Abstract
BACKGROUND:
Insomnia is connected with a lifted hazard for neurocognitive dysfunction and psychiatric disarranges. Clinical observations of psychosomatic patients indicate that their distorted somatopsychic functioning necessitates their practice of yoga-like therapy. Sleep and its modifications and management have also been explained well in ayurveda. This study aimed to compare the effectiveness of Yoga and Nasya Karma on the sleep quality, stress, cognitive function, and quality of life of people suffering from acute insomnia.
MATERIAL AND METHODS:
It was an open-label, randomized controlled trial. A total of 120 participants were randomly (computer-generated randomization) equally allocated to three groups, yoga group (G-1), ayurveda group (G-2), and control group (G-3). All the groups were assessed on the first day before the start of the yoga regime and the 48th day. Participants in the study were included in the age group of 18 to 45 years, fulfilling DSM-V criteria for insomnia, physically fit for the yoga module, and Nasya procedure. Outcomes were measured by the Pittsburgh Sleep Quality Index (PSQI) questionnaire, Perceived Stress Scale (PSS), cognitive failure questionnaire, and WHO Quality of Life Scale-Brief (WHOQOL-Brief). Proportions and frequencies were described for categorical variables and compared using the Chi-square test. ANOVA (one-way) and post hoc analysis, Bonferroni test, were performed for multiple comparisons in groups at a significance level of P < 0.05 using SPSS (23 version).
RESULTS:
A total of 112 participants were analyzed as per protocol analysis. All groups have observed significant mean differences for stress (<0.05) and sleep quality (<0.05). All five aspects of quality of life – general health (<0.05), physical health (<0.01), psychological health (<0.05), social health (<0.05), and environmental health (<0.05) – had a significant mean difference in all three groups. All three aspects of cognitive failure, forgetfulness (<0.05), distractibility (<0.05), and false triggers (<0.01) had a significant mean difference in scores for all three groups.
CONCLUSION:
Yoga practice was effective, followed by ayurveda and the control group in reducing stress and improving sleep, cognitive function, and quality of life.
Keywords: Ayurveda, cognitive, insomnia, Nasya Karma, quality of life, sleep, stress, yoga
Introduction
Insomnia can be described as dissatisfaction with rest quality, difficulty falling asleep, frequent night arousals, and arousing prior to the morning or the desired time.[1,2] Most reports recommend predominance rates of insomnia disorder at 5% to 15%.[3,4,5] Insomnia could be an ongoing issue in 31% to 75% of patients, with more than two-thirds reporting side effects for at least 1 year.[1,5] It is additionally associated with daytime fatigue, languor, impedance in cognitive execution, and mood changes. Insomnia differs from sleep deprivation as it is challenging to rest despite having adequate opportunities.[1] Given the expanded work weight and social challenges in an advanced society, many people cannot get adequate sleep and endure sleep disturbance.[6,7,8] A detailed study shows that around 30% of grown-ups show some sleep issues.[9] Different measurements can be utilized to characterize sleep, such as sleep quality (e.g., fulfilled with sleep), sleep amount (e.g., add up to sleep time, sleep period time, time in bed), and daytime languor (e.g., the likelihood of falling asleep but alert).[10] An agreement that disturbed sleep significantly hinders physical and mental well-being has come.[11] For example, destitute sleep has been connected with a lifted hazard for cardiovascular illness, diabetes, hypertension, mortality, obesity, pain, neurocognitive dysfunction, and psychiatric disarranges.[12,13,14,15,16] Outstandingly, both sleep and stress-responsive physiological frameworks are transiently and functionally controlled by the biological process, and it has been well established that sleep incorporates a close relationship with the stress-responsive physiological frameworks.[17,18,19,20] The lack of sleep might impact bodily reactions to stress.[21,22] Poor sleep may be an imperative hazard factor for stress-related diseases, including cardiovascular illnesses and temperament disorders.[21] Besides this, insomnia is often associated with cognitive impairment, such as poor memory, attention, concentration, and performance of simple tasks.[23] Also, insomnia and its associated conditions worsen their quality of life.[24] Clinical observations of psychosomatic patients indicate that their distorted somatopsychic functioning necessitates their practice of yoga-like therapy.[25] It is emphasized that physical yogic exercise is meant to prepare the body for mental practices such as samadhi.[26] Mindfulness meditation is increasingly incorporated into mental health interventions, and its theoretical concepts have influenced basic research on psychopathology.[27] Yoga is restorative management for psychophysiological effects. It incorporates a comprehensive approach to physical, mental, and spiritual well-being.[25] Components of yoga have been explored for their viability and its practice as a comprehensive multi-component discipline.[25,28,29] Sleep and its modifications and management have also been explained well in ayurveda. Nidrä is one of the three pillars capable of supporting a healthy life. The heart is the seat of cetanä. When it is secured by thomas (numbness, haziness), all living creatures tend to fall asleep. The viewpoints of emotional well-being, nourishment, emaciation, strength and weakness, virility, cognition, life, and death depend upon ideal sleep.[30] In persons whose Kapha has diminished and vätta or pitta has expanded and those whose intellect and body are distressed by illness or bodily injury, sleep does not be satisfactory, resulting in nidränäç or sleep disorder.[31] Many herbal drugs that overcome sleep-related disorders are mentioned. Brahmi tail (Bacopa monnieri) is used for Abhyanga because of its sedative and medhya properties.[32] The present study has novelty as it aimed to compare the potential appropriateness and adequacy of a basic yoga module with Nasya Karma to alleviate stress and insomnia and consequently their cognitive function and quality of life. These practices require little preparation that can be practiced individually on an everyday premise by patients with insomnia.
Material and Methods
Study design and sample size
It was an open-label, randomized controlled trial. There were three groups in total, one for the yoga group (G-1), the second for the ayurveda group (G-2), and the third for the control group (G-3). Computer-generated randomization was performed. Participants were randomly equally allocated to three groups, yoga group (G-1), ayurveda group (G-2), and control group (G-3). All the groups were assessed on the first day before the start of the yoga regime and the 48th day. The sample size was calculated based on the previous study (Bankar et al., 2013) on the beneficial effects of yoga on insomnia.[33] The effect size and its equivalent of partial eta square with alpha 0.05 and power 0.9 with three groups and three measurements are used to estimate the sample size. The optimal sample size estimated is 100. With the assumption of attrition rate (~20%) during the study, the total sample size planned is 120.
Study setting and participants
For the present clinical study, both male and female participants were screened based on DSM-5. The participants were recruited from the out-patient department (OPD) of the Panchakarma Dept. of Ayurveda University. The study's participants were included based on the inclusion and exclusion criteria below.
Participant selection criteria
Participants from 18 to 45 years were included in the study, fulfilling DSM-V criteria for insomnia, willing to participate, and physically fit for the yoga module and the Nasya procedure. Patients had an allergy to oil application primarily through the nasal route; any severe respiratory ailments (URTI, allergic rhinitis, sinusitis, asthma); any severe psychiatric disorder (schizophrenia, mania, bipolar disorders, OCD); chronic illness (diabetes mellitus, hypertension); taking medications such as alpha-blockers, beta-blockers, corticosteroids, ace inhibitors, and statins, drug withdrawal syndromes (barbiturates, tranquilizers); substance abuse such as alcohol ingestion and withdrawal; endocrine or metabolic disorders (hypothyroidism or hyperthyroidism); and pregnant and lactating women were excluded.
Study intervention
Yoga Group (G-1): The yoga session included physical activity, relaxation, regulated breathing, and philosophical aspects. It was an integrated approach to yoga, derived from principles in ancient texts emphasizing that yoga should promote health at all levels. The session was for 60 minutes daily, 6 days a week. The yoga practices followed the approved protocol based on a paper by Dr. Manjunath and Dr. Shirley Telles, “Influence of Yoga & Ayurveda on self-rated sleep in a geriatric population.”
Yoga Nidrä – 1 day a week. Jal ëeti – 3 days in a week.
Ayurveda Group (G-2): Patients were administered in this group's Nasya (Pratimarça) procedure. As Pratimarça Nasya was a daily regimen, each sitting included two drops in each nostril for 48 days, regularly in the morning and evening.
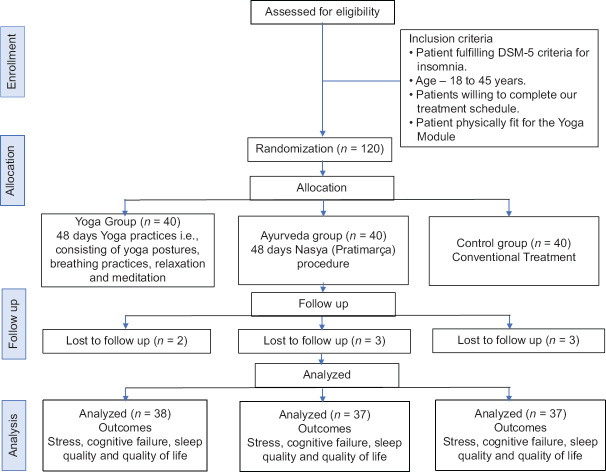
Control Group (G-3): This group followed the conventional medical treatment. Pre-post-intervention data were collected. Figure 1 CONSORT flow diagram
Figure 1.
CONSORT Flow Diagram
Data collection
Data were collected from the selected participants through four questionnaires as Pittsburgh Sleep Quality Index (PSQI), Perceived Stress Scale (PSS), cognitive failure questionnaire (CFQ), and WHO Quality of Life Scale-Brief (WHOQOL-Brief). Details about the nature of the study's intervention were explained to participants, and informed consent was taken from them.
The PSQI questionnaire measures the quality and sleeps patterns. It has seven domains measuring “good” to “poor” sleep: subjective sleep quality, sleep latency, sleep duration, sleep disturbances, habitual sleep efficiency, daytime dysfunction, and sleep medication last month. The client rates each of these seven domains of sleep. Scoring is based on a 0 to 3 scale. Scoring 3 depicts the extreme negative on the Likert Scale. A total sum of “5” or greater indicates a “poor” sleeper.[34]
The PSS is a widely used instrument for measuring stress. Stressful life events are closely associated with the onset of insomnia and are mediated by certain predisposing personality factors. Insomniacs, compared to controls, tend to be more discontent, both as children and as adults, have less satisfying inter-personal relations, and have relatively poor self-concepts, leading to inadequate coping mechanisms for dealing with stress.
All the items on this scale are easy to respond to, and alternatives are simple to grasp. All questions are general and are relatively free of content specific to any group. It consists of 25 items scored on a 5-point Likert scale ranging from 0 (never) to 4 (very often). The questions in the PSS ask about thoughts and feelings in the last month.[35]
The CFQ is used to measure standard cognitive errors. The questionnaire was designed to assess the frequency of lapses in three areas, perception, memory, and motor function and was proposed by the authors to tap a single factor coined “cognitive failures.” It is a 5-point Likert scale ranging from 0 (never) to 4 (very often). Respondents were asked to assess the number of cognitive failures within the past 4 weeks before filling out the questionnaire.[36]
For measurements of subjective quality of life (QoL), the WHOQOL-Brief was used. The WHOQOL-Brief (Field Trial Version) includes four domains and two items scored individually about overall perception of quality of life and health. The four domain scores are scaled positively. Higher scores indicate a higher quality of life. Three items of the WHOQOL Brief must be reversed before scoring.[37]
Data extraction and analysis
The data extraction was performed on the first day and the 48th day for the yoga, ayurveda, and control groups. After the pre- and post-intervention data collection, data were checked for normality, and appropriate statistical tests were applied. The Kolmogorov–Smirnov Z test checked the normality of data. The Statistical Package for Social Sciences (SPSS version 23, SPSS, Inc., Chicago, IL) is used for analysis. All quantitative variables were measured as mean, standard deviation, and standard error. Proportions and frequencies were described for categorical variables and compared using the Chi-square test. All applied statistical tests were two-sided and performed at a significance level of P < 0.05. ANOVA (One-way) was applied to explore the between- and within-group differences among three study groups. Post hoc analysis, Bonferroni test, was performed for multiple comparisons in groups.
Ethical consideration
Ethical permission was taken from the Institutional Ethical Committee (IEC). An ethical certificate number is RES/IEC-SVYASA/195/2021.
Results
Results were analyzed as per protocol analysis. A total of 112 participants were analyzed, and the drop-out rate was 6.66%. In the yoga, ayurveda, and control groups, 38, 37, and 37 participants were available post intervention, respectively. Table 1 describes the participant's sociodemographic characteristics. It showed that the mean age of participants was matched, and there was no statistically significant difference. Sociodemographic classifications were described in the table as per modified Kuppuswamy and Udai Pareekh's scale.[38]
Table 1.
Sociodemographic characteristics of participants
| Variables | Categories | Yoga Group (n=40) Frequency % | Ayurveda Group (n=40) Frequency % | Control Group (n=40) Frequency % | Sleep Quality (P) |
|---|---|---|---|---|---|
| Age (Mean±SD) | 34.6±7.07 | 32.15±6.94 | 31.8±7.24 | ||
| Gender | Male | 26 (65) | 22 (55) | 25 (62.5) | <0.05* |
| Female | 14 (35) | 18 (45) | 15 (32.5) | ||
| Educational Qualification | Up to 12th standard | 5 (12.5) | 4 (10) | 9 (22.5) | 0.21 |
| Graduation | 22 (55) | 21 (52.5) | 20 (50) | ||
| Post- Graduation | 13 (32.5) | 15 (37.5) | 11 (27.5) | ||
| Habitat | Urban | 35 (87.5) | 31 (77.5) | 32 (40) | <0.001** |
| Rural | 5 (12.5) | 9 (22.5) | 8 (20) | ||
| Marital status | Married | 32 (40) | 21 (52.5) | 24 (60) | <0.05* |
| Single | 6 (15) | 10 (25) | 13 (32.5) | ||
| Separated | 2 (5) | 9 (47.5) | 3 (7.5) | ||
| Occupation | Government job | 10 (25) | 5 (12.5) | 8 (20) | <0.01** |
| Private job | 22 (55) | 26 (65) | 12 (30) | ||
| Self-employed | 1 (2.5) | 3 (7.5) | 11 (27.5) | ||
| No occupation | 7 (17.5) | 6 (15) | 9 (22.5) | ||
| Socioeconomic Status | Lower | - | - | <0.001** | |
| Upper Lower | 3 (7.5) | 4 (10) | 2 (5) | ||
| Lower Middle | 33 (82.5) | 31 (77.5) | 29 (72.5) | ||
| Upper middle | 4 (10) | 5 (12.5) | 9 (22.5) | ||
| Upper | - | - | - | - | |
Note Chi-Square’ test, P value significant as * represents <0.05 and ** represents <0.01. SD, standard deviation
Stress and sleep quality
Results showed a significant association of selected variables such as gender (<0.05), habitat (<0.001), occupation (<0.05), marital status (<0.05), and socioeconomic status (<0.01) with sleep quality. Table 2 depicts the descriptive statistics for stress and sleep quality variables in yoga, ayurveda, and control groups. It can be noted that the post-intervention mean ± SD for a perceived stress test was the lowest in the yoga group (11.73 ± 1.96), followed by the ayurveda group (16.51 ± 4.49) and control group (17.91 ± 4.62). Accordingly, yoga practice reduced the stress level of insomnia patients more than the ayurveda and control groups.
Table 2.
Descriptive statistics for stress, sleep, cognitive failure, and quality of life variables in yoga, ayurveda, and control groups
| Dependent Variable | (I) Groups | n | Mean | Std. Deviation | Std. Error | 95% Confidence Interval for Mean | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Lower Bound | Upper Bound | ||||||
| PSS | 1 | 38 | 11.7368 | 1.96846 | 0.31933 | 11.0898 | 12.3839 |
| 2 | 37 | 16.5135 | 4.49457 | 0.73890 | 15.0149 | 18.0121 | |
| 3 | 37 | 17.9189 | 4.62108 | 0.75970 | 16.3782 | 19.4597 | |
| Total | 112 | 15.3571 | 4.67860 | 0.44209 | 14.4811 | 16.2332 | |
| PSQI | 1 | 38 | 4.6316 | 2.28297 | 0.37035 | 3.8812 | 5.3820 |
| 2 | 37 | 9.1892 | 3.80670 | 0.62582 | 7.9200 | 10.4584 | |
| 3 | 37 | 11.8649 | 6.54541 | 1.07606 | 9.6825 | 14.0472 | |
| Total | 112 | 8.5268 | 5.42095 | 0.51223 | 7.5118 | 9.5418 | |
| WHOQOL-Brief | |||||||
| General Health | 1 | 38 | 7.9211 | 1.14801 | 0.18623 | 7.5437 | 8.2984 |
| 2 | 37 | 7.0811 | 1.32032 | 0.21706 | 6.6409 | 7.5213 | |
| 3 | 37 | 6.5946 | 1.38362 | 0.22747 | 6.1333 | 7.0559 | |
| Total | 112 | 7.2054 | 1.38940 | 0.13129 | 6.9452 | 7.4655 | |
| Physical Health | 1 | 38 | 29.1053 | 3.02056 | 0.49000 | 28.1124 | 30.0981 |
| 2 | 37 | 26.1351 | 3.72799 | 0.61288 | 24.8922 | 27.3781 | |
| 3 | 37 | 22.7297 | 4.05277 | 0.66627 | 21.3785 | 24.0810 | |
| Total | 112 | 26.0179 | 4.44381 | 0.41990 | 25.1858 | 26.8499 | |
| Psychological Health | 1 | 38 | 24.2368 | 3.01738 | 0.48948 | 23.2451 | 25.2286 |
| 2 | 37 | 21.6486 | 3.19910 | 0.52593 | 20.5820 | 22.7153 | |
| 3 | 37 | 18.8378 | 4.00356 | 0.65818 | 17.5030 | 20.1727 | |
| Total | 112 | 21.5982 | 4.05916 | 0.38355 | 20.8382 | 22.3583 | |
| Social Health | 1 | 38 | 12.1842 | 1.81369 | 0.29422 | 11.5881 | 12.7804 |
| 2 | 37 | 10.7297 | 2.06355 | 0.33925 | 10.0417 | 11.4178 | |
| 3 | 37 | 9.9730 | 1.89277 | 0.31117 | 9.3419 | 10.6041 | |
| Total | 112 | 10.9732 | 2.12009 | 0.20033 | 10.5762 | 11.3702 | |
| Environment Health | 1 | 38 | 32.8684 | 3.48875 | 0.56595 | 31.7217 | 34.0151 |
| 2 | 37 | 28.8378 | 5.51520 | 0.90669 | 26.9990 | 30.6767 | |
| 3 | 37 | 25.5135 | 4.65845 | 0.76585 | 23.9603 | 27.0667 | |
| Total | 112 | 29.1071 | 5.48931 | 0.51869 | 28.0793 | 30.1350 | |
| Cognitive Failure | |||||||
| Forgetfulness | 1 | 38 | 10.2632 | 3.20206 | 0.51944 | 9.2107 | 11.3156 |
| 2 | 37 | 15.1351 | 3.35958 | 0.55231 | 14.0150 | 16.2553 | |
| 3 | 37 | 18.8649 | 6.57927 | 1.08163 | 16.6712 | 21.0585 | |
| Total | 112 | 14.7143 | 5.80529 | 0.54855 | 13.6273 | 15.8013 | |
| Distractibility | 1 | 38 | 10.8158 | 3.76940 | 0.61148 | 9.5768 | 12.0548 |
| 2 | 37 | 14.5676 | 3.64799 | 0.59973 | 13.3513 | 15.7839 | |
| 3 | 37 | 17.0541 | 6.81072 | 1.11968 | 14.7832 | 19.3249 | |
| Total | 112 | 14.1161 | 5.54709 | 0.52415 | 13.0774 | 15.1547 | |
| False triggers | 1 | 38 | 11.0789 | 3.07897 | 0.49948 | 10.0669 | 12.0910 |
| 2 | 37 | 15.5135 | 4.66441 | 0.76682 | 13.9583 | 17.0687 | |
| 3 | 37 | 17.5405 | 7.42965 | 1.22143 | 15.0634 | 20.0177 | |
| Total | 112 | 14.6786 | 5.95965 | 0.56313 | 13.5627 | 15.7945 | |
Note: PSS, Perceived Stress Scale; PSQI, Pittsburgh Sleep Quality Scale; WHOQOL-Brief, WHO Quality of Life Scale-Brief; Std., standard; Sig., significant. Groups: 1, Yoga; 2, Ayurveda; 3, Control
Simultaneously, participants’ sleep quality was also improved in the yoga group (4.63 ± 2.28), followed by the ayurveda group (9.18 ± 3.80) and control group (11.86 ± 6.54). The lowest mean value can be observed in the yoga group. Table 3 describes the results of the ANOVA (one-way) test. All groups have observed that stress variables had significant mean differences (F-26.275, P value 0.011). Participants’ sleep quality also had a significant mean difference (F-24.271, P value 0.021) in all groups.
Table 3.
Mean differences for stress, sleep, cognitive failure, and quality of life in yoga, ayurveda, and control groups
| Sum of Squares | Mean Square | F | Sig. | ||
|---|---|---|---|---|---|
| PSS | Between Groups | 790.346 | 395.173 | 26.275 | <0.01** |
| Within Groups | 1639.368 | 15.040 | |||
| Total | 2429.714 | ||||
| PSQI | Between Groups | 1005.078 | 502.539 | 24.271 | <0.05* |
| Within Groups | 2256.842 | 20.705 | |||
| Total | 3261.920 | ||||
| WHOQOL-Brief | |||||
| General Health | Between Groups | 33.838 | 16.919 | 10.220 | <0.05* |
| Within Groups | 180.439 | 1.655 | |||
| Total | 214.277 | ||||
| Physical health | Between Groups | 762.764 | 381.382 | 29.087 | <0.01** |
| Within Groups | 1429.201 | 13.112 | |||
| Total | 2191.964 | ||||
| Psychological health | Between Groups | 546.592 | 273.296 | 23.231 | <0.05* |
| Within Groups | 1282.328 | 11.764 | |||
| Total | 1828.920 | ||||
| Social health | Between Groups | 94.939 | 47.469 | 12.808 | <0.05* |
| Within Groups | 403.981 | 3.706 | |||
| Total | 498.920 | ||||
| Environment health | Between Groups | 1018.102 | 509.051 | 23.849 | <0.01* |
| Within Groups | 2326.612 | 21.345 | |||
| Total | 3344.714 | ||||
| Cognitive Failure | |||||
| Forgetfulness | Between Groups | 1396.840 | 698.420 | 32.477 | <0.05* |
| Within Groups | 2344.017 | 21.505 | |||
| Total | 3740.857 | ||||
| Distractibility | Between Groups | 740.808 | 370.404 | 15.095 | <0.05* |
| Within Groups | 2674.683 | 24.538 | |||
| Total | 3415.491 | ||||
| False triggers | Between Groups | 821.233 | 410.616 | 14.340 | <0.01** |
| Within Groups | 3121.196 | 28.635 | |||
| Total | 3942.429 |
PSS, Perceived Stress Scale; PSQI, Pittsburgh Sleep Quality Scale; WHOQOL-Brief, WHO Quality of Life Scale-Brief; Std., standard; significant mean difference; * represents <0.05 and ** represents <0.01. Sig., significant. Groups: 1, Yoga; 2, Ayurveda; 3, Control
Quality of life
Table 2 also describes the participants’ quality of life scores under sub-heads of general health, physical health, psychological health, social health, and environment health in all groups. In the yoga group, general health scores (7.92 ± 1.14) were nearly similar to those in the ayurveda group (7.08 ± 1.32) but higher than those in the control group (6.54 ± 1.38).
Physical health scores were the highest in the yoga group (29.10 ± 3.02) compared to the ayurveda (26.13 ± 3.72) and control groups (22.72 ± 4.05). The psychological, social, and environmental health scores of participants were improved in the yoga group compared to the ayurveda and control groups [Table 2].
All five aspects, general health (F-10.220, P value 0.038), physical health (F-29.087, P value 0.001), psychological health (F-23.23, P value 0.021), social health (F-12.808, P value 0.045), and environmental health (F-23.849, P value 0.013) had a significant mean difference in all three groups.
Cognitive function
The cognitive Failure questionnaire has been divided into three aspects – forgetfulness, distractibility, and false triggers. Post-intervention mean scores for forgetfulness were the lowest in the yoga group (10.2632 ± 3.20206) compared to the ayurveda (15.1351 ± 3.35958) and control groups (18.8649 ± 6.57927). Distractibility scores were also the lowest in the yoga group (10.8158 ± 3.76940) compared to other groups. The table also depicted the lower and upper bounds with a standard error for all outcomes in each group [Table 2].
All three aspects, forgetfulness (F-32.477, P value 0.011), distractibility (F-15.095, P value 0.020), and false triggers (F-14.340, P value 0.001), had significant mean differences in scores for all three groups [Table 3]. Post hoc analysis was also applied for multiple comparisons, values which show a significant difference in all groups [Tables 4-6].
Table 4.
Multiple comparisons for stress and sleep quality in all groups
| Dependent Variable | (I) Groups | (J) Groups | MD (I-J) | Std. Error | Sig. | 95% Confidence Interval | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Lower Bound | Upper Bound | ||||||
| PSS | 1 | 2 | -4.77667* | 0.89570 | <0.01** | -6.9546 | -2.5988 |
| 3 | -6.18208* | 0.89570 | <0.05* | -8.3600 | -4.0042 | ||
| 2 | 1 | 4.77667* | 0.89570 | <0.01** | 2.5988 | 6.9546 | |
| 3 | -1.40541 | 0.90165 | 0.366 | -3.5978 | 0.7870 | ||
| 3 | 1 | 6.18208* | 0.89570 | <0.01** | 4.0042 | 8.3600 | |
| 2 | 1.40541 | 0.90165 | 0.366 | -0.7870 | 3.5978 | ||
| PSQI | 1 | 2 | -4.55761* | 1.05093 | <0.01** | -7.1129 | -2.0023 |
| 3 | -7.23329* | 1.05093 | <0.05* | -9.7886 | -4.6780 | ||
| 2 | 1 | 4.55761* | 1.05093 | <0.05* | 2.0023 | 7.1129 | |
| 3 | -2.67568* | 1.05792 | <0.05* | -5.2480 | -0.1034 | ||
| 3 | 1 | 7.23329* | 1.05093 | <0.01** | 4.6780 | 9.7886 | |
| 2 | 2.67568* | 1.05792 | <0.05* | 0.1034 | 5.2480 | ||
Note: Post hoc analysis, Bonferroni test for multiple comparisons. PSS, Perceived Stress Scale; PSQI, Pittsburgh Sleep Quality Scale; Std., Standard; Significant mean difference; * represents <0.05 and ** represents <0.01. Sig., significant, MD Mean Difference. Groups: 1, Yoga; 2, Ayurveda; 3, Control
Table 6.
Multiple comparisons for cognitive function in all groups
| Dependent Variable | (I) Groups | (J) Groups | Mean Difference (I-J) | Std. Error | Sig. | 95% Confidence Interval | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Lower Bound | Upper Bound | ||||||
| Forgetfulness | 1 | 2 | -4.87198* | 1.07104 | <0.05* | -7.4762 | -2.2678 |
| 3 | -8.60171* | 1.07104 | <0.05* | -11.2059 | -5.9975 | ||
| 2 | 1 | 4.87198* | 1.07104 | 0.060 | 2.2678 | 7.4762 | |
| 3 | -3.72973* | 1.07816 | <0.05* | -6.3513 | -1.1082 | ||
| 3 | 1 | 8.60171* | 1.07104 | <0.001** | 5.9975 | 11.2059 | |
| 2 | 3.72973* | 1.07816 | <0.05* | 1.1082 | 6.3513 | ||
| Distractibility | 1 | 2 | -3.75178* | 1.14409 | <0.001** | -6.5336 | -0.9699 |
| 3 | -6.23826* | 1.14409 | <0.05* | -9.0201 | -3.4564 | ||
| 2 | 1 | 3.75178* | 1.14409 | <0.05* | 0.9699 | 6.5336 | |
| 3 | -2.48649 | 1.15169 | 0.099 | -5.2868 | 0.3138 | ||
| 3 | 1 | 6.23826* | 1.14409 | <0.001** | 3.4564 | 9.0201 | |
| 2 | 2.48649 | 1.15169 | 0.099 | -0.3138 | 5.2868 | ||
| False triggers | 1 | 2 | -4.43457* | 1.23591 | <0.01** | -7.4397 | -1.4295 |
| 3 | -6.46159* | 1.23591 | <0.01** | -9.4667 | -3.4565 | ||
| 2 | 1 | 4.43457* | 1.23591 | <0.001** | 1.4295 | 7.4397 | |
| 3 | -2.02703 | 1.24412 | 0.318 | -5.0521 | 0.9980 | ||
| 3 | 1 | 6.46159* | 1.23591 | <0.001** | 3.4565 | 9.4667 | |
| 2 | 2.02703 | 1.24412 | 0.318 | -0.9980 | 5.0521 | ||
Note: Post hoc analysis, Bonferroni test, for multiple comparisons. PSS, Perceived Stress Scale; PSQI, Pittsburgh Sleep Quality Scale; WHOQOL-Brief, WHO Quality of Life Scale-Brief; Std., Standard; significant mean difference; * represents <0.05 and ** represents <0.01. Sig., significant; MD, mean difference; LB, lower bound; UB, upper bound. Groups: 1, Yoga; 2, Ayurveda; 3, Control
Table 5.
Multiple comparisons for quality of life in all groups
| Dependent Variable | (I) Groups | (J) Groups | Mean Difference (I-J) | Std. Error | Sig. | 95% Confidence Interval | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Lower Bound | Upper Bound | ||||||
| WHOQOL-Brief | |||||||
| General Health | 1 | 2 | 0.83997* | 0.29716 | <0.05* | 0.1174 | 1.5625 |
| 3 | 1.32646* | 0.29716 | <0.01** | 0.6039 | 2.0490 | ||
| 2 | 1 | -0.83997* | 0.29716 | <0.05* | -1.5625 | -0.1174 | |
| 3 | 0.48649 | 0.29913 | 0.320 | -0.2409 | 1.2138 | ||
| 3 | 1 | -1.32646* | 0.29716 | <0.01** | -2.0490 | -0.6039 | |
| 2 | -0 0.48649 | 0.29913 | 0.320 | -1.2138 | 0.2409 | ||
| Physical health | 1 | 2 | 2.97013* | 0.83632 | <0.01** | 0.9366 | 5.0036 |
| 3 | 6.37553* | 0.83632 | <0.01** | 4.3420 | 8.4090 | ||
| 2 | 1 | -2.97013* | 0.83632 | <0.01** | -5.0036 | -0.9366 | |
| 3 | 3.40541* | 0.84187 | <0.05* | 1.3584 | 5.4524 | ||
| 3 | 1 | -6.37553* | 0.83632 | <0.05* | -8.4090 | -4.3420 | |
| 2 | -3.40541* | 0.84187 | <0.05* | -5.4524 | -1.3584 | ||
| Psychological health | 1 | 2 | 2.58819* | 0.79218 | <0.01** | 0.6620 | 4.5144 |
| 3 | 5.39900* | 0.79218 | <0.01** | 3.4728 | 7.3252 | ||
| 2 | 1 | -2.58819* | 0.79218 | <0.01** | -4.5144 | -0.6620 | |
| 3 | 2.81081* | 0.79744 | <0.01** | 0.8718 | 4.7498 | ||
| 3 | 1 | -5.39900* | 0.79218 | <0.001** | -7.3252 | -3.4728 | |
| 2 | -2.81081* | 0.79744 | <0.001** | -4.7498 | -0.8718 | ||
| Social health | 1 | 2 | 1.45448* | 0.44464 | <0.05* | 0.3734 | 2.5356 |
| 3 | 2.21124* | 0.44464 | <0.001** | 1.1301 | 3.2924 | ||
| 2 | 1 | -1.45448* | 0.44464 | <0.05** | -2.5356 | -0.3734 | |
| 3 | 0.75676 | 0.44759 | 0.281 | -0.3316 | 1.8451 | ||
| 3 | 1 | -2.21124* | 0.44464 | <0.001** | -3.2924 | -1.1301 | |
| 2 | -0.75676 | 0.44759 | 0.281 | -1.8451 | 0.3316 | ||
| Environment | 1 | 2 | 4.03058* | 1.06705 | <0.001** | 1.4361 | 6.6251 |
| 3 | 7.35491* | 1.06705 | <0.001** | 4.7604 | 9.9494 | ||
| 2 | 1 | -4.03058* | 1.06705 | <0.01** | -6.6251 | -1.4361 | |
| 3 | 3.32432* | 1.07414 | <0.01** | 0.7126 | 5.9361 | ||
| 3 | 1 | -7.35491* | 1.06705 | <0.01** | -9.9494 | -4.7604 | |
| 2 | -3.32432* | 1.07414 | <0.05* | -5.9361 | -0.7126 | ||
Note: post hoc analysis, Bonferroni test, for multiple comparisons. WHOQOL-Brief, WHO Quality of Life Scale-Brief; Std., Standard; significant mean difference; *represents <0.05 and ** represents <0.01. Sig., significant; MD, mean difference; LB, lower bound; UB, upper bound. Groups: 1, Yoga; 2, Ayurveda; 3, Control
Discussion
Acute insomnia is considered an emotional disorder. It is associated with specific personality traits in patients.[2,3] As yoga aims to bring consensus between mind and body,[26,27] this study assessed the effectiveness of a basic set of yoga exercises, requiring little preparation that patients can practice individually on an everyday premise with insomnia. The study compared the results with ayurveda and standard care. This randomized control trial describes yoga as a helpful therapy for acute insomnia patients. After an intervention, participants in the yoga group improved global sleep quality, subjective sleep quality, wake-after-sleep onset, daytime dysfunction, and sleep efficiency compared with ayurveda and standard care. In the same group, we also found stress reduction and improved cognitive function and quality of life. Because of physiopathology, insomnia is associated with increased psychological symptoms, cognitive dysfunction, perceived stress, and poor quality of life as precipitating and perpetuating factors.[39,40] Increasing melatonin levels and anxiety reduction affect sleep quality and confirm yoga's effectiveness in stress reduction.[41] Morning yoga exercise enhances night parasympathetic drive and more curative sleep. In addition, the probable mechanisms were linked to the cognitive structuring effects of the yoga practice.[42] Consistently, studies have reported improvement in objective sleep quality, even measuring by polysomnography and sleep diary.[43,44] Yoga reduces stress and improves general health in the young population by reducing sympathetic activity.[45] Another trial with a mindfulness program for stress reduction suggested significant effects on stress, anxiety, and cognitive emotion regulation (P < 001).[46] Even yoga was safe and effective in improving sleep quality and life in older adults.[47] One week of residential yoga training program reduced the occupational stress in the participants aged 40–59.[48] A quasi-experimental study states the effectiveness of yoga in coping with stress and anxiety and enhancing happiness in professional students.[49]
According to ayurveda, an individual's nature (Prakriti in Sanskrit) could consist of different doshas, with one dosha being predominant in some cases. Ayurveda looks at several aspects of an individual's lifestyle.[50] The present study found improvement in sleep quality and reduction in stress with improvement in cognitive function and, ultimately, the quality of life in the ayurveda group compared to standard therapy. However, the scores were not like those of yoga practice but improved compared to standard therapy. Therefore, the role of ayurveda cannot be neglected in patients with insomnia. Previous studies have come up with biochemical, hematological, and physiological variations in different Prakriti, and sleep is also considered to be influenced by psychological factors.[51] Studies also claimed its effectiveness in enhancing memory and cognitive functions.[52,53] Few studies suggested the failure of short-term effects of Bacopa monnieri supplementation to improve sleep patterns and quality of life in comparison to the placebo in adults with insomnia.[54] In contrast, another trial on healthy adults identified mood-enhancing effects and reduced cortisol levels, evincing a physiological mechanism for cognitive stress reduction with supplementation of Bacopa monnieri. It was evidenced that Bacopa monnieri supplementation produced some adaptogenic and nootropic effects.[55] A systematic review of six randomized controlled trials observed that Bacopa improves memory-free recall and cognitive abilities in studies across the cognitive domains.[56] Evidence from animal trials has consistently suggested its anxiolytic or antidepressant effects.[57,58] One trial has explored its safety and efficacy in enhancing cognitive performance in participants with age 65 or more.[59]
After discussing studies with yoga and ayurveda practice in reducing stress and improving sleep quality, cognitive function, and quality of life, it needs to emphasize that the present study's results with yoga practice are consistent with previous studies. However, the availability of limited literature with similar efficacy of ayurveda emphasized further research for its acceptance in reducing stress and improving sleep quality, cognitive function, and quality of life.
Strength and limitations
The present study compared the two interventions (Yoga and Nasya karma) individually with the control group in the same population. The sample size was also adequate, and the drop-out rate was meager compared to other studies in the same intervention. However, it was an open-label trial. Subjective questionnaires were used to measure and compare the results.
Conclusion
The study concluded that yoga as a holistic treatment could bring significant changes in insomnia patients and help with various psychosocial and cognitive parameters, which can ultimately help alleviate stress and improve the quality of life compared to ayurveda and standard therapy. A vital advantage of the yoga intervention is its recognition and acceptance as a health practice, which should also add to the attractiveness of such a treatment for insomnia patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Vahia VN. Diagnostic and statistical manual of mental disorders 5: A quick glance. Indian J Psychiatry. 2013;55:220–3. doi: 10.4103/0019-5545.117131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sateia MJ. International classification of sleep disorders-third edition: Highlights and modifications. Chest. 2014;146:1387–94. doi: 10.1378/chest.14-0970. [DOI] [PubMed] [Google Scholar]
- 3.Ohayon MM, Reynolds CF., 3rd Epidemiological and clinical relevance of insomnia diagnosis algorithms according to the DSM-IV and the International Classification of Sleep Disorders (ICSD) Sleep Med. 2009;10:952–60. doi: 10.1016/j.sleep.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morin CM, LeBlanc M, Bélanger L, Ivers H, Mérette C, Savard J. Prevalence of insomnia and its treatment in Canada. Can J Psychiatry. 2011;56:540–8. doi: 10.1177/070674371105600905. [DOI] [PubMed] [Google Scholar]
- 5.Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379:1129–41. doi: 10.1016/S0140-6736(11)60750-2. [DOI] [PubMed] [Google Scholar]
- 6.Bixler E. Sleep and society: An epidemiological perspective. Sleep Med. 2009;10(Suppl 1):S3–6. doi: 10.1016/j.sleep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Owens J. Classification and epidemiology of childhood sleep disorders. Prim Care. 2008;35:533–46. doi: 10.1016/j.pop.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Shochat T. Impact of lifestyle and technology developments on sleep. Nat Sci Sleep. 2012;4:19–31. doi: 10.2147/NSS.S18891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Léger D, Poursain B, Neubauer D, Uchiyama M. An international survey of sleeping problems in the general population. Curr Med Res Opin. 2008;24:307–17. doi: 10.1185/030079907x253771. [DOI] [PubMed] [Google Scholar]
- 10.Buysse DJ. Sleep health: Can we define it? Does it matter. Sleep. 2014;37:9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matricciani L, Bin YS, Lallukka T, Kronholm E, Wake M, Paquet C, et al. Rethinking the sleep-health link. Sleep Health. 2018;4:339–48. doi: 10.1016/j.sleh.2018.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Cox RC, Olatunji BO. Sleep in the anxiety-related disorders: A meta-analysis of subjective and objective research. Sleep Med Rev. 2020;51:101282. doi: 10.1016/j.smrv.2020.101282. [DOI] [PubMed] [Google Scholar]
- 13.Grandner MA. Sleep, health, and society. Sleep Med Clin. 2017;12:1–22. doi: 10.1016/j.jsmc.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guo X, Zheng L, Wang J, Zhang X, Zhang X, Li J, et al. Epidemiological evidence for the link between sleep duration and high blood pressure: A systematic review and meta-analysis. Sleep Med. 2013;14:324–32. doi: 10.1016/j.sleep.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Pandi-Perumal SR, Monti JM, Burman D, Karthikeyan R, BaHammam AS, Spence DW, et al. Clarifying the role of sleep in depression: A narrative review. Psychiatry Res. 2020;291:113239. doi: 10.1016/j.psychres.2020.113239. [DOI] [PubMed] [Google Scholar]
- 16.Thomas SJ, Calhoun D. Sleep, insomnia, and hypertension: Current findings and future directions. J Am Soc Hypertens. 2017;11:122–9. doi: 10.1016/j.jash.2016.11.008. [DOI] [PubMed] [Google Scholar]
- 17.Antonijevic IA, Steiger A. Depression-like changes of the sleep-EEG during high dose corticosteroid treatment in patients with multiple sclerosis. Psychoneuroendocrinology. 2003;28:780–95. doi: 10.1016/s0306-4530(02)00085-9. [DOI] [PubMed] [Google Scholar]
- 18.Hori H, Teraishi T, Sasayama D, Ozeki Y, Matsuo J, Kawamoto Y, et al. Poor sleep is associated with exaggerated cortisol response to the combined dexamethasone/CRH test in a non-clinical population. J Psychiatr Res. 2011;45:1257–63. doi: 10.1016/j.jpsychires.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 19.Steiger A, Dresler M, Kluge M, Schüssler P. Pathology of sleep, hormones and depression. Pharmacopsychiatry. 2013;46(Suppl 1):S30–5. doi: 10.1055/s-0033-1337921. [DOI] [PubMed] [Google Scholar]
- 20.Van Reeth O, Weibel L, Spiegel K, Leproult R, Dugovic C, Maccari S. PHYSIOLOGY OF SLEEP (REVIEW)–Interactions between stress and sleep: From basic research to clinical situations. Sleep Med Rev. 2000;4:201–19. [Google Scholar]
- 21.Meerlo P, Sgoifo A, Suchecki D. Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems, and stress responsivity. Sleep Med Rev. 2008;12:197–210. doi: 10.1016/j.smrv.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 22.van Dalfsen JH, Markus CR. The influence of sleep on human hypothalamic-pituitary-adrenal (HPA) axis reactivity: A systematic review. Sleep Med Rev. 2018;39:187–94. doi: 10.1016/j.smrv.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 23.Hamdy RC, Kinser A, Dickerson K, Kendall-Wilson T, Depelteau A, Copeland R, et al. Insomnia and mild cognitive impairment. Gerontol Geriatr Med. 2018;4:2333721418778421. doi: 10.1177/2333721418778421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ishak WW, Bagot K, Thomas S, Magakian N, Bedwani D, Larson D, et al. Quality of life in patients suffering from insomnia. Innov Clin Neurosci. 2012;9:13–26. [PMC free article] [PubMed] [Google Scholar]
- 25.Goyeche JR. Yoga as therapy in psychosomatic medicine. Psychother Psychosom. 1979;31:373–81. doi: 10.1159/000287361. [DOI] [PubMed] [Google Scholar]
- 26.Michalsen A, Kessler C. Science-based yoga-Stretching mind, body, and soul. Forsch Komplementmed. 2013;20:176–8. doi: 10.1159/000353542. [DOI] [PubMed] [Google Scholar]
- 27.Wielgosz J, Goldberg SB, Kral TRA, Dunne JD, Davidson RJ. Mindfulness Meditation and Psychopathology. Annu Rev Clin Psychol. 2019;15:285–316. doi: 10.1146/annurev-clinpsy-021815-093423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sharma I, Singh P. Treatment of neurotic illnesses by yogic techniques. Indian J Med Sci. 1989;43:76–9. [PubMed] [Google Scholar]
- 29.Raub JA. Psychophysiologic effects of Hatha Yoga on musculoskeletal and cardiopulmonary function: A literature review. J Altern Complement Med. 2002;8:797–812. doi: 10.1089/10755530260511810. [DOI] [PubMed] [Google Scholar]
- 30.Astanga Hrudayam with Sarvanga Sundara Commentary of Arunadatta and Ayurveda rasayana of Hemadri. (sutrasthana,) Edited by Bhisagacharya Hari Shastri Paradakara Vaidya; Chaukhamba Orientalia. Varanasi. 2009;8:14–4. [Google Scholar]
- 31.Murthy KR Srikanth, Sushruta Samhita by Acharya Susruta, English translation, Reprint Varanasi, Chaukhambha Orientalia. 2010;24:1–222. [Google Scholar]
- 32.Sastri J L N, Vijnana D. Knowledge on vedic herbs, controversial herbs and ignored medicinal plants. Chaukhamba Orientalia Varanasi. 2011;5:86. [Google Scholar]
- 33.Bankar MA, Chaudhari SK, Chaudhari KD. Impact of long term Yoga practice on sleep quality and quality of life in the elderly. J Ayurveda Integr Med. 2013;4:28–32. doi: 10.4103/0975-9476.109548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Buysse D, Reynolds C, Monk T, Berman S, Kupfer D. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 35.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–96. [PubMed] [Google Scholar]
- 36.Broadbent DE, Cooper PF, FitzGerald P, Parkes KR. The Cognitive Failures Questionnaire (CFQ) and its correlates. Br J Clin Psychol. 1982;21:1–16. doi: 10.1111/j.2044-8260.1982.tb01421.x. [DOI] [PubMed] [Google Scholar]
- 37.The WHOQOL Group. The World Health Organization Quality of Life assessment (WHOQOL): Development and general psychometric properties. Soc Sci Med. 1998;46:1569–85. doi: 10.1016/s0277-9536(98)00009-4. [DOI] [PubMed] [Google Scholar]
- 38.Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh's scale updated for 2019. J Family Med Prim Care. 2019;8:1846–9. doi: 10.4103/jfmpc.jfmpc_288_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kozasa EH, Hachul H, Monson C, Pinto L, Jr, Garcia MC, Mello LE, et al. Mind-body interventions for the treatment of insomnia: A review. Braz J Psychiatry. 2010;32:437–43. doi: 10.1590/s1516-44462010000400018. [DOI] [PubMed] [Google Scholar]
- 40.Ellis JG, Perlis ML, Espie CA, Grandner MA, Bastien CH, Barclay NL, et al. The natural history of insomnia: Predisposing, precipitating, coping, and perpetuating factors over the early developmental course of insomnia. Sleep. 2021;44:zsab095. doi: 10.1093/sleep/zsab095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ferracioli-Oda E, Qawasmi A, Bloch MH. Meta-analysis: Melatonin for the treatment of primary sleep disorders. PLoS One. 2013;8:e63773. doi: 10.1371/journal.pone.0063773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deepak KK. Neurophysiological mechanisms of induction of meditation: A hypothetico-deductive approach. Indian J Physiol Pharmacol. 2002;46:136–58. [PubMed] [Google Scholar]
- 43.Williams J, Roth A, Vatthauer K, Mc Crae CS. Cognitive behavioral treatment of insomnia. Chest J. 2013;143:554. doi: 10.1378/chest.12-0731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carney CE, Buysse DJ, Ancoli-Israel S, Edinger JD, Krystal AD, Lichstein KL, et al. The consensus sleep diary: Standardizing prospective sleep self-monitoring. Sleep. 2012;35:287–302. doi: 10.5665/sleep.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tripathi MN, Kumari S, Ganpat TS. Psychophysiological effects of yoga on stress in college students. J Educ Health Promot. 2018;7:43. doi: 10.4103/jehp.jehp_74_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shahidi S, Akbari H, Zargar F. Effectiveness of mindfulness-based stress reduction on emotion regulation and test anxiety in female high school students. J Educ Health Promot. 2017;6:87. doi: 10.4103/jehp.jehp_98_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Halpern J, Cohen M, Kennedy G, Reece J, Cahan C, Baharav A. Yoga for improving sleep quality and quality of life for older adults. Altern Ther Health Med. 2014;20:37–46. [PubMed] [Google Scholar]
- 48.Verma A, Shete SU, Doddoli G. Impact of residential yoga training on occupational stress and health promotion in principals. J Educ Health Promot. 2020;9:30. doi: 10.4103/jehp.jehp_394_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kinchen E, Loerzel V, Portoghese T. Yoga and perceived stress, self-compassion, and quality of life in undergraduate nursing students. J Educ Health Promot. 2020;9:292. doi: 10.4103/jehp.jehp_463_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Balkrishna A. A practical approach to the science of ayurveda: A comprehensive guide for healthy living. Haridwar, India: Divya Prakashan, Divya Yoga Mandir Trust; 2013. [Google Scholar]
- 51.Tripathi PK, Patwardhan K, Singh G. The basic cardiovascular responses to postural changes, exercise, and cold pressor test: Do they vary in accordance with the dual constitutional types of ayurveda? Evid Based Complement Alternat Med 2011. 2011:251850. doi: 10.1155/2011/251850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schlebusch L, Bosch BA, Polglase G, Kleinschmidt I, Pillay BJ, Cassimjee MH. A double-blind, placebo-controlled, double-centre study of the effects of an oral multivitamin-mineral combination on stress. S Afr Med J. 2000;90:1216–23. [PubMed] [Google Scholar]
- 53.Murphy BM, Frigo LC. Development, implementation, and results of a successful multidisciplinary adverse drug reaction reporting program in a university teaching hospital. Hosp Pharm. 1993;28:1199–204. [PubMed] [Google Scholar]
- 54.Lopresti AL, Smith SJ, Ali S, Metse AP, Kalns J, Drummond PD. Effects of a Bacopa monnieri extract (Bacognize®) on stress, fatigue, quality of life and sleep in adults with self-reported poor sleep: A randomised, double-blind, placebo-controlled study. J Funct Foods. 2021;85:104671. [Google Scholar]
- 55.Benson S, Downey LA, Stough C, Wetherell M, Zangara A, Scholey A. An Acute, Double-Blind, Placebo-Controlled Cross-over Study of 320 mg and 640 mg Doses of Bacopa monnieri (CDRI 08) on Multitasking Stress Reactivity and Mood. Phytother Res. 2014;28:551–9. doi: 10.1002/ptr.5029. [DOI] [PubMed] [Google Scholar]
- 56.Pase MP, Kean J, Sarris J, Neale C, Scholey AB, Stough C. The cognitive-enhancing effects of Bacopa monnieri: A systematic review of randomized, controlled human clinical trials. J Altern Complement Med. 2012;18:647–52. doi: 10.1089/acm.2011.0367. [DOI] [PubMed] [Google Scholar]
- 57.Hazra S, Kumar S, Saha GK, Mondal AC. Reversion of BDNF, Akt and CREB in Hippocampus of Chronic Unpredictable Stress Induced Rats: Effects of Phytochemical, Bacopa Monnieri. Psychiatry Investig. 2017;14:74–80. doi: 10.4306/pi.2017.14.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zu X, Zhang M, Li W, Xie H, Lin Z, Yang N, et al. Antidepressant-like effect of bacopaside I in mice exposed to chronic unpredictable mild stress by modulating the hypothalamic-pituitary-adrenal axis function and activating BDNF signaling pathway. Neurochem Res. 2017;42:3233–44. doi: 10.1007/s11064-017-2360-3. [DOI] [PubMed] [Google Scholar]
- 59.Calabrese C, Gregory WL, Leo M, Kraemer D, Bone K, Oken B. Effects of a standardized Bacopa monnieri extract on cognitive performance, anxiety, and depression in the elderly: A randomized, double-blind, placebo-controlled trial. J Altern Complement Med. 2008;14:707–13. doi: 10.1089/acm.2008.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]