Abstract
Objective
To estimate the pooled prevalence of sexual dysfunction (SD) in women with multiple sclerosis (MS).
Methods
We systematically searched PubMed, Scopus, EMBASE, Web of Science, and google scholar and also gray literature up to October 2021.
The search strategy includes:
(“Multiple Sclerosis” OR “MS” OR “Disseminated Sclerosis” OR (Disseminated AND Sclerosis) OR (Sclerosis AND Multiple)) AND (“Sexual Dysfunction” OR (Sexual AND Dysfunction) OR (Sexual AND Dysfunctions) OR (Sexual AND Disorders) OR (Sexual AND Disorder) OR “Sexual Dysfunctions” OR “Sexual Disorders” OR “Sexual Disorder” OR “Psychosexual Dysfunctions” OR (Dysfunction AND Psychosexual) OR (Dysfunctions AND Psychosexual) OR “Psychosexual Dysfunction” OR “Psychosexual Disorders” OR (Disorder AND Psychosexual) OR (Disorders AND Psychosexual) OR “Psychosexual Disorder” OR “Hypoactive Sexual Desire Disorder” OR “Sexual Aversion Disorder” OR (Aversion Disorders AND Sexual) OR (Disorders AND Sexual Aversion) OR “Sexual Aversion Disorders” OR “Orgasmic Disorder” OR (Disorders AND Orgasmic) OR “Orgasmic Disorders” OR “Sexual Arousal Disorder” OR (Arousal Disorders AND Sexual) OR (Disorders AND Sexual Arousal) OR “Sexual Arousal Disorders” OR “Frigidity”).
Results
We found 2150 articles by literature search, after deleting duplicates 1760 remained. Fifty-six articles remained for meta-analysis. The pooled prevalence of SD in MS patients estimated as 61% (95%CI:56–67%) (I2:95.7%, P < 0.001). The pooled prevalence of Anorgasmia in MS patients estimated as 29% (95%CI:20–39%) (I2:85.3%, P < 0.001). The pooled odds of developing SD in MS women estimated as 3.05(95%CI: 1.74–5.35) (I2:78.3%, P < 0.001). The pooled prevalence of decreased vaginal lubrication in MS patients estimated as 32%(95%CI:27–37%) (I2 = 94.2%, P < 0.001). The pooled prevalence of reduced libido was 48%(95%CI:36–61%) (I2:92.6%, P < 0.001). The pooled prevalence of arousal problems was 40%(95%CI: 26–54%) (I2:97.4%, P < 0.001). The pooled prevalence of intercourse satisfaction was 27% (95%CI: 8–46%) (I2:99%, P < 0.001).
Conclusion
The result of this systematic review and meta-analysis show that the pooled prevalence of SD in women with MS is 61% and the odds of developing SD in comparison with controls is 3.05.
Keywords: Sexual dysfunction, Multiple sclerosis, Prevalence
Introduction
Multiple sclerosis (MS) is a degenerative, neurologic disease of the central nervous system (CNS) affecting women more than men [1]. It usually occurs between 20 and 50 years of age, while MS-related complications include both physical and psychological consequences [2]. One of the most common multi-dimensional complications is sexual dysfunction (SD) involving physiological, psychosocial, and interpersonal factors [3]. It is suggested that women with MS have problems regarding finding a partner, building a relationship, and marital issues [3]. SD has negative impacts on health-related quality of life (HRQoL), especially on youth [4, 5]. It can be found at any stages of the disease, and is present at early stage in some cases [6, 7]. The exact etiology of SD in MS is not clear, but physical disability, psychological difficulties, and also side effects of medications could cause SD [8, 9].
Primary SD is the consequence of neurological changes in the body, while secondary SD is due to MS-related complications such as fatigue, pain, spasticity, bladder, and bowel dysfunction [10]. Tertiary SD is related to psychological consequences of MS such as depression, anxiety, and cognitive impairment / and cultural issues regarding sexual consultant in different nations [10].
Loss of orgasm, libido, lubrication, and increased spasticity are common during sexual activity in women with MS [11, 12].
Different factors such as age, disease duration, disability level, bladder dysfunction, cognitive impairment, and disease course influence SD in MS women [13–15].
Up to now, different original studies have been conducted and three previous systematic reviews and meta-analyses estimated the pooled prevalence of SD in women with MS [16–18]. The aim of this system and meta-analysis is to update the prevalence of SD in MS women.
Methods
Eligibility criteria
Inclusion criteria were
Cross-sectional studies, Articles that had been published in the English language.
Exclusion criteria
Case-report, RCT studies.
We followed The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 for reporting this systematic review [19].
Information sources
Two independent researchers systematically searched PubMed, Scopus, EMBASE, Web of Science, and google scholar and also gray literature up to October 2021.
The search strategy includes
(“Multiple Sclerosis” OR “MS” OR “Disseminated Sclerosis” OR (Disseminated AND Sclerosis) OR (Sclerosis AND Multiple)) AND (“Sexual Dysfunction” OR (Sexual AND Dysfunction) OR (Sexual AND Dysfunctions) OR (Sexual AND Disorders) OR (Sexual AND Disorder) OR “Sexual Dysfunctions” OR “Sexual Disorders” OR “Sexual Disorder” OR “Psychosexual Dysfunctions” OR (Dysfunction AND Psychosexual) OR (Dysfunctions AND Psychosexual) OR “Psychosexual Dysfunction” OR “Psychosexual Disorders” OR (Disorder AND Psychosexual) OR (Disorders AND Psychosexual) OR “Psychosexual Disorder” OR “Hypoactive Sexual Desire Disorder” OR “Sexual Aversion Disorder” OR (Aversion Disorders AND Sexual) OR (Disorders AND Sexual Aversion) OR “Sexual Aversion Disorders” OR “Orgasmic Disorder” OR (Disorders AND Orgasmic) OR “Orgasmic Disorders” OR “Sexual Arousal Disorder” OR (Arousal Disorders AND Sexual) OR (Disorders AND Sexual Arousal) OR “Sexual Arousal Disorders” OR “Frigidity”).
Selection process
After obtaining the results, and importing them to Endnote, they omitted duplicates. Then titles, and abstracts were screening, and potential full texts were obtained. The researchers extracted data from each study, entered in Excel, and in the case of discrepancies, the third researcher solved the problem.
Data items
Data regarding first author, country of origin, number of enrolled patients, number of cases with SD, mean age, mean EDSS, mean duration of the disease, were collected.
Statistical analysis
All statistical analyses were performed using STATA (Version 14.0; Stata Corp LP, College Station, TX, USA). To determine heterogeneity, Inconsistency (I2) was calculated.
We used random effects model.
Effect measures
The pooled prevalence of domains of sexual function were estimated. The pooled odds ratio(OR) of developing sexual dysfunction in women with MS comparing to healthy controls were calculated.
Results
We found 2150 articles by literature search, after deleting duplicates 1760 remained. Fifty-six articles remained for meta-analysis (Fig. 1).
Fig. 1.
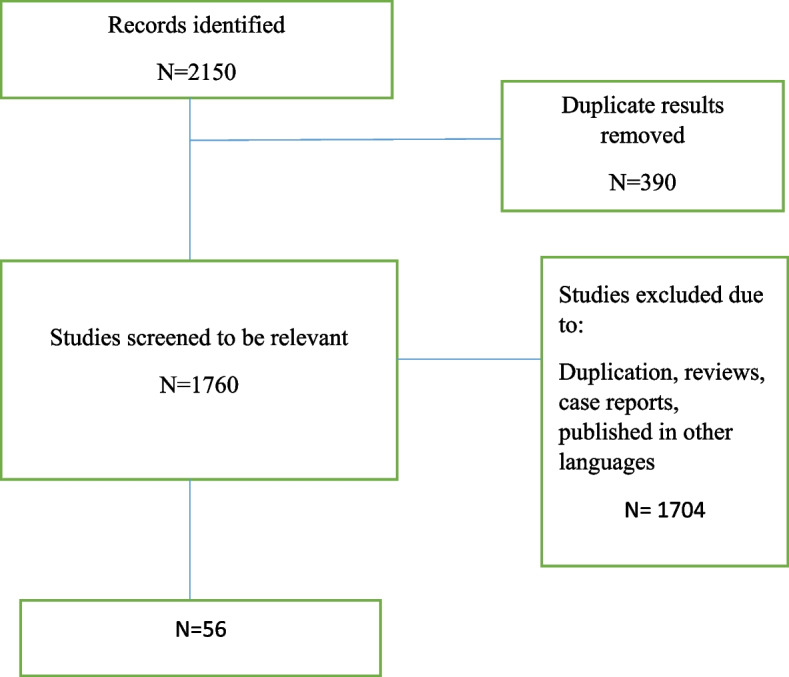
Flow diagram summarizing the selection of eligible studies
Included studies were published between 1996, and 2021.Most included studies were from Iran, followed by Italy, and Turkey. The mean age of participants ranged between 24.7, and 50.7 years, and EDSS ranged between 1.7 and 5. The most frequent applied questionnaire was FSFI (Table 1).
Table 1.
Basic characteristics of included studies
| Author | Year | Country | Design | T. MS All female |
MS type RRMS SPMS PPMS CIS |
Age | EDSS | Disease duration | Measurements | Total sexual dysfunction in PwMS | Anorgasmia |
|---|---|---|---|---|---|---|---|---|---|---|---|
| M Zorzon [12] | 1999 | Italy | Case control | 70 |
RR 50 PP 16 SP 4 |
40.2(10.9) | 2.6(1.7) | 10.7(8.5) | Szasz Sexual Functioning Scale | 44 | 21 |
| M. Zorzon [20] | 2001 | Italy | Cohort | 64 | NR | NR | NR | NR | Szasz Sexual Functioning Scale | 24 | 24 |
| Kisic-Tepavcevic Darija [21] | 2015 | Serbia | cohort | 66 | NR | NR | NR | NR | Szasz sexual functioning scale | 45 | 8 |
| DK Tepavcevic [5] | 2008 | Serbia | cross-sectional | 78 |
RR 54 SP 22 PP 2 |
41.7(9.3) | 4.6(1.6) | 9.1(6.7) | Szasz sexual functioning scale | 66 | 12 |
| Marita P. McCabe [22] | 1996 | Australia | Cross-sectional | 74 | NR | NR | NR | NR |
Szasz At least one problem |
59 | 17 |
| Iris Zavoreo [23] | 2016 | Croatia | Cross sectional | 56 | NR | NR | NR | NR | SSS | NR | NR |
| Aleksandra Kołtuniuk [24] | 2020 | Poland | Cross-sectional | 101 |
RR 82 SP 14 PP 5 |
36.7(9.56) | NR | 75.1(50.2) months | SSQ | 55 | NR |
| M. Lew-Starowicz [25] | 2013 | Poland | Cross-sectional | 137 | NR | 50.7(7) | NR | 16.4(8.6) | SFQ28 | 113 | NR |
| MW Nortvedt [26] | 2001 | Norway | Cross-sectional | 118 | NR | NR | NR | NR | SF-36 | 67 | NR |
| Sacco E [27] | 2011 | Italy | Cross-sectional | 65 | NR | NR | NR | NR | PISQ-12 | 22 | 24 |
| R Vazirinejad [28] | 2008 | Iran | Cross-sectional | 126 | NR | NR | NR | NR | MSQOL-54 | 115 | NR |
| Jing Wu [29] | 2020 | Australia | Cross-sectional | 1591 | NR | NR | NR | NR | MSQOL-54 | NR | NR |
| Z. Tulek [30] | 2011 | Turkey | cross-sectional | 70 | NR | NR | NR | NR | MSQOL-54 | NR | NR |
| MW Nortvedt [31] | 2007 | Norway | Cross-sectional | 40 | NR | NR | NR | NR | MSQoL-54 | NR | NR |
| Claudia H. Marck [32] | 2016 | Australia | Cross-sectional | 1663 | NR | NR | NR | NR | MSQOL-54 | 925 | NR |
| Effat Merghati-Khoei [33] | 2013 | Iran | Cross-sectional | 132 | NR | 36.9(8.3) | NR | 6.8(5.3) | MSISQ-19 | 115 | NR |
| Vida Ghasemi [34] | 2020 | Iran | Cross-sectional | 260 |
RR 212 SP 36 PP 12 |
37.83(7.34) | 2.02 (1.52) | 6.96(5.06) |
MSISQ-19 44.19(16) |
198 Primary SD 176 Secondary SD 158 Tertiary SD 126 |
NR |
| Dilaram Billur Çelik [13] | 2013 | Turkey | Cross-sectional | 44 | NR | NR | NR | NR | MSISQ-19 |
32 Primary SD 19 Seconder SD 25 Tertiary SD 13 |
NR |
| M. Demirkiran [35] | 2006 | Turkey | Cross-sectional | 33 | NR | NR | NR | NR | MSISQ-19 | 27 | NR |
| Sarah Abdo [36] | 2020 | Egypt |
Cross-sectional ABS |
43 | NR | 24.71(3.55) | NR | NR | MSISQ-19 |
24 Primary SD 43 secondary SD 7 Tertiary SD 43 |
NR |
| Edgar Carnero Contentti [37] | 2019 | Argentina | Cross-sectional | 137 |
RR 112 PP 9 SP 18 |
49.1(10.2) | NR | 7.5(0.5) | MSISQ-19 |
119 Primary SD 99 Secondary SD 103 Tertiary SD 88 |
NR |
| Patrick Altmann [38] | 2021 | Italy | cross-sectional | 53 | NR | NR | NR | NR | MSISQ-19 | 25 | NA |
| Fereshteh Ashtari [39] | 2014 | Iran | cross-sectional | 271 | NR |
36.1(8) n = 173 33.6(7.9) n = 98 |
NR |
78.4(53.5) n = 173 60.4(36.8) n = 98 |
MSISQ-19 |
173 Primary SD 142 secondary SD 102 tertiary SD 120 |
NA |
| Kowsar Qaderi [40] | 2014 | Iran | Cross-sectional | 132 | NR | 36.9(8.3) | NR | NR | MSISQ-19 | 110 | NR |
| Sabine Salhofer-Polanyi [41] | 2016 | Austria | Cross-sectional | 42 | NR | 34(7) | Median 1.75 | NR | MSISQ-19 |
15 Primary SD 28 Secondary SD 17 Tertiary SD 14 |
NR |
| Hanna Pašiü [42] | 2019 | Croatia | Cross-sectional | 75 | NR | NR | NR | NR | MSISQ-15 | NR | NR |
| Stenager E [43] | 1996 | Denmark | cohort | 27 | NR | NR | NR | NR | MRD | 16 | NR |
| Marita P. McCabe [44] | 2002 | Australia | Case–control | 237 | NR | 44.45 | NR | NR | ISS | 194 | NR |
| Marita P. Mccabe [45] | 2003 | Australia | Cohort | 321 | NR | NR | NR | NR | ISS | 278 | NR |
| Cira Fraser [14] | 2008 | USA | cross-sectional | 219 | NR | 45.4(9.3) | NR | NR | Guy’s Neurological Disability Scale | 106 | NR |
| Simon Dupont [46] | 1996 | UK | Cross-sectional | 65 | NR | NR | NR | NR | GRISS | 11 | 18 |
| Vassilios Tzortzis [7] | 2008 | Greece | Cross-sectional | 63 |
RR 58 PP 5 |
33(6.4) |
mean 2.5, range 0–3.5 |
Mean 2.7 Range 19–51 |
FSFI | 22 | NR |
| Aleksandra Kołtuniuk [24] | 2020 | Poland | Cross-sectional | 101 |
RR 82 SP 14 PP 5 |
36.7(9.56) | NR | 75.1(50.2) months | FSFI | 45 | NR |
| Katharina M. Hösl [47] | 2018 | USA | Cross-sectional | 83 |
RR 76 SP 6 PP 1 |
Median 36.2 | NR | NR | FSFI | 37 | NR |
| Fatemeh Nazari [48] | 2020 | Iran | Cross-sectional | 300 |
RR 243 PMS 39 CIS 18 |
36.35(7.33) | 2.06(1.85) | 7.37(5.40) | FSFI | 209 | NR |
| Pawel Bartnik [49] | 2017 | Poland | Cross-sectional | 86 | RR 86 | 32.03(7.22) | 2.03(1.44) | 7.87(5.38) | FSFI | 21 | NR |
| Marcin Popek [50] | 2018 | Poland | case–control | 55 | NR | NR | NR | NR |
FSFI 26.24(7.22) |
22 | NR |
| Fatih Firdolas [51] | 2012 | Turkey | Cross sectional | 23 |
RR 17 SP 6 |
NR |
2(0.22) N = 17 5.91(0.53) N = 6 |
NR | FSFI | 12 | NR |
| Giulia Gava [52] | 2019 | Italy | Case–control | 153 | NR | 47.3(10.5) | 3.1(2.2) | 13.5(8.7) |
FSFI 17.9(12.7) |
64 | NR |
| Ilan Gruenwald [53] | 2007 | Israel | cross-sectional | 41 |
RR 38 SP 3 |
Median 2.5 | Median 10 | FSFI | 25 | NR | |
| Charalampos Konstantinidis [54] | 2018 | Greece | cross-sectional | 248 | NR | 45.84(8.448) | NR | 12.78(2.18) | FSFI | 160 | NR |
| Giuseppe Lombardi [55] | 2011 | Italy | Cross-sectional | 54 | NR |
Mean:34.7 (26–44) |
Mean:2.9 (1.5–6) |
Mean 8.6 (2–18) |
FSFI | 31 | NR |
| Fariba Askari [2] | 2016 | Iran | Cross-sectional | 86 |
RR 81 SP 5 |
33.4(6.5) | NR | NR | FSFI | 58 | NR |
| Khadijeh Mohammadi [56] | 2013 | Iran | cross-sectional | 226 |
RR 169 PP 4 SP 53 |
35.7(8.07) | NR | 1.8(0.79) | FSFI | 125 | NR |
| Alireza Alehashemi [57] | 2019 | Iran | case–control | 64 |
RR 60 SP 4 |
35.25(8.07) |
Mean 2 Range 0–6 |
Mean 52.5 months (ranging from 6 to 84.5) |
FSFI 22.86 (5.36) |
53 | NR |
| Ramezani, M.A [58] | 2018 | Iran | Cross-sectional | 70 | NR | NR | NR | NR | FSFI | 44 | NR |
| Jeroen R. Scheepe [59] | 2015 | Netherlands | Cross-sectional | 50 | NR | NR | NR | NR | FSFI | 16 | NR |
| Tzitzika, M [54] | 2018 | Greece |
Cross-sectional ABS |
267 | NR | NR | NR | NR | FSFI | 172 | NR |
| Julia Koehn [60] | 2014 | Germany | Cross-sectional | 82 | NR | 36.7(9.5) | NR | 69(75.1) Months |
FSFI 3.31(1.2) |
37 | NR |
| Mahsa Ghajarzadeh [11] | 2013 | Iran | Case–control | 100 |
RR 95 SP 5 |
32.8(7.6) | 5(4.8) | 13(3.1) |
FSFI 23.2(7.1) |
66 | NR |
| Volkan Solmaz, [61] | 2018 | Turkey | Case–control | 42 |
RR 34 SP 7 PP 1 |
41.9(8.06) |
Median 2.2(0–7) |
Mean range: 8.9(25–1) |
FSFI 15.84(6.33) |
40 | NR |
| E. Fragala [62] | 2015 | Italy | Cross-sectional | 75 | NR | NR | NR | NR |
FSFI median (IQR) 16.0 (2.0–25.5) |
51 | NR |
| Marian Petersen [63] | 2020 | Denmark | Cross-sectional | 180 | NR | NR | NR | NR | CSFQ | 116 | NR |
| Dilaram Billur Çelik [13] | 2013 | Turkey | Cross-sectional | 44 | NR | NR | NR | NR | ASEX | NR | NA |
| Betu¨l Kılıc [64] | 2012 | Turkey | cross-sectional | 23 | NR | Mean 39.83 (8.88) | NR | 8.09(7.29) |
Arizona Sexual Experiences Scale 17.91(5.75) |
14 | NR |
| Rocco Salvatore CalabrJ [65] | 2018 | Italy | Cross-sectional | 54 | NR | NR | NR | NR | 40-item ad hoc questionnaire | NR | 31 |
| Author | Hyporgasmia | Decrease vaginal lubrication | Change in vaginal sensation | Reduce libido | Painful intercourse | Lack of sexual desire | Partner satisfaction problems | satisfaction | Arousal Problems | T control |
Total sexual dysfunction in control |
|---|---|---|---|---|---|---|---|---|---|---|---|
| M Zorzon [12] | 17 | 25 | 19 | 22 | NR | NR | NR | NR | NR | 71 | 8 |
| M. Zorzon [20] | 25 | 25 | 28 | NR | NR | NR | NR | NR | NA | NA | |
| Kisic-Tepavcevic Darija [21] | 27 | 27 | 18 | 47 | NR | NR | NR | NR | NR | NA | NA |
| DK Tepavcevic [5] | 35 | 30 | 21 | 58 | NR | NR | NR | NR | NR | NA | NA |
| Marita P. McCabe [22] | NR | 14 | NR | NR | 1 | 21 | NR | NR | NR | NA | NA |
| Iris Zavoreo [23] | 12 | 11 | NR | NR | NR | 14 | NR | NR | NR | NA | NA |
| Aleksandra Kołtuniuk [24] | NR | NR | NR | NR | NR | NR | NR | NR | NR | ||
| M. Lew-Starowicz [25] | 54 | 66 | 65 | NR | NR | 79 | NR | NR | 62 | NA | NA |
| MW Nortvedt [26] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Sacco E [27] | NR | NR | NR | NR | 20 | 21 | NR | 29 | NR | NA | NA |
| R Vazirinejad [28] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Jing Wu [29] | 929 | 808 | NR | NR | NR | 1017 | 549 | NR | NR | NA | NA |
| Z. Tulek [30] | 35 | 28 | NR | NR | NR | 37 | 23 | NR | NR | NA | NA |
| MW Nortvedt [31] | 28 | 20 | NR | NR | NR | 25 | 18 | NR | NR | NA | NA |
| Claudia H. Marck [32] | 599 | 514 | NR | NR | NR | 695 | 238 | NR | NR | NA | NA |
| Effat Merghati-Khoei [33] | 100 | 80 | 46 | 77 | NR | NR | NR | NR | NR | NA | NA |
| Vida Ghasemi [34] | 156 | 82 | 31 | NA | NR | 966 | NR | NR | NR | NA | NA |
| Dilaram Billur Çelik [13] | 10 | 10 | NR | NR | NR | 9 | NR | NR | NR | NA | NA |
| M. Demirkiran [35] | 22 | 17 | 19 | 21 | NR | NR | NR | NR | 20 | NA | NA |
| Sarah Abdo [36] | NR | 3 | NA | 11 | NR | NR | NR | NR | NR | NA | NA |
| Edgar Carnero Contentti [37] | 55 | 44 | 27 | NR | NR | 53 | NR | NA | NA | NA | NA |
| Patrick Altmann [38] | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Fereshteh Ashtari [39] | 112 | 70 | 48 | NR | NR | 92 | NR | NR | NR | NA | NA |
| Kowsar Qaderi [40] | 83 | 67 | 38 | 64 | NR | NR | NR | NR | NR | NA | NA |
| Sabine Salhofer-Polanyi [41] | 17 | 12 | 6 | 20 | NR | NR | NR | NR | 11 | NA | NA |
| Hanna Pašiü [42] | 19 | 16 | 13 | NR | NR | 19 | 11 | NR | NR | NA | NA |
| Stenager E [43] | 3 | 4 | 6 | 15 | NR | NR | NR | NR | NR | NA | NA |
| Marita P. McCabe [44] | 101 | 78 | 81 | NR | 40 | 96 | NR | NR | 73 | 190 mean age = 44.35 years | 146 |
| Marita P. Mccabe [45] | 101 | 78 | 81 | NR | 40 | 96 | NR | NR | 73 | 239 | 191 |
| Cira Fraser [14] | NR | NR | 5 | NR | NR | 15 | 2 | NA | NA | ||
| Simon Dupont [46] | NR | NR | NR | NR | 26 | NR | NR | 7 | NR | NA | NA |
| Vassilios Tzortzis [7] | NR | NR | NR | NR | NR | NR | NR | NR | NR | 61 | 13 |
| Aleksandra Kołtuniuk [24] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Katharina M. Hösl [47] | NR | NR | NR | NR | NR | NR | NR | NR | NR | 21 | 1 |
| Fatemeh Nazari [48] | 111 | 71 | NR | NR | 51 | 116 | NR | 70 | 116 | NA | NA |
| Pawel Bartnik [49] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Marcin Popek [50] | NR | NR | NR | NR | NR | NR | NR | NR | NR |
55 29.91 (3.79) |
12 |
| Fatih Firdolas [51] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Giulia Gava [52] | NR | NR | NR | NR | NR | NR | NR | NR | NR |
153 Age:48.5(9.6) FSFI:21.1(11.2) |
24 |
| Ilan Gruenwald [53] | 22 | NR | NR | NR | 3 | 25 | NR | NR | 13 | NA | NA |
| Charalampos Konstantinidis [54] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Giuseppe Lombardi [55] | NR | NR | NR | NR | NR | 12 | NR | NR | NR | NA | NA |
| Fariba Askari [2] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Khadijeh Mohammadi [56] | 81 | 41 | 29 | 77 | 54 | 100 | NA | NA | |||
| Alireza Alehashemi [57] | NR | NR | NR | NR | NR | NR | NR | NR | NR |
64 24.39 (4.75) |
NR |
| Ramezani, M.A [58] | NR | NR | NR | NR | 36 | 21 | NR | NR | NR | NA | NA |
| Jeroen R. Scheepe [59] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Tzitzika, M [54] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Julia Koehn [60] | NR | NR | NR | NR | NR | NR | NR | NR | NR |
21 Age 36.5(11.8) FSFI: 4.5(0.7) |
1 |
| Mahsa Ghajarzadeh [11] | NR | NR | NR | NR | NR | NR | NR | NR | NR |
50 Age 31.8(8.4) FSFI: 26.8(5.2) |
NR |
| Volkan Solmaz, [61] | NR | NR | NR | NR | NR | NR | NR | NR | NR |
41 Age:39.7(7.3) FSFI:31.01(3.53) |
NR |
| E. Fragala [62] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Marian Petersen [63] | 118 | NR | NR | NR | NR | 131 | NR | 131 | 151 | NA | NA |
| Dilaram Billur Çelik [13] | 4 | 5 | NA | 5 | NR | NR | NR | 6 | 7 | NA | NA |
| Betu¨l Kılıc [64] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Rocco Salvatore CalabrJ [65] | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
Totally 8980 patients were evaluated and the total number of patients with SD was 4245.
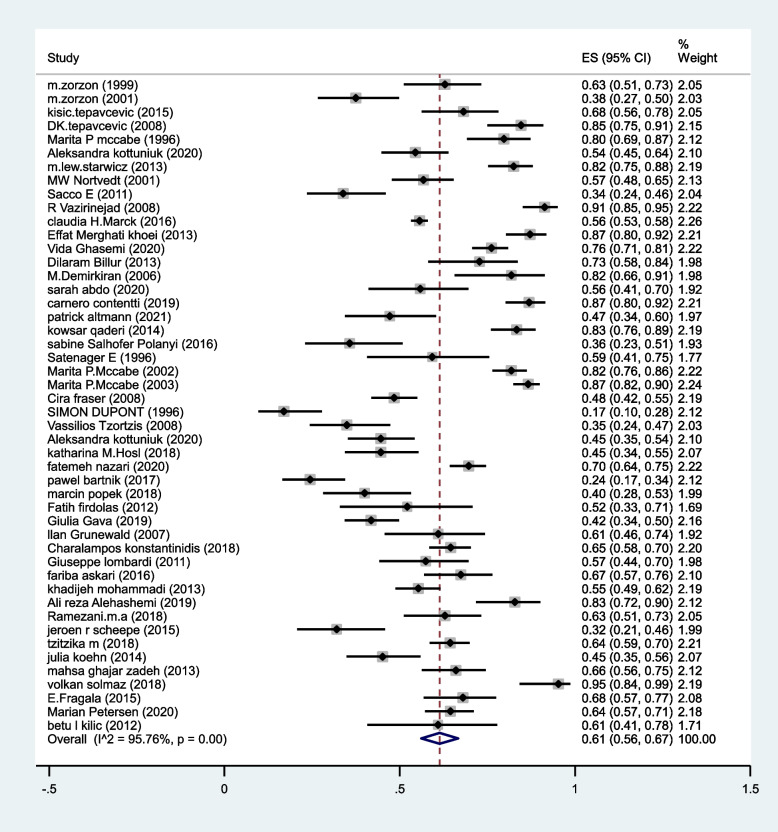
The pooled prevalence of SD in MS patients estimated as 61% (95%CI:56–67%) (I2:95.7%, P < 0.001) (Fig. 2).
Fig. 2.
The pooled prevalence of SD in MS patients
The pooled prevalence of Anorgasmia in MS patients estimated as 29% (95%CI:20–39%) (I2:85.3%, P < 0.001) (Fig. 3).
Fig. 3.
The pooled prevalence of anorgasmia in MS patients
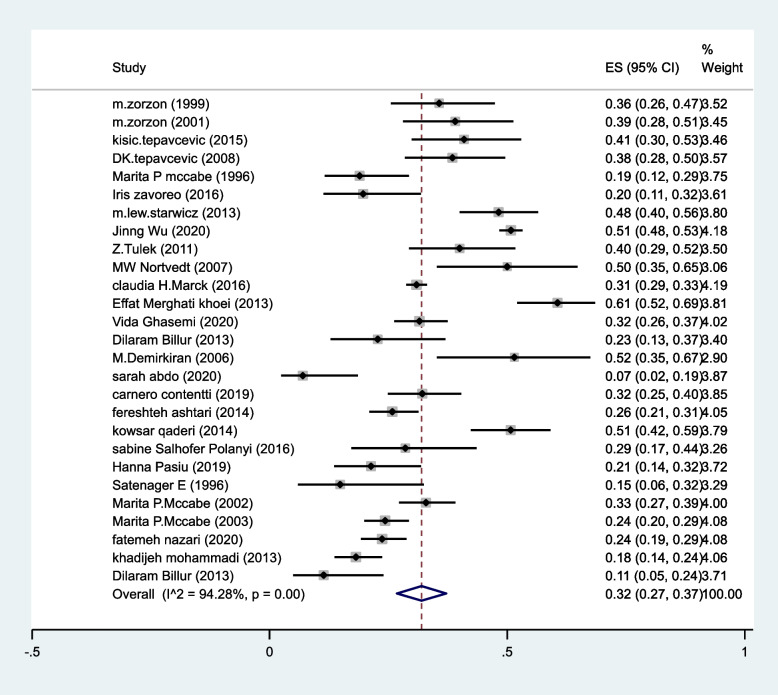
The pooled prevalence of decreased vaginal lubrication in MS patients estimated as 32%(95%CI:27–37%) (I2 = 94.2%, P < 0.001) (Fig. 4).
Fig. 4.
The pooled prevalence of decreased vaginal lubrication in MS patients
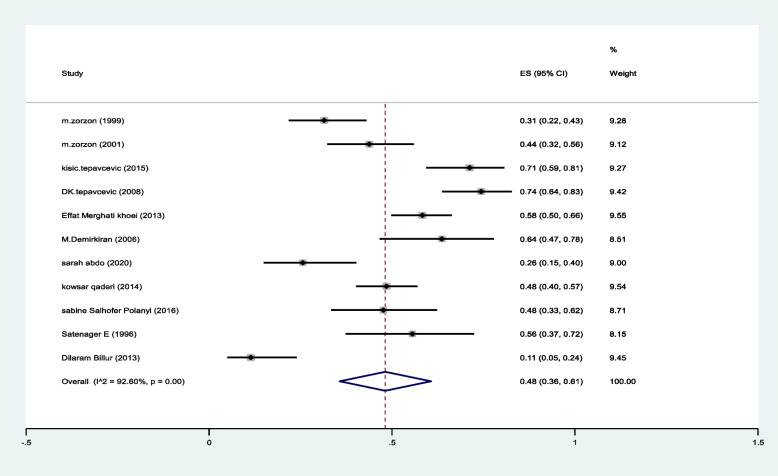
The pooled prevalence of reduced libido was 48%(95%CI:36–61%) (I2:92.6%, P < 0.001) (Fig. 5).
Fig. 5.
The pooled prevalence of reduced libido in MS patients
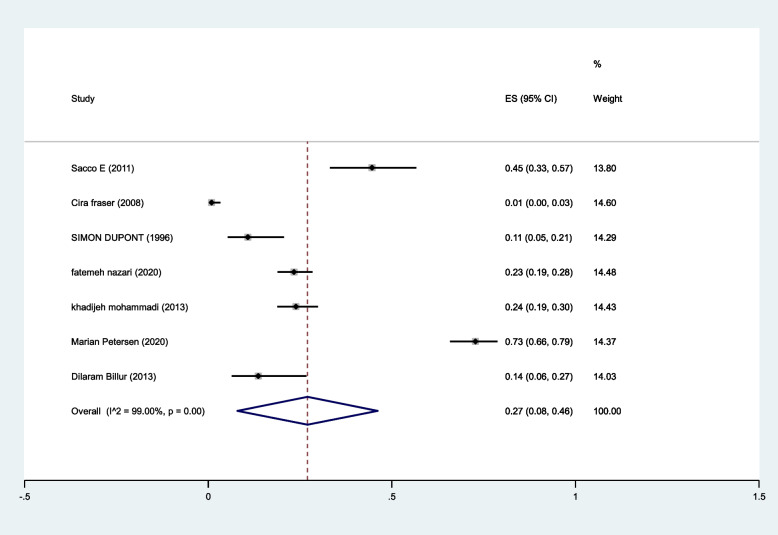
The pooled prevalence of intercourse satisfaction was 27% (95%CI: 8–46%) (I2:99%, P < 0.001) (Fig. 6).
Fig. 6.
The pooled prevalence of reduced libido in MS patients
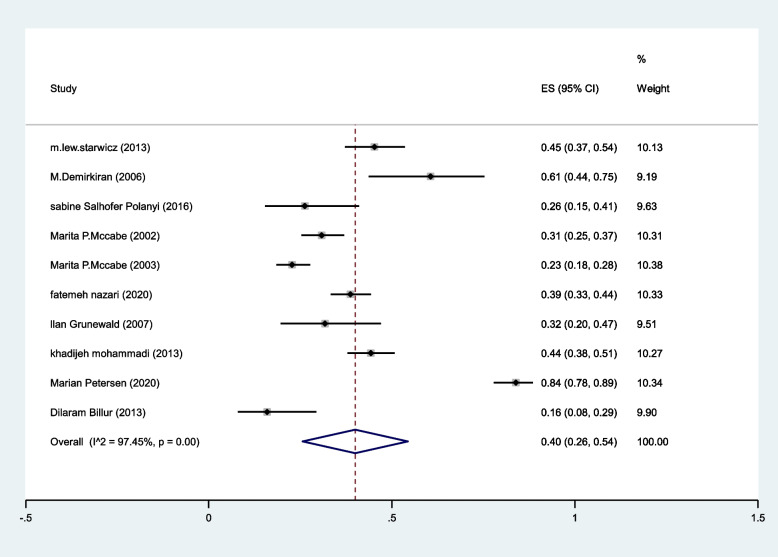
The pooled prevalence of arousal problems was 40%(95%CI: 26–54%) (I2:97.4%, P < 0.001) (Fig. 7).
Fig. 7.
The pooled prevalence of arousal problems in MS patients
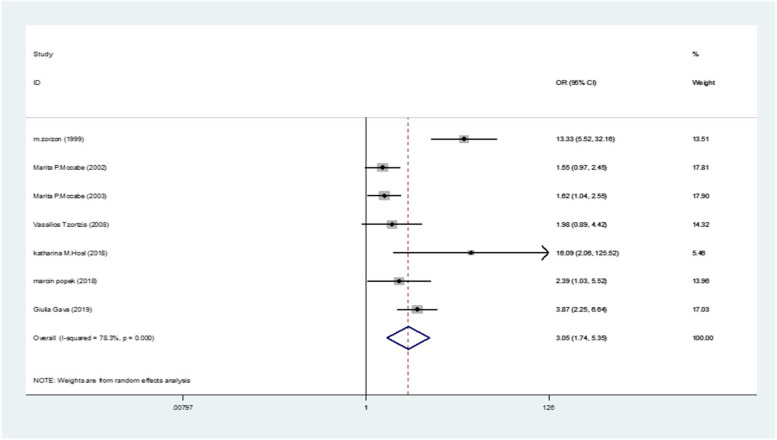
The pooled odds of developing SD in MS women estimated as 3.05(95%CI: 1.74–5.35) (I2:78.3%, P < 0.001) (Fig. 8).
Fig. 8.
The pooled odds of developing SD in women with compared to healthy controls
Discussion
MS is a neurological disease characterized by a wide range of physical, and psychological complications. The prevalence of SD in MS is near five times higher than general population [12, 66], although it is considered poorly in this population.
To our knowledge, this is the first comprehensive systematic review and meta-analysis including all related studies evaluating SD in women with MS. We included all studies which used different questionnaires. The pooled prevalence of SD was estimated as 61%, and the most common SD complaint was reduced libido (the pooled prevalence was estimated as 48%), we also found that the pooled prevalence of intercourse satisfaction was 27%.
We included all studies which applied different diagnostic tools, so out estimate would be higher than previous ones.
In a previous systematic review and meta-analysis which was conducted by Zhao et al., the relative risk (RR) of developing SD in MS women was 1.87 which shows that women with MS have 87% increased risk of developing SD [16]. They also reported lower pooled scores of desires, arousal, orgasm, satisfaction, pain, and lubrication in MS group.
In our previous systematic review, which we included only studies that applied FSFI questionnaire for evaluating SD in MS, the pooled prevalence of SD estimated as 55% [18].
In 2008, Tzorts et al. evaluated 63 women with MS using FSFI questionnaire, and reported SD in22 and reported no depression in affected cases [7].
Zorzon et al. used Szasz Sexual Functioning Scale for SD assessment and reported SD in 44 out of 70 cases. Anorgasmia or hyporgasmia followed by decreased vaginal lubrication were the most affected subscales [12].
The variation about the prevalence of SD in included studies is due to unclear definition of SD, diverse inclusion, and exclusion criteria, various diagnostic methods, no standardized tools, and cultural issues.
SD is an important issue in marital life which is ignored by most physicians and patients. It is a multi-dimensional issue which affects quality of life as well as psychological well-being. Different factors such as disease duration, disability level, psychological disorders such as depression, anxiety, and stress are considered to play role in SD development in MS while there is controversies between studies [11].
Most physicians do not pay attention to this part of their patient’s lives, and patients hesitate to talk about intimate issues.
Depression is negatively correlated with FSFI score and its subscales in a previous original study [11]. On the other hand, it is shown that depression is related with both libido reduction and arousal problems [67, 68].
In another study, higher age was associated with increased SD prevalence in MS [69] while Çelik et al. reported that SD should be evaluated in MS women at earlier stages and disease duration or disability level are not prognostic factors for developing SD [13]. Zhao et al. in their meta-analysis showed that disease duration longer than ten years, increases the risk of SD 2.5fold in MS cases [16].
Another influencing factor is bladder dysfunction in MS cases which negatively affects their sexual activity [70]. Fragala et al. investigated SD in 91% of MS women with detrusor over-activity and 66% without detrusor over-activity [62].
The association refers to S2, S3 and S4 innervation of bladder, which control sexual response [10]. On the other hand, detrusor dysfunction as a MS-related complication may reflect severe neurological disability and SD [71].
Zivadinov et al. investigated that physical disorders, depression, age at MS onset, and also neurological impairment while they reported no correlation between SD and duration of the disease [15].
Higher disability level, depression and anxiety were related with SD presence in Demirkian et al. study [72].
This systematic review has some strength. First, we included all studies which evaluated SD. Second, the number of included studies is high. Third, we analyzed all subscales of SD.
We also had some limitations. First, all included studies used various diagnostic tools. Second, there was no clear definition of SD. Third, inclusion criteria of participants differed between studies.
Conclusion
The result of this systematic review and meta-analysis show that the pooled prevalence of SD in women with MS is 61% and the odds of developing SD in comparison with controls is 3.05.
Acknowledgements
None.
Authors’ contributions
A.Y: Study design and data analysis. N.E: Data gathering and article writing. O.M: Data analysis and article writing. M.G: Methodology and article writing. All authors reviewed the manuscript.
Funding
None.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ghajarzadeh M, Foroushani AR, Ghezelbash P, Ghoreishi A, Maghbooli M, Yousefi M, et al. Prevalence of multiple sclerosis (MS) in Zanjan province of Iran. Int J Prev Med. 2020;11:116. doi: 10.4103/ijpvm.IJPVM_419_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Askari F, Ghajarzadeh M, Jalilian R, Azimi A, Togha M, Sahraian MA, et al. Comparison of sexual dysfunction in women with migraine and multiple sclerosis (MS) Maedica. 2016;11(1):44. [PMC free article] [PubMed] [Google Scholar]
- 3.Bronner G, Elran E, Golomb J, Korczyn A. Female sexuality in multiple sclerosis: the multidimensional nature of the problem and the intervention. Acta Neurol Scand. 2010;121(5):289–301. doi: 10.1111/j.1600-0404.2009.01314.x. [DOI] [PubMed] [Google Scholar]
- 4.Schairer LC, Foley FW, Zemon V, Tyry T, Campagnolo D, Marrie RA, et al. The impact of sexual dysfunction on health-related quality of life in people with multiple sclerosis. Mult Scler J. 2014;20(5):610–616. doi: 10.1177/1352458513503598. [DOI] [PubMed] [Google Scholar]
- 5.Tepavcevic D, Kostic J, Basuroski I, Stojsavljevic N, Pekmezovic T, Drulovic J. The impact of sexual dysfunction on the quality of life measured by MSQoL-54 in patients with multiple sclerosis. Mult Scler J. 2008;14(8):1131–1136. doi: 10.1177/1352458508093619. [DOI] [PubMed] [Google Scholar]
- 6.Donze C, Hautecoeur P. Urinary, sexual, and bowel disorders in early-stage multiple sclerosis. Rev Neurol. 2009;165:S148–S155. doi: 10.1016/S0035-3787(09)72127-7. [DOI] [PubMed] [Google Scholar]
- 7.Tzortzis V, Skriapas K, Hadjigeorgiou G, Mitsogiannis I, Aggelakis K, Gravas S, et al. Sexual dysfunction in newly diagnosed multiple sclerosis women. Mult Scler J. 2008;14(4):561–563. doi: 10.1177/13524585080140040901. [DOI] [PubMed] [Google Scholar]
- 8.Askari F, Ghajarzadeh M, Mohammadifar M, Azimi A, Sahraian MA, Owji M. Anxiety in patients with multiple sclerosis: association with disability, depression, disease type and sex. Acta Med Iran. 2014;52:889–92. [PubMed] [Google Scholar]
- 9.Ghajarzadeh M, Sahraian MA, Fateh R, Daneshmand A. Fatigue, depression and sleep disturbances iniranian patients with multiple sclerosis. 2012. [PubMed]
- 10.Drulovic J, Kisic-Tepavcevic D, Pekmezovic T. Epidemiology, diagnosis and management of sexual dysfunction in multiple sclerosis. Acta Neurol Belg. 2020;120:791–797. doi: 10.1007/s13760-020-01323-4. [DOI] [PubMed] [Google Scholar]
- 11.Ghajarzadeh M, Jalilian R, Mohammadifar M, Sahraian MA, Azimi A. Sexual function in women with multiple sclerosis. Acta Med Iran. 2014;52:315–8. [PubMed] [Google Scholar]
- 12.Zorzon M, Zivadinov R, Bosco A, Bragadin LM, Moretti R, Bonfigli L, et al. Sexual dysfunction in multiple sderosis: a case-control study. 1. Frequency and comparison of groups. Mult Scler J. 1999;5(6):418–27. doi: 10.1177/135245859900500i609. [DOI] [PubMed] [Google Scholar]
- 13.Çelik DB, Poyraz EÇ, Bingöl A, İdiman E, Özakbaş S, Kaya D. Sexual dysfunction ın multiple sclerosis: gender differences. J Neurol Sci. 2013;324(1–2):17–20. doi: 10.1016/j.jns.2012.08.019. [DOI] [PubMed] [Google Scholar]
- 14.Fraser C, Mahoney J, McGurl J. Correlates of sexual dysfunction in men and women with multiple sclerosis. J Neurosci Nurs. 2008;40(5):312–317. doi: 10.1097/01376517-200810000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Zivadinov R, Zorzon M, Bosco A, Bragadin LM, Moretti R, Bonfigli L, et al. Sexual dysfunction in multiple sderosis: II. Correlation analysis. Mult Scler J. 1999;5(6):428–431. doi: 10.1177/135245859900500i610. [DOI] [PubMed] [Google Scholar]
- 16.Zhao S, Wang J, Liu Y, Luo L, Zhu Z, Li E, et al. Association between multiple sclerosis and risk of female sexual dysfunction: a systematic review and meta-analysis. J Sex Med. 2018;15(12):1716–1727. doi: 10.1016/j.jsxm.2018.09.016. [DOI] [PubMed] [Google Scholar]
- 17.Polat Dunya C, Tulek Z, Uchiyama T, Haslam C, Panicker JN. Systematic review of the prevalence, symptomatology and management options of sexual dysfunction in women with multiple sclerosis. Neurourol Urodyn. 2020;39(1):83–95. doi: 10.1002/nau.24232. [DOI] [PubMed] [Google Scholar]
- 18.Azimi A, Hanaei S, Sahraian MA, Mohammadifar M, Ramagopalan SV, Ghajarzadeh M. Prevalence of sexual dysfunction in women with multiple sclerosis: a systematic review and meta-analysis. Maedica. 2019;14(4):408. doi: 10.26574/maedica.2019.14.4.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 20.Zorzon M, Zivadinov R, Bragadin LM, Moretti R, De Masi R, Nasuelli D, et al. Sexual dysfunction in multiple sclerosis: a 2-year follow-up study. J Neurol Sci. 2001;187(1–2):1–5. doi: 10.1016/S0022-510X(01)00493-2. [DOI] [PubMed] [Google Scholar]
- 21.Darija K-T, Tatjana P, Goran T, Nebojsa S, Irena D, Sarlota M, et al. Sexual dysfunction in multiple sclerosis: a 6-year follow-up study. J Neurol Sci. 2015;358(1–2):317–323. doi: 10.1016/j.jns.2015.09.023. [DOI] [PubMed] [Google Scholar]
- 22.McCabe MP, McDonald E, Deeks AA, Vowels LM, Cobain MJ. The impact of multiple sclerosis on sexuality and relationships. J Sex Res. 1996;33(3):241–248. doi: 10.1080/00224499609551840. [DOI] [Google Scholar]
- 23.Zavoreo I, Gržinčić T, Preksavec M, Madžar T, Bašić Kes V. Sexual dysfunction and incidence of depression in multiple sclerosis patients. Acta Clin Croatica. 2016;55(3):402–6. doi: 10.20471/acc.2016.55.03.08. [DOI] [PubMed] [Google Scholar]
- 24.Kołtuniuk A, Przestrzelska M, Karnas A, Rosińczuk J. The association between sexual disorders and the quality of life of woman patients with multiple sclerosis: findings of a prospective, observational, and cross-sectional survey. Sex Med. 2020;8(2):297–306. doi: 10.1016/j.esxm.2020.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lew-Starowicz M, Rola R. Prevalence of sexual dysfunctions among women with multiple sclerosis. Sex Disabil. 2013;31(2):141–153. doi: 10.1007/s11195-013-9293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nortvedt M, Riise T, Myhr K, Landtblom A-M, Bakke A, Nyland H. Reduced quality of life among multiple sclerosis patients with sexual disturbance and bladder dysfunction. Mult Scler J. 2001;7(4):231–235. doi: 10.1177/135245850100700404. [DOI] [PubMed] [Google Scholar]
- 27.Sacco E, Sebastianelli A, Batocchi AP, Pinto F, Totaro A, Volpe A, et al. Sexual dysfunctions in patients affected by multiple sclerosis: evaluation in a contemporary cohort from a referral center. 26th annual EAU congress 2011. Italy: Elsevier Science BV; 2011.
- 28.Vazirinejad R, Lilley J, Ward C. A health profile of adults with multiple sclerosis living in the community. Mult Scler J. 2008;14(8):1099–1105. doi: 10.1177/1352458508092264. [DOI] [PubMed] [Google Scholar]
- 29.Wu J, Jelinek GA, Weiland T, Hedström AK, Alfredsson L, Neate S, et al. Perceived cognitive impairment is associated with sexual dysfunction in people with multiple sclerosis: a 2.5-year follow-up study of a large international cohort. Mult Scler Relat Disord. 2020;45:102410. doi: 10.1016/j.msard.2020.102410. [DOI] [PubMed] [Google Scholar]
- 30.Tulek Z, Durna Z, Eraksoy M. Exploring sexual problems among patients with multiple sclerosis. 2011. [DOI] [PubMed]
- 31.Nortvedt M, Riise T, Frugaård J, Mohn J, Bakke A, Skår A, et al. Prevalence of bladder, bowel and sexual problems among multiple sclerosis patients two to five years after diagnosis. Mult Scler J. 2007;13(1):106–112. doi: 10.1177/1352458506071210. [DOI] [PubMed] [Google Scholar]
- 32.Marck CH, Jelinek PL, Weiland TJ, Hocking JS, De Livera AM, Taylor KL, et al. Sexual function in multiple sclerosis and associations with demographic, disease and lifestyle characteristics: an international cross-sectional study. BMC Neurol. 2016;16(1):1–9. doi: 10.1186/s12883-016-0735-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Merghati-Khoei E, Qaderi K, Amini L, Korte JE. Sexual problems among women with multiple sclerosis. J Neurol Sci. 2013;331(1–2):81–85. doi: 10.1016/j.jns.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ghasemi V, Simbar M, Ozgoli G, Nabavi SM, Majd HA. Prevalence, dimensions, and predictor factors of sexual dysfunction in women of Iran Multiple Sclerosis Society: a cross-sectional study. Neurol Sci. 2020;41(5):1105–1113. doi: 10.1007/s10072-019-04222-6. [DOI] [PubMed] [Google Scholar]
- 35.Demirkiran M, Sarica Y, Uguz S, Yerdelen D, Aslan K. Multiple sclerosis patients with and without sexual dysfunction: are there any differences? Mult Scler. 2006;12(2):209–214. doi: 10.1191/135248506ms1253oa. [DOI] [PubMed] [Google Scholar]
- 36.Abdo S, Adly M, Elmehdawy K, Alfaqeeh A, Hamdy S, Naseer MA, et al. Sexual dysfunction in women with early multiple sclerosis. Management. 2020;4:4. [Google Scholar]
- 37.Contentti EC, Pettinicchi JP, Caride A, López PA. Sexual dysfunction in patients with multiple sclerosis from Argentina: what are the differences between women and men? Sex Disabil. 2019;37(4):521–539. doi: 10.1007/s11195-019-09603-5. [DOI] [Google Scholar]
- 38.Altmann P, Leutmezer F, Leithner K, Monschein T, Ponleitner M, Stattmann M, et al. Predisposing factors for sexual dysfunction in multiple sclerosis. Front Neurol. 2021;12:618370. doi: 10.3389/fneur.2021.618370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ashtari F, Rezvani R, Afshar H. Sexual dysfunction in women with multiple sclerosis: dimensions and contributory factors. J Res Med Sci. 2014;19(3):228. [PMC free article] [PubMed] [Google Scholar]
- 40.Qaderi K, Khoei EM. Sexual problems and quality of life in women with multiple sclerosis. Sex Disabil. 2014;32(1):35–43. doi: 10.1007/s11195-013-9318-4. [DOI] [Google Scholar]
- 41.Salhofer-Polanyi S, Wöber C, Prohazka R, Dal-Bianco A, Bajer-Kornek B, Zebenholzer K. Similar impact of multiple sclerosis and migraine on sexual function in women. Wien Klin Wochenschr. 2017;129(3–4):115–120. doi: 10.1007/s00508-016-1066-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pašiü H, Vujeviü L, Pašiü MB, Mustaþ F, Rajiþ F, Vidrih B, et al. Sexual dysfunction and depression in patients with multiple sclerosis in Croatia. Psychiatr Danub. 2019;31(5):S831–S838. [PubMed] [Google Scholar]
- 43.Stenager E, Stenager E, Jensen K. Sexual function in multiple sclerosis. A 5-year follow-up study. Italian J Neurol Sci. 1996;17(1):67–9. doi: 10.1007/BF01995711. [DOI] [PubMed] [Google Scholar]
- 44.McCabe MP. Relationship functioning and sexuality among people with multiple sclerosis. J Sex Res. 2002;39(4):302–309. doi: 10.1080/00224490209552154. [DOI] [PubMed] [Google Scholar]
- 45.McCabe MP, McKern S, McDonald E, Vowels LM. Changes over time in sexual and relationship functioning of people with multiple sclerosis. J Sex Marital Ther. 2003;29(4):305–321. doi: 10.1080/00926230390195506-2372. [DOI] [PubMed] [Google Scholar]
- 46.Dupont S. Sexual function and ways of coping in patients with multiple sclerosis and their partners. Sex Marital Ther. 1996;11(4):359–372. doi: 10.1080/02674659608404450. [DOI] [Google Scholar]
- 47.Hösl KM, Deutsch M, Wang R, Roy S, Winder K, Niklewski G, et al. Sexual dysfunction seems to trigger depression in female multiple sclerosis patients. Eur Neurol. 2018;80(1–2):34–41. doi: 10.1159/000492126. [DOI] [PubMed] [Google Scholar]
- 48.Nazari F, Shaygannejad V, Mohammadi Sichani M, Mansourian M, Hajhashemi V. Sexual dysfunction in women with multiple sclerosis: prevalence and impact on quality of life. BMC Urol. 2020;20(1):1–10. doi: 10.1186/s12894-020-0581-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bartnik P, Wielgoś A, Kacperczyk J, Pisarz K, Szymusik I, Podlecka-Piętowska A, et al. Sexual dysfunction in female patients with relapsing-remitting multiple sclerosis. Brain Behav. 2017;7(6):e00699. doi: 10.1002/brb3.699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Popek M, Grabowska-Popek A, Mitosek-Szewczyk K, Stelmasiak Z. Is multiple sclerosis only a neurological problem? Evaluation of sexual dysfunctions in a group of multiple sclerosis patients. Med Studies/Stud Med. 2018;34(2):127–132. [Google Scholar]
- 51.Firdolas F, Ozan T, Onur R, Bulut S, Orhan I. Evaluation of sexual function in women at two stages of multiple sclerosis. World J Urol. 2013;31(4):929–933. doi: 10.1007/s00345-012-0891-4. [DOI] [PubMed] [Google Scholar]
- 52.Gava G, Visconti M, Salvi F, Bartolomei I, Seracchioli R, Meriggiola MC. Prevalence and psychopathological determinants of sexual dysfunction and related distress in women with and without multiple sclerosis. J Sex Med. 2019;16(6):833–842. doi: 10.1016/j.jsxm.2019.03.011. [DOI] [PubMed] [Google Scholar]
- 53.Gruenwald I, Vardi Y, Gartman I, Juven E, Sprecher E, Yarnitsky D, et al. Sexual dysfunction in females with multiple sclerosis: quantitative sensory testing. Mult Scler J. 2007;13(1):95–105. doi: 10.1177/1352458506071134. [DOI] [PubMed] [Google Scholar]
- 54.Konstantinidis C, Tzitzika M, Bantis A, Nikolia A, Samarinas M, Kratiras Z, et al. Female sexual dysfunction among Greek women with multiple sclerosis: correlations with organic and psychological factors. Sex Med. 2019;7(1):19–25. doi: 10.1016/j.esxm.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lombardi G, Celso M, Bartelli M, Cilotti A, Del Popolo G. Female sexual dysfunction and hormonal status in multiple sclerosis patients. J Sex Med. 2011;8(4):1138–1146. doi: 10.1111/j.1743-6109.2010.02161.x. [DOI] [PubMed] [Google Scholar]
- 56.Mohammadi K, Rahnama P, Mohseni SM, Sahraian MA, Montazeri A. Determinants of sexual dysfunction in women with multiple sclerosis. BMC Neurol. 2013;13(1):1–6. doi: 10.1186/1471-2377-13-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alehashemi A, Mostafavian Z, Dareini N. Sexual function in Iranian female multiple sclerosis patients. Open Access Maced J Med Sci. 2019;7(8):1303. doi: 10.3889/oamjms.2019.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ramezani M, Hajiseyedsadeghi M, Ghaemmaghami A. 236 Sexual dysfunction and marital satisfaction in multiple sclerosis. J Sex Med. 2018;15(7):S215. doi: 10.1016/j.jsxm.2018.04.200. [DOI] [Google Scholar]
- 59.Scheepe JR, Alamyar M, Pastoor H, Hintzen RQ, Blok BF. Female sexual dysfunction in multiple sclerosis: Results of a survey among Dutch urologists and patients. Neurourol Urodyn. 2017;36(1):116–120. doi: 10.1002/nau.22884. [DOI] [PubMed] [Google Scholar]
- 60.Koehn J, Linker R, Intravooth T, Crodel C, Deutsch M, Lee D-H, et al. Multiple Sclerosis Compromises Various Aspects of Female Sexual Function (P6. 166). Germany: AAN Enterprises; 2014.
- 61.Solmaz V, Ozlece HK, Him A, Güneş A, Cordano C, Aksoy D, et al. Evaluation of the association between sexual dysfunction and demyelinating plaque location and number in female multiple sclerosis patients. Neurol Res. 2018;40(8):683–688. doi: 10.1080/01616412.2018.1462752. [DOI] [PubMed] [Google Scholar]
- 62.Fragala E, Russo G, Di Rosa A, Giardina R, Privitera S, Favilla V, et al. Relationship between urodynamic findings and sexual function in multiple sclerosis patients with lower urinary tract dysfunction. Eur J Neurol. 2015;22(3):485–492. doi: 10.1111/ene.12595. [DOI] [PubMed] [Google Scholar]
- 63.Petersen M, Kristensen E, Giraldi L, Giraldi A. Sexual dysfunction and mental health in patients with multiple sclerosis and epilepsy. BMC Neurol. 2020;20(1):1–9. doi: 10.1186/s12883-020-1625-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kılıc B, Unver V, Bolu A, Demirkaya S. Sexual dysfunction and coping strategies in multiple sclerosis patients. Sex Disabil. 2012;30(1):3–13. doi: 10.1007/s11195-011-9243-3. [DOI] [Google Scholar]
- 65.Calabrò RS, Russo M, Dattola V, De Luca R, Leo A, Grisolaghi J, et al. Sexual function in young individuals with multiple sclerosis: does disability matter? J Neurosci Nurs. 2018;50(3):161–166. doi: 10.1097/JNN.0000000000000367. [DOI] [PubMed] [Google Scholar]
- 66.Rees PM, Fowler CJ, Maas CP. Sexual function in men and women with neurological disorders. Lancet. 2007;369(9560):512–525. doi: 10.1016/S0140-6736(07)60238-4. [DOI] [PubMed] [Google Scholar]
- 67.Angst J. Sexual problems in healthy and depressed persons. Int Clin Psychopharmacol. 1998;13 Suppl 6:S1–4. doi: 10.1097/00004850-199807006-00001. [DOI] [PubMed] [Google Scholar]
- 68.Casper RC, Redmond DE, Katz MM, Schaffer CB, Davis JM, Koslow SH. Somatic symptoms in primary affective disorder: presence and relationship to the classification of depression. Arch Gen Psychiatry. 1985;42(11):1098–1104. doi: 10.1001/archpsyc.1985.01790340082012. [DOI] [PubMed] [Google Scholar]
- 69.Timkova V, Mikula P, Linkova M, Szilasiova J, Nagyova I. Sexual functioning in patients with multiple sclerosis and its association with social support and self-esteem. Psychol Health Med. 2021;26(8):980–990. doi: 10.1080/13548506.2020.1800054. [DOI] [PubMed] [Google Scholar]
- 70.DasGupta R, Fowler CJ. Sexual and urological dysfunction in multiple sclerosis: better understanding and improved therapies. Curr Opin Neurol. 2002;15(3):271–278. doi: 10.1097/00019052-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 71.Fragalà E, Privitera S, Giardina R, Di Rosa A, Russo GI, Favilla V, et al. Determinants of sexual impairment in multiple sclerosis in male and female patients with lower urinary tract dysfunction: results from an Italian cross-sectional study. J Sex Med. 2014;11(10):2406–2413. doi: 10.1111/jsm.12635. [DOI] [PubMed] [Google Scholar]
- 72.Demirkiran M, Sarica Y, Uguz S, Yerdelen D, Aslan K. Multiple sclerosis patients with and without sexual dysfunction: are there any differences? Mult Scler J. 2006;12(2):209–211. doi: 10.1191/135248506ms1253oa. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.