Abstract
Iron overload is a condition involving excessive iron deposit in various organs, the liver being the main target organ for iron deposition and overload which are associated with significant liver morbidity and mortality. Iron overload can be categorized into primary and secondary causes. Primary iron overload, so-called hereditary hemochromatosis, is a well-recognized disease with available standard treatment recommendations. However, secondary iron overload is a more diverse disease with many unclear areas to be explored. Secondary iron overload is more prevalent than primary iron overload and occurs as a consequence of various causes which differ significantly across geographic regions. The main causes of secondary iron overload are iron-loading anemias, and chronic liver disease. The liver-related outcomes, patient outcomes, and treatment recommendations in these patients differ depending on the cause of iron overload. This review summarizes the causes, pathophysiology, liver-related outcomes, disease outcomes, and treatments of secondary iron overload.
Keywords: Iron overload, Hemochromatosis, Cirrhosis, Hepatocellular carcinoma, Thalassemia
Graphical abstract
Introduction
Iron overload is an important condition which may cause significant liver morbidity and mortality. Primary iron overload (hereditary hemochromatosis, HH) is caused by inheritance of mutated hemochromatosis-related genes. Secondary iron overload is a consequence of a wide-spectrum of causes, including hematologic disorders causing ineffective erythropoiesis, anemic conditions requiring repeated transfusion of red blood cells (RBCs), and chronic liver diseases. The cause of iron overload significantly differs across geographic regions which is largely attributed to ethnic differences due to the mutation of the homeostatic iron regulator (HFE) gene1,2 and the worldwide distribution of thalassemia.3
In this review, we summarize and discuss the cause, pathophysiology, clinical outcomes and treatment recommendations for various causes of secondary iron overload. Relevant publications in the PubMed database were selected for this review using the inclusion of the search terms ‘hemochromatosis’ or ‘iron overload’ and ‘liver’. Only the articles published in the English language were reviewed.
Physiology of iron metabolism
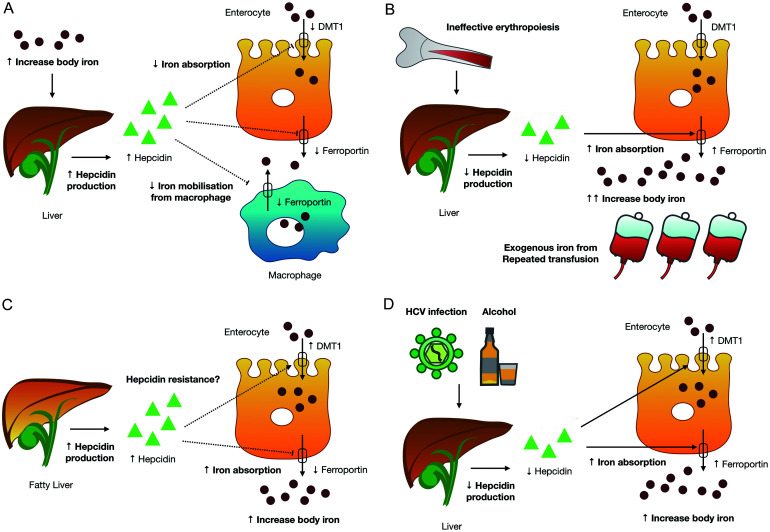
The normal adult human body contains 3–5 g of iron with over 70% being utilized for erythropoiesis, being present in the form of heme.4 The major locations used for storage of iron are the liver (20%), and tissue macrophages (5%). Muscle myoglobin contains approximately 2.5% of body iron and small iron amounts are present in the plasma. Ferritin is a cytosolic protein which plays a significant role in intracellular iron storage of excess body iron. In the physiologic condition, iron loss is minimal at 1–2 mg per day5 and the human body lacks mechanisms to excrete excess iron from the body. Only 1–2 mg of iron per day from the diet is required to maintain body iron balance. Rate of iron absorption is negatively correlated with body iron and the regulation of iron absorption from enterocytes plays an important role in inhibiting excess iron absorption, thereby preventing iron overload. Hepcidin, a liver-derived peptide, has the ability to control iron absorption from the intestine and iron recycling from macrophages. If the level of iron in the body is high, hepcidin binds to ferroportin, a transmembrane protein expressed on enterocytes and macrophages that acts as a cellular iron exporter.4,6 This leads to a reduction in iron absorption and limiting iron released into the bloodstream. Hepcidin-mediated regulation of iron homeostasis is shown in Figure 1A.6
Fig. 1. Hepcidin-mediated regulation of iron homeostasis and pathophysiology of iron overload in various diseases.
(A) Hepcidin-mediated regulation of iron homeostasis (adapted from Brissot P, et al.6). (B) Pathophysiology of iron overload in iron-loading anemias. (C) Pathophysiology of iron overload in non-alcoholic fatty liver disease. (D) Pathophysiology of iron overload in hepatitis C virus infection, and alcoholic liver disease. DMT1, divalent metal transporter 1.
Evaluation of iron overload and hyperferritinemia
Iron overload is a condition in which excessive iron is deposited in various organs, such as the liver, heart, pancreas, endocrine gland, joints, and skin. Evidence of iron overload is essential for the diagnosis of this condition. The iron study is the initial test to determine increased body iron contents, including serum iron (SI), total iron-binding capacity, and ferritin. Serum ferritin measurement has proved to be a valuable tool which has a good diagnostic accuracy for iron overload in the liver,7 however hyperferritinemia is not always equivalent to iron overload as it can result from systemic inflammation or malignancy. Elevated serum ferritin with or without elevation of transferrin saturation (TSAT) indicates the need for further evaluation for an increased in iron stores. TSAT is another important marker for the evaluation of iron overload. It reflects the body’s iron stores as well as the balance between reticuloendothelial iron release and bone marrow iron uptake. TSAT is approximately 30% under normal physiologic conditions,8 and it is usually elevated in cases where there is increased body iron. Expert consensus considers the upper limit of normal TSAT to be 45% and the elevation above this level is suggestive of iron overload.9 Ferritin is an acute-phase reactant and TSAT is typically low in inflammatory condtions.10 However, TSAT could also be normal to mildly elevated in certain causes of iron overload, e.g., nonalcoholic fatty liver disease, hepatitis C infection,8,11 and chronic kidney disease.9
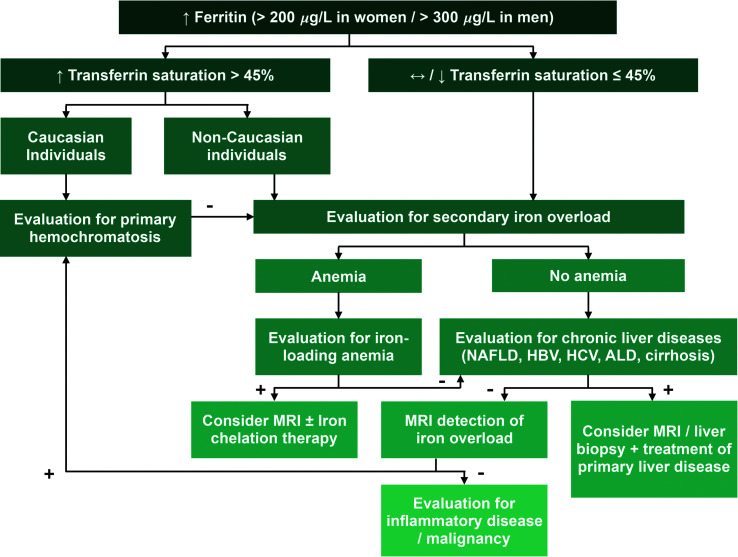
The prevalence of HH, and secondary iron overload ranged from 0–41%, and 4.8–35% respectively, in various populations with hyperferritinemia.12 The exclusion of acquired secondary iron overload is the recommended next step in management of this condition. In Caucasian populations, the high prevalence of HFE mutation13 supports the need for further genetic testing, while in non-white populations in which there is a low prevalence of this mutation,13 confirmation of iron overload by liver biopsy or other non-invasive method is proposed as the next step management. In Asia-Pacific populations, HH is uncommon and most of the HH patients are non-HFE hemochromatosis.14 A proposed algorithm of approach to patients with hyperferritinemia is shown in Figure 2.
Fig. 2. Proposed algorithm of approach to patients with hyperferritinemia.
ALD, alcoholic liver disease; HBV, hepatitis B virus; HCV, hepatitis C virus; MRI, magnetic resonance imaging; NAFLD, non-alcoholic fatty liver disease.
Liver biopsy is a standard procedure for the direct quantitative evaluation of hepatic iron content, measuring hepatic iron concentration (HIC) and the hepatic iron index. Iron overload is defined as HIC that exceeds the upper reference limit of 1.8 mg/g of dry weight liver tissue.15 HIC has been shown to be representative of total body iron.16 Although it is the gold standard for assessment of HIC and evaluation of liver fibrosis, liver biopsy is an invasive procedure with possible intra-liver iron concentration variability, especially in smaller samples17,18 or in the presence of cirrhosis.5 As an alternative to this invasive procedure, non-invasive methods to assess hepatic iron content have been developed. Currently, two non-invasive liver iron quantification methods are used, magnetic resonance imaging (MRI) and superconducting quantum interference device biomagnetic liver susceptometry (SQUID-BLS). SQUID-BLS is not widely available, which limits its use. MRI is a validated technique for determining HIC. The correlation between the results of MRI and liver biopsy for the detection of moderate to high iron overload from various causes is excellent.19,20 Therefore, MRI is currently considered an alternative standard non-invasive method for assessment of HIC.
Liver fibrosis assessment in patients with hemochromatosis is essential for prognostic evaluation and liver biopsy remains the gold standard. Liver stiffness measurement either by magnetic resonance elastography (MRE) or by transient elastography (TE) is widely conducted in various liver diseases. In a study of HH patients with elevated ferritin (>1,000 ng/mL) and/or raised transaminases, all patients with liver stiffness ≥13.9 kPa had severe fibrosis as determined by histological examination.21 With the use of TE, liver biopsy could be restricted to the 39% of patients who had intermediate or invalid TE results.21 Liver stiffness assessed by TE has also been shown to have a positive correlation with fibrosis stage in thalassemia patients.22 However, specific cut-off values for stratification of fibrosis stages has yet to be defined. MRE is generally an accurate method for detecting patients with advanced fibrosis.23 Despite that, the presence of high liver iron causing a very low hepatic signal is associated with failure of the standard gradient recall echo-based MRE techniques.24 To our knowledge, there have been no reports specifically comparing the MRE technique to liver biopsy results in patients with hemochromatosis. Additionally, no proposed cut-off level for each fibrosis stage is available due to limited data. Whether non-invasive techniques could substitute liver biopsy is currently inconclusive and more data is required. At present, liver biopsy should be considered only in cases in which a liver sample is required to evaluate concomitant liver diseases, in cases where the biochemical and radiologic results are discordant, for liver fibrosis assessment, or in the rare cases where MRI is unavailable.
Etiologies of secondary iron overload and their pathophysiology, and liver-related outcomes
Etiologies of secondary iron overload can be categorized into two main types of disorders, specifically iron-loading anemias, and chronic liver diseases (Table 1). Summary of the causes of secondary iron overload and their pathophysiology are shown in Figure 1.
Table 1. Major causes of secondary iron overload.
| Iron-loading anemias |
|---|
| With ineffective erythropoiesis |
| Thalassemia major or transfusion dependent thalassemia |
| Thalassemia intermedia or non-transfusion dependent thalassemia |
| Myelodysplastic syndrome |
| Sideroblastic anemia |
| Without ineffective erythropoiesis |
| Post hematopoietic stem cell transplantation |
| Sickle cell disease |
| Aplastic anemia |
| Chronic hemolytic anemia requiring red blood cells transfusion |
| Chronic kidney disease |
| Iron-loading anemias |
|---|
| Chronic liver diseases |
| Non-alcoholic fatty liver disease |
| Chronic viral hepatitis B and hepatitis C infection |
| Alcoholic liver disease |
| Cirrhosis and advanced liver disease |
Iron-loading anemias
Hematologic disorders requiring RBCs transfusion causes iron overload by acquiring iron from transfused blood. Conditions with ineffective erythropoiesis, characterized by the destruction of erythroblasts within the marrow, directly increase body iron. Additionally ineffective erythropoiesis suppresses hepcidin.25 Therefore, despite increased body iron, intestinal iron absorption is increased in these patients.
Thalassemia
Thalassemia is an inherited hemolytic syndrome caused by a reduction in or no production of the globin chains of hemoglobin. It is the most widely-recognized cause of iron-loading anemia causing iron overload. There are two most important types of thalassemia, alpha and beta, named after the affected globin chains. Thalassemia can be classified into three types based on disease severity and the need for transfusion. (1) Thalassemia minor with rare blood transfusion requirement, includes patients with the thalassemia alpha or beta trait, and homozygous HbE. (2) Thalassemia intermedia (TI) or nontransfusion-dependent thalassemia (NTDT) includes patients with beta thalassemia intermedia, HbE/β-thalassemia, and deletional HbH disease who occasionally require blood transfusion. (3) Thalassemia major (TM) or transfusion dependent thalassemia (TDT), includes patients with β-thalassemia major, severe HbE/β-thalassemia, and non-deletional HbH disease who regularly require blood transfusion.
Each RBC unit contains 200–250 mg of iron. Inevitable iron loading from repeated transfusion is the main mechanism of iron overload in patients with TDT. However, in NTDT patients, iron overload is more likely to be related to increased iron absorption secondary to hepcidin suppression from ineffective erythropoiesis.25 There are different patterns of organ complication of iron overload in patients with TDT, and NTDT. Selective involvement of liver rather than the myocardium is observed in NTDT patients.26,27 Complications of iron overload in TDT patients present early in life after 10–20 transfusions, while NTDT patients develop complications at 10–15 years of age. Liver fibrosis is found in 20–45%, and cirrhosis is found in 8–9% of thalassemia patients.28–30 Liver-related causes account for 5% of the deaths of TM patients.31 Advances in thalassemia treatment extends patients’ lives.32 The incidence of hepatocellular carcinoma (HCC) in thalassemia patients is increasing in parallel to the aging population of thalassemia.32 The annual incidence of HCC is estimated to be 1–2% and the risk in TI is twice greater than in TM patients.33,34 It is worth noting that high concomitant infection with viral hepatitis C has been observed.35 This condition is significantly related to the course of liver complications, especially the development of HCC in TDT patients.33,35,36 HCC may also develop in patients who are not infected with viral hepatitis, mainly in patients with TI.36 Despite cirrhosis being the strongest risk factor for HCC development, HCC occurrence in thalassemia patients with noncirrhotic liver were reported.37,38 HCC is now a well-recognized complication in the thalassemia population and regular HCC surveillance in liver cirrhosis patients is advocated.
Hematopoietic stem cell transplant patients
Hematopoietic stem cell transplantation (HSCT) is a cure of beta thalassemia major. The significant effect of pre-transplantation iron toxicity status on transplant outcomes in thalassemia patients has been recognized since the 1980s.39 The concept of regular and adequate chelation therapy being a key to successful transplantation is well accepted.39 Despite the curative nature of this treatment, patients may still have acquired iron overload prior to the transplantation as a consequence of the process of ineffective erythropoiesis and transfusions before and during transplantation. Liver damage caused by iron overload in these patients does not revert follow transplantation, and majority of the patients have progression of fibrosis after transplantation.40 Furthermore, bone marrow and liver iron released from the toxicity of pre-transplantation conditioning regimen may potentiate this condition.41 High iron loading with hepatic iron contents over 16 mg/g dry weight is associated with fibrosis progression following transplantation.42 When post-HSCT iron depletion is regular and efficient, hepatic fibrosis and even cirrhosis can be reversed.41 This highlights the need for both long-term monitoring of hepatic and iron status and adequate iron depletion treatment. Phlebotomy until complete removal of excess iron is an effective treatment43 and is a preferred method in this setting. Alternatively, deferasirox is a relatively safe and effective treatment with higher rates of patient satisfaction compared to phlebotomy.44
In transplant patients with other malignant and nonmalignant disorders besides thalassemia, serum ferritin has been identified as a surrogate marker associated with post-transplantation adverse outcomes.19 However, the impact of pretransplant iron overload on transplant outcomes, including mortality and complications, is inconclusive as there are multiple studies with conflicting results.45–48 The heterogeneity of underlying diseases with varying prognoses differ from homogenous thalassemia populations, and the varying duration of iron overload may in part explained these results. The pre-transplantation packed red cell transfusion burden of 20 or more correlated well with increased hepatic iron, and is a better predictor than ferritin level.47 Iron overload in a post-HSCT population is prevalent at 32% in adult allogeneic HSCT patients,49 and 26% in childhood cancer survivors who had HSCT.50 Excess iron is associated with cardiac, liver, and endocrine organ dysfunction.50 Iron overload is also a significant cause of liver dysfunction after allogeneic HSCT in these patients with the dysfunction being caused solely by iron overload in 10% of cases.51 Normalization of alanine aminotransferase in these patients was shown to be achievable by iron depletion therapy.51
Other hematologic disorders
Myelodysplastic syndrome (MDS) causes iron overload as a result of transfusion and ineffective erythropoiesis. Selective deposition of iron in the liver in MDS patients is observed. There is a relatively low rate of myocardial siderosis despite a higher degree of hepatic siderosis.26 Hepatic iron overload is very common in MDS with a prevalence of 68% and is associated with a significant decrease in patient survival.52 Any cases of anemia that required transfusion could cause hepatic iron overload and its consequences such as liver fibrosis.53 In a cohort of combining patients with anemia from other causes besides MDS and thalassemia, hepatic siderosis was found in 57% of patients.26 In patients with sickle cell disease (SCD), the autopsy findings revealed 23% with liver iron deposition, and 13% with liver cirrhosis.54 Transfusion volume was correlated with HIC and liver fibrosis in SCD patients requiring transfusion.55 Iron chelation is necessary in SCD patients with iron overload to prevent hepatic complications.
Anemia of chronic inflammation is characterized by active inflammatory illnesses leading to anemia. Iron dysregulation resulting in reduction of iron uptake at various sites is considered one of the pathogeneses of this condition. Hepcidin overproduction is induced by inflammatory cytokines, predominantly by interleukin-6,10,56 which leads to the degradation of ferroportin, thereby reducing iron released to plasma and inducing iron sequestration in macrophages. Hypoferremia, which is associated with high plasma ferritin and hepcidin levels, is a characteristic of this type of anemia. Ferritin is an acute-phase protein that is elevated during inflammation.57 For that reason, the condition is generally described as hyperferritinemia and iron sequestration rather than iron overload. However, iron overload may occur in that setting if the patient has received recurrent transfusions. To our knowledge, there is no study evaluating the prevalence and outcomes of liver iron overload in anemia of inflammation. It is expected that patient outcomes would be influenced by the quantity of blood transfused, as well as by the underlying causes of the inflammation.
Chronic kidney disease
Liver iron deposition is common in hemodialysis patients with a prevalence of 57%, which is negatively correlated with the degree of anemia.7 Changes in iron metabolism in chronic kidney disease patients is recognized but with unclear mechanisms. Shifting of the iron pool to the liver,33 and a blockade of iron utilization from reticuloendothelial cells have been proposed.4 Before the use of erythropoiesis stimulating agents, regular RBCs transfusion and parenteral iron administration have been important treatments to correct anemia in hemodialysis patients which lead to iron overload. After an introduction of erythropoiesis stimulating agents, which improve anemia and reduce iron overload, the concern regarding transfusion-related iron overload is reduced. However, parenteral iron is now regularly administered to replenish iron stores in hemodialysis patients and cause the cumulative iron dose to correlate with HIC.58 Despite high rates of liver iron overload, the presence of excess iron in the liver was not found to be associated with liver fibrosis,7,59 which suggests the limited clinical significance of this condition. Current international guideline does not recommend routine iron supplementation in patients with TSAT index >30% or serum ferritin >500 ng/mL due to limited data regarding risks and benefits.60
Chronic liver disease
More than a quarter of patients with chronic liver diseases have excessive iron deposition evidenced by liver biopsy specimens.61 Iron overload is found in patients with nonalcoholic fatty liver disease (NAFLD), alcoholic liver disease (ALD), viral hepatitis, and advanced liver disease.
Non-alcoholic fatty liver disease
The association between iron overload and liver steatosis in patients with insulin-resistant syndrome was first documented in the late 1990s.62 Hyperferritinemia is detected in about one-third of NAFLD patients,63 which is associated with hepatic iron deposition, a presence of non-alcoholic steatohepatitis (NASH), and worsened histologic activity, and is a predictor of advanced fibrosis.64 Increasingly higher mortality was also observed in NAFLD patients with high ferritin compared to those with normal ferritin value.65 The term, dysmetabolic iron overload syndrome (DIOS) is an iron overload condition characterized by hyperferritinemia or hepatic iron overload with normal or moderately increased TSAT associated with various components of metabolic syndrome.66 DIOS is detected in about one-third to half of patients with NAFLD.67,68
Stainable iron is found in the liver in 48% of patients with biopsy-proven NAFLD and is associated with higher hepatic events.68 In general, the pattern of iron deposition can present in three ways; parenchymal (hepatocellular) deposition, mesenchymal (reticuloendothelial system) deposition, or a mixed pattern. The patterns correlate with the mechanisms of iron deposition, iron stores in the reticuloendothelial system reflecting inflammatory causes, and iron deposition in hepatocytes is related to transfusion-related or primary iron overload. Iron overload in patients with NAFLD can present as any of these patterns and the pattern may be associated with the severity of disease and outcomes. The presence of mesenchymal iron is associated with increased liver-related events,68 and the mixed pattern is found to be associated with the diagnosis of NASH.69 However, another study reported more severe liver disease in patients with predominant hepatocellular iron deposition.70
Currently, the mechanisms underlying iron overload in patients with NAFLD is uncertain. Increased duodenal iron absorption through the upregulation of divalent metal transporter 1 (DMT1) in patients with NASH was demonstrated despite high serum hepcidin.71 Hepcidin increase in patients with NAFLD, and its role in DIOS remain elusive. Preserved hepcidin upregulation in response to increased iron stores is observed in patients with DIOS.72,73 However, a subtle hepcidin resistance state was demonstrated by impaired ability to limit iron absorption following iron challenge.74 This mechanism might partially explains increased DMT1 upregulation despite high hepcidin level. A genetic predisposition to iron accumulation may also contribute to the pathogenesis. In an Italian cohort of patients with NAFLD, the variants of genes related to iron metabolism, specifically ceruloplasmin, are associated with NAFLD-associated liver iron deposition, high ferritin levels, higher iron stores and more severe liver fibrosis.75 There is no association between HFE genotype and NAFLD.76 The homozygous H63D, and the combined heterozygous C282Y/H63D genotypes are found more frequently in patients with DIOS than in general population.77 However, the role of heterozygous mutation, and the effect of HFE mutation specifically in DIOS with NAFLD remained unknown. The elevation of SI or TSAT were associated with a 2- to 3-fold increased risk of HCC in patients with NAFLD.78 Evidence from case-control study shows that liver iron deposition was more frequent in patients with NASH cirrhosis and HCC than those without HCC.79 The risk of HCC in NAFLD patients with iron overload has not yet been evaluate in longitudinal study and the causal relationship cannot be concluded by current evidences.
Viral hepatitis
HIC is higher in patients with hepatitis C virus (HCV) and hepatitis B virus (HBV) infection than in other causes of chronic hepatitis.80 Approximately one-third of HCV patients had hyperferritinemia, but only half of the cases were associated with hepatic iron overload.81 In a cohort of HCV patients, serum ferritin was not found to be related to fibrosis and it only increases when alcoholism co-exists with HCV infection.82 The hepatitis C virus suppresses hepcidin expression83,84 resulting in upregulation of ferroportin, and increased duodenal iron absorption.85 Iron overload is well-recognized in patients with hepatitis C and is identified as an important factor associated with advanced disease.86 It is unclear whether hepatic iron is a surrogate marker for disease severity or the stimulating factor for increased hepatic inflammation and fibrosis. Current literatures leans toward the former as several studies show no correlation between baseline liver iron and liver fibrosis81 and progression of liver fibrosis.87 Prior to the direct-acting antivirals treatment era, there were efforts to evaluate the effect of phlebotomy on liver biochemical and histology,88 the increasing effectiveness of antiviral therapy,89 or for the treatment in those who fail to achieve sustained virological response.90 Currently, as direct-acting antivirals treatment cures more than 95% of treated patients, the role of phlebotomy might need to be re-evaluated.
Data on liver iron overload in patients infected with HBV is limited and the pathophysiology of this condition is rarely reported. Hepatic iron deposit is detected in 35.1% of patients and is more common in patients with hepatitis D virus-coinfection, in which there are more severe iron deposits and more advanced fibrosis than in monoinfected patients.91 The degree of iron deposition is less in HBV patients than in those with HCV.86 Serum hepcidin, and prohepcidin, a prohormone of hepcidin appears to be lower in patients with HBV,92,93 and the lower prohepcidin concentrations are related to the more advanced liver disease.93 Currently, there are no reports regarding the liver outcomes in patients with HBV and iron overload. The data regarding the treatment of this condition is also limited. Treatment with a combination of phlebotomy and deferoxamine was only described in a case report on a patient on long-term adefovir showing improvement of HIC.94 Another case report demonstrated complete resolution of iron overload symptoms and almost normalization of ferritin level with nucleoside analogue treatment.95
Alcoholic liver diseases
Iron deposition is common in patients with ALD with a prevalence of 57%.96 Iron overload plays a significant role in a pathogenesis of ALD by inducing oxidative stress. Alcohol down-regulates hepcidin leading to upregulation of iron transporters expression in the duodenum and increases iron absorption.97 Active alcohol drinking is a major factor associated with iron overload.98 Most of the studies found that HFE mutation carriers are not related to severity of liver disease99–101 and that the iron overload in this setting is not relevant to HFE status. Presence of hepatic iron increases the risk of death in patients with alcohol-associated cirrhosis with a relative risk of 2.27 (95% CI: 1.23–4.19).102 Increased liver iron overload is associated with a higher risk of HCC in alcohol-associated cirrhosis.103 A study to evaluate the treatment with phlebotomy in patients with compensated alcohol-associated liver cirrhosis was started in 2011, and terminated in 2015 due to delayed recruitment.104 Therefore, despite the apparent risk of iron overload in the progression of ALD, the treatment with phlebotomy has not yet been evaluated.
Cirrhosis, end-stage liver disease, hepatocellular carcinoma, and liver transplantation
Iron overload is detected in patients with other causes of end-stage liver disease (ESLD) besides the causes that are well-known as being related to iron overload.105 The pathogenesis of iron overload in patients with cirrhosis excepting those with HH is poorly understood. Multifactorial causes, such as extravascular hemolysis caused by hypersplenism, RBCs transfusion, exogenous oral iron in the state of reduced hepcidin level, and portosystemic shunting may have contributed to this phenomena.106 Stainable hepatic iron was detected in 32–37% of explanted liver105,107 with a more common prevalence in patients with nonbiliary cirrhosis.105 The presence of hepatic hemosiderosis in cirrhotic patients is associated with more advanced liver disease, accelerates hepatic decompensation, and decreases survival.108
It has been postulated from preclinical studies that chronic iron overload causes direct hepatocarcinogenesis by generation of reactive oxygen species, resulting in oxidative damage, and subsequent mutagenesis.109 Iron overload is associated with the presence of HCC in patients with ESLD of diverse etiologies.110 A large case-control study in Japan demonstrated that lower plasma hepcidin and higher plasma ferritin levels were associated with an increased risk of liver cancer (HR: 4.49, 95% CI: 2.71–7.43).111 Increased HIC is not a determinant of hepatic outcome after liver transplantation.107 However, iron loading in non-HFE related ESLD may be associated with concurrent pancreatic112 and cardiac iron overload.112,113 These patients are at increased risk of cardiovascular complication after liver transplantation for ESLD.114 Thorough cardiovascular evaluation prior to transplantation to investigate potential subclinical myocardial dysfunction in candidates with elevated ferritin or evidence of iron overload in other organs is recommended.
Treatment of secondary iron overload
The aim of treatment is to prevent and restore organ damage by reduction of body iron. Currently, phlebotomy and iron chelation are the two main treatments in this setting. A summary of the outcomes of secondary iron overload and the treatments recommended for each disease is shown in Table 2.
Table 2. Summary of laboratory findings, disease outcomes, liver-related outcomes, and recommendations for the treatment of iron overload in secondary iron overload.
| Cause | Laboratory findings | Disease outcomes and liver-related outcomes | Treatment recommendations |
|---|---|---|---|
| Thalassemia major | ↑Ferritin; ↑TSAT; ↓Hepcidin | ↑Liver fibrosis/cirrhosis; ↑HCC; ↓HSCT outcome | Deferasirox/deferiprone/deferoxamine |
| Thalassemia intermedia | ↑Ferritin; ↑TSAT; ↓Hepcidin | ↑Liver fibrosis/cirrhosis; ↑HCC | Deferasirox/deferiprone/deferoxamine |
| Ex-thalassemia (Post HSCT) | ↑Ferritin; ↑TSAT; | ↑Liver fibrosis/cirrhosis | Phlebotomy/deferasirox until excess iron is completely removed |
| Post HSCT (other diseases besides thalassemia) | ↑Ferritin; ↑TSAT | ↑Liver dysfunction | Phlebotomy or deferoxamine in patients with unstable erythroid engraftment |
| Myelodysplastic syndrome | ↑Ferritin; ↑TSAT; ↔Hepcidin | ↓Patient survival | Deferasirox |
| Sickle cell disease | ↑Ferritin; ↑TSAT; ↔/↓Hepcidin | ↑Liver fibrosis/cirrhosis | Deferasirox/deferiprone/deferoxamine |
| Chronic kidney disease | ↑Ferritin; ↔/↑TSAT; ↑Hepcidin | ↔Liver fibrosis | Judicious parenteral iron administration when TSAT index >30% or serum ferritin levels >500 ng/mL |
| Nonalcoholic fatty liver disease | ↑Ferritin; ↔/↑TSAT; ↑Hepcidin | ↑NASH; ↑Histologic activity; ↑Advanced fibrosis; ↑Hepatic events | No recommendation (Phlebotomy is not recommended) |
| Chronic viral hepatitis B infection | ↑Ferritin; ↑TSAT; | ↑Liver fibrosis (in patients with HDV coinfection) | No recommendation (antiviral treatment may improve iron overload) |
| Chronic viral hepatitis C infection | ↑Ferritin; ↔/↑TSAT; ↓Hepcidin | ↔Liver fibrosis | No recommendation |
| Alcoholic liver disease | ↑Ferritin; ↑TSAT; ↓Hepcidin | ↑Death/HCC (in patients with cirrhosis) | No recommendation |
| Advance liver disease | ↑Ferritin; ↑TSAT | ↑HCC; ↔LT outcomes (concurrent cardiac iron overload may increase risk of LT cardiovascular complications) | No recommendation |
HCC, hepatocellular carcinoma; HDV, hepatitis D virus; HSCT, hematopoietic stem cell transplantation; LT, liver transplantation; NASH, non-alcoholic steatohepatitis; TSAT, transferrin saturation.
Phlebotomy
Phlebotomy is the cornerstone treatment of HH and HSCT patients. Its role has been evaluated in diverse causes of iron overload without anemia. In patients with NAFLD, venesection significantly reduces serum ferritin and HIC.115 However, its effect on NAFLD outcomes shows conflicting results. A randomized-controlled trial by Valenti et al.116 showed significant histologic improvement following phlebotomy in an iron-depleted group compared to control.117 However, subsequent studies demonstrated null effects.117,118 It does not improve liver biochemistry in patients with DIOS and is associated with high rates of poor adherence to treatment, and treatment-related fatigue in a quarter of patients.118 Therefore, phlebotomy in NAFLD patients lacks supporting beneficial evidence and is not recommended. Venesection treatment in other chronic liver diseases was discussed earlier. Data supporting its use is lacking and is not routinely recommended. Phlebotomy is not considered the treatment of choice of iron overload in ineffective erythropoiesis-related anemia diseases because phlebotomy-induced anemia will further cause hepcidin dysregulation and increases intestinal iron absorption.
Iron chelating agents
Iron chelation is the mainstay treatment for patients with secondary iron overload with anemia, especially thalassemia patients. The association between iron overload and morbidity in thalassemia patients has been strongly substantiated and the need for chelation therapy is well established. Currently, there are three types of iron chelators. The use of these chelators in TM showed significant decreases of HIC.119–121 The first chelator that was approved is deferoxamine. It has a short half-life and is administered intravenously or subcutaneously, which has a significant impact on patient compliance and quality of life. The second is deferiprone, which is an oral chelator. Long-term use of deferiprone is associated with progression cessation of hepatic fibrosis in the majority of TM patients.122 Its most serious side effect is agranulocytosis and the neutrophil count should be monitored. The third is deferasirox. It use is associated with significant improvement in HIC and liver stiffness in TDT patients.123 It is also effective in reducing liver iron in NTDT patients,124 and MDS or AA patients with transfusional iron overload.125
Conclusions
Secondary iron overload is an important condition which significantly influence the liver outcomes in affected patients. Iron overload is a well-recognized complication of chronic transfusion in patients with iron-loading anemias. It is associated with increased liver fibrosis and cirrhosis in these patients. Iron chelation therapy is required to prevent iron overload and for the treatment of liver-related complications in patients with iron-loading anemias. In addition to liver-related complications, this condition may also have significant impact on primary hematologic disorders. The data relevant to patients with chronic liver disease is limited and currently, there is no treatment recommended. Future studies in patients with chronic liver disease should aim to explore the mechanisms associated with iron overload, the population at risk of liver-related complications, and the effect of treatments for iron overload on patient outcomes.
Abbreviations
- ALD
alcoholic liver disease
- DIOS
dysmetabolic iron overload syndrome
- DMT1
divalent metal transporter 1
- ESLD
end-stage liver disease
- HBV
hepatitis B virus
- HCC
hepatocellular carcinoma
- HCV
hepatitis C virus
- HH
hereditary hemochromatosis
- HIC
hepatic iron concentration
- HSCT
hematopoietic stem cell transplantation
- MDS
myelodysplastic syndrome
- MRE
magnetic resonance elastography
- MRI
magnetic resonance imaging
- NAFLD
nonalcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
- NTDT
nontransfusion-dependent thalassemia
- RBC
red blood cell
- SCD
sickle cell anemia
- SI
serum iron
- SQUID-BLS
superconducting quantum interference device biomagnetic liver susceptometry
- TDT
transfusion-dependent thalassemia
- TE
transient elastography
- TI
thalassemia intermedia
- TM
thalassemia major, TSAT, transferrin saturation
References
- 1.Lee JY, Yoo KH, Hahn SH. HFE gene mutation, C282Y causing hereditary hemochromatosis in Caucasian is extremely rare in Korean population. J Korean Med Sci. 2000;15(2):179–182. doi: 10.3346/jkms.2000.15.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Acton RT, Barton JC, Snively BM, McLaren CE, Adams PC, Harris EL, et al. Geographic and racial/ethnic differences in HFE mutation frequencies in the Hemochromatosis and Iron Overload Screening (HEIRS) Study. Ethn Dis. 2006;16(4):815–821. [PubMed] [Google Scholar]
- 3.De Sanctis V, Kattamis C, Canatan D, Soliman AT, Elsedfy H, Karimi M, et al. beta-Thalassemia Distribution in the Old World: an Ancient Disease Seen from a Historical Standpoint. Mediterr J Hematol Infect Dis. 2017;9(1):e2017018. doi: 10.4084/MJHID.2017.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Papanikolaou G, Pantopoulos K. Systemic iron homeostasis and erythropoiesis. IUBMB Life. 2017;69(6):399–413. doi: 10.1002/iub.1629. [DOI] [PubMed] [Google Scholar]
- 5.Williams R, Pitcher CS. Iron metabolism and the liver with particular reference to the pathogenesis of haemochromatosis. Postgrad Med J. 1963;39:193–204. doi: 10.1136/pgmj.39.450.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brissot P, Pietrangelo A, Adams PC, de Graaff B, McLaren CE, Loreal O. Haemochromatosis. Nat Rev Dis Primers. 2018;4:18016. doi: 10.1038/nrdp.2018.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carrilho P, Fidalgo P, Lima A, Bastos L, Soares E, Manso R, et al. Post-mortem liver and bone marrow iron quantification in haemodialysis patients: A prospective cohort study. EBioMedicine. 2022;77:103921. doi: 10.1016/j.ebiom.2022.103921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gkouvatsos K, Papanikolaou G, Pantopoulos K. Regulation of iron transport and the role of transferrin. Biochim Biophys Acta. 2012;1820(3):188–202. doi: 10.1016/j.bbagen.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 9.Fishbane S, Kowalski EA, Imbriano LJ, Maesaka JK. The evaluation of iron status in hemodialysis patients. J Am Soc Nephrol. 1996;7(12):2654–2657. doi: 10.1681/ASN.V7122654. [DOI] [PubMed] [Google Scholar]
- 10.Ganz T. Anemia of Inflammation. N Engl J Med. 2019;381(12):1148–1157. doi: 10.1056/NEJMra1804281. [DOI] [PubMed] [Google Scholar]
- 11.Milic S, Mikolasevic I, Orlic L, Devcic E, Starcevic-Cizmarevic N, Stimac D, et al. The Role of Iron and Iron Overload in Chronic Liver Disease. Med Sci Monit. 2016;22:2144–2151. doi: 10.12659/msm.896494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sandnes M, Ulvik RJ, Vorland M, Reikvam H. Hyperferritinemia-A Clinical Overview. J Clin Med. 2021;10(9):2008. doi: 10.3390/jcm10092008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adams PC, Reboussin DM, Barton JC, McLaren CE, Eckfeldt JH, McLaren GD, et al. Hemochromatosis and iron-overload screening in a racially diverse population. N Engl J Med. 2005;352(17):1769–1778. doi: 10.1056/NEJMoa041534. [DOI] [PubMed] [Google Scholar]
- 14.Lok CY, Merryweather-Clarke AT, Viprakasit V, Chinthammitr Y, Srichairatanakool S, Limwongse C, et al. Iron overload in the Asian community. Blood. 2009;114(1):20–25. doi: 10.1182/blood-2009-01-199109. [DOI] [PubMed] [Google Scholar]
- 15.Nuttall KL, Palaty J, Lockitch G. Reference limits for copper and iron in liver biopsies. Ann Clin Lab Sci. 2003;33(4):443–450. [PubMed] [Google Scholar]
- 16.Walker RJ, Miller JP, Dymock IW, Shilkin KB, Williams R. Relationship of hepatic iron concentration to histochemical grading and to total chelatable body iron in conditions associated with iron overload. Gut. 1971;12(12):1011–1014. doi: 10.1136/gut.12.12.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Villeneuve JP, Bilodeau M, Lepage R, Cote J, Lefebvre M. Variability in hepatic iron concentration measurement from needle-biopsy specimens. J Hepatol. 1996;25(2):172–177. doi: 10.1016/s0168-8278(96)80070-5. [DOI] [PubMed] [Google Scholar]
- 18.Urru SA, Tandurella I, Capasso M, Usala E, Baronciani D, Giardini C, et al. Reproducibility of liver iron concentration measured on a biopsy sample: a validation study in vivo. Am J Hematol. 2015;90(2):87–90. doi: 10.1002/ajh.23878. [DOI] [PubMed] [Google Scholar]
- 19.Gandon Y, Guyader D, Heautot JF, Reda MI, Yaouanq J, Buhe T, et al. Hemochromatosis: diagnosis and quantification of liver iron with gradient-echo MR imaging. Radiology. 1994;193(2):533–538. doi: 10.1148/radiology.193.2.7972774. [DOI] [PubMed] [Google Scholar]
- 20.St Pierre TG, Clark PR, Chua-anusorn W, Fleming AJ, Jeffrey GP, Olynyk JK, et al. Noninvasive measurement and imaging of liver iron concentrations using proton magnetic resonance. Blood. 2005;105(2):855–861. doi: 10.1182/blood-2004-01-0177. [DOI] [PubMed] [Google Scholar]
- 21.Legros L, Bardou-Jacquet E, Latournerie M, Guillygomarc’h A, Turlin B, Le Lan C, et al. Non-invasive assessment of liver fibrosis in C282Y homozygous HFE hemochromatosis. Liver Int. 2015;35(6):1731–1738. doi: 10.1111/liv.12762. [DOI] [PubMed] [Google Scholar]
- 22.Fraquelli M, Cassinerio E, Roghi A, Rigamonti C, Casazza G, Colombo M, et al. Transient elastography in the assessment of liver fibrosis in adult thalassemia patients. Am J Hematol. 2010;85(8):564–568. doi: 10.1002/ajh.21752. [DOI] [PubMed] [Google Scholar]
- 23.Marti-Aguado D, Rodriguez-Ortega A, Alberich-Bayarri A, Marti-Bonmati L. Magnetic Resonance imaging analysis of liver fibrosis and inflammation: overwhelming gray zones restrict clinical use. Abdom Radiol (NY) 2020;45(11):3557–3568. doi: 10.1007/s00261-020-02713-1. [DOI] [PubMed] [Google Scholar]
- 24.Wagner M, Corcuera-Solano I, Lo G, Esses S, Liao J, Besa C, et al. Technical Failure of MR Elastography Examinations of the Liver: Experience from a Large Single-Center Study. Radiology. 2017;284(2):401–412. doi: 10.1148/radiol.2016160863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Camaschella C, Nai A. Ineffective erythropoiesis and regulation of iron status in iron loading anaemias. Br J Haematol. 2016;172(4):512–523. doi: 10.1111/bjh.13820. [DOI] [PubMed] [Google Scholar]
- 26.Ho PJ, Hiwase D, Ramakrishna R, Viiala N, Solterbeck A, Traficante R, et al. Cardiac and hepatic siderosis in myelodysplastic syndrome, thalassemia and diverse causes of transfusion-dependent anemia: the TIMES study. Hemasphere. 2019;3(3):e224. doi: 10.1097/HS9.0000000000000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tantiworawit A, Charoenkwan P, Hantrakool S, Choeyprasert W, Sivasomboon C, Sanguansermsri T. Iron overload in non-transfusion-dependent thalassemia: association with genotype and clinical risk factors. Int J Hematol. 2016;103(6):643–648. doi: 10.1007/s12185-016-1991-5. [DOI] [PubMed] [Google Scholar]
- 28.Li CK, Chik KW, Lam CW, To KF, Yu SC, Lee V, et al. Liver disease in transfusion dependent thalassaemia major. Arch Dis Child. 2002;86(5):344–347. doi: 10.1136/adc.86.5.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prati D, Maggioni M, Milani S, Cerino M, Cianciulli P, Coggi G, et al. Clinical and histological characterization of liver disease in patients with transfusion-dependent beta-thalassemia. A multicenter study of 117 cases. Haematologica. 2004;89(10):1179–1186. [PubMed] [Google Scholar]
- 30.Chan LKL, Mak VWM, Chan SCH, Yu ELM, Chan NCN, Leung KFS, et al. Liver complications of haemoglobin H disease in adults. Br J Haematol. 2021;192(1):171–178. doi: 10.1111/bjh.17115. [DOI] [PubMed] [Google Scholar]
- 31.Daar S, Al Khabori M, Al Rahbi S, Hassan M, El Tigani A, Pennell DJ. Cardiac T2* MR in patients with thalassemia major: a 10-year long-term follow-up. Ann Hematol. 2020;99(9):2009–2017. doi: 10.1007/s00277-020-04117-z. [DOI] [PubMed] [Google Scholar]
- 32.Borgna-Pignatti C, Vergine G, Lombardo T, Cappellini MD, Cianciulli P, Maggio A, et al. Hepatocellular carcinoma in the thalassaemia syndromes. Br J Haematol. 2004;124(1):114–117. doi: 10.1046/j.1365-2141.2003.04732.x. [DOI] [PubMed] [Google Scholar]
- 33.Borgna-Pignatti C, Garani MC, Forni GL, Cappellini MD, Cassinerio E, Fidone C, et al. Hepatocellular carcinoma in thalassaemia: an update of the Italian Registry. Br J Haematol. 2014;167(1):121–126. doi: 10.1111/bjh.13009. [DOI] [PubMed] [Google Scholar]
- 34.Restivo Pantalone G, Renda D, Valenza F, D’Amato F, Vitrano A, Cassara F, et al. Hepatocellular carcinoma in patients with thalassaemia syndromes: clinical characteristics and outcome in a long term single centre experience. Br J Haematol. 2010;150(2):245–247. doi: 10.1111/j.1365-2141.2010.08180.x. [DOI] [PubMed] [Google Scholar]
- 35.Mancuso A, Sciarrino E, Renda MC, Maggio A. A prospective study of hepatocellular carcinoma incidence in thalassemia. Hemoglobin. 2006;30(1):119–124. doi: 10.1080/03630260500455565. [DOI] [PubMed] [Google Scholar]
- 36.Fragatou S, Tsourveloudis I, Manesis G. Incidence of hepatocellular carcinoma in a thalassemia unit. Hemoglobin. 2010;34(3):221–226. doi: 10.3109/03630269.2010.485071. [DOI] [PubMed] [Google Scholar]
- 37.Moukhadder HM, Roumi JE, Bou-Fakhredin R, Taher AT. Hepatocellular Carcinoma in a beta-Thalassemia Intermedia Patient: Yet Another Case in the Expanding Epidemic. Hemoglobin. 2018;42(1):58–60. doi: 10.1080/03630269.2018.1434197. [DOI] [PubMed] [Google Scholar]
- 38.Papadopoulos N, Kountouras D, Malagari K, Tampaki M, Theochari M, Koskinas J. Characteristics and Prognosis of Hepatocellular Carcinoma in Multi-Transfused Patients with beta-Thalassemia. Experience of a Single Tertiary Center. Mediterr J Hematol Infect Dis. 2020;12(1):e2020013. doi: 10.4084/MJHID.2020.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Angelucci E, Pilo F, Coates TD. Transplantation in thalassemia: Revisiting the Pesaro risk factors 25 years later. Am J Hematol. 2017;92(5):411–413. doi: 10.1002/ajh.24674. [DOI] [PubMed] [Google Scholar]
- 40.Ghavamzadeh A, Mirzania M, Kamalian N, Sedighi N, Azimi P. Hepatic iron overload and fibrosis in patients with beta thalassemia major after hematopoietic stem cell transplantation: A pilot study. Int J Hematol Oncol Stem Cell Res. 2015;9(2):55–59. [PMC free article] [PubMed] [Google Scholar]
- 41.Rostami T, Monzavi SM, Poustchi H, Khoshdel AR, Behfar M, Hamidieh AA. Analysis of determinant factors of liver fibrosis progression in ex-thalassemic patients. Int J Hematol. 2021;113(1):145–157. doi: 10.1007/s12185-020-02998-4. [DOI] [PubMed] [Google Scholar]
- 42.Angelucci E, Muretto P, Nicolucci A, Baronciani D, Erer B, Gaziev J, et al. Effects of iron overload and hepatitis C virus positivity in determining progression of liver fibrosis in thalassemia following bone marrow transplantation. Blood. 2002;100(1):17–21. doi: 10.1182/blood.v100.1.17. [DOI] [PubMed] [Google Scholar]
- 43.Angelucci E, Muretto P, Lucarelli G, Ripalti M, Baronciani D, Erer B, et al. Treatment of iron overload in the “ex-thalassemic”. Report from the phlebotomy program. Ann N Y Acad Sci. 1998;850:288–293. doi: 10.1111/j.1749-6632.1998.tb10485.x. [DOI] [PubMed] [Google Scholar]
- 44.Inati A, Kahale M, Sbeiti N, Cappellini MD, Taher AT, Koussa S, et al. One-year results from a prospective randomized trial comparing phlebotomy with deferasirox for the treatment of iron overload in pediatric patients with thalassemia major following curative stem cell transplantation. Pediatr Blood Cancer. 2017;64(1):188–196. doi: 10.1002/pbc.26213. [DOI] [PubMed] [Google Scholar]
- 45.Trottier BJ, Burns LJ, DeFor TE, Cooley S, Majhail NS. Association of iron overload with allogeneic hematopoietic cell transplantation outcomes: a prospective cohort study using R2-MRI-measured liver iron content. Blood. 2013;122(9):1678–1684. doi: 10.1182/blood-2013-04-499772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Armand P, Sainvil MM, Kim HT, Rhodes J, Cutler C, Ho VT, et al. Does iron overload really matter in stem cell transplantation? Am J Hematol. 2012;87(6):569–572. doi: 10.1002/ajh.23188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wermke M, Schmidt A, Middeke JM, Sockel K, von Bonin M, Schonefeldt C, et al. MRI-based liver iron content predicts for nonrelapse mortality in MDS and AML patients undergoing allogeneic stem cell transplantation. Clin Cancer Res. 2012;18(23):6460–6468. doi: 10.1158/1078-0432.CCR-12-1683. [DOI] [PubMed] [Google Scholar]
- 48.Sivgin S, Baldane S, Deniz K, Zararsiz G, Kaynar L, Cetin M, et al. Increased Hepatic Iron Content Predicts Poor Survival in Patients With Iron Overload Who Underwent Allogeneic Hematopoietic Stem Cell Transplantation. Clin Lymphoma Myeloma Leuk. 2016;16(Suppl):S10–S18. doi: 10.1016/j.clml.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 49.Majhail NS, DeFor T, Lazarus HM, Burns LJ. High prevalence of iron overload in adult allogeneic hematopoietic cell transplant survivors. Biol Blood Marrow Transplant. 2008;14(7):790–794. doi: 10.1016/j.bbmt.2008.04.009. [DOI] [PubMed] [Google Scholar]
- 50.Schempp A, Lee J, Kearney S, Mulrooney DA, Smith AR. Iron Overload in Survivors of Childhood Cancer. J Pediatr Hematol Oncol. 2016;38(1):27–31. doi: 10.1097/MPH.0000000000000444. [DOI] [PubMed] [Google Scholar]
- 51.Tomas JF, Pinilla I, Garcia-Buey ML, Garcia A, Figuera A, Gomez-Garcia de Soria VGG, et al. Long-term liver dysfunction after allogeneic bone marrow transplantation: clinical features and course in 61 patients. Bone Marrow Transplant. 2000;26(6):649–655. doi: 10.1038/sj.bmt.1702532. [DOI] [PubMed] [Google Scholar]
- 52.Mantovani LF, Santos FPS, Perini GF, Nascimento CMB, Silva LP, Wroclawski CK, et al. Hepatic and cardiac and iron overload detected by T2* magnetic resonance (MRI) in patients with myelodisplastic syndrome: A cross-sectional study. Leuk Res. 2019;76:53–57. doi: 10.1016/j.leukres.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 53.Schafer AI, Cheron RG, Dluhy R, Cooper B, Gleason RE, Soeldner JS, et al. Clinical consequences of acquired transfusional iron overload in adults. N Engl J Med. 1981;304(6):319–324. doi: 10.1056/NEJM198102053040603. [DOI] [PubMed] [Google Scholar]
- 54.Darbari DS, Kple-Faget P, Kwagyan J, Rana S, Gordeuk VR, Castro O. Circumstances of death in adult sickle cell disease patients. Am J Hematol. 2006;81(11):858–863. doi: 10.1002/ajh.20685. [DOI] [PubMed] [Google Scholar]
- 55.Brown K, Subramony C, May W, Megason G, Liu H, Bishop P, et al. Hepatic iron overload in children with sickle cell anemia on chronic transfusion therapy. J Pediatr Hematol Oncol. 2009;31(5):309–312. doi: 10.1097/MPH.0b013e3181a1c143. [DOI] [PubMed] [Google Scholar]
- 56.Ganz T, Nemeth E. Iron sequestration and anemia of inflammation. Semin Hematol. 2009;46(4):387–393. doi: 10.1053/j.seminhematol.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kernan KF, Carcillo JA. Hyperferritinemia and inflammation. Int Immunol. 2017;29(9):401–409. doi: 10.1093/intimm/dxx031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ferrari P, Kulkarni H, Dheda S, Betti S, Harrison C, St Pierre TG, et al. Serum iron markers are inadequate for guiding iron repletion in chronic kidney disease. Clin J Am Soc Nephrol. 2011;6(1):77–83. doi: 10.2215/CJN.04190510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fishbane S, Miyawaki N, Masani N. Hepatic iron in hemodialysis patients. Kidney Int. 2004;66(4):1714–1715. doi: 10.1111/j.1523-1755.2004.938_7.x. [DOI] [PubMed] [Google Scholar]
- 60.Kliger AS, Foley RN, Goldfarb DS, Goldstein SL, Johansen K, Singh A, et al. KDOQI US commentary on the 2012 KDIGO Clinical Practice Guideline for Anemia in CKD. Am J Kidney Dis. 2013;62(5):849–859. doi: 10.1053/j.ajkd.2013.06.008. [DOI] [PubMed] [Google Scholar]
- 61.Sikorska K, Stalke P, Lakomy EA, Michalska Z, Witczak-Malinowska K, Stolarczyk J. Disturbances of iron metabolism in chronic liver diseases. Med Sci Monit. 2003;9(Suppl 3):64–67. [PubMed] [Google Scholar]
- 62.Mendler MH, Turlin B, Moirand R, Jouanolle AM, Sapey T, Guyader D, et al. Insulin resistance-associated hepatic iron overload. Gastroenterology. 1999;117(5):1155–1163. doi: 10.1016/s0016-5085(99)70401-4. [DOI] [PubMed] [Google Scholar]
- 63.Valenti L, Dongiovanni P, Fracanzani AL, Santorelli G, Fatta E, Bertelli C, et al. Increased susceptibility to nonalcoholic fatty liver disease in heterozygotes for the mutation responsible for hereditary hemochromatosis. Dig Liver Dis. 2003;35(3):172–178. doi: 10.1016/s1590-8658(03)00025-2. [DOI] [PubMed] [Google Scholar]
- 64.Kowdley KV, Belt P, Wilson LA, Yeh MM, Neuschwander-Tetri BA, Chalasani N, et al. Serum ferritin is an independent predictor of histologic severity and advanced fibrosis in patients with nonalcoholic fatty liver disease. Hepatology. 2012;55(1):77–85. doi: 10.1002/hep.24706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hagstrom H, Nasr P, Bottai M, Ekstedt M, Kechagias S, Hultcrantz R, et al. Elevated serum ferritin is associated with increased mortality in non-alcoholic fatty liver disease after 16 years of follow-up. Liver Int. 2016;36(11):1688–1695. doi: 10.1111/liv.13144. [DOI] [PubMed] [Google Scholar]
- 66.Deugnier Y, Bardou-Jacquet E, Laine F. Dysmetabolic iron overload syndrome (DIOS) Presse Med. 2017;46(12 Pt 2):e306–e311. doi: 10.1016/j.lpm.2017.05.036. [DOI] [PubMed] [Google Scholar]
- 67.Dongiovanni P, Fracanzani AL, Fargion S, Valenti L. Iron in fatty liver and in the metabolic syndrome: a promising therapeutic target. J Hepatol. 2011;55(4):920–932. doi: 10.1016/j.jhep.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 68.Eder SK, Feldman A, Strebinger G, Kemnitz J, Zandanell S, Niederseer D, et al. Mesenchymal iron deposition is associated with adverse long-term outcome in non-alcoholic fatty liver disease. Liver Int. 2020;40(8):1872–1882. doi: 10.1111/liv.14503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Buzzetti E, Petta S, Manuguerra R, Luong TV, Cabibi D, Corradini E, et al. Evaluating the association of serum ferritin and hepatic iron with disease severity in non-alcoholic fatty liver disease. Liver Int. 2019;39(7):1325–1334. doi: 10.1111/liv.14096. [DOI] [PubMed] [Google Scholar]
- 70.Valenti L, Fracanzani AL, Bugianesi E, Dongiovanni P, Galmozzi E, Vanni E, et al. HFE genotype, parenchymal iron accumulation, and liver fibrosis in patients with nonalcoholic fatty liver disease. Gastroenterology. 2010;138(3):905–912. doi: 10.1053/j.gastro.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 71.Hoki T, Miyanishi K, Tanaka S, Takada K, Kawano Y, Sakurada A, et al. Increased duodenal iron absorption through up-regulation of divalent metal transporter 1 from enhancement of iron regulatory protein 1 activity in patients with nonalcoholic steatohepatitis. Hepatology. 2015;62(3):751–761. doi: 10.1002/hep.27774. [DOI] [PubMed] [Google Scholar]
- 72.Marmur J, Beshara S, Eggertsen G, Onelov L, Albiin N, Danielsson O, et al. Hepcidin levels correlate to liver iron content, but not steatohepatitis, in non-alcoholic fatty liver disease. BMC Gastroenterol. 2018;18(1):78. doi: 10.1186/s12876-018-0804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ruivard M, Laine F, Deugnier Y. Iron absorption in nonalcoholic steatohepatitis and dysmetabolic iron overload syndrome. Hepatology. 2016;63(5):1737–1738. doi: 10.1002/hep.28296. [DOI] [PubMed] [Google Scholar]
- 74.Rametta R, Dongiovanni P, Pelusi S, Francione P, Iuculano F, Borroni V, et al. Hepcidin resistance in dysmetabolic iron overload. Liver Int. 2016;36(10):1540–1548. doi: 10.1111/liv.13124. [DOI] [PubMed] [Google Scholar]
- 75.Corradini E, Buzzetti E, Dongiovanni P, Scarlini S, Caleffi A, Pelusi S, et al. Ceruloplasmin gene variants are associated with hyperferritinemia and increased liver iron in patients with NAFLD. J Hepatol. 2021;75(3):506–513. doi: 10.1016/j.jhep.2021.03.014. [DOI] [PubMed] [Google Scholar]
- 76.Hernaez R, Yeung E, Clark JM, Kowdley KV, Brancati FL, Kao WH. Hemochromatosis gene and nonalcoholic fatty liver disease: a systematic review and meta-analysis. J Hepatol. 2011;55(5):1079–1085. doi: 10.1016/j.jhep.2011.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Castiella A, Urreta I, Zapata E, de Juan M, Alustiza JM, Emparanza JI, et al. Dysmetabolic iron overload syndrome and its relationship with HFE gene mutations and with liver steatosis. Dig Liver Dis. 2020;52(6):683–685. doi: 10.1016/j.dld.2020.04.001. [DOI] [PubMed] [Google Scholar]
- 78.Yu YC, Luu HN, Wang R, Thomas CE, Glynn NW, Youk AO, et al. Serum Biomarkers of Iron Status and Risk of Hepatocellular Carcinoma Development in Patients with Nonalcoholic Fatty Liver Disease. Cancer Epidemiol Biomarkers Prev. 2022;31(1):230–235. doi: 10.1158/1055-9965.EPI-21-0754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sorrentino P, D’Angelo S, Ferbo U, Micheli P, Bracigliano A, Vecchione R. Liver iron excess in patients with hepatocellular carcinoma developed on non-alcoholic steato-hepatitis. J Hepatol. 2009;50(2):351–357. doi: 10.1016/j.jhep.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 80.Piperno A, D’Alba R, Fargion S, Roffi L, Sampietro M, Parma S, et al. Liver iron concentration in chronic viral hepatitis: a study of 98 patients. Eur J Gastroenterol Hepatol. 1995;7(12):1203–1208. doi: 10.1097/00042737-199512000-00014. [DOI] [PubMed] [Google Scholar]
- 81.Guyader D, Thirouard AS, Erdtmann L, Rakba N, Jacquelinet S, Danielou H, et al. Liver iron is a surrogate marker of severe fibrosis in chronic hepatitis C. J Hepatol. 2007;46(4):587–595. doi: 10.1016/j.jhep.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 82.Martin-Gonzalez C, Pelazas-Gonzalez R, Fernandez-Rodriguez C, Aleman-Valls R, Martinez-Riera A, Ortega-Toledo P, et al. Ferritin and liver fibrosis among patients with chronic hepatitis C virus infection. J Trace Elem Med Biol. 2020;61:126542. doi: 10.1016/j.jtemb.2020.126542. [DOI] [PubMed] [Google Scholar]
- 83.Girelli D, Pasino M, Goodnough JB, Nemeth E, Guido M, Castagna A, et al. Reduced serum hepcidin levels in patients with chronic hepatitis C. J Hepatol. 2009;51(5):845–852. doi: 10.1016/j.jhep.2009.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Inomata S, Anan A, Yamauchi E, Yamauchi R, Kunimoto H, Takata K, et al. Changes in the Serum Hepcidin-to-ferritin Ratio with Erythroferrone after Hepatitis C Virus Eradication Using Direct-acting Antiviral Agents. Intern Med. 2019;58(20):2915–2922. doi: 10.2169/internalmedicine.2909-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sato M, Miyanishi K, Tanaka S, Sakurada A, Sakamoto H, Kawano Y, et al. Increased Duodenal Iron Absorption through Upregulation of Ferroportin 1 due to the Decrement in Serum Hepcidin in Patients with Chronic Hepatitis C. Can J Gastroenterol Hepatol. 2018;2018:2154361. doi: 10.1155/2018/2154361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fujita N, Sugimoto R, Urawa N, Araki J, Mifuji R, Yamamoto M, et al. Hepatic iron accumulation is associated with disease progression and resistance to interferon/ribavirin combination therapy in chronic hepatitis C. J Gastroenterol Hepatol. 2007;22(11):1886–1893. doi: 10.1111/j.1440-1746.2006.04759.x. [DOI] [PubMed] [Google Scholar]
- 87.Ryder SD, Irving WL, Jones DA, Neal KR, Underwood JC, Trent Hepatitis CSG. Progression of hepatic fibrosis in patients with hepatitis C: a prospective repeat liver biopsy study. Gut. 2004;53(3):451–455. doi: 10.1136/gut.2003.021691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Yano M, Hayashi H, Wakusawa S, Sanae F, Takikawa T, Shiono Y, et al. Long term effects of phlebotomy on biochemical and histological parameters of chronic hepatitis C. Am J Gastroenterol. 2002;97(1):133–137. doi: 10.1111/j.1572-0241.2002.05436.x. [DOI] [PubMed] [Google Scholar]
- 89.Desai TK, Jamil LH, Balasubramaniam M, Koff R, Bonkovsky HL. Phlebotomy improves therapeutic response to interferon in patients with chronic hepatitis C: a meta-analysis of six prospective randomized controlled trials. Dig Dis Sci. 2008;53(3):815–822. doi: 10.1007/s10620-007-9945-7. [DOI] [PubMed] [Google Scholar]
- 90.Sartori M, Andorno S, Rossini A, Boldorini R, Bozzola C, Carmagnola S, et al. Phlebotomy improves histology in chronic hepatitis C males with mild iron overload. World J Gastroenterol. 2010;16(5):596–602. doi: 10.3748/wjg.v16.i5.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sebastiani G, Tempesta D, Alberti A. Hepatic iron overload is common in chronic hepatitis B and is more severe in patients coinfected with hepatitis D virus. J Viral Hepat. 2012;19(2):e170–176. doi: 10.1111/j.1365-2893.2011.01508.x. [DOI] [PubMed] [Google Scholar]
- 92.Hou SW, Wang ZF, Guan SH, Yang K, Wang Q, Chen LW, et al. Alterations in the Iron Homeostasis Network of Hepatocytes Caused by Hepatitis B Virus. Clin Lab. 2019;65(4) doi: 10.7754/Clin.Lab.2018.180914. [DOI] [PubMed] [Google Scholar]
- 93.Yonal O, Akyuz F, Demir K, Ciftci S, Keskin F, Pinarbasi B, et al. Decreased prohepcidin levels in patients with HBV-related liver disease: relation with ferritin levels. Dig Dis Sci. 2010;55(12):3548–3551. doi: 10.1007/s10620-010-1183-8. [DOI] [PubMed] [Google Scholar]
- 94.Zou DM, Rong DD, Zhao H, Su L, Sun WL. Improvement of chronic hepatitis B by iron chelation therapy in a patient with iron overload: A case report. Medicine (Baltimore) 2017;96(52):e9566. doi: 10.1097/MD.0000000000009566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tey TT, Yiu R, Leow WQ. Hepatitis B-Associated Symptomatic Iron Overload, with Complete Resolution after Nucleoside Analogue Treatment. Case Rep Gastrointest Med. 2021;2021:8407257. doi: 10.1155/2021/8407257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Jakobovits AW, Morgan MY, Sherlock S. Hepatic siderosis in alcoholics. Dig Dis Sci. 1979;24(4):305–310. doi: 10.1007/BF01296545. [DOI] [PubMed] [Google Scholar]
- 97.Dostalikova-Cimburova M, Balusikova K, Kratka K, Chmelikova J, Hejda V, Hnanicek J, et al. Role of duodenal iron transporters and hepcidin in patients with alcoholic liver disease. J Cell Mol Med. 2014;18(9):1840–1850. doi: 10.1111/jcmm.12310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Costa Matos L, Batista P, Monteiro N, Ribeiro J, Cipriano MA, Henriques P, et al. Iron stores assessment in alcoholic liver disease. Scand J Gastroenterol. 2013;48(6):712–718. doi: 10.3109/00365521.2013.781217. [DOI] [PubMed] [Google Scholar]
- 99.Robinson G, Narasimhan S, Weatherall M, Beasley R. Hemochromatosis gene mutations, liver function tests and iron status in alcohol-dependent patients admitted for detoxification. J Gastroenterol Hepatol. 2007;22(6):852–854. doi: 10.1111/j.1440-1746.2006.04519.x. [DOI] [PubMed] [Google Scholar]
- 100.Gleeson D, Evans S, Bradley M, Jones J, Peck RJ, Dube A, et al. HFE genotypes in decompensated alcoholic liver disease: phenotypic expression and comparison with heavy drinking and with normal controls. Am J Gastroenterol. 2006;101(2):304–310. doi: 10.1111/j.1572-0241.2006.00439.x. [DOI] [PubMed] [Google Scholar]
- 101.Grove J, Daly AK, Burt AD, Guzail M, James OF, Bassendine MF, et al. Heterozygotes for HFE mutations have no increased risk of advanced alcoholic liver disease. Gut. 1998;43(2):262–266. doi: 10.1136/gut.43.2.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ganne-Carrie N, Christidis C, Chastang C, Ziol M, Chapel F, Imbert-Bismut F, et al. Liver iron is predictive of death in alcoholic cirrhosis: a multivariate study of 229 consecutive patients with alcoholic and/or hepatitis C virus cirrhosis: a prospective follow up study. Gut. 2000;46(2):277–282. doi: 10.1136/gut.46.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nahon P, Sutton A, Rufat P, Ziol M, Thabut G, Schischmanoff PO, et al. Liver iron, HFE gene mutations, and hepatocellular carcinoma occurrence in patients with cirrhosis. Gastroenterology. 2008;134(1):102–110. doi: 10.1053/j.gastro.2007.10.038. [DOI] [PubMed] [Google Scholar]
- 104.Mueller S, Rausch V. The role of iron in alcohol-mediated hepatocarcinogenesis. Adv Exp Med Biol. 2015;815:89–112. doi: 10.1007/978-3-319-09614-8_6. [DOI] [PubMed] [Google Scholar]
- 105.Ludwig J, Hashimoto E, Porayko MK, Moyer TP, Baldus WP. Hemosiderosis in cirrhosis: a study of 447 native livers. Gastroenterology. 1997;112(3):882–888. doi: 10.1053/gast.1997.v112.pm9041250. [DOI] [PubMed] [Google Scholar]
- 106.Fierro-Fine A, Guerin L, Hicsasmaz H, Brown KE. Clinical Factors Associated with Hepatocellular Iron Deposition in End-stage Liver Disease. J Clin Transl Hepatol. 2020;8(3):231–239. doi: 10.14218/JCTH.2020.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Stuart KA, Fletcher LM, Clouston AD, Lynch SV, Purdie DM, Kerlin P, et al. Increased hepatic iron and cirrhosis: no evidence for an adverse effect on patient outcome following liver transplantation. Hepatology. 2000;32(6):1200–1207. doi: 10.1053/jhep.2000.20348. [DOI] [PubMed] [Google Scholar]
- 108.Kayali Z, Ranguelov R, Mitros F, Shufelt C, Elmi F, Rayhill SC, et al. Hemosiderosis is associated with accelerated decompensation and decreased survival in patients with cirrhosis. Liver Int. 2005;25(1):41–48. doi: 10.1111/j.1478-3231.2005.01022.x. [DOI] [PubMed] [Google Scholar]
- 109.Asare GA, Mossanda KS, Kew MC, Paterson AC, Kahler-Venter CP, Siziba K. Hepatocellular carcinoma caused by iron overload: a possible mechanism of direct hepatocarcinogenicity. Toxicology. 2006;219(1-3):41–52. doi: 10.1016/j.tox.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 110.Ko C, Siddaiah N, Berger J, Gish R, Brandhagen D, Sterling RK, et al. Prevalence of hepatic iron overload and association with hepatocellular cancer in end-stage liver disease: results from the National Hemochromatosis Transplant Registry. Liver Int. 2007;27(10):1394–1401. doi: 10.1111/j.1478-3231.2007.01596.x. [DOI] [PubMed] [Google Scholar]
- 111.Miyamoto Y, Nakano S, Ihira H, Yamaji T, Katagiri R, Sawada N, et al. Association of plasma iron status with subsequent risk of total and site-specific cancer: A large case-cohort study within JPHC Study. Cancer Prev Res (Phila) 2022;15(10):669–678. doi: 10.1158/1940-6207.CAPR-22-0151. [DOI] [PubMed] [Google Scholar]
- 112.Abu Rajab M, Guerin L, Lee P, Brown KE. Iron overload secondary to cirrhosis: a mimic of hereditary haemochromatosis? Histopathology. 2014;65(4):561–569. doi: 10.1111/his.12417. [DOI] [PubMed] [Google Scholar]
- 113.O’Glasser AY, Scott DL, Corless CL, Zaman A, Sasaki A, Gopal DV, et al. Hepatic and cardiac iron overload among patients with end-stage liver disease referred for liver transplantation. Clin Transplant. 2010;24(5):643–651. doi: 10.1111/j.1399-0012.2009.01136.x. [DOI] [PubMed] [Google Scholar]
- 114.Rhee JW, Zhang S, Gallo A, Ahmed A, Kawana M. Severe Cardiovascular Complications Following Liver Transplantation in Patients With Iron Overload. JACC Case Rep. 2022;4(11):677–681. doi: 10.1016/j.jaccas.2021.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Beaton MD, Chakrabarti S, Adams PC. Inflammation is not the cause of an elevated serum ferritin in non-alcoholic fatty liver disease. Ann Hepatol. 2014;13(3):353–356. [PubMed] [Google Scholar]
- 116.Valenti L, Fracanzani AL, Dongiovanni P, Rovida S, Rametta R, Fatta E, et al. A randomized trial of iron depletion in patients with nonalcoholic fatty liver disease and hyperferritinemia. World J Gastroenterol. 2014;20(11):3002–3010. doi: 10.3748/wjg.v20.i11.3002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Adams LA, Crawford DH, Stuart K, House MJ, St Pierre TG, Webb M, et al. The impact of phlebotomy in nonalcoholic fatty liver disease: A prospective, randomized, controlled trial. Hepatology. 2015;61(5):1555–1564. doi: 10.1002/hep.27662. [DOI] [PubMed] [Google Scholar]
- 118.Laine F, Ruivard M, Loustaud-Ratti V, Bonnet F, Cales P, Bardou-Jacquet E, et al. Metabolic and hepatic effects of bloodletting in dysmetabolic iron overload syndrome: A randomized controlled study in 274 patients. Hepatology. 2017;65(2):465–474. doi: 10.1002/hep.28856. [DOI] [PubMed] [Google Scholar]
- 119.Cappellini MD, Cohen A, Piga A, Bejaoui M, Perrotta S, Agaoglu L, et al. A phase 3 study of deferasirox (ICL670), a once-daily oral iron chelator, in patients with beta-thalassemia. Blood. 2006;107(9):3455–3462. doi: 10.1182/blood-2005-08-3430. [DOI] [PubMed] [Google Scholar]
- 120.Porter JB, Elalfy MS, Taher AT, Aydinok Y, Chan LL, Lee SH, et al. Efficacy and safety of deferasirox at low and high iron burdens: results from the EPIC magnetic resonance imaging substudy. Ann Hematol. 2013;92(2):211–219. doi: 10.1007/s00277-012-1588-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Pennell DJ, Berdoukas V, Karagiorga M, Ladis V, Piga A, Aessopos A, et al. Randomized controlled trial of deferiprone or deferoxamine in beta-thalassemia major patients with asymptomatic myocardial siderosis. Blood. 2006;107(9):3738–3744. doi: 10.1182/blood-2005-07-2948. [DOI] [PubMed] [Google Scholar]
- 122.Wu SF, Peng CT, Wu KH, Tsai CH. Liver fibrosis and iron levels during long-term deferiprone treatment of thalassemia major patients. Hemoglobin. 2006;30(2):215–218. doi: 10.1080/03630260600642534. [DOI] [PubMed] [Google Scholar]
- 123.Maira D, Cassinerio E, Marcon A, Mancarella M, Fraquelli M, Pedrotti P, et al. Progression of liver fibrosis can be controlled by adequate chelation in transfusion-dependent thalassemia (TDT) Ann Hematol. 2017;96(11):1931–1936. doi: 10.1007/s00277-017-3120-9. [DOI] [PubMed] [Google Scholar]
- 124.Taher AT, Porter J, Viprakasit V, Kattamis A, Chuncharunee S, Sutcharitchan P, et al. Deferasirox reduces iron overload significantly in nontransfusion-dependent thalassemia: 1-year results from a prospective, randomized, double-blind, placebo-controlled study. Blood. 2012;120(5):970–977. doi: 10.1182/blood-2012-02-412692. [DOI] [PubMed] [Google Scholar]
- 125.Cheong JW, Kim HJ, Lee KH, Yoon SS, Lee JH, Park HS, et al. Deferasirox improves hematologic and hepatic function with effective reduction of serum ferritin and liver iron concentration in transfusional iron overload patients with myelodysplastic syndrome or aplastic anemia. Transfusion. 2014;54(6):1542–1551. doi: 10.1111/trf.12507. [DOI] [PubMed] [Google Scholar]