Background
In this issue of the Journal, Tian and colleagues confirmed the J-shaped relationship between alcohol consumption and health based on analyzing 918,529 adults from the repeated National Health Interview Survey (NHIS) from 1997 to 2014 [1]. In addition to several cause-specific mortality, Tian and colleagues’ findings are largely confirmatory to previous studies using NHIS [2, 3] and several large systematic review and meta-analysis on this issue [4–6].
The “J-shaped” relationship refers to a protective health effect at a lower level of consumption; while above a certain threshold, it greatly increases health risks. This study found that compared with lifetime abstainers, current infrequent, light, and moderate drinkers had a lower risk of all-cause mortality (current infrequent: − 13%; light: − 23%; moderate: − 18%) and cardio-vascular disease mortality (infrequent: − 14%; light: − 24%; moderate: − 22%), respectively. However, it is important to address several methodological issues when interpreting the J-shaped association.
Main text
Firstly, the issue of misclassification must be considered, which pertains to the exclusion of “sick quitters” or the “abstainer bias” from the definition of the reference group [7]. In order to mitigate this error, some studies have attempted to define the reference group as lifetime abstainers, while excluding ex-drinkers, as done by Tian et al. [1]. However, also using lifetime nondrinkers as reference, an updated systematic review and meta-analysis of 107 cohort studies with near half million participants concluded that the low-volume alcohol drinking was not associated with protection against death from all causes [8].
Secondly, other likely biases included the potentials for reverse causation, a possibility that individuals who are already in poor health may be more likely to be abstainers and individuals with high health conscious and in good shape also tends to be more reasonable drinkers, which could lead to better health. In addition, in the Western societies where most J-shape studies derived from, it is possible that light to moderate drinking may be associated with active social and family life, higher socioeconomic status, healthier lifestyle choices, and access to better healthcare, which may independently contribute to better health outcomes.
Thirdly, alcohol can be addictive, and even moderate consumption can lead to dependence and addiction in susceptible individuals. Therefore, promoting even moderate alcohol consumption based on a J-shaped relationship may send mixed messages and result in increased alcohol consumption, leading to negative population health outcomes.
Fourthly, it seems that when determining what constitutes as an optimal level of alcohol consumption, in epidemiological terms, theoretical minimal exposure level (THML) varies significantly among individuals and disease burden across different regions [9, 10]. For instance, for young population age, it is close to zero consumption while the potential beneficial effect particularly with respect to cardiovascular disease maybe more salient in older age groups and geographic locations where CVD burden are high.
Fifthly, the standard of alcohol consumption is also challenging for drinkers to adhere to, and the impact of different drinking amounts on average life expectancy has been studied previously [11]. The findings revealed that the benefits of moderate drinking were negated by a two to fourfold increase in oral and esophageal cancer risk, and excessive drinking resulted in a significant reduction in life expectancy. Therefore, the threshold for safe alcohol consumption is often ambiguous.
It is challenging to tease out the direct effects of alcohol consumption from these biases and confounding factors in observational studies. However, these inconsistent findings may be resolved by some methodological advancement. To address causal questions in observational studies, Mendelian randomization has been used, and it was found that it is not possible to draw conclusion on the causal role of moderate drinking and cardio-metabolic health [12]. The same conclusion has been drawn from a genetic epidemiological study which shows that the apparently protective effects of moderate alcohol intake against stroke are largely non-causal [13]. This year (2023), the World Health Organization (WHO) published a statement indicating that “when it comes to alcohol consumption, there is no safe amount that does not affect health” [14] and alcohol is responsible for 3 million deaths in 2016 globally and 5.1% of the global burden of disease and injury estimated by the WHO [15]. The updated guidance on alcohol health in Canada also presented a continuum of risk and stated that “Drinking less is better” [16].
Conclusion
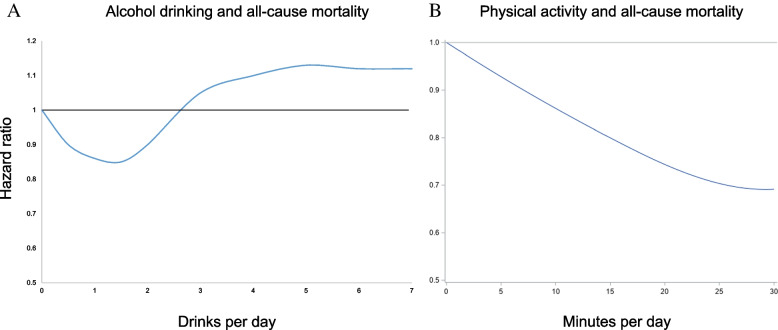
In conclusion, while some studies have suggested a J-shaped relationship, there are limitations in the study design, confounding factors, and individual variability that challenge the generalizability and interpretation of these findings. More recent studies with advanced methodological designs have challenged the J-shape association. It is also important to consider societal/population-level harmful effects of alcohol use and alternative health-promoting strategies when evaluating the implications of the J-shaped relationship. Here, we provide relative risk curve of physical activity in comparison to a debated typical J-shaped for life-time abstainer (Fig. 1). In contrast to less is more in alcohol use; many alternative healthy lifestyle choices mean more is merrier.
Fig. 1.
Relative risk curve of physical activity in comparison to a disputed typical J-shaped risk for alcohol drinking. Individuals who engage in 15–20 min of physical activity per day experience a similar level of reduced mortality as in the debated J-shaped association between moderate drinking and health. Figure 1A data source is from Tian et al. study [1]. Figure 1B data source is from our previous cohort study [17]
Acknowledgements
The data used in this research was authorized by MJ Health Research Foundation (Authorization Code: MJHRFB2014001C). The study design, data collection, data analysis, data interpretation, writing of the report, and submission for publication were independently decided by the authors and had no relation to the funding source. We are grateful to the Health and Welfare Data Science Center and National Health Research Institutes for providing administrative and technical support.
Authors’ contributions
MKT and WG drafted the article, analyzed the data, constructed the figure, and submitted it for publication. All authors read and approved the final manuscript.
Funding
Wayne Gao has received research funding from the following: TMU110-AE1-B06 and TMU1106216-003-111 from Taipei Medical University, MOST111-2314-B-038-044 from the Ministry of Science and Technology Taiwan, and DP2-111-21121-01-O-12 from the Ministry of Education Taiwan. The funding source had no role in the study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to submit the paper for publication.
Availability of data and materials
The MJ Health Research Foundation administered MJ Health Survey Database and MJ BioData. Data will be shared on request to the corresponding author with permission of MJ Health Research Foundation.
Declarations
Ethics approval and consent to participate
Ethical reviews for this study were approved by the China Medical University.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Reference
- 1.Tian Y, Liu J, Zhao Y, Jiang N, Liu X, Zhao G, et al. Alcohol consumption and all-cause and cause-specific mortality among U.S. adults. BMC Med. 2023. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-02907-6. [DOI] [PMC free article] [PubMed]
- 2.Mukamal KJ, Chen CM, Rao SR, Breslow RA. Alcohol consumption and cardiovascular mortality among US adults, 1987 to 2002. J Am Coll Cardiol. 2010;55:1328–35. doi: 10.1016/j.jacc.2009.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xi B, Veeranki SP, Zhao M, Ma CW, Yan YK, Mi J. Relationship of alcohol consumption to all-cause, cardiovascular, and cancer-related mortality in US adults. J Am Coll Cardiol. 2017;70:913–22. doi: 10.1016/j.jacc.2017.06.054. [DOI] [PubMed] [Google Scholar]
- 4.Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bergmann MM, Rehm J, Klipstein-Grobusch K, Boeing H, Schütze M, Drogan D, et al. The association of pattern of lifetime alcohol use and cause of death in the European prospective investigation into cancer and nutrition (EPIC) study. Int J Epidemiol. 2013;42:1772–90. doi: 10.1093/ije/dyt154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Castelnuovo A, Costanzo S, Bagnardi V, Donati MB, Iacoviello L, de Gaetano G. Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med. 2006;166:2437–45. doi: 10.1001/archinte.166.22.2437. [DOI] [PubMed] [Google Scholar]
- 7.Klatsky AL. Alcohol and cardiovascular mortality: common sense and scientific truth. J Am Coll Cardiol. 2010;55:1336–8. doi: 10.1016/j.jacc.2009.10.057. [DOI] [PubMed] [Google Scholar]
- 8.Zhao J, Stockwell T, Naimi T, Churchill S, Clay J, Sherk A. Association between daily alcohol intake and risk of all-cause mortality: a systematic review and meta-analyses. JAMA Netw Open. 2023;6:e236185-e. doi: 10.1001/jamanetworkopen.2023.6185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.G. B. D. Alcohol Collaborators Alcohol use and burden for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392:1015–35. doi: 10.1016/S0140-6736(18)31310-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.G. B. D. Alcohol Collaborators Population-level risks of alcohol consumption by amount, geography, age, sex, and year: a systematic analysis for the Global Burden of Disease Study 2020. Lancet. 2022;400:185–235. doi: 10.1016/S0140-6736(22)00847-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu YT, Lee JH, Tsai MK, Wei JC, Wen CP. The effects of modest drinking on life expectancy and mortality risks: a population-based cohort study. Sci Rep. 2022;12:7476. doi: 10.1038/s41598-022-11427-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van de Luitgaarden IAT, van Oort S, Bouman EJ, Schoonmade LJ, Schrieks IC, Grobbee DE, et al. Alcohol consumption in relation to cardiovascular diseases and mortality: a systematic review of Mendelian randomization studies. Eur J Epidemiol. 2022;37:655–69. doi: 10.1007/s10654-021-00799-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Millwood IY, Walters RG, Mei XW, Guo Y, Yang L, Bian Z, et al. Conventional and genetic evidence on alcohol and vascular disease aetiology: a prospective study of 500 000 men and women in China. Lancet. 2019;393:1831–42. doi: 10.1016/S0140-6736(18)31772-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson BO, Berdzuli N, Ilbawi A, Kestel D, Kluge HP, Krech R, et al. Health and cancer risks associated with low levels of alcohol consumption. Lancet Public Health. 2023;8:e6–e7. doi: 10.1016/S2468-2667(22)00317-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Alcohol 2023 [Cited 2023 May 24]. Available from: https://www.who.int/health-topics/alcohol#tab=tab_1.
- 16.Paradis C, Butt P, Shield K, Poole N, Wells S, Naimi T, et al. Canada’s Guidance on Alcohol and Health: Final Report Ottawa, Ont.: Canadian Centre on Substance Use and Addiction; 2023 [Cited 2023 May 24]. Available from: https://ccsa.ca/canadas-guidance-alcohol-and-health-final-report.
- 17.Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, et al. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet. 2011;378:1244–53. doi: 10.1016/S0140-6736(11)60749-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The MJ Health Research Foundation administered MJ Health Survey Database and MJ BioData. Data will be shared on request to the corresponding author with permission of MJ Health Research Foundation.