cell (iPSC) organoids contain a spectrum of developing neurons, exhibiting an inside-out patterning that includes immature neurons that migrate radially away from the neurogenic region to integrate into the tissue as mature neurons (73). Organoids were used to show that Zika virus (ZIKV) infection leads to loss of the ventricular zone and neuronal layers, mimicking microcephaly observed in ZIKV infection of developing fetuses (74, 75). Brain organoids also have been used to study La Crosse virus (LACV), a neurotropic orthobunyavirus related to RVFV (76, 77). LACV infection of brain organoids decreases structural complexity by inducing loss of cells undergoing neuron development (77).
An alternative 3D model is the organotypic brain-slice culture model, which is used to study molecular and cellular brain functions and neurodegenerative disorders, including Alzheimer disease. Brain-slice cultures allow cell-cell interactions and structural integrity to be somewhat maintained, while preventing influence of peripheral infiltrating cells, such as leukocytes (78). Brains are typically obtained from young postnatal mice or rats, sectioned into 100–500 μm thickness, and maintained in culture for extended periods (79, 80). These organotypic-slice cultures have been used to study other neurotropic arboviruses, including WNV and ZIKV (81–83), offering insight into neuropathogenesis of these viruses in a physiologically relevant ex vivo system. Neither organoid nor brain-slice cultures have yet to be reported for the study of RVFV, but these models may allow important experimental questions to be answered.
CONCLUSIONS AND UNANSWERED QUESTIONS
Many unanswered questions remain despite significant progress in understanding mechanisms underlying RVFV neuropathogenesis. While there is now a better grasp of how RVFV causes lethal disease after aerosol exposure in Lewis rats, we do not know how the virus gets to the brain after peripheral infection and why Lewis rats survive subcutaneous infection despite this fact. Data from studies of Lewis rats and AGMs highlight the importance of induction of early innate and adaptive immune responses in controlling disease. In addition, the mechanism by which RVFV infection results in delayed-onset encephalitis has not been explored using any animal model. The development of additional animal models that reliably allow RVFV neuroinvasion following peripheral inoculation would assist in answering some of these questions. The ocular disease aspect of RVFV pathogenesis is poorly understood and deserves consideration.
Importantly, the neurological animal models described in this review have not been used to investigate the efficacy of therapeutic interventions. Now that rat and monkey models of RVF encephalitis have been characterized to some extent, vaccines and therapeutics should be tested for efficacy in these animals. Recognizing that prevention or amelioration of virus replication in the brain is difficult, approaches such as mucosal (intranasal) vaccination could be tested for the capacity to prevent disease following inoculation by peripheral, intranasal, or aerosol routes. Targeting of therapeutic drugs to the CNS, while difficult, also could be evaluated using these models.
Finally, limited data exist on the basic biology of RVFV infection in the CNS. The role of resident CNS cells—including neurons, microglia, and astrocytes—during RVFV infection and pathogenesis remains understudied. Using alternative models such as cerebral organoids or organotypic brain-slice cultures, in addition to animal models, could shed light on the contributions of resident brain cells during RVFV disease.
ACKNOWLEDGMENTS
This work was supported by NIH/NINDS R01NS101100, NIH/NIAID R01AI150792, and NIH/NIAID R01AI161765.
DISCLOSURE STATEMENT
The authors declare no competing interests. The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
LITERATURE CITED
- 1.Daubney R, Hudson JR, Garnham PC. 1931. Enzootic hepatitis or Rift Valley fever. An undescribed virus disease of sheep cattle and man from East Africa. J. Pathol. Bacteriol 34:545–79 [Google Scholar]
- 2.Murithi RM, Munyua P, Ithondeka PM, Macharia JM, Hightower A, et al. 2011. Rift Valley fever in Kenya: history of epizootics and identification of vulnerable districts. Epidemiol. Infect 139:372–80 [DOI] [PubMed] [Google Scholar]
- 3.Barr JN, Weber F, Schmaljohn CS. 2021. Bunyavirales: the viruses and their replication. In Fields Virology: Emerging Viruses, ed. Howley PM, Knipe DM, Whelan SPJ, pp. 706–49. Philadelphia: Wolters Kluwer. 7th ed. [Google Scholar]
- 4.Chamchod F, Cosner C, Cantrell RS, Beier JC, Ruan S. 2015. Transmission dynamics of Rift Valley fever virus: effects of live and killed vaccines on epizootic outbreaks and enzootic maintenance. Front. Microbiol 6:1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Odendaal L, Clift SJ, Fosgate GT, Davis AS. 2020. Ovine fetal and placental lesions and cellular tropism in natural Rift Valley fever virus infections. Vet. Pathol 57:791–806 [DOI] [PubMed] [Google Scholar]
- 6.Shieh WJ, Paddock CD, Lederman E, Rao CY, Gould LH, et al. 2010. Pathologic studies on suspect animal and human cases of Rift Valley fever from an outbreak in Eastern Africa, 2006–2007. Am. J. Trop. Med. Hyg 83:38–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davies FG, Martin V. 2006. Recognizing Rift Valley fever. Vet. Ital 42:31–53 [PubMed] [Google Scholar]
- 8.Abd el-Rahim IH, Abd el-Hakim U, Hussein M. 1999. An epizootic of Rift Valley fever in Egypt in 1997. Rev. Sci. Tech 18:741–48 [DOI] [PubMed] [Google Scholar]
- 9.LaBeaud AD, Pfeil S, Muiruri S, Dahir S, Sutherland LJ, et al. 2015. Factors associated with severe human Rift Valley fever in Sangailu, Garissa County, Kenya. PLOS Negl. Trop. Dis 9:e0003548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anyangu AS, Gould LH, Sharif SK, Nguku PM, Omolo JO, et al. 2010. Risk factors for severe Rift Valley fever infection in Kenya, 2007. Am. J. Trop. Med. Hyg 83:14–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Madani TA, Al-Mazrou YY, Al-Jeffri MH, Mishkhas AA, Al-Rabeah AM, et al. 2003. Rift Valley fever epidemic in Saudi Arabia: epidemiological, clinical, and laboratory characteristics. Clin. Infect. Dis 37:1084–92 [DOI] [PubMed] [Google Scholar]
- 12.Bron GM, Strimbu K, Cecilia H, Lerch A, Moore SM, et al. 2021. Over 100 years of Rift Valley fever: a patchwork of data on pathogen spread and spillover. Pathogens 10(6):708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laughlin LW, Meegan JM, Strausbaugh LJ, Morens DM, Watten RH. 1979. Epidemic Rift Valley fever in Egypt: observations of the spectrum of human illness. Trans. R. Soc. Trop. Med. Hyg 73:630–33 [DOI] [PubMed] [Google Scholar]
- 14.Gear J, De Meillon B, Measroch V, Davis DH, Harwin H. 1951. Rift Valley fever in South Africa. 2. The occurrence of human cases in the Orange Free State, the North-Western Cape Province, the Western and Southern Transvaal. B. Field and laboratory investigation. S. Afr. Med. J 25:908–12 [PubMed] [Google Scholar]
- 15.Al-Hazmi M, Ayoola EA, Abdurahman M, Banzal S, Ashraf J, et al. 2003. Epidemic Rift Valley fever in Saudi Arabia: a clinical study of severe illness in humans. Clin. Infect. Dis 36:245–52 [DOI] [PubMed] [Google Scholar]
- 16.El Mamy AB, Baba MO, Barry Y, Isselmou K, Dia ML, et al. 2011. Unexpected Rift Valley fever outbreak, northern Mauritania. Emerg. Infect. Dis 17:1894–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hassan OA, Ahlm C, Sang R, Evander M. 2011. The 2007 Rift Valley fever outbreak in Sudan. PLOS Negl. Trop. Dis 5:e1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McMillen CM, Hartman AL. 2018. Rift Valley fever in animals and humans: current perspectives. Antivir. Res 156:29–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anyamba A, Chretien JP, Formenty PB, Small J, Tucker CJ, et al. 2006. Rift Valley fever potential, Arabian Peninsula. Emerg. Infect. Dis 12:518–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zouaghi K, Bouattour A, Aounallah H, Surtees R, Krause E, et al. 2021. First serological evidence of Crimean-Congo hemorrhagic fever virus and Rift Valley fever virus in ruminants in Tunisia. Pathogens 10(6):769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Endale A, Michlmayr D, Abegaz WE, Geda B, Asebe G, et al. 2021. Sero-prevalence of West Nile virus and Rift Valley fever virus infections among cattle under extensive production system in South Omo area, southern Ethiopia. Trop. Anim. Health Prod 53:92. [DOI] [PubMed] [Google Scholar]
- 22.Cosseddu GM, Doumbia B, Scacchia M, Pinoni C, Di Provvido A, et al. 2021. Sero-surveillance of emerging viral diseases in camels and cattle in Nouakchott, Mauritania: an abattoir study. Trop. Anim. Health Prod 53:195. [DOI] [PubMed] [Google Scholar]
- 23.Halawi AD, Saasa N, Pongombo BL, Kajihara M, Chambaro HM, et al. 2019. Seroprevalence of Rift Valley fever in cattle of smallholder farmers in Kwilu Province in the Democratic Republic of Congo. Trop. Anim. Health Prod 51:2619–27 [DOI] [PubMed] [Google Scholar]
- 24.Blomstrom AL, Scharin I, Stenberg H, Figueiredo J, Nhambirre O, et al. 2016. Seroprevalence of Rift Valley fever virus in sheep and goats in Zambezia, Mozambique. Infect. Ecol. Epidemiol 6:31343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nielsen SS, Alvarez J, Bicout DJ, Calistri P, Depner K, et al. 2020. Rift Valley Fever—epidemiological update and risk of introduction into Europe. EFSA J 18:e06041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mweya CN, Mboera LEG, Kimera SI. 2017. Climate influence on emerging risk areas for Rift Valley fever epidemics in Tanzania. Am. J. Trop. Med. Hyg 97:109–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nanyingi MO, Munyua P, Kiama SG, Muchemi GM, Thumbi SM, et al. 2015. A systematic review of Rift Valley fever epidemiology 1931–2014. Infect. Ecol. Epidemiol 5:28024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim Y, Metras R, Dommergues L, Youssouffi C, Combo S, et al. 2021. The role of livestock movements in the spread of Rift Valley fever virus in animals and humans in Mayotte, 2018–19. PLOS Negl. Trop. Dis 15:e0009202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ksiazek TG, Jouan A, Meegan JM, Le Guenno B, Wilson ML, et al. 1989. Rift Valley fever among domestic animals in the recent West African outbreak. Res. Virol 140:67–77 [DOI] [PubMed] [Google Scholar]
- 30.Meegan JM. 1979. The Rift Valley fever epizootic in Egypt 1977–78. 1. Description of the epizootic and virological studies. Trans. R. Soc. Trop. Med. Hyg 73(6):618–23 [DOI] [PubMed] [Google Scholar]
- 31.Javelle E, Lesueur A, Pommier de Santi V, de Laval F, Lefebvre T, et al. 2020. The challenging management of Rift Valley Fever in humans: literature review of the clinical disease and algorithm proposal. Ann. Clin. Microbiol. Antimicrob 19:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Uwishema O, Adanur I, Babatunde AO, Hasan MM, Elmahi OKO, et al. 2021. Viral infections amidst COVID-19 in Africa: implications and recommendations. J. Med. Virol 93:6798–802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al-Hazmi A, Al-Rajhi AA, Abboud EB, Ayoola EA, Al-Hazmi M, et al. 2005. Ocular complications of Rift Valley fever outbreak in Saudi Arabia. Ophthalmology 112:313–18 [DOI] [PubMed] [Google Scholar]
- 34.Mohamed M, Mosha F, Mghamba J, Zaki SR, Shieh WJ, et al. 2010. Epidemiologic and clinical aspects of a Rift Valley fever outbreak in humans in Tanzania, 2007. Am. J. Trop. Med. Hyg 83:22–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dodd KA, McElroy AK, Jones TL, Zaki SR, Nichol ST, Spiropoulou CF. 2014. Rift Valley fever virus encephalitis is associated with an ineffective systemic immune response and activated T cell infiltration into the CNS in an immunocompetent mouse model. PLOS Negl. Trop. Dis 8:e2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith DR, Steele KE, Shamblin J, Honko A, Johnson J, et al. 2010. The pathogenesis of Rift Valley fever virus in the mouse model. Virology 407:256–67 [DOI] [PubMed] [Google Scholar]
- 37.Reed C, Lin K, Wilhelmsen C, Friedrich B, Nalca A, et al. 2013. Aerosol exposure to Rift Valley fever virus causes earlier and more severe neuropathology in the murine model, which has important implications for therapeutic development. PLOS Negl. Trop. Dis 7:e2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leger P, Nachman E, Richter K, Tamietti C, Koch J, et al. 2020. NSs amyloid formation is associated with the virulence of Rift Valley fever virus in mice. Nat. Commun 11:3281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lang Y, Henningson J, Jasperson D, Li Y, Lee J, et al. 2016. Mouse model for the Rift Valley fever virus MP12 strain infection. Vet. Microbiol 195:70–77 [DOI] [PubMed] [Google Scholar]
- 40.Bales JM, Powell DS, Bethel LM, Reed DS, Hartman AL. 2012. Choice of inbred rat strain impacts lethality and disease course after respiratory infection with Rift Valley fever virus. Front. Cell Infect. Microbiol 2:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Albe JR, Boyles DA, Walters AW, Kujawa MR, McMillen CM, et al. 2019. Neutrophil and macrophage influx into the central nervous system are inflammatory components of lethal Rift Valley fever encephalitis in rats. PLOS Pathog 15:e1007833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hartman AL, Powell DS, Bethel LM, Caroline AL, Schmid RJ, et al. 2014. Aerosolized Rift Valley fever virus causes fatal encephalitis in African green monkeys and common marmosets. J. Virol 88:2235–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wonderlich ER, Caroline AL, McMillen CM, Walters AW, Reed DS, et al. 2018. Peripheral blood biomarkers of disease outcome in a monkey model of Rift Valley fever encephalitis. J. Virol 92:e01662–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith DR, Bird BH, Lewis B, Johnston SC, McCarthy S, et al. 2012. Development of a novel nonhuman primate model for Rift Valley fever. J. Virol 86:2109–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Barbeau DJ, Cartwright HN, Harmon JR, Spengler JR, Spiropoulou CF, et al. 2021. Identification and characterization of Rift Valley fever virus-specific T cells reveals a dependence on CD40/CD40L interactions for prevention of encephalitis. J. Virol 95(23):e01506–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Anderson GW Jr., Slone TW Jr., Peters CJ. 1988. The gerbil, Meriones unguiculatus, a model for Rift Valley fever viral encephalitis. Arch. Virol 102:187–96 [DOI] [PubMed] [Google Scholar]
- 47.Cartwright HN, Barbeau DJ, McElroy AK. 2020. Rift Valley fever virus is lethal in different inbred mouse strains independent of sex. Front. Microbiol 11:1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.do Valle TZ, Billecocq A, Guillemot L, Alberts R, Gommet C, et al. 2010. A new mouse model reveals a critical role for host innate immunity in resistance to Rift Valley fever. J. Immunol 185:6146–56 [DOI] [PubMed] [Google Scholar]
- 49.Gray KK, Worthy MN, Juelich TL, Agar SL, Poussard A, et al. 2012. Chemotactic and inflammatory responses in the liver and brain are associated with pathogenesis of Rift Valley fever virus infection in the mouse. PLOS Negl. Trop. Dis 6:e1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reed C, Steele KE, Honko A, Shamblin J, Hensley LE, Smith DR. 2012. Ultrastructural study of Rift Valley fever virus in the mouse model. Virology 431:58–70 [DOI] [PubMed] [Google Scholar]
- 51.Dodd KA, McElroy AK, Jones ME, Nichol ST, Spiropoulou CF. 2013. Rift Valley fever virus clearance and protection from neurologic disease are dependent on CD4+ T cell and virus-specific antibody responses. J. Virol 87:6161–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Harmon JR, Spengler JR, Coleman-McCray JD, Nichol ST, Spiropoulou CF, McElroy AK. 2018. CD4 T cells, CD8 T cells, and monocytes coordinate to prevent Rift Valley fever virus encephalitis. J. Virol 92(24):e01270–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cartwright HN, Barbeau DJ, Doyle JD, McElroy AK. 2021. A novel mouse model of Rift Valley fever virus encephalitis. Abstract presented at the 40th Annual American Society for Virology Meeting, July 19–23 [Google Scholar]
- 54.Peters CJ, Slone TW. 1982. Inbred rat strains mimic the disparate human response to Rift Valley fever virus infection. J. Med. Virol 10:45–54 [DOI] [PubMed] [Google Scholar]
- 55.Peters CJ, Anderson GW Jr. 1981. Pathogenesis of Rift Valley fever. Viruses 3(5):493–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Anderson GW Jr., Rosebrock JA, Johnson AJ, Jennings GB, Peters CJ. 1991. Infection of inbred rat strains with Rift Valley fever virus: development of a congenic resistant strain and observations on agedependence of resistance. Am. J. Trop. Med. Hyg 44:475–80 [DOI] [PubMed] [Google Scholar]
- 57.Busch CM, Callicott RJ, Peters CJ, Morrill JC, Womack JE. 2015. Mapping a major gene for resistance to Rift Valley fever virus in laboratory rats. J. Hered 106:728–33 [DOI] [PubMed] [Google Scholar]
- 58.Caroline AL, Kujawa MR, Oury TD, Reed DS, Hartman AL. 2016. Inflammatory biomarkers associated with lethal Rift Valley fever encephalitis in the Lewis rat model. Front. Microbiol 6:1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schwarz MM, McMillen CM, Demers MJ, Hartman A. 2021. Development of a rat model of Rift Valley fever virus ocular disease. Abstract presented at the 40th Annual American Society for Virology Meeting, July 19–23 [Google Scholar]
- 60.Boyles DA, Schwarz MM, Albe JR, McMillen CM, O’Malley KJ, et al. 2021. Development of Rift Valley fever encephalitis in rats is mediated by early infection of olfactory epithelium and neuroinvasion across the cribriform plate. J. Gen. Virol 102:001522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Walters AW, Kujawa MR, Albe JR, Reed DS, Klimstra WB, Hartman AL. 2019. Vascular permeability in the brain is a late pathogenic event during Rift Valley fever virus encephalitis in rats. Virology 526:173–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cosgriff TM, Morrill JC, Jennings GB, Hodgson LA, Slayter MV, et al. 1989. Hemostatic derangement produced by Rift Valley fever virus in rhesus monkeys. Rev. Infect. Dis 11(Suppl. 4):S807–14 [DOI] [PubMed] [Google Scholar]
- 63.Morrill JC, Jennings GB, Johnson AJ, Cosgriff TM, Gibbs PH, Peters CJ. 1990. Pathogenesis of Rift Valley fever in rhesus monkeys: role of interferon response. Arch. Virol 110:195–212 [DOI] [PubMed] [Google Scholar]
- 64.Peters CJ, Jones D, Trotter R, Donaldson J, White J, et al. 1988. Experimental Rift Valley fever in rhesus macaques. Arch. Virol 99:31–44 [DOI] [PubMed] [Google Scholar]
- 65.Morrill JC, Peters CJ. 2011. Protection of MP-12–vaccinated rhesus macaques against parenteral and aerosol challenge with virulent Rift Valley fever virus. J. Infect. Dis 204:229–36 [DOI] [PubMed] [Google Scholar]
- 66.Barbeau DJ, Albe JR, Nambulli S, Tilston-Lunel NL, Hartman AL, et al. 2020. Rift Valley fever virus infection causes acute encephalitis in the ferret. mSphere 5:e00798–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.van Velden DJ, Meyer JD, Olivier J, Gear JH, McIntosh B. 1977. Rift Valley fever affecting humans in South Africa: a clinicopathological study. S. Afr. Med. J 51:867–71 [PubMed] [Google Scholar]
- 68.Ikegami T, Makino S. 2011. The pathogenesis of Rift Valley fever. Viruses 3:493–519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gaudreault NN, Indran SV, Bryant PK, Richt JA, Wilson WC. 2015. Comparison of Rift Valley fever virus replication in North American livestock and wildlife cell lines. Front. Microbiol 6:664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Moy RH, Gold B, Molleston JM, Schad V, Yanger K, et al. 2014. Antiviral autophagy restricts Rift Valley fever virus infection and is conserved from flies to mammals. Immunity 40:51–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ritter M, Bouloy M, Vialat P, Janzen C, Haller O, Frese M. 2000. Resistance to Rift Valley fever virus in Rattus norvegicus: genetic variability within certain ‘inbred’ strains. J. Gen. Virol 81:2683–88 [DOI] [PubMed] [Google Scholar]
- 72.Chiaradia I, Lancaster MA. 2020. Brain organoids for the study of human neurobiology at the interface of in vitro and in vivo. Nat. Neurosci 23:1496–508 [DOI] [PubMed] [Google Scholar]
- 73.Zhang BZ, Chu H, Han S, Shuai H, Deng J, et al. 2020. SARS-CoV-2 infects human neural progenitor cells and brain organoids. Cell Res 30:928–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Qian X, Nguyen HN, Jacob F, Song H, Ming GL. 2017. Using brain organoids to understand Zika virusinduced microcephaly. Development 144:952–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Qian X, Nguyen HN, Song MM, Hadiono C, Ogden SC, et al. 2016. Brain-region-specific organoids using mini-bioreactors for modeling ZIKV exposure. Cell 165:1238–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vahey GM, Lindsey NP, Staples JE, Hills SL. 2021. La Crosse virus disease in the United States, 2003–2019. Am. J. Trop. Med. Hyg 105:807–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Winkler CW, Woods TA, Groveman BR, Carmody AB, Speranza EE, et al. 2019. Neuronal maturation reduces the type I IFN response to orthobunyavirus infection and leads to increased apoptosis of human neurons. J. Neuroinflamm 16:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Humpel C 2015. Organotypic brain slice cultures: a review. Neuroscience 305:86–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Croft CL, Cruz PE, Ryu DH, Ceballos-Diaz C, Strang KH, et al. 2019. rAAV-based brain slice culture models of Alzheimer’s and Parkinson’s disease inclusion pathologies. J. Exp. Med 216:539–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Busch J, Chey S, Sieg M, Vahlenkamp TW, Liebert UG. 2021. Mutated measles virus matrix and fusion protein influence viral titer in vitro and neuro-invasion in Lewis rat brain slice cultures. Viruses 13(4):605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rosenfeld AB, Doobin DJ, Warren AL, Racaniello VR, Vallee RB. 2017. Replication of early and recent Zika virus isolates throughout mouse brain development. PNAS 114:12273–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Clarke P, Leser JS, Tyler KL. 2021. Intrinsic innate immune responses control viral growth and protect against neuronal death in an ex vivo model of West Nile virus-induced central nervous system disease. J. Virol 95:e0083521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Buttner C, Heer M, Traichel J, Schwemmle M, Heimrich B. 2019. Zika virus-mediated death of hippocampal neurons is independent from maturation state. Front. Cell Neurosci 13:389. [DOI] [PMC free article] [PubMed] [Google Scholar]


