Abstract
The BCL-2 inhibitor venetoclax has revolutionized the treatment of acute myeloid leukemia (AML) in patients not benefiting from intensive chemotherapy. Nevertheless, treatment failure remains a challenge, and predictive markers are needed, particularly for relapsed or refractory AML. Ex vivo drug sensitivity testing may correlate with outcomes, but its prospective predictive value remains unexplored. Here we report the results of the first stage of the prospective phase II VenEx trial evaluating the utility and predictiveness of venetoclax sensitivity testing using different cell culture conditions and cell viability assays in patients receiving venetoclax-azacitidine. Participants with de novo AML ineligible for intensive chemotherapy, relapsed or refractory AML, or secondary AML were included. The primary endpoint was the treatment response in participants showing ex vivo sensitivity and the key secondary endpoints were the correlation of sensitivity with responses and survival. Venetoclax sensitivity testing was successful in 38/39 participants. Experimental conditions significantly influenced the predictive accuracy. Blast-specific venetoclax sensitivity measured in conditioned medium most accurately correlated with treatment outcomes; 88% of sensitive participants achieved a treatment response. The median survival was significantly longer for participants who were ex vivo-sensitive to venetoclax (14.6 months for venetoclax-sensitive patients vs. 3.5 for venetoclax-insensitive patients, P<0.001). This analysis illustrates the feasibility of integrating drug-response profiling into clinical practice and demonstrates excellent predictivity. This trial is registered with ClinicalTrials.gov identifier: NCT04267081
Introduction
A long-term goal in leukemia and cancer research has been the determination of responses to anti-cancer therapy in the laboratory prior to clinical treatment, in analogy to the success of antibiotic sensitivity testing in microbial disease.1 The development of targeted therapies and technological advances has highlighted the approach again in acute myeloid leukemia (AML), as genomic data are often neither actionable nor predictive.2 We and others, including the Beat AML program, have previously demonstrated that drug sensitivity profiling provides clinically actionable therapeutic insights for individual patients with AML.3,4
However, only a few prospective trials have analyzed the predictiveness of ex vivo drug sensitivity testing,5,6 and more data are needed to demonstrate its clinical utility.7 Sensitivity to drugs is currently tested using multiple techniques. This diversity highlights the importance of understanding how different parameters influence the results. In AML, bone marrow is often a heterogeneous mix of cells consisting of leukemic blasts and more mature leukemic and healthy cells. Thus, commonly used homogeneous cell viability assays cannot accurately measure blast-specific drug responses. To overcome this limitation, immunofluorescence microscopy and flow cytometry-based assays have been implemented to evaluate responses at the single-cell level.8,9 We previously demonstrated that a flow cytometry-based assay can determine the venetoclax sensitivity of each cell population.10 Importantly, blast-specific results of drug sensitivity differ dramatically from the sensitivity of bulk samples. An as yet unexplored challenge is the effect of culture conditions on ex vivo responses and correlation with treatment outcomes. Our previous work showed that conditioned medium (CM) derived from HS-5 bone marrow stromal cells, which closely resembles the bone marrow microenvironment, improves cell viability and alters the results of ex vivo drug sensitivity testing.11
For AML, predicting treatment outcome is extremely relevant. New therapeutic options have emerged, but there is heterogeneity in responses, and difficulties in identifying patients who will benefit from these therapies.2 The B-cell lymphoma 2 (BCL-2) inhibitor venetoclax is an excellent illustration of this challenge. In patients ineligible for induction therapy, venetoclax combined with the hypomethylating agent azacitidine showed acceptable safety and favorable responses. In the Viale-A trial complete remission (CR) and complete remission with incomplete blood recovery (CRi) were observed in 66% of the participants and the median overall survival was 14.7 months.12 In a single-center trial of relapsed or refractory (R/R) patients, 40% achieved CR/CRi, with the median overall survival being 7.8 months.13 While certain genetic changes correlate with treatment outcomes (e.g., IDH2, NPM1, and TP53),14,15 not all patients harbor these alterations. Furthermore, based on existing data, mutations are unable to predict response to venetoclax-azacitidine pre-cisely.16,17 Thus, novel approaches are needed to identify patients who will benefit, particularly in the R/R setting. Previous retrospective studies have shown that ex vivo sensitivity to venetoclax is associated with treatment responses in small cohorts of patients with AML,3 myelodysplastic syndromes,18 and B-cell acute lymphoblastic leukemia.19 In addition, BH3 profiling showed that combined MCL-1 and BCL-XL dependency correlated inversely with the achievement of CR in 19 AML patients treated with venetoclax and a hypomethylating agent.20 However, no prospective clinical trials have analyzed the ability of ex vivo drug sensitivity testing to predict outcomes following venetoclax treatment. Furthermore, a systematic evaluation of the effects of cell culture conditions and different drug testing platforms (e.g., bone marrow bulk analysis with luminescent cell viability assay or targeted flow cytometry) remains unexplored. These gaps in knowledge have also hindered the development of pre-clinical models. Therefore, we designed this prospective VenEx trial to evaluate the usability of ex vivo drug sensitivity testing in a clinical context and to evaluate the correlation of drug sensitivity test results with outcomes of venetoclax-azacitidine treatment in AML.
Methods
More detailed information of the methods and analyses is provided in the Online Supplementary Appendix.
Study design and participants
The VenEx trial is an ongoing, multicenter, two-stage, open-label, phase II trial evaluating the correlation of ex vivo sensitivity to venetoclax with clinical outcomes in chemotherapy-ineligible patients with de novo, secondary, or R/R AML treated with venetoclax and azacitidine. Ineligibility for standard induction therapy was defined by modified Ferrara criteria21 which include age (≥70 years); clinically relevant comorbidities, such as decreased left ventricular ejection fraction (<50%), chronic stable angina, or controlled congestive heart failure; and decreased lung diffusion capacity (≤65%) or forced expiratory volume in 1 second ≤65%. For relapsed patients with non-core binding factor AML, an age criterion of ≥55 years was allowed. For participants younger than 55 years, additional inclusion criteria included either a remission duration of less than 12 months or relapse after allogeneic stem cell transplantation. Ex vivo drug sensitivity testing was obligatory for all participants at screening. The main exclusion criteria were a blast count ≤10% in the bone marrow or peripheral blood, depending on which was used for ex vivo drug testing, and previous venetoclax therapy for myeloid malignancy.
The study is being conducted by the Finnish AML Group at five university hospitals in Finland. The Helsinki University Hospital District is the trial’s sponsor and the study is funded by independent institutions and foundations. The funders do not have any role in the study design, data collection, data analysis, data interpretation, or report writing. The study is being conducted in accordance with the Declaration of Helsinki and International Council for Harmonization on Good Clinical Practice guidelines. The study protocol, which was approved by an independent ethics committee and competent authority, is available in the Online Supplementary Material. All participants provided written informed consent before initiation of the study.
Screening procedures and venetoclax sensitivity analysis
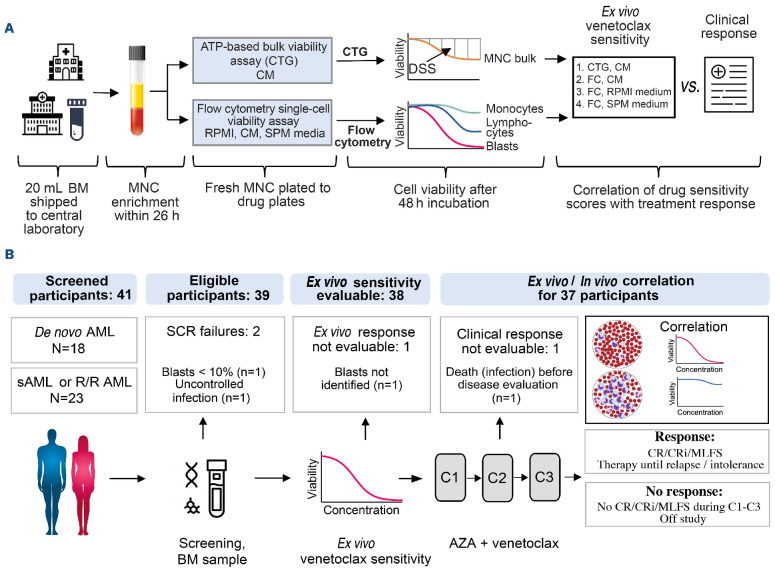
At screening, all participants underwent bone marrow sampling. When the bone marrow could not be aspirated, peripheral blood with a blast count >10% was used for analyses. For drug sensitivity testing, 20 mL of bone marrow (n=37) or 30 mL of peripheral blood (n=2) were shipped from five trial sites to the central laboratory in EDTA tubes at room temperature. Mononuclear cells were isolated using Ficoll gradient centrifugation and plated in two different drug plates within 26 hours of sampling. The drug plates contained venetoclax, a vene-toclax–azacitidine combination, and other BCL-2 family inhibitors across a 10,000-fold concentration range (Online Supplementary Table S1). After incubation with the drugs for 48 hours, cell viability was assessed in parallel using CellTiterGlo® (CTG) and flow cytometry. The trial outline is presented in Figure 1A.
For the flow cytometry-based drug sensitivity assay, cells were plated in 96-well, conical-bottomed plates with 100,000 cells/well in 100 mL of the appropriate medium. Venetoclax sensitivity was measured in three different cell culture conditions: (i) RPMI + 10% fetal bovine serum, (ii) CM (medium derived from the HS-5 cell line), and (iii) StemSpan SFEM II + 20 ng/mL of FLT3L + stem cell factor + thrombopoietin (SPM) (Online Supplementary Table S2). Following incubation for 48 hours, cells were stained with an antibody mix containing CD45, CD34, CD117, CD14, CD11b, CD64, and CD38, and then stained with markers of apoptosis (annexin V) and dead cells (7-aminoactinomycin D; 7-AAD). Flow cytometry data were acquired using an iQue Screener PLUS instrument (Sartorius, Germany), and ForeCyt software (Sartorius) was used to analyze the cells. The gating strategy is presented in Online Supplementary Figures S1 and S2. The number of remaining viable blasts in each well was counted and normalized to the number in control wells containing dimethylsulfoxide (DMSO) (Online Supplementary Figure S3). For the CTG-based drug sensitivity assay, cells were suspended in 25 mL of CM and plated in 384-well plates with 10,000 cells/well. After incubation for 48 hours, 25 mL of CTG were added to each well, and the intensity of the luminescence was measured using the PHERAstar FS plate reader (BMG LABTECH, Germany). Drug sensitivity scores (DSS) derived from the optimized area under the dose-response curve calculations22 indicated the efficacy of both viability assays (Online Supplementary Figure S3). Quality control metrics and reproducibility of the assay are described in the Online Supplementary Methods and Online Supplementary Figure S4.
Figure 1.
Sample processing and trial outline. (A) Outline of sample processing and drug sensitivity testing. (B) Outline of study recruitment, including number of participants, reasons for screening failure, and number of participants eligible for ex vivo/in vivo correlation. BM: bone marrow; MNC: mononuclear cells; CTG: CellTiterGlo®; CM: conditioned medium; DSS: drug sensitivity score; FC: flow cytometry; AML: acute myeloid leukemia; sAML: secondary AML; R/R AML: relapsed and/or resistant AML; SCR: screening; C: cycle; AZA: azacitidine; CR: complete remission; CRi: CR with incomplete blood recovery; MLFS: morphological leukemia-free state.
Treatment
During the first stage of the trial, all participants received the study treatment regardless of their venetoclax sensitivity testing results (n=39). The results were not communicated to the investigators. The study treatment consisted of 28-day cycles of azacitidine (75 mg/m2 on days 1-7) and venetoclax (400 mg daily for a maximum of 28 days). For responding participants, a cycle could be prolonged up to 42 days to enable blood count recovery. After a CR/CRi or a morphological leukemia-free state (MLFS) had been reached, the cycle of venetoclax administration was reduced to 21 days, and then, after three cycles, to 14 days in each cycle. Treatment response was assessed at day 29 of cycle 1, cycle 3, and cycle 6, and then every three cycles. For participants not in CR, CRi, or MLFS at day 29 of cycle 1, the bone marrow was also evaluated at day 29 of cycle 2. Those participants refractory to the study treatment after three cycles were taken off the trial.
Assessments and statistical analyses
The primary endpoint was the treatment response during the first three therapy cycles in participants who showed ex vivo sensitivity to venetoclax. The cutoff value for sensitivity was evaluated retrospectively after all trial participants had been evaluated for treatment response. The investigators assessed the response using criteria defined by the European LeukemiaNet for AML in 2017.23 The key secondary endpoint was the correlation of ex vivo drug sensitivity with overall survival and the overall response rate. Both recruiting cohorts and trial phases are analyzed separately. The Online Supplementary Appendix provides details on the statistical analyses.
Results
Enrollment and patients’ demographics
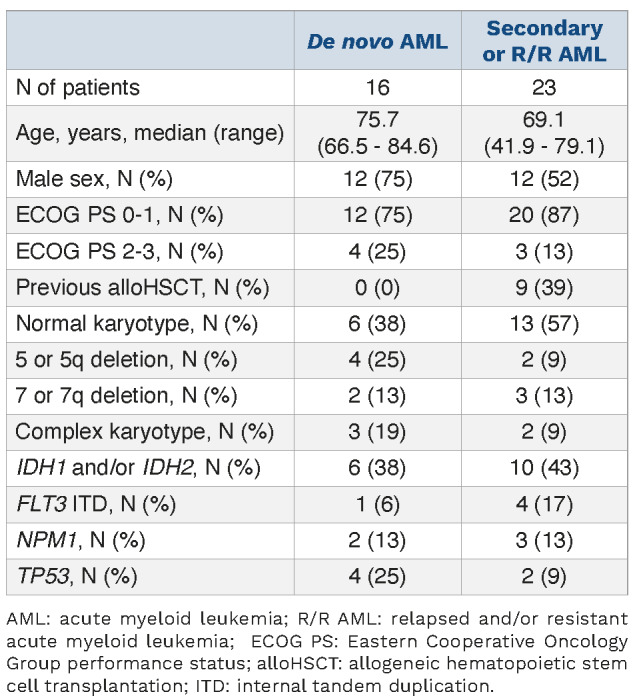
Between February 2020 and January 2021, 41 participants were recruited for the first part of the VenEx trial to evaluate the feasibility, predictiveness, and best cut-off value for drug sensitivity testing to venetoclax (Figure 1B). Screening failed in two participants, in one case because of uncontrolled infection and in the other because of a low bone marrow blast count (6%). Of the eligible participants, 16 had de novo AML, 15 had R/R AML and eight had secondary AML. All participants with secondary AML had an antecedent myelodysplastic syndrome or chronic myelomonocytic leukemia previously treated with a hypomethylating agent, chemotherapy or both and were analyzed together with the R/R participants. The patients’ characteristics are presented in Table 1. Of participants with de novo AML, 75% (12/16) achieved CR/CRi, while 39% (9/23) of those with secondary or R/R AML did so. The overall response rate (CR, CRi or MLFS) was 88% (14/16) for de novo AML and 52% (12/23) for secondary or R/R AML (Online Supplementary Table S3).
Drug sensitivity testing was technically successful in 38/39 participants treated with venetoclax–azacitidine. In one participant, the leukemic blasts were not robustly identified using the flow cytometry assay because of low CD34+ and CD117+ cell counts (< 2%), which was likely the result of hemodilution. One participant died of pneumonia during cycle 1 on day 13. Thus, the in vivo/ex vivo correlation was evaluable in 37 participants (Figure 1B). The median cell viability of the bone marrow mononuclear cells was 90% after mononuclear cell separation and 75% after 48 hours of incubation in CM (Online Supplementary Figure S5A). A minor decrease in cell viability was observed after 48 hours of incubation in shipped samples processed the following morning when compared to samples processed on the same day (79% vs. 66%) (Online Supplementary Figure S5B, C). Importantly, decreased viability did not affect ex vivo venetoclax sensitivity (Online Supplementary Figure S5D, E). These results demonstrate that drug testing can be performed in a clinical context with a high success rate.
Table 1.
Patients’ characteristics.
Culture conditions and method of assessing sensitivity influence venetoclax responses
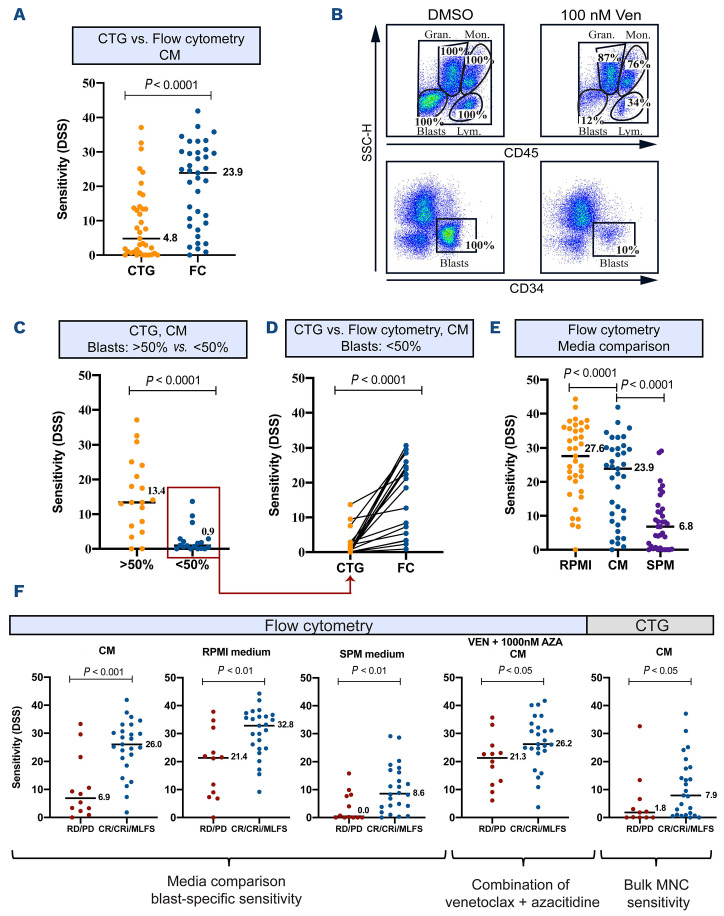
For drug sensitivity testing, 20 mL of bone marrow or 30 mL of peripheral blood were shipped to the central laboratory and ex vivo venetoclax sensitivity was assessed with different methods and culture conditions. DSS derived from the area under the dose-response curves indicated efficacy (Figure 1A, Online Supplementary Figure S3). Flow cytometry (blast-specific sensitivity) and CTG (bulk mononuclear cell sensitivity) assays were used to analyze ex vivo venetoclax sensitivity from the trial participants’ samples in CM. Bulk sensitivity assessed using CTG was significantly lower than the sensitivity determined by the blast-specific flow cytometry assay (median DSS: 4.8 vs. 23.9, respectively, P<0.0001) (Figure 2A). Flow cytometry showed that monocytic and granulocytic cells were resistant to venetoclax, causing decreased bulk sensitivity in the CTG assay (Figure 2B). Accordingly, most samples with blast counts of <50% were resistant to venetoclax in the CTG assay (median DSS: 0.9 vs. 13.4) (Figure 2C, Online Supplementary Figure S6). Thus, for the samples with low blast counts, CTG measurement provided a resistant phenotype, even though the blasts were sensitive to venetoclax when assessed by flow cytometry (Figure 2D).
To gain insight into the influence of cell culture conditions, cells were cultured in three different media (RPMI, CM and SPM), and venetoclax sensitivity was assessed using flow cytometry. After 48 hours, cell viability in the DMSO control was similar to that in all types of media (70-76%) (Online Supplementary Figure S7A). The number of CD14+ cells increased in all types of media during the 48 hours of culture, whereas the number of CD34+ cells increased significantly only in the SFEM II medium supplemented with FLT3, stem cell factor and thrombopoietin (SPM) (Online Supplementary Figure S7B). In RPMI medium, the blasts were highly sensitive to venetoclax, whereas in CM, the efficacy of venetoclax was lower (median DSS: 27.6 vs. 23.9, P<0.0001) (Figure 2E). The sensitivity to venetoclax was drastically lower when cells were cultured in the SPM medium (median DSS: 6.8, P<0.0001) (Figure 2E). Median venetoclax dose-response curves for each assay are presented in Online Supplementary Figure S8.
We explored further whether specific genotypic or phenotypic features of the blasts correlated with venetoclax sensitivity in different media. In all genotypic and phenotypic subgroups blasts exhibited the highest venetoclax sensitivity in RPMI medium, less sensitivity in CM and the lowest in SPM medium (Online Supplementary Figure S9A). In all three media, blasts with SRSF2 mutations showed increased ex vivo sensitivity to venetoclax compared to wildtype blasts. In contrast, blasts in samples in which the blast phenotype was defined as CD34+CD38– were more resistant to venetoclax (Online Supplementary Figure S9B, Online Supplementary Table S4). Together, these findings demonstrate that the cell viability assays and cell culture conditions substantially affect the ex vivo efficacy of venetoclax, whereas the genotype or immunophenotype associated with ex vivo venetoclax responses remains similar across all types of media.
Blast-specific venetoclax sensitivity in conditioned medium provides best response prediction
After the first 39 participants had been evaluated for treatment response, we examined which assay and medium provided the best separation of venetoclax-azacitidine treatment outcomes as defined by cumulative overall response (CR/CRi/MLFS) versus resistant disease during the first three treatment cycles. The best separation of non-responding and responding participants occurred when blast-specific venetoclax sensitivity was measured using flow cytometry in CM (median DSS: 6.9 vs. 26.0, P<0.001) (Figure 2F). When the ex vivo/in vivo correlation was assessed using CTG, several participants who responded to treatment were resistant to venetoclax ex vivo (Figure 2F). Similarly, the cytokine-rich SPM medium yielded false-resistant phenotype predictions in blast-specific flow cytometry measurements. In contrast, the overall sensitivity was higher in RPMI medium, leading to increased ex vivo venetoclax sensitivity in samples from patients who failed to achieve a clinical response. Considering that patients received venetoclax-azacitidine, we also assessed the ex vivo efficacy of the combination by flow cytometry by adding 300 nM or 1,000 nM of azacitidine to the venetoclax-containing wells across the entire concentration range in CM. We observed that adding azacitidine increased the sensitivity of the blasts from the participants with in vivo-resistant AML. Importantly, ex vivo testing of the venetoclax-azacitidine combination led to decreased predictive accuracy (Figure 2F, Online Supplementary Figure S10A). We also evaluated whether the increased sensitivity was restricted to a particular phenotype or genotype but could not detect correlations (Online Supplementary Figure S10B). These results indicate that venetoclax sensitivity measured using a blast-specific flow cytometry assay and CM provides the best distinction between responding and non-responding patients.
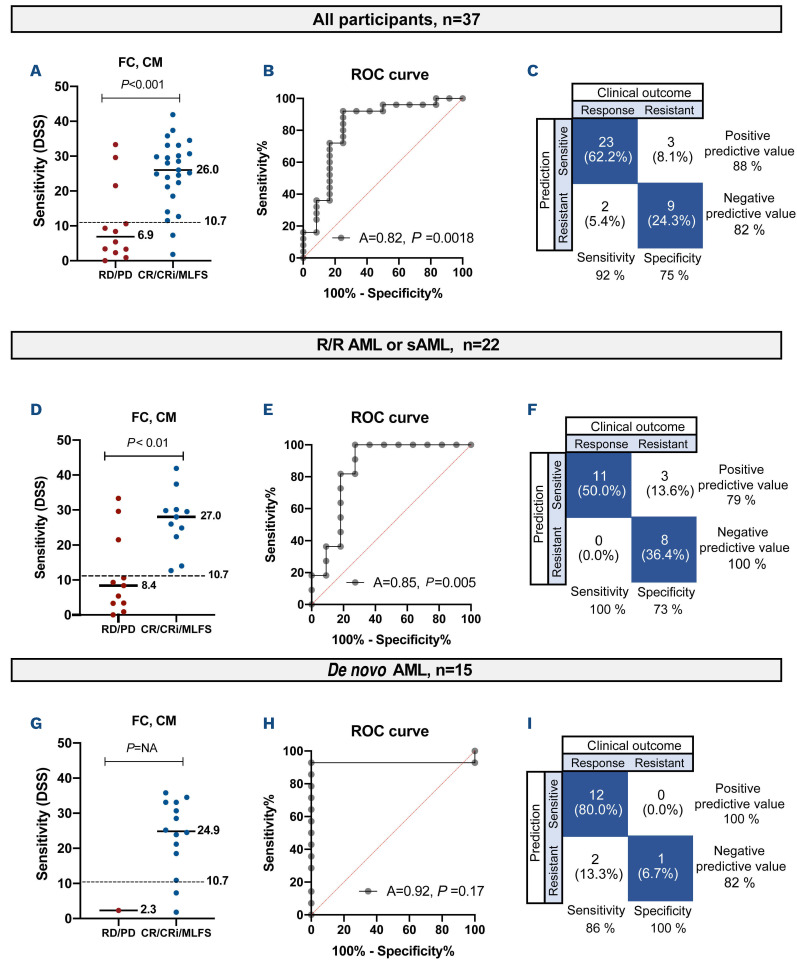
Using receiver operating characteristic (ROC) curve analysis, the greatest area under the ROC curve (AUROC = 0.82) was obtained for blast-specific venetoclax sensitivity in CM (Online Supplementary Table S5). Using a DSS threshold of 10.7, the test’s sensitivity was 92%, its specificity was 75%, and its positive predictive value (identification of patients as re-sponders) was 88% (Figure 3A-C). In the R/R cohort, the test’s positive predictive value was 79%, and no false predictions of resistance were observed (Figure 3D-F). In de novo AML, all but one participant achieved treatment response, and thus, venetoclax sensitivity testing produced limited additional value for de novo participants (Figure 3G-I).
Figure 2.
Comparison of venetoclax sensitivity among different assays and cell culture media. (A) Venetoclax sensitivity of trial participants (n=37) assessed using CellTiterGlo® (CTG) and flow cytometry (FC) assays and expressed as measured by the drug sensitivity score. The line represents the median. The P value was calculated using a two-tailed Wilcoxon matched-pairs signed-rank test. (B) FC scatter plot of a sample treated with dimethylsulfoxide (DMSO) control or 100 nM of venetoclax for 48 h. Blasts, lymphocytes, monocytic cells, and granulocytic cells are gated in the upper row plots using side scatter versus CD45, and in the lower row blasts are gated using CD34. Absolute numbers of viable cells present after treatment with 100 nM of venetoclax in each gate were normalized to the number of cells present in the wells containing the DMSO control. (C) Comparison of sensitivity to venetoclax between samples with blast counts <50% (n=19) and >50% (n=18), assessed using the CTG assay in conditioned medium. The line represents the median. The P value was calculated using the Mann-Whitney U test. (D) Sensitivity to venetoclax of samples with blast counts <50% (n=19), assessed using the CTG or FC assay. The line represents the median. The P value was calculated using a two-tailed Wilcoxon matched-pairs signed-rank test. (E) Blast-specific venetoclax sensitivity measured using FC in three different cell culture media. The line represents the median. The P value was calculated using a two-tailed Wilcoxon matched-pairs signed-rank test. (F) The drug sensitivity scores for venetoclax determined using different assays and media and plotted for each participant (n=37). Participants were divided into responders (n=25) and non-responders (n=12). The line represents the median. The P value was calculated using a one-tailed Mann-Whitney U test. CM: conditioned medium; SSC: side scatter; Gran: granulocytes; Mon: monocytes; Lym: lymphocytes; DSS: drug sensitivity score; RD: refractory disease; PD: progressive disease; CR: complete remission; CRi: complete remission with incomplete blood recovery; MLFS: morphological leukemia-free state; AZA: azacitidine.
Figure 3.
Determination of the predictive value of drug sensitivity testing in different cohorts of patients. (A) The sensitivity of each participant to venetoclax, determined using flow cytometry and conditioned medium and expressed as a drug sensitivity score (DSS). The participants are divided into responders and non-responders. The dashed line at DSS 10.7 represents the best cutoff value. The P value was calculated using a one-tailed Mann-Whitney U test. (B) Receiver operating characteristic (ROC) curve analysis of DSS and clinical response using the Wilson-Brown method. (C) Sensitivity, specificity, positive predictive value and negative predictive value of the test when using the cutoff value of DSS 10.7, illustrated in a confusion matrix. (D) DSS versus clinical response in relapsed/refractory (R/R) or secondary acute myeloid leukemia (sAML). The P value was calculated using a one-tailed Mann-Whitney U test. (E) ROC analysis of R/R or sAML. (F) Predictive value of the test in R/R or sAML. (G) DSS versus clinical response in de novo AML. The P value was calculated using a one-tailed Mann-Whitney U test. (H) ROC analysis of de novo AML. (I) Predictive value of the test in de novo AML. DSS: drug sensitivity score; FC: flow cytometry; CM: conditioned medium; RD: refractory disease; PD: progressive disease; CR: complete remission; CRi: complete remission with incomplete blood recovery; MLFS: morphological leukemia-free state.
Of the de novo participants exhibiting ex vivo sensitivity (DSS >10.7), 92% (11/12) had a CR/CRi, whereas of participants with secondary or R/R AML, 57% (8/14) had a CR/CRi (Online Supplementary Table S3). The overall response rate (CR, CRi, or MLFS) for ex vivo drug-sensitive de novo AML was 100% (12/12), whereas it was 79% (11/14) for R/R or secondary AML.
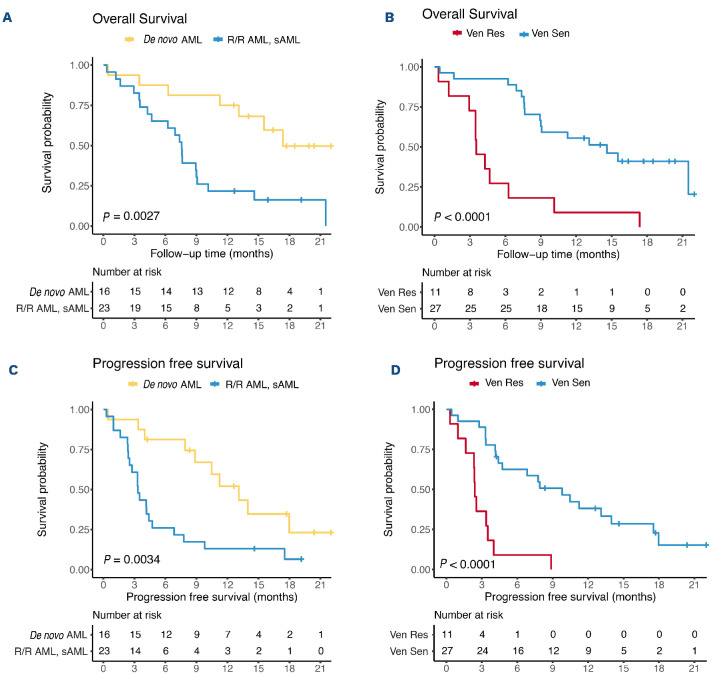
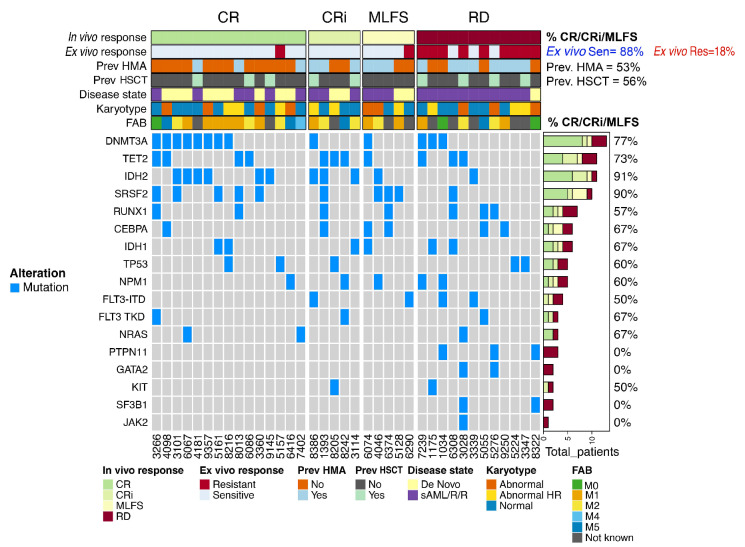
Ex vivo venetoclax sensitivity predicts longer survival
At a median follow-up of 18.6 months, the median overall survival of patients with de novo AML was 17.4 months (95% CI: NR) whereas that for patients with secondary or R/R AML was 7.6 months (95% CI: 6.5-8.6 months) (Figure 4A, Online Supplementary Figure S11). These results are similar to those in previous reports.12,13 Notably, ex vivo venetoclax sensitivity (determined by flow cytometry in CM) also correlated with survival: the median overall survival for patients with DSS <10.7 (ex vivo-resistant) was 3.5 months (95% CI: 2.5-4.6 months), and that for patients with DSS >10.7 (ex vivo-sensitive) was 14.6 months (95% CI: 8.8-20.4 months, P<0.001) (Figure 4B). Moreover, greater sensitivity correlated with longer survival (r=0.518, P<0.001) (Online Supplementary Figure S12). The median progression-free survival for patients with de novo AML was 13.1 months (95% CI: 8.7-17.5 months) whereas that for patients with secondary or R/R AML was 3.3 months (95% CI: 2.5-4.2 months) (Figure 4C). The median progression-free survival for ex vivo-resistant patients was 2.4 months (95% CI: 2.2-2.6 months) and that for ex vivo-sensitive patients was 9.8 months (95% CI: 5.5-14.1 months) (Figure 4D). As reported earlier,15,24 in our cohort, patients harboring IDH2 or SRSF2 mutations had a high likelihood of responding (91% and 90%, respectively), whereas participants with PTPN11 (n=3) failed to respond to the treatment (Figure 5). Importantly, other genetic alterations did not clearly associate with treatment responses. In comparison, the use of drug sensitivity testing in this cohort showed that 88% of ex vivo-sensitive patients responded to the treatment.
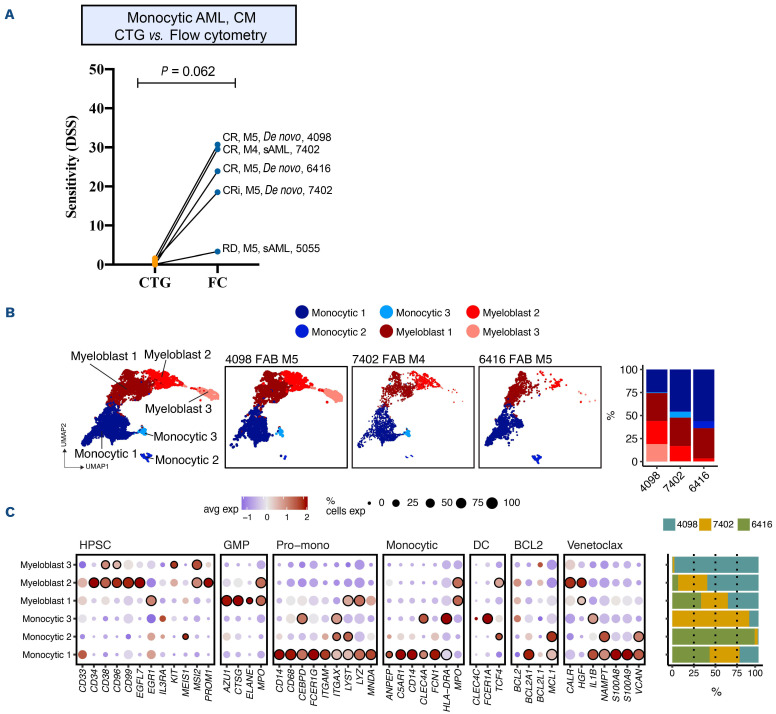
Progenitor cell sensitivity associates with venetoclax response in monocytic acute myeloid leukemia
We and others have previously shown that monocytic AML samples (M4/M5 according to the French-American-British [FAB] classification) are resistant to venetoclax ex vivo.10,25 Furthermore, Pei et al. found a correlation between FAB M5 phenotype and in vivo venetoclax resistance.16 In our trial, four participants had FAB M5 AML, and one had M4 AML. The patients’ characteristics and treatment responses are presented in Online Supplementary Table S6. Confirming the earlier ex vivo findings,10 monocytic samples were resistant to venetoclax when using the CTG assay on bulk bone marrow (Figure 6A). However, four of the five participants achieved remission. Intriguingly, we observed that monocytic disease has distinctive cell population-specific response patterns. The blast cell fraction (defined by CD34 or CD117 positivity) exhibited vene-toclax sensitivity in all cases that achieved a clinical response (Figure 6A, Online Supplementary Table S6). In contrast, the monocytic/granulocytic cell fraction was less sensitive in all samples (Online Supplementary Figure S13). Accordingly, the CD34+ cell fraction enriched from two samples that had a high number of monocytic/granulo-cytic cells exhibited increased venetoclax sensitivity in the CTG assay (Online Supplementary Figure S14).
To assess whether the gene expression signature could explain the distinct venetoclax responses, we performed single-cell RNA sequencing on two monocytic samples and one myelomonocytic sample. Monocytic cells expressing CD14 accounted for 25-50% of the leukemic cells in each sample and selectively expressed MCL1, BCL2A1, and S100A9/S100A9 but not BCL2 (Figure 6B, C). In contrast, CD34 progenitor cells showed increased BCL2 expression accompanied by low BCL2A1 and MCL1 expression, which may explain the observed sensitivity to venetoclax. Together, these findings suggest that the less mature progenitor cells of monocytic AML samples are sensitive to venetoclax ex vivo and progenitor cell sensitivity also correlates with clinical responses.
Discussion
This interim analysis illustrates the technical feasibility of integrating venetoclax drug response profiling into clinical practice for patients with AML. Furthermore, the study demonstrates that the correlation between in vivo and ex vivo responses is profoundly affected by the selected cell culture medium and the method of assaying viability. In the first stage of the trial, we determined the optimal cutoff value for venetoclax sensitivity retrospectively and observed the best in vivo/ex vivo correlation using CM coupled with a blast-specific flow cytometry assay.
We observed that response evaluation using bulk bone marrow was associated with false predictions of resistance. Our flow cytometry data demonstrated that different cell populations have distinct sensitivity to venetoclax, and thus, less sensitive cell populations - especially monocytic and granulocytic ones - blur the sensitivity of blasts. Earlier studies assessing bulk mononuclear cell drug sensitivity demonstrated that monocytic AML samples have reduced sensitivity to venetoclax.25,26 Accordingly, in a retrospective analysis of 100 patients with newly diagnosed AML, patients with FAB M5 AML were less likely to get a clinical response.16 In our cohort, four out of five participants with AML FAB subtypes M4 and M5 achieved remission. Blast-specific ex vivo venetoclax sensitivity was associated with treatment response in all participants, whereas all samples were resistant when bulk sample sensitivity was assessed using CTG. Interestingly, scRNA sequencing of three monocytic/myelomonocytic single-cell RNA samples showed that the expression of several genes associated with venetoclax resistance based on preclinical studies, such as BCL2A125 and S100A8/S100A9,27 were observed mainly in mature monocytes. In contrast, in primitive blasts, the expression of BCL2 was higher and the expression of MCL1 was lower. The distinct venetoclax sensitivity of monocytic cells and blasts was also reflected in individual participants whose monocytosis persisted after blast clearance (Online Supplementary Figure S15, Supplementary Table S6). Although our sample size is limited, our results highlight the importance of assessing drug sensitivity and gene expression at the progenitor cell level, particularly in monocytic samples and samples with low blast counts.-
Figure 4.
Overall survival based on disease state and ex vivo sensitivity to venetoclax. (A) The median overall survival for de novo acute myeloid leukemia (AML) versus secondary AML (sAML) or relapsed/refractory AML (R/R AML) was 17.4 months (95% confidence interval [95% CI]: not reached) and 7.6 months (95% CI: 6.5-8.6), respectively. (B) The median overall survival for participants with a drug sensitivity score <10.7 (ex vivo-resistant) versus >10.7 (ex vivo-sensitive) was 3.5 months (95% CI: 2.5-4.6) and 14.6 months (95% CI: 8.8-20.4), respectively. Participants alive at the data cutoff day were censored. The median follow-up time was 18.6 months. (C) The median progression-free survival for de novo AML versus sAML or R/R AML was 13.1 months and 3.3 months, respectively. (D) The median progression-free survival for ex vivo drug-resistant versus ex vivo drug-sensitive patients was 9.8 versus 2.4 months, respectively. Progression-free survival was defined as the number of days from the date of the first dose to the date when the patient was deemed refractory or the earliest evidence of relapse or death. Ven Res: resistant to venetoclax; Ven Sen, sensitive to venetoclax.
The effect of the cell culture medium was critical when assessing blast-specific ex vivo responses. Sensitivity to venetoclax was significantly lower in the SPM medium supplemented with cytokines than in RPMI medium and CM. Some false predictions of resistance might be due to several cytokines (including FLT3L, stem cell factor, and thrombopoietin) and other supplements in the SPM medium, leading to the activation of kinase signaling pathways (including, for example, the JAK-STAT and RAS-ERK pathways) associated with venetoclax resistance.11,15,28 Thus, SPM medium may artificially “desensitize” cells ex vivo, which are in fact sensitive in vivo in the bone marrow compartment. In contrast, the overall sensitivity was higher in RPMI medium, leading to false predictions of sensitivity. This might be due to the lack of cytokines and other factors in this medium, which may decrease the apoptotic threshold of the blasts compared to a more protective bone marrow environment in vivo. These findings suggest that CM can be used in venetoclax sensitivity testing for primary patients’ samples, based on the superior in vivo/ex vivo correlation. Importantly, most pre-clinical studies utilize an ex vivo venetoclax sensitivity assessment of cell lines and primary patients’ samples to study resistance mechanisms. Based on our findings, the mechanisms identified might be highly method-dependent; thus, methods capable of mimicking in vivo responses and assessing blast-specific responses might increase the relevance of these studies in the future.
Newly diagnosed AML patients harboring IDH1/IDH2 and NPM1 mutations have shown high response rates and favorable survival with venetoclax and hypomethylating agent therapy, whereas patients with RAS and TP53 mutations have worse outcomes.12,15,29 Similar observations have been made in R/R AML, but the data are more li-mited.13,14 Thus, venetoclax sensitivity testing may help to guide therapy for patients who lack the mutation associated with treatment response, particularly in the R/R setting. We observed that IDH2 and SRSRF2 mutations were accompanied by high treatment response rates (overall response rates, 91% and 90%, respectively). In our cohort, NPM1 mutation was not predictive of treatment response (overall response rate, 60%), whereas PTPN11 was associated with resistance. The small sample size and heterogeneous population of patients might have diminished the observed predictive values of the mutations, but significantly, drug testing was able to predict responses across the entire cohort of patients, with a positive predictive value of 88%. Importantly, ex vivo drug sensitivity testing could predict not only the treatment response, but also survival: the overall survival for ex vivo-drug-resistant participants was 3.5 months, whereas patients showing ex vivo drug sensitivity had an overall survival of 14.6 months (P<0.001).
Figure 5.
Genetic predictors of response. Treatment responses, drug testing predictions, previous treatment with a hypomethylating agent, prior allogeneic stem cell transplantation, disease state, French-American-British subtype and recurrent mutations at the time of the screening presented in an OncoPrint heatmap. Percentages correspond to the number of responders with a specific feature. CR: complete remission; CRi: complete remission with incomplete blood recovery; MLFS: morphological leukemia-free state; RD: resistant disease; Sen: sensitive; Res: resistant; HMA: hypomethylating agent; HSCT: allogeneic hematopoietic stem cell transplantation; Prev: previous; FAB: French-American-British; ITD: internal tandem duplication; TKD: tyrosine kinase domain; sAML/R/R: secondary or relapsed and/or resistant acute myeloid leukemia.
Figure 6.
Cell populations in monocytic acute myeloid leukemia samples have distinct drug response paterns and gene expression profiles. (A) Drug sensitivity score of five myelomonocytic/monocytic samples measured using CellTiterGlo® or flow cytometry assays in conditioned medium. Clinical responses (complete remission/complete remission with incomplete blood recovery/resistant disease) are annotated in the graph. The P value was calculated using a two-tailed Wilcoxon matched-pairs signed-rank test. (B) Uniform Manifold Approximation and Projection (UMAP) representation of monocytic and progenitor cells from three bone marrow samples profiled by single-cell RNA sequencing. The samples were taken from three patients with acute myeloid leukemia before venetoclax-azacitidine treatment. The bar plot on the right shows the proportion of cell phenotypes in each sample. (C) Expression of a set of canonical markers used to identify monocytic and progenitor cell populations. Expression of BCL2 family genes and genes associated with response to venetoclax based on preclinical studies. Dot size corresponds to the percentage of cells expressing a given gene in a given cluster, and dot color corresponds to the average expression of a given gene in a given cluster. Circled dots are differentially expressed in the cluster (Padj<0.05, Bonferroni corrected t test). The clusters are the same as shown in panel (B), and their distributions across patients are shown in the bar plot on the right. DSS: drug sensitivity score; AML: acute myeloid leukemia; CM: conditioned medium; CTG: CellTiterGlo®; sAML: secondary AML; CR: complete remission; CRi: complete remission with incomplete blood recovery; RD: resistant disease; FAB: French-American-British; HPSC: hematopoietic stem and progenitor cell; GMP: granulocyte-monocyte progenitor; Pro-mono: pro-monocyte; DC: dendritic cells; BCL2: BCL2 family gene; Venetoclax: genes associated with venetoclax resistance based on preclinical studies.
Although drug testing provided promising results, some challenges exist. First, adequate quality controls, collection, and prompt delivery of fresh tumor material from sites require precise coordination of clinical units, laboratories, and logistics. Second, we observed two false predictions of resistance in de novo participants. While we observed that sensitivity to venetoclax predicted treatment response better than combinatory venetoclax-aza-citidine sensitivity, it is probable that our short assay fails to capture azacitidine sensitivity and a possible apopto-sis-priming effect adequately. Third, the assay cannot identify small, resistant subclones that might be selected, leading to rapid relapse. Another potential caveat is the fact that ex vivo sensitivity testing was conducted in a single laboratory. The forthcoming pan-Nordic LD-VenEx trial (Eudra-CT 2020-005461-14) will evaluate the feasibility of this approach in a multilaboratory setting.
The second part of the trial is still underway. Reflecting the high response rates in the de novo participants, the second part of the trial includes all de novo patients in the study treatment, irrespective of venetoclax sensitivity. However, ex vivo venetoclax sensitivity is observationally tested. For R/R and secondary AML patients, venetoclax sensitivity testing is used for the selection of patients, and only participants exhibiting ex vivo sensitivity (DSS >10.7) receive study therapy.
In summary, although new AML therapy options have the potential to improve patients’ outcomes, the challenge remains to identify the factors predicting response and to target therapies to only those patients who could be expected to benefit from them. In the interim analysis of our VenEx trial, we showed that ex vivo testing for venetoclax sensitivity was feasible in AML with a high success rate. In addition, our results provide essential data to be used in preclinical studies exploring venetoclax sensitivity and resistance. Nevertheless, novel prospective trials are needed to assess the usability of ex vivo drug sensitivity testing for other therapies as well as to repurpose anticancer agents to further personalize patients’ care.
Supplementary Material
Acknowledgments
The authors would like to thank the patients, their families, and physicians for their participation in the trial. We especially want to express gratitude to VenEx study nurses and coordinators: Sari Nikkola, Päivi Pellikka, Carita Rantanen, Satu Määttä-Halonen, Kirsi Kvist-Mäkelä, Elina Ellilä, Jenni Raali, and Saara Vaalas. We acknowledge the personnel at the FIMM Single Cell Analytics Unit and FIMM High Throughput Biomedicine Unit, which are hosted by the University of Helsinki and supported by HiLIFE and Biocenter Finland, for their expert technical assistance.
Funding Statement
Funding: This study received funding from the Finnish Medical Foundation, Cancer Foundation Finland, Helsinki University Hospital Comprehensive Cancer Center, Helsinki University, iCAN – Digital Precision Medicine and FiCAN South. HK and MK are supported by the Foundation for the Finnish Cancer Institute. SKy received support from the Finnish Medical Foundation.
References
- 1.Hourigan CS, Karp JE. Personalized therapy for acute myeloid leukemia. Cancer Discov. 2013;3(12):1336-1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Estey E, Levine RL, Löwenberg B. Current challenges in clinical development of “targeted therapies”: the case of acute myeloid leukemia. Blood. 2015;125(16):2461-2466. [DOI] [PubMed] [Google Scholar]
- 3.Malani D, Kumar A, Brück O, et al. Implementing a functional precision medicine tumor board for acute myeloid leukemia. Cancer Discov. 2022;12(2):388-401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tyner JW, Tognon CE, Bottomly D, et al. Functional genomic landscape of acute myeloid leukaemia. Nature. 2018;562(7728):526-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kornauth C, Pemovska T, Vladimer GI, et al. Functional precision medicine provides clinical benefit in advanced aggressive hematologic cancers and identifies exceptional responders. Cancer Discov. 2022;12(2):372-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martínez-Cuadrón D, Gil C, Serrano J, et al. A precision medicine test predicts clinical response after idarubicin and cytarabine induction therapy in AML patients. Leuk Res. 2019;76:1-10. [DOI] [PubMed] [Google Scholar]
- 7.Letai A, Bhola P, Welm AL. Functional precision oncology: testing tumors with drugs to identify vulnerabilities and novel combinations. Cancer Cell. 2022;40(1):26-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennett TA, Montesinos P, Moscardo F, et al. Pharmacological profiles of acute myeloid leukemia treatments in patient samples by automated flow cytometry: a bridge to individualized medicine. Clin Lymphoma Myeloma Leuk. 2014;14(4):305-318. [DOI] [PubMed] [Google Scholar]
- 9.Snijder B, Vladimer GI, Krall N, et al. Image-based ex-vivo drug screening for patients with aggressive haematological malignancies: interim results from a single-arm, open-label, pilot study. Lancet Haematol. 2017;4(12):e595-e606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuusanmäki H, Leppä A-M, Pölönen P, et al. Phenotype-based drug screening reveals association between venetoclax response and differentiation stage in acute myeloid leukemia. Haematologica. 2020;105(3):708-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karjalainen R, Pemovska T, Popa M, et al. JAK1/2 and BCL2 inhibitors synergize to counteract bone marrow stromal cell-induced protection of AML. Blood. 2017;130(6):789-802. [DOI] [PubMed] [Google Scholar]
- 12.DiNardo CD, Jonas BA, Pullarkat V, et al. Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N Engl J Med. 2020;383(7):617-629. [DOI] [PubMed] [Google Scholar]
- 13.DiNardo CD, Maiti A, Rausch CR, et al. 10-day decitabine with venetoclax for newly diagnosed intensive chemotherapy ineligible, and relapsed or refractory acute myeloid leukaemia: a single-centre, phase 2 trial. Lancet Haematol. 2020;7(10):e724-e736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stahl M, Menghrajani K, Derkach A, et al. Clinical and molecular predictors of response and survival following venetoclax therapy in relapsed/refractory AML. Blood Adv. 2021;5(5):1552-1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DiNardo CD, Tiong IS, Quaglieri A, et al. Molecular patterns of response and treatment failure after frontline venetoclax combinations in older patients with AML. Blood. 2020;135(11):791-803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pei S, Pollyea DA, Gustafson A, et al. Monocytic subclones confer resistance to venetoclax-based therapy in patients with acute myeloid leukemia. Cancer Discov. 2020;10(4):536-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cherry EM, Abbott D, Amaya M, et al. Venetoclax and azacitidine compared with induction chemotherapy for newly diagnosed patients with acute myeloid leukemia. Blood Adv. 2021;5(24):5565-5573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spinner MA, Aleshin A, Santaguida MT, et al. Ex vivo drug screening defines novel drug sensitivity patterns for informing personalized therapy in myeloid neoplasms. Blood Adv. 2020;4(12):2768-2778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seyfried F, Demir S, Hörl RL, et al. Prediction of venetoclax activity in precursor B-ALL by functional assessment of apoptosis signaling. Cell Death Dis. 2019;10(8):571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhatt S, Pioso MS, Olesinski EA, et al. Reduced mitochondrial apoptotic priming drives resistance to BH3 mimetics in acute myeloid leukemia. Cancer Cell. 2020;38(6):872-890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferrara F, Barosi G, Venditti A, et al. Consensus-based definition of unfitness to intensive and non-intensive chemotherapy in acute myeloid leukemia: a project of SIE, SIES and GITMO group on a new tool for therapy decision making. Leukemia. 2013;27(5):997-999. [DOI] [PubMed] [Google Scholar]
- 22.Yadav B, Pemovska T, Szwajda A, et al. Quantitative scoring of differential drug sensitivity for individually optimized anticancer therapies. Sci Rep. 2014;4:5193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Döhner H, Estey E, Grimwade D, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424-447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stahl M, Menghrajani K, Derkach A, et al. Clinical and molecular predictors of response and survival following venetoclax therapy in relapsed/refractory AML. Blood Adv. 2021;5(5):1552-1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang H, Nakauchi Y, Köhnke T, et al. Integrated analysis of patient samples identifies biomarkers for venetoclax efficacy and combination strategies in acute myeloid leukemia. Nat Cancer. 2020;1(8):826-839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bisaillon R, Moison C, Thiollier C, et al. Genetic characterization of ABT-199 sensitivity in human AML. Leukemia. 2019;34(1):63-74. [DOI] [PubMed] [Google Scholar]
- 27.Karjalainen R, Liu M, Kumar A, et al. Elevated expression of S100A8 and S100A9 correlates with resistance to the BCL-2 inhibitor venetoclax in AML. Leukemia. 2019;33(10):2548-2553. [DOI] [PubMed] [Google Scholar]
- 28.Schumich A, Prchal-Murphy M, Maurer-Granofszky M, et al. Phospho-profiling linking biology and clinics in pediatric acute myeloid leukemia. HemaSphere. 2020;4(1):e312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pollyea DA, Pratz KW, Wei AH, et al. Outcomes in patients with poor-risk cytogenetics with or without TP53 mutations treated with venetoclax and azacitidine. Clin Cancer Res. 2022;28(24):5272-5279. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.