Abstract
Objectives:
To develop symptom networks and examine the longitudinal relationships of depressive symptoms among middle-aged and older adults in China.
Method:
This study used three-wave data from the China Health and Retirement Longitudinal Study (2013 (T1), 2015 (T2), and 2018 (T3)). Depressive symptoms were measured by the 10-item Center for Epidemiologic Studies Depression Scale (CES-D). A multilevel vector autoregression model (VAR) was used to identify ten depressive symptoms dynamically interacting with each other over time.
Results:
A total of 3,558 participants were included in the final analysis. The strongest direct effects were “D10: felt fearful” -> “D6: felt everything I did was an effort” (β=0.14). “D10: felt fearful” reported the largest value of out-predictability (r=0.064) and out-strength (r=0.635). “D3: felt depressed” reported the largest value of in-predictability (r=0.077) and in-strength (r=0.545). Substantial heterogeneity in the network may stem from an individual’s sex and place of residence.
Conclusions:
“Felt fearful” was the strongest predictor compared to the other nine depressive symptoms based on node centrality. Our study suggests that, after understanding the causes of fear, strategies to reduce fear should be incorporated into multimodal interventions for middle-aged and older adults with depressive symptoms.
Keywords: depression, symptom network, psychopathology, psychosomatic disorders
Introduction
As one of the leading causes of the global burden of diseases, depressive symptoms are defined as a feeling of sadness, melancholy, and helplessness, accompanied by mood changes and somatic symptoms (Alexopoulos, 2005). In middle-aged and older adults, the manifestation of depressive symptoms is complex. The most prevalent depressive symptoms in middle-aged and older adults are “having little interest or pleasure in doing things”, “feeling down”, “feeling tired”, and “restless sleep” (Kroenke et al., 2001). Among the depressive symptoms, negative emotions (e.g. feeling sad and depressed), lack of positive affects (e.g. feeling hopeful and happy), and somatic symptoms (e.g. restless sleep and poor appetite) are the most common clusters of depressive symptoms (Anderson, 2001). Previous studies have identified complex relationships among negative emotions cluster, positive affects cluster, and somatic symptoms cluster (Okur Güney et al., 2019; Groen et al., 2021). If middle-aged and older adults with depressive symptoms are not treated promptly, the complexity of symptoms may put them at higher risk for various physical and psychological conditions (Birk et al., 2019).
In China, depressive symptoms are common among middle-aged and older adults and are recognized as one of the major barriers to healthy aging. Previous studies have shown that there are significant gender and regional differences in the prevalence and severity of depressive symptoms (Liu et al., 2020; Luo et al., 2018). Furthermore, the major causes of depression are context-and culture-specific. The complex interactions between depressive symptoms vary across populations and cultural contexts. In China, deterioration of physical and cognitive health, financial burden, rapid changes in social and cultural values, and family support and conflict are major causes of depressive symptoms in middle-aged and older adults (Wang et al., 2019; Zou et al., 2018). These factors may lead to different longitudinal relationships in the psychopathology of depressive symptoms in the Chinese context compared to other contexts. It is crucial to identify the mechanisms of how each depressive symptom interacts with each other within this population and its subgroups. A better understanding of the interactions of depressive symptoms is essential for the development of tailored and context-specific interventions.
Most previous research studied depression as a holistic conception and ignored the complex relationships within various constructs of depressive symptoms. Analysis of depression as a summary scale provides limited insight into the interplay of depressive symptoms. Moreover, the prevalence of comorbid multiple depressive symptoms is high, reaching 20.0% (95% CI, 17.5%–22.8%) in middle-aged and older adults, according to previous studies based on different diagnostic criteria (Tang et al., 2021). Previous studies have identified that having co-occurring symptoms may increase network connectivity, which is the prime property for detecting prognostic changes (Lydon-Staley et al., 2019; Vittengl et al., 2022). Therefore, intervening in core symptoms may be more effective than psychotherapeutic interventions that target overall symptoms. Core and bridge symptoms represent promising therapeutic targets as they may accelerate the deactivation of symptom interactions (Kaiser et al., 2021). Evidence on which depressive symptoms are the core symptom in middle-aged and older adults in the psychopathology of depressive symptoms is a prerequisite to the development of effective and precise psychotherapeutic interventions. There is a need to have a better understanding of the complex relationships among symptoms.
In this study, we used symptom networks to answer how depressive symptoms interacted with each other and what were the core depressive symptoms in middle-aged and older adults. The symptom network is defined as a new paradigm for analyzing the complex interconnections and putative causal relationships among multiple symptoms. Although the concept of symptom networks originated in psychopathology network models, over the past three years, the paradigm has been used to capture the complex causal relationships between psychological symptoms and somatic symptoms of various chronic diseases (Rha & Lee, 2020; Schweren et al., 2017; Zhu et al., 2019). Symptom networks explore and visualize internal mechanisms of symptoms in a given population, which can help researchers identify potential causalities of symptoms and explore core symptoms from a mechanistic perspective. Indices of symptom networks, such as centrality and density, have been reported in previous studies to be more sensitive indicators than symptom severity and prevalence (Zhu et al., 2021a; Zhu et al., 2021b). Minor changes in symptom, that is not statistically significant measured by symptom severity, could be detected by these indicators in symptom networks.
However, few studies have adopted a symptom network approach to elucidate the complex relationships across depressive symptoms in middle-aged and older adults and to explore how these relationships differ across sex and place of residence subgroups. It remains unclear which symptoms are the core symptoms in this population. Empirical evidence is needed for developing precise psychotherapeutic interventions for middle-aged and older adults with depression. Therefore, the aims of this study were 1) to identify longitudinal relationships in the psychopathology of depressive symptoms in middle-aged and older adults and 2) to explore the core symptom in the symptom networks.
Methods
Participants
This study used three-wave data from the China Health and Retirement Longitudinal Study (CHARLS) in 2013 (T1), 2015 (T2), and 2018 (T3). The CHARLS is a national survey conducted by Peking University and longitudinally collects social, economic, and health data on China’s aging population at both individual and community levels. CHARLS adopts multi-stage stratified probabilities proportional to size (PPS) sampling which provides a nationally representative sample for our study. Detailed information on the CHARLS study design, recruitment methods, and ethical approval can be found elsewhere (Zhao et al., 2014). We only included data from the most recent three waves (2013, 2015, and 2018) because these data reflect the mental health status of the most current cohort of middle-aged and old adult populations. To examine the longitudinal relationships between depressive symptoms assessed two years apart, we include participants aged 45 years and older at T1 who had completed two waves of follow-up. A total of 3,558 participants were included in the study.
Measures
Depressive symptoms
Depressive symptoms were measured by the 10-item Center for Epidemiologic Studies Depression Scale (CES-D) in CHARLS (Irwin et al., 1999). Participants were asked if they experienced the following symptoms during the past week: “D1: happy”, “D2: felt lonely”, “D3: felt depressed”, “D4: sleep was restless”, “D5: could not get going”, “D6: felt everything I did was an effort”, “D7: felt hopeful about the future”, “D8: bothered by things”, “D9: had trouble keeping my mind”, and “D10: felt fearful”. The responses include rarely or none of the time (0), some of the time (1), occasionally (2), and most of the time (3). The measure showed high levels of internal consistency in our sample (Cronbach’s alpha ranges from 0.674 to 0.810 at three waves of the data).
Socio-demographic characteristics
Socio-demographic characteristics included age (continuous), sex (men=1; women=2), ethnicity (Han Chinese=1; minority=2), educational attainment (illiterate=1; primary school or below=2; middle school=3; high school=4; college or above=5), marital status (married=1; widowed=2; divorce=3; single=4), place of residence (rural area=1; urban area=2; The place of residence is determined by participants’ household registration), self-reported health (total score: 5; higher scores indicate better health conditions), and self-reported number of chronic diseases (total number ranges from 0 to14. These chronic diseases included hypertension, dyslipidemia, diabetes, cancer, chronic lung diseases, liver disease, cardiovascular disease, stroke, kidney disease, stomach or other digestive disease, psychiatric disease, memory-related disease, arthritis or rheumatism, and asthma).
Data analysis
R software 4.0.2 was used to perform statistical analysis. Due to network analysis not allowing missing data, participants with missing CES-D and covariates data in either wave 2013 (T1), 2015 (T2), and 2018 (T3) were categorized as excluded samples. We used frequencies, percentages, means, and standard deviations (SDs) to describe demographic variables and the severity of depressive symptoms. We further used chi-square tests and t-tests to compare the characteristics and symptom frequency between the participants in the study and those who excluded from the study.
Characterization and interconnectedness of depression networks
A multilevel vector autoregression model (VAR) was used to identify ten depressive symptoms dynamically interacting with each other over time in a network architecture. We used a comprehensive random effect modeling strategy that may be better suited to the context of symptom network inference in psychopathology (Bringmann et al., 2013). In the symptom network, a node represents individual psychological symptoms of depression. An edge represents an independent relationship between two nodes. The thickness of the edge represents the effect size between two nodes. We use the Fruchterman-Reingold algorithm to construct a directed dynamic network graph. In this algorithm, the force vector determines the nodes (Traud et al., 2009). The nodes with the strongest correlation are located in the center of the network, and the nodes with similar characteristics are closer. Sociodemographic characteristics significantly associated with the total CES-D score in T3 were controlled in the networks as covariates. Subgroup networks were conducted to examine the predictive relationships between symptoms in sex and place of residence subgroups. Covariates including age, sex, educational attainment, marital status, self-reported health, and self-reported number of chronic diseases that differed significantly at baseline between subgroups were included as covariates in subgroups analysis.
Accuracy and stability of networks
To evaluate the accuracy and stability of the networks, we perform the bootstrapping method using the R package bootnet (Epskamp & Fried, 2015). Accuracy was assessed by calculating 95% confidence intervals (CIs) for the edge weight values. In addition, we used a nonparametric bootstrapping method (1,000 bootstrap samples) to construct the CIs. To determine whether network connectivity and centrality estimates differ by variable, we conducted a guided difference test for marginal weights and centrality indices in LASSO regularization of dynamic networks based on multivariate correlation matrices.
Node centrality and predictability
A centrality analysis was conducted to identify the most central symptoms of the ten depressive symptoms. We used in-strength (the total value of incoming edges connected to a symptom) and out-strength (the total value of outcoming edges connected to a symptom) to identify the most central symptoms from a symptom mechanism perspective. Nodes with higher values of out-strength indicated it is more likely to affect connected nodes than other nodes. Conversely, nodes with higher values of in-strength indicate it is more likely to be affected by connected nodes. We identified the bridge symptoms between two clusters (positive affect cluster and negative symptom cluster) by calculating the bridge strength (the sum of absolute in-strength and out-strength) of ten symptoms (Jones et al., 2021). Moreover, we used the mgm package to identify the predictability of each node (Haslbeck & Waldorp, 2015). Symptoms with high predictability values indicate that we can control the symptom through its neighboring nodes. In contrast, if the predictability value is low, we need to intervene directly in the symptom or look for markers outside the network.
Results
Participant characteristics and symptom prevalence and severity
Table 1 shows the participant characteristics (n=3,558). The mean age of the participants was 59.30 (SD=8.86) years old, ranging from 45 to 91 years. Most participants were women (53.37%), Han Chinese (92.09%), obtained a primary school diploma or less (45.47%), married (88.06%), and lived in rural areas (87.58%). The mean score of self-rated health was 3.57 (SD=0.95). The median number of self-reported chronic diseases was 2.
Table 1.
Socio-demographic characteristics of participants at enrollment (N=3558)
| Characteristics | Full sample (N=3558) |
Sex |
P Value | Place of residence |
P Value | ||
|---|---|---|---|---|---|---|---|
| Men (n1=1659) |
Women (n2=1899) |
Rural (n4=3116) |
Urban (n3=442) |
||||
|
| |||||||
| Age | 59.30±8.86 (45–91) | 59.95±8.87 (45–91) | 58.72±8.81 (45–90) | <0.0001 | 59.01±8.78 (45–91) | 61.30±9.17 (45–85) | <0.0001 |
| Gender | – | 0.007 | |||||
| Men | 1659 (46.63%) | 1659 (100.00%) | 0 (0.00%) | 1426 (45.76%) | 233 (52.71%) | ||
| Women | 1899 (53.37%) | 0 (0.00%) | 1889 (100.00%) | 1690 (54.24%) | 209 (47.29%) | ||
| Ethnicity/race | 0.260 | 0.127 | |||||
| Han | 3245 (91.20%) | 1523 (91.80%) | 1722 (90.68%) | 2833 (90.92%) | 412 (93.21%) | ||
| Minority | 313 (8.80%) | 136 (8.20%) | 177 (9.32%) | 283 (9.08%) | 30 (6.79%) | ||
| Educational attainment | <0.0001 | <0.0001 | |||||
| Illiterate | 990 (27.82%) | 231 (13.92%) | 759 (39.97%) | 951 (30.52%) | 39 (8.82%) | ||
| Primary school or below | 1618 (45.47%) | 864 (52.08%) | 754 (39.71%) | 1474 (47.30%) | 144 (32.58%) | ||
| Middle school | 620 (17.43%) | 362 (21.82%) | 258 (13.59%) | 496 (15.92%) | 124 (28.05%) | ||
| High school | 221 (6.21%) | 132 (7.96%) | 89 (4.69%) | 155 (4.97%) | 66 (14.93%) | ||
| College or above | 109 (3.06%) | 70 (4.22%) | 39 (2.05%) | 40 (1.28%) | 69 (15.61%) | ||
| Marital status | <0.0001 | 0.006 | |||||
| Married | 3133 (88.06%) | 1518 (91.50%) | 1615 (85.04%) | 2750 (88.25%) | 383 (86.65%) | ||
| Widowed | 358 (10.06%) | 93 (5.61%) | 265 (13.95%) | 309 (9.92%) | 49 (11.09%) | ||
| Divorce | 30 (0.84%) | 19 (1.15%) | 11 (0.58%) | 21 (0.67%) | 9 (2.04%) | ||
| Single | 37 (1.04%) | 29 (1.75%) | 8 (.42%) | 36 (1.16%) | 1 (0.23%) | ||
| Place of residence | 0.007 | – | |||||
| Urban | 442 (12.42%) | 233 (14.04%) | 209 (11.01%) | 0 (0.00%) | 3166 (100.00%) | ||
| Rural | 3116 (87.58%) | 1426 (85.86%) | 1690 (88.99%) | 3166 (100.00%) | 0 (0.00%) | ||
| Self-rated health | 3.57±0.95 (1–5) | 3.47±0.95 (1–5) | 3.65±0.94 (1–5) | <0.0001 | 3.60±0.95 (1–5) | 3.37±0.91 (1–5) | <0.0001 |
| Self-reported number of chronic diseases | 2 (1–2) | 1 (1–1) | 2 (2–2) | 0.004 | 2 (1–2) | 1 (1–2) | 0.884 |
Table 2 shows the prevalence and frequency of the ten depressive symptoms. The most prevalent positive affect at T1, T2, and T3 was “D1: happy” (T1: 68.44%; T2: 77.66%; T3: 78.50%). The most prevalent negative symptom at T1, T2, and T3 was “D4: sleep was restless” (T1: 53.06%; T2: 54.92%; T3: 58.12%). The most frequent positive affect was “D1: happy” (T1: 2.49±1.22; T2: 2.84±1.22; T3: 2.87±1.20). The most frequent negative symptom was “D4: sleep was restless” (T1: 2.09±1.20; T2: 2.11±1.23; T3: 2.27±1.26).
Table 2.
Prevalence and frequency of depressive symptoms in T1, T2, and T3 (N=3558)
| Label | Item | T1 | T2 | T3 | |||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Prevalence | Frequency | Prevalence | Frequency | Prevalence | Frequency | ||
|
| |||||||
| D1 | Happy | 2435 (68.44%) |
2.49±1.22 | 2763 (77.66%) |
2.84±1.22 | 2793 (78.50%) |
2.87±1.20 |
| D2 | Felt lonely | 894 (25.13%) |
1.46±0.89 | 1159 (32.57%) |
1.56±1.01 | 1288 (36.20%) |
1.71±1.10 |
| D3 | Felt depressed | 1565 (43.99%) |
1.80±1.03 | 1859 (52.25%) |
1.93±1.10 | 1928 (54.19%) |
1.99±1.12 |
| D4 | Sleep was restless | 1888 (53.06%) |
2.09±1.20 | 1954 (54.92%) |
2.11±1.23 | 2068 (58.12%) |
2.27±1.26 |
| D5 | Could not get going | 613 (17.23%) |
1.30±0.75 | 922 (25.91%) |
1.40±0.88 | 1029 (28.92%) |
1.50±0.96 |
| D6 | Everything an effort | 1622 (45.59%) |
1.88±1.11 | 1770 (49.75%) |
1.96±1.18 | 1989 (55.90%) |
2.12±1.20 |
| D7 | Felt hopeful | 2218 (62.34%) |
2.37±1.27 | 2406 (67.62%) |
2.50±1.29 | 2529 (71.08%) |
2.60±1.27 |
| D8 | Bothered by things | 1607 (45.17%) |
1.82±1.07 | 1788 (50.25%) |
1.93±1.15 | 1892 (53.17%) |
2.00±1.15 |
| D9 | Had trouble keeping mind | 1502 (42.21%) |
1.75±1.03 | 1716 (48.23%) |
1.88±1.13 | 1907 (53.18%) |
1.98±1.13 |
| D10 | Felt fearful | 569 (15.99%) |
1.28±0.72 | 823 (23.13%) |
1.35±0.83 | 909 (25.54%) |
1.45±0.90 |
Supplementary Table S1 shows the results of the comparisons of characteristics and symptom frequency between the participants in the study and those who excluded from the study. The included samples were younger (P<0001), had higher number of minorities (P=0.015) and lower educational attainment (P<0.0001), and had more rural residents (P<0.0001) than the excluded samples.
Interference in the full sample network
The accuracy plots and case-drop bootstrapping results showed high accuracy of the network (see Supplementary Figure S1). The case-drop bootstrapping results suggested strong stability for in-expected influence (coefficient=0.75), out-expected influence (coefficient=0.75), and closeness (coefficient=0.67) (see Supplementary Figure S2). Figure 1a shows the dynamic network. All edge weights are given in Supplementary Table S2. In the dynamic symptom network, the strongest direct positive effects were “D10: felt fearful” -> “D6: felt everything I did was an effort” (β=0.14), followed by “D10: felt fearful” -> “D8: bothered by things” (β=0.13), “D6: felt everything I did was an effort” -> “D3: felt depressed” (β=0.11), “D10: felt fearful” -> “D5: could not get going” (β=0.11), and “D8: bothered by things” -> “D9: had trouble keeping my mind” (β=0.11). The strongest direct negative effects were “D9: had trouble keeping my mind” -> “D1: happy” (β=−0.06) and “D6: felt everything I did was an effort” -> “D7: felt hopeful about the future” (β=−0.06).
Figure 1.
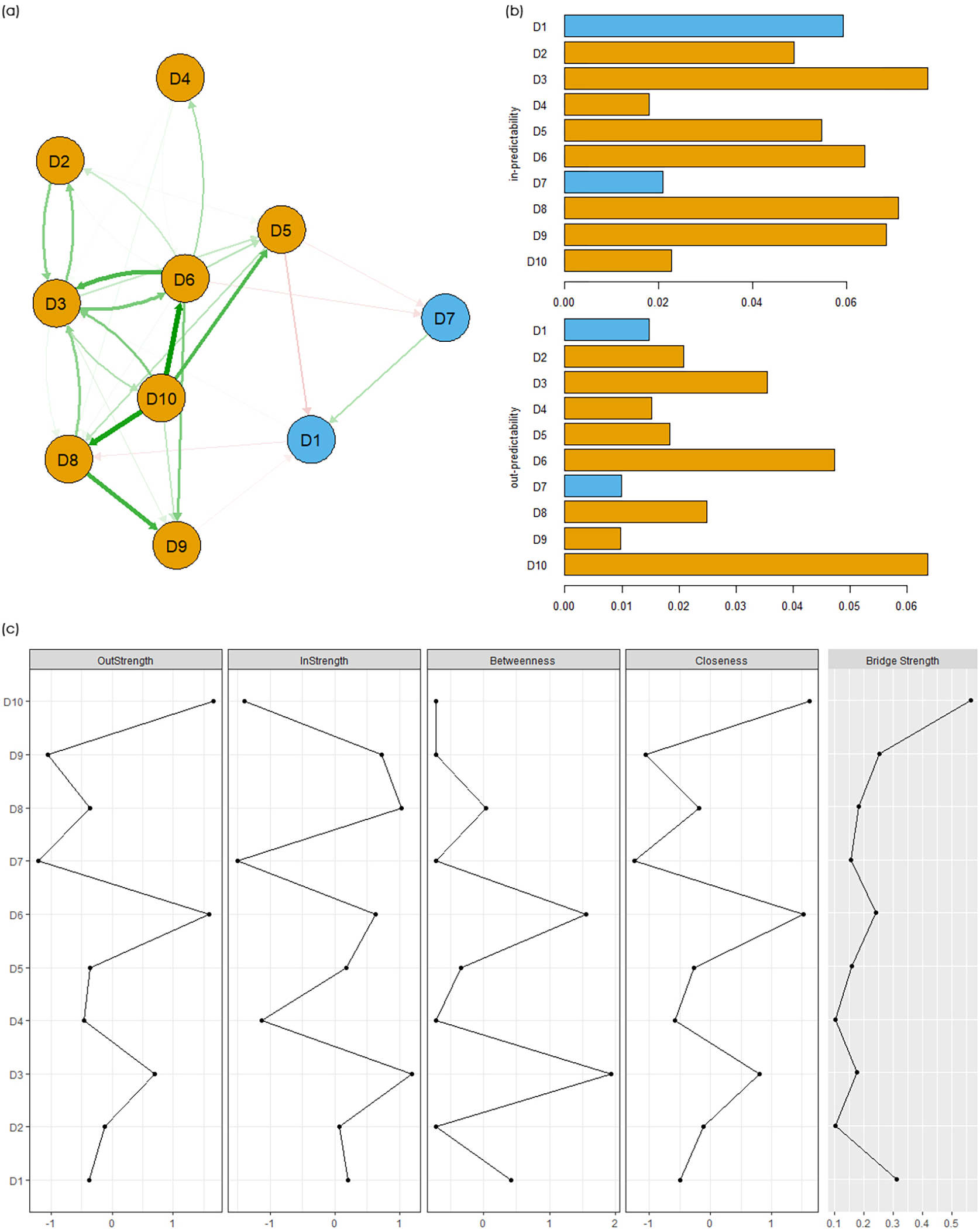
Dynamic networks in full sample (N=3558). (a) Dynamic networks; (b) In-predictability and out-predictability of 10 nodes; (c) Node inshrength, out-strength, and bridge strength of 10 nodes. D1=happy, D2=felt lonely, D3=felt depressed, D4=sleep was restless, D5=could not get going, D6=felt everything I did was an effort, D7=felt hopeful about the future, D8=bothered by things, D9=had trouble keeping my mind, and D10=felt fearful. Blue nodes and bars represent positive affects. Yellow nodes and bars represent negative symptoms.
Figures 1b and 1c show the predictability, centrality, and bridge centrality of 10 nodes. All values are presented in Supplementary Table S3. “D3: felt depressed” reported the largest value of in-predictability (r=0.077) and in-strength (r=0.545), followed by “D8: bothered by things” (in-predictability: r=0.071; in-strength: r=0.525). “D10: felt fearful” reported the largest value of out-predictability (r=0.064) and out-strength (r=0.635), followed by “D6: felt everything I did was an effort” (out-predictability: r=0.047; out-strength: r=0.625). Between two clusters (positive affects and negative symptoms), “D1: happy” had the largest value of bridge strength in the positive affects cluster (r=0.313) and “D10: felt fearful” had the largest value of bridge strength in the negative symptoms cluster (r=0.565).
Differences in dynamic networks in men and women
Figures 2a and 2b show the dynamic network in men and women. In men (Figure 2a), the strongest direct positive effects were “D10: felt fearful” -> “D8: bothered by things” (β=0.16), followed by “D10: felt fearful” -> “D6: felt everything I did was an effort” (β=0.15) and “D6: felt everything I did was an effort” -> “D3: felt depressed” (β=0.15). The strongest direct negative effects were “D2: felt lonely” -> “D1: happy” (β=−0.11). However, in women (Figure 2b), the strongest direct positive effects were “D8: bothered by things” -> “D9: had trouble keeping my mind” (β=0.13), followed by “D10: felt fearful” -> “D6: felt everything I did was an effort” (β=0.12). The strongest direct negative effects were “D5: could not get going” -> “D1: happy” (β=−0.12). All edge weights, accuracy, and stability indicators are given in Supplementary Tables S4 and S5 and Figures S3–S6.
Figure 2.
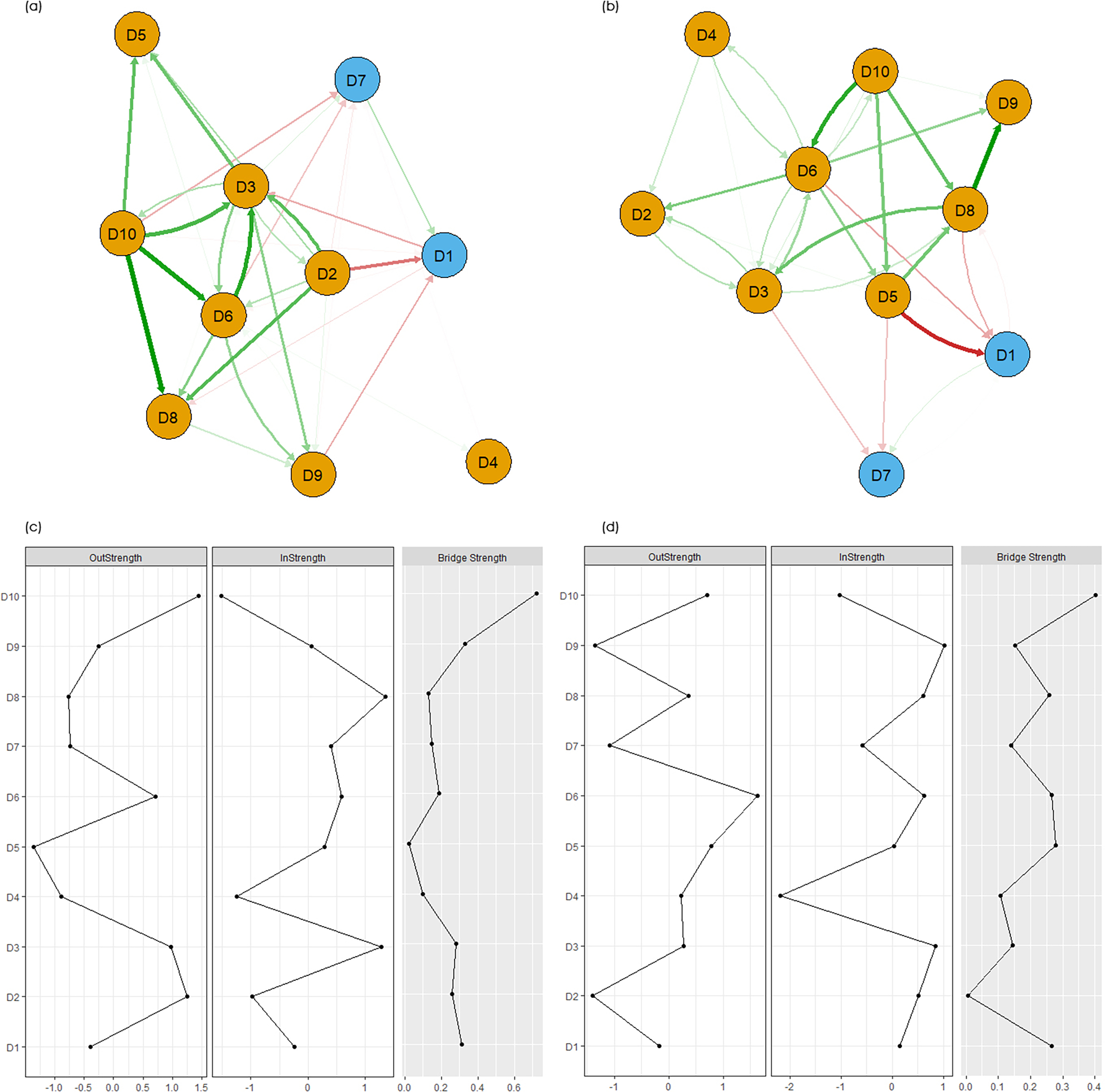
Dynamic networks in men and women. (a) Dynamic networks in men; (b) Dynamic networks in women; (c) Centrality and bridge centrality of 10 nodes in men’s network; (d) Centrality and bridge centrality of 10 nodes in women’s network. D1=happy, D2=felt lonely, D3=felt depressed, D4=sleep was restless, D5=could not get going, D6=felt everything I did was an effort, D7=felt hopeful about the future, D8=bothered by things, D9=had trouble keeping my mind, and D10=felt fearful. Blue nodes and bars represent positive affects. Yellow nodes and bars represent negative symptoms.
Figures 2c and 2d show the centrality and bridge centrality of nodes in men and women. All values of centrality indicators were shown in Supplementary Tables S6 and S7. In dynamic networks in men, “D8: bothered by things” reported the largest value of in-predictability (r=0.092) and in-strength (r=0.626). “D10: felt fearful” reported the largest value of out-predictability (r=0.095) and out-strength (r=0.769). However, in women, “D9: had trouble keeping my mind” reported the largest value of in-predictability (r=0.062) and in-strength (r=0.471). “D6: felt everything I did was an effort” reported the largest value of out-predictability (r=0.045) and out-strength (r=0.597). “D1: happy” has the largest value of bridge strength in the positive affects cluster (r=0.265) and “D10: felt fearful” has the largest value of bridge strength in the negative symptoms cluster (r=0.403).
Differences in dynamic networks in urban and rural populations
Figures 3a and 3b show the dynamic network in urban and rural populations. In urban populations (Figure 3a), the strongest direct positive effects were “D5: could not get going” -> “D3: felt depressed” (β=0.24), followed by “D3: felt depressed” -> “D6: felt everything I did was an effort” (β=0.18) and “D5: could not get going” -> “D6: felt everything I did was an effort” (β=0.16). The strongest direct negative effects were “D10: felt fearful” -> “D7: felt hopeful about the future” (β=−0.22). However, in rural populations (Figure 3b), the strongest direct positive effects were “D10: felt fearful” -> “D6: felt everything I did was an effort” (β=0.12), “D10: felt fearful” -> “D8: bothered by things” (β=0.12), and “D8: bothered by things” -> “D9: had trouble keeping my mind” (β=0.12). The strongest direct negative effects were “D5: could not get going” -> “D1: happy” (β=−0.07). All edge weights, accuracy, and stability indicators are given in Supplementary Tables S8 and S9 and Figures S7–S10.
Figure 3.
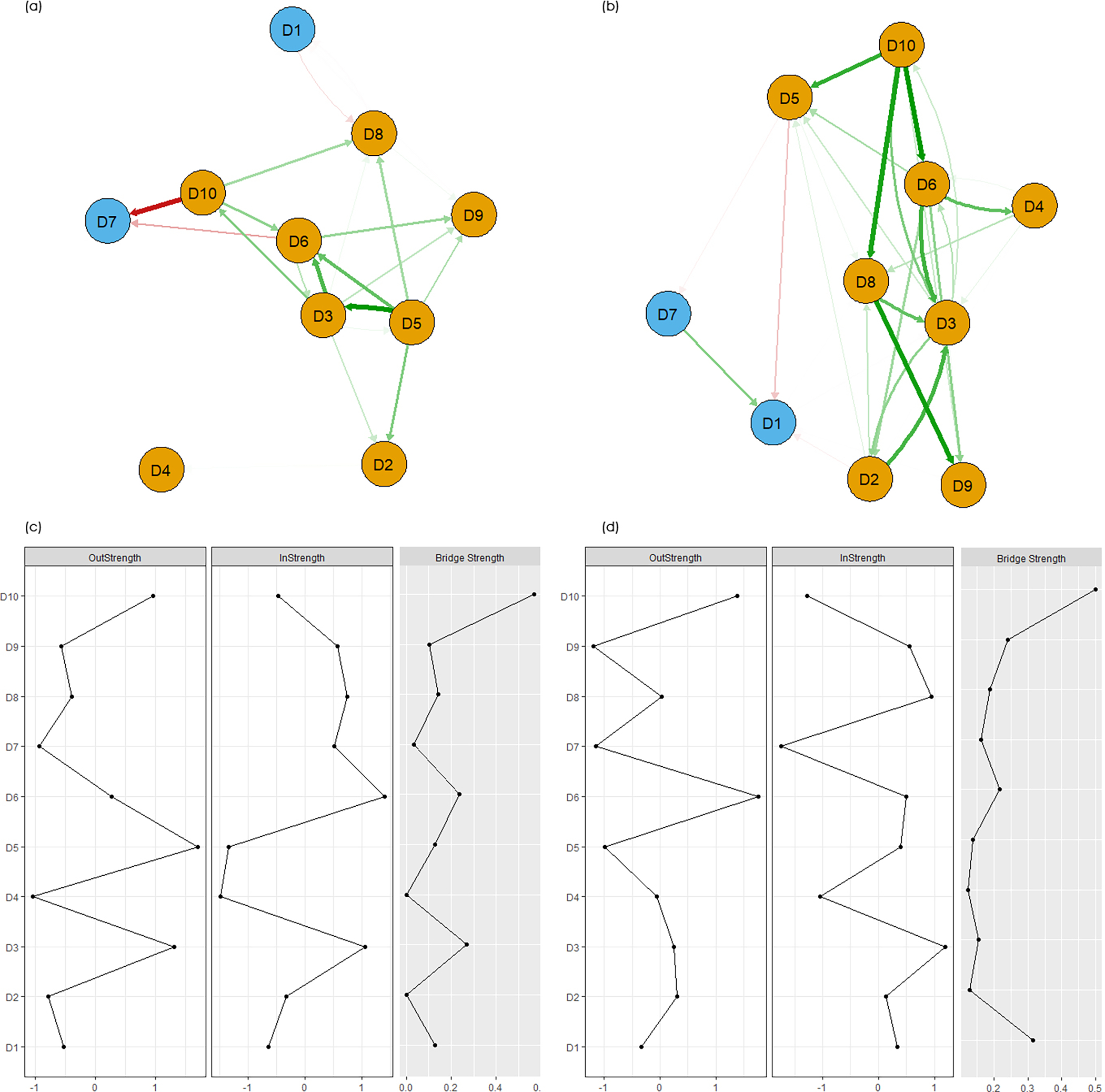
Dynamic networks in urban and rural populations. (a) Dynamic networks in urban populations; (b) Dynamic networks in rural populations; (c) Centrality and bridge centrality of 10 nodes in network in urban populations; (d) Centrality and bridge centrality of 10 nodes in network in rural populations. D1=happy, D2=felt lonely, D3=felt depressed, D4=sleep was restless, D5=could not get going, D6=felt everything I did was an effort, D7=felt hopeful about the future, D8=bothered by things, D9=had trouble keeping my mind, and D10=felt fearful. Blue nodes and bars represent positive affects. Yellow nodes and bars represent negative symptoms.
Figures 3c and 3d show the centrality and bridge centrality of nodes in urban and rural populations. All values of centrality indicators were shown in Supplementary Tables S10 and S11. In dynamic networks in urban populations, “D6: felt everything I did was an effort” reported the largest value of in-predictability (r=0.088) and in-strength (r=0.518). “D5: could not get going” reported the largest value of out-predictability (r=0.128) and out-strength (r=0.783). “D1: happy” has the largest value of bridge strength in the positive affects cluster (r=0.127) and “D10: felt fearful” has the largest value of bridge strength in the negative symptoms cluster (r=0.571). However, in rural populations, “D3: felt depressed” reported the largest value of in-predictability (r=0.075) and in-strength (r=0.526). “D10: felt fearful” reported the largest value of out-predictability (r=0.054). “D6: felt everything I did was an effort” reported the largest value of out-strength (r=0.614). “D1: happy” has the largest value of bridge strength in the positive affects cluster (r=0.314) and “D10: felt fearful” has the largest value of bridge strength in the negative symptoms cluster (r=0.501).
Discussion
To our knowledge, this is the first study to use a VAR network approach to identify longitudinal relationships across ten depressive symptoms in middle-aged and older adults in China. Despite the low prevalence and frequency of “felt fearful”, it was the strongest predictor of depressive symptoms compared to the other nine symptoms based on node centrality. “Felt fearful” was also the most crucial bridge node between the negative symptoms cluster and the positive affects cluster. However, substantial heterogeneity in the network may stem from individuals’ sex and place of residence. Understanding the psychopathology of depressive symptoms through this study may provide empirical evidence for the development of efficient and precise psychotherapeutic interventions.
Although “felt fearful” reported the lowest prevalence and frequency compared to other symptoms, it had the highest out-strength after adjusting for other symptoms at T1 and covariates, suggesting that “felt fearful” is the strongest predictor of other depressive symptoms. In short, depression in middle-aged and older adults in China may arise from fear. Previous studies showed that the most common fears in older adults are reduced dignity, poor physical conditions, low levels of cognitive function, loss of independence, and financial difficulties (Barnett & Adams, 2018; Shao et al., 2021). Fear leads to individuals’ increasing physical and mental frailty, making it difficult for them to find hobbies, go out, and meet friends after retirement (Bartholomaeus et al., 2019). Our study also demonstrates reciprocal paths between fear and other depressive symptoms. Feeling fearful may in turn increase thoughts of worthlessness.
Different from the other studies’ results, we found that loneliness and social isolation were not major contributing factors to fear among Chinese older adults in this study (Achterbergh et al., 2020; Wu et al., 2020). In this study, fear can also reflect a sense of insecurity. In Chinese culture, adult children’s sense of filial piety plays an important role in parents’ financial security and mental health status (Yang et al., 2018; Chen et al., 2019). Filial piety is a traditional norm in Chinese culture. While an attitude of respect for parents and ancestors is a universal value shared by most cultures, filial piety in Chinese culture is almost equivalent to the social obligation for children to care for their parents throughout their lives (Bedford & Yeh, 2021). This form of social responsibility provides emotional and financial security for older adults in China. The sense of obligation is not affected by whether adult children live with their parents or not. In addition, previous studies conducted in China found that the higher the filial expectations of older adults for their children, the less loneliness they experience (Zheng & Li, 2022; Ren et al., 2022). Chinese older adults have a high sense of filial expectations. They expect their children to fulfill their filial responsibility through their communications and daily exchanges. With higher filial expectations, older adults often provide support to their children as much as they can, and expect to receive support from their children when it is time to repay. This expectation reduces the experience of loneliness in the process of interacting with their children (Ren et al., 2022). Therefore, low levels of cumulative loneliness may not cause them to feel fear and do not lead to the appearance of other depressive symptoms eventually.
In addition, in the networks of the full sample and subgroups, “felt fearful” is the main bridge node between the depressive symptoms cluster and the positive affects cluster. Bridge symptoms are considered to be the core symptom for the emergence and maintenance of clusters (Castro et al. 2019). This suggests that precise psychotherapeutic treatments should aim to alleviate bridge symptoms. In our study, “felt fearful” predicted decreased positive affects, including “felt hopeful” and “happy”. However, positive affects did not strongly impact the changes in “felt fearful”. These results indicate that positive psychological interventions, developing an individual’s character strengths through identifying their successes and areas of growth, may not adequately address the fundamental causes of depression. These findings have the potential of explaining why the long-term effects of positive psychology interventions on depression do not last beyond three months (Bolier et al., 2013; Donaldson et al., 2019). Bolier and colleagues’ systematic review also showed that positive psychology interventions did not significantly change levels of depression after a three-months follow-up (Bolier et al., 2013). Positive psychology has three pillars: positive subjective experiences, positive traits, and positive institutions. None of the pillars aim to fix negative emotions, negative thinking, and negative well-being. As stated by Donaldson et al., accentuating the positive symptoms does not mean simultaneously attenuating the negative symptoms (Donaldson et al., 2019).
We also found heterogeneity in the psychopathology of depressive symptoms in men and women. Unlike depressive symptoms in men that stem from fear, depressive symptoms in women may be caused by a decline in physical, cognitive, and mental health status (Hyde & Mezulis, 2020). The trigger for feelings of worthlessness could be anything subtle in daily life. This partly explains why the prevalence of depressive symptoms is significantly higher in older women than in older men. Previous studies have mainly explained sex differences in depression from a sociological and social-structural perspective that a higher level of sex differences in depression is strongly associated with more severe gender inequalities (Parker & Brotchie, 2010; Lee et al., 2009; Elliott, 2001). Our study provides a new explanation for understanding the magnitude of psychological gender differences from a psychopathological perspective.
Furthermore, although women reported a higher frequency of depressive symptoms than men, which is consistent with previous studies, the weighted sum of all absolute connections (network density) and strength centrality (Σstrength) in women’s networks were smaller than in men’s networks. Network density and Σstrength are two key indicators of prognosis and emotional vulnerability. While the usefulness of these indicators is still under debate, these indicators have been widely used in previous studies (Shin et al., 2022; Zhu et al., 2021). Our results indicate that middle-aged and older men are more emotionally vulnerable than women. This finding is consistent with previous studies regarding how sociological knowledge shapes psychological resilience and vulnerability through the meanings people attach to gender roles (Pudrovska, 2010). In the face of fear, men rely more on their individual abilities than on support from other people and communities (Ozbay et al., 2007). Middle-aged and older men are particularly emotionally vulnerable to depressive symptoms, thus, it underscores the importance of using new indicators in this population. There is also a need to design psychotherapeutic interventions specifically targeting their emotional vulnerability when developing interventions to address depressive symptoms.
The psychopathology of depressive symptoms differed significantly between urban and rural populations. Similar to the full sample, depressive symptoms in the rural populations were caused by fear. However, among urban residents, depressive symptoms were triggered by “could not get going” in daily life. Although urban residents in China have higher levels of income, better health care coverage, and higher living standards compared to rural populations, they face a higher cost of living which puts pressure on people who are already struggling in financial strain (Li et al., 2016). The health status of urban residents may be another trigger for not getting “going”. According to the national report, only 26.8% of older adults in urban areas currently live with their children, and even in the senior group aged 80 and above, the proportion of living independently is 48%, which is much higher than 16% in rural areas (Gu et al., 2019; Zhang et al., 2019). Therefore, if middle-aged and older adults in urban areas report poor health and no family members can take care of them, the thoughts that they “could not get going” may trigger other depressive symptoms.
Limitations
Although this is the first study on the longitudinal relationships between depressive symptoms in middle-aged and older adults in China, some limitations warrant attention. First, this study explored longitudinal relationships across ten depressive symptoms by using the CES-D 10 items version. Other depressive symptoms not included in this study may have a higher value of centrality indices. Future studies should use the full version of CES-D to further verify the study findings. Second, this study assessed three waves of data which are two years apart. The results can only show the long-term longitudinal relationships across depressive symptoms. It may not be sensitive enough to reflect the longitudinal relationships in the short term. Third, symptoms were assessed using only one item. It is still not as reliable as using a combination of multiple items. However, this approach is a common practice in psychopathology. Finally, there are significant differences between the excluded and included samples in age, ethnicity, educational attainment, and place of residence. The attrition issue is a particular concern for minorities, younger adults, individuals with low levels of education, and rural residents; thus, might limit the generalizability of the study findings.
Conclusions
This study used a nationally representative sample of middle-aged and older adults in China. We identified the longitudinal relationships in the psychopathology of depressive symptoms in middle-aged and older adults and further explored differences across gender and place of residence subgroups. We found that despite the low prevalence and frequency of “felt fearful” reports, it was the strongest predictor of depressive symptoms compared to the other nine depressive symptoms based on nodal centrality. However, substantial network heterogeneity may come from an individual’s sex and place of residence. This study provides the knowledge base for designing more precise and effective psychotherapeutic interventions for middle-aged and older adults in China. Health care professionals should pay a higher alert when middle-aged and older adults report a high frequency of feeling fearful. Understanding the causes of fear is a prerequisite for interventions. We recommend that fear-decreasing modules should be included in the multimodal interventions for depression or depressive symptoms. To reduce the level of fear, interventions such as exposure therapy, cognitive behavioral therapy, yoga therapy, and animal-assisted therapy could be used to target this symptom. Network density and the sum of all absolute strength centrality should also be incorporated into clinical practice as key indicators of emotional vulnerability, particularly in middle-aged and older men.
Supplementary Material
Funding
This study is partially supported by the National Institutes of Health (P30AG059304, P50MD017356).
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
Ethics approval
CHARLS project were reviewed and approved by Peking University. For more details on consent to participate and consent for publication, please see CHARLS’s official website (https://charls.pku.edu.cn/).
References
- Achterbergh L, Pitman A, Birken M, Pearce E, Sno H, & Johnson S (2020). The experience of loneliness among young people with depression: a qualitative meta-synthesis of the literature. BMC psychiatry, 20(1), 415. 10.1186/s12888-020-02818-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexopoulos GS (2005). Depression in the elderly. Lancet (London, England), 365(9475), 1961–1970. 10.1016/S0140-6736(05)66665-2 [DOI] [PubMed] [Google Scholar]
- Barnett MD, & Adams CM (2018). Ageism and aging anxiety among young adults: Relationships with contact, knowledge, fear of death, and optimism. Educational Gerontology, 44(11), 693–700. [Google Scholar]
- Bartholomaeus JD, Van Agteren J, Iasiello MP, Jarden A, & Kelly D (2019). Positive Aging: The Impact of a Community Wellbeing and Resilience Program. Clinical gerontologist, 42(4), 377–386. 10.1080/07317115.2018.1561582 [DOI] [PubMed] [Google Scholar]
- Bedford O, & Yeh KH (2021). Evolution of the Conceptualization of Filial Piety in the Global Context: From Skin to Skeleton. Frontiers in psychology, 12, 570547. 10.3389/fpsyg.2021.570547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birk JL, Kronish IM, Moise N, Falzon L, Yoon S, & Davidson KW (2019). Depression and multimorbidity: Considering temporal characteristics of the associations between depression and multiple chronic diseases. Health psychology: official journal of the Division of Health Psychology, American Psychological Association, 38(9), 802–811. 10.1037/hea0000737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, & Bohlmeijer E (2013). Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC public health, 13, 119. 10.1186/1471-2458-13-119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bringmann LF, Vissers N, Wichers M, Geschwind N, Kuppens P, Peeters F, Borsboom D, & Tuerlinckx F (2013). A network approach to psychopathology: new insights into clinical longitudinal data. PloS one, 8(4), e60188. 10.1371/journal.pone.0060188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro D, Ferreira F, de Castro I, Rodrigues AR, Correia M, Ribeiro J, & Ferreira TB (2019). The Differential Role of Central and Bridge Symptoms in Deactivating Psychopathological Networks. Frontiers in psychology, 10, 2448. 10.3389/fpsyg.2019.02448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L, Alston M, & Guo W (2019). The influence of social support on loneliness and depression among older elderly people in China: Coping styles as mediators. Journal of community psychology, 47(5), 1235–1245. 10.1002/jcop.22185 [DOI] [PubMed] [Google Scholar]
- Dogaheh ER, Mohammadkhani P, & Dolatshahi B (2011). Comparison of group and individual cognitive-behavioral therapy in reducing fear of negative evaluation. Psychological reports, 108(3), 955–962. 10.2466/02.21.PR0.108.3.955-962 [DOI] [PubMed] [Google Scholar]
- Donaldson SI, Lee JY, & Donaldson SI (2019). Evaluating positive psychology interventions at work: A systematic review and meta-analysis. International Journal of Applied Positive Psychology, 4(3), 113–134. [Google Scholar]
- Elliott M (2001). Gender differences in causes of depression. Women & health, 33(3–4), 163–177. [PubMed] [Google Scholar]
- Epskamp S, & Fried EI (2020). Bootstrap methods for various network estimation routines. Comprehensive R Archive Network. [Google Scholar]
- Foa EB, & McLean CP (2016). The Efficacy of Exposure Therapy for Anxiety-Related Disorders and Its Underlying Mechanisms: The Case of OCD and PTSD. Annual review of clinical psychology, 12, 1–28. 10.1146/annurev-clinpsy-021815-093533 [DOI] [PubMed] [Google Scholar]
- Gleeson H, Hafford-Letchfield T, Quaife M, Collins DA, & Flynn A (2019). Preventing and responding to depression, self-harm, and suicide in older people living in long term care settings: a systematic review. Aging & mental health, 23(11), 1467–1477. 10.1080/13607863.2018.1501666 [DOI] [PubMed] [Google Scholar]
- Groen RN, van Gils A, Emerencia AC, Bos EH, & Rosmalen J (2021). Exploring temporal relationships among worrying, anxiety, and somatic symptoms. Journal of psychosomatic research, 146, 110293. 10.1016/j.jpsychores.2020.110293 [DOI] [PubMed] [Google Scholar]
- Gu D, Feng Q, & Yeung WJ (2019). Reciprocal Dynamics of Solo-Living and Health Among Older Adults in Contemporary China. The journals of gerontology. Series B, Psychological sciences and social sciences, 74(8), 1441–1452. 10.1093/geronb/gby140 [DOI] [PubMed] [Google Scholar]
- Haslbeck J, & Waldorp LJ (2015). mgm: Estimating time-varying mixed graphical models in high-dimensional data. arXiv preprint arXiv:1510.06871. [Google Scholar]
- Hyde JS, & Mezulis AH (2020). Gender Differences in Depression: Biological, Affective, Cognitive, and Sociocultural Factors. Harvard review of psychiatry, 28(1), 4–13. 10.1097/HRP.0000000000000230 [DOI] [PubMed] [Google Scholar]
- Irwin M, Artin KH, & Oxman MN (1999). Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Archives of internal medicine, 159(15), 1701–1704. 10.1001/archinte.159.15.1701 [DOI] [PubMed] [Google Scholar]
- Jones PJ, Ma R, & McNally RJ (2021). Bridge Centrality: A Network Approach to Understanding Comorbidity. Multivariate behavioral research, 56(2), 353–367. 10.1080/00273171.2019.1614898 [DOI] [PubMed] [Google Scholar]
- Kaiser T, Herzog P, Voderholzer U, & Brakemeier EL (2021). Unraveling the comorbidity of depression and anxiety in a large inpatient sample: Network analysis to examine bridge symptoms. Depression and anxiety, 38(3), 307–317. 10.1002/da.23136 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: validity of a brief depression severity measure. Journal of general internal medicine, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson DN. Treating depression in old age: the reasons to be positive. Age Ageing. 2001;30(1):13–17. doi: 10.1093/ageing/30.1.13 [DOI] [PubMed] [Google Scholar]
- Lee S, Tsang A, Huang YQ, He YL, Liu ZR, Zhang MY, Shen YC, & Kessler RC (2009). The epidemiology of depression in metropolitan China. Psychological medicine, 39(5), 735–747. 10.1017/S0033291708004091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li LW, Liu J, Xu H, & Zhang Z (2016). Understanding Rural-Urban Differences in Depressive Symptoms Among Older Adults in China. Journal of aging and health, 28(2), 341–362. 10.1177/0898264315591003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li LW, Liu J, Xu H, & Zhang Z (2016). Understanding Rural-Urban Differences in Depressive Symptoms Among Older Adults in China. Journal of aging and health, 28(2), 341–362. 10.1177/0898264315591003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D, Xi J, Hall BJ, Fu M, Zhang B, Guo J, & Feng X (2020). Attitudes toward aging, social support and depression among older adults: Difference by urban and rural areas in China. Journal of affective disorders, 274, 85–92. 10.1016/j.jad.2020.05.052 [DOI] [PubMed] [Google Scholar]
- Luo H, Li J, Zhang Q, Cao P, Ren X, Fang A, Liao H, & Liu L (2018). Obesity and the onset of depressive symptoms among middle-aged and older adults in China: evidence from the CHARLS. BMC public health, 18(1), 909. 10.1186/s12889-018-5834-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lydon-Staley DM, Xia M, Mak HW, & Fosco GM (2019). Adolescent Emotion Network Dynamics in Daily Life and Implications for Depression. Journal of abnormal child psychology, 47(4), 717–729. 10.1007/s10802-018-0474-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okur Güney ZE, Sattel H, Witthöft M, & Henningsen P (2019). Emotion regulation in patients with somatic symptom and related disorders: A systematic review. PloS one, 14(6), e0217277. 10.1371/journal.pone.0217277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D, & Southwick S (2007). Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont (Pa. : Township)), 4(5), 35–40. [PMC free article] [PubMed] [Google Scholar]
- Parker G, & Brotchie H (2010). Gender differences in depression. International review of psychiatry (Abingdon, England), 22(5), 429–436. 10.3109/09540261.2010.492391 [DOI] [PubMed] [Google Scholar]
- Pudrovska T (2010). Why is Cancer More Depressing for Men than Women among Older White Adults?. Social forces; a scientific medium of social study and interpretation, 89(2), 535–558. 10.1353/sof.2010.0102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren P, Emiliussen J, Christiansen R, Engelsen S, & Klausen SH (2022). Filial Piety, Generativity and Older Adults’ Wellbeing and Loneliness in Denmark and China. Applied research in quality of life, 17(5), 3069–3090. 10.1007/s11482-022-10053-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rha SY, & Lee J (2021). Stable Symptom Clusters and Evolving Symptom Networks in Relation to Chemotherapy Cycles. Journal of pain and symptom management, 61(3), 544–554. 10.1016/j.jpainsymman.2020.08.008 [DOI] [PubMed] [Google Scholar]
- Schweren L, van Borkulo CD, Fried E, & Goodyer IM (2018). Assessment of Symptom Network Density as a Prognostic Marker of Treatment Response in Adolescent Depression. JAMA psychiatry, 75(1), 98–100. 10.1001/jamapsychiatry.2017.3561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao J, Yang H, Lei X, Li J, & Zhang Q (2021). The Shackles of Fear: A Moderated Mediation Model of How Fear of Aging May Increase Older Adults’ Vulnerability to Fraud. Clinical gerontologist, 44(5), 567–576. 10.1080/07317115.2019.1676354 [DOI] [PubMed] [Google Scholar]
- Shin KE, Newman MG, & Jacobson NC (2022). Emotion network density is a potential clinical marker for anxiety and depression: Comparison of ecological momentary assessment and daily diary. The British journal of clinical psychology, 61 Suppl 1(Suppl 1), 31–50. 10.1111/bjc.12295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang T, Jiang J, & Tang X (2021). Prevalence of depressive symptoms among older adults in mainland China: A systematic review and meta-analysis. Journal of affective disorders, 293, 379–390. 10.1016/j.jad.2021.06.050 [DOI] [PubMed] [Google Scholar]
- Traud AL, Frost C, Mucha PJ, & Porter MA (2009). Visualization of communities in networks. Chaos (Woodbury, N.Y.), 19(4), 041104. 10.1063/1.3194108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vittengl JR, Clark LA, Thase ME, & Jarrett RB (2022). Does Symptom Linkage Density Predict Outcomes in Cognitive Therapy for Recurrent Depression?. Journal of psychopathology and behavioral assessment, 44(2), 469–480. 10.1007/s10862-021-09914-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Yang H, Guo Z, Liu B, & Geng S (2019). Socio-demographic characteristics and co-occurrence of depressive symptoms with chronic diseases among older adults in China: the China longitudinal ageing social survey. BMC psychiatry, 19(1), 310. 10.1186/s12888-019-2305-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu B (2020). Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Global health research and policy, 5, 27. 10.1186/s41256-020-00154-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang F, Zhang J, & Wang J (2018). Correlates of loneliness in older adults in Shanghai, China: does age matter?. BMC geriatrics, 18(1), 300. 10.1186/s12877-018-0994-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Liu Z, Zhang L, Zhu P, Wang X, & Huang Y (2019). Association of living arrangements with depressive symptoms among older adults in China: a cross-sectional study. BMC public health, 19(1), 1017. 10.1186/s12889-019-7350-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Hu Y, Smith JP, Strauss J, & Yang G (2014). Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). International journal of epidemiology, 43(1), 61–68. 10.1093/ije/dys203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng X, & Li H (2022). How Chinese children’s filial piety beliefs affect their parents’ life satisfaction and loneliness. PsyCh journal, 11(6), 863–872. 10.1002/pchj.558 [DOI] [PubMed] [Google Scholar]
- Zhu Z, Guo M, Dong T, Han S, Hu Y, & Wu B (2022). Assessing psychological symptom networks related to HIV-positive duration among people living with HIV: a network analysis. AIDS care, 34(6), 725–733. 10.1080/09540121.2021.1929815 [DOI] [PubMed] [Google Scholar]
- Zhu Z, Hu Y, Xing W, Guo M, Zhao R, Han S, & Wu B (2019). Identifying Symptom Clusters Among People Living With HIV on Antiretroviral Therapy in China: A Network Analysis. Journal of pain and symptom management, 57(3), 617–626. 10.1016/j.jpainsymman.2018.11.011 [DOI] [PubMed] [Google Scholar]
- Zhu Z, Wen H, Yang Z, Han S, Fu Y, Zhang L, Hu Y, & Wu B (2021). Evolving symptom networks in relation to HIV-positive duration among people living with HIV: A network analysis. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases, 108, 503–509. 10.1016/j.ijid.2021.05.084 [DOI] [PubMed] [Google Scholar]
- Zhu Z, Xing W, Hu Y, Wu B, & So W (2021). Paradigm shift: Moving from symptom clusters to symptom networks. Asia-Pacific journal of oncology nursing, 9(1), 5–6. 10.1016/j.apjon.2021.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou C, Chen S, Shen J, Zheng X, Wang L, Guan L, Liu Q, & Yang Y (2018). Prevalence and associated factors of depressive symptoms among elderly inpatients of a Chinese tertiary hospital. Clinical interventions in aging, 13, 1755–1762. 10.2147/CIA.S170346 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


