Abstract
Background
Sensitive and reproducible detection of residual disease after treatment is a major challenge for patients with locally advanced head and neck cancer. Indeed, the current imaging techniques are not always reliable enough to determine the presence of residual disease. The aim of the NeckTAR trial is to assess the ability of circulating DNA (cDNA), both tumoral and viral, at three months post-treatment, to predict residual disease, at the time of the neck dissection, among patients with partial cervical lymph node response on PET-CT, after potentiated radiotherapy.
Methods
This will be an interventional, multicentre, single-arm, open-label, prospective study. A blood sample will be screened for cDNA before potentiated radiotherapy and after 3 months if adenomegaly persists on the CT scan 3 months after the end of treatment. Patients will be enrolled in 4 sites in France. Evaluable patients, i.e. those with presence of cDNA at inclusion, an indication for neck dissection, and a blood sample at M3, will be followed for 30 months. Thirty-two evaluable patients are expected to be recruited in the study.
Discussion
The decision to perform neck dissection in case of persistent cervical adenopathy after radio-chemotherapy for locally advanced head and neck cancer is not always straightforward. Although studies have shown that circulating tumour DNA is detectable in a large proportion of patients with head and neck cancer, enabling the monitoring of response, the current data is insufficient to allow routine use of this marker. Our study could lead to better identification of patients who do not have residual lymph node disease in order to avoid neck dissection and preserve their quality-of-life while maintaining their prospects of survival.
Trial registration
Clinicaltrials.gov: NCT05710679, registered on 02/02/2023, https://clinicaltrials.gov/ct2/show/. Identifier with the French National Agency for the Safety of Medicines and Health Products (ANSM): N°ID RCB 2022-A01668-35, registered on July 15th, 2022.
Keywords: Head and neck cancer, Potentiated radiotherapy, Residual disease, Circulating DNA, HPV-HR
Background
With about 600 000 new cases per year, head and neck cancers (HNC) rank in 6th position among the most common malignancies worldwide [1, 2]. More than half of the patients present a locally advanced stage at diagnosis [3]. The main risk factors for developing HNC are tobacco and alcohol consumption. High-risk papillomavirus (HPV) infection is also a cause of HNC, particularly for oropharynx cancer [4–6]. Despite treatment, 30 to 50% of patients relapse within 2 years and median survival does not then exceed one year [7–9]. The standard treatments for HNC are radiotherapy, surgery and chemotherapy [6].
Post-treatment follow-up of patients requires, among other things, a thorough clinical examination and repeated imagery investigations. The main difficulty lies in the interpretation of the results of these examinations as a result of post-operative and post-radiation changes that are difficult to distinguish from residual or recurrent tumour [10, 11].
The persistence of residual disease at the end of radiotherapy treatment is a major prognostic issue. 18F-fluorodeoxyglucose (FDG) positron emission tomography-computed tomography (PET-CT)-guided surveillance, with a negative predictive value of 95–97%, has proven to be non-inferior to cervical curage in CETEC with residual adenomegaly after radio-chemotherapy [12, 13]. Cervical curage is now indicated only if the response assessed by PET-CT is only partial. Nevertheless, the ability of PET-CT to predict residual disease is unsatisfactory because of a high frequency of false positives, due to inflammatory remodelling, with a positive predictive value of about 20–50% [14].
Currently, up to 50% of patients have residual adenomegaly after treatment, and only 30% have viable disease at the time of neck dissection [15, 16]. However, the acute and late complications to which patients who have undergone adenectomy are exposed are not negligible and can damage their quality-of-life (haemorrhage, scar disunion, alteration of swallowing function, etc.) [17–19].
Sensitive and reproducible detection of residual disease after treatment is a major issue for these patients. This is the context of our study, which aims to evaluate the prediction of residual disease using circulating DNA detection after potentiated radiotherapy for locally advanced head and neck cancer.
Methods/design
Study design
This interventional study is designed as a multicentre, single-arm, open-label, prospective study. The study has been registered on Clinicaltrials.gov (NCT05710679, 02/02/2023).
We expect to enrol 32 evaluable patients, i.e. with an indication for neck dissection and a blood sample at M3, to meet the primary objective. The enrolment period is expected to be 36 months. Each patient will be followed until two years after radiotherapy, reaching a total of 30 months.
Coordination and participating institutions
The Centre Jean PERRIN (Clermont-Ferrand, France) sponsors the NeckTAR trial and is responsible for coordination, trial management, data management and trial monitoring.
This multicentre study is currently being conducted in 4 sites in France. The list of the study sites is available on https://clinicaltrials.gov/ct2/show/NCT05710679.
Study objectives and endpoints
Primary objectives and endpoint
The primary objective of the study is to assess, at three months post-treatment, the ability of cDNA, tumoral and viral, to predict residual disease at the time of neck dissection among patients with partial cervical lymph node response after potentiated radiotherapy.
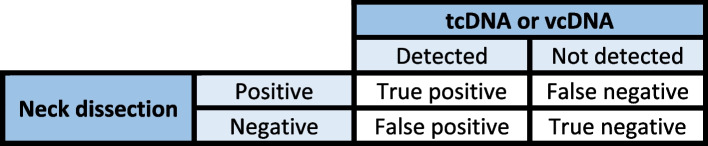
All patients with an indication for neck dissection will provide a blood sample for cDNA testing. To conclude on the diagnostic performance of post-treatment cDNA detection, we will compare the presence or absence of cDNA in the blood sample and the presence or absence of residual disease at the time of neck dissection (Fig. 1).
Fig. 1.
Confusion diagram
Secondary objectives and endpoints
Assessment of the cDNA detection rate among patients with residual adenomegaly after treatment. This will be evaluated according to cDNA detection and response on CT-scan.
Assessment of the relationship between cDNA detection and metabolic lymph node response on PET scan after treatment among patients with residual adenomegaly. This endpoint will be evaluated according to cDNA detection and objective metabolic response at three months after potentiated radiotherapy.
Assessment of the prognostic value of cDNA detection 3 months after the end of potentiated radiotherapy for patients with residual adenomegaly. This endpoint will be evaluated using overall survival and progression-free survival.
Assessment of the prognosis value of the presence of residual adenomegaly. This will be evaluated using overall survival and progression-free survival.
Assessment of the concordance of mutational profiles and HPV-HR genotypes between the primary tumour and cDNA at diagnosis. This endpoint will be evaluated on the basis of the mutational profiles from FFPE blocks and the inclusion blood sample.
Assessment of concordance between p16 immunohistochemistry and HPV-HR genotyping on the primary tumour.
Test of the concordance between real-time PCR and NGS on FFPE blocks for simultaneous detection and genotyping of HPV-HR at diagnosis.
Assessment of the relationship between ctDNA and cvDNA detection at diagnosis and the clinical, paraclinical and pathological features of the cancer.
Assessment of inter-observer reproducibility of the interpretation of SUVmax measures of residual cervical adenomegaly. A centralized review of the initial and three months post-treatment PET-CT will be performed by the sponsor’s nuclear medicine department.
Participant eligibility
The exhaustive list of selection criteria is presented in Table 1. Patients with a recent diagnosis of locally-advanced head and neck cancer with lymph node involvement and never previously treated and for whom potentiated radiotherapy is indicated are eligible. After the signature of informed consent, a blood sample will be taken (2 tubes of 9 mL) and a FPPE block (from the tumour or a lymph node biopsy) will be recovered and sent to the sponsor. Centralized analyses will be conducted to identify specific tumour mutations on FFPE blocks and to search for the presence of cDNA in the blood sample. Patients for whom neither specific tumour mutations nor cDNA is found will be considered as screening failures.
Table 1.
Selection criteria
| Inclusion criteria | Non-inclusion criteria |
|---|---|
| Age ≥ 18 and ≤ 80 years old | Tumor of the nasopharynx, sinuses, nasal cavity, salivary glands or thyroid cancer |
| Epidermoïd carcinoma histologically confirmed, never treated, with lymph node envolvment | Treatment with radiotherapy only |
| Stage III (N1), stage IVa (minimum N1) or IVb, resectable but not operated or unresectable, with potentiated radiotherapy indication | Contraindication for neck dissection |
| Oral cavity, oropharynx, hypopharynx or larynx, cervical adenopathies without a primitive | Metastatic disease (stage IVc) |
| Tumoral sample FFPE available before the treatment initiation | History of treatment for a head and neck cancer |
| Presence of cDNA in the initial blood sample | History of other cancer within 3 years (except carcinoma in situ, basal cell skin carcinoma, localized prostate cancer Gleason 6) |
| Tumor-specific variant detected on FFPE and leucocytes | Pregnant or breastfeeding woman |
| Written informed consent signed | Patient under guardianship or curatorship |
| Affiliation to the French social security system | Psychological disorder (cognitive disorders, mental alertness, etc.) or social (deprivation of liberty by judicial or administrative decision) or geographical reasons that may compromise medical monitoring of the trial or compliance with treatment |
Blood sample for cDNA research
Each participant will provide a blood sample at inclusion, before the initiation of potentiated radiotherapy. Then, at the three-month evaluation of the disease, a second blood sample will be collected for the patients with residual lymph nodes on the scan.
After DNA extraction, a specific panel, defined previously and including the main mutation of head and neck cancer and HPV, will be applied to each of the samples to search for specific HNC mutations on ctDNA.
Study procedures and participant timeline
A SPIRIT flow diagram gives an overview of the study procedures (Table 2). After the inclusion visit, patients will be monitored twice during potentiated radiotherapy: at the beginning and at the end of radiotherapy. A visit is then planned three months after the end of radiotherapy. The other follow-up visits will be carried out every 6 months (M9, M15, M21, M27). The diagrammatic illustration of the study is presented in Fig. 2.
Table 2.
Spirit flow diagram
| Potentiated radiotherapy | Follow-up visits | |||||||
|---|---|---|---|---|---|---|---|---|
| Assessment | Baseline | W1 | W7 | M3 | M9 | M15 | M21 | M27 |
| Day | -30 à 0 | 0 à 7 | 42 à 49 | |||||
| Medical history | x | |||||||
| Clinical examination | x | x | x | x | x | x | x | x |
| Blood sample for cDNA research | x | xa | ||||||
| Cervico-thoracic scan | x | x | x | x | x | x | ||
| PET-CT scan | x | xa | ||||||
| Histological examination of the tumor or a lymph node | x | |||||||
| Mutation profiling by NGS on FFPE, plasma and leukocytes | x | |||||||
| p16 immunohistochemistry on FFPE | x | |||||||
| HR-HPV genotyping by real-time PCR on FFPE | x | |||||||
| HR-HPV genotyping by NGS on FFPE | x | |||||||
| Doses received, fractionation for radiotherapy | x | |||||||
| Data on the potentiating treatment received | x | |||||||
W Week, M Month, FFPE Formol fixed paraffine embedded, PET-CT positon-emission tomography computed-tomography, cDNA circulating DNA, PCR Polymerase chain reaction, HR-HPV High risk human papilloma virus
aIn case of residual cervical adenomegaly at cervico-thoracic scan
Fig. 2.
Scheme of the study
Statistical analysis
Sample size calculations
Since the negative predictive value (NPV) of PET-CT to detect residual nodal disease in the context of our study is known to be very good (95–97%), we choose to focus on the group of patients with an indication for salvage adenectomy. The detection of ct/cvDNA should enable the identification of patients for whom this adenectomy is indeed necessary. This question means assessing the positive predictive value (PPV) of the ct/cvDNA predictor (detectable versus non-detectable) in relation to the lymph node dissection result (positive versus negative). For sample size determination, we hypothesise that the PPV of ct/cvDNA is at least 85% (the value obtained by Tanaka et al. being 100% from a calculation performed on 6 patients with detectable cvDNA [20]). Given an estimated 50% positive dissection rate among patients with an indication for salvage adenectomy, the inclusion of 28 patients is required to ensure a power of 80% at an alpha risk of 5% to show a PPV is greater than 50% (value taken as reference, equal to the upper limit of the imagery PPV estimate). This sample size will also enable the estimation of the NPV with a 95% confidence interval (CI) (Wilson) with a half-length equal to 16.5% (for an expected NPV of 89.7% obtained by Tanaka et al. [20]). To ensure the inclusion of 28 patients with adenectomy indication, n = 56 patients are required, since the proportion of patients with this indication after imagery following potentiated radiotherapy is estimated to be about 50% in our study population. Finally, assuming a low attrition rate of 10% (the time between inclusion and end of treatment being relatively short), n = 63 patients are required. Taking into account the additional risk that only 85% of the patients will have detectable ct/cvDNA [21], we estimate that it will be necessary to screen around 75 patients.
Recruitment will be complete once 32 patients with an indication for neck dissection are included and evaluable (this sample size takes into account the 10% attrition rate).
Data analysis
Analyses of the primary endpoint
The primary analysis of the trial is the estimation of the PPV of ctDNA/cvDNA detection at 3 months post-treatment in predicting the outcome of neck dissection. The contingency table for this analysis is presented in Fig. 1. This analysis will be performed on the population undergoing neck dissection. A point estimate and CI will be provided and the PPV will be compared to the reference value of 50% using an exact binomial test.
Analyses of secondary endpoints
Secondary analyses will be performed primarily on all patients (regardless of indication for neck dissection), and also in the subgroup of patients with an indication for neck dissection (as for the primary objective).
The relationship between ctDNA/cvDNA detection at 3 months post-treatment and the treatment failure rate, as well as the relapse rate during follow-up, will be evaluated using the classic diagnostic performance measures calculated on contingency tables (including PPV, NPV, sensitivity, specificity, overall accuracy). In addition, for concordance analyses (of binary variables) between ctDNA/cvDNA and primary tumour, between p16 IHS and real-time PCR, and between real-time PCR and NGS, Cohen's kappa method will also be used.
Survival will be analysed using Kaplan–Meier curves (and log-rank test if relevant). The prognostic value of the presence of residual adenomegaly will be assessed using a Cox model. Other prognostic factors for survival will be investigated using firstly univariate Cox models, and then multivariate models to assess the prognostic value of the presence of residual adenomegaly in particular, and to identify possible confounding factors. For patients with ct/cvDNA collection and analysis at 3 months after the end of treatment, the prognostic impact of ct/cvDNA detection at 3 months in particular will be analysed.
The relationship between ctDNA/cvDNA detection at diagnosis and the clinical, para-clinical and pathological characteristics of the cancer will be performed using McNemar's test, Wilcoxon's signed rank test, Spearman's correlation and multiple linear or logistic regression models, depending on the type of data.
Inter-observer reliability will be assessed using Cohen's kappa method on three-level criteria (positive, doubtful lymph node involvement, or negative).
Data management and monitoring
The data collected for the study will be registered on an electronic case report form (eCRF) (Ennov Clinical). Data will be pseudonymised using a specific identification code. Each centre will manage a table for the correspondence between specific identification codes and patient identity. The access to the eCRF is limited to the investigators, clinical research associates (CRA), project manager, biostatistician, data-manager and monitor CRA. The monitoring of the data will be performed by the monitor CRA mandated by the sponsor and according to the study data monitoring plan. On-site and off-site monitoring visits will be conducted and monitoring reports will be drafted to ensure traceability.
Independent data monitoring committee (IDMC)
An independent trial monitoring committee will be set up. It will be composed of three members with specific areas of expertise (biostatistician, oncologist, head and neck surgeon). This committee will meet after the analysis of the results of the neck dissection for the first 20 eligible patients, i.e. who had a neck dissection and a blood sample at M3.
The main objective of this committee will be to ensure that the assumptions used to calculate the number of subjects are met. A readjustment of the number of eligible subjects needed to meet the objective can be performed subject to the opinion of this committee.
The recruitment rate will also be analysed in order to judge the feasibility of the study (recruitment rate compatible with its continuation).
Discussion
The improvement in detection of residual disease after treatment for advanced head and neck cancer is a current challenge. Our study is part of this context and aims to more efficiently identify patients who do not have residual disease. This will avoid them having undergo neck dissection and will preserve their quality-of-life while maintaining their survival.
As underlined by Yang and colleagues, in the studies focused on ctDNA mutation in the plasma of HNSCC patients, there are very few analyses of the concordance with tumour samples, and few analyses of sensitivity or specificity [22]. One of the strengths of our study is that the proposed analytical technology is a massive parallel sequencing or NGS capture panel integrating the main genes involved in HNSCC as well as the E7 genomic region of HR-HPV. This panel will allow on the one hand simultanous identification of informative tumor variants and detection/genotyping of HR-HPV on FFPE tissue; on the other hand their respective follow-up on circulating DNA. Evaluation of specificity and sensitivity of techniques will also be performed before analyzing patient samples.
Trial status
The study was approved by the ethics committee on December 29th, 2022 (CPP Ouest-1). The recruitment is expected to begin in the first half of 2023. Follow-up and data collection will be complete in 2028.
Acknowledgements
None.
Abbreviations
- cDNA
Circulating deoxyribonucleic acid
- CI
Confidence interval
- ctDNA
Circulating tumour deoxyribonucleic acid
- cvDNA
Circulating viral deoxyribonucleic acid
- CRA
Clinical research associate
- eCRF
Electronic case report form
- FFPE
Formol-fixed paraffin-embedded
- HNC
Head and neck cancer
- HR-HPV
High risk human papilloma virus
- NGS
Next generation sequencing
- NPV
Negative predictive value
- PCR
Polymerase chain reaction
- PET-CT
Positon emission tomography computed tomography
- PPV
Positive predictive value
- SUVmax
Maximum standardized uptake value
Authors’ contributions
Conception and design: MB. Coordinator of the study: MB. Revision of the study design and protocol: MB, AG, XD, IM, MCF, AC. Study coordination: MB, AG. Biological sample analyses: AC, MCF. Statistical analysis: IM. Obtaining funding and supervision: MB, AG. Drafting the manuscript: AG. Revision, adaptation and final approval of the manuscript: All authors. Accountable for all aspects of the work: All authors.
Funding
This work is supported by the Inter-Regional Group for Clinical Research and Innovation – Auvergne Rhône Alpes (GIRCI AURA), grant number PHRCI-2021–56. The funding parties are not involved in the design and conduct of the study, nor in the collection, management, analysis, and interpretation of the data.
They are not involved in the drafting of the present project.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
The study protocol (v1, 28.11.2022) obtained approval from the French Ethics Committee of Comité de Protection des Personnes Ouest-1.
The study is conducted in accordance with the Helsinki Declaration, the Good Clinical Practice (GCP) guidelines of the International Conference on Harmonisation (ICH–E6, 17/07/96), General Data Protection Regulation (GDPR) and local regulatory requirements. Written informed consent will be obtained from each patient by the investigator before any study-related assessment starts.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Qian JM, Schoenfeld JD. Radiotherapy and Immunotherapy for Head and Neck Cancer: Current Evidence and Challenges. Front Oncol. 2020;10:608772. doi: 10.3389/fonc.2020.608772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee Y-G, Kang EJ, Keam B, Choi J-H, Kim J-S, Park KU, et al. Treatment strategy and outcomes in locally advanced head and neck squamous cell carcinoma: a nationwide retrospective cohort study (KCSG HN13–01) BMC Cancer. 2020;20:813. doi: 10.1186/s12885-020-07297-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chaturvedi AK, Anderson WF, Lortet-Tieulent J, Curado MP, Ferlay J, Franceschi S, et al. Worldwide Trends in Incidence Rates for Oral Cavity and Oropharyngeal Cancers. J Clin Oncol. 2013;31:4550–4559. doi: 10.1200/JCO.2013.50.3870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carper MB, Goel S, Zhang AM, Damrauer JS, Cohen S, Zimmerman MP, et al. Activation of the CREB Coactivator CRTC2 by Aberrant Mitogen Signaling promotes oncogenic functions in HPV16 positive head and neck cancer. Neoplasia. 2022;29:100799. doi: 10.1016/j.neo.2022.100799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun Z, Sun X, Chen Z, Du J, Wu Y. Head and Neck Squamous Cell Carcinoma: Risk Factors, Molecular Alterations, Immunology and Peptide Vaccines. Int J Pept Res Ther. 2022;28:19. doi: 10.1007/s10989-021-10334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suh Y, Amelio I, Guerrero Urbano T, Tavassoli M. Clinical update on cancer: molecular oncology of head and neck cancer. Cell Death Dis. 2014;5:e1018. doi: 10.1038/cddis.2013.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ionna F, Bossi P, Guida A, Alberti A, Muto P, Salzano G, et al. Recurrent/Metastatic Squamous Cell Carcinoma of the Head and Neck: A Big and Intriguing Challenge Which May Be Resolved by Integrated Treatments Combining Locoregional and Systemic Therapies. Cancers. 2021;13:2371. doi: 10.3390/cancers13102371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferris RL, Blumenschein G, Fayette J, Guigay J, Colevas AD, Licitra L, et al. Nivolumab for Recurrent Squamous-Cell Carcinoma of the Head and Neck. N Engl J Med. 2016;375:1856–1867. doi: 10.1056/NEJMoa1602252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hwang I, Choi SH, Kim Y-J, Kim KG, Lee AL, Yun TJ, et al. Differentiation of Recurrent Tumor and Posttreatment Changes in Head and Neck Squamous Cell Carcinoma: Application of High b-Value Diffusion-Weighted Imaging. AJNR Am J Neuroradiol. 2013;34:2343–2348. doi: 10.3174/ajnr.A3603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Ginkel JH, Huibers MMH, Noorlag R, de Bree R, van Es RJJ, Willems SM. Liquid Biopsy: A Future Tool for Posttreatment Surveillance in Head and Neck Cancer? Pathobiology. 2017;84:115–120. doi: 10.1159/000452861. [DOI] [PubMed] [Google Scholar]
- 12.Yao M, Smith RB, Graham MM, Hoffman HT, Tan H, Funk GF, et al. The role of FDG PET in management of neck metastasis from head-and-neck cancer after definitive radiation treatment. Int J Radiat Oncol Biol Phys. 2005;63:991–999. doi: 10.1016/j.ijrobp.2005.03.066. [DOI] [PubMed] [Google Scholar]
- 13.Mehanna H, Wong W-L, McConkey CC, Rahman JK, Robinson M, Hartley AGJ, et al. PET-CT Surveillance versus Neck Dissection in Advanced Head and Neck Cancer. N Engl J Med. 2016;374:1444–1454. doi: 10.1056/NEJMoa1514493. [DOI] [PubMed] [Google Scholar]
- 14.Moeller BJ, Rana V, Cannon BA, Williams MD, Sturgis EM, Ginsberg LE, et al. Prospective risk-adjusted [18F]Fluorodeoxyglucose positron emission tomography and computed tomography assessment of radiation response in head and neck cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2009;27:2509–2515. doi: 10.1200/JCO.2008.19.3300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liauw SL, Mancuso AA, Amdur RJ, Morris CG, Villaret DB, Werning JW, et al. Postradiotherapy neck dissection for lymph node-positive head and neck cancer: the use of computed tomography to manage the neck. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24:1421–1427. doi: 10.1200/JCO.2005.04.6052. [DOI] [PubMed] [Google Scholar]
- 16.Thariat J, Ang KK, Allen PK, Ahamad A, Williams MD, Myers JN, et al. Prediction of neck dissection requirement after definitive radiotherapy for head-and-neck squamous cell carcinoma. Int J Radiat Oncol Biol Phys. 2012;82:e367–374. doi: 10.1016/j.ijrobp.2011.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Machtay M, Moughan J, Trotti A, Garden AS, Weber RS, Cooper JS, et al. Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26:3582–3589. doi: 10.1200/JCO.2007.14.8841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siddiqui F, Movsas B. Management of Radiation Toxicity in Head and Neck Cancers. Semin Radiat Oncol. 2017;27:340–349. doi: 10.1016/j.semradonc.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Sroussi HY, Epstein JB, Bensadoun R-J, Saunders DP, Lalla RV, Migliorati CA, et al. Common oral complications of head and neck cancer radiation therapy: mucositis, infections, saliva change, fibrosis, sensory dysfunctions, dental caries, periodontal disease, and osteoradionecrosis. Cancer Med. 2017;6:2918–2931. doi: 10.1002/cam4.1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tanaka H, Takemoto N, Horie M, Takai E, Fukusumi T, Suzuki M, et al. Circulating tumor HPV DNA complements PET-CT in guiding management after radiotherapy in HPV-related squamous cell carcinoma of the head and neck. Int J Cancer. 2021;148:995–1005. doi: 10.1002/ijc.33287. [DOI] [PubMed] [Google Scholar]
- 21.Hilke FJ, Muyas F, Admard J, Kootz B, Nann D, Welz S, et al. Dynamics of cell-free tumour DNA correlate with treatment response of head and neck cancer patients receiving radiochemotherapy. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2020;151:182–189. doi: 10.1016/j.radonc.2020.07.027. [DOI] [PubMed] [Google Scholar]
- 22.Yang X, Xu X, Zhang C, Ji T, Wan T, Liu W. The diagnostic value and prospects of gene mutations in circulating tumor DNA for head and neck cancer monitoring. Oral Oncol. 2022;128:105846. doi: 10.1016/j.oraloncology.2022.105846. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.