Abstract
Background and Aims
The recently proposed concept of metabolic dysfunction-associated fatty liver disease (MAFLD) has remained controversial. We aimed to describe the features and associated outcomes to examine the diagnostic ability of MAFLD for identifying high-risk individuals.
Methods
In this retrospective cohort study, we enrolled 72,392 Chinese participants between 2014 and 2015. Participants were classified as MAFLD, nonalcoholic fatty liver disease (NAFLD), non-MAFLD-NAFLD, and a normal control group. The primary outcomes were liver-related and cardiovascular disease (CVD) events. Person-years of follow-up were calculated from enrolment to the diagnosis of the event, or the last date of data (June, 2020).
Results
Of the 72,392 participants, 31.54% (22,835) and 28.33% (20,507) qualified the criteria for NAFLD or MAFLD, respectively. Compared with NAFLD, MAFLD patients were more likely to be male, overweight, and have higher biochemical indices including liver enzyme levels. Lean MAFLD diagnosed with ≥2 or ≥3 metabolic abnormalities presented similar clinical manifestations. During the median follow-up of 5.22 years, 919 incident cases of severe liver disease and 2,073 CVD cases were recorded. Compared with the normal control group, the NAFLD and MAFLD groups had a higher cumulative risk of liver failure and cardiac-cerebral vascular diseases. There were no significant differences in risk between the non-MAFLD-NAFLD and normal group. Diabetes-MAFLD group had the highest incidence of liver-related and cardiac-cerebral vascular diseases, lean MAFLD came second, and obese-MAFLD had the lowest incidence.
Conclusions
This real-world study provided evidence for rationally assessing the benefit and practicability of the change in terminology from NAFLD to MAFLD. MAFLD may be better than NAFLD in identifying fatty liver with worse clinical features and risk profile.
Keywords: Metabolic-associated fatty liver disease, Non-alcoholic fatty liver disease, Liver-related disease, Cardiac vascular disease, Cerebral vascular disease
Graphical abstract
Introduction
Over the past decades, nonalcoholic fatty liver disease (NAFLD) has emerged as the most common chronic liver disease in the world, affecting nearly 1 billion people globally.1–3 NAFLD is a multisystem disorder and the clinical burden of the disease is not limited to liver-related complications, but also involves extrahepatic diseases.4,5 In 2020, an international expert consensus panel proposed a novel concept of Metabolic dysfunction-associated fatty liver disease (MAFLD) to describe liver disease associated with known metabolic dysfunction.6 The new concept is defined by a set of positive diagnostic criteria for fatty liver disease (FLD) associated with metabolic dysfunction, rather than by exclusion criteria. The increasing prevalence of MAFLD coexists with other chronic liver diseases, and has the critical importance of proposing a diagnosis based on inclusion criteria. Younossi et al.7,8 reckoned that the term is ambiguous, as it is never accurate to assign a single name to a disease as heterogeneous as NAFLD. Hence, there is no clear consensus on the change in definition from NAFLD to MAFLD.
While cross-sectional studies point to the difference in the features of MAFLD and NAFLD,9,10 it is not clear whether the MAFLD definition is more practical for identifying patients with worse clinical features. Inconsistencies in cross-sectional studies may have many reasons, including limitation of study design, small sample size, and reverse causation. A cohort study, which is prospectively designed from cause to outcome, can examine the causal association between FLD groups and the long-term outcome. Therefore, risk assessment of long-term outcomes based on cohort study data may provide real-world evidence to provide the reasoning for the change in definition. To fill this gap in the literature, we conducted a large retrospective cohort study of 72,392 Chinese adults to evaluate the rationality of the MAFLD definitions by assessing the risk of liver-related and cardiac-cerebral vascular diseases.
Methods
Study participants
This was a single-center, retrospective cohort study conducted in China. We enrolled 121,020 health check examinees who visited the Health Promotion Center of the First Affiliated Hospital of Nanjing Medical University in Jiangsu between January 2014 and December 2015. All patients underwent abdominal ultrasonography as part of their routine health examination. Of those, 31,886 were excluded because of duplicate records, lack of data for the diagnosis of MAFLD (n=11,893), lack of data for alcohol consumption (n=3,310), having a history of hepatocellular carcinoma (HCC), cirrhosis, liver failure, cardiovascular or cerebrovascular disease (n=1,539). The study cohort thus comprised 72,392 participants (Supplementary Fig. 1). The First Affiliated Hospital with Nanjing Medical University Ethics Review Board approved the study protocol and informed consent was obtained from all subjects.
Group definitions
According to the guidelines for the prevention and treatment for NAFLD (2018 update), abdominal ultrasonography was performed for hepatic steatosis.11 The severity of hepatic steatosis (negative, mild, moderate, and severe) was assessed based on the imaging findings retrieved from medical records. The MAFLD group included participants with fatty liver with the following three conditions: overweight or obese, a body mass index (BMI) ≥23 kg/m2 in Asians, type 2 diabetes mellitus (T2DM), or two or more of the following metabolic conditions:6 (1) waist circumference ≥90 cm in men and ≥80 cm in women (central obesity); (2) blood pressure ≥130/85 mmHg or receiving antihypertension medication; (3) plasma triglycerides ≥1.7 mmol/L or receiving lipid-lowering drugs; (4) plasma high-density lipoprotein-cholesterol (HDL-C) < 1.0 mmol/L in men and <1.3 mmol/L in women, or receiving specific drug treatment; (5) prediabetes, a fasting plasma glucose (FPG) of 5.6–6.9 mmol/L or a hemoglobin A1c (HbA1c) of 5.7–6.4%; (6) a homeostasis model assessment of insulin resistance (HOMA-IR) score ≥2.5; and (7) plasma high-sensitivity C-reactive protein level >2 mg/L. Participants with a BMI <23.0 kg/m2 who had ≥2 or ≥3 metabolic abnormalities were recorded as thinner with ≥2 metabolic abnormalities (1,242 participants) or thinner with ≥3 metabolic abnormalities (457 participants).
The definition of NAFLD was based on ultrasound evidence of fatty liver and the exclusion of both secondary causes such as viral hepatitis or drug-induced hepatitis, and excessive alcohol consumption (≥30 g/d for men and ≥20 g/d for women) based on the detailed medical history including medications, alcohol consumption, and laboratory data. The non-MAFLD-NAFLD group included those who satisfied the diagnostic criteria for NAFLD but not the definition of MAFLD. The group was characterized by fatty liver without competing causes of steatosis (e.g., alcohol, viral hepatitis, or other causes), obesity, metabolic dysfunction, and diabetes. Similarly, the non-NAFLD-MAFLD group included those who met the diagnostic criteria for MAFLD but not those of NAFLD. The non-NAFLD-MAFLD group included fatty liver patients with obesity, metabolic dysfunction, or diabetes regardless of having other competing causes of steatosis. The MAFLD with NAFLD group included those who met the diagnostic criteria for both MAFLD and NAFLD, and the non-NAFLD with non-MAFLD group included those not satisfying the diagnostic criteria of either MAFLD or NAFLD.
Demographic and clinical characteristics
Demographic and clinical variables were obtained from the health examination database, including age, sex, alcohol consumption, weight, height, waist circumference, severity of hepatic steatosis estimated by ultrasound (mild, moderate, or severe hepatic steatosis), history of diabetes and hypertension, hepatitis B virus (HBV) and hepatitis C virus (HCV) infection, laboratory indices (related metabolic indices, liver biochemistry, and tumor markers), and BMI (kg/m2). Venous blood samples for laboratory testing were collected after overnight fasting of at least 8 h. The metabolic indices included blood urea nitrogen (BUN), creatinine, albumin, HbA1c, FPG, total cholesterol (TC), triglyceride (TG), low-density lipoprotein-cholesterol (LDL-C), and HDL-C. Liver biochemistry included total bilirubin (TBIL), alanine aminotransferase (ALT), aspartate aminotransferase (AST), γ-glutamyl transferase (GGT), alkaline phosphatase (ALP), and lactic dehydrogenase (LDH). Tumor markers included alpha fetoprotein (AFP) and carcinoembryonic antigen (CEA). Two noninvasive liver fibrosis scores with published formulae and cutoffs were calculated to evaluate liver fibrosis, AST-to-platelet ratio index (APRI) and fibrosis-4 index (FIB-4). The APRI index was calculated as (AST level/upper limit of normal) / platelet count (109/L) × 100. The higher cutoff value (1.50) was identified as the criteria for significant fibrosis.12 The FIB-4 index was derived by age (years), serum levels of AST (U/L), ALT (U/L), and platelet count (109/L) as previously described.13 The low cut-off value (1.30) was found to have good diagnostic accuracy for discriminating advanced fibrosis.
Outcomes
For each participant, hospitalization information was obtained by telephone interviews conducted yearly. We collected the diagnoses and International Classification of Diseases–Tenth Revision (ICD-10) codes from electronic medical records (EMR). The primary outcomes were liver-related and cardiac-cerebral vascular event, including cirrhosis (ICD-10 K70.2-K70.3, K74.1-K74.6), HCC; ICD-10 C22.1, C24.0, and C24.8-C24.9), liver failure (hepatic failure; ICD-10 K72.0, K72.1, and K72.9), coronary heart disease (ICD-10 I24.0-I24.1, I25.0-I25.1), stroke (ICD-10 I63, I69.3-I69.4, and G46.3-G46.4), heart failure (ICD-10 I11.0, I11.9, I13.0, I13.2, and I50), and cardiomyopathy (ICD-10 I40-I43). Person-years of follow-up were calculated as the time from enrolment to the diagnosis of the event, or the date at death, or the last date of data collection (June, 2020), whichever came first. Median follow-up was calculated using the more robust reverse Kaplan–Meier method.
Statistical analysis
Continuous variables were reported as means ± standard deviation (SD) and between-group differences were assessed using the Student’s t-test, Welch’s t-test, or the Wilcoxon rank-sum (Mann-Whitney U) test. Multigroup comparisons were performed using one-way analysis of variance or the linear mixed-effects model depending on whether the assumption of variance equality for analysis of variance was confirmed, followed by post-hoc Bonferroni’s correction. Multiple comparisons and the unequal sample size between groups increase the probability of type I error. Categorical variables were reported as frequency and percentage, and between-group differences were assessed using chi-squared or Fisher’s exact tests. Comparisons of categorical variables between multiple groups were followed by Bonferroni’s correction. Survival analysis was performed using Cox proportional hazards models or the accelerated failure time (AFT) model. Multivariable analysis was used to estimate the association between the FLD groups and outcomes, adjusting for age at baseline (continuous) and sex (female or male). As previously described, the multivariable model was adjusted by sociodemographic indices including age, sex, race, income, and marital status.14,15 However, owing to the lack of availability of data for other sociodemographic features, only age and sex were adjusted for in the model.
We performed stratified analysis by sex and HBV infection status. The statistical analysis was performed with Stata version 15.0 (Stata Corp, TX, United States) and R version 4.0.3. Two-sided p-values <0.05 were considered statistically significant. For comparisons among four groups in Table 1 and among five groups in Supplementary Table 1, all p-values shown are the Bonferroni-corrected with six and ten multiple tests in consideration of convenience. Statistical tests were performed for six or ten comparisons, with a type I error threshold of p′<0.0083 and 0.005 (α=0.05 with Bonferroni’s correction for multiple comparisons).
Table 1. Comparison of clinical parameters according to presence of MAFLD, NAFLD, and non-MAFLD-NAFLD.
| Variables | Normal (n=48 790) | NAFLD (n=22 835) | MAFLD (n=20 507) | non-MAFLD-NAFLD (n=2 574) | Pa for MAFLD vs. NAFLD | Pa for MAFLD vs. non-MAFLD-NAFLD | Pa for non-MAFLD-NAFLD vs. normal |
|---|---|---|---|---|---|---|---|
| Age, years | 43.04±15.54 | 48.60±14.42 | 48.83±14.39 | 46.70±14.31 | 0.520 | <0.001*** | <0.001*** |
| Male, % | 25 389 (52.04) | 15 975 (69.96) | 14 801 (72.18) | 1 383 (53.73) | <0.001*** | <0.001*** | 0.563 |
| Severity of fatty liver | |||||||
| Mild, % | 0 (0) | 13 316 (58.31) | 11 506 (56.11) | 1 959 (76.11) | |||
| Moderate, % | 0 (0) | 9 293 (40.70) | 8 790 (42.86) | 599 (23.27) | |||
| Severe, % | 0 (0) | 226 (0.99) | 211 (1.03) | 16 (0.62) | |||
| BMI, Kg/m2 | 22.49±10.73 | 26.03±2.96 | 26.38±2.79 | 21.75±1.13 | <0.001*** | <0.001*** | <0.001*** |
| Excess Alcohol Use, % | 110 (0.23) | 0 (0) | 84 (0.41) | 0 (0) | <0.001*** | <0.001*** | 0.042* |
| Diabetes, % | 1 953 (4.17) | 2 726 (12.12) | 2 763 (13.67) | 0 (0) | <0.001*** | <0.001*** | <0.001*** |
| Hypertension, % | 10 139 (20.78) | 10 171 (44.54) | 9 941 (48.48) | 350 (13.60) | <0.001*** | <0.001*** | <0.001*** |
| Platelets, 109/L | 222.39±54.91 | 226.39±56.24 | 225.53±56.57 | 231.52±53.54 | 0.692 | <0.001*** | <0.001*** |
| BUN, mmoL | 4.87±1.79 | 5.09±1.23 | 5.11±1.24 | 4.90±1.17 | 0.292 | <0.001*** | 1.000 |
| Creatinine, µmolL | 69.24±19.78 | 72.73±16.76 | 73.29±16.88 | 68.36±14.65 | 0.003* | <0.001*** | 0.025* |
| TBIL, µmolL | 13.30±5.47 | 13.07±5.21 | 13.10±5.19 | 12.93±5.48 | 1.000 | 1.000 | 0.030* |
| ALT, U/L | 20.62±19.30 | 33.47±24.68 | 34.45±25.27 | 26.59±19.63 | <0.001*** | <0.001*** | <0.001*** |
| AST, U/L | 22.15±11.43 | 26.27±15.82 | 26.60±16.13 | 24.05±12.97 | 0.230 | <0.001*** | <0.001*** |
| GGT, U/L | 26.44±34.74 | 43.15±39.53 | 44.52±40.30 | 33.69±33.28 | 0.008** | <0.001*** | <0.001*** |
| ALP, U/L | 74.58±22.36 | 81.55±22.07 | 81.86±22.06 | 78.56±21.80 | 1.000 | <0.001*** | <0.001*** |
| LDH, U/L | 181.79±34.03 | 190.83±36.43 | 191.42±36.73 | 185.86±32.88 | 0.894 | <0.001*** | <0.001*** |
| Albumin, g/L | 45.51±2.85 | 45.69±2.75 | 45.72±2.75 | 45.50±2.79 | 1.000 | 0.011* | 1.000 |
| HbA1c, % | 5.53±0.62 | 5.83±0.87 | 5.87±0.89 | 5.47±0.36 | 0.554 | <0.001*** | 0.031* |
| FPG, mmol/L | 5.18±0.90 | 5.66±1.37 | 5.72±1.43 | 5.16±0.50 | <0.001*** | <0.001*** | 0.254 |
| TC, mmol/L | 5.00±0.95 | 5.34±1.02 | 5.35±1.02 | 5.29±1.00 | 1.000 | 0.026* | <0.001*** |
| TG, mmol/L | 1.23±0.84 | 2.13±1.70 | 2.19±1.74 | 1.56±1.18 | <0.001*** | <0.001*** | <0.001*** |
| LDL-C, mmol/L | 3.15±0.75 | 3.48±0.77 | 3.49±0.77 | 3.42±0.78 | 1.000 | <0.001*** | <0.001*** |
| HDL-C, mmol/L | 1.41±0.32 | 1.22±0.26 | 1.20±0.26 | 1.34±0.29 | <0.001*** | <0.001*** | <0.001*** |
| APRI score, mean ± SD | 0.27±0.23 | 0.31±0.23 | 0.32±0.24 | 0.28±0.18 | 0.137 | <0.001*** | 0.395 |
| APRI score >1.5, n (%) | 81 (0.20) | 58 (0.29) | 56 (0.31) | 4 (0.17) | 1.000 | 1.000 | 1.000 |
| FIB-4 score, mean ± SD | 1.13±1.09 | 1.15±0.68 | 1.16±0.68 | 1.11±0.70 | 1.000 | 0.030* | 1.000 |
| FIB-4 score >1.3, n (%) | 11 531 (28.05) | 6 335 (31.16) | 5 777 (31.67) | 643 (27.75) | 1.000 | <0.001*** | 1.000 |
| AFP | 3.10±6.19 | 3.13±2.22 | 3.13±2.26 | 3.12±1.82 | 1.000 | 1.000 | 1.000 |
| CEA | 2.05±5.51 | 2.21±3.33 | 2.23±2.94 | 2.05±5.43 | 1.000 | 0.611 | 1.000 |
ap value was the Bonferroni-corrected with six multiple comparisons. *p<0.05, **p<0.01 and ***p<0.001. AFP, alpha fetoprotein; ALP, alkaline phosphatase; ALT, alanine aminotransferase; APRI, alanine aminotransferase -to-platelet ratio index; AST, aspartate aminotransferase; BMI, body mass index; BUN, blood urea nitrogen; CEA, carcinoembryonic antigen; FIB-4, Fibrosis-4 index; FPG, fasting plasma glucose; GGT, γ-glutamyl transferase; HbA1c, glycated haemoglobin; HDL-C, high-density lipoprotein-cholesterol; LDH, lactic dehydrogenase; LDL-C, low-density lipoprotein-cholesterol; MAFLD, metabolic associated fatty liver disease; NAFLD, non-alcoholic fatty liver disease; TBIL, total bilirubin; TC, total cholesterol; TG, triglyceride.
Results
Baseline characteristics
Of the 72,392 eligible participants, 22,835 (31.54%) satisfied the NAFLD criteria. The prevalence of FLD was lower when defined by MAFLD (28.33%, Table 1), and 2,574 participants previously classified as NAFLD did not meet the MAFLD criteria (non-MAFLD-NAFLD), 246 (0.34%) classified as MAFLD did not satisfy the NAFLD criteria (non-NAFLD-MAFLD), and 20,261 (27.99%) who met the criteria for both NAFLD and MAFLD (Supplementary Table 1). Compared with the NAFLD group, the MAFLD group was more likely to be male, overweight, and have severe hepatic steatosis and higher biochemical indices, including serum levels of ALT, GGT, FGP, TG, and HDL-C (Table 1). Besides, only 84 patients in the MAFLD group had alcohol-associated liver disease. Although not satisfying the conditions for NAFLD, the non-NAFLD-MAFLD group were also predominantly male, overweight, had worse hepatic steatosis, and higher non-invasive liver fibrosis scores, and had significantly worse biochemical indices, including serum levels of liver enzymes and related metabolic and liver biochemical indices compared with the non-FLD (normal) group and the non-MAFLD-NAFLD group (Supplementary Table 1). Of note, after excluding patients with concurrent diagnosis of NAFLD and MAFLD, differences of the biochemical indices between the non-MAFLD-NAFLD and the non-NAFLD-MAFLD group were greater than those between the NAFLD and MAFLD group (Table 1 and Supplementary Table 1). The non-MAFLD-NAFLD group versus non-NAFLD-MAFLD group: mean ALT, 26.59 vs. 43.65, mean GGT, 33.69 vs. 54.85, and mean TG, 1.56 vs. 2.04; NAFLD versus MAFLD group: mean ALT, 33.47 vs. 34.45, mean GGT, 43.15 vs. 44.52, and mean TG, 2.13 vs. 2.19. Comparatively, the non-MAFLD-NAFLD group had a more modest clinical features than the NAFLD and MAFLD groups. The results of the comparison indicated the capacity of packing more severe cases of the new FLD definition.
The clinical indices of different MAFLD subtypes were compared (Supplementary Table 2). Among the 20,507 MAFLD patients, 19,053 with BMIs ≥23.0 kg/m2 were assigned to the BMI-related MAFLD group (obese-MAFLD), and 2,763 with diabetes assigned to the diabetes-related MAFLD group (diabetes-MAFLD). We found that the two groups had similar clinical manifestations, except for metabolic abnormalities. The thinner with ≥2 metabolic abnormalities group was characterized by generally worse clinical features compared with the participants without fatty livers, including serum levels of liver enzymes, HbA1c, FPG, serum lipids, and indicators of hepatic fibrosis.
Risk of liver-related and cardiac-cerebrovascular disease
In the 72,392 participants, 1,274 stroke, 952 coronary heart disease, 793 liver failure, 522 heart failure, 123 cirrhosis, 40 cardiomyopathy, and 39 hepatocellular carcinoma (HCC) events occurred during the median follow-up of 5.22 (interquartile range: 5.21–5.22) years. The incidence rates of the events were 357.49/100,000, 280.07/100,000, 229.34/100,000, 147.60/100,000, 31.22/100,000, 12.05/100,000, and 10.47/100,000 participant years, respectively (Supplementary Fig. 2).
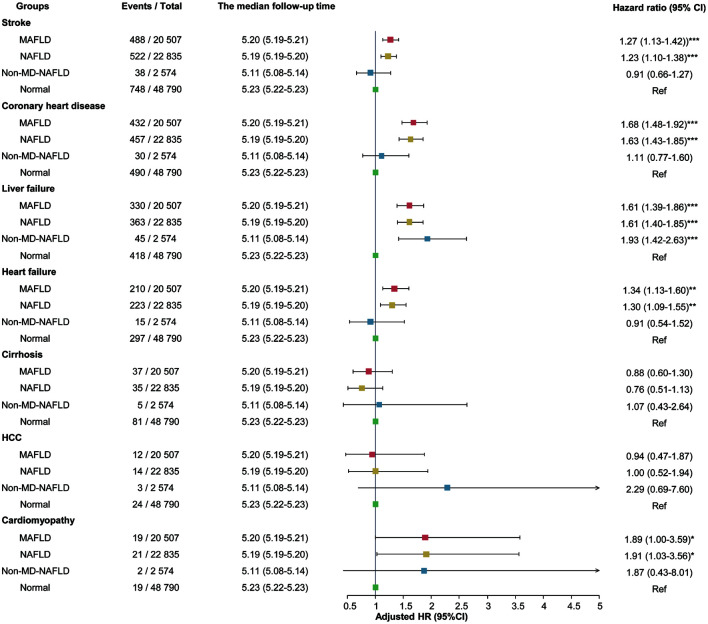
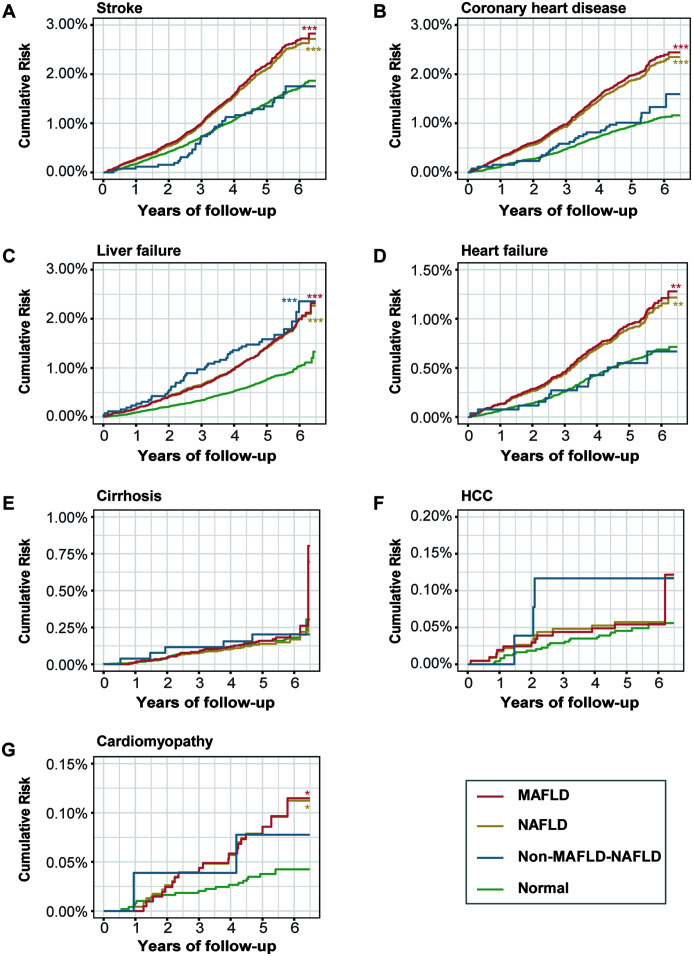
Supplementary Figure 3 shows the incident rates of liver-related and cardiac-cerebral vascular diseases in the FLD groups. The association of different FLD groups with the risk of liver-related and cardiac-cerebral vascular diseases was examined by the Kaplan-Meier method (Fig. 1). The MAFLD and NAFLD groups had a higher cumulative risk of stroke, CHD, liver failure, and heart failure than the normal group. Multivariable Cox regression analysis showed that MAFLD and NAFLD were significantly associated with increased risk of the diseases. The adjusted hazard ratios (HRs) for stroke were 1.27 and 1.23 (95% CI, 1.13–1.42 and 1.10–1.38, respectively; both p<0.001). The adjusted HRs for stroke were 1.27 and 1.23 (95% CI, 1.13–1.42 and 1.10–1.38, respectively; both p<0.001). The adjusted HRs for CHD were 1.68 (95% CI, 1.48–1.92; p<0.001) and 1.63 (95% CI, 1.43–1.85; p<0.001). The adjusted HRs for liver failure were 1.61 (95% CI, 1.39–1.86; p<0.001) and 1.61 (95% CI, 1.40–1.85; p<0.001). The adjusted HRs for heart failure were 1.34 (95% CI, 1.13–1.60; p=0.001) and 1.30 (95% CI, 1.00–1.55; p=0.003) (Fig. 2). Similar results were seen after adjusting for age and sex (p<0.05, Supplementary Table 3). We did not observe significant differences in the risk of HCC or cirrhosis, mostly because of insufficient outcomes. We did not detect significant differences in the risk of liver-related or cardiac-cerebral vascular disease in the non-MAFLD-NAFLD and normal groups.
Fig. 1. Cumulative risk of developing incident (A) Stroke, (B) Coronary heart disease, (C) Liver failure, (D) Heart failure, (E) Cirrhosis, (F) Hepatocellular carcinoma, (G) Cardiomyopathy in four different classifications of fatty liver.
The normal group was the reference. Survival models were adjusted for age and sex. *p<0.05, **p<0.01. ***p<0.001.
Fig. 2. Impact of four different classifications of fatty liver on liver-related and cardiovascular disease outcomes. Hazard ratios were obtained from adjusted survival models with the normal group as reference.
The MAFLD participants were assigned to three subtypes, obese-MAFLD, diabetes-MAFLD, and lean-MAFLD (participants with BMIs <23.0 kg/m2 and with ≥2 metabolic abnormalities) (Table 2). Diabetes-MAFLD had the highest incidence of liver-related and cardiac-cerebral vascular disease, lean MAFLD had the second-highest incidence, and obese-MAFLD had the lowest incidence. Unadjusted logistic regression results showed that the three subtypes were significantly associated with increased risk of liver failure, coronary heart disease, and stroke. In addition, diabetes-MAFLD and lean MAFLD were associated with significantly higher risk.
Table 2. Adjusted hazard ratios of incident severe liver disease and cardio-cerebrovascular disease in MAFLD defined by different criteria.
| Outcomes | No. of total | The median follow-up time [Years (95%CI)] | PYs | No. of events | Incidence rate per 100 000 PYs | HR (95% CI) | P | aHRa (95% CI) | P | P b |
|---|---|---|---|---|---|---|---|---|---|---|
| Cirrhosis c | 0.606 | |||||||||
| Normal | 48 790 | 5.23 (5.22 - 5.23) | 261,514.7 | 81 | 30.97 | Ref | Ref | Ref | Ref | |
| Obese-MAFLD | 19 053 | 5.20 (5.20 - 5.21) | 101,733.5 | 35 | 34.40 | 1.12 (0.75–1.66) | 0.579 | 0.91 (0.61–1.36) | 0.645 | |
| Diabetes-MAFLD | 2 763 | 5.27 (5.25 – 5.32) | 14,829.4 | 10 | 67.43 | 2.20 (1.14–4.25) | 0.018* | 1.13 (0.58–2.20) | 0.715 | |
| Lean MAFLD | 1 242 | 5.11 (5.06 - 5.18) | 6,559.5 | 2 | 30.49 | 1.00 (0.25–4.09) | 0.994 | 0.62 (0.15–2.52) | 0.501 | |
| HCCc | 0.833 | |||||||||
| Normal | 48 790 | 5.23 (5.22 - 5.23) | 261,644.7 | 24 | 9.17 | Ref | Ref | Ref | Ref | |
| Obese-MAFLD | 19 053 | 5.20 (5.20 - 5.21) | 101,772.1 | 11 | 10.81 | 1.18 (0.58–2.41) | 0.652 | 0.93 (0.46–1.91) | 0.847 | |
| Diabetes-MAFLD | 2 763 | 5.27 (5.25 – 5.32) | 14,839.9 | 3 | 20.22 | 2.20 (0.66–7.31) | 0.198 | 0.98 (0.29–3.27) | 0.975 | |
| Lean MAFLD | 1 242 | 5.11 (5.06 - 5.18) | 6,560.4 | 1 | 15.24 | 1.67 (0.23–12.32) | 0.617 | 1.08 (0.15–8.02) | 0.940 | |
| Liver failured | 0.004** | |||||||||
| Normal | 48 790 | 5.23 (5.22 - 5.23) | 260,823.5 | 418 | 160.26 | Ref | Ref | Ref | Ref | |
| Obese-MAFLD | 19 053 | 5.20 (5.20 - 5.22) | 101,168.1 | 302 | 298.51 | 1.87 (1.60–2.18) | <0.001*** | 1.62 (1.39–1.89) | <0.001*** | |
| Diabetes-MAFLD | 2 763 | 5.27 (5.25 – 5.31) | 14,668.9 | 69 | 470.38 | 2.94 (2.25–3.83) | <0.001*** | 1.87 (1.44–2.44) | <0.001*** | |
| Lean MAFLD | 1 242 | 5.11 (5.06 - 5.18) | 6,529.5 | 25 | 382.88 | 2.40 (1.60–3.61) | <0.001*** | 1.66 (1.10–2.49) | 0.015* | |
| Coronary heart diseasec | 0.215 | |||||||||
| Normal | 48 790 | 5.23 (5.22 - 5.23) | 260,513.7 | 490 | 188.09 | Ref | Ref | Ref | Ref | |
| Obese-MAFLD | 19 053 | 5.21 (5.20 - 5.21) | 100,852.4 | 389 | 385.71 | 2.05 (1.79–2.34) | <0.001*** | 1.69 (1.48–1.93) | <0.001*** | |
| Diabetes-MAFLD | 2 763 | 5.27 (5.25 – 5.32) | 14,487.7 | 144 | 993.95 | 5.29 (4.39–6.37) | <0.001*** | 2.32 (1.93–2.80) | <0.001*** | |
| Lean MAFLD | 1 242 | 5.11 (5.06 - 5.18) | 6,502.0 | 30 | 461.40 | 2.45 (1.70–3.54) | <0.001*** | 1.38 (0.96–2.00) | 0.086 | |
| Strokec | 0.579 | |||||||||
| Normal | 48 790 | 5.23 (5.22 - 5.23) | 259,944.7 | 748 | 287.75 | Ref | Ref | Ref | Ref | |
| Obese-MAFLD | 19 053 | 5.21 (5.20 - 5.21) | 100,816.0 | 439 | 435.45 | 1.52 (1.35–1.70) | <0.001*** | 1.28 (1.14–1.44) | <0.001*** | |
| Diabetes-MAFLD | 2 763 | 5.27 (5.25 – 5.33) | 14,439.3 | 172 | 1,191.20 | 4.15 (3.52–4.90) | <0.001*** | 1.77 (1.50–2.09) | <0.001*** | |
| Lean MAFLD | 1 242 | 5.11 (5.06 - 5.18) | 6,485.6 | 38 | 585.91 | 2.04 (1.47–2.83) | <0.001*** | 1.07 (0.77–1.49) | 0.670 | |
| Heart failurec | 0.309 | |||||||||
| Normal | 48 790 | 5.23 (5.22 - 5.23) | 261,016.5 | 297 | 113.79 | Ref | Ref | Ref | Ref | |
| Obese-MAFLD | 19 053 | 5.20 (5.19 - 5.21) | 101,347.8 | 192 | 189.45 | 1.66 (1.39–2.00) | <0.001*** | 1.38 (1.15–1.65) | 0.001** | |
| Diabetes-MAFLD | 2 763 | 5.27 (5.25 – 5.32) | 14,658.9 | 70 | 477.53 | 4.19 (3.23–5.44) | <0.001*** | 1.87 (1.44–2.43) | <0.001*** | |
| Lean MAFLD | 1 242 | 5.11 (5.06 - 5.18) | 6,538.5 | 12 | 183.53 | 1.61 (0.90–2.87) | 0.105 | 0.89 (0.50–1.59) | 0.699 | |
| Cardiomyopathyc | 0.527 | |||||||||
| Normal | 48 790 | 5.23 (5.22 - 5.23) | 261,659.8 | 19 | 7.26 | Ref | Ref | Ref | Ref | |
| Obese-MAFLD | 19 053 | 5.20 (5.20 - 5.21) | 101,768.6 | 18 | 17.69 | 2.44 (1.28–4.64) | 0.007** | 1.94 (1.02–3.71) | 0.044* | |
| Diabetes-MAFLD | 2 763 | 5.27 (5.25 – 5.32) | 14,840.1 | 4 | 26.95 | 3.71 (1.26–10.91) | 0.017* | 1.81 (0.61–5.35) | 0.287 | |
| Lean MAFLD | 1 242 | 5.11 (5.06 - 5.18) | 6,562.3 | 1 | 15.24 | 2.10 (0.28–15.67) | 0.470 | 1.31 (0.17–9.83) | 0.794 |
aModels were adjusted for age at baseline (continuous) and sex (female or male). bTests of proportional hazards assumption for adjusted models. cSurvival analysis was started by Cox proportional hazards models. dSurvival analysis was started by AFT model. *p<0.05, **p<0.01 and ***p<0.001. aHR, adjusted hazard ratio; HCC, hepatocellular carcinoma; HR, hazard ratio; MAFLD, metabolic associated fatty liver disease; PYs, person-years.
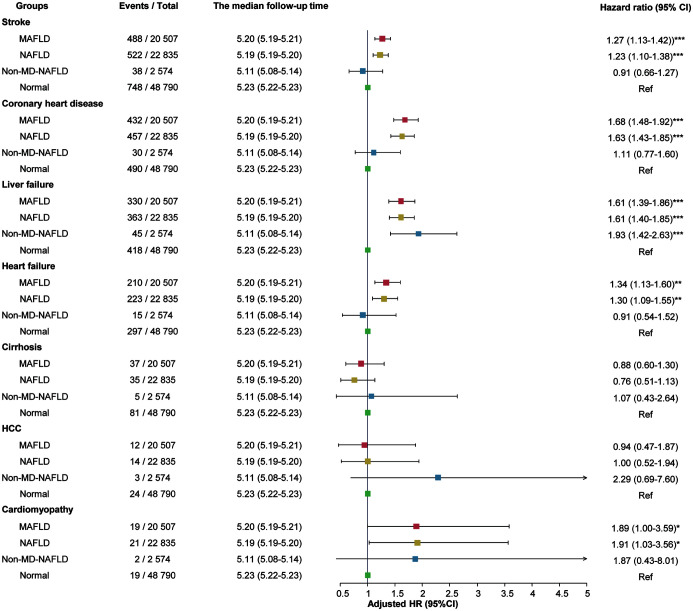
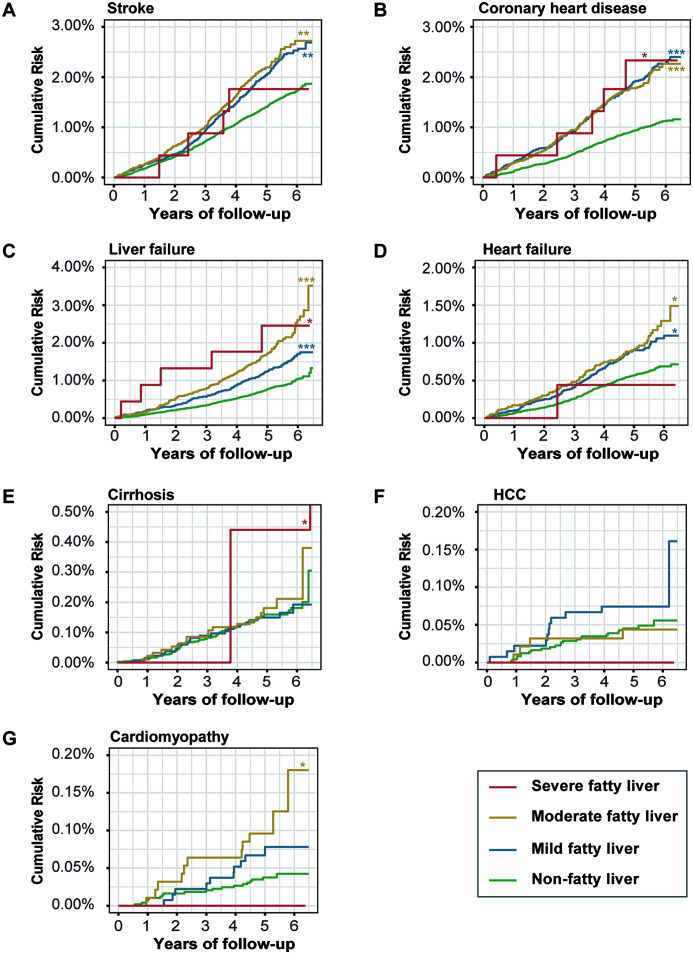
Association of steatosis severity with liver-related and cardiac-cerebral vascular outcomes is shown in Supplementary Table 4. The moderate and severe FLD group had higher cumulative risks of stroke, CHD, liver failure, heart failure, and cirrhosis than the non-FLD group (Fig. 3). Multivariable Cox regression analysis found that moderate and severe FLD patients had a significant association with increased risk of the diseases [adjusted HR for stroke: 1.24 (95% CI, 1.07–1.44) and 1.35 (95% CI, 0.50–3.60), p=0.005 and 0.552, respectively; adjusted HR for CHD: 1.54 (95% CI, 1.30–1.83) and 2.42 (95% CI, 1.00–5.84), p<0.001 and p<0.049, respectively]. The adjusted HRs for liver failure were 1.99 (95% CI, 1.67–2.38; p<0.001) and 2.68 (95% CI, 1.11–6.47; p<0.029). The adjusted HRs for heart failure were 1.34 (95% CI, 1.06–1.68; p=0.014) and 0.78 (95% CI, 0.11–5.54; p=0.802) (Supplementary Table 4). We conducted sensitivity analyses stratified by sex (Supplementary Table 5) and HBV infection (Supplementary Table 6). The associations of MAFLD and NAFLD with liver failure and individual cardiac-cerebral vascular diseases were statistically significant in all subgroups. We did not observe significant differences in risk in the non-MAFLD-NAFLD and normal group in any subgroup.
Fig. 3. Cumulative risk of developing incident (A) Stroke, (B) Coronary heart disease, (C) Liver failure, (D) Heart failure, (E) Cirrhosis, (F) Hepatocellular carcinoma, (G) Cardiomyopathy in four groups by steatosis severity.
Non-fatty liver was the reference. Survival models were adjusted for age and sex. *p<0.05, **p<0.01. ***p<0.001.
Discussion
The principal finding of this study was that MAFLD definition had better ability to identify patients with clinical characteristics significantly worse than the NAFLD definition. Although a significant proportion of patients qualified the diagnostic criteria for both NAFLD and MAFLD, non-NAFLD-MAFLD group showed significantly worse clinical manifestations. In addition, thin patients diagnosed with ≥2 or ≥3 metabolic abnormalities presented a similar clinical manifestation. We saw that FLD was associated with a higher risk of cardiac-cerebral vascular events, despite whether defined as MAFLD or NAFLD. Participants with NAFLD but not MAFLD had a similar risk with those without fatty liver, but were at risk lower than those with MAFLD.
Ever since the introduction of MAFLD to replace NAFLD by a panel of international experts, the novel terminology of MAFLD has sparked widespread discussion and concern, but has gained increasing acceptance and endorsement.6,16–19 Real-world studies on MAFLD must provide strong evidence for rationally assessing the benefit and practicability of the change in terminology. Our study confirmed the rationality of the term change from three parts: 1) MAFLD was found more sensitive than NAFLD in discriminating patients with poorer clinical features and fibrosis at risk. Our results followed an earlier cross-sectional study based on the third National Health and Nutrition Examination Surveys of the United States (NHANES III).9 The study found that compared with NAFLD, MAFLD patients were significantly older, had higher BMI level, higher proportions of metabolic comorbidities, and were at a higher risk of disease progression. Another study of 765 Japanese patients also showed that the MAFLD definition better identified patients with significant fibrosis evaluated by non-invasive tests, which follows our results.20 2) Patients diagnosed with NAFLD but without MAFLD had a similar risk of liver-related and cardio-cerebral vascular diseases as in those without fatty liver. Similarly, in recent studies, the NAFLD-only group was associated with lower CVD risk and CVD-related mortality and all-cause mortality.14,21 the NAFLD-only patients had a generally “healthier” characteristics when compared with MAFLD patients. 3) Another concern is the cut-off threshold for the number of metabolic abnormalities. To date, this is among the few studies reporting that lean-MAFLD with ≥2 metabolic abnormalities has similar clinical features as those with ≥ 3 metabolic abnormalities. On the whole, the new definition of MAFLD can identify patients with metabolically complicated fatty liver, and leaves out a small fraction of individuals with metabolically uncomplicated fatty liver, which confers a lower risk of disease progression.
NAFLD is strongly associated with metabolic conditions such as overweight/obesity and T2DM.22 However, NAFLD can be diagnosed in so-called lean (non-obese) individuals with BMI < 23 kg/m2, the prevalence of which ranges between 3.7% and 7.0% in the general population.23 A meta-analysis suggested that the non-obese or lean NAFLD population was more likely to die from causes related to cardiovascular disease than the obese NAFLD population [cardiovascular-related mortality (per 1,000 PY), 4.0 (0.1–14.9) vs 2.4 (0.0–13.3)], indicating that individuals with BMI < 23 kg/m2 cannot be overlooked.23 In our analysis, the cardiac-cerebral vascular disease incidence rate was higher in the lean MAFLD group than in the obese MAFLD group, which follows the previous findings. Of note, the diabetes-MAFLD group had the highest risk of cardiac-cerebral vascular disease, which should be further elucidated.
Another recently published research based on NHANES III (1988–1994) data and the NHANES survey cycle (2017–2018) showed different findings from our study.24 This discrepancy may be attributable to the vast differences in the study population, classification details and the study outcomes. The participants in our study were Chinese (predominantly Han ethnicity) and had a greater proportion of males (57.89%) and lesser proportion of alcohol-drinkers (0.26%). In contrast, the study population in the previous study comprised of 76.0% non-Hispanic White, 49.5% males, and 15.0% excessive drinkers. The proportion of excessive drinkers in our study was similar to that in a cohort study exploring the epidemiological impact of MAFLD which randomly sampled from the census database of the Hong Kong Government, in which the proportion was only 0.9%.10 Beyond that, in our study, only 34.15% patients in non-NAFLD-MAFLD group were noted to have alcoholic fatty liver (ALD), but in the research, 99% patients in non-NAFLD-MAFLD group had ALD and the identification ability of MAFLD for high-risk FLD patients was attributed to the impact of ALD on poor outcomes. On the other hand, when diagnosing FLD, our study included all patients with hepatic steatosis, which follows previous studies,9,14,20 despite the severity (mild, moderate, or severe), but the research only focused on individuals with moderate or severe hepatic steatosis. In addition, the grouping approach based on NAFLD, MAFLD, and non-MAFLD-NAFLD in our study is similar to that in earlier studies but different from the research.9 Considering the overlapping patients in the NAFLD and MAFLD groups, we also compared the non-MAFLD-NAFLD group and the non-NAFLD-MAFLD group, and the significant differences of biochemical indices were still seen. Moreover, our study focused on the incidence risk of liver-related and cardio-cerebral vascular disease while the outcomes of the research were mortality from any cause and specific causes.
To the best of our knowledge, this is the first large-size Chinese population study to describe the distinctions in clinical features and disease progression between MAFLD and NAFLD. This study confirms the diagnostic ability and the efficacy of the new diagnostic criteria in identifying high-risk individuals and supports the redefinition of the nomenclature considering the inclusive and clinically practical value of MAFLD. However, some limitations of our study should be considered while interpreting the results. First, the study population was derived from physical examinees at a single hospital. This may have limited the representativeness of our findings and our results may have been affected by referral bias. However, the relatively long enrolment period and follow-up time and the large-size of the cohort add to the robustness of the correlation results. Second, all hepatic steatosis patients were diagnosed by ultrasonography examination instead of liver biopsy, the gold-standard. Liver biopsy is not recommended and practiced for the diagnosis of hepatic steatosis because of its invasiveness, high costs, sampling variability, and poor acceptability.25 Ultrasonography examination is the most commonly used imaging method because of its wider availability, low-cost, convenience, and acceptability.25 Besides, ultrasonography has an acceptable diagnostic accuracy for hepatic steatosis, with sensitivity and specificity of 84.8% and 93.6% for moderate to severe steatosis and 82% and 80% for ≥5% histologically defined steatosis.26,27
Conclusions
In a large-sized longitudinal Chinese cohort, MAFLD definition showed a distinct advantage over NAFLD in identifying a significant subset of patients with worrying clinical manifestations and worse prognosis. Participants with NAFLD but without MAFLD did not show a significantly higher risk of poor prognosis than those without fatty liver. The proposed concept of MAFLD can promote early identification and interventions for hepatic steatosis patients at a higher risk of intrahepatic and extrahepatic complications. The redefinition can help reduce the long-term risks of cardiovascular and cerebrovascular diseases.
Supporting information
Abbreviations
- ALT
alanine aminotransferase
- BMI
body mass index
- FLD
fatty liver disease
- GGT
γ-glutamyl transferase
- HbA1c
glycated hemoglobin
- HBV
hepatitis B virus
- HCC
hepatocellular carcinoma
- ICD-10
International Classification of Diseases-Tenth Revision
- MAFLD
metabolic-associated fatty liver disease
- NAFLD
non-alcoholic fatty liver disease
- TG
triglyceride
Ethical statement
The First Affiliated Hospital with Nanjing Medical University Ethics Review Board approved the study protocol and informed consent was obtained from all subjects.
Data sharing statement
Individual participant data will not be shared on public, but be available from the correspondence authors on request through E-mail.
References
- 1.Younossi Z, Tacke F, Arrese M, Chander Sharma B, Mostafa I, Bugianesi E, et al. Global Perspectives on Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis. Hepatology. 2019;69(6):2672–2682. doi: 10.1002/hep.30251. [DOI] [PubMed] [Google Scholar]
- 2.Younossi ZM. Non-alcoholic fatty liver disease - A global public health perspective. J Hepatol. 2019;70(3):531–544. doi: 10.1016/j.jhep.2018.10.033. [DOI] [PubMed] [Google Scholar]
- 3.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 4.Adams LA, Anstee QM, Tilg H, Targher G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut. 2017;66(6):1138–1153. doi: 10.1136/gutjnl-2017-313884. [DOI] [PubMed] [Google Scholar]
- 5.Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62(1 Suppl):S47–S64. doi: 10.1016/j.jhep.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 6.Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J Hepatol. 2020;73(1):202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 7.Younossi ZM, Rinella ME, Sanyal AJ, Harrison SA, Brunt EM, Goodman Z, et al. From NAFLD to MAFLD: Implications of a Premature Change in Terminology. Hepatology. 2021;73(3):1194–1198. doi: 10.1002/hep.31420. [DOI] [PubMed] [Google Scholar]
- 8.Fouad Y, Elwakil R, Elsahhar M, Said E, Bazeed S, Ali Gomaa A, et al. The NAFLD-MAFLD debate: Eminence vs evidence. Liver Int. 2021;41(2):255–260. doi: 10.1111/liv.14739. [DOI] [PubMed] [Google Scholar]
- 9.Lin S, Huang J, Wang M, Kumar R, Liu Y, Liu S, et al. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int. 2020;40(9):2082–2089. doi: 10.1111/liv.14548. [DOI] [PubMed] [Google Scholar]
- 10.Wong VW, Wong GL, Woo J, Abrigo JM, Chan CK, Shu SS, et al. Impact of the New Definition of Metabolic Associated Fatty Liver Disease on the Epidemiology of the Disease. Clin Gastroenterol Hepatol. 2021;19(10):2161–2171.e5. doi: 10.1016/j.cgh.2020.10.046. [DOI] [PubMed] [Google Scholar]
- 11.National Workshop on Fatty Liver and Alcoholic Liver Disease, Chinese Society of Hepatology, Chinese Medical Association, Fatty Liver Expert Committee, Chinese Medical Doctor Association Guidelines of prevention and treatment for nonalcoholic fatty liver disease: a 2018 update. Zhonghua Gan Zang Bing Za Zhi. 2018;26(3):195–203. doi: 10.3760/cma.j.issn.1007-3418.2018.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003;38(2):518–526. doi: 10.1053/jhep.2003.50346. [DOI] [PubMed] [Google Scholar]
- 13.Vilar-Gomez E, Chalasani N. Non-invasive assessment of non-alcoholic fatty liver disease: Clinical prediction rules and blood-based biomarkers. J Hepatol. 2018;68(2):305–315. doi: 10.1016/j.jhep.2017.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Nguyen VH, Le MH, Cheung RC, Nguyen MH. Differential Clinical Characteristics and Mortality Outcomes in Persons With NAFLD and/or MAFLD. Clin Gastroenterol Hepatol. 2021;19(10):2172–2181.e6. doi: 10.1016/j.cgh.2021.05.029. [DOI] [PubMed] [Google Scholar]
- 15.Kanwal F, Kramer JR, Li L, Dai J, Natarajan Y, Yu X, et al. Effect of Metabolic Traits on the Risk of Cirrhosis and Hepatocellular Cancer in Nonalcoholic Fatty Liver Disease. Hepatology. 2020;71(3):808–819. doi: 10.1002/hep.31014. [DOI] [PubMed] [Google Scholar]
- 16.Mendez-Sanchez N, Arrese M, Gadano A, Oliveira CP, Fassio E, Arab JP, et al. The Latin American Association for the Study of the Liver (ALEH) position statement on the redefinition of fatty liver disease. Lancet Gastroenterol Hepatol. 2021;6(1):65–72. doi: 10.1016/s2468-1253(20)30340-x. [DOI] [PubMed] [Google Scholar]
- 17.Nan Y, An J, Bao J, Chen H, Chen Y, Ding H, et al. The Chinese Society of Hepatology position statement on the redefinition of fatty liver disease. J Hepatol. 2021;75(2):454–461. doi: 10.1016/j.jhep.2021.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Shiha G, Alswat K, Al Khatry M, Sharara AI, Örmeci N, Waked I, et al. Nomenclature and definition of metabolic-associated fatty liver disease: a consensus from the Middle East and north Africa. Lancet Gastroenterol Hepatol. 2021;6(1):57–64. doi: 10.1016/s2468-1253(20)30213-2. [DOI] [PubMed] [Google Scholar]
- 19.Shiha G, Korenjak M, Eskridge W, Casanovas T, Velez-Moller P, Högström S, et al. Redefining fatty liver disease: an international patient perspective. Lancet Gastroenterol Hepatol. 2021;6(1):73–79. doi: 10.1016/S2468-1253(20)30294-6. [DOI] [PubMed] [Google Scholar]
- 20.Yamamura S, Eslam M, Kawaguchi T, Tsutsumi T, Nakano D, Yoshinaga S, et al. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD. Liver Int. 2020;40(12):3018–3030. doi: 10.1111/liv.14675. [DOI] [PubMed] [Google Scholar]
- 21.Lee H, Lee YH, Kim SU, Kim HC. Metabolic Dysfunction-Associated Fatty Liver Disease and Incident Cardiovascular Disease Risk: A Nationwide Cohort Study. Clin Gastroenterol Hepatol. 2021;19(10):2138–2147.e10. doi: 10.1016/j.cgh.2020.12.022. [DOI] [PubMed] [Google Scholar]
- 22.Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 23.Ye Q, Zou B, Yeo YH, Li J, Huang DQ, Wu Y, et al. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(8):739–752. doi: 10.1016/S2468-1253(20)30077-7. [DOI] [PubMed] [Google Scholar]
- 24.Younossi ZM, Paik JM, Al Shabeeb R, Golabi P, Younossi I, Henry L. Are there outcome differences between NAFLD and metabolic-associated fatty liver disease? Hepatology. 2022;76(5):1423–1437. doi: 10.1002/hep.32499. [DOI] [PubMed] [Google Scholar]
- 25.Castera L, Friedrich-Rust M, Loomba R. Noninvasive Assessment of Liver Disease in Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2019;156(5):1264–1281.e4. doi: 10.1053/j.gastro.2018.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hernaez R, Lazo M, Bonekamp S, Kamel I, Brancati FL, Guallar E, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology. 2011;54(3):1082–1090. doi: 10.1002/hep.24452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ballestri S, Mantovani A, Byrne CD, Lonardo A, Targher G. Diagnostic accuracy of ultrasonography for the detection of hepatic steatosis: an updated meta-analysis of observational studies. Metabolism and Target Organ Damage. 2021;1(1):7. doi: 10.20517/mtod.2021.05. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.