Abstract
Background and Hypothesis
Psychotic experiences (PEs) are associated with increased risk for mental disorders, in particular persistent PEs. PEs therefore might be useful within intervention research. We sought to systematically determine the incidence and persistence of PEs in the general population.
Study Design
A double-blind search of databases (Embase, Pubmed PMC, Psychinfo, Medline, and Web of Science) from inception to January 2023 and data extraction, were conducted. Study quality was assessed using the NIH assessment tool. Random effects models were conducted to calculate pooled incidence rate per person-year and proportion of persistent PEs per year. Age and study design were all examined using subgroup analyses. Demographic, risk factors, and outcomes for incidence and persistence of PEs were reported in a narrative synthesis.
Study Results
Using a double-blind screening method for abstract (k = 5763) and full text (k = 250) were screened. In total 91 samples from 71 studies were included, of which 39 were included in a meta-analysis (incidence: k = 17, n = 56 089; persistence: k = 22, n = 81 847). Incidence rate was 0.023 per person-year (95% CI [0.0129;0.0322]). That is, for every 100 people, 2 reported first onset PEs in a year. This was highest in adolescence at 5 per 100(13–17 years). The pooled persistence rate for PEs was 31.0% (95% CI [26.65,35.35]) This was highest in adolescence at 35.8%. Cannabis was particularly associated with incidence of PEs, and persistence of PEs were associated with multiple mental disorders.
Conclusions
Each year incidence of PEs is 2 of every 100 people, and persists each year in 31% of cases, this risk is highest in adolescents.
Introduction
Prevention, the reduction of symptoms, and stopping of new incidences, is a key objectives of public mental health.1,2 Within this context, psychotic experiences (PEs) have become an area of growing interest.3–5 PEs are defined as hallucinations/delusions which can occur outside of a psychotic disorder in the general population.3 PEs are proposed to represent a marker of severe psychopathology,6–8 and a transdiagnostic marker for developing mental disorder.3,9 Within this framework, PEs could be extremely valuable to the field of intervention.
Individuals who report PEs are at a 4-fold increased risk for developing a psychotic disorder and a 3-fold risk for any mental disorder.10 These poor outcomes are particularly pronounced in those who report repeated PEs events (persistence). Persistent PEs are associated with greater risk of developing a mental disorder, poor functioning, higher healthcare costs, and elevated risk of self-harm and suicidal behavior.11–17 Within this context, PEs, particularly persistent PEs, could be viewed as an early risk “marker” of potential poor mental health outcomes.3,9 For this potential utility to be fully assessed, accurate information on rates of persistence across the life span are needed. One meta-analysis to date measured rates of persistence as a secondary outcome18 and found a median rate of 20%, but only found 9 estimates from 6 studies. A large-scale retrospective study found a similar rate of approximately 20%,19 but there remains a deficit in information on rates of persistent PEs, and if these differ across a lifetime.
Previous systematic reviews have reported that the prevalence of PEs are 5%–7% in adulthood,18,20,21 and higher in childhood (~17%) and adolescence (7%–8%).22 There is less clarity, however, about the incidence of PEs. Prevalence measures the current burden of a disease ie, the number of PEs, but it cannot give information on rates of new onset of a disease23 eg, over the next year. Incidence provides this information, examining the risk of getting a disease (ie, reporting a new onset PEs), within a given time period.23 This is a key factor both for research into understanding PEs development and for determining resources23 eg, early health centers or interventions. There have been 2 previous reviews that examined incidence, but these were both carried out approximately a decade or more ago.18,20 No previous systematic review has examined persistence of PEs as a primary aim. Many studies on the incidence and persistence of PEs have been published since this time, allowing more precise meta-analytic estimates to be calculated now. What is more, studies suggest that incidence of PEs varies by age,24 which is an important factor to consider when potentially utilizing PEs in interventions.
We aimed to conduct a systematic review and meta-analysis of the incidence and persistence of PEs in the general population, to address this deficit and better inform future research in the field of PEs and intervention.
Methods
Study Protocol Registered on PROSPERO (CRD42020205484)
Search Strategy.
A systematic review of the databases (Embase, Psychinfo, Web of Science, MEDLINE, and Pubmed PMC) and gray literature (Conference proceedings detected in databases, Open gray, open DOAR, trials.gov, Lenus, Worldcat) was conducted from inception to January 2021 by LS and FM, and an update was conducted in January 2023 by LS, JB & JM. The search terms for PEs were “Delus*” OR “hallucinat*” OR “paranoi*” OR “psychoses” OR “psychosis” OR “psychotic” OR “schizophr*” OR “schizotyp*” OR “psychotic experience*” OR “psychotic like experience*.” To measure incidence and persistence the terms “incidence” OR “incidence rate” OR “follow up” OR “persistent” OR “persistence” OR “repeated” OR “reoccurrence” and to measure sample the terms “general population” OR “normal population” OR “normal individuals” OR “normal sample” OR “healthy population” OR “healthy individuals” OR “healthy sample” OR “community individuals” OR “community sample” OR nonpsychotic OR subclinical OR “non-patient” were used.
Results of the search were imported to Endnote, where duplicates (k = 3464) were removed. Abstrackr25 was used for abstract screening. Following methods outlined by,25 a pre-determined list of inclusion–exclusion criteria were used by all screeners (supplementary material 1 and 2). References of all included studies were screened.
Definition.
PEs within this study are defined as hallucinations/delusions which occur outside of a psychotic disorder, in the general population. This definition does not reflect the entire scope of subclinical phenomenon, such as negative symptoms, cognitive deficits, or schizotypal traits. There are several key reasons for this; From preliminary searches, hallucination/delusions are the definitions used by papers for symptoms termed “PEs/psychotic like experiences/psychotic symptoms”; Negative/disorganized symptoms tend to persist without remission,26,27 and these differences in presentation between PEs and other subclinical phenomenon would risk biasing/hiding results, if used under one term; Symptoms such as schizotypal traits are argued to represent a “trait” characteristic, which has a less clinically pathological trajectory.28
Incidence is defined as new onset of a PEs within a specific time period. Persistence is defined as the presence of PEs at more than one-time point in the same individual.
Abstract Screening.
Using abstrackr25 4 screeners (LS, FM, JB, and JM) reviewed study abstracts. To meet criteria for the abstract screening (supplementary material 1), the study needed to:
Report on original data.
Have a sample of ≥100 participants.
Have recruited a general population sample, or nonpsychotic clinical sample.
Report on PE incidence/persistence, or report on multiple timepoints where PEs was measured.
Exclusion criteria for abstract screening included:
Reporting only on hypnopompic/hypnagogic hallucinations.
Sample only included those who met criteria for first-episode psychosis/psychotic disorder.
Sample only included those who met criteria for clinical-high risk or ultra-high-risk criteria.
Full Text Screening.
All studies which met abstract criteria (k = 250) were screened with 2 initial criteria (supplementary material 2):
Study met definition of PE.
Study reports on sufficient data to be used in a systematic review.
If a study met these criteria, they were divided into 1 of the 3 categories, where additional thresholds were included. Studies could be screened in multiple categories. These categories were;
Incidence studies; studies that report on incidence, incidence rate, or cumulative incidence.
Persistent studies; studies that report on persistent PEs or multiple timepoints of PEs.
Repeated measures studies; any additional studies which measured PEs at multiple timepoints, but which did not specifically measure incidence/persistence of PEs. This third category was included to screen for any additional papers which may have usable data for analysis, but where incidence/persistence were not the primary aim of the study.
For incidence studies, the following additional criteria were screened for; (1) Studies report on a measure of incidence., (2) Study reports a specific time period in which PEs incidence was measured. Persistent PEs category was screened with the additional criteria: (1) Study reports on a measure of persistent PEs, (2) Study has clear explanation on collection of PEs data at multiple timepoints. For the repeated measure study-2 additional criteria were applied; (1) Study has specific time period between baseline and follow-up study, (2) Incidence/persistence can be clearly determined.
Study Selection and Data Extraction.
Following a double-blind screening of the data by independent reviewers (LS, FM, JB, and JM), the screeners met and reviewed studies that were selected for inclusion. Consensus was high (97.41%), and all those where reviewers differed (k = 156) were reviewed. The full-text screening was conducted (k = 250) double-blind and independent (LS, FM). Quality assessment of studies was conducted using the National Heart, Lung, and Blood Institute quality assessment tool for observational cohort and cross-sectional studies and tool for case–control studies (supplementary table 1, https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools). For the main analysis, studies which report PEs to be “suspected/definite” or “definite” (eg, self-report or by confirmed by clinical interview), both measures were recorded. For details on all studies see (supplementary table 2).
Data extraction were done by two independent reviewers (LS, FM), and differences were reviewed. Data were extracted on study name, authors, year of publication, country of sample, study type (case–-control, cohort, survey),the baseline age of sample, the number of individuals reporting PEs, number of controls, PEs rating instrument and whether self-report or interview, and if sample could be considered enriched in any way from random sampling (supplementary table 3) were collected. At follow up data was collected was: Time period to follow up, PEs measure, measure type, measure definition (supplementary table 4), measure language (supplementary table 5), number of incident PEs, number of persisting PEs, number of remitting PEs, controls. Latent models categories (where applicable), number in each latent model category (where applicable). Additional measures (demographics, risk factors, outcomes) which were examined based on incidence/persistence eg, sex differences between those with persistent/transient PEs, were also recorded (supplementary table 6).
Data Analysis.
Analysis was conducted using R.29 Incidence and persistent analysis were conducted separately. Only studies which reported on observed variable data were used for the meta-analysis. Several studies used one dataset, however inclusion of multiple studies from one dataset risked skewing results. Therefore, if both studies were eligible based on all previous criteria, the following measures were used to determine which sample would be included; (1) Study used a cohort design instead of case–control, and (2) Largest sample size. These criteria were sufficient to determine the most appropriate sample to use for all studies. A narrative synthesis was used for studies which reported only modeling data, but could not be included for meta-analysis (supplementary table 7).
Incidence rate was calculated per person-year, using a random effects model using the restricted maximum likelihood method. Incidence rate per person-year is a method of reporting incidence, where you can directly incorporate time and sample as a denominator ie, you can measure the incidence rate for 100 people in 1 year, or 50 people in 10 years. For this study incidence rate is reported per person-year, and in text per-100-person-year, for clarity. The sample was weighted using inverse variance and heterogeneity between studies was measured using Thompson and Higgins I2 statistic30 and τ2. Outlier analysis was conducted using leave-out analysis and case deletion diagnostics (studentized residuals, difference in fits values, Cook’s distances, heterogeneity measures, hat values, and weighting). A second analysis including criteria “definite” instead of “suspect/definite” for studies which provided both was conducted. Moderator analysis examined difference in age of sample, interview type (self-report or clinical interview), enrichment, language of measure, and Q-test was used to test to assess significance of differences in subgroups. Mixed-effect models were used, random effects for the analysis and fixed effect analysis to compare differences between groups, reported as a chi-squared test.
For the persistence analysis, a proportion analysis was conducted31 between those who reported PEs at both timepoints compared to those who reported only at baseline. The proportions were calculated per year, and additionally weighted by sample size. A random effects model of pooled proportion was conducted, heterogeneity between studies was measured using Thompson and Higgins I2 statistic and τ2. Outlier analysis was conducted using case leave-out-analysis and deletion diagnostics (studentized residuals, difference in fits values, Cook’s distances, heterogeneity measures, hat values, and weighting). A second analysis including criteria “definite” instead of “suspect/definite” for studies that provided both was conducted. Moderator analysis with mixed-effect models were conducted using the same measures as incidence, and between cohort and case–control studies.
A majority of measures (demographic, risk factor, and outcomes) were not assessed in a sufficient number of studies (supplementary table 6) to be used in a meta-analysis. A narrative synthesis was conducted on measures where 3 or more studies on independent samples had reported on a measure. Age was treated as a categorical variable, due to the lack of specificity in age reported in studies for follow-up data. This category was defined as: Children (<13 years old), adolescents (13–17 years), adults (18–64 years) and older adults (≥65 years). Given the small sample sizes, language was turned into a categorical variable, comparing studies conducted in English (most common language) vs other languages. If the measure was used in its original form or had been adapted to a different language (supplementary table 4) was also compared.
Results
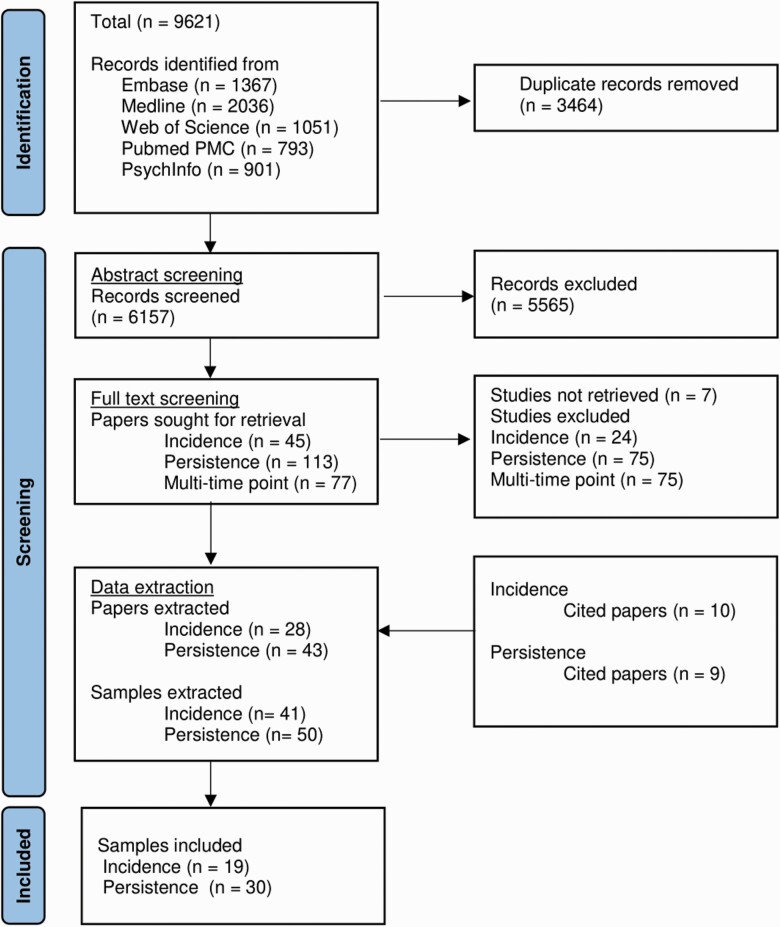
The search strategy yielded a total of k = 9621 papers, once duplicates (k = 3464) were removed, the remaining (k = 6157) papers were screened. The final sample included 28 papers reporting on incidence, and 43 papers reporting on persistence (figure 1). After excluding repeated samples, the total was 19 samples from 16 papers for incidence of PEs14,24,32–44 and 30 samples from 29 papers for persistence.13–15,17,19,34,38,43–62 For full detail see (supplementary table 2). Two incidence papers had more than one usable sample35,38 (In graphs labeled as Hielscher et al., 2020a (baseline - T1 follow-up)/2020b (T1 – T2 follow-up) and Monshouwer et al., 2022a (baseline - T1 follow-up)/2022b (T1 – T2 follow up)/2022c (T2 – T3 follow-up). Two papers report on usable samples from one sample.32,33 One persistence paper reported on 2 different samples (In graphs labeled as Cougnard et al., 2007 EDSP/NEMSIS).49 Five studies14,38,43–45 reported both incidences of PEs and persistent PEs and were included in both meta-analyses.
Fig. 1.
PRISMA flowchart.
Narrative Synthesis
Demographics.
Four incidence studies38,43,63,64 examined sex, 243,64 found no significant effect of sex on incidence of PEs. While 2 papers38,63 using one sample, showed female participants had higher incidence of PEs. There was little consensus about urbanicity, reported as nonsignificant,38,63 that rural background showed higher incidence,43 or that urban background had higher incidence of certain subtypes (auditory, visual, and haptic) PEs.39 Age was broadly found to be nonsignificant,33,43,64 with 2 studies supporting incidence was lower in older adults38 and higher in young people.63 Most studies found educational level did not affect incidence of PEs,33,41,43 with only one study38 finding that those with incident PEs had lower rates of college-level education.
Similar to incidence, a majority of studies13,33,50,53,65 found no differences based on sex between persistence and other groups (control/transient PEs). Those that did report significant differences found female participants had higher rates of persistent PEs.38,52,66 Measures of socioeconomic status were generally not found to be significantly different for those with persistent PEs.13,33,50 Older age was associated with lower persistence of PEs in most38,50 but not all33 studies.
Risk Factors.
A majority of studies37–39,43,63,67 showed that cannabis use increased risk for incident PEsm although one38 found this association was only present for cannabis abuse, not dependence. Another63 observed that this significant association was only in those with PEs and cooccurring mental disorders. One study found the association between cannabis and incident PEs, but not in a fully adjusted model which included prior substance use and antecedent mental disorders.68 Incidence of PEs was significantly elevated in those with poorer general functioning,33,39 social functioning,63 and cognitive function.38,69
Cannabis use, unlike incidence, was not found to be a significant factor for persistence of PEs.32,38,70 Trauma was significantly associated with persistence of PEs by a majority,13,32,38 but not all70 studies. Mental disorders at baseline were examined in several studies; anxiety disorder was found to be a significant risk factor for persistence of PEs,32,38,53 but not in all studies.50,70 Mood disorder at baseline generally was not associated with persistence of PEs,14,32,50,53,70 although 2 studies did find those with a mood disorder had higher rates of persistent PEs38,52 compared to those with remitting PEs and healthy controls. A broad range of psychopathology measures were examined including internalizing/externalizing problems, nightmares, and behavior problems. Studies showed a general trend that higher psychopathology was associated with higher rates of persistent PEs.13,33,65,71 Rimvall et al.,14 did not find a significant difference in psychopathology at baseline between persistent PEs and remitted PEs.
Outcomes.
No outcomes were measured by more than 3 samples for incident PEs. Three studies looked about distress about PEs,32,52,54 and found that those with persistent PEs reported more distress about PEs. Looking at functional outcomes, all studies13,52–54 found impairments in the persistent PEs group, compared to remitted and controls. This included lower general functioning,13,52 greater impairment,53 lower social functioning, and quality of life.54 Examining mental health outcomes, those with persistent PEs had higher rates of psychosis,13,48,54,72 substance abuse disorders,13,14,48 and suicide ideation, behaviors, and attempts.14,15,48,52 A majority of studies examining mood disorder did show higher rates of mood disorders in those with persistent PEs,13,17,32,34,52 but one study did not find a significant difference between persistent PEs hallucinations and controls,48 and a second44 found a nonsignificant change in depression score for those with persistent PEs.
Meta-Analysis
Incidence of PEs
Nineteen samples from 17 studies were included in the incidence analysis14,24,32–44,69,73 (table 1). One study69 did not assess if the PEs were new onset (ie, incident), and so were excluded. This left 17 samples from 15 studies,1–15 sample size was large (n = 56 089). Two studies32,33 used a case–control design (supplementary table 3). The rest used a cohort study designs and the whole reported sample could be used. Six included incidence papers24,36,38,39,64,74 had both a “suspect/definite” and “definite” criteria for one sample. One sample Hielscher et al., 2020a (baseline–T1 follow-up)35 failed to meet the assumptions of heterogeneity (supplementary table 8) and so was excluded from analysis. For details on the countries and measures used in included studies, see (supplementary material 3 and 4; tables 4 and 5)
Table 1.
Incidence Psychotic experiences (PEs) Papers Included in Final Analysis
| Authors | Title | Sample | Follow-up (years) |
PEs measure (baseline) | PEs measure (follow-up) |
|---|---|---|---|---|---|
| Sullivan et al., 2020 | A Population-Based Cohort Study Examining the Incidence and Impact of Psychotic Experiences From Childhood to Adulthood, and Prediction of Psychotic Disorder | ALSPAC (n = 7919) |
12 | PLIKSi (age-12) Interview |
PLIKSi (age-24) Interview |
| Bartels-Velthuis et al., 2016 | Course of auditory vocal hallucinations in childhood: 11-year follow-up study | (n = 694) | 11 | AVHRS Interview |
AVHRS-Q, CAPE Self-report |
| Bartels-Velthuis et al., 2011 | Course of auditory vocal hallucinations in childhood: 5-year follow-up study | (n = 694) | 5.1 | AVHRS Interview |
AVHRS Interview |
| Tien, 1991 | Distributions of hallucinations in the population | ECA (n = 15 258) |
1 | DIS Interview |
DIS Interview |
| Moriyama et al., 2021 | Evidence for an interrelated cluster of Hallucinatory experiences in the general population: an incidence study | NEMESIS (n = 7076) |
3 | CIDI Interview |
CIDI Interview |
| Hielscher et al., 2020 | Mediators of the association between psychotic experiences and future non-suicidal self-injury and suicide attempts: results from a three-wave, prospective adolescent cohort study | HEALing Project (n = 1100) |
1 | DISC-R Interview |
DISC-R Interview |
| Hielscher et al., 2020 | Mediators of the association between psychotic experiences and future non-suicidal self-injury and suicide attempts: results from a three-wave, prospective adolescent cohort study | HEALing Project (n = 1100) |
2 | DISC-R Interview |
DISC-R Interview |
| Kırlı et al., 2019 | Psychotic experiences and mood episodes predict each other bidirectionally: a 6-year follow-up study in a community-based population | TürkSch (n = 4011) |
6 | CIDI Interview |
CIDI Interview |
| Rimvall et al., 2020 | Psychotic experiences from preadolescence to adolescence: when should we be worried about adolescent risk behaviors? | CCC (n = 1632) |
5 | KSADS Interview |
PLIKSq Self-report |
| Soares et al., 2017 | Psychotic symptoms in older people without dementia from a Brazilian community-based sample: A 7 years’ follow-up | (n = 690) | 7 | CAMDEX Interview |
CAMDEX Interview |
| Wiles et al., 2006 | Self-reported psychotic symptoms in the general population: results from the longitudinal study of the British National Psychiatric Morbidity Survey | NPMS (n = 2406) |
1.5 | PSQ Interview |
PSQ Interview |
| Gregersen et al., 2022 | Developmental Pathways and Clinical Outcomes of Early Childhood Psychotic Experiences in Preadolescent Children at Familial High Risk of Schizophrenia orBipolar Disorder: A Prospective, Longitudinal Cohort Study - The Danish High Risk and Resilience Study, VIA 11 | Via 11 (n = 447) |
4 | KSADS-PL Interview |
KSADS-PL Interview |
| Kuepper et al., 2011 | Continued cannabis use and risk of incidence and persistence of psychotic symptoms: 10 year follow-up cohort study | EDSP (n = 1923) |
5.1 | M-CIDI Interview |
M-CIDI Interview |
| Monshouwer et al., 2022a | Prevalence, incidence, and persistence of psychotic experiences in the general population: results of a 9-year follow-up study | NEMESIS II (n = 4769) |
3 | CIDI Interview |
CIDI Interview |
| Monshouwer et al., 2022b | Prevalence, incidence, and persistence of psychotic experiences in the general population: results of a 9-year follow-up study | NEMESIS II (n = 4080) |
3 | CIDI Interview |
CIDI Interview |
| Monshouwer et al., 2022c | Prevalence, incidence, and persistence of psychotic experiences in the general population: results of a 9-year follow-up study | NEMESIS II (n = 3477) |
3 | CIDI Interview |
CIDI Interview |
| Poulton et al., 2000 | Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study | Dunedin (n = 761) |
15 | DISC-C Interview |
DIS Interview |
| Yamasaki et al., 2018 | The association between changes in depression/anxiety and trajectories of psychotic-like experiences over a year in adolescence | (n = 887) | 1 | DISC-C Interview |
DISC-C Interview |
For more details on measures see (supplementary eTable 4). Note: ALSPAC, Avon Longitudinal Study of Parents and Children; ECA, NIMH Epidemiologic Catchment Area Program; NEMESIS, Netherlands Mental Health Survey and Incidence Study; HEALing, Helping to Enhance Adolescent Living study; TürkSch, TürkSch, Izmir Mental Health Survey; CCC, Copenhagen Child Cohort; NPMS, National Psychiatric Morbidity National Psychiatric Morbidity Survey; VIA11, VIA 11 Study; EDSP, Early Developmental Stages of Psychopathology study; NEMESIS II, Netherlands Mental Health Survey and Incidence Study-2; Dunedin, Dunedin Multidisciplinary Health and Development Study; PLIKSi, Psychosis-like-symptoms semi-structured interview; AHVRS, Auditory Vocal Hallucination Rating Scale; DIS, NIMH Diagnostic Interview Schedule; CIDI, Composite International Diagnostic Interview; DISC-R, The Diagnostic Interview Schedule for Children, Revised; KSADS, Kiddie Schedule for Affective Disorders and Schizophrenia; CAMDEX, Cambridge Mental Disorders of the Elderly Examination; PSQ, Psychosis Screening Questionnaire; KSADS-PL, Kiddie Schedule for Affective Disorders and Schizophrenia, Present and Lifetime version; M-CIDI, Munich Composite International Diagnostic Interview; DISC-C, Diagnostic Interview Schedule for Children; AVHRS-Q, Auditory Vocal Hallucination Rating Scale, Self-report; CAPE, Community Assessment of Psychic Experience; PLIKSq, Psychosis-like-symptoms self-report questionnaire.
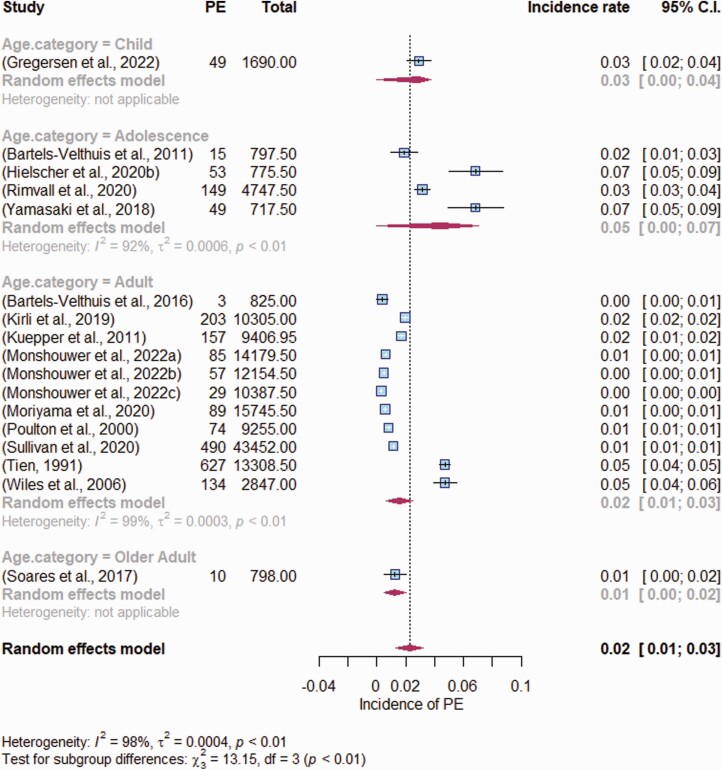
A meta-analysis was conducted using the 17 incidence samples. The pooled incidence rate per person-year was 0.0225 (95% CI [0.0129; 0.0322]) ie, each year, of 100 people 2 will report a PEs for the first time (figure 2), and showed high heterogeneity between studies (I2 = 98.4, 95% CI [98.1%; 98.7%]: τ2 = 0.0004,95% CI [0.0002–0.0010]). Use of “definite” criteria, instead of the “suspect/definite” available in certain studies24,36,38,39,64,74 showed a slightly lower incidence rate per person-year of 0.0205(95% CI [0.0112,0.0297]), but confidence intervals substantially overlapped with the primary analysis.
Fig. 2.
Random effects model of the Incidence rates of psychotic experiences per person-year, divided by age category. Total = total person-years per study, Age category = age at follow-up (to measure new incidence): Adolescence = 13–17 years; Adult = 18–64 years; Older adult = 65+ years old. The dotted line represents the overall pooled estimate, the pooled estimate for each subgroup and overall are shown in the diamonds. The box shows each studies weighted portion, and the horizontal line shows each studies confidence interval.
Using stratification, the incidence rate per person was calculated for each age group (figure 2). Incidence rate for children (age <13) was 3 incident PEs each year, for every 100 people (k = 1, IR = 0.0290). It was highest in adolescence (age 13–17), finding that for every 100 adolescents, 5 would develop PEs in a given year (k = 4, IR = 0.0455; 95% CI [0.0206; 0.0703]). In adulthood (age 18–64) for every 100 adults, 2 would report an incident PEs (k = 11, IR = 0.0155; 95% CI [0.0060; 0.0250]). In older adults (age >64) for every 100 older adults, 1 would report an incident PEs (k = 1, IR = 0.0125; 95% CI [0.0048; 0.0203]) (figure 2). Between-group differences were significant (Q = 13.15,P = .0043).
Examining study design (Self-report vs clinical report, enrichment) found studies that used self-report measures (k = 2, IR = 0.0175;95%CI [0.0000,0.0447]) and those which used clinical interview (k = 15, IR = 0.0233; 95% CI[0.0126,0.0340]) did not show significant differences (Q = 0.15, P = .70). Studies considered “enriched” (supplementary table 3) (k = 4, IR = 0.0289; 95% CI[0.0028,0.0551]) were not significantly different (Q = 0.32, P = .57), than studies not classified as enriched (k = 13, IR = 0.0208; 95% CI[0.0103,0.0312]).
Looking at study population (Language of measure (adapted vs original, English vs other languages (supplementary table 5)), if the measure was conducted in the language it was originally designed for (k = 13, IR = 0.0211; 95% CI[0.0101,0.0320]) or a measure translated from a different language (k = 4, IR = 0.0280; 95% CI[0.0042,0.0517]) was not significantly different (Q = 0.27, P = .61). Similarly, comparing studies conducted in English (k = 4, IR = 0.0327; 95% CI[0.0047,0.0607]) compared to other languages (k = 13, IR = 0.0196,95% CI[0.0099,0.0292]) was nonsignificant (Q = 0.76, P = .39).
Persistence of PEs
A total of 30 studies were included in this analysis (table 2). Of these, 655–57,59,61,62 used latent modeling methods (supplementary table 7). The remaining 2413–15,17,19,34,38,43–49,51–54,58,60,70,75 reported on specific values of the number of PEs at baseline and follow-up. However, 2 studies70,75 used a cross-sectional and case–control study design ie, recruited a specific number of persistent PEs, and could therefore not be assumed to accurately reflect rates of persistence. Additionally, one study50 did not provide a time period in which the persistent PEs events took place, and was excluded from the meta-analysis. This left 21 papers with a large sample (n = 81 847) for analysis. Five of these studies13,16,34,47,58 report on case–control samples. One persistence study38 had both the criteria of “suspect/definite” and “definite” for PEs. One study46 failed to meet the assumptions of heterogeneity (supplementary table 8) and so was excluded from analysis. For details on the countries and measures used in included studies, see (supplementary material 3 and 4)
Table 2.
Persistence Psychotic experiences (PEs) Papers Included in Final Analysis
| Authors | Title | Sample | Follow-up Time (Years) |
PEs Measure Baseline | PEs Measure Follow-up |
|---|---|---|---|---|---|
| Bartels-Velthuis et al 2012 | Auditory hallucinations in childhood: associations with adversity and delusional ideation | (n = 170) | 5 | AVHRS Interview |
AVHRS Interview |
| Bartels-Velthuis et al., 2011 | Course of auditory vocal hallucinations in childhood: 5-year follow-up study | (n = 170) | 5.1 | AVHRS Interview |
AVHRS Interview |
| Janessens et al., 2016 | Developmental course of subclinical positive and negative psychotic symptoms and their associations with genetic risk status and impairment | GROUP (n = 1131) |
3 | CAPE Self-report |
CAPE Self-report |
| Cougnard et al., 2007 | Does normal developmental expression of psychosis combine with environmental risk to cause persistence of psychosis? A psychosis proneness--persistence model | EDSP (n = 2452) |
3.5 | SCL-R-90 Self-report |
CIDI Interview |
| Cougnard et al., 2007 | Does normal developmental expression of psychosis combine with environmental risk to cause persistence of psychosis? A psychosis proneness--persistence model | NEMESIS (n = 4786) |
3 | CIDI Interview |
CIDI Interview |
| Hafeez et al., 2020 | Early persistence of psychotic-like experiences in a community sample of adolescents | (n = 848) | 1.12 | CAPE Self-report |
CAPE Self-report |
| Connell et al., 2016 | Hallucinations in adolescents and risk for mental disorders in adulthood: Prospective evidence from the MUSP birth cohort study | MUSP (n = 3535) |
9 | YSR Self-report |
YASR Self-report |
| De Loore et al., 2011 | Persistence and outcome of auditory hallucinations in adolescence: a longitudinal general population study of 1800 individuals | (n = 1780) | 2 | DISC Interview |
DISC Interview |
| Calkins et al., 2017 | Persistence of psychosis spectrum symptoms in the Philadelphia Neurodevelopmental Cohort: a prospective 2-year follow-up | PNC (n = 503) |
2 | KSADS, PSR Interview |
KSADS, SIPS, PSR Interview |
| Downs et al., 2013 | Persisting psychotic-like experiences are associated with both externalizing and internalizing psychopathology in a longitudinal general population child cohort | (n = 7552) | 1.92 | DISC Interview |
DISC Interview |
| Martin ey al., 2014 | Psychotic experiences and psychological distress predict contemporaneous and future non-suicidal self-injury and suicide attempts in a sample of Australian school-based adolescents | HEALing (n = 1896) |
1 | DISC Interview |
DISC Interview |
| Rimvall et al., 2020 | Psychotic experiences from preadolescence to adolescence: When should we be worried about adolescent risk behaviors? | CCC (n = 1632) |
5 | KSADS Interview |
PLIKSq Self-report |
| McGrath et al., 2015 | Psychotic experiences in the general population: a cross-national analysis based on 31 261 respondents from 18 countries | WMH (n = 31 261) |
0 | CIDI Interview |
- |
| Steenhuis et al., 2016 | Religiosity in young adolescents with auditory vocal hallucinations | (n = 605) | 5 | AVHRS Interview |
AVHRS Interview |
| Wiles et al., 2006 | Self-reported psychotic symptoms in the general population: results from the longitudinal study of the British National Psychiatric Morbidity Survey | NPMS (n = 3536) |
1.5 | PSQ Interview |
PSQ Interview |
| Yamasaki et al., 2018 | The association between changes in depression/anxiety and trajectories of psychotic-like experiences over a year in adolescence | (n = 877) | 1 | DISC Interview |
DISC Interview |
| Gregersen et al., 2022 | Developmental Pathways and Clinical Outcomes of Early Childhood Psychotic Experiences in Preadolescent Children at Familial High Risk of Schizophrenia or Bipolar Disorder: A Prospective, Longitudinal Cohort | Via 11 (n = 447) |
4 | KSADS-PL Interview |
KSADS-PL Interview |
| Adewuya et al., 2023 | The 3-year progression of clinically significant psychotic-like experiences in a general adult population in lagos, nigeria | LSMHS (n = 11246) |
3 | PQB Interview |
PQB Interview |
| Wang et al., 2021 | The Bidirectional Associations Between Insomnia and Psychotic-Like Experiences Before and During the COVID-19 Pandemic | (n = 910) | 1.5 | CAPE Self-report |
CAPE Self-report |
| Monshouwer et al., 2022 | Prevalence, incidence, and persistence of psychotic experiences in the general population: results of a 9-year follow-up study | NEMESIS II (n = 6646) |
3 | CIDI Interview |
CIDI Interview |
| Ergul et al., 2022 | A 6-year follow-up study in a community-based population: Is neighborhood-level social capital associated with the risk of emergence and persistence of psychotic experiences and transition to psychotic disorder? | TürkSch (n = 2175) |
6 | CIDI Interview |
CIDI Interview |
| Isaksson et al., 2022 | Psychotic-like experiences from adolescence to adulthood: A longitudinal study | SALVe (n = 1834) |
6 | DIS Interview |
DIS Interview |
For more details on measures see (supplementary eTable 4). Note. GROUP, Genetic Risk and Outcome of Psychosis; EDSP, Early Developmental Stages of Psychopathology study; NEMESIS, Netherlands Mental Health Survey and Incidence Study; MUSP, Mater-University of Queensland Study of Pregnancy; PNC, Philadelphia Neurodevelopmental Cohort; HEALing, Helping to Enhance Adolescent Living study; CCC, Copenhagen Child Cohort; WMH, World Health Organization World Mental Health survey; NPMS, National Psychiatric Morbidity Survey; VIA 11, VIA 11 study; LSMHS, the Lagos State Mental Health Survey; NEMESIS II, Netherlands Mental Health Survey and Incidence Study-2; TürkSch, TürkSch, Izmir Mental Health Survey; SALVe, the Survey of Adolescent Life in Vastmanland; AHVRS, Auditory Vocal Hallucination Rating Scale; CAPE, Community Assessment of Psychic Experiences; SCL-R-90, the self-report Symptom Checklist 90-R; CIDI, Composite International Diagnostic Interview; YSR, Youth Self-Report; DISC, The Diagnostic Interview Schedule for Children; KSADS, Kiddie Schedule for Affective Disorders and Schizophrenia; PSR, PRIME Screen Revisited; PSQ, Psychosis Screening Questionnaire; KSADS-PL, Kiddie Schedule for Affective Disorders and Schizophrenia, Present and Lifetime version; PQB, Prodromal Questionnaire-Brief Version; DIS, NIMH Diagnostic Interview Schedule; YASR, Youth Adult Self-Report; SIPS, Structured Interview for Prodromal Syndromes; PLIKSq, Psychosis-like-symptoms self-report questionnaire.
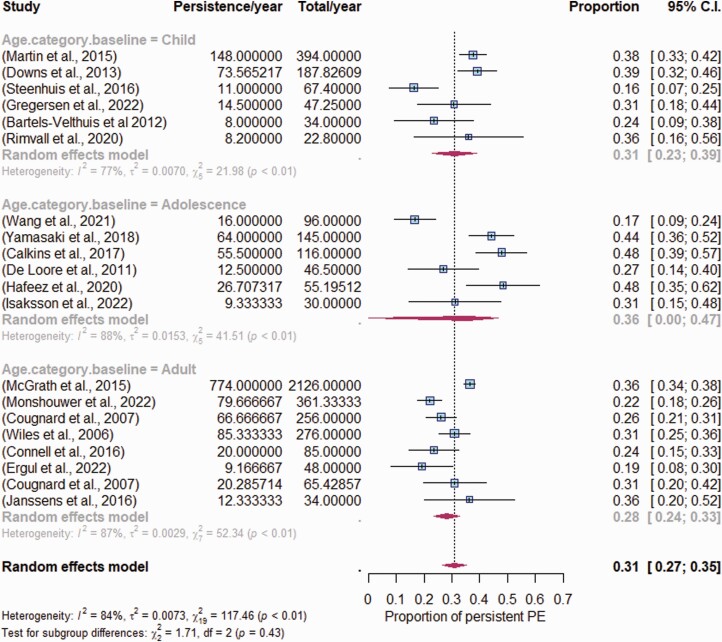
The pooled proportion analysis found that 31% of those reporting PEs at baseline reported a second PEs within a given year(β = 0.3100, SE = 0.0222, z-value = 13.9717, 95% CI[26.65, 35.35]; Figure 3). There was high heterogeneity between studies (I2 = 86.16%, 95% CI[72.6,93.6]); τ2 = 0.0073). Including the “definite” criteria for the available study38 did not substantially change the persistence proportion-per year (30.9%, 95% CI[26.48,35.33]; β = 0.3090, SE = 0.0226, z-value = 13.6826), and had substantial overlap in confidence interval with the primary analysis.
Moderator analysis of age showed those who were children when PEs were first recorded, 30.8% reported persistent PEs (k = 6, 95% CI[22.8,38.9]; Figure 3). Of those who were adolescents at baseline, 35.8% reported persistence (k = 6, 95% CI[24.9;46.7]; Figure 3), and of those who were adults at baseline 28.2% reported persistence (k =8, 95% CI[23.5, 32.8]; Figure 3). Difference between age subgroups was nonsignificant (Q = 1.71, df = 2, P = .43).
Fig. 3.
Random effects model of pooled proportion of persistent Psychotic experiences (PEs) compared to remitted PEs, by age category. Persistence/year is the rate of persistence per year, Total/year = total sample person-year per study. Age category = age at follow-up (to measure new incidence): Adolescence = 13–17 years; Adult = 18–64 years; Older adult = 65+ years old. The dotted line represents the overall pooled estimate, the pooled estimate for each subgroup and overall are shown in the diamonds. The box shows each studies weighted portion, and the horizontal line shows each studies confidence interval.
Study design (self-report vs interview; cohort vs case–control; enrichment) found differences between self-report vs clinical interview were nonsignificant (Q = 2.13, P = .34) Self-report both times (k = 9, 30.7%; 95% CI[23.9,37.5]) Clinical interview both timepoints (k = 8, 32.4%; 95% CI[24.9,39.9]) Self-report/clinical interview at different timepoints (k = 3, 36.1%; 95% CI[30.7,41.6]). Cohort vs case–control design similarly showed no significant difference (Q = 0.28, P = 0.59), cohort design (k = 15; 31.8%; 95% CI[27.1,36.4]) compared to case–control (k = 5; 28.5%, 95% CI[17.3,39.6]). This was also observed when examining any study which may be classified as “enriched” (supplementary table 3) eg, case–control or oversampling (Q = 0.00, P = .99), enriched(k = 9, 31.0%, 95% CI[24.7,37.3]), general (k = 11, 31.1%, 95% CI[24.8,37.3]).
Study measures differences (language of measure, original vs adapted, or English vs other languages (supplementary table 5)) found some differences. If the language of the measure used was the original one (k = 15, 31.37%, 95% CI[26.48,36.25]), or adapted from a preexisting measure (k = 5, 29.78%, 95% CI[19.53,40.03]) were nonsignificant (Q = 0.08, P = .7839). However, when looking at if the measure was conducted in English (k = 9; 35.78%, 95% CI[30.23,41.32]) or a different language (k = 11; 27.24%, 95% CI[21.61,32.87]), found there was a significant difference (Q = 4.48, P = .034).
Discussion
This systematic review and meta-analysis investigated the incidence rate per year of PEs in the general population, as well as the persistence rate of PEs. Two key findings emerged: The incidence rate of PEs per year was 0.0225 per person-years ie, for every 100 individuals, 2 will report new onset PEs in a given year. This was highest in adolescents at 5 per 100 people each year, and lowest in older adults (1 per 100 people). Secondly, the pooled proportion of persistent PEs was 31.0% and was particularly high in studies of adolescents 35.8% (aged 13–17). These key findings provide information that increases the future utility of PEs for intervention research.
This is the first study to calculate incidence rate per person-year, which is the measure needed to estimate expected incidence in a population over a specific length of time. Our study suggests that PEs do occur across a life span, at about 2 per 100 people each year, regardless of age. Interestingly, this result was not significantly affected by definition of PEs (“suspected/definite” or “definite”), or if the measure was self-report or clinically validated. Supporting the evidence that self-report is reasonably effective at detecting PEs.76 Similarly, measures adapted into new languages did not report substantially different incidence of PEs to measures in their original language, or if the measure was in English or another language. Incidence is an important measure for research, knowledge of expected numbers of PEs, allows for the study of the causes of PEs,23 or to assess if an intervention has prevented PEs.4 Similarly, knowing the incidence of PEs is important for policy, giving accurate information on the rates of new onset PEs in a given year.23
Persistence of PEs was higher than the previously reported 20%,19,20 with our study finding that a about one-third of those who experience PEs will have a second PEs each year. The differences in definition of PEs, clinical interview vs self-report and type of study (case–control vs cohort) were all nonsignificant. Given the findings suggesting age of sample may affect rates of persistence, it may be that the growing number of longitudinal studies in younger samples14,15,47,51,58 is increasing the rates of persistent PEs. Alternatively, it may be because this is the first systematic review with a primary objective to measure persistent PEs, rather than a secondary outcome, yielding a larger sample size and reducing selection bias. At the same time, it is important to note that while the rate of persistent PEs was high, the majority of participants reported no PEs at any time point, and a majority who reported PEs experienced only transient PEs.
One study design measure which was found to be significantly different was the language used (English vs other languages), which might be interpreted as a crude proxy for cultural differences. Given the limited number of samples (k = 50), which were even more restricted given repeated samples across multiple studies (k = 20) it was not possible to look at language at a more nuanced level, or differences at the country/region level. There is substantial evidence that differences in psychosis rates exist between countries77 and different communities within countries.78 This same pattern may occur within PEs, but to determine it, there is a need for more PEs research, particularly in under-examined regions.
Both incidence and persistence of PEs were highest rates in adolescence (age 13–17) and indicates that adolescence is a sensitive developmental period. It also suggests that this is a key age for detecting and intervening for PEs. The incidence rate was found to be 4.5 in every 100 adolescents each year reporting a new onset PEs, and 35.8% of those reporting PEs in adolescence will report PEs again at follow-up. One reason for this vulnerability to PEs in adolescents may be cooccurrence of mental disorders, many of which begin in adolescence.79 The adverse outcomes associated with transient PEs,11,12,80 and particularly with persistent PEs13–17,44 have been well documented.
Our initial aim had been to conduct a meta-analysis including frequently measured demographic, risk, or outcome factors for incidence/persistence of PEs. However, there were insufficient measures to do this, and so a narrative synthesis was conducted. For both incidence38,63 and persistence38,52,66 of PEs, there was some evidence to support female sex being associated with higher rates, but a majority of studies found no difference.13,33,43,50,53,64,65 Urbanicity38,39,43,63 and education38,39,43,63 was inconsistently associated with incidence of PEs,38,39,43,63 and socioeconomic status was not significantly associated with persistence of PEs.13,33,50 Risk factors for incidence suggested poor functioning38,39,43,63,67 at baseline, and cannabis33,38,39,43,63,64 were associated with increased risk for incident PEs. Interestingly, cannabis was not found to be a substantial risk factor for persistence of PEs.32,38,70 Anxiety disorder at baseline was inconsistently associated with higher persistence of PEs.33,38,50,53,70 Other risk factors that generally showed increased risk for persistence included trauma13,33,38,70 and high psychopathology.12,13,33,66,71 Outcomes of persistent PEs included poor functioning,13,52–54 and higher rates of psychosis,13,48,54,72 substance abuse,13,14,48 suicide risk,12,14,48,52 and mood disorder.13,17,32,34,44,48,52 Overall, evidence supports the adverse consequences of PEs, consistent with previous literature. However, research, and particularly replication, is still lacking. Knowledge is also lacking on what causes incidence of PEs and for PEs to persist. More information is needed beyond differences in prevalence of PEs, particularly to determine need and utility of interventions.
Future Directions
Intervention
Prevention is the key to public mental health,1 and within this, PEs could be a valuable tool for detecting those at risk for developing mental disorder.3,10 The results of our study suggests this may be particularly true for adolescents.
Screening.
One policy-level approach could be the introduction of PEs into standard screening tools eg, in mental health services. PEs are relatively easy to screen, with even one-item self-report measures providing good levels of accuracy in detecting PEs.81 This review shows the literature is indicating a high rate of PEs in adolescence, making this group particularly important to screen. A wider implementation of PEs screening tools in adolescent and child services would improve detection and would be a potentially important step in identifying those at greater risk for adverse outcomes.
Intervention.
A new area of interventions are studies aimed at prevention.4,5 Previous studies in school-based and college based have observed a positive effect in reducing and preventing new incidences of PEs.4,5 However, mediators such as bullying and self-esteem82,83 have been linked to a reduction in PEs. PEs could be a primary target to improve eg, through self-esteem or bullying interventions. Reduction could be the key step to preventing persistence of PEs, which were shown in this study to have adverse outcomes.
Assessment.
PEs could be used as a tool to develop preventative treatments eg, PEs used as a recruitment tool for the particularly vulnerable, identifying differences in response to treatment, or used as a measure of long-term efficacy of the intervention (ie, examine rates of persistent PEs in samples). Previous work has shown those with PEs84 do show different responses to treatment, and PEs may be an important component to interventions, even when not directly targeting PEs.
Limitations
Several limitations of this review should be noted; The vast majority of included studies were from Europe or North America. Steps were taken to reduce this, eg, no exclusion criteria such as “must be in English” were included, but it still occurred. It should therefore be noted the incidence and persistence of PEs reflect economically wealthy regions. The meta-analysis used only one measure of persistent PEs or incidence of PEs per sample, as a way to reduce the risk of bias, given the repeated use of samples across studies. The search strategy included terms for general population (“general population,” “community sample” etc.), and may not have included purely clinical samples. Finally, meta-analysis for demographics, risk factors, and outcomes could not be done due to low replication across studies.
Conclusion
This is the largest systematic review to date of incidence of PEs, and the first with a primary aim of examining rates of persistence of PEs. We have found valuable estimates needed to determine if interventions are effective ie, incidence rate per person-year, which can be used to determine prevention, and persistence rate per year, which can be used to determine reduction. The results indicate that PEs is a common occurrence, and that on average 2 in every 100 people will report new onset PEs each year. PEs are proposed to represent a marker of severe psychopathology,7,8 and our findings suggest that developing high psychopathology is not uncommon across the life span. Persistence is particularly associated with poor outcomes,13,15 and our study suggests that there is a 1 in 3 chance of reporting persistent PEs. There is a growing body of literature on PEs but there is a need to expand beyond academic research, into clinical practice and preventative treatment, particularly in young people.
Supplementary Material
Acknowledgment
To the best of our knowledge, no author has a conflict of interest to disclose.
Contributor Information
Lorna Staines, Department of Psychiatry, Royal College of Surgeons in Ireland, Dublin 2, Ireland.
Colm Healy, Department of Psychiatry, Royal College of Surgeons in Ireland, Dublin 2, Ireland.
Felim Murphy, Department of Psychiatry, Royal College of Surgeons in Ireland, Dublin 2, Ireland.
Jonah Byrne, Department of Psychiatry, Royal College of Surgeons in Ireland, Dublin 2, Ireland.
Jennifer Murphy, Department of Psychiatry, Royal College of Surgeons in Ireland, Dublin 2, Ireland.
Ian Kelleher, Division of Psychiatry, Centre for Clinical Brain Sciences, University of Edinburgh, Edinburgh, EH10 5HF, UK.
David Cotter, Department of Psychiatry, Royal College of Surgeons in Ireland, Dublin 2, Ireland; Department Psychiatry, Beaumont Hospital, Dublin 9, Ireland.
Mary Cannon, Department of Psychiatry, Royal College of Surgeons in Ireland, Dublin 2, Ireland; Department Psychiatry, Beaumont Hospital, Dublin 9, Ireland.
Funding
This study was completed as part of the iHEAR study, the iHEAR study is a European Research Council funded project (grant number: 724809). DC and HC are funded by a Wellcome Trust Innovations Award, number 220438Z/20/Z), and in part by a research grant from Science Foundation Ireland (SFI) under Grant Number 16/RC/3948415 and co-funded under the European Regional Development Fund and by FutureNeuro industry partners. CH and MC are funded by the Health Research Board Investigator Lead Project (ILP-PHR-2019-009). Additionally, thanks are extended to Prof. Murphy and Dr Clarke for help in the write-up of the manuscript.
References
- 1. Campion J, Javed A, Vaishnav M, Marmot M.. Public mental health and associated opportunities. Indian J Psychiatry. 2020;62(1):3–6. doi: 10.4103/psychiatry.IndianJPsychiatry_687_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fusar-Poli P, Correll CU, Arango C, Berk M, Patel V, Ioannidis JPA.. Preventive psychiatry: a blueprint for improving the mental health of young people. World Psychiatry. 2021;20(2):200–221. doi: 10.1002/wps.20869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Staines L, Healy C, Coughlan H, et al. Psychotic experiences in the general population, a review; definition, risk factors, outcomes and interventions. Psychol Med. 2022;52(15):3297–3308. doi: 10.1017/S0033291722002550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. DeTore NR, Luther L, Deng W, et al. Efficacy of a transdiagnostic, prevention-focused program for at-risk young adults: a waitlist-controlled trial. Psychol Med. 2022:1–10. doi: 10.1017/S0033291722000046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Staines L, Healy C, Corcoran P, et al. Investigating the effectiveness of three school based interventions for preventing psychotic experiences over a year period – a secondary data analysis study of a randomized control trial. BMC Public Health. 2023;23(1):219. doi: 10.1186/s12889-023-15107-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guloksuz S, van Os J.. The slow death of the concept of schizophrenia and the painful birth of the psychosis spectrum. Psychol Med. 2018;48(2):229–244. doi: 10.1017/S0033291717001775 [DOI] [PubMed] [Google Scholar]
- 7. Guloksuz S. The trough of disillusionment: a critique of the “transition” paradigm. Eur Psychiatry. 2021;64(S1):S17–S17. doi: 10.1192/j.eurpsy.2021.68 [DOI] [Google Scholar]
- 8. Stochl J, Khandaker GM, Lewis G, et al. Mood, anxiety and psychotic phenomena measure a common psychopathological factor. Psychol Med. 2015;45(7):1483–1493. doi: 10.1017/S003329171400261X [DOI] [PubMed] [Google Scholar]
- 9. McGorry PD, Hartmann JA, Spooner R, Nelson B.. Beyond the “at risk mental state” concept: transitioning to transdiagnostic psychiatry. World Psychiatry. 2018;17(2):133–142. doi: 10.1002/wps.20514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Healy C, Brannigan R, Dooley N, et al. Childhood and adolescent psychotic experiences and risk of mental disorder: a systematic review and meta-analysis. Psychol Med. 2019;49(10):1589–1599. doi: 10.1017/S0033291719000485 [DOI] [PubMed] [Google Scholar]
- 11. Bromet EJ, Nock MK, Saha S, et al. ; World Health Organization World Mental Health Survey Collaborators. Association between psychotic experiences and subsequent suicidal thoughts and behaviors: a cross-national analysis from the world health organization world mental health surveys. JAMA Psychiatry. 2017;74(11):1136–1144. doi: 10.1001/jamapsychiatry.2017.2647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rimvall MK, van Os J, Verhulst F, et al. Mental health service use and psychopharmacological treatment following psychotic experiences in preadolescence. Am J Psychiatry. 2020;177(4):318–326. doi: 10.1176/appi.ajp.2019.19070724 [DOI] [PubMed] [Google Scholar]
- 13. Calkins ME, Moore TM, Satterthwaite TD, et al. Persistence of psychosis spectrum symptoms in the Philadelphia Neurodevelopmental Cohort: a prospective two-year follow-up. World Psychiatry. 2017;16(1):62–76. doi: 10.1002/wps.20386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rimvall MK, van Os J, Rask CU, et al. Psychotic experiences from preadolescence to adolescence: when should we be worried about adolescent risk behaviors? Eur Child Adolesc Psychiatry. 2020;29(9):1251–1264. doi: 10.1007/s00787-019-01439-w [DOI] [PubMed] [Google Scholar]
- 15. Martin G, Thomas H, Andrews T, Hasking P, Scott JG.. Psychotic experiences and psychological distress predict contemporaneous and future non-suicidal self-injury and suicide attempts in a sample of Australian school-based adolescents. Psychol Med. 2015;45(2):429–437. doi: 10.1017/S0033291714001615 [DOI] [PubMed] [Google Scholar]
- 16. Connell M, Betts K, McGrath JJ, et al. Hallucinations in adolescents and risk for mental disorders and suicidal behaviour in adulthood: prospective evidence from the MUSP birth cohort study. Schizophr Res. 2016;176(2-3):546–551. doi: 10.1016/j.schres.2016.06.009 [DOI] [PubMed] [Google Scholar]
- 17. De Loore E, Gunther N, Drukker M, et al. Persistence and outcome of auditory hallucinations in adolescence: a longitudinal general population study of 1800 individuals. Schizophr Res. 2011;127(1):252–256. doi: 10.1016/j.schres.2011.01.015 [DOI] [PubMed] [Google Scholar]
- 18. Linscott RJ, van Os J.. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43(6):1133–1149. doi: 10.1017/S0033291712001626 [DOI] [PubMed] [Google Scholar]
- 19. McGrath JJ, Saha S, Al-Hamzawi A, et al. Psychotic experiences in the general population: a cross-national analysis based on 31,261 respondents from 18 countries. JAMA Psychiatry. 2015;72(7):697–705. doi: 10.1001/jamapsychiatry.2015.0575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L.. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness–persistence–impairment model of psychotic disorder. Psychol Med. 2009;39(2):179–195. doi: 10.1017/S0033291708003814 [DOI] [PubMed] [Google Scholar]
- 21. Yates K, Lång U, Peters EM, et al. Hallucinations in the general population across the adult lifespan: prevalence and psychopathologic significance. Br J Psychiatry. 2021 Dec:652–658. doi: 10.1192/bjp.2021.100 [DOI] [PubMed] [Google Scholar]
- 22. Kelleher I, Connor D, Clarke MC, Devlin N, Harley M, Cannon M.. Prevalence of psychotic symptoms in childhood and adolescence: a systematic review and meta-analysis of population-based studies. Psychol Med. 2012;42(9):1857–1863. doi: 10.1017/S0033291711002960 [DOI] [PubMed] [Google Scholar]
- 23. Tenny S, Hoffman MR.. Prevalence. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. Accessed March 16, 2022. http://www.ncbi.nlm.nih.gov/books/NBK430867/ [Google Scholar]
- 24. Sullivan SA, Kounali D, Cannon M, et al. A population-based cohort study examining the incidence and impact of psychotic experiences from childhood to adulthood, and prediction of psychotic disorder. Am J Psychiatry. 2020;177(4):308–317. doi: 10.1176/appi.ajp.2019.19060654 [DOI] [PubMed] [Google Scholar]
- 25. Polanin JR, Pigott TD, Espelage DL, Grotpeter JK.. Best practice guidelines for abstract screening large-evidence systematic reviews and meta-analyses. Res Synth Methods. 2019;10(3):330–342. doi: 10.1002/jrsm.1354 [DOI] [Google Scholar]
- 26. Carrión RE, Demmin D, Auther AM, et al. Duration of attenuated positive and negative symptoms in individuals at clinical high risk: associations with risk of conversion to psychosis and functional outcome. J Psychiatr Res. 2016;81:95–101. doi: 10.1016/j.jpsychires.2016.06.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Demjaha A, Valmaggia L, Stahl D, Byrne M, McGuire P.. Disorganization/Cognitive and negative symptom dimensions in the at-risk mental state predict subsequent transition to psychosis. Schizophr Bull. 2012;38(2):351–359. doi: 10.1093/schbul/sbq088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Michel C, Flückiger R, Kindler J, Hubl D, Kaess M, Schultze-Lutter F.. The trait-state distinction between schizotypy and clinical high risk: results from a one-year follow-up. World Psychiatry. 2019;18(1):108–109. doi: 10.1002/wps.20595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. R Core Team. R: A Language and Environment for Statistical Computing . Vienna: R Foundation for Statistical Computing; 2020. https://www.R-project.org/ [Google Scholar]
- 30. Higgins JPT, Thompson SG.. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 31. Wang N. How to Conduct a Meta-Analysis of Proportions in R: A Comprehensive Tutorial. CUNY: Research Gate, John Jay College of Criminal Justice; 2018. doi: 10.13140/RG.2.2.27199.00161 [DOI] [Google Scholar]
- 32. Bartels-Velthuis AA, Wigman JTW, Jenner JA, Bruggeman R, Os J van.. Course of auditory vocal hallucinations in childhood: 11-year follow-up study. Acta Psychiatr Scand. 2016;134(1):6–15. doi: 10.1111/acps.12571 [DOI] [PubMed] [Google Scholar]
- 33. Bartels-Velthuis AA, Willige G van de, Jenner JA, Os J van, Wiersma D.. Course of auditory vocal hallucinations in childhood: 5-year follow-up study. Br J Psychiatry. 2011;199(4):296–302. doi: 10.1192/bjp.bp.110.086918 [DOI] [PubMed] [Google Scholar]
- 34. Gregersen M, Jepsen JRM, Rohd SB, et al. Developmental pathways and clinical outcomes of early childhood psychotic experiences in preadolescent children at familial high-risk of schizophrenia or bipolar disorder: a prospective, longitudinal cohort study - The Danish High Risk and Resilience Study, VIA 11. Am J Psychiatry. 2022;179(9):628–639. [DOI] [PubMed] [Google Scholar]
- 35. Hielscher E, DeVylder JE, Hasking P, Connell M, Martin G, Scott JG.. Mediators of the association between psychotic experiences and future non-suicidal self-injury and suicide attempts: results from a three-wave, prospective adolescent cohort study. Eur Child Adolesc Psychiatry. 2020. doi: 10.1007/s00787-020-01593-6 [DOI] [PubMed] [Google Scholar]
- 36. Kırlı U, Binbay T, Drukker M, et al. Psychotic experiences and mood episodes predict each other bidirectionally: a 6-year follow-up study in a community-based population. Soc Psychiatry Psychiatr Epidemiol. 2019;54(3):331–341. doi: 10.1007/s00127-018-1641-8 [DOI] [PubMed] [Google Scholar]
- 37. Kuepper R, Os J van, Lieb R, Wittchen HU, Höfler M, Henquet C.. Continued cannabis use and risk of incidence and persistence of psychotic symptoms: 10 year follow-up cohort study. BMJ. 2011;342:d738. doi: 10.1136/bmj.d738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Monshouwer K, Have M, Tuithof M, et al. Prevalence, incidence, and persistence of psychotic experiences in the general population: results of a 9-year follow-up study. Psychol Med. 2022:1–12. doi: 10.1017/S0033291722002690 [DOI] [PubMed] [Google Scholar]
- 39. Moriyama TS, Drukker M, Guloksuz S, et al. Evidence for an interrelated cluster of Hallucinatory experiences in the general population: an incidence study. Psychol Med. 2021;51(12):2034–2043. doi: 10.1017/S0033291720000793. [DOI] [PubMed] [Google Scholar]
- 40. Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H.. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57(11):1053–1058. doi: 10.1001/archpsyc.57.11.1053 [DOI] [PubMed] [Google Scholar]
- 41. Soares WB, Santos EB, Bottino CMC, Elkis H.. Psychotic symptoms in older people without dementia from a Brazilian community-based sample: a seven years’ follow-up. PLoS One. 2017;12(6):e0178471. doi: 10.1371/journal.pone.0178471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tien AY. Distributions of hallucinations in the population. Soc Psychiatry Psychiatr Epidemiol. 1991;26(6):287–292. doi: 10.1007/BF00789221 [DOI] [PubMed] [Google Scholar]
- 43. Wiles NJ, Zammit S, Bebbington P, Singleton N, Meltzer H, Lewis G.. Self-reported psychotic symptoms in the general population: results from the longitudinal study of the British National Psychiatric Morbidity Survey. Br J Psychiatry. 2006;188(6):519–526. doi: 10.1192/bjp.bp.105.012179 [DOI] [PubMed] [Google Scholar]
- 44. Yamasaki S, Usami S, Sasaki R, et al. The association between changes in depression/anxiety and trajectories of psychotic-like experiences over a year in adolescence. Schizophr Res. 2018;195:149–153. doi: 10.1016/j.schres.2017.10.019 [DOI] [PubMed] [Google Scholar]
- 45. Ergül C, Drukker M, Binbay T, et al. A 6-year follow-up study in a community-based population: is neighbourhood-level social capital associated with the risk of emergence and persistence of psychotic experiences and transition to psychotic disorder? Psychol Med. 2022:1–13. doi: 10.1017/S0033291722000642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Adewuya AO, Oladipo OE, Imarah T, Asmal L, Emsley R.. The 3-year progression of clinically significant psychotic-like experiences in a general adult population in Lagos, Nigeria. Soc Psychiatry Psychiatr Epidemiol. 2023;58(1):91–103. doi: 10.1007/s00127-022-02358-z [DOI] [PubMed] [Google Scholar]
- 47. Bartels-Velthuis AA, van de Willige G, Jenner JA, Wiersma D, van Os J.. Auditory hallucinations in childhood: associations with adversity and delusional ideation. Psychol Med. 2012;42(3):583–593. doi: 10.1017/S0033291711001590 [DOI] [PubMed] [Google Scholar]
- 48. Connell M, Betts K, McGrath JJ, et al. Hallucinations in adolescents and risk for mental disorders and suicidal behaviour in adulthood: prospective evidence from the MUSP birth cohort study. Schizophr Res. 2016;176(2–3):546–551. doi: 10.1016/j.schres.2016.06.009 [DOI] [PubMed] [Google Scholar]
- 49. Cougnard A, Marcelis M, Myin-Germeys I, et al. Does normal developmental expression of psychosis combine with environmental risk to cause persistence of psychosis? A psychosis proneness–persistence model. Psychol Med. 2007;37(4):513–527. doi: 10.1017/S0033291706009731 [DOI] [PubMed] [Google Scholar]
- 50. DeVylder JE, Lehmann M, Chen F.. Social and clinical correlates of the persistence of psychotic experiences in the general population. Schizophr Res. 2015;169(1):286–291. doi: 10.1016/j.schres.2015.08.039 [DOI] [PubMed] [Google Scholar]
- 51. Downs JM, Cullen AE, Barragan M, Laurens KR.. Persisting psychotic-like experiences are associated with both externalising and internalising psychopathology in a longitudinal general population child cohort. Schizophr Res. 2013;144(1-3):99–104. doi: 10.1016/j.schres.2012.12.009 [DOI] [PubMed] [Google Scholar]
- 52. Hafeez D, Yung AR.. Early persistence of psychotic-like experiences in a community sample of adolescents. Early Interv Psychiatry. 2020. doi: 10.1111/eip.13096 [DOI] [PubMed] [Google Scholar]
- 53. Isaksson J, Angenfelt M, Frick MA, Olofsdotter S, Vadlin S.. Psychotic-like experiences from adolescence to adulthood: a longitudinal study. Schizophr Res. 2022;248:1–7. doi: 10.1016/j.schres.2022.07.010 [DOI] [PubMed] [Google Scholar]
- 54. Janssens M, Boyette LL, Heering HD, Bartels-Velthuis AA, Lataster T; Genetic Risk and Outcome of Psychosis investigators. Developmental course of subclinical positive and negative psychotic symptoms and their associations with genetic risk status and impairment. Schizophr Res. 2016;174(1–3):177–182. doi: 10.1016/j.schres.2016.03.028 [DOI] [PubMed] [Google Scholar]
- 55. Lin A, Wigman JTW, Nelson B, et al. The relationship between coping and subclinical psychotic experiences in adolescents from the general population – a longitudinal study. Psychol Med. 2011;41(12):2535–2546. doi: 10.1017/S0033291711000560 [DOI] [PubMed] [Google Scholar]
- 56. Mackie CJ, Castellanos-Ryan N, Conrod PJ.. Developmental trajectories of psychotic-like experiences across adolescence: impact of victimization and substance use. Psychol Med. 2011;41(1):47–58. doi: 10.1017/S0033291710000449 [DOI] [PubMed] [Google Scholar]
- 57. Rössler W, Riecher-Rössler A, Angst J, et al. Psychotic experiences in the general population: a twenty-year prospective community study. Schizophr Res. 2007;92(1–3):1–14. doi: 10.1016/j.schres.2007.01.002 [DOI] [PubMed] [Google Scholar]
- 58. Steenhuis LA, Bartels-Velthuis AA, Jenner JA, et al. Religiosity in young adolescents with auditory vocal hallucinations. Psychiatry Res. 2016;236:158–164. doi: 10.1016/j.psychres.2015.12.014 [DOI] [PubMed] [Google Scholar]
- 59. Thapar A, Heron J, Jones RB, Owen MJ, Lewis G, Zammit S.. Trajectories of change in self-reported psychotic-like experiences in childhood and adolescence. Schizophr Res. 2012;140(1):104–109. doi: 10.1016/j.schres.2012.06.024 [DOI] [PubMed] [Google Scholar]
- 60. Wang D, Zhou L, Wang J, Sun M.. The bidirectional associations between insomnia and psychotic-like experiences before and during the COVID-19 pandemic. Nat Sci Sleep. 2021;13:2029–2037. doi: 10.2147/NSS.S335508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wigman JTW, Van Winkel R, Raaijmakers QAW, et al. Evidence for a persistent, environment-dependent and deteriorating subtype of subclinical psychotic experiences: a 6-year longitudinal general population study. Psychol Med. 2011;41(11):2317–2329. doi: 10.1017/S0033291711000304 [DOI] [PubMed] [Google Scholar]
- 62. Wigman JTW, van Winkel R, Jacobs N, et al. A twin study of genetic and environmental determinants of abnormal persistence of psychotic experiences in young adulthood. Am J Med Genet B Neuropsychiatr Genet. 2011;156(5):546–552. doi: 10.1002/ajmg.b.31193 [DOI] [PubMed] [Google Scholar]
- 63. Hasmi L, Pries LK, ten Have M, et al. What makes the psychosis “clinical high risk” state risky: psychosis itself or the co-presence of a non-psychotic disorder? Epidemiol Psychiatr Sci. 2021;30:e53. doi: 10.1017/S204579602100041X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Köhler S, van Os J, de Graaf R, Vollebergh W, Verhey F, Krabbendam L.. Psychosis risk as a function of age at onset. Soc Psychiatry Psychiatr Epidemiol. 2007;42(4):288–294. doi: 10.1007/s00127-007-0171-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Fonville L, Drakesmith M, Zammit S, Lewis G, Jones DK, David AS.. MRI indices of cortical development in young people with psychotic experiences: influence of genetic risk and persistence of symptoms. Schizophr Bull. 2019;45(1):169–179. doi: 10.1093/schbul/sbx195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Fonville L, Cohen Kadosh K, Drakesmith M, et al. Psychotic experiences, working memory, and the developing brain: a multimodal neuroimaging study. Cereb Cortex. 2015;25(12):4828–4838. doi: 10.1093/cercor/bhv181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. van Os J. Is there a continuum of psychotic experiences in the general population? Epidemiol Psichiatr Soc. 2003;12(4):242–252. doi: 10.1017/s1121189x00003067 [DOI] [PubMed] [Google Scholar]
- 68. Degenhardt L, Saha S, Lim CCW, et al. The associations between psychotic experiences and substance use and substance use disorders: findings from the World Health Organization World Mental Health surveys. Addict Abingdon Engl. 2018;113(5):924–934. doi: 10.1111/add.14145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Henderson AS, Korten AE, Levings C, et al. Psychotic symptoms in the elderly: a prospective study in a population sample. Int J Geriatr Psychiatry. 1998;13(7):484–492. doi: [DOI] [PubMed] [Google Scholar]
- 70. Peters E, Ward T, Jackson M, et al. Clinical, socio-demographic and psychological characteristics in individuals with persistent psychotic experiences with and without a “need for care.”. World Psychiatry. 2016;15(1):41–52. doi: 10.1002/wps.20301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Thompson A, Lereya ST, Lewis G, Zammit S, Fisher HL, Wolke D.. Childhood sleep disturbance and risk of psychotic experiences at 18: UK birth cohort. Br J Psychiatry. 2015;207(1):23–29. doi: 10.1192/bjp.bp.113.144089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Dominguez M de G, Saka MC, can Saka M, Lieb R, Wittchen HU, van Os J.. Early expression of negative/disorganized symptoms predicting psychotic experiences and subsequent clinical psychosis: a 10-year study. Am J Psychiatry. 2010;167(9):1075–1082. doi: 10.1176/appi.ajp.2010.09060883 [DOI] [PubMed] [Google Scholar]
- 73. Hanssen M, Bak M, Bijl R, Vollebergh W, Os JV.. The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol. 2005;44(2):181–191. doi: 10.1348/014466505X29611 [DOI] [PubMed] [Google Scholar]
- 74. Krabbendam L, Janssen I, Bak M, Bijl RV, de Graaf R, van Os J.. Neuroticism and low self-esteem as risk factors for psychosis. Soc Psychiatry Psychiatr Epidemiol. 2002;37(1):1–6. doi: 10.1007/s127-002-8207-y [DOI] [PubMed] [Google Scholar]
- 75. Peters E, Ward T, Jackson M, et al. Clinical relevance of appraisals of persistent psychotic experiences in people with and without a need for care: an experimental study. Lancet Psychiatry. 2017;4(12):927–936. doi: 10.1016/S2215-0366(17)30409-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Steen Y van der, Myin-Germeys I, Nierop M van, et al. “False-positive” self-reported psychotic experiences in the general population: an investigation of outcome, predictive factors and clinical relevance. . Epidemiol Psychiatr Sci. 2019;28(5):532–543. doi: 10.1017/S2045796018000197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Saha S, Chant D, Welham J, McGrath J.. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2(5):e141e141. doi: 10.1371/journal.pmed.0020141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. McGrath J, Saha S, Welham J, El Saadi O, MacCauley C, Chant D.. A systematic review of the incidence of schizophrenia: the distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med. 2004;2(1):13. doi: 10.1186/1741-7015-2-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE.. Lifetime prevalence and age-of-onset distributions of DSM-iv disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- 80. Staines L, Healy C, Kelleher I, Cotter D, Burns A, Cannon M.. The association between transient childhood psychotic experiences and psychosocial outcomes in young adulthood: Examining the role of mental disorders and adult attachment. Early Interv Psychiatry. 2023. doi: 10.1111/eip.13382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Kelleher I, Harley M, Murtagh A, Cannon M.. Are screening instruments valid for psychotic-like experiences? a validation study of screening questions for psychotic-like experiences using in-depth clinical interview. Schizophr Bull. 2011;37(2):362–369. doi: 10.1093/schbul/sbp057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Kelleher I, Keeley H, Corcoran P, et al. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am J Psychiatry. 2013;170(7):734–741. doi: 10.1176/appi.ajp.2012.12091169 [DOI] [PubMed] [Google Scholar]
- 83. Healy C, Coughlan H, Clarke M, Kelleher I, Cannon M.. What mediates the longitudinal relationship between psychotic experiences and psychopathology? J Abnorm Psychol. 2020;129(5):505–516. doi: 10.1037/abn0000523 [DOI] [PubMed] [Google Scholar]
- 84. Knight C, Russo D, Stochl J, et al. Prevalence of and recovery from common mental disorder including psychotic experiences in the UK Primary Care Improving Access to Psychological Therapies (IAPT) Programme. J Affect Disord. 2020;272:84–90. doi: 10.1016/j.jad.2020.04.015 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.