Abstract
Background
Healthcare professionals are highly likely to experience various causes of work-related stress, which often leads to burnout. This became even more obvious during the Covid-19 pandemic. This systematic review aimed to analyze articles where psychological interventions with elements of mindfulness (PIM) were used to support healthcare professionals to foster well-being and reduce burnout levels. Compared to other recently published reviews, it is unique, due to its focus on a wide group of healthcare professionals, a broader selection of psychological interventions, and the evaluation of any sustained effects.
Methods
Systematic searches were carried out in February 2021 with different combinations of Boolean operators within six electronic databases: PubMed, EBSCOhost, MEDLINE, PsycArticles, Cochrane Library, JSTOR and Cobiss. We included articles that had been published in the last ten years (2011 to 2021) and which reported on original research focused on evaluating the influence of PIM on healthcare professionals. MERSQI was used to assess the quality of the included studies.
Results
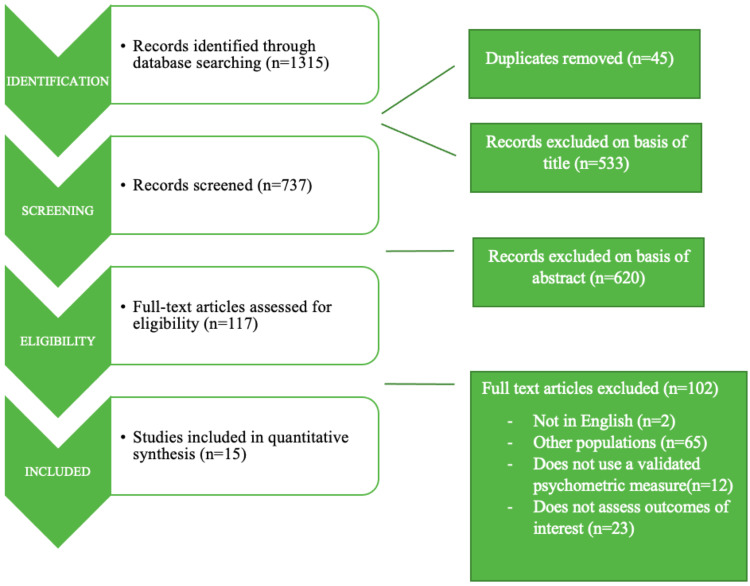
Of 1315 identified studies, 15 were included in this systematic review. Regardless of the specific type, duration and setting (individual vs group) of PIM applied, the results demonstrated a positive impact on well-being and burnout in participating healthcare professionals. The most studied interventions involved MBSR (mindfulness-based stress reduction) and other mindfulness training programmes, in online as well as in-person versions.
Conclusion
Given the new reality with the presence of the SARS-Cov-2 virus, it is of the utmost importance to offer feasible, effective interventions for burnout reduction to vulnerable groups of healthcare professionals. By focusing on their needs, several key aspects of burnout and mindfulness could be efficiently improved; this review demonstrates that short, online interventions could be as effective as longer, in-person ones.
Keywords: mindfulness, burnout, perceived stress, well-being, Covid-19, MBSR
Introduction
Healthcare professionals (HCP) are a vulnerable population as they are highly likely to experience various causes of work-related stress.1 During the Covid-19 pandemic the existing risk was heightened, as HCP were often exposed to close contact with infected patients, an excessive workload, constantly changing protocols, and subsequent physical and emotional exhaustion.2,3 As a consequence, we are currently facing high burnout rates in a variety of HCP, including physicians, nurses, psychologists, and others.3–6 A recent Canadian survey revealed that over 40% of nurses reported burnout.7 Studies conducted in China during the Covid-19 outbreak showed high rates of sleep problems, psychological distress, anxiety, and depressive symptoms in more than 70% of samples of surveyed HCP.2 Similarly, in Spain over 80% of HCP working during the Covid-19 pandemic reported psychological distress.8
The current situation in healthcare worldwide can be harmful for HCP and their organizations,9,10 as burnout in HCP adversely affects quality of care and threatens professionalism.11,12 At the organizational level, burnout has been related to low performance, high turnover intentions, suboptimal care, and medical errors.13 These are solid arguments for the crucial importance of safeguarding the mental health of HCP, and thus improving the success of healthcare delivery.2
There have been several training programmes developed recently to combat burnout and improve the wellbeing of HCP; however, mindfulness training is one of the most thoroughly studied worldwide. Mindfulness is defined as an awareness which arises when paying attention to the present moment without judgement, with openness, acceptance, and curiosity.14 In 1977, Jon Kabat-Zinn began developing MBSR (mindfulness-based stress reduction) for application in healthcare, by integrating Buddhist and other contemplative practices with modern psychological knowledge about stress coping and resilience.15 Mindfulness training has been implemented for HCP as a means of decreasing burnout, improving patient care, and increasing satisfaction at work.16,17 Krasner et al18 working with primary physicians, concluded that modified MBSR training resulted in improvements in different aspects of burnout, empathy, and mindfulness. Training also resulted in more emotional stability, higher work engagement, and better responsiveness to patients’ problems. A recent study for frontline health workers during the Covid-19 outbreak in Spain confirmed the feasibility, safety and effectiveness of a brief on-site mindfulness-based intervention designed to reduce stress.2 Our previous systematic review, conducted in 2021, which was focused on the professional group of physicians, also confirmed that regardless of the specific type of psychological intervention with mindfulness (PIM) used, the results demonstrated a positive impact on empathy and well-being, and a reduction in burnout in the participating physicians.19
Given the high workload burden, and understanding the existing challenges of the Covid-19 pandemic, it is very important to be able to offer feasible, easily accessible interventions, which take the least time for the effective burnout prevention for vulnerable groups of HCP.
In this systematic review, we wanted to find out:
Are PIMs effective in reducing burnout among healthcare professionals?
What are the differences in effectiveness of PIMs with regard to their formats (online vs in-person), duration, and setting (individual vs group)?
Materials and Methods
This review analyzes the effect of psychological interventions with elements of mindfulness (PIM) on reduction of burnout and increased well-being for a group of healthcare professionals. In one way, it is a continuation and upgrade of a previously published paper by the same authors19 which focused on a target group of physicians.
The review is reported according to the PRISMA guidelines.20
Search Strategy
Systematic searches were conducted in February 2021 within six electronic databases: PubMed, EBSCOHost Medline, PsycARTICLES, the Cochrane Library, JSTOR and Cobiss (the Slovenian national library information system). Different combinations of Boolean operators were used: mindfulness, empathy, medicine, family medicine, general practice, primary care, burnout, healthcare professionals, doctors, physicians, intervention, MBSR and support groups. Additional articles were hand-searched from the lists of references in the articles we included.
A detailed search strategy is presented in Figure 1.
Figure 1.
Presentation of detailed search strategy.
Inclusion and Exclusion Criteria
This study included research papers (i) published in the last ten years, (ii) written in English, which had (iii) a quantitative or mixed-method design, and (iv) presented original research where PIM was implemented for burnout reduction in group of healthcare professionals.
Studies were excluded where the psychological interventions (PIM) (i) were used for educational or patients’ treatment purposes, and (ii) focused solely on one professional group.
Data Extraction
Data extraction was conducted independently by two reviewers (S.O.T., P.S.-Z.). In the case of disagreement, a third reviewer was included (Z.K.K.).
For the selected studies, the following information was extracted: author and year of the study’s research; sample size; topic and study type; experimental design; specialty of participants; intervention characteristics; study methods; instruments and measures; and main findings.
Quality Assessment
The MERSQI (Medical Education Research Study Quality Instrument) was used for the quality assessment of the included studies; its criteria are data type, data analysis, study design, sampling, and validity of assessments.21 A study can be appointed a total of 18 points, with a maximum of three points in each domain. The initial MERSQI assessment was made by S.O.T., and the evaluation and verification were completed by Z.K.K. and P.S.-Z.
Results
Search Results and Study Characteristics
Of 1315 identified articles, 15 studies met all the inclusion criteria and were analyzed. All the reviewed studies were interventional and used a quantitative or mixed methodological design. In the Supplementary Material, there is a detailed description of the characteristics of the included studies. Table 1 summarizes the main characteristics of the reviewed studies.
Table 1.
Main Characteristics of the Reviewed Studies
| Author/Year/Ref No./Location | Study Design | Sample Size | Intervention (See Table 2 for Details) | Main Findings | QA |
|---|---|---|---|---|---|
| 1. Kemper (2017);22 USA | Prospective non-randomized pre-post intervention study | 178 | Three 1h online mindfulness modules | Small but significant increase in mindfulness scores | 11 |
| 2. Dobkin (2016);23 France | Prospective non-randomized pre-post intervention study | 27 | 8-week MBSR | Significant reductions in stress and burnout; increase in mindfulness and meaningfulness | 11 |
| 3. Kemper et al (2015);24 USA | Prospective non-randomized pre-post intervention study | 513 | 12 1h online modules; mind-body skills training programme | Acute improvements in stress levels, mindfulness, empathy and resilience | 11 |
| 4. Goodman et al (2012);25 USA | Prospective non-randomized pre-post intervention study | 93 | 8-week MBSR + 1-day retreat | Significant reduction in burnout scores and improvements in mental well-being | 10 |
| 5. Asuero et al (2014);26 Spain | Randomized controlled trial | 68 | 8-week mindfulness training and group discussions + 1-day retreat | Improvement in all measured scales – total mood disturbance, mindfulness, burnout and empathy | 12.5 |
| 6. Sallon et al (2015);27 Israel | Prospective non-randomized pre-post controlled intervention study | 215 | Caring for caregivers – 8 months of weekly workshops | Significant improvements in quality of work, decrease in symptoms of perceived stress and emotional exhaustion associated with burnout | 10.5 |
| 7. Moody et al (2013);28 USA, Israel | Randomized controlled pilot study | 48 | 8-week mindfulness training | No significant improvement in scores of burnout, perceived stress or depression | 12.5 |
| 8. Abeni et al (2014);29 Italy | Prospective non-randomized pre-post intervention study | 34 | Modified “Balint Group” method according to a mindfulness technique | Development of more adaptive ways of using defence mechanisms | 10 |
| 9. Lamothe et al (2018);30 Canada | Prospective non-randomized pre-post intervention study | 37 | 8-week MBSR | Significant improvements in perspective taking, identification of one’s own emotions, and emotional acceptance | 11.5 |
| 10. Gracia Gozalo et al (2019);31 Spain | Prospective non-randomized pre-post intervention study | 32 | 8-week mindfulness training | A decrease in emotional exhaustion and an increase in self-compassion | 11 |
| 11. Suyi et al (2017);32 Singapore | Prospective non-randomized pre-post intervention study | 37 | Modified MBSR | Significant improvements in four of the five mindfulness facets and compassion levels; gains maintained at 3 months follow-up | 11 |
| 12. Steinberg et al (2017);33 USA | Randomized controlled pilot study | 32 | 8-week mindfulness training | Significant increase in work satisfaction which negatively correlated with burnout | 12.5 |
| 13. Kemper et al (2015);34 USA | Prospective non-randomized pre-post intervention study | 103 | Online MBS training – 12 1h modules | Significant improvements in stress, mindfulness, and confidence in providing calm, compassionate care | 11.5 |
| 14. Barattucci et al (2019);35 Italy | Prospective non-randomized pre-post intervention study | 602 | IARA training programme | Improvement in emotional regulation, anxiety and stress 6 months after intervention | 11.5 |
| 15. Janssen et al (2020);36 Netherlands | Prospective non-randomized pre-post intervention study | 30 | MBSR | Significant improvements in mindfulness, burnout dimension PA, quality of sleep, positive emotions and self-efficacy | 10.5 |
Abbreviations: QA, quality assessment; USA, United States of America; MBSR, Mindfulness Based Stress Reduction; MBS, Mind Body Skills; IARA, an Italian acronym translatable into meeting, compliance, responsibility, autonomy.
Participants
In the reviewed studies, the participants were a heterogeneous group of HCP from various clinical environments, such as primary care, mental health professionals, and various hospital staff (paediatric oncology staff members, nurses and physicians from the departments of haematology and oncology, intensive care and surgical intensive care unit personnel, staff from a hospital specializing in musculoskeletal problems). The HCP included physicians, residents/trainees, nurses and nursing assistants, psychologists, dietitians, social workers, mental health professionals, and health researchers.
Interventions
All the interventions included elements of mindfulness, despite their great variety in duration, content, schedule, and mode of administration. The most often used intervention was MBSR (four studies), followed by mindfulness training (three studies). Of the 15 studies, four were conducted online. The duration was from a 1-hour module to 30 weekly sessions. A more detailed description of the included interventions is outlined in Table 2.
Table 2.
Detailed Information About the Interventions
| Author (Year); Ref No. | Intervention/Duration | Description |
|---|---|---|
| 1. Kemper (2017);22 | Three 1h online mindfulness modules |
|
| 2. Dobkin (2016);23 | 8-week MBSR + 1-day retreat 2.5h per class on a weekly basis for 8 consecutive weeks |
MBSR is a systematic approach to group mindfulness training. Classes opened with meditation practice, and included mindful movement, sitting and body scan meditations; specific exercises were extended as homework. Two classes focused on stress management and three included exercises to enhance communication skills. Group discussions were encouraged. |
| 3. Kemper et al (2015);24 | Mind-body skills (MBS) training 12 1h online modules |
3 modules for each of 4 types of mind-body skills: (1) Focused attention meditation (relaxation response); (2) Mindfulness; (3) Guided imagery and hypnosis (including autogenic training); and (4) Positive affect-generating meditation (such as gratitude and loving-kindness). The participants were allowed to complete the modules in any number, any order, and in any combination. |
| 4. Goodman et al (2012);25 | 8-week MBSR + 1-day retreat | 4 types of formal mindfulness practices were taught (body scan, mindful movement, walking meditation, sitting meditation). Each class had a topic: (1) Overview of mindfulness; (2) Applying mindfulness in everyday life; (3) Mindful movement; (4) Applying mindfulness to challenging situations; (5) Mindful communication; (6) Practising appreciation; (7) Compassion meditation; (8) Review. |
| 5. Asuero et al (2015);26 | 8-week mindfulness training + 1-day retreat | Each weekly session included four types of activities: (1) Educational presentation of different topics; (2) Formal mindfulness meditation; (3) Narrative and appreciative inquiry exercises; (4) Discussion. |
| 6. Sallon et al (2015);27 | Caring for caregivers (CCG) 8 months of workshops (30 weekly sessions – 2.25 hours/week + a final full-day workshop) | Five components of CCG intervention: (1) Cognitive (mindfulness training); (2) Somatic (body awareness-relaxation; mindful movement and postural alignment); (3) Emotive-expressive (drawing/journalling/listening circle); (4) Dynamic-interactive (movement/interactive dance); and (5) Hands-on (acupressure/shiatsu). |
| 7. Moody et al (2013);28 | 8-week mindfulness-based course (initial 6h session;6 weekly 1h follow-up sessions; final 3h wrap-up session) | Primary focus on the experiential practices (body scan, sitting meditation, mindful movement, STOP technique (Stop, Take a breath, Observe, Proceed), “loving-kindness” meditation) and discussion about them, and 20% didactic information (cultivating awareness of body sensations, thoughts, and emotions during pleasant and unpleasant events; identifying perceptual biases and filters; exploring individual reactivity to stress; reflecting on meaningful experiences and practice; training in skilful listening and communication, exploring self-care). |
| 8. Abeni et al (2014);29 | “Balint group” modified according to a mindfulness technique 30 1h sessions |
This method promotes a group process of exploration and training based on reflection on the relational experience with patients, focusing on the development of attentive awareness of sensations, thoughts, and perceptions of reality at the time of the session. |
| 9. Lamothe et al (2018);30 | 8-week MBSR | MBSR as already described. Participants received a workbook and audio recordings of guided meditations to help them with home practice. |
| 10. Gracia Gozalo et al (2019);31 | 8-week mindfulness training Short practices (5–8 min) in the course of 8 weeks |
On Monday of each week, the participants received a text file via WhatsApp explaining the exercise, and an audio file that could be used for guided meditation. Each day the participants received a practice reminder message in the form of a motivating phrase, image or video. Session objectives: (1) introduction to mindfulness; (2) knowing attention and internal anchoring in breathing; (3) attention to the body; (4) attention to thoughts; (5) informal practice; (6) knowing techniques in movement; (7) knowing the potential in emotional regulation; (8) introduction to compassion. |
| 11. Suyi et al (2017);32 | Modified MBSR 6 weekly 2h sessions |
Topics: (1) introduction to practice; (2) perception and engaging with practice; (3) awareness of being stuck in one’s life and how to get unstuck; (4) reacting and responding to stress, exploring perceptions and thoughts; (5) mindful communication in stressful situations; (6) cultivating kindness towards oneself and others. During the training, meditation practices were taught. Participants were asked to practise 30 min of formal meditation daily. |
| 12. Steinberg et al (2017);33 | 8-week mindfulness-based intervention (weekly 1h group session at the workplace during work hours) | Participants were asked to do 20-minute daily individual practices. |
| 13. Kemper et al (2015);34 | Online MBS (mind-body skills) training 12 1h modules |
4 general topics: (1) focused attention meditation (relaxation response); (2) mindfulness meditation; (3) positive affect meditation (positive or sacred word, gratitude, and loving-kindness/compassion meditation); (4) guided imagery/hypnosis (autogenic training; guided imagery to prepare for surgery, procedures, or childbirth; and guided imagery for sleep and changing habits). |
| 14. Barattucci et al (2019);35 | IARA training programme 4 meetings for 8 hours Group training (18–22 participants per group) |
1st meeting: IARA principles, creation of a working group, developing awareness of here and now 2nd meeting: techniques of counselling, improving emotional awareness and patient-centred care 3rd meeting: SWOT analysis, creative imagination, IARA techniques 4th meeting: seven psychological types, planning changes, improving awareness of people’s qualities |
| 15. Janssen et al (2020);36 | 8-week MBSR + 1 day silence during working hours |
|
Measuring Instruments
A wide variety of psychometric instruments were used. Among the most common were the Maslach Burnout Inventory (MBI) (in nine studies); the Perceived Stress Scale (PSS) and the Five Facet Mindfulness Questionnaire (FFMQ) (in six studies); and the Cognitive and Affective Mindfulness Scale-Revised (CAMS-R) and the Mindful Attention Awareness Scale (MAAS) (in three studies). Mindfulness was examined by three different measures, the FFMQ, the CAMS-R and the MAAS; in one study all three were used.22
Nearly all the studies examining mindfulness with the FFMQ reported a significant increase in mindfulness scores post intervention.22,23,26,32,36 In the case of the PSS the results were also quite homogeneous; in five studies a reduction in perceived stress was reported, although one28 reported no significant improvement in the perceived stress scores. In the studies reporting burnout with the MBI, in general an improvement was confirmed. In two studies post-interventional scores were not reported,24,33 and in one study it was done only graphically.31 Janssen et al36 reported a significant improvement in PA, but did not find any significant changes in work engagement and mental distance (burnout dimensions in the Dutch version of the MBI). The study by Moody et al,28 carried out with a multidisciplinary group of paediatric oncology staff members, showed no significant improvement in burnout or perceived stress scores. One possible explanation for such results may be that nearly all the participants showed signs of burnout at baseline. However, the qualitative analysis in the same study revealed reduced stress, an improved sense of inner peace, joy and compassion, better focus, and less somatic symptoms in the intervention group.28
Sustained Effect Measurement
Two studies examined whether there was a sustained effect after the intervention. Suyi at al.32 showed that participants maintained improvements on self-compassion and mindfulness at the three month follow-up. There was no change observed for burnout. Barattucci et al35 found that the HCPs who attended mindfulness-based IARA training had better scores for anxiety, stress, and emotional regulation six months after the intervention, compared to the control group.
Comparison of Online vs In-Person Interventions
In the fifteen included studies, there were four online and eleven in-person interventions. Despite the great variety in the duration and characteristics of the online interventions, generally an improvement was reported. Kemper et al22 reported a significant improvement in mindfulness scores. In another study using elective 1-hour modules of mind-body skills training,24 Kemper et al confirmed improvements in empathy, mindfulness, resilience, and stress. The main advantage was that online MBS training reached diverse health professionals. Gracia Gozalo et al31 reported improvements in self-compassion and emotional exhaustion after an 8-week mindfulness programme based on individual training.
Assessing Study Quality – MERSQI Scores
The mean MERSQI score of the included studies was 11.2, and the minimum appointed score was 10 and the maximum 12.5. The lower MERSQI results were found to be mostly due to the following: study design as there were many single group pre-post studies; small sample sizes; only one involved institution; use of self-assessment tools by participants; and not reporting the validity of the evaluation instrument. Moreover, the data analysis of the included studies did not exceed the descriptive analysis.
Discussion
Main Findings
The results of this systematic review demonstrated a positive impact on the selected psychological measures, regardless of the specific type of PIM used. The most commonly studied interventions involved MBSR and other mindfulness training programmes, the latter in online as well as in-person versions. These findings are in line with a previously published review by the same authors,19 carried out on a professional group of physicians only.
Comparison to Other Studies
The results of this systematic review are concordant with the findings of other recently published review papers,37,38 showing that mindfulness-based interventions present an effective tool which could improve the psychological functioning of HCP. This knowledge is essential today as, during the Covid-19 pandemic, HCP working in the frontline were likely to experience an increased volume and intensity of work, as well as facing added pressure due to new working environments, constantly changing protocols, and exposure to trauma and contagion.39–41 On top of organizational and personal challenges, the fear of Covid-19 contagion seems to be an additional burden which is associated with negative effects on mental health of HCP.39
This review is unique in several aspects when compared to other review papers.42,43 It involves a wide and heterogeneous group of HCP, whereas others are focused mostly on one specific group (eg nurses, primary physicians, psychologists, etc.). It seems that the same mindfulness-based interventions can be used regardless of the profession of the healthcare team members. In primary care, integrated care is more and more important,44 and it can involve many healthcare professionals. This review suggests that a common approach to strengthening the resilience and mental health of all team members is feasible and effective.
The review’s most important characteristic is the inclusion of various interventions in online and in-person formats, from which we can gain a better understanding of the efficiency, feasibility, and cost-effectiveness of the two formats. As already stated, four studies used an online approach22,24,31,34 from which we can conclude that online training is feasible, less time-consuming, and associated with significant improvements in perceived stress and mindfulness. This finding is in line with a recently published (2022) randomized controlled trial carried out with undergraduate nursing students during the Covid pandemic in China.45 A 6-week online mindfulness intervention was confirmed to be effective in improving mental health and reducing the symptoms of anxiety and stress.45 In-person interventions were all designed for group training, whereas online interventions were carried out individually.
Theoretical Implications
Based on these findings, we can summarize that there were no major differences between group and individual training, and it seems that the online format is as effective as an in-person format, which is also in line with other studies.46
One crucial piece of information for future planning is also the presence of a sustained effect, which is included in this review. It seems that mindfulness-based interventions have the potential to provide a long-term positive effect.32,35
This review also showed that even training with a short duration can lead to significant benefits for HCP, which has also been confirmed by other researchers.47,48
Least but not last, it seems very important to consider several variables associated with reactivity to stress and predisposing HCP to burnout. Important predictors of burnout syndrome are exhaustion, depression, anxiety, decreased professional satisfaction, stigmatization, young age and female gender. Young age can be connected to several explanations, such as longer working hours, higher empathy, and lack of experience. Emotional intelligence also plays an important role in mitigating reactivity to stress. There are contradictory data on the connection between relationship status and sensitivity to burnout.49,50
Since specialties in the front line are at the highest risk of developing burnout,51 it is worth mentioning that the majority of the included studies were conducted in a hospital environment, some of them in a very specific population, eg paediatric oncology staff members,28 staff in an intensive care unit,31 or mental health professionals.32 It is therefore especially important for future studies to also address HCP in primary care. All our findings are intriguing in terms of effective burnout prevention, so future studies should focus on answering questions about long-term impact and cost-effectiveness when comparing in-person and online interventions. It is also recommended that effective interventions are identified and offered in the first place to the most vulnerable groups of HCP.
Practical Implications
HCP, especially at the primary care level, are overburdened with work and find it difficult to attend in-person activities.18 Based on the results of our study, they can be encouraged to attend online activities without the fear of them not being effective.
Healthcare workers need to understand the importance of maintaining and preserving their own mental health and resilience. Achieving mindfulness in their daily lives and work should become part of their daily routine. Our study showed that there is a need to include education on this topic in the curricula of undergraduate and postgraduate healthcare studies.
The findings of this study could be used not only by managers of healthcare organizations but also by HCP themselves to improve their resilience; they can still benefit significantly even by attending short training courses.
Strengths and Limitations
This review has several strengths. It follows PRISMA reporting guidelines with a clear demonstration of a search strategy, and a high number of included studies. In contrast to other reviews, which focused on a specific professional group, this review includes a heterogeneous group of HCP which could upgrade our knowledge of burnout in this setting, as well as the role of mindfulness-based interventions in addressing the problem. The studies were conducted in eight different countries, which is positive from the aspect of generalization. Apart from the United States, Canada, and European countries, one was carried out in Israel, and another in Singapore. The review is unique because of its comparison of in-person and online interventions, and the special focus on follow-up and the measurement of a sustained effect after the completion of the intervention.
As rather weak experimental designs were used in most of the studies, with different durations of intervention applied and various instruments administered for the assessment of psychological qualities, it was a challenge to compare the results and generalize the main findings. Some studies used small samples and some reports presented a substantial risk of bias. Some studies did not have a control group, and the participants were mostly self-selected based on their interest, and did not evaluate the baseline levels of sensitivity to burnout of the participating HCP.
Based on these limitations, there is a strong suggestion for future research to thoroughly describe the implemented interventions and to use methodologically rigorous and uniform designs, eg the same psychometric measure for each quality and the same duration of intervention.
Conclusion
This review provided solid evidence that by offering HCP effective, feasible interventions focused on their needs we could efficiently improve several key aspects of burnout, empathy, and mindfulness, and also indirectly influence patient care. The interventions offered can be shaped in such a way that would not significantly affect the already busy schedule of HCP, as short and on-line interventions have been shown to be as effective as long, in-person ones. Nevertheless, the inclusion of mindfulness education in undergraduate and postgraduate curricula could be very important; it could enable a long-term positive effect on the health of HCP.
There are several important questions yet to be addressed by future research: What are the long-term impacts and cost-effectiveness of different formats (in-person vs online), durations and types of specific PIM for HCP? How long does the sustained effect last and what is the optimum frequency of refresher courses to sustain or augment their effects? How can training programmes support ongoing practice? How much impact can be attributed to the group support offered by in-person training? How do initial stress and burnout levels affect cooperation and the likelihood of ongoing practice? It is also recommended that effective interventions are identified and offered in the first place to the most vulnerable groups of HCP.
We believe that the new findings presented in this review would be accepted as a positive challenge for healthcare system management and HCP themselves during the Covid-19 pandemic and beyond, as well as being an inspiration for researchers to initiate further investigation in this field.
Acknowledgments
The authors P.S.-Z. and Z.K.K. acknowledge financial support from the Slovenian Research Agency, a research core funding Research in The Field of Public Health No. P3―0339.
Disclosure
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.European Agency for Safety and Health at Work. European opinion poll on occupational safety and health; 2013. Available from: https://osha.europa.eu/en/facts-and-figures/european-opinion-polls-safety-and-health-work/european-opinion-poll-occupational-safety-and-health-2013. Accessed November 15, 2021.
- 2.Rodriguez-Vega B, Palao Á, Muñoz-Sanjose A, et al. Implementation of a mindfulness-based crisis intervention for frontline healthcare workers during the COVID-19 outbreak in a public general hospital in Madrid, Spain. Front Psychiatry. 2020;11:562578. doi: 10.3389/fpsyt.2020.562578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ollis L, Shanahan P. Stress, psychological distress and support in a health care organization during Covid-19: a cross-sectional study. J Nurs Manag. 2022;30(2):359–366. doi: 10.1111/jonm.13526 [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, Sloan JA, Habermann TM. The well-being of physicians. Am J Med. 2003;114(6):513–519. doi: 10.1016/s0002-9343(03)00117-7 [DOI] [PubMed] [Google Scholar]
- 5.Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse burnout and patient satisfaction. Med Care. 2004;42(2 Suppl):II57–II66. doi: 10.1097/01.mlr.0000109126.50398.5a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rupert PA, Morgan DJ. Work setting and burnout among professional psychologists. Prof Psychol Res Pr. 2005;36:544–550. doi: 10.1037/0735-7028.36.5.544 [DOI] [Google Scholar]
- 7.Bosak J, Kilroy S, Chênevert D, Flood P. Examining the role of transformational leadership and mission valence on burnout among hospital staff. J Organ Eff. 2021;8(2):208–227. doi: 10.1108/JOEPP-08-2020-0151 [DOI] [Google Scholar]
- 8.Gómez-Salgado J, Domínguez-Salas S, Romero-Martín M, Romero A, Coronado-Vázquez V, Ruiz-Frutos C. Work engagement and psychological distress of health professionals during the COVID-19 pandemic. J Nurs Manag. 2021;29(5):1016–1025. doi: 10.1111/jonm.13239 [DOI] [PubMed] [Google Scholar]
- 9.Chou LP, Li CY, Hu SC. Job stress and burnout in hospital employees: comparisons of different medical professions in a regional hospital in Taiwan. BMJ Open. 2014;4(2):e004185. doi: 10.1136/bmjopen-2013-004185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Verweij H, Van der Heijden FMMA, Van Hoo MLM, et al. The contribution of work characteristics, home characteristics and gender to burnout in medical residents. Adv Health Sci Educ Theory Pract. 2017;22:803–818. doi: 10.1007/s10459-016-9710-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Poghosyan L, Clarke SP, Finlayson M, Aiken LH. Nurse burnout and quality of care: cross-national investigation in six countries. Res Nurs Health. 2010;33(4):288–298. doi: 10.1002/nur.20383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shanafelt T, Dyrbye L. Oncologist burnout: causes, consequences, and responses. J Clin Oncol. 2012;30(11):1235–1241. doi: 10.1200/JCO.2011.39.7380 [DOI] [PubMed] [Google Scholar]
- 13.Bria M, Baban A, Dumitrascu DL. Systematic review of burnout risk factors among European healthcare professionals. Cogn Brain Behav. 2012;16(3):423–452. [Google Scholar]
- 14.Schuman-Olivier Z, Trombka M, Lovas DA, et al. Mindfulness and behavior change. Harv Rev Psychiatry. 2020;28(6):371–394. doi: 10.1097/HRP.0000000000000277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. J Psychosom Res. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7 [DOI] [PubMed] [Google Scholar]
- 16.Ludwig DS, Kabat-Zinn J. Mindfulness in medicine. JAMA. 2008;300(11):1350–1352. doi: 10.1001/jama.300.11.1350 [DOI] [PubMed] [Google Scholar]
- 17.Irving JA, Dobkin PL, Park J. Cultivating mindfulness in health care professionals: a review of empirical studies of mindfulness-based stress reduction (MBSR). Complement Ther Clin Pract. 2009;15(2):61–66. doi: 10.1016/j.ctcp.2009.01.002 [DOI] [PubMed] [Google Scholar]
- 18.Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302(12):1284–1293. doi: 10.1001/jama.2009.1384 [DOI] [PubMed] [Google Scholar]
- 19.Onuk Tement S, Klemenc-Ketiš Z, Miroševič Š, Selič-Zupančič P. The impact of Psychological Interventions with Elements of Mindfulness (PIM) on empathy, well-being, and reduction of burnout in physicians: a systematic review. Int J Environ Res Public Health. 2021;18(21):11181. doi: 10.3390/ijerph182111181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.2236/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reed DA, Cook DA, Beckman TJ, Levine RB, Kern DE, Wright SM. Association between funding and quality of published medical education research. JAMA. 2007;298(9):1002–1009. doi: 10.1001/jama.298.9.1002 [DOI] [PubMed] [Google Scholar]
- 22.Kemper KJ. Brief online mindfulness training: immediate impact. J Evid Based Complementary Altern Med. 2017;22(1):75–80. doi: 10.1177/2156587216639199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dobkin PL, Bernardi NF, Bagnis CI. Enhancing clinicians’ well-being and patient-centered care through mindfulness. J Contin Educ Health Prof. 2016;36(1):11–16. doi: 10.1097/CEH.0000000000000021 [DOI] [PubMed] [Google Scholar]
- 24.Kemper KJ, Khirallah M. Acute effects of online mind-body skills training on resilience, mindfulness, and empathy. J Evid Based Complementary Altern Med. 2015;20(4):247–253. doi: 10.1177/2156587215575816 [DOI] [PubMed] [Google Scholar]
- 25.Goodman MJ, Schorling JB. A mindfulness course decreases burnout and improves well-being among healthcare providers. Int J Psychiatry Med. 2012;43(2):119–128. doi: 10.2190/PM.43.2.b [DOI] [PubMed] [Google Scholar]
- 26.Asuero AM, Queraltó JM, Pujol-Ribera E, Berenguera A, Rodriguez-Blanco T, Epstein RM. Effectiveness of a mindfulness education program in primary health care professionals: a pragmatic controlled trial. J Contin Educ Health Prof. 2014;34(1):4–12. doi: 10.1002/chp.21211 [DOI] [PubMed] [Google Scholar]
- 27.Sallon S, Katz-Eisner D, Yaffe H, Bdolah-Abram T. Caring for the caregivers: results of an extended, five-component stress-reduction intervention for hospital staff. Behav Med. 2017;43(1):47–60. doi: 10.1080/08964289.2015.1053426 [DOI] [PubMed] [Google Scholar]
- 28.Moody K, Kramer D, Santizo RO, et al. Helping the helpers: mindfulness training for burnout in pediatric oncology – a pilot program. J Pediatr Oncol Nurs. 2013;30(5):275–284. doi: 10.1177/1043454213504497 [DOI] [PubMed] [Google Scholar]
- 29.Abeni MS, Magni M, Conte ML, et al. Psychological care of caregivers, nurses and physicians: a study of a new approach. Cancer Med. 2014;3(1):101–110. doi: 10.1002/cam4.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lamothe M, McDuff P, Pastore YD, Duval M, Sultan S. Developing professional caregivers’ empathy and emotional competencies through mindfulness-based stress reduction (MBSR): results of two proof-of-concept studies. BMJ Open. 2018;8(1):e018421. doi: 10.1136/bmjopen-2017-018421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gracia Gozalo RM, Ferrer Tarrés JM, Ayora Ayora A, Alonso Herrero M, Amutio Kareaga A, Ferrer Roca R. Application of a mindfulness program among healthcare professionals in an intensive care unit: effect on burnout, empathy and self-compassion. Med Intensiva. 2019;43(4):207–216. doi: 10.1016/j.medin.2018.02.005 [DOI] [PubMed] [Google Scholar]
- 32.Suyi Y, Meredith P, Khan A. Effectiveness of mindfulness intervention in reducing stress and burnout for mental health professionals in Singapore. Explore. 2017;13(5):319–326. doi: 10.1016/j.explore.2017.06.001 [DOI] [PubMed] [Google Scholar]
- 33.Steinberg BA, Klatt M, Duchemin AM. Feasibility of a mindfulness-based intervention for surgical intensive care unit personnel. Am J Crit Care. 2016;26(1):10–18. doi: 10.4037/ajcc2017444 [DOI] [PubMed] [Google Scholar]
- 34.Kemper KJ, Lynn J, Mahan JD. What is the impact of online training in mind-body skills? J Evid Based Complementary Altern Med. 2015;20(4):275–282. doi: 10.1177/2156587215580882 [DOI] [PubMed] [Google Scholar]
- 35.Barattucci M, Padovan AM, Vitale E, Rapisarda V, Ramaci T, De Giorgio A. Mindfulness-based IARA model® proves effective to reduce stress and anxiety in health care professionals. A six-month follow-up study. Int J Environ Res Public Health. 2019;16(22):4421. doi: 10.3390/ijerph16224421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Janssen M, Van der Heijden B, Engels J, Korzilius H, Peters P, Heerkens Y. Effects of mindfulness-based stress reduction training on healthcare professionals’ mental health: results from a pilot study testing its predictive validity in a specialized hospital setting. Int J Environ Res Public Health. 2020;17(24):9420. doi: 10.3390/ijerph17249420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kriakous SA, Elliott KA, Lamers C, Owen R. The effectiveness of mindfulness-based stress reduction on the psychological functioning of healthcare professionals: a systematic review. Mindfulness. 2021;12(1):1–28. doi: 10.1007/s12671-020-01500-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Conversano C, Ciacchini R, Orrù G, Di Giuseppe M, Gemignani A, Mindfulness PA. Compassion, and self-compassion among health care professionals: what’s new? A systematic review. Front Psychol. 2020;11:1683. doi: 10.3389/fpsyg.2020.01683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Celmeçe N, Menekay M. The effect of stress, anxiety and burnout levels of healthcare professionals caring for Covid-19 patients on their quality of life. Front Psychol. 2020;11:597624. doi: 10.3389/fpsyg.2020.597624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Serrão C, Duarte I, Castro L, Teixeira A. Burnout and depression in Portuguese healthcare workers during the Covid-19 pandemic: the mediating role of psychological resilience. Int J Environ Res Public Health. 2021;18(2):636. doi: 10.3390/ijerph18020636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nutting R, Ofei-Dodoo S, Rose-Borcherding K, Strella G. Brief mindfulness intervention for emotional distress, resilience, and compassion in family physicians during Covid-19: a pilot study. PRiMER. 2022;6:3. doi: 10.22454/PRiMER.2022.746202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Clough BA, March S, Chan RJ, Casey LM, Phillips R, Ireland MJ. Psychosocial interventions for managing occupational stress and burnout among medical doctors: a systematic review. Syst Rev. 2017;6(1):1–19. doi: 10.1186/s13643-017-0526-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wexler TM, Schellinger J. Mindfulness-based stress reduction for nurses: an integrative review. J Holist Nurs. 2022;25:8980101221079472. doi: 10.1177/08980101221079472 [DOI] [PubMed] [Google Scholar]
- 44.Poplas Susič A, Klemenc-Ketiš Z. Successful implementation of integrated care in Slovenian primary care. Zdr Varst. 2021;60(1):1–3. doi: 10.2478/sjph-2021-0001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dai Z, Jing S, Wang H, et al. Mindfulness-based online intervention on mental health among undergraduate nursing students during coronavirus disease 2019 pandemic in Beijing, China: a randomized controlled trial. Front Psychiatry. 2022;13:949477. doi: 10.3389/fpsyt.2022.949477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vaona A, Banzi R, Kwag KH, et al. E-learning for health professionals. Cochrane Database Syst Rev. 2018;1(1):CD011736. doi: 10.1002/14651858.CD011736.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fortney L, Luchterhand C, Zakletskaia L, Zgierska A, Rakel D. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: a pilot study. Ann Fam Med. 2013;11(5):412–420. doi: 10.1370/afm.1511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sood A, Sharma V, Schroeder DR, Gorman B. Stress Management and Resiliency Training (SMART) program among department of radiology faculty: a pilot randomized clinical trial. Explore. 2014;10(6):358–363. doi: 10.1016/j.explore.2014.08.002 [DOI] [PubMed] [Google Scholar]
- 49.Taranu SM, Ilie AC, Turcu AM, et al. Factors associated with burnout in healthcare professionals. Int J Environ Res Public Health. 2022;19(22):14701. doi: 10.3390/ijerph192214701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pérez-Fuentes MC, Molero-Jurado MM, Gázquez-Linares JJ, Simón-Márquez MM. Analysis of burnout predictors in nursing: risk and protective psychological factors. Eur J Psychol. 2019;11:33–40. doi: 10.5093/ejpalc2018a13 [DOI] [Google Scholar]
- 51.Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377–1385. doi: 10.1001/archinternmed.2012.3199 [DOI] [PubMed] [Google Scholar]