Abstract
This overview aimed to describe the situation of healthcare access in sub-Saharan Africa, excluding South Africa, during the COVID-19 pandemic. A PubMed® search from March 31, 2020, to August 15, 2022, selected 116 articles. Healthcare access and consequences of COVID-19 were assessed based on comparisons with months before its onset or an identical season in previous years. A general reduction of healthcare delivery, associated with the decline of care quality, and closure of many specialty services were reported. The impact was heterogeneous in space and time, with an increase in urban areas at the beginning of the pandemic (March-June 2020). The return to normalcy was gradual from the 3rd quarter of 2020 until the end of 2021. The impact of COVID-19 on the health system and its use was attributed to (a) conjunctural factors resulting from government actions to mitigate the spread of the epidemic (containment, transportation restrictions, closures of businesses, and places of entertainment or worship); (b) structural factors related to the disruption of public and private facilities and institutions, in particular, the health system; and (c) individual factors linked to the increase in costs, impoverishment of the population, and fear of contamination or stigmatization, which discouraged patients from going to health centers. They have caused considerable socio-economic damage. Several studies emphasized some adaptability of the healthcare offer and resilience of the healthcare system, despite its unpreparedness, which explained a return to normal activities as early as 2022 while the COVID-19 epidemic persisted. There appears to be a strong disproportion between the moderate incidence and severity of COVID-19 in sub-Saharan Africa, and the dramatic impact on healthcare access. Several articles make recommendations for lowering the socioeconomic consequences of future epidemics to ensure better management of health issues.
Keywords: COVID-19, pandemic, impact, health service, healthcare access, Sub-Saharan Africa
Background
The numbers of COVID-19 cases and deaths in sub-Saharan Africa (SSA), excluding South Africa which accounts for nearly half of the reported COVID-19 cases in SSA, have been lower than in other continents for reasons that remain unclear [1-6]. However, excess mortality (i.e., the number of deaths exceeding expected all-cause mortality) was particularly high - more than 100 times the mortality directly attributed to COVID-19 - suggesting a very strong deleterious synergy between morbidity factors [6, 7].
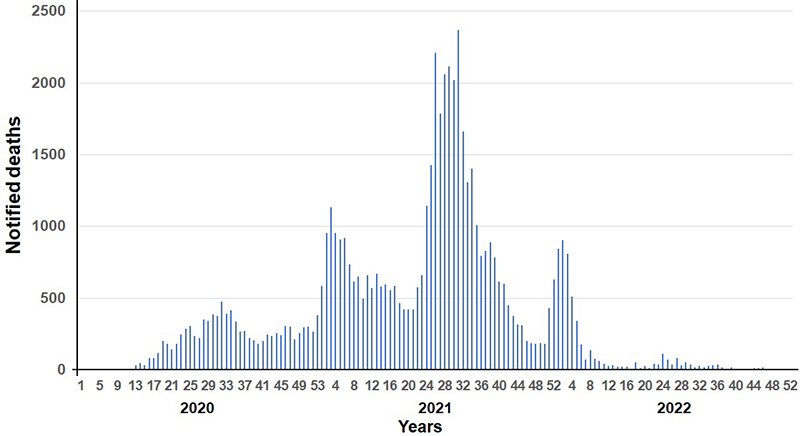
According to the COVID-19 dashboard edited and updated daily by the WHO Africa Regional Office, the first cases of COVID-19 were detected in Nigeria on February 28, 2020, and in Senegal on March 2, 2020, in travelers [8]. At least five epidemic waves occurred between March 2020 and August 2022, showing increasing incidence up to and including the fourth wave (November 2021 to March 2022), while mortality was highest during the second and third waves, from December 2020 to April 2021 (beta and then gamma variants), and June 2021 to September 2021 (delta variant), respectively (Figures 1 and 2). The first wave from March to June 2020, apparently mild, was accompanied by highly restrictive protective measures in most SSA countries [1], justified by international pressure and particularly pessimistic models of the impact of the pandemic on other diseases [9-15].
Figure 1. Weekly incidence of COVID-19 in the different regions of sub-Saharan Africa (except South Africa).
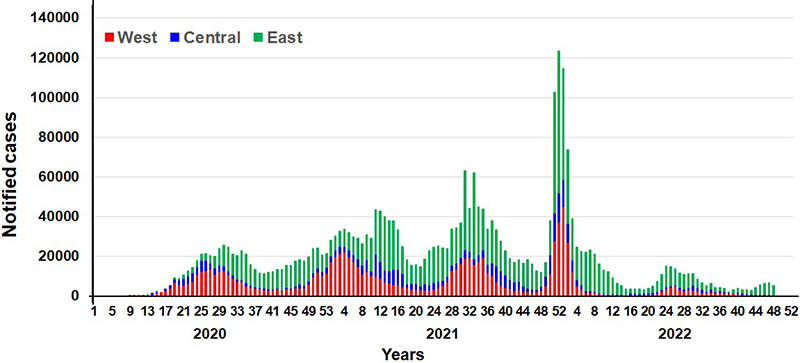
Figure 2. Weekly mortality of COVID-19 in the different regions of sub-Saharan Africa (except South Africa).
Access to healthcare requires that five specific dimensions be met: (a) availability, which reflects the adequacy between supply and demand, (b) accessibility, which implies geographical and logistical proximity between the patient and the health center, (c) accommodation, i.e. good quality services adapted to the needs of the public, (d) affordability for the population concerned, and (e) acceptability of the healthcare offered by people and health personnel [16].
A review of the literature during the COVID-19 pandemic period provided an overview of the situation of healthcare access and use of the healthcare system by the population in SSA countries excluding South Africa. This study aimed to identify the main impacts of reduced access to care by mentioning the causes identified by practitioners and researchers involved in the pandemic.
PubMed® was searched using the keywords "COVID, Africa, Public health, Impact" targeting publications published from March 31, 2020, to August 15, 2022. Articles were selected in two steps, without language restriction (Figure 3). In step one, the title, abstract, and keywords were used to determine studies on health service utilization and access to healthcare, excluding South Africa. Studies from South Africa were not included because of its more developed health system and significantly higher resources than other countries in the region. In step two, a review of the objectives and methodology of each preselected article led to the rejection of editorials, comments on other articles, and responses to comments, as well as studies with incomplete data (more than 20% missing data) or small sample sizes (less than 30 individuals) considered insufficiently representative. The analysis of the articles selected in step two focused on healthcare system access, healthcare utilization, and the specific constraints of some vulnerable groups (people living with HIV (PLHIV), tuberculosis (TB) patients, children, women of childbearing age, sex workers, etc.). It was assessed based on comparisons with the months prior to the onset of COVID-19 or an identical season in previous years. The indicators used were the number of vaccinations, visits to various medical services (including prenatal visits and hospital deliveries), hospitalizations, and screening and management of endemic or chronic diseases (malaria, tuberculosis, HIV, diabetes, hypertension, cancers, etc.).
Figure 3. Flow chart of selected articles used in the review.
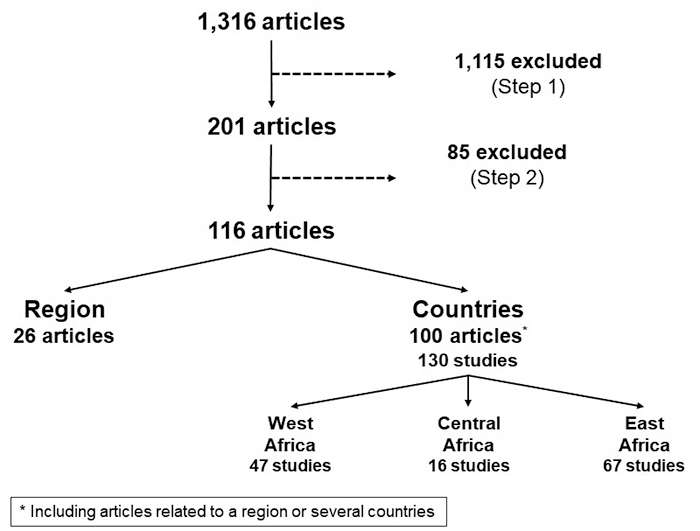
After the various stages of the selection process, 116 articles were retained out of the 1,316 identified at the first step (Figure 3). In addition to the 26 articles involving all or part of the sub-Saharan region, 100 articles described 130 studies conducted in 27 countries, more than half of which were in Ethiopia (16 studies), Ghana (11 studies), Kenya (14 studies), Nigeria (19 studies), and Uganda (11 studies) (Table 1). The central region of SSA was the least represented with 12% of the articles, versus 36% for West Africa and 52% for East Africa.
Table 1. List of SSA countries where studies regarding the impact of COVID-19 were carried out (111 publications selected on August 15, 2022).
| Countries | August 15, 2022 | References |
|---|---|---|
| Region | 26 | [1-3, 8, 10-13, 17-34] |
| Botswana | 1 | [19] |
| Burkina Faso | 4 | [19, 32-34] |
| Cameroon | 4 | [19, 35-37] |
| Congo | 1 | [19] |
| Cote d'Ivoire | 2 | [34,38] |
| DR Congo | 3 | [33, 39, 40] |
| Ethiopia | 16 | [15, 19, 32, 41-54] |
| Ghana | 11 | [19, 55-64] |
| Guinea | 1 | [65] |
| Guinea Bissau | 1 | [34] |
| Kenya | 14 | [19, 30, 33, 56, 66-76] |
| Malawi | 4 | [30, 75, 77, 78] |
| Mali | 2 | [30, 79] |
| Mozambique | 5 | [19, 80- 83] |
| Namibia | 2 | [19, 84] |
| Niger | 1 | [85] |
| Nigeria | 19 | [15, 19, 32, 33, 70, 74, 86- 98] |
| Uganda | 11 | [9, 30, 50, 76, 99-105] |
| Rwanda | 3 | [19, 106, 107] |
| Senegal | 1 | [108] |
| Sierra Leone | 5 | [34, 50, 109-111] |
| Somalia | 1 | [6] |
| Soudan | 2 | [19, 75] |
| Tanzania | 3 | [15, 19, 50] |
| Zambia | 6 | [4, 15, 19, 112- 114] |
| Zimbabwe | 7 | [19, 77, 79, 115- 119] |
Impact of COVID-19 on healthcare access
During the COVID-19 epidemic, healthcare services suffered a dramatic decline. The reduction in patient flow, sometimes up to 70%, affected all medical and surgical units - with significant cancellations or postponements of urgent responses - as well as preventive medicine units affecting the entire population [17-19, 32, 35-37, 41, 57, 66-68, 80, 85-87, 99, 109], and delays in the supply of drugs [19]. The number of consultations and hospitalizations decreased mainly in the second quarter of 2020 and then gradually increased again [35, 42]. Hospitalizations seem to have been more affected than consultations [17, 42, 46], as well as urban versus rural health facilities [17].
Paradoxically, despite the pessimistic predictions of models anticipating a doubling of malaria deaths in case of service interruption, access to basic clinical services in charge of malaria diagnosis was little disrupted in most countries with moderate or high malaria burden in 2020 thanks to the implementation of an adapted response [13]. For example, in Ghana, the number of malaria consultations among children and pregnant women decreased in March and April 2020 but straightened after that [57]. In Uganda, there was no difference between the observed and expected number of consultations for confirmed or suspected malaria cases [100].
Many TB screening appointments were missed due to reduced attendance at health facilities, leading to decrease diagnosis and initiation of treatment [43, 44, 88, 112]. In Zambia, specific intervention measures have resulted in the resumption of consultations in July 2020 and normalization in September 2021 [112].
Many PLHIV have refrained from counseling regardless of the reason and have suspended antiretroviral therapy (ART) [69, 101-103]. However, in Uganda, the number of people receiving prevention of vertical transmission of HIV has rapidly stabilized [101].
Across the SSA, there has been a decline in access to sexual and reproductive health services, institutional delivery, antenatal care, family planning, and HIV care. An increase in teenage pregnancies has been reported [20]. In Mozambique, overall antenatal visits decreased as well as cesarean sections and hospital deliveries, while home deliveries increased [80]. In contrast, in Kinshasa (Democratic Republic of Congo) maternal health services and vaccinations were poorly affected [39].
Childhood vaccinations (BCG, diphtheria-tetanus-pertussis, measles-rubella) have fallen sharply, leading to a worrying reduction in immunization coverage, raising fears of a resurgence of these diseases [36, 38, 45, 58, 80, 89, 108]. After the first wave, the trend reversed and returned to pre-March 2020 levels [68, 89].
In specialty services, including cardiology, urology, rheumatology, radiology, oncology, ophthalmology, and dentistry, visits have declined by more than 50% or even stopped in some places [21, 39, 59, 60, 65, 90-92, 116, 117].
People with chronic diseases had great difficulty accessing essential medicines during the COVID-19 lockdown, leading to deteriorating health conditions for most of them [69, 84, 94, 113].
The decline in blood donation began as soon as COVID-19 was announced, leading first to an interruption in mobile blood drive campaigns and then to the closure of blood donation centers in most countries [97]. In Nigeria, for example, the number of blood transfusions was dramatically reduced, partially offset by family replacement donations (FRDs) - the practice of drawing blood from a patient's family member. These decreases have been more pronounced for voluntary blood donations than for FDR, probably due to stronger incentives than pandemic-related constraints. However, it is not excluded that the family used a paid donor presented as an FDR [97].
The impact of COVID-19 on health services was very heterogeneous across localities - generally higher in urban than in rural areas - and over time, with a strong increase in the first months of the pandemic, and then according to the epidemic waves, which were not synchronous in different countries [3, 22, 35, 39, 42, 68, 89, 101, 112]. A comparative study using the same indicators and the same methodology showed the strong influence of the local context even if it is not always possible to determine the causes [77].
Vulnerable populations, including transgender people, sex workers, and drug users, were turned away from medical services, especially sexual and reproductive health services [81, 93].
However, several studies noted a gradual improvement between epidemic waves and a certain capacity to adapt the healthcare supply [39, 46, 57, 68, 82, 89, 100, 101, 112], and even a good resilience of the health system or the patients themselves [23, 47, 103, 105, 110, 113].
Access to healthcare was directly affected by the governmental measures taken to contain COVID-19 [24, 37, 38, 44, 48, 57, 69, 70, 84, 94, 99, 106, 108]. The implementation of physical distancing measures (containment, curfews, closure of businesses and places of entertainment or worship) impeded the movement of people and goods, and thus the seeking, provisioning, and delivery of healthcare, increasing tensions between healthcare personnel and patients [44, 57, 67, 69, 71, 99, 108, 116].
Inadequate health system preparedness was reported. It was due to (A) low availability of the health service, (B) inadequate resources and equipment, and (C) lack of appropriate testing, and therapeutic response for COVID-19 [26]. The reduction in staffing and the detour of human resources to meet the healthcare needs due to COVID-19 have led to a disorganization of the healthcare offer, in particular a prioritization of basic services with a general reduction in services or even suspension of care considered non-urgent (dentistry, physiotherapy, physical rehabilitation, etc.) [19, 57, 67, 99, 109]. In addition, there was a lack of personal protective equipment (disinfectant, masks, gloves, gowns, glasses, etc.) [57, 69]. This inability to meet the needs of the population has greatly contributed to their mistrust of institutions [25, 57].
A large proportion of the population refused to visit health centers for fear of contamination and stigma [19, 24, 25, 37, 38, 44, 48, 58, 64, 67, 70, 94-96, 99, 107, 109, 118, 119].
Many healthcare workers refused to care for patients for fear of contracting the virus themselves [37, 57, 50, 67, 78, 94, 99]. In addition, the increased workload and stigma they faced caused fatigue and stress, even depression, and increased absenteeism [78].
The exacerbation of pre-existing barriers (poverty, additional costs, and poor respect for confidentiality) has been highlighted by vulnerable populations to explain their reluctance to visit health centers [93, 118].
Finally, all the specific dimensions necessary to maintain healthcare access - as described by Penchansky and Thomas [16] were hampered by the pandemic (Table 2).
Table 2. Impact of COVID-19 on each of the components of healthcare access (definitions of healthcare access according to Penchansky & Thomas, 1981 [16]).
| Dimension | Definition | Obstruction due to COVID-19 | References |
|---|---|---|---|
| Availability | Adequacy between the supply and the demand | Closure of some health centers Organization worsening Health personnel overwork Shortage of health products Delay/cancellation of health interventions | [24, 28, 55, 61, 64, 67, 69, 74, 95, 102] |
| Accessibility | Relationship between the location of service or supply and the location of clients | Transportation restrictions and cost Confinement | [24, 44, 48, 55, 61, 64, 70, 71, 84, 94, 99, 106-108, 116] |
| Accommodation | Relationship between the service or supply resources, and the client’s ability and perception of their appropriateness | Complexity of COVID-19 protocols Disbelief from patients Reallocation of resources Bureaucracy | [26, 48, 61, 63, 64, 84, 93, 118, 119] |
| Affordability | Relationship between cost of services and client's income | Cost increase Loss of purchasing power | [33, 37, 44, 55, 70, 94, 96, 99] |
| Acceptability | Relationship between the client’s attitude and reaction and provider’s practice | Fear of contamination by COVID-19 Fear of being diagnosed positive Fear of stigma Loss of trust in health personnel Distrust of Western medicine Stress or depression Infodemic | [12, 19, 24, 25, 34, 37, 44, 48, 52, 55, 58, 61, 64, 67, 70, 74, 94, 95,107, 118, 119] |
Nearly all studies showed a sharp decline in healthcare activity and access during the early months of the pandemic, followed by a gradual return to normal starting in the third quarter of 2020 and continuing through the end of 2021 (Table 3). The heterogeneity of the impact was significant, both temporally - based on epidemic waves that did not occur simultaneously across SSA - and spatially, according to different environmental and socioeconomic contexts. Although inadequate reporting and low frequency of reverse transcriptase-polymerase chain reaction (RT-PCR) testing of COVID-19 samples did not provide an accurate picture of the incidence and severity of the epidemic in SSA, no correlation appeared to exist with its impact on the healthcare system and its utilization. The causes remain speculative: differences in the socioeconomic environment, variable performance of the efficacy reporting system or the diagnosis and screening policy, and restrictive prevention measures [2, 3, 5]. However, it is possible to highlight that the incidence and mortality of the first wave, between March and June 2020, were barely noticeable, whereas they increased in the following waves (Figures 1 and 2), while healthcare access, dramatic at the beginning of the epidemic, tended to normalize. As soon as the first cases of COVID-19 appeared, drastic protective measures were taken in most countries: border closure, containment or curfew, travel and transportation bans, and business shutting down [1]. However, these measures were gradually reduced until they disappeared. It is questionable whether the governmental measures were successful in containing the epidemic in its early stages, or in delaying its expansion, whereas the gradual mitigation of the confinements from the second quarter of 2020 would have led to an increase in cases [1, 2, 5, 12].
Table 3. Decrease in access to health services in sub-Saharan Africa between April 2020 and June 2022 (expressed as % of activities excluding pandemic or wave of transmission).
| Countries | OMS-AFRO | Cameroon | Cote d'Ivoire | Ethiopia | Ghana | Guinea | Kenya | Malawi | Mozambique | Niger | Nigeria | Uganda | Rwanda | Senegal | Sierra Leone | Zambia | Zimbabwe | References |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Services | ||||||||||||||||||
| Immunization | -40- -60 | -26- -99 | +15- -12 | -11- -47 | -20 | -61 | -20 | -9- -16 | -42- -50 | [17, 36, 38, 45, 50, 63, 80, 85, 89, 101, 108] | ||||||||
| Outpatients | +1- -57 | -71 | -25 | -50 | [46, 65, 67, 103] | |||||||||||||
| Pediatric outpatients | -34- -52 | [27, 36] | ||||||||||||||||
| Inpatients | -10- -73 | -75 | -14 | -15 | [46, 65, 67, 109] | |||||||||||||
| Pediatric inpatients | -17 | -25 | -50 | -14 | -9 | [17, 35, 37, 77, 87, 99, 109] | ||||||||||||
| Family planning | -98- +47 | -50 | -28 | [20, 41, 46, 63, 80, 93] | ||||||||||||||
| Prenatal visits | -2- -6 | -34- -45 | -7 | -26 | -60 | [20, 27, 35, 36, 48, 80, 101] | ||||||||||||
| Stillbirth rate | +19 | +36 | -7 | [54, 99, 115] | ||||||||||||||
| Ophthalmology | -46 | [92] | ||||||||||||||||
| Emergencies | +19- -47 | [46, 54] | ||||||||||||||||
| Accidents | -36 | -41 | [54, 98] | |||||||||||||||
| Dialysis | -53 | [46] | ||||||||||||||||
| Deliveries | -2- -6 | -35 | -50 | -5 | -14 | [17, 20, 63, 86, 101, 115] | ||||||||||||
| Planned surgery | -92- -70 | [41, 116] | ||||||||||||||||
| Diabetes / HTA consultations | [39, 49] | |||||||||||||||||
| Malaria diagnosis | -3- -7 | -9 | -5 | [28, 57, 100, 107] | ||||||||||||||
| HIV consultations and/or decrease ART | -43 | -22 | -34 | -36 | [20, 28, 29, 54, 55, 79, 93, 102, 103, 112] | |||||||||||||
| Rabies consultations | -38- -45 | [38] | ||||||||||||||||
| TB diagnosis | -11 | -15 | -73 | -25 | -22 | [28, 43, 82, 88, 93, 110, 112] | ||||||||||||
| TB management | -17- -70 | -72 | [42-44, 88, 93] | |||||||||||||||
| Cancer diagnosis | -51- -99 | [54] |
In any case, the authors are unanimous in describing the socioeconomic disorganization caused by the government measures, making them unacceptable to the population to the point that they were quickly relaxed. Three types of factors explained the decline in healthcare access: conjunctural, linked to government measures for the mitigation of transmission; structural, resulting from the dysfunction of the health system; and individual, involving the reactions of health personnel and the population.
Conjunctural factors
The Public Health and Social Measures Severity (PHSM) index can be applied to the governmental response to the epidemic (e.g., mask bearing, closure of schools, offices, businesses, places of worship, and entertainment, and prohibition of international travel and transportation) to assess its impact on the epidemic [50]. A high PHSM index, which combines several restrictive or even coercive measures, leads to a general disorganization of the society that generates stress with numerous psychological, social, and economic consequences. It prevents access to health facilities, many of which were temporarily closed due to containment and transport restriction measures. In addition, the lack of supplies, including sanitary equipment and medicines, and the failure of many businesses and trades, especially in the informal sector which is a crucial part of the economy in SSA, has led to concerns, logistical constraints, and a loosening of social links [27, 32, 55, 74, 84, 101, 108, 114].
Government restrictions have been responsible for the loss of huge numbers of jobs, especially in the informal sector, and resources that have led to a dramatic decline in purchasing power and prevented patients from accessing basic healthcare, which is their sole responsibility in most SSA countries [38, 57, 61]. Increased costs, due to logistical constraints and shortages, have only exacerbated patient insolvency [22, 33, 44, 62, 70, 94, 99, ].
Finally, rumors (infodemia) from all sources, and misconceptions or misinformation about diseases and healthcare, contributed to discouraging people from attending health centers, but also to school dropout and a range of psychosocial consequences such as mental health disorders, domestic violence, and prostitution [25, 34, 38, 56-58, 66, 72, 73, 95, 104, 105, 120].
Structural factors
The overall unpreparedness of the health system (lack of availability of services, inadequate resources and equipment, insufficient testing and appropriate responses to the pandemic, including a shortage of personal protective equipment) was obvious and greatly accentuated the disorganization of the health system caused by conjunctural factors [14, 24-26, 37, 39, 44, 48, 50, 61, 63, 68, 69, 71, 74, 76, 78, 83, 84, 96, 99, 106, 108, 116, 118]. Added to this were the detour of resources [26, 28, 48, 119], an increase in overwork - due to the management of COVID-19 and the absenteeism of health workers who were ill, without transport or exhausted -, and the lack of training to face the new situations [51, 105].
The health information system and mandatory reporting were severely disrupted, preventing surveillance and the implementation of targeted interventions [118]. This may have led to an underestimation of the impact of COVID-19 on the overall health system and healthcare access. This situation has largely contributed to the demotivation of health personnel, their lack of attention to the public, and to increasing anxiety, and psychological disorders [51-53, 61, 118].
The delay or reduction of many healthcares, interruption of services, mitigation of transmission risk strategies or recommendations, difficulties in the supply of drugs and health products, high cost of the latter, and the shortage of essential medicines discouraged people who suspended their seek for healthcare [19, 24, 27, 57, 69, 78, 84, 94].
Individual factors
Many factors have been put forward to explain the population's reluctance to travel, including visiting a health center. In addition to personal reasons, primarily the fear of contamination and resulting stigmatization, as well as the drop in income that limits many activities, conjunctural factors (lack of transportation, containment, curfews) and structural factors (insufficient human and material resources) explain the refusal to consult and the lack of access to healthcare. Fear of contamination, for themselves or their relatives, also concerned most health workers, especially those who had never experienced a major epidemic [37, 83, 118]. They often saw themselves as victims of stigma and discrimination [83, 97].
Recommendations
Several studies have successfully tested strategies to address the observed deficiencies. Improved service delivery relies on technological innovations and adaptations, such as the use of self-tests, telemedicine through telephone or videoconferencing for diagnosis or prescription of drugs, and the use of drones for the distribution of health products [12, 19, 21, 26, 28, 29 37, 71]. In addition, reorganizing community services, arranging drug supplies, providing early non-pharmacological interventions (e.g., vector control), raising public awareness, and adapting treatment protocols were proving successful [15, 23, 26, 30, 47, 63, 70, 78, 84, 97, 110, 111, 113, 112].
Patient flows and supply of health products, including personal protective equipment, need to be regulated [12, 26, 46, 84]. In the event of service failures during the epidemic period, catch-up measures, including routine vaccinations, should be adopted [11, 58]. Collaboration between healthcare providers and public health services is a key element of the healthcare delivery system [74]. This includes the appropriate use of standardized health indicators and more accurate consideration of factors limiting the management of co-morbidities [20, 49].
Training of health workers in patient intake and management, and improvement of alternative diagnostic and therapeutic techniques, such as appropriate drug dispensing (e.g., provision of ART or TB treatment for several months) would help to anticipate difficulties that are bound to arise in accessing healthcare, in the supply of drugs, or health facility access [15, 23, 78, 113, 119].
The role of community health workers in the management of patients with conditions other than COVID-19, particularly in the most vulnerable slums and rural areas, requires stronger support and recognition [30, 85, 119]. Strengthening and expanding existing social protection schemes would reduce the deleterious consequences of epidemics in general and ensure more effective resilience, especially among vulnerable populations [47].
Misinformation and rumors should be controlled by appropriate information strategies with clear and simple messages, targeting community and opinion leaders, including religious ones, artists, and trusted individuals [20, 34, 38, 63].
Finally, legislation on domestic violence and the maintenance of constant surveillance, including in times of restricted movement and social disorganization, should be adjusted [75, 76].
This study was not intended to be exhaustive or to detail changes in healthcare access, but to identify the main impacts of COVID-19 on the organization and use of the health system in SSA. The outcomes of a literature review, such as this one, depend largely on the quality of the studies, i.e., their representativeness, the validity of the samples selected, and the relevance of the analyses performed. The procedures used to select the samples, the decision criteria, the presentation of the results and their discussion were not of the same quality according to the study, even if all the articles came from indexed peer-reviewed journals. In addition, health centers were not randomly selected, and some sample sizes were small. However, despite these limitations, the convergence of the raw data supported the validity of the results. The decline in healthcare access appeared in all studies with similar levels and kinetics over time, giving them credibility.
Conclusion
The causes of the impact of COVID-19 on access to healthcare are multifactorial. However, restrictive government measures limiting travel, transport, supply, and the opening of public places, including shops and places of entertainment or worship, have blocked all social and economic activities with considerable deleterious consequences. The disorganization affected the whole of society, including the health system which was not prepared for it. In addition, at the individual level, the fear of contamination, reduction in income, economic and social disorder, in particular the loss of confidence in the health system, and stress increased by the infodemia explained the population's reluctance to healthcare access [34, 120]. The drastic measures taken at the beginning of the pandemic probably slowed and delayed its spread but at the cost of dramatic psychosocial and economic consequences.
Fortunately, although healthcare access was severely hampered (Table 2), the return to normal was rapid, showing the resilience of the health system, and a certain confidence of the population [40].
This epidemic, coming after many others, such as the one due to the Ebola virus [121], will be followed by new ones, which will require adapted responses that consider conjunctural and structural components such as the training of health personnel, appropriate equipment, available health products, precise procedures and information for the population. The general unpreparedness and lack of anticipation of the risk, forcing a disproportionate response, represents a socio-economic cost that will be less and less accepted by the populations in the future.
Footnotes
Availability of data and materials: Not applicable.
Funding : Not applicable.
Ethics approval: Not applicable.
Consent for publication: Not applicable.
References
- Impouma B, Mboussou F, Farham B, Wolfe CM, Johnson K, Clary C, Mihigo R, Nsenga N, Talisuna A, Yoti Z, Flahault A, Keiser O, Gueye AS, Cabore J, Moeti M. The COVID-19 pandemic in the WHO African region: the first year (February 2020 to February 2021) Epidemiol Infect. 2021;149:e263. doi: 10.1017/S0950268821002429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James A, Dalal J, Kousi T, Vivacqua D, Câmara DCP, Dos Reis IC, Botero Mesa S, Ng'ambi W, Ansobi P, Bianchi LM, Lee TM, Ogundiran O, Stoll B, Chimbetete C, Mboussou F, Impouma B, Hofer CB, Coelho FC, Keiser O, Abbate JL. An in-depth statistical analysis of the COVID-19 pandemic's initial spread in the WHO African region. BMJ Glob Health. 2022;7(4):e007295. doi: 10.1136/bmjgh-2021-007295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musa SS, Wang X, Zhao S, Li S, Hussaini N, Wang W, He D. The Heterogeneous Severity of COVID-19 in African Countries: A Modeling Approach. Bull Math Biol. 2022;84(3):32. doi: 10.1007/s11538-022-00992-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mwananyanda L, Gill CJ, MacLeod W, Kwenda G, Pieciak R, Mupila Z, Lapidot R, Mupeta F, Forman L, Ziko L, Etter L, Thea D. Covid-19 deaths in Africa: prospective systematic postmortem surveillance study. BMJ. 2021;372(334) doi: 10.1136/bmj.n334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wamai RG, Hirsch JL, Van Damme W, Alnwick D, Bailey RC, Hodgins S, Alam U, Anyona M. What could explain the lower COVID-19 burden in Africa despite considerable circulation of the SARS-CoV-2 virus? Int J Environ Res Public Health. 2021;18(16):8638. doi: 10.3390/ijerph18168638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warsame A, Bashiir F, Freemantle T, Williams C, Vazquez Y, Reeve C, Aweis A, Ahmed M, Checchi F, Dalmar A. Excess mortality during the COVID-19 pandemic: a geospatial and statistical analysis in Mogadishu, Somalia. Int J Infect Dis. 2021;113:190–199. doi: 10.1016/j.ijid.2021.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COVID-19 Excess Mortality Collaborators Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet. 2022;399(10334):1513–1536. doi: 10.1016/S0140-6736(21)02796-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OMS AFRO Tableau de bord COVID-19. Bureau régional Afrique de l’Organisation mondiale de la santé. 2022. [24 août 2022]. [ https://who.maps.arcgis.com/apps/dashboards/0c9b3a8b68d0437a8cf28581e9c063a9 .
- Bell D, Hansen KS, Kiragga AN, Kambugu A, Kissa J, Mbonye AK. Predicting the Impact of COVID-19 and the Potential Impact of the Public Health Response on Disease Burden in Uganda. Am J Trop Med Hyg. 2020;103(3):1191–1197. doi: 10.4269/ajtmh.20-0546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan CF, McCann N, Stover J, Freedberg KA, Ciaranello AL. Do not forget the children: a model-based analysis on the potential impact of COVID-19-associated interruptions in paediatric HIV prevention and care. J Int AIDS Soc. 2022;25(1):e25864. doi: 10.1002/jia2.25864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaythorpe KA, Abbas K, Huber J, Karachaliou A, Thakkar N, Woodruff K, Li X, Echeverria-Londono S. VIMC Working Group on COVID-19 Impact on Vaccine Preventable Disease, Ferrari M, Jackson ML, McCarthy K, Perkins TA, Trotter C, Jit M. Impact of COVID-19-related disruptions to measles, meningococcal A, and yellow fever vaccination in 10 countries. Elife. 2021;10:e67023. doi: 10.7554/eLife.67023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inzaule SC, Ondoa P, Loembe MM, Tebeje YK, Ouma AEO, Nkengasong JN. COVID-19 and indirect health implications in Africa: Impact, mitigation measures, and lessons learned for improved disease control. PLoS Med. 2021;18(6):e1003666. doi: 10.1371/journal.pmed.1003666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OMS . Rapport Mondial sur le paludisme. Geneva: World Health Organization; 2021. [24/08/2022]. CC BY-NC-SA 3.0 IGO. 0 IGO [ https://www.who.int/teams/global-malaria-programme/reports/world-malaria-report-2021 . [Google Scholar]
- Ray N. Impacts de la pandémie de Covid-19 sur le contrôle des autres maladies en Afrique - Après les vagues, le tsunami. Rev Med Suisse. 2021;17(730):521–523. [PubMed] [Google Scholar]
- Shi B, Zheng J, Xia S, Lin S, Wang X, Liu Y, Zhou XN, Liu J. Accessing the syndemic of COVID-19 and malaria intervention in Africa. Infect Dis Poverty. 2021;10(1):5. doi: 10.1186/s40249-020-00788-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- Amouzou A, Maïga A, Faye CM, Chakwera S, Melesse DY, Mutua MK, Thiam S, Abdoulaye IB, Afagbedzi SK, Ag Iknane A, Ake-Tano OS, Akinyemi JO, Alegana V, Alhassan Y, Sam AE, Atweam DK, Bajaria S, Bawo L, Berthé M, Blanchard AK, Bouhari HA, Boulhassane OMA, Bulawayo M, Chooye O, Coulibaly A, Diabate M, Diawara F, Esleman O, Gajaa M, Garba KHA, Getachew T, Jacobs C, Jacobs GP, James F, Jegede AS, Joachim C, Kananura RM, Karimi J, Kiarie H, Kpebo D, Lankoandé B, Lawanson AO, Mahamadou Y, Mahundi M, Manaye T, Masanja H, Millogo MR, Mohamed AK, Musukuma M, Muthee R, Nabié D, Nyamhagata M, Ogwal J, Orimadegun A, Ovuoraye A, Pongathie AS, Sable SP, Saydee GS, Shabini J, Sikapande BM, Simba D, Tadele A, Tadlle T, Tarway-Twalla AK, Tassembedo M, Tehoungue BZ, Terera I, Traoré S, Twalla MP, Waiswa P, Wondirad N, Boerma T. Health service utilisation during the COVID-19 pandemic in sub-Saharan Africa in 2020: a multicountry empirical assessment with a focus on maternal, newborn and child health services. BMJ Glob Health. 2022;7(5):e008069. doi: 10.1136/bmjgh-2021-008069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- theglobalfund.org Fonds Mondial de lutte contre le sida, la tuberculose et le paludisme. Impact du COVID-19 sur les services de lutte contre le VIH, la tuberculose et le paludisme et les systèmes de santé - Mises à jour. 2021. [24/08/2022]. 18. 2021 ; 18 pages [ http://covid-19_2020-disruption-impact_report_fr.pdf .
- Martei YM, Rick TJ, Fadelu T, Ezzi MS, Hammad N, Quadri NS, Rodrigues B, Simonds H, Grover S, Incrocci L, Vanderpuye V. Impact of COVID-19 on Cancer Care Delivery in Africa: A Cross-Sectional Survey of Oncology Providers in Africa. JCO Glob Oncol. 2021;7:368–377. doi: 10.1200/GO.20.00569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng'andu M, Mesic A, Pry J, Mwamba C, Roff F, Chipungu J, Azgad Y, Sharma A. Sexual and reproductive health services during outbreaks, epidemics, and pandemics in sub-Saharan Africa: a literature scoping review. Syst Rev. 2022;11(1):161. doi: 10.1186/s13643-022-02035-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akintayo RO, Akpabio AA, Kalla AA, Dey D, Migowa AN, Olaosebikan H, Bahiri R, El Miedany Y, Hadef D, Hamdi W, Oyoo O, Slimani S, Yerima A, Taha Y, Adebajo AO, Adelowo OO, Tikly M, Ghozlani I, Ben Abdelghani K, Fouad NA, Mosad D, El Mikkawy D, Abu-Zaid MH, Abdel-Magied RA. The impact of COVID-19 on rheumatology practice across Africa. Rheumatology (Oxford) 2021;60(1):392–398. doi: 10.1093/rheumatology/keaa600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mashige KP, Osuagwu UL, Ulagnathan S, Ekpenyong BN, Abu EK, Goson PC, Langsi R, Nwaeze O, Timothy CG, Charwe DD, Oloruntoba R, Miner CA, Ishaya T, Ovenseri-Ogbomo GO, Agho KE. Economic, Health and Physical Impacts of COVID-19 Pandemic in Sub-Saharan African Regions: A Cross Sectional Survey. Risk Manag Healthc Policy. 2021;14:4799–4807. doi: 10.2147/RMHP.S324554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabore A, Palmer SL, Mensah E, Ettiegne-Traore V, Monteil R, Sintondji F, Tine J, Tesfaye D, Ogoussan K, Stukel D, Fuller BB, Sanchez K, Pou B, Dembele B, Weaver A, Reid S, Milord MD, Kassankogno Y, Seim A, Shott J. Restarting Neglected Tropical Diseases Programs in West Africa during the COVID-19 pandemic: lessons learned and best practices. Am J Trop Med Hyg. 2021;105(6):1476–1482. doi: 10.4269/ajtmh.21-0408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Oirschot J, Ooms GI, Waldmann B, Kadam P. Snakebite incidents, prevention and care during COVID-19: Global key-informant experiences. Toxicon X. 2021;10:100075. doi: 10.1016/j.toxcx.2021.100075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ameyaw EK, Ahinkorah BO, Seidu AA, Njue C. Impact of COVID-19 on maternal healthcare in Africa and the way forward. Arch Public Health. 2021;79(1):223. doi: 10.1186/s13690-021-00746-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessema GA, Kinfu Y, Dachew BA, Tesema AG, Assefa Y, Alene KA, Aregay AF, Ayalew MB, Bezabhe WM, Bali AG, Dadi AF, Duko B, Erku D, Gebrekidan K, Gebremariam KT, Gebremichael LG, Gebreyohannes EA, Gelaw YA, Gesesew HA, Kibret GD, Leshargie CT, Meazew MW, Mekonnen A, Mirkuzie AH, Mohammed H, Tekle DY, Tesfay FH. The COVID-19 pandemic and healthcare systems in Africa: a scoping review of preparedness, impact and response. BMJ Glob Health. 2021;6(12):e007179. doi: 10.1136/bmjgh-2021-007179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adu PA, Stallwood L, Adebola SO, Abah T, Okpani AI. The direct and indirect impact of COVID-19 pandemic on maternal and child health services in Africa: a scoping review. Glob Health Res Policy. 2022;7(1):20. doi: 10.1186/s41256-022-00257-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanda-Kapata P, Ntoumi F, Kapata N, Lungu P, Mucheleng'anga LA, Chakaya J, Tembo J, Himwaze C, Ansumana R, Asogun D, Mfinanga S, Nyasulu P, Mwaba P, Yeboah-Manu D, Zumla A, Nachega JB. Tuberculosis, HIV/AIDS and Malaria Health Services in sub-Saharan Africa - A Situation Analysis of the Disruptions and Impact of the COVID-19 Pandemic. Int J Infect Dis. 2022;124(Suppl 1):S41–S46. doi: 10.1016/j.ijid.2022.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rick F, Odoke W, van den Hombergh J, Benzaken AS, Avelino-Silva VI. Impact of coronavirus disease (COVID-19) on HIV testing and care provision across four continents. HIV Med. 2022;23(2):169–177. doi: 10.1111/hiv.13180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballard M, Olsen HE, Millear A, Yang J, Whidden C, Yembrick A, Thakura D, Nuwasiima A, Christiansen M, Ressler DJ, Omwanda WO, Lassala D, Palazuelos D, Westgate C, Munyaneza F. Continuity of community-based healthcare provision during COVID-19: a multicountry interrupted time series analysis. BMJ Open. 2022;12(5):e052407. doi: 10.1136/bmjopen-2021-052407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masresha B, Luce R, Katsande R, Dosseh A, Tanifum P, Lebo E, Byabamazima C, Kfutwah A. The impact of the COVID-19 pandemic on measles surveillance in the World Health Organisation African Region, 2020. Pan Afr Med J. 2021;39:192. doi: 10.11604/pamj.2021.39.192.29491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assefa N, Sié A, Wang D, Korte ML, Hemler EC, Abdullahi YY, Lankoande B, Millogo O, Chukwu A, Workneh F, Kanki P, Baernighausen T, Berhane Y, Fawzi WW, Oduola A. Reported Barriers to Healthcare Access and Service Disruptions Caused by COVID-19 in Burkina Faso, Ethiopia, and Nigeria: A Telephone Survey. Am J Trop Med Hyg. 2021;105(2):323–330. doi: 10.4269/ajtmh.20-1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gummerson E, Cardona C, Anglewicz P, Zachary B, Guiella G, Radloff S. The wealth gradient and the effect of COVID-19 restrictions on income loss, food insecurity and healthcare access in four sub-Saharan African geographies. PLoS One. 2021;16(12):e0260823. doi: 10.1371/journal.pone.0260823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seytre B. Public perceptions, more than misinformation, explain poor adherence to proven COVID-19 control measures. Am J Trop Med Hyg. 2022;106(4):1000–1002. doi: 10.4269/ajtmh.21-1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chelo D, Mekone Nkwelle I, Nguefack F, Mbassi Awa HD, Enyama D, Nguefack S, Noukeu Njinkui D, Tony Nengom J, Nguefack-Tsague G, Koki Ndombo PO. Decrease in hospitalizations and increase in deaths during the covid-19 epidemic in a pediatric hospital, Yaounde-Cameroon and prediction for the coming months. Fetal Pediatr Pathol. 2021;40(1):18–31. doi: 10.1080/15513815.2020.1831664. [DOI] [PubMed] [Google Scholar]
- Chelo D, Nguefack F, Enyama D, Nansseu R, Feudjo Tefoueyet G, Mbassi Awa HD, Mekone Nkwelle I, Nguefack-Tsague G, Ndenbe P, Koki Ndombo PO. Impact and projections of the COVID-19 epidemic on attendance and routine vaccinations at a pediatric referral hospital in Cameroon. Arch Pediatr. 2021;28(6):441–450. doi: 10.1016/j.arcped.2021.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enyama D, Chelo D, Noukeu Njinkui D, Mayouego Kouam J, Fokam Djike Puepi Y, Mekone Nkwele I, Ndenbe P, Nguefack S, Nguefack F, Kedy Koum D, Tetanye E. Impact of the COVID-19 pandemic on pediatricians' clinical activity in Cameroon. Arch Pediatr. 2020;27(8):423–427. doi: 10.1016/j.arcped.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touré HA, Noufe S, Oussou KR, N'Guessan K, Setchi SM, Ano AMN, Tiembre I, Bénie BVJ. Effets de la pandémie à Covid-19 sur les activités vaccinales d'un centre de vaccination de référence de Treichville en Côte d'Ivoire. Med Trop Sante Int. 2021;1(2) doi: 10.48327/mtsibulletin.n1.2021.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hategeka C, Carter SE, Chenge FM, Katanga EN, Lurton G, Mayaka SM, Mwamba DK, van Kleef E, Vanlerberghe V, Grépin KA. Impact of the COVID-19 pandemic and response on the utilisation of health services in public facilities during the first wave in Kinshasa, the Democratic Republic of the Congo. BMJ Glob Health. 2021;6(7):e005955. doi: 10.1136/bmjgh-2021-005955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho LS, Bertone MP, Mansour W, Masaka C, Kakesa J. Health system resilience during COVID-19 understanding SRH service adaptation in North Kivu. Reprod Health. 2022;19(1):135. doi: 10.1186/s12978-022-01443-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdela SG, Berhanu AB, Ferede LM, van Griensven J. Essential Healthcare Services in the Face of COVID-19 Prevention: Experiences from a Referral Hospital in Ethiopia. Am J Trop Med Hyg. 2020;103(3):1198–1200. doi: 10.4269/ajtmh.20-0464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beyene NW, Sitotaw AL, Tegegn B, Bobosha K. The impact of COVID-19 on the tuberculosis control activities in Addis Ababa. Pan Afr Med J. 2021;38:243. doi: 10.11604/pamj.2021.38.243.27132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arega B, Negesso A, Taye B, Weldeyohhans G, Bewket B, Negussie T, Teshome A, Endazenew G. Impact of COVID-19 pandemic on TB prevention and care in Addis Ababa, Ethiopia: a retrospective database study. BMJ Open. 2022;12(2):e053290. doi: 10.1136/bmjopen-2021-053290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilot D, Woldeamanuel Y, Manyazewal T. Real-Time Impact of COVID-19 on Clinical Care and Treatment of Patients with Tuberculosis: A Multicenter Cross-Sectional Study in Addis Ababa, Ethiopia. Ann Glob Health. 2021;87(1):109. doi: 10.5334/aogh.3481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miretu DG, Asfaw ZA, Addis SG. Impact of COVID-19 pandemic on vaccination coverage among children aged 15 to 23 months at Dessie town, Northeast Ethiopia, 2020. Hum Vaccin Immunother. 2021;17(8):2427–2436. doi: 10.1080/21645515.2021.1883387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dandena F, Teklewold B, Anteneh D. Impact of COVID-19 and mitigation plans on essential health services: institutional experience of a hospital in Ethiopia. BMC Health Serv Res. 2021;21(1):1105. doi: 10.1186/s12913-021-07106-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deshpande AS, Mulat AK, Mao W, Diab MM, Ogbuoji O. Coverage of social assistance in Ethiopia during the COVID-19 pandemic: a time-to-event analysis. BMJ Glob Health. 2022;7(7):e008432. doi: 10.1136/bmjgh-2022-008432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tadesse E. Antenatal Care Service Utilization of Pregnant Women Attending Antenatal Care in Public Hospitals During the COVID-19 Pandemic Period. Int J Womens Health. 2020;12:1181–1188. doi: 10.2147/IJWH.S287534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayele TA, Shibru H, Mequanent Sisay M, Melese T, Fentie M, Azale T, Belachew T, Shitu K, Alamneh TS. The effect of COVID-19 on poor treatment control among ambulatory Hypertensive and/or Diabetic patients in Northwest Ethiopia. PLoS One. 2022;17(5):e0266421. doi: 10.1371/journal.pone.0266421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quaglio G, Cavallin F, Nsubuga JB, Lochoro P, Maziku D, Tsegaye A, Azzimonti G, Kamunga AM, Manenti F, Putoto G. The impact of the COVID-19 pandemic on health service use in sub-Saharan Africa. Public Health Action. 2022;12(1):34–39. doi: 10.5588/pha.21.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimels T. Has the COVID-19 pandemic impacted healthcare service uptake at hospitals in Addis Ababa? Ethiop J Health Sci. 2021;31(4):689–698. doi: 10.4314/ejhs.v31i4.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deressa W, Worku A, Abebe W, Gizaw M, Amogne W. Risk perceptions and preventive practices of COVID-19 among healthcare professionals in public hospitals in Addis Ababa, Ethiopia. PLoS One. 2021;16(6):e0242471. doi: 10.1371/journal.pone.0242471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GebreEyesus FA, Tarekegn TT, Amlak BT, Shiferaw BZ, Emeria MS, Geleta OT, Terefe TF, Mammo Tadereregew M, Jimma MS, Degu FS, Abdisa EN, Eshetu MA, Misganaw NM, Chanie ES. Levels and predictors of anxiety, depression, and stress during COVID-19 pandemic among frontline healthcare providers in Gurage zonal public hospitals, Southwest Ethiopia, 2020: A multicenter cross-sectional study. PLoS One. 2021;16(11):e0259906. doi: 10.1371/journal.pone.0259906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desta AA, Woldearegay TW, Gebremeskel E, Alemayehu M, Getachew T, Gebregzabiher G, et al. Impacts of COVID-19 on essential health services in Tigray, Northern Ethiopia: A pre-post study. PLoS One. 2021;16(8):e0256330. doi: 10.1371/journal.pone.0256330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraham SAA, Doe PF, Osei Berchie G, Agyare E, Ayisi Addo S, Obiri-Yeboah D. Explorative-descriptive study on the effects of COVID-19 on access to antiretroviral therapy services: the case of a teaching hospital in Ghana. BMJ Open. 2022;12(5):e056386. doi: 10.1136/bmjopen-2021-056386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood SN, Yirgu R, Wondimagegnehu A, Qian J, Milkovich RM, Decker MR, Glass N, Seid F, Zekarias L, Zimmerman LA. Impact of the COVID-19 pandemic on intimate partner violence during pregnancy: evidence from a multimethods study of recently pregnant women in Ethiopia. BMJ Open. 2022;12(4):e055790. doi: 10.1136/bmjopen-2021-055790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuschen AK, Abdul-Mumin A, Adokiya M, Lu G, Jahn A, Razum O, Winkler V, Müller O. Impact of the COVID-19 pandemic on malaria cases in health facilities in northern Ghana: a retrospective analysis of routine surveillance data. Malar J. 2022;21(1):149. doi: 10.1186/s12936-022-04154-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bimpong KA, Nuertey BD, Seidu AS, Ajinkpang S, Abdul-Mumin A. Decline in Uptake of Childhood Vaccinations in a Tertiary Hospital in Northern Ghana during the COVID-19 Pandemic. Biomed Res Int. 2021;2021:6995096. doi: 10.1155/2021/6995096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akudjedu TN, Botwe BO, Wuni AR, Mishio NA. Impact of the COVID-19 pandemic on clinical radiography practice in low resource settings: The Ghanaian radiographers' perspective. Radiography (Lond) 2021;27(2):443–452. doi: 10.1016/j.radi.2020.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hewlett SA, Blankson PK, Konadu AB, Osei-Tutu K, Aprese D, Adjei M, Yawson AE, Donkor P, Nyako EA. COVID-19 pandemic and dental practice in Ghana. Ghana Med J. 2020;54(4):100–103. doi: 10.4314/gmj.v54i4s.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abraham SA, Berchie GO, Doe PF, Agyare E, Addo SA, Obiri-Yeboah D. Effects of COVID-19 pandemic on ART Service delivery: perspectives of healthcare workers in a Teaching Hospital in Ghana. BMC Health Serv Res. 2021;21(1):1295. doi: 10.1186/s12913-021-07330-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frimpong EK, Yamoah P, Wiafe E, Demana PH, Matlala M. Market Women's Perspectives on Coronavirus Disease 2019 (COVID-19): The Case of Ghana and South Africa. Int J Environ Res Public Health. 2022;19(15):9658. doi: 10.3390/ijerph19159658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agbozo F, Jahn A. COVID-19 in Ghana: challenges and countermeasures for maternal health service delivery in public health facilities. Reprod Health. 2021;18(1):151. doi: 10.1186/s12978-021-01198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahorlu CS, Okyere D, Pi-Bansa S, Otchere J, Marfo B, Asemanyi-Mensah K, Opare JL, Long EF, de Souza DK. COVID-19 related perception among some community members and frontline healthcare providers for NTD control in Ghana. BMC Infect Dis. 2022;22(1):106. doi: 10.1186/s12879-022-07084-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry IS, Baldé EY, Béavogui M, Camara A, Samoura A, Koïvogui K, Koïvogui D, Soumaoro M, Sow A, Kourouma M, Bah MB, Baldé MA, Sylla IS, Koné A, Diakité S, Sylla D, Baldé MD, Condé M. Impact de la pandémie de COVID-19 sur les activités du service de cardiologie de l’hôpital national Ignace Deen du CHU de Conakry. Ann Cardiol Angeiol (Paris) 2021;70(2):102–105. doi: 10.1016/j.ancard.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker MR, Wood SN, Thiongo M, Byrne ME, Devoto B, Morgan R, Bevilacqua K, Williams A, Stuart HC, Wamue-Ngare G, Heise L, Glass N, Anglewicz P, Gummerson E, Gichangi P. Gendered health, economic, social and safety impact of COVID-19 on adolescents and young adults in Nairobi, Kenya. PLoS One. 2021;16(11):e0259583. doi: 10.1371/journal.pone.0259583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitau T, Kamita M, Muli E, Mweni S, Waithanji R, Mutisya F, Kirira P, Nzioka A, Figueroa J, Makokha F. The impact of measures to curb COVID-19 on patient attendance at 10 hospitals in Machakos County, Kenya. J Glob Health. 2021;11:05016. doi: 10.7189/jogh.11.05016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wambua S, Malla L, Mbevi G, Kandiah J, Nwosu AP, Tuti T, Paton C, Wambu B, English M, Okiro EA. Quantifying the indirect impact of COVID-19 pandemic on utilisation of outpatient and immunisation services in Kenya: a longitudinal study using interrupted time series analysis. BMJ Open. 2022;12(3):e055815. doi: 10.1136/bmjopen-2021-055815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhula S, Opanga Y, Oramisi V, Ngugi C, Ngunu C, Carter J, Marita E, Osur J, Memiah P. Impact of the First Wave of the COVID-19 Pandemic on HIV/AIDS Programming in Kenya: Evidence from Kibera Informal Settlement and COVID-19 Hotspot Counties. Int J Environ Res Public Health. 2021;18(11):6009. doi: 10.3390/ijerph18116009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed SAKS, Ajisola M, Azeem K, Bakibinga P, Chen YF, Choudhury NN, Fayehun O, Griffiths F, Harris B, Kibe P, Lilford RJ, Omigbodun A, Rizvi N, Sartori J, Smith S, Watson SI, Wilson R, Yeboah G, Aujla N, Azam SI, Diggle PJ, Gill P, Iqbal R, Kabaria C, Kisia L, Kyobutungi C, Madan JJ, Mberu B, Mohamed SF, Nazish A, Odubanjo O, Osuh ME, Owoaje E, Oyebode O, Porto de Albuquerque J, Rahman O, Tabani K, Taiwo OJ, Tregonning G, Uthman OA, Yusuf R, Improving Health in Slums Collaborative Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Glob Health. 2020;5(8):e003042. doi: 10.1136/bmjgh-2020-003042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gichuna S, Hassan R, Sanders T, Campbell R, Mutonyi M, Mwangi P. Access to Healthcare in a time of COVID-19: Sex Workers in Crisis in Nairobi, Kenya. Glob Public Health. 2020;15(10):1430–1442. doi: 10.1080/17441692.2020.1810298. [DOI] [PubMed] [Google Scholar]
- Pinchoff J, Friesen EL, Kangwana B, Mbushi F, Muluve E, Ngo TD, Austrian K. How has COVID-19-related income loss and household stress affected adolescent mental health in Kenya? J Adolesc Health. 2021;69(5):713–720. doi: 10.1016/j.jadohealth.2021.07.023. [DOI] [PubMed] [Google Scholar]
- Zulaika G, Bulbarelli M, Nyothach E, van Eijk A, Mason L, Fwaya E, Obor D, Kwaro D, Wang D, Mehta SD, Phillips-Howard PA. Impact of COVID-19 lockdowns on adolescent pregnancy and school dropout among secondary schoolgirls in Kenya. BMJ Glob Health. 2022;7(1):e007666. doi: 10.1136/bmjgh-2021-007666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abu TZ, Elliott SJ. The critical need for WASH in emergency preparedness in health settings, the case of COVID-19 pandemic in Kisumu Kenya. Health Place. 2022;76:102841. doi: 10.1016/j.healthplace.2022.102841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed SAE, Changole J, Wangamati CK. Impact of the COVID-19 pandemic on intimate partner violence in Sudan, Malawi and Kenya. Reprod Health. 2021;18(1):222. doi: 10.1186/s12978-021-01272-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy CM, Bukuluki P, Casey SE, Jagun MO, John NA, Mabhena N, Mwangi M, McGovern T. Impact of COVID-19 on gender-based violence prevention and response services in Kenya, Uganda, Nigeria, and South Africa: a cross-sectional survey. Front Glob Womens Health. 2022;2:780771. doi: 10.3389/fgwh.2021.780771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimhuya S, Neal SR, Chimhini G, Gannon H, Cortina Borja M, Crehan C, Nkhoma D, Chiyaka T, Wilson E, Hull-Bailey T, Fitzgerald F, Chiume M, Heys M. Indirect impacts of the COVID-19 pandemic at two tertiary neonatal units in Zimbabwe and Malawi: an interrupted time series analysis. BMJ Open. 2022;12(6):e048955. doi: 10.1136/bmjopen-2021-048955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phiri MM, MacPherson EE, Panulo M, Chidziwisano K, Kalua K, Chirambo CM, Kawalazira G, Gundah Z, Chunda P, Morse T. Preparedness for and impact of COVID-19 on primary healthcare delivery in urban and rural Malawi: a mixed methods study. BMJ Open. 2022;12(6):e051125. doi: 10.1136/bmjopen-2021-051125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagaon-Teyssier L, Kamissoko A, Yattassaye A, Diallo F, Rojas Castro D, Delabre R, Pouradier F, Maradan G, Bourrelly M, Cissé M, Vidal L, Keïta BD, Spire B. Assessment of mental health outcomes and associated factors among workers in community-based HIV care centers in the early stage of the COVID-19 outbreak in Mali. Health Policy Open. 2020;1:100017. doi: 10.1016/j.hpopen.2020.100017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- das Neves Martins Pires PH, Macaringue C, Abdirazak A, Mucufo JR, Mupueleque MA, Zakus D, Siemens R, Belo CF. Covid-19 pandemic impact on maternal and child health services access in Nampula, Mozambique: a mixed methods research. BMC Health Serv Res. 2021;21(1):860. doi: 10.1186/s12913-021-06878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aantjes C, Muchanga V, Munguambe K. Exposed and unprotected: Sex worker vulnerabilities during the COVID-19 health emergency in Mozambique. Glob Public Health. 2022;24:1–15. doi: 10.1080/17441692.2022.2092184. [DOI] [PubMed] [Google Scholar]
- Manhiça I, Augusto O, Sherr K, Cowan J, Cuco RM, Agostinho S, Macuacua BC, Ramiro I, Carimo N, Matsinhe MB, Gloyd S, Chicumbe S, Machava R, Tembe S, Fernandes Q. COVID-19-related healthcare impacts: an uncontrolled, segmented time-series analysis of tuberculosis diagnosis services in Mozambique, 2017-2020. BMJ Glob Health. 2022;7(4):e007878. doi: 10.1136/bmjgh-2021-007878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powelson J, Magadzire BP, Draiva A, Denno D, Ibraimo A, Benate BBL, Jahar LC, Marrune Z, Chilundo B, Chinai JE, Emerson M, Beima-Sofie K, Lawrence E. Determinants of immunisation dropout among children under the age of 2 in Zambézia province, Mozambique: a community-based participatory research study using Photovoice. BMJ Open. 2022;12(3):e057245. doi: 10.1136/bmjopen-2021-057245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirivangani T, Alpo B, Kibuule D, Gaeseb J, Adenuga BA. Impact of COVID-19 pandemic on pharmaceutical systems and supply chain - a phenomenological study. Explor Res Clin Soc Pharm. 2021;2:100037. doi: 10.1016/j.rcsop.2021.100037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdoulaye MB, Oumarou B, Moussa H, Anya BM, Didier T, Nsiari-Muzeyi BJ, Katoto P, Wiysonge CS. Impact de la pandémie de la COVID-19 sur l’utilisation des services de santé dans la ville de Niamey : une analyse dans 17 formations sanitaires de janvier à juin 2020. Pan Afr Med J. 2021;39:159. doi: 10.11604/pamj.2021.39.159.28282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezenwa BN, Fajolu IB, Nabwera H, Wang D, Ezeaka CV, Allen S. Impact of COVID-19 lockdown measures on institutional delivery, neonatal admissions and prematurity: a reflection from Lagos, Nigeria. BMJ Paediatr Open. 2021;5(1):e001029. doi: 10.1136/bmjpo-2021-001029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seyi-Olajide JO, Bode CO, Ihediwa GC, Elebute OA, Alakaloko FM, Ladipo-Ajayi OA, Ademuyiwa AO. Impact of corona virus disease 2019 pandemic on paediatric surgery in a sub-saharan tertiary hospital: An observational study. Niger Postgrad Med J. 2022;29(2):102–109. doi: 10.4103/npmj.npmj_761_21. [DOI] [PubMed] [Google Scholar]
- Odume B, Falokun V, Chukwuogo O, Ogbudebe C, Useni S, Nwokoye N, Aniwada E, Olusola Faleye B, Okekearu I, Nongo D, Odusote T, Lawanson A. Impact of COVID-19 on TB active case finding in Nigeria. Public Health Action. 2020;10(4):157–162. doi: 10.5588/pha.20.0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato R. Pattern of vaccination delivery around COVID-19 lockdown in Nigeria. Hum Vaccin Immunother. 2021;17(9):2951–2953. doi: 10.1080/21645515.2021.1908061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aladelusi TO, Atiba FA, Gbadebo SO, Adeyemo YI, Olusanya AA, Akadiri OA. COVID-19 outbreak and dental healthcare provision in Nigeria: a national survey. BMC Oral Health. 2021;21(1):493. doi: 10.1186/s12903-021-01860-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph A, Olatosi B, Haider MR, Adegboyega BC, Lasebikan NN, Aliyu UM, Ali-Gombe M, Jimoh MA, Biyi-Olutunde OA, Awofeso O, Fatiregun OA, Oboh EO, Nwachukwu E, Zubairu IH, Otene SA, Iyare OI, Andero T, Musbau AB, Ajose A, Onitilo AA. Patient's Perspective on the Impact of COVID-19 on Cancer Treatment in Nigeria. JCO Glob Oncol. 2022;8:e2100244. doi: 10.1200/GO.21.00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osaguona VB, Osahon AI, Uhumwangho OM. Impact of COVID-19 on Ophthalmic Outpatient Services in An Eye Care Center in Southern Nigeria. Niger J Clin Pract. 2021;24(9):1338–1342. doi: 10.4103/njcp.njcp_668_20. [DOI] [PubMed] [Google Scholar]
- Folayan MO, Arije O, Enemo A, Sunday A, Muhammad A, Nyako HY, Abdullah RM, Okiwu H, Undelikwo VA, Ogbozor PA, Amusan O, Alaba OA, Lamontagne E. Factors associated with poor access to HIV and sexual and reproductive health services in Nigeria for women and girls living with HIV during the COVID-19 pandemic. Afr J AIDS Res. 2022;21(2):171–182. doi: 10.2989/16085906.2022.2104169. [DOI] [PubMed] [Google Scholar]
- Awucha EN, Chinelo Janefrances O, Chima Meshach A, Chiamaka Henrietta J, Ibilolia Daniel A, Esther Chidiebere N. Impact of the COVID-19 Pandemic on Consumers' Access to Essential Medicines in Nigeria. Am J Trop Med Hyg. 2020;103(4):1630–1634. doi: 10.4269/ajtmh.20-0838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afolalu OO, Atekoja OE, Oyewumi ZO, Adeyeye SO, Jolayemi KI, Akingbade O. Perceived impact of coronavirus pandemic on uptake of healthcare services in South West Nigeria. Pan Afr Med J. 2021;40:26. doi: 10.11604/pamj.2021.40.26.28279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adesunkanmi AO, Ubom AE, Olasehinde O, Fasubaa OB, Ijarotimi OA, Adesunkanmi ARK, Okon NE. Impact of COVID-19 on the cost of surgical and obstetric care: experience from a Nigerian teaching hospital and a review of the Nigerian situation. Pan Afr Med J. 2020;37(1):15. doi: 10.11604/pamj.supp.2020.37.1.25935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oreh AC, Irechukwu C, Biyama F, Nnabuihe A, Ihimekpen A, Oshiame D, Bozegha T, Leo-Nnadi I, Izedonmwen O, Oga E, Suberu EJ, Odiabara K, Amedu OJ. COVID-19 impact on Nigeria's national blood service commission - Lessons for Low- and Middle-Income Countries (LMICs) Niger Postgrad Med J. 2022;29(1):6–12. doi: 10.4103/npmj.npmj_720_21. [DOI] [PubMed] [Google Scholar]
- Okoye OG, Olaomi OO, Gwaram UA, Apollo KD. The impact of COVID-19 lockdown on acute trauma patients seen at the National Hospital Trauma Centre Abuja, Nigeria. Pan Afr Med J. 2021;38:414. doi: 10.11604/pamj.2021.38.414.28431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedstrom A, Mubiri P, Nyonyintono J, Nakakande J, Magnusson B, Vaughan M, Waiswa P, Batra M. Impact of the early COVID-19 pandemic on outcomes in a rural Ugandan neonatal unit: A retrospective cohort study. PLoS One. 2021;16(12):e0260006. doi: 10.1371/journal.pone.0260006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Namuganga JF, Briggs J, Roh ME, Okiring J, Kisambira Y, Sserwanga A, Kapisi JA, Arinaitwe E, Ebong C, Ssewanyana I, Maiteki-Ssebuguzi C, Kamya MR, Staedke SG, Dorsey G, Nankabirwa JI. Impact of COVID-19 on routine malaria indicators in rural Uganda: an interrupted time series analysis. Malar J. 2021;20(1):475. doi: 10.1186/s12936-021-04018-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt JF, Ouma J, Lubyayi L, Amone A, Aol L, Sekikubo M, Nakimuli A, Nakabembe E, Mboizi R, Musoke P, Kyohere M, Namara Lugolobi E, Khalil A, Le Doare K. Indirect effects of COVID-19 on maternal, neonatal, child, sexual and reproductive health services in Kampala, Uganda. BMJ Glob Health. 2021;6(8):e006102. doi: 10.1136/bmjgh-2021-006102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz JI, Muddu M, Kimera I, Mbuliro M, Ssennyonjo R, Ssinabulya I, Semitala FC. Impact of a COVID-19 National Lockdown on Integrated Care for Hypertension and HIV. Glob Heart. 2021;16(1):9. doi: 10.5334/gh.928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner Z, Mukasa B, Nakakande J, Stecher C, Saya U, Linnemayr S. Impact of the COVID-19 pandemic on use of hiv care, antiretroviral therapy adherence, and viral suppression: an observational cohort study from Uganda. J Acquir Immune Defic Syndr. 2021;88(5):448–456. doi: 10.1097/QAI.0000000000002811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuwematsiko R, Nabiryo M, Bomboka JB, Nalinya S, Musoke D, Okello D, Wanyenze RK. Unintended socio-economic and health consequences of COVID-19 among slum dwellers in Kampala, Uganda. BMC Public Health. 2022;22(1):88. doi: 10.1186/s12889-021-12453-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sserwanja Q, Kawuki J, Kim JH. Increased child abuse in Uganda amidst COVID-19 pandemic. J Paediatr Child Health. 2021;57(2):188–191. doi: 10.1111/jpc.15289. [DOI] [PubMed] [Google Scholar]
- Pierre G, Uwineza A, Dzinamarira T. Attendance to HIV Antiretroviral Collection Clinic Appointments During COVID-19 Lockdown. A Single Center Study in Kigali, Rwanda. AIDS Behav. 2020;24(12):3299–3301. doi: 10.1007/s10461-020-02956-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakizimana D, Ntizimira C, Mbituyumuremyi A, Hakizimana E, Mahmoud H, Birindabagabo P, Musanabaganwa C, Gashumba D. The impact of Covid-19 on malaria services in three high endemic districts in Rwanda: a mixed-method study. Malar J. 2022;21(1):48. doi: 10.1186/s12936-022-04071-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sow A, Gueye M, Boiro D, Ba A, Ba ID, Faye PM, Fall AL, Ndiaye O. Impact de la COVID-19 sur la vaccination de routine en milieu hospitalier au Sénégal. Pan Afr Med J. 2020;37:364. doi: 10.11604/pamj.2020.37.364.25805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sevalie S, Youkee D, van Duinen AJ, Bailey E, Bangura T, Mangipudi S, Mansaray E, Odland ML, Parmar D, Samura S, van Delft D, Wurie H, Davies JI, Bolkan HA, Leather AJM. The impact of the COVID-19 pandemic on hospital utilisation in Sierra Leone. BMJ Glob Health. 2021;6(10):e005988. doi: 10.1136/bmjgh-2021-005988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakoh S, Jiba DF, Baldeh M, Adekanmbi O, Barrie U, Seisay AL, Deen GF, Salata RA, Yendewa GA. Impact of COVID-19 on Tuberculosis Case Detection and Treatment Outcomes in Sierra Leone. Trop Med Infect Dis. 2021;6(3):154. doi: 10.3390/tropicalmed6030154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonsenso D, Iodice F, Cinicola B, Raffaelli F, Sowa S, Ricciardi W. Management of Malaria in Children Younger Than 5 Years Old During Coronavirus Disease 2019 Pandemic in Sierra Leone: A Lesson Learned? Front Pediatr. 2021;8:587638. doi: 10.3389/fped.2020.587638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lungu PS, Kerkhoff AD, Muyoyeta M, Kasapo CC, Nyangu S, Kagujje M, Chimzizi R, Nyimbili S, Khunga M, Kasese-Chanda N, Musonda V, Tambatamba B, Kombe CM, Sakulanda C, Sampa K, Silumesii A, Malama K. Interrupted time-series analysis of active case-finding for tuberculosis during the COVID-19 pandemic, Zambia. Bull World Health Organ. 2022;100(3):205–215. doi: 10.2471/BLT.21.286109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pry JM, Sikombe K, Mody A, Iyer S, Mutale J, Vlahakis N, Savory T, Wa Mwanza M, Mweebo K, Mwila A, Mwale C, Mukumbwa-Mwenechanya M, Kerkhoff AD, Sikazwe I, Bolton Moore C, Mwamba D, Geng EH, Herce ME. Mitigating the effects of COVID-19 on HIV treatment and care in Lusaka, Zambia: a before-after cohort study using mixed effects regression. BMJ Glob Health. 2022;7(1):e007312. doi: 10.1136/bmjgh-2021-007312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hearst MO, Hughey L, Magoon J, Mubukwanu E, Ndonji M, Ngulube E, Makhoul Z. Rapid health impact assessment of COVID-19 on families with children with disabilities living in low-income communities in Lusaka, Zambia. PLoS One. 2021;16(12):e0260486. doi: 10.1371/journal.pone.0260486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakespeare C, Dube H, Moyo S, Ngwenya S. Resilience and vulnerability of maternity services in Zimbabwe: a comparative analysis of the effect of Covid-19 and lockdown control measures on maternal and perinatal outcomes, a single-centre cross-sectional study at Mpilo Central Hospital. BMC Pregnancy Childbirth. 2021;21(1):416. doi: 10.1186/s12884-021-03884-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimamise C, Munjanja SP, Machinga M, Shiripinda I. Impact of Covid-19 pandemic on obstetric fistula repair program in Zimbabwe. PLoS One. 2021;16(4):e0249398. doi: 10.1371/journal.pone.0249398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murewanhema G. Reduced cervical cancer screening in Zimbabwe as an indirect impact of the COVID-19 pandemic: implications for prevention. Pan Afr Med J. 2021;38:131. doi: 10.11604/pamj.2021.38.131.27852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madzima B, Makoni T, Mugurungi O, Mudariki G, Mpofu A, Dube F, Munangaidzwa L, Taramusi I. The impact of the COVID-19 pandemic on people living with HIV in Zimbabwe. Afr J AIDS Res. 2022;21(2):194–200. doi: 10.2989/16085906.2022.2103004. [DOI] [PubMed] [Google Scholar]
- Moyo I, Mavhandu-Mudzusi AH, Haruzivishe C. Frontline healthcare workers' experiences of providing care during the COVID-19 pandemic at a COVID-19 centre in Bulawayo, Zimbabwe: A phenomenological study. Curationis. 2022;45(1):e1–11. doi: 10.4102/curationis.v45i1.2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briand SC, Cinelli M, Nguyen T, Lewis R, Prybylski D, Valensise CM, Colizza V, Tozzi AE, Perra N, Baronchelli A, Tizzoni M, Zollo F, Scala A, Purnat T, Czerniak C, Kucharski AJ, Tshangela A, Zhou L, Quattrociocchi W. Infodemics: A new challenge for public health. Cell. 2021;184(25):6010–6014. doi: 10.1016/j.cell.2021.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chippaux JP. Outbreaks of Ebola virus disease in Africa: the beginnings of a tragic saga. J Venom Anim Toxins incl Trop Dis. 2014;20(1):44. doi: 10.1186/1678-9199-20-44. [DOI] [PMC free article] [PubMed] [Google Scholar]


