Abstract
Background
Social determinants of health (SDoHs) are nonmedical factors that significantly impact health and longevity. We found no published reviews on the biology of SDoHs in schizophrenia-spectrum psychotic disorders (SSPD).
Study Design
We present an overview of pathophysiological mechanisms and neurobiological processes plausibly involved in the effects of major SDoHs on clinical outcomes in SSPD.
Study Results
This review of the biology of SDoHs focuses on early-life adversities, poverty, social disconnection, discrimination including racism, migration, disadvantaged neighborhoods, and food insecurity. These factors interact with psychological and biological factors to increase the risk and worsen the course and prognosis of schizophrenia. Published studies on the topic are limited by cross-sectional design, variable clinical and biomarker assessments, heterogeneous methods, and a lack of control for confounding variables. Drawing on preclinical and clinical studies, we propose a biological framework to consider the likely pathogenesis. Putative systemic pathophysiological processes include epigenetics, allostatic load, accelerated aging with inflammation (inflammaging), and the microbiome. These processes affect neural structures, brain function, neurochemistry, and neuroplasticity, impacting the development of psychosis, quality of life, cognitive impairment, physical comorbidities, and premature mortality. Our model provides a framework for research that could lead to developing specific strategies for prevention and treatment of the risk factors and biological processes, thereby improving the quality of life and increasing the longevity of people with SSPD.
Conclusions
Biology of SDoHs in SSPD is an exciting area of research that points to innovative multidisciplinary team science for improving the course and prognosis of these serious psychiatric disorders.
Keywords: epigenetics, microbiome, neurodevelopment, racism, social connections, oxytocin
Introduction
The importance of social and environmental factors for health has been known for millennia. Ancient Greeks defined health as a state of dynamic equilibrium between internal and external environment.1 Yet medicine has traditionally focused on assessments and interventions based on within-patient factors. Recently, the World Health Organization highlighted the contribution of nonmedical social determinants of health (SDoHs) such as childhood trauma, poverty, social isolation, and discrimination including racism, to health and healthcare disparities, and stressed a need for changing public health policies.2–4 Alternatively, and as a complement to genome and other omics, Wild5 introduced the concept of Exposome—a cumulative measure of environmental exposures and corresponding biological responses that can be derived from biological samples including blood, urine, and tissues.6 For both SDoHs and Exposome, the lists of proposed social factors have grown several folds.7,8 In the past, many schizophrenia researchers expected that genetics would explain most of the risk for this illness, and that social factors had little relevance in this regard. Heritability estimates from family studies are only partially explained by genetics, because discordance in SSPD occurs in roughly 50% of identical twin pairs.9
The exposome approach encompasses a life-course perspective from conception onwards and its impact on illnesses including schizophrenia.10 Similarly, the SDoH literature suggests these factors are associated with higher rates of schizophrenia-spectrum psychotic disorders (SSPD) and worse outcomes.11,12 Yet, how the SDoHs or the exposome biologically impact health in people with SSPD has received inadequate attention. In addition to characteristics of mental health (eg, positive and negative symptoms, long-term course, and psychotic relapses), health in SSPD includes cognitive functioning and physical health. Schizophrenia is notably characterized by high physical comorbidity including accelerated biological aging and a 15- to 20-year shorter lifespan compared to the general population. In recent decades, this longevity gap has increased, possibly because of worse access to healthy social and environmental factors in people with SSPD13 Long-term use of antipsychotics, especially atypicals, increases the risk of metabolic syndrome and heart disease, which contribute to premature mortality in patients with schizophrenia.14–17
The accompanying scoping review18 has focused on published studies of 9 major SDoHs in SSPD. Of these factors, at least some research has been conducted on early-life adversities, social disconnection, racism, poverty, migration, disadvantaged neighborhoods, and food insecurity, related to possible biological mechanisms through which these SDoHs might impact health outcomes. However, we did not find relevant neurobiological investigations of the other 2 major SDoHs – viz., homelessness and incarceration. Although some studies have reported damaging effects of incarceration on brain functioning,19,20 we found no such studies in people with SSPD.
Methods
We found no published review article with “biology of SDoHs in schizophrenia” in their titles or keywords. Therefore, we qualitatively reviewed and summarized the literature on biology relevant to each specified SDoH in SSPD, including investigations done in persons without SSPD or in animals. Given the broad scope of the topic of biology of SDoHs relevant to SSPD, we have sought to provide an overview and a selective review of the literature.
Results
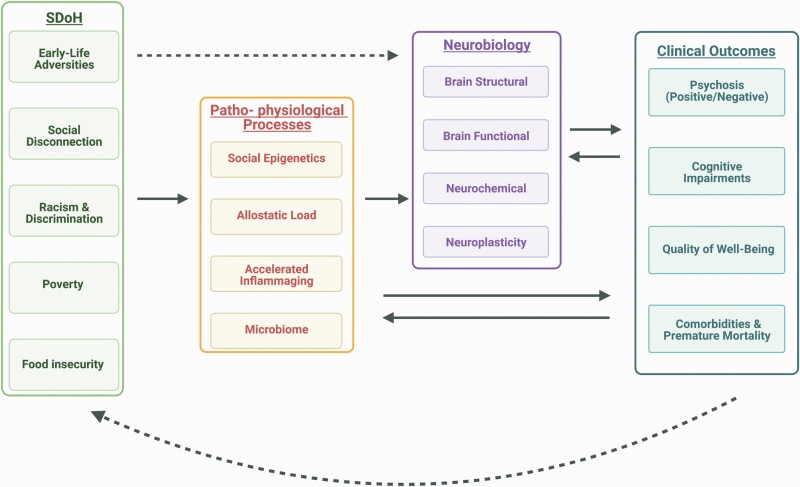
Below, we discuss a putative framework for considering the biological effects of SDoHs in persons with SSPD. figure 1 presents a proposed schema of the pathogenesis of adverse effects of SDoHs on clinical outcomes in SSPD through pathophysiological mechanisms impacting neurobiological processes. table 1 lists these components of the framework along with appropriate assessment measures. While some of these mechanisms are not directly based on empirical evidence in SSPD patients, there is indirect supportive evidence available from other human and animal studies. The main clinical outcome considered is the development of an SSPD, although secondary outcomes such as physical comorbidities and cognitive impairment are also important. Adverse clinical outcomes can exacerbate SDoHs, creating a vicious cycle. The framework presents, “in principle,” potential relations between SDoHs and biology, and should be considered a framework to guide future research on SSPD.
Fig. 1.
Proposed biological model of the effects of social determinants of health (SDoHs) on outcomes in schizophrenia-spectrum psychotic disorders.
Table 1.
Clinical and Biological Measures for Constructs in the Proposed Model of the Effects of SDoHs on Outcomes in SSPD
| (I) Social Determinants of Health (SDoHs) |
| Early-Life Adversities: Childhood Trauma Questionnaire; Composite International Diagnostic Interview; Bullying and Friendship Interview Schedule; Hospital Records |
| Social disconnection: Social Network Interview Schedule; WHO Quality of Life Scale Social Relationship subscale; (Modified) Social Support and Social Network Interview; Pattison Psychosocial Kinship Inventory |
| Racism and other forms of discrimination: Perceived Racism Scale; Experience of Discrimination scale; Everyday Discrimination Scale; Perceived Ethnic Discrimination Questionnaire—Community Version, with a Lifetime Exposure Discrimination subscale |
| Poverty: Direct Poverty Measure (income-based, official), Supplemental Poverty Measure (non-income resources based. |
| Food Insecurity: Food Insecurity Index |
| (II) Systemic Pathophysiological Processes (with Biomarkers): |
| Social epigenetics: DNA methylation (DNAm), Transposable Elements (TE) |
| Allostatic Load: Cortisol, Epinephrine, Norepinephrine, Systolic and Diastolic Blood pressure, Body Mass Index (BMI) |
| Accelerated Inflammaging: hs-CRP, IL-6, IL-8, TNF-α, Telomere Length, and Epigenetic markers |
| Microbiome: Alpha and Beta Diversity, Specific microbial species (relative abundance) |
| (III) Neurobiological Mechanisms (with Biological Assessments): |
| Brain Structural Changes: Structural MRI |
| Brain Functional Changes: Functional neuroimaging including fMRI, SPECT, PET, DTI |
| Neurochemical Changes: Oxytocin, Cortisol, and BDNF |
| Neuroplasticity: NMDA Receptor activity |
| (IV) Schizophrenia Phenotype or Clinical Outcomes |
| Symptoms of psychosis: Positive and Negative symptoms: Scales for Assessment of Positive and Negative Symptoms (SAPS and SANS, resp.) |
| Cognitive impairments: MATRICS neurocognitive battery |
| Quality of Well-Being: Medical Outcomes Study—Short Form-36 (MOS-SF-36) |
| Comorbidities and Premature Mortality: Cumulative Illness Rating Scale (CIRS) |
SSPD, Schizophrenia-Spectrum Psychotic Disorders; SDoHs, Social Determinants of Health.
Below we describe, systemic pathophysiological processes that affect various tissues and organs in the body, and neurobiological mechanisms that affect the nervous system, which are plausibly involved in the biological impact of SDoHs on SSPD. We summarize each of these constructs with a brief description and suggested assessment method/s, followed by a discussion of the reported associations between these constructs and SSPD-related SDoHs.
Systemic Pathophysiological Processes
Social Epigenetics.
The emerging field of social epigenetics concerns the molecular processes that modulate gene expression in response to exposures, including social environment. The main epigenetic processes studied which modify the expression of genes are DNA methylation (DNAm), histone modification, and the actions of noncoding RNA. Like DNA, epigenetic mechanisms are essential for cell functioning, but unlike DNA, epigenetic processes are metastable and can change over development. Some epigenetic patterns controlling gene expression may be inherited across generations. Conserved changes in global methylation and gene expression are observed across tissues in association with age, including the brain.21 The methylation profile in blood can serve as an “epigenetic clock” to compute an individual’s biological age, which may differ from their chronological age,22 with positive and negative life exposures contributing to variations in methylation profiles. DNA sequences have a very high fidelity of transmission across generations except for a small number of de novo point mutations arising in each generation. These new mutations contribute to serious psychiatric disorders such as SSPD.23 Mutations can disrupt the genes involved in epigenetic regulation or methylation binding sites to produce phenotypes analogous to epigenetic effects.24
Early-Life Adversities
Epigenetic effects from early-life stress have large effects in shaping neural circuit development and increase risk for subsequent psychopathology.25 Previous explanatory models included the “Developmental Origins of Disease,” which associates prenatal and early-life stressors with health outcomes,26 and the “Weathering” hypothesis, which considers how lived experiences of adversity, including marginalization and racism, cause physiological dysregulation, and accelerated aging.27 Current studies specifically support the stress-sensitive methylation of neurotransmitter signaling pathways that impact genes involved in neuronal survival, such as BDNF, and inflammatory pathways.28
Social Disconnection
Social disconnection can alter gene expression at any time in life, thus impairing neurobehavioral social processes in genetically susceptible individuals. Human and animal (voles, macaques) studies indicate that the susceptibility to negative effects of social adversity is associated with differential methylation or expression of the oxytocin receptor genes29–32 or serotonin transporter genes.33
Allostatic Load.
Allostatic load is a multisystem construct measuring the cumulative burden of stress on the body marked by physiological dysregulation.34 Unlike positive or tolerable stress, toxic stress results from strong, frequent, or prolonged activation of stress response systems. Persistent biological disruptions during developmentally sensitive periods can result in enduring structural changes and/or physiologic dysregulations leading to problems in physical, mental, and cognitive health. The most common index of allostatic load consists of 6 biomarkers: Cortisol, epinephrine, norepinephrine, systolic and diastolic blood pressure, and body mass index.35
Early-Life Adversities
Early, cumulative, and prolonged stress activation due to chronic aversive life conditions like greater neighborhood disadvantage in childhood or worsening neighborhood conditions over maturation predispose a person to psychosis,36,37 by increasing allostatic load.
Racism
Various forms of discrimination, raising allostatic load, are seen throughout life at higher rates among Black women in the United States.38 Maternal and fetal obstetrical complications including infections, maternal inflammation and stress, depressed fetal intrauterine growth, and fetal hypoxia are associated with increased risk of SSPD in the offspring.39These have been attributed to SDoHs including environmental exposures, neighborhood factors, discrimination, and stress. Black and Latinx women demonstrate lower cortisol levels and blunted cortisol response because of chronic exposure to discrimination and structural inequity.40 Cortisol is essential for fetal development, and low cortisol in late pregnancy is associated with greater risk of schizophrenia in the offspring.41
Migration
Migrants and refugees have an increased risk of SSPD, likely conferred pre-, peri-, and post-migration, from allostatic load caused by the trauma of forced migration, human rights violations, poverty, reduced healthcare access, economic limitations, and adverse interactions with the host culture.
Accelerated Inflammaging.
Inflammaging refers to an increase in systemic chronic inflammatory status that accelerates the biological aging process. SSPD is associated with accelerated aging, evidenced by multiple comorbidities with aging-related diseases such as diabetes, hypertension, and heart disease, resulting in premature mortality.13,42–46 This is driven largely by systemic inflammation and immune dysfunction, leading to a pro-inflammatory geno-pheno-type.47 Several studies have reported increased levels of biomarkers of inflammation in SSPD.46,48,49 A meta-analysis of studies of telomere length in leukocytes comparing individuals with schizophrenia and healthy controls showed mixed results.50 The difference between biological and chronological age is assessable by epigenetic “clocks,” which measure the degree of methylation at thousands of CpG sites.51 Measures of accelerated biological aging include blood levels of cytokines (hs-CRP, IL-6, IL-8, and TNF-α), telomere length, and epigenetic markers.45
Social Disconnection
The neuro-immune sequelae of social disconnection and social isolation are demonstrated in human and animal studies. In adult rhesus macaques living in a large outdoor field colony of 80–100 peers, individuals relocated to indoor single housing showed a 30%–50% reduction in circulating immune cells with upregulated pro-inflammatory monocytes and a 10%–20% reduction in Type I interferon antiviral gene expression.52 These immunological consequences of social isolation emerged within 48 hours and persisted for at least 2 weeks, resulting in markedly increased viral replication in blood cells and solid tissues. Social isolation is known to be associated with worse mental, cognitive, and physical health in SSPD, including greater mortality.53,54
Racism
Consonant with the weathering hypothesis mentioned above, persistent exposure to discrimination has been reported to predict inflammation leading to greater comorbidity, although the evidence regarding inflammation was inconsistent.55,56 A recent study57 found evidence supporting a link between discrimination among minoritized individuals and markers of inflammation – ie, IL-6, CRP, and fibrinogen. In Australian youth from Indigenous or ethnic minority backgrounds, racial discrimination was associated with increased BMI, waist circumference, systolic blood pressure, IL-6 and, marginally with TNF-α, after adjusting for sociodemographic covariates.58
Microbiome
The microbiome refers to the collection of microorganisms—including bacteria, archaea, microbial eukaryotes, fungi, and viruses—that inhabit the human body and that group’s genetic content. The microbial composition is impacted by pregnancy course, nutrition, stress, infections, medications, and other factors. Dysbiosis, or disruption of the gut microbial community, is associated with chronic inflammatory conditions. A healthy microbiome has potent anti-inflammatory effects that may mitigate epigenetic mechanisms signaling inflammation and accelerated aging.59,60 Gut microbiome-brain axis represents a network of chemical transmitters, neural connections, and immune signals facilitating bidirectional communication between gut microbiota and brain.61,62 Studies show significant inverse associations between food insecurity and cognitive function, particularly for general cognition and executive function.63 Although these studies did not include people with SSPD, both food insecurity and cognitive impairment are common in SSPD.
Social Disconnection
Microbial transfer between community members can promote fitness, and children raised in crowded households have higher microbial diversity, which is associated with better health.64 Social isolation, common in SSPD, may reduce microbial diversity and contribute to worse health. In a study of 184 community-dwelling older adults, within-subject gut microbial diversity correlated negatively with loneliness and positively with wisdom, compassion, social support, and social engagement.65
Disadvantaged Neighborhoods (Urbanicity and Lower Socioeconomic Status)
Built environments in biodiverse settings are more likely to have environmental microbes beneficial to the immune system.66 However, antimicrobial medications reduce microbial diversity. The “hygiene hypothesis” suggests that increased antimicrobial use leads to higher incidences of allergies and autoimmune conditions.67 Thus, an increasingly urbanized life could affect the microbiome and in turn, the immune dysregulation associated with SSPD.
Food Insecurity
Food intake affects microbiota directly. Increased fiber consumption is associated with gut microbiota-mediated protection against chronic inflammation, but such diets are less accessible to low-income and marginalized groups with food insecurity.68,69 TMAO (Trimethylamine-N-oxide), a compound linked to atherosclerosis and cardiovascular disease, is usually acquired through red meat.70 Nguyen et al.71 reported that individuals with schizophrenia had significantly lower loads of the enzyme that metabolizes TMAO. Additionally, upregulation of pathways related to short-chain fatty acid synthesis and tryptophan metabolism are associated with the schizophrenia gut microbiome.72
Neurobiological Mechanisms
Structural Brain Changes.
Brain structural changes are typically assessed with MRI.
Childhood Poverty
Reviews of the literature link childhood poverty to detrimental effects on neural development, using cross-sectional MRI data73 and heightened risk of later psychopathology, including psychotic symptoms.74,75 Perhaps due to “exposomal” factors,10 studies using MRI at one timepoint indicate youth living in poverty show lower total cortical brain volume, especially in prefrontal and subcortical regions, including hippocampus and amygdala, and altered connectivity between these regions.76–78 The North American Prodromal Longitudinal Study of youth at clinical high risk for psychosis showed in cross-sectional data that poverty was associated with lower hippocampal volume,79 and deprivation, in contrast to the experience of abuse, was associated with smaller cortical and right hippocampal volumes.80 A cross-sectional study examining chronic symptoms in 596 Latinx Americans reported qualitatively positive association between income and relative hippocampal volume in schizophrenia patients, but a negative association in controls.81 A recent large population-based Adolescent Brain Cognitive Development study, using cross-sectional data, found that global structural impairments, especially in volume, partially accounted for associations between poverty and psychotic-like experiences in mid-childhood.82 Longitudinal MRI analyses are required to disentangle the associations between poverty, neural development, and psychotic symptoms.
Social Disconnection
Cross-sectional work finds association of social disconnection with reduced gray matter volume in hippocampus and dorsolateral and orbitofrontal cortices.53,83 Social isolation increases the average time between psychosis onset and treatment initiation. Longitudinal MRI findings indicate longer durations of untreated psychosis result in greater hippocampal atrophy.84
Functional Brain Changes.
Functional neuroimaging is commonly employed to assess functional brain changes.
Racism and Neighborhood
Race-related negative life experiences reportedly produce lower amygdala reactivity in Blacks compared to Whites.85 Neighborhood disadvantages including crime and resource limitations are linked to increased amygdala-inferior parietal connectivity. Race-related discrimination is associated with greater salience network connectivity (amygdala-dorsal anterior cingulate cortex or ACC, amygdala-insula), spontaneous amygdala activity, and amygdala-thalamus functional connectivity in Black adults.86These alterations may alter connectivity with dorsolateral prefrontal cortex (DLPFC) and impair cognitive control including response inhibition and context maintenance. Parietal activation helps provide the DLPFC with the ability to shift attentional focus and information on learned stimulus–response pairings. The ACC is a part of the “control loop” necessary for detecting response conflict, and signaling when inhibition may improve task performance. Increased parietal activation and reduced ACC activation are associated with schizophrenia development among genetically high-risk persons.87
Neurochemical Changes.
Neurochemical systems that have been investigated in SSPD include oxytocin, cortisol, and brain-derived neurotrophic factor (BDNF). A recent review88 reported mixed results in 15 studies of oxytocin levels in serum or plasma of persons with schizophrenia as well as in 42 intervention trials of intranasal oxytocin as an augmentation to antipsychotics, most of which were double-blind randomized controlled trials. Glucocorticoid pathways, which impact the HPA axis, produce lasting effects on stress sensitivity and cortisol release, and reduce the neurotrophic effects of BDNF.89
Childhood Poverty
Impoverished environments can lead to extended HPA axis activation, resulting in altered glucocorticoid release, especially in regions with high glucocorticoid receptor expression like hippocampus, amygdala, and prefrontal cortex.90,91
When impacted by chronic stress, these regions may contribute to the development of psychotic symptoms.92–94
Social Disconnection
Neural correlates of social cognition and behavior in animal models and healthy humans suggest potential neurochemical mechanisms that might mediate the influence of SDoHs on schizophrenia. Social information is processed by specific neural circuits modulated by oxytocin, serotonin, dopamine, and other molecules.95 Rodents exposed to other intimidating rodents become submissive and develop a sensitized dopaminergic system; this “social defeat” has been proposed as a plausible (but unproven) model for schizophrenia.96 Numerous social stimuli trigger oxytocin release from hypothalamic neurons, including social touch97 and mutual eye contact.98 This release can modulate information processing early in sensory pathways99–101 to increase the salience of social stimuli and modulate neural plasticity. Social information is subsequently processed by a network of oxytocin-sensitive brain regions, including nucleus accumbens, which is critical for social reward learning, amygdala, which determines the valence of social stimuli, and hippocampus, which forms social memories. These neural processes culminate in behavioral output and endocrine signaling, which can have far-reaching effects on health and somatic physiology.102
Cannabis Use
The use of cannabis is widespread across ethnic and socioeconomic groups who use it for different reasons.103–106 Yet, Black and Latinx youth in the US report higher rates of smoking marijuana compared to their White counterparts.107 Emerging evidence suggests that location of108 and ease of access to dispensaries109,110 may be disproportionately greater for transitional-age minoritized youth. Dispensary density may be associated with hospitalization related to cannabis use, particularly among lower socioeconomic status (SES) or minoritized youth.111 Alcohol and tobacco literature also demonstrates increased use of these substances related to greater ease of access.112,113 Black and Latinx girls are disproportionately exposed to stress and trauma, including childhood maltreatment, poverty, and community violence, which are associated with early-onset cannabis114,115 consumption.116
Early, frequent cannabis use may increase the risk of psychosis 2-3-fold as repeated delta-9-tetrahydrocannabinol exposure leads to a decrease in the effective dopaminergic tone,117 as is seen with other drugs of abuse, resulting in flat affect and anhedonia. A British study revealed that daily use of potent cannabis products increased risk of psychotic disorder 5-folds,114 and a much larger European study of different population groups found in multivariate logistic regression that the risk from daily use of cannabis of varied potencies was only modestly dependent on the age of onset of use115—ie, frequency of use had a far greater impact.
A functional polymorphism in the catechol-O-methyltransferase (COMT) gene is associated with increased dopamine signaling and reduced prefrontal cortex dopamine levels.118 Adolescents with this polymorphism who use cannabis are at 5-fold greater risk of developing a psychotic disorder than those without.119 There is likely an interaction between level of adversity and cannabis use related to psychiatric outcomes.120 Cannabis use ranks among the topmost well-replicated environmental factors, including recreational drugs, relevant to developing schizophrenia in terms of effect size.121–123
Changes in Neuroplasticity.
Neuroplasticity refers to the ability of the brain to modify its function or structure in response to experience and use. Neuroplasticity consists of multiple mechanisms that allow the brain to learn and remember, predict and plan, coordinate and execute movements, and recover after injury. The mechanisms that underlie brain plasticity can be functional (changes in the physiology of a synapse) and/or structural (anatomical changes in the brain).124,125 NMDA receptors (NMDAR) are commonly studied to assess neuroplasticity.
Several lines of evidence suggest impaired neuroplasticity in schizophrenia, particularly through hypofunctional excitatory NMDARs.126,127 Hypofunctional NMDARs expressed on GABAergic neurons result in decreased inhibitory GABA production and release, and thus disinhibition of excitatory glutamatergic neurons and dysfunctional circuitry.128 Hypofunctional NMDARs on excitatory neurons reduce dopaminergic innervation and activity of glutamatergic and GABAergic neurons.129 Postmortem studies show altered expression of NMDAR subunits and related signaling molecules in schizophrenia.130 Genetic linkage studies identify several candidate susceptibility genes directly linked to NMDAR-mediated.131 A single photon emission tomography study showed reduced NMDARs in the hippocampus of medications-free individuals with schizophrenia.132 Clinically, NMDAR antagonists exacerbate symptoms in persons with schizophrenia and produce a psychotic state in healthy individuals that mimics positive, negative, and cognitive features of schizophrenia.133,134
Early-Life Adversities
In a finding relevant to SSPD, lower SES in childhood or downward SES trajectory starting from childhood was associated with lower blood flow in prefrontal cortex in adulthood.135 This suggests a deficit in activities that promote neuroplasticity during development, as neuroplasticity deficits can lead to lower blood flow in the prefrontal cortex attributable to the cerebrovascular processes.136 Thus, lower blood flow can be a marker of what occurred during brain development from certain childhood SDoHs, including low SES, threats, deprivation, and traumas,135 pointing toward a mechanism that deserves additional research.
Social Disconnection
Preclinical studies show a negative impact of social disconnection on prefrontal and hippocampal plasticity.137,138 Social isolation and its detrimental impact on plasticity could be an outcome of the illness itself, or an outcome of the interaction among other SDoHs.139There seems to be an interaction between gender and impact of social isolation on hippocampal plasticity and the potential of ketamine to rescue hippocampal plasticity.138 Women’s psychosis is more influenced by trauma compared to men, and consequently needs more trauma-informed interventions.140
Racism
Structural racism comprises multiple pathways which result in poor education, impoverished environments, limited access to care and recovery programs, and comorbidities, which are all associated directly or indirectly with impaired neuroplasticity.
Discussion
Schizophrenia is caused, in part, by a number of genes; however, social factors such as early-life adversities including childhood poverty increase that risk significantly through epigenetics and other processes. Other SDoHs such as social isolation, racism, migration, and socioeconomically disadvantaged neighborhoods contribute to cumulative toxic stress, which increases allostatic load and leads to accelerated biological aging. These pathophysiological perturbations can result in specific pathological changes in brain structure, function, chemistry, and neuroplasticity. The resulting neuro-psycho-physical pathology leads to greater severity and worse course of the illness along with increased physical comorbidity and premature mortality.
Collectively, research suggests that, through systemic pathophysiological and neurobiological processes, SDoHs such as early-life adversities, social disconnection, racism, and poverty interact with psychological and biological factors to form a vicious cycle in which each contributing factor exacerbates the adverse impact of others. While these pathways have not yet been explicitly examined in the context of psychosis, it is plausible that these processes may be at play in linking SDoHs to increased risk and severity of schizophrenia and worse course and prognosis. Based on the limitations of the published research (see below), it is difficult to establish a definitive sequence of events that associate SDoHs with pathological changes at systemic and neurobiological levels, leading to greater incidence of and worse outcomes in SSPD. However, several areas where possible explanations of this type have been offered are listed below.
(1) Some investigators141,142 have proposed a Bayesian model for higher rates of schizophrenia among migrants, refugees, and marginalized communities who experience severe stress from discrimination and social exclusion. These adverse experiences challenge the individuals’ prior knowledge and social trust that existed in their earlier social life, leading to increased focus on current environmental stimuli, particularly when the persons feel threatened. Those at high risk for psychosis may overinterpret or misinterpret ambiguous or unfamiliar situations as being hostile. This stimulates stress-associated increases in striatal dopaminergic neurotransmission and reduces prefrontal dopamine release, impairing cortical processing of unfamiliar or threatening stimuli and leading to paranoid thinking.
(2) Cacioppo, Cole, and colleagues have postulated a bidirectional association between social isolation and adverse pathophysiological and neurobiological effects, resulting in a vicious neurobehavioral cycle.143–148 In the absence of a supportive social community, a systemic network of threat detection and response circuits activates the sympathetic nervous system, altering immune cell gene expression and cell development via beta-adrenergic signaling pathways in the blood, lymphoid organs, and bone marrow, resulting in increased inflammatory biology.143–148 This “conserved transcriptional response to adversity,” which was adaptive in ancestral times, incurs substantial health costs in modern cultural conditions where social disconnection becomes chronic.145,149 On the other hand, peripheral immune activity can reciprocally regulate brain function in general and neurobiological substrates of social connection in particular.149,150 Circulating pro-inflammatory cytokines can trigger the brain to release a package of “sickness behaviors” that includes fatigue, anxiety, and reduced social motivation. The resultant reductions in social interaction may trigger a vicious cycle of social disconnection, inflammatory defense response, and further withdrawal.151–156 These biological threat responses are amplified among individuals from lower socioeconomic strata or unsafe physical environments such as violent neighborhoods.157,158
(3) The social defeat hypothesis of SSPD159 states that the negative experience of social exclusion leads to sensitization or increased baseline activity of mesolimbic dopamine system, increasing the risk of SSPD in early-generation migrants.159 However, limitations of this hypothesis include unclear definition and presumed immeasurability of social defeat.160
(4) Cannabis use is a major risk factor for SSPD, especially in minoritized youth.109,111,122,123 The mechanism by which THC increases vulnerability to psychosis is well-described, via mesolimbic dopaminergic projections from ventral tegmental area to nucleus accumbens, identified in positive symptoms161 and incentive salience.162 Importantly, cannabis exposure is preventable.
(5) Muscatell et al.’s model56 describes possible neural and inflammatory mechanisms linking racism and health. Racism may disrupt connectivity among the salience, default mode, and executive control networks, leading to greater sympathetic nervous system signaling, HPA axis activation, and increased expression of pro-inflammatory genes. Persistence of such pathology results in chronic physical and mental health conditions. This model relates to serious mental illnesses including SSPD.
The literature reviewed has several limitations. Most of the published clinical studies were cross-sectional, employed variable clinical, and biomarker assessments, had different sample sizes, and often did not control for various interacting and confounding variables. Some of the studies, although relevant to this topic, did not include persons with SSPD. There are excellent studies in animals that appear relevant to schizophrenia, although the animal models of schizophrenia used had important limitations.163 A majority of the studies focused on the risk of developing schizophrenia although a few examined other important health outcomes such as severity of psychopathology and physical comorbidity. A barrier to understanding neurobiology of SDoHs in SSPD is a lack of longitudinal studies using validated clinical and biological measures to test model-based causal hypotheses. Such research is critical for developing biologically based interventions as well as prevention strategies. Our review is a first step in that process.
The putative model presented in figure 1 and table 1 offers a possible conceptual framework for designing future studies of how specific SDoHs increase the risk and worsen the outcomes in people with SSPD. Prospective longitudinal investigations with large samples of diverse groups of persons with SSPD and well-matched comparison individuals, employing the various suggested measures and sophisticated multivariate statistical analyses are warranted.
There is also a critical need for developing and testing interventions, both income-based and service-based, in children and adults with schizophrenia, at the biological level. Examining the biological effects of interventions will provide objective, measurable evidence regarding the benefits of the interventions and also deeper insights into how certain experiences can have lasting effects on behavior and health. Below are some examples of intervention research relevant to biology of SDoHs.
Social Integration.
The interface between peripheral threat responses and central nervous system-mediated social motivation creates a complex feedback network that likely evolved to maintain social resilience under favorable social conditions but can inadvertently perpetuate social disadvantages under unfavorable conditions.151,152 However, this reciprocal regulatory system also offers counterintuitive opportunities to break the vicious cycle of social isolation and biological defense by engaging in prosocial activity, which has been found to be surprisingly effective in reducing perceptions of social isolation, lowering inflammatory pathology, and enhancing antiviral immune response.164–167 Pragmatic interventions promoting positive social interactions should be tested.
Social Safety Net and Resilience.
Previous work indicates that an increased social safety net may mitigate the impact of poverty on brain development and may, therefore, lower the risk of developing psychosis spectrum symptoms.168 A recent study reported strong associations between childhood poverty with its neural effects and psychosis spectrum symptoms.82 It is also important to investigate to what extent resilience and social support interact to attenuate the risk of poverty-associated structural neural impairments and development of psychosis.
Oxytocin.
Some evidence suggests that interventions timed around an individual’s first episode of psychosis might delay or reduce the risk of progression to schizophrenia by disrupting this cycle.169 Given its role in social cognition, the oxytocin system is a promising therapeutic target for alleviating the negative symptoms of schizophrenia. However, while oxytocin increases the salience of social information and facilitates social learning, it does not necessarily induce prosocial behavior.170 As such, it is critical to pair any oxytocin-mediated therapy with a positive psychosocial therapeutic strategy to enhance social learning and reinforce the rewarding properties of social interactions.171,172 This approach has recently shown efficacy in treating other psychiatric disorders with social deficits, including autism173 and post-traumatic stress disorder or PTSD.174 If effective for schizophrenia, oxytocin-based pharmaco-psycho-social interventions might do more than alleviate symptoms – they might also mitigate the biopsychosocial feedback loop contributing to disease progression.
Maternal and Childhood Nutrition
Maternal.
Obesity during pregnancy is associated with increased risk of neurodevelopmental disorders, including autism spectrum disorder, in the offspring.175 In an animal study, maternal high-fat diet (MHFD) induced a shift in microbial ecology that negatively impacted offspring’s social behavior.175 Social deficits and gut microbial dysbiosis in MHFD offspring were prevented by co-housing with offspring of mothers on a regular diet (MRD). MHFD offspring had fewer oxytocin immunoreactive neurons in the hypothalamus than MRD offspring. Using metagenomics and precision microbiota reconstitution, the investigators identified a single commensal strain, L. reuteri, that increased oxytocin levels and corrected social deficits in MHFD offspring. If extrapolated to humans, these findings suggest that future probiotic treatment may relieve behavioral abnormalities associated with neurodevelopmental disorders.176
Childhood.
To date, there is very little published research on childhood nutrition in relationship to psychosis risk. One study reported marginal evidence for an association between altered levels of omega-6 fatty acids in childhood and increased risk of later psychosis,177 but more work is clearly warranted.
Neurostimulation.
Noninvasive Brain Stimulation (NIBS) comprises several modalities that modulate brain activities, including electrical and magnetic forms of stimulation. NIBS is believed to cause therapeutic effects by targeting neuroplasticity-based mechanisms.178,179 NIBS, through its modulation of brain plasticity, has the potential to remedy cognitive impairment or, also, if appropriately timed, provide resilience against adverse SDoHs’ detrimental effects. It may be combined with trauma-informed treatments, especially in women with schizophrenia having a history of early-life adversities.140
In sum, the proposed biological model points to the direction of future research that could suggest specific strategies for prevention and treatment of the risk factors, thereby promoting better mental, physical, and cognitive health in people with SSPD. We believe that biology of SDoHs in schizophrenia is an exciting new frontier for research that has a strong potential for innovative multidisciplinary team science which can markedly improve the symptoms, course, and prognosis of this serious and life-shortening illness.
Supplementary Material
Acknowledgment
We thank (1) Vivian Pender, MD, for making Social Determinants of Mental Health her 2021–2022 Presidential Theme for the American Psychiatric Association, and appointing a Task Force, (2) Aurelie Menigoz, PhD, for her artistic contribution in designing figure 1, (3) Varsha D. Badal, PhD, for helping with the bibliography, and (4) The anonymous reviewers of this manuscript who suggested invaluable improvements.
Contributor Information
Dilip V Jeste, Department of Psychiatry, University of California, San Diego (Retired), CA, USA.
Dolores Malaspina, Departments of Psychiatry, Neuroscience and Genetics, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
Kara Bagot, Department of Psychiatry, Addiction Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
Deanna M Barch, Departments of Psychological and Brain Sciences, Psychiatry, and Radiology, Washington University in St. Louis, St. Louis, MO, USA.
Steve Cole, Departments of Psychiatry and Biobehavioral Sciences, and Medicine, University of California, Los Angeles, CA, USA.
Faith Dickerson, Department of Psychology, Sheppard Pratt, Baltimore, MD, USA.
Amanda Dilmore, Department of Pediatrics, University of California, San Diego, CA, USA.
Charles L Ford, Center for Translational Social Neuroscience, Department of Psychiatry, Emory University, Atlanta, GA, USA.
Nicole R Karcher, Department of Psychiatry, Washington University in St. Louis, St. Louis, MO, USA.
Joan Luby, Department of Psychiatry (Child), Washington University in St. Louis, St. Louis, MO, USA.
Tarek Rajji, Adult Neurodevelopment and Geriatric Psychiatry Division, Centre for Addiction and Mental Health, Toronto, ON, Canada.
Adrián A Pinto-Tomas, Biochemistry Department, School of Medicine, Universidad de Costa Rica, San José, Costa Rica.
Larry J Young, Center for Translational Social Neuroscience, Department of Psychiatry, Emory University, Atlanta, GA, USA.
Funding
The contribution of AAPT was supported by the Space for Advanced Studies of the University of Costa Rica (UCREA), UCR project B9-333 and the International Life Sciences Institute (ILSI), UCR project C0325. The contribution of DM was supported by NIH R01 Grants MH110418 and MH104964. The contribution of DMB was supported by NIH Grants U01DA041120 and R01MH066031. The contributions of DVJ and SC were supported by NIMH grant 2R01MH094151-08. The contribution of FD was supported by SMRI grant 07R-1690. The contribution of JL was supported by NIMH grant R01MH113883. The contribution of LJY was supported by NIH Grants P50MH100023 and OD P51OD011132. The contribution of NK was supported by NIH Grant K23MH121792-01. All the Authors have declared that they have no conflicts of interest in relation to the subject of this study.
Presentation
A part of this research was presented at the annual conference of the American College of Neuropsychopharmacology (ACNP) in a Study Group co-chaired by Dilip Jeste and Dolores Malaspina, on December 7, 2022, in Phoenix, Arizona, USA.
References
- 1. Tountas Y. The historical origins of the basic concepts of health promotion and education: the role of ancient Greek philosophy and medicine. Health Promot Int. 2009;24(2):185–192. [DOI] [PubMed] [Google Scholar]
- 2. Wilkinson RG, Marmot M, Organization WH.. Social determinants of health: the solid facts: Copenhagen: WHO Regional Office for Europe; 1998. [Google Scholar]
- 3. WHO. Commission on Social Determinants of Health, Closing the gap in a generation: health equity through action on the social determinants of health: final report of the commission on social determinants of health. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 4. WHO. Prevention of mental disorders: effective interventions and policy options: Summary report. Geneva, Switzerland: World Health Organization; 2004.
- 5. Wild CP. Complementing the genome with an “exposome”: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol Biomarkers Prev. 2005;14(8):1847–1850. [DOI] [PubMed] [Google Scholar]
- 6. Miller GW. Integrating the exposome into a multi-omic research framework. Exposome. 2021;1(1):osab002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Islam MM. Social determinants of health and related inequalities: confusion and implications. Front Public Health. 2019;7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Buck Louis GM, Smarr MM, Patel CJ.. The exposome research paradigm: an opportunity to understand the environmental basis for human health and disease. Curr Environ Health Rep. 2017;4(1):89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gottesman II, Shields J.. A polygenic theory of schizophrenia. Int. J. Ment. Health Syst. 1972;1(1–2):107–115. [Google Scholar]
- 10. Pries LK, Erzin G, Rutten BPF, van Os J, Guloksuz S.. Estimating aggregate environmental risk score in psychiatry: the exposome score for schizophrenia. Front Psychiatry. 2021;12:671334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Compton MT, Shim RS.. The social determinants of mental health. Focus. 2015;13(4):419–425. [Google Scholar]
- 12. Jeste DV, Pender VB.. Social determinants of mental health: recommendations for research, training, practice, and policy. JAMA psychiatry. 2022;79(4):283–284. [DOI] [PubMed] [Google Scholar]
- 13. Lee EE, Liu J, Tu X, Palmer BW, Eyler LT, Jeste DV.. A widening longevity gap between people with schizophrenia and general population: a literature review and call for action. Schizophr Res. 2018;196:9–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jin H, Meyer JM, Mudaliar S, Jeste DV.. Impact of atypical antipsychotic therapy on leptin, ghrelin, and adiponectin. Schizophr Res. 2008;100(1-3):70–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jin H, Shih P-aB, Golshan S, et al. Comparison of longer-term safety and effectiveness of 4 atypical antipsychotics in patients over age 40: a trial using equipoise-stratified randomization. J Clin Psychiatry. 2012;73(1):3483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kahl KG, Westhoff-Bleck M, Krüger TH.. Effects of psychopharmacological treatment with antipsychotic drugs on the vascular system. Vascul Pharmacol. 2018;100:20–25. [DOI] [PubMed] [Google Scholar]
- 17. Sjo CP, Stenstrøm AD, Bojesen AB, Frølich JS, Bilenberg N.. Development of metabolic syndrome in drug-naive adolescents after 12 months of second-generation antipsychotic treatment. J Child Adolesc Psychopharmacol. 2017;27(10):884–891. [DOI] [PubMed] [Google Scholar]
- 18. Jester D, Thomas M, Sturm ET, et al. Social determinants of health for schizophrenia spectrum disorders. Schizophrenia Bulletin. 2023;49:837–850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bradshaw EA. Tombstone towns and toxic prisons: prison ecology and the necessity of an anti-prison environmental movement. Critical Criminology. 2018;26:407–422. [Google Scholar]
- 20. Ligthart S, Van Oploo L, Meijers J, Meynen G, Kooijmans T.. Prison and the brain: neuropsychological research in the light of the European Convention on Human Rights. New J Eur Crim Law. 2019;10(3):287–300. [Google Scholar]
- 21. Horvath S, Zhang Y, Langfelder P, et al. Aging effects on DNA methylation modules in human brain and blood tissue. Genome Biol. 2012;13(10):R971–R918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hannum G, Guinney J, Zhao L, et al. Genome-wide methylation profiles reveal quantitative views of human aging rates. Mol Cell. 2013;49(2):359–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Acuna-Hidalgo R, Veltman JA, Hoischen A.. New insights into the generation and role of de novo mutations in health and disease. Genome Biol. 2016;17(1):241. doi:10.1186/s13059-016-1110-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Milekic M, Xin Y, O’donnell A, et al. Age-related sperm DNA methylation changes are transmitted to offspring and associated with abnormal behavior and dysregulated gene expression. Mol Psychiatry. 2015;20(8):995–1001. [DOI] [PubMed] [Google Scholar]
- 25. Malave L, van Dijk MT, Anacker C.. Early life adversity shapes neural circuit function during sensitive postnatal developmental periods. Transl Psychiatry. 2022;12(1):306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gluckman PD, Hanson MA.. Developmental origins of disease paradigm: a mechanistic and evolutionary perspective. Pediatr Res. 2004;56(3):311–317. [DOI] [PubMed] [Google Scholar]
- 27. Geronimus AT. The weathering hypothesis and the health of African-American women and infants: evidence and speculations. Ethn Dis Summer. 1992;2(3):207–221. [PubMed] [Google Scholar]
- 28. Ray M, Wallace MK, Grayson SC, et al. Epigenomic links between social determinants of health and symptoms: a scoping review. Biol Res Nurs. 2022;10998004221147300. doi:10.1177/10998004221147300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Baker M, Lindell SG, Driscoll CA, et al. Early rearing history influences oxytocin receptor epigenetic regulation in rhesus macaques. Proc Natl Acad Sci U S A. 2017;114(44):11769–11774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Smearman EL, Almli LM, Conneely KN, et al. Oxytocin receptor genetic and epigenetic variations: association with child abuse and adult psychiatric symptoms. Child Dev. 2016;87(1):122–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Danoff JS, Wroblewski KL, Graves AJ, et al. Genetic, epigenetic, and environmental factors controlling oxytocin receptor gene expression. Clin Epigenetics. 2021;13(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Barrett CE, Arambula SE, Young LJ.. The oxytocin system promotes resilience to the effects of neonatal isolation on adult social attachment in female prairie voles. Transl Psychiatry. 2015;5(7):e606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gianaros PJ, Manuck SB.. Neurobiological pathways linking socioeconomic position and health. Psychosom Med. 2010;72(5):450–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rodriquez EJ, Kim EN, Sumner AE, Nápoles AM, Pérez-Stable EJ.. Allostatic load: importance, markers, and score determination in minority and disparity populations. J Urban Health. 2019;96(suppl 1):3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Whelan E, O’Shea J, Hunt E, Dockray S.. Evaluating measures of allostatic load in adolescents: a systematic review. Psychoneuroendocrinology. 2021;131:105324. [DOI] [PubMed] [Google Scholar]
- 36. Hastings PD, Serbin LA, Bukowski W, et al. Predicting psychosis-spectrum diagnoses in adulthood from social behaviors and neighborhood contexts in childhood. Dev Psychopathol. 2020;32(2):465–479. [DOI] [PubMed] [Google Scholar]
- 37. Morgan C. Migration, ethnicity and psychosis. In: Psychotic disorders: Comprehensive Conceptualization and Treatments. Tamminga, C.A., Jim van Os, and Elena Ivleva, M.D. eds. New York: Oxford University Press; 2020. [Google Scholar]
- 38. Menon R, Dunlop AL, Kramer MR, Fortunato SJ, Hogue CJ.. An overview of racial disparities in preterm birth rates: caused by infection or inflammatory response? Acta Obstet Gynecol Scand. 2011;90(12):1325–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Davies C, Segre G, Estradé A, et al. Prenatal and perinatal risk and protective factors for psychosis: a systematic review and meta-analysis. Lancet Psychiatry. 2020;7(5):399–410. [DOI] [PubMed] [Google Scholar]
- 40. Glynn LM, Schetter CD, Chicz-DeMet A, Hobel CJ, Sandman CA.. Ethnic differences in adrenocorticotropic hormone, cortisol and corticotropin-releasing hormone during pregnancy. Peptides. 2007;28(6):1155–1161. [DOI] [PubMed] [Google Scholar]
- 41. Ellman LM, Murphy SK, Maxwell SD, et al. Maternal cortisol during pregnancy and offspring schizophrenia: influence of fetal sex and timing of exposure. Schizophr Res. 2019;213:15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kirkpatrick B, Messias E, Harvey PD, Fernandez-Egea E, Bowie CR.. Is schizophrenia a syndrome of accelerated aging? Schizophr Bull. 2008;34(6):1024–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Jeste DV, Wolkowitz OM, Palmer BW.. Divergent trajectories of physical, cognitive, and psychosocial aging in schizophrenia. Schizophr Bull. 2011;37(3):451–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Jeste DV. Neurobiology of “positive psychiatry.”. Schizophr Bull. 2022;48(3):533–535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Nguyen TT, Eyler LT, Jeste DV.. Systemic biomarkers of accelerated aging in schizophrenia: a critical review and future directions. Schizophr Bull. 2018;44(2):398–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Campeau A, Mills RH, Stevens T, et al. Multi-omics of human plasma reveals molecular features of dysregulated inflammation and accelerated aging in schizophrenia. Mol Psychiatry. 2022;27(2):1217–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rath S, Hawsawi YM, Alzahrani F, Khan MI.. Epigenetic regulation of inflammation: The metabolomics connection. Semin Cell Dev Biol. 2022:S1084-9521(22)00270-1. doi:10.1016/j.semcdb.2022.09.008. [DOI] [PubMed] [Google Scholar]
- 48. Adamowicz DH, Shilling PD, Palmer BW, et al. Associations between inflammatory marker profiles and neurocognitive functioning in people with schizophrenia and non-psychiatric comparison subjects. J Psychiatr Res. 2022;149:106–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Klaus F, Nguyen TT, Thomas ML, et al. Peripheral inflammation levels associated with degree of advanced brain aging in schizophrenia. Front Psychiatry. 2022;13:966439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Polho G, De-Paula V, Cardillo G, Dos Santos B, Kerr D.. Leukocyte telomere length in patients with schizophrenia: a meta-analysis. Schizophr Res. 2015;165(2–3):195–200. [DOI] [PubMed] [Google Scholar]
- 51. Horvath S. DNA methylation age of human tissues and cell types. Genome Biol. 2013;14(10):R115R115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Cole SW, Cacioppo JT, Cacioppo S, et al. The Type I interferon antiviral gene program is impaired by lockdown and preserved by caregiving. Proc Natl Acad Sci USA. 2021;118(29):e2105803118. doi:10.1073/pnas.2105803118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Eglit GML, Palmer BW, Martin AS, Tu X, Jeste DV.. Loneliness in schizophrenia: construct clarification, measurement, and clinical relevance. PLoS One. 2018;13(3):e0194021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. National Academies of Sciences E, Medicine. Social isolation and loneliness in older adults: Opportunities for the health care system. Washington, DC:National Academies Press; 2020. [PubMed] [Google Scholar]
- 55. Simons RL, Lei MK, Klopack E, Zhang Y, Gibbons FX, Beach SRH.. Racial discrimination, inflammation, and chronic illness among african american women at midlife: support for the weathering perspective. J Racial Ethn Health Disparities. 2021;8(2):339–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Muscatell KA, Alvarez GM, Bonar AS, et al. Brain–body pathways linking racism and health. Am Psychol. 2022;77(9):1049–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Surachman A, Jenkins AI, Santos AR, Almeida DM.. Socioeconomic status trajectories across the life course, daily discrimination, and inflammation among Black and white adults. Psychoneuroendocrinology. 2021;127:105193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Priest N, Truong M, Chong S, et al. Experiences of racial discrimination and cardiometabolic risk among Australian children. Brain Behav Immun. 2020;87:660–665. [DOI] [PubMed] [Google Scholar]
- 59. Bidell MR, Hobbs ALV, Lodise TP.. Gut microbiome health and dysbiosis: A clinical primer. Pharmacotherapy. 2022.;42:849–857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Agus A, Clément K, Sokol H.. Gut microbiota-derived metabolites as central regulators in metabolic disorders. Gut. 2021;70(6):1174–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Dickerson F, Dilmore AH, Godoy-Vitorino F, et al. The microbiome and mental health across the lifespan. Curr Top Behav Neurosci. 2023;61:119–140. doi:10.1007/7854_2022_384. [DOI] [PubMed] [Google Scholar]
- 62. Morais LH, Schreiber HL, Mazmanian SK.. The gut microbiota-brain axis in behaviour and brain disorders. Nat Rev Microbiol. 2021;19(4):241–255. [DOI] [PubMed] [Google Scholar]
- 63. Royer MF, Guerithault N, Braden BB, Laska MN, Bruening M.. Food insecurity is associated with cognitive function: a systematic review of findings across the life course. J. Transl. Med. 2021;1(3):205–222. [Google Scholar]
- 64. Sherwin E, Bordenstein SR, Quinn JL, Dinan TG, Cryan JF.. Microbiota and the social brain. Science. 2019;366(6465):eaar2016. doi:10.1126/science.aar2016. [DOI] [PubMed] [Google Scholar]
- 65. Nguyen TT, Zhang X, Wu T-C, et al. Association of loneliness and wisdom with gut microbial diversity and composition: an exploratory study. Front Psychiatry. 2021;12:395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Gilbert JA, Stephens B.. Microbiology of the built environment. Nat Rev Microbiol. 2018;16(11):661–670. [DOI] [PubMed] [Google Scholar]
- 67. Eder W, von Mutius E.. Hygiene hypothesis and endotoxin: what is the evidence? Curr Opin Allergy Clin Immunol. 2004;4(2):113–117. [DOI] [PubMed] [Google Scholar]
- 68. Storey M, Anderson P.. Income and race/ethnicity influence dietary fiber intake and vegetable consumption. Nutr Res. 2014;34(10):844–850. [DOI] [PubMed] [Google Scholar]
- 69. Zagorsky JL, Smith PK.. The association between socioeconomic status and adult fast-food consumption in the U.S. Econ Hum Biol. 2017;27(Pt A):12–25. [DOI] [PubMed] [Google Scholar]
- 70. Koeth RA, Wang Z, Levison BS, et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat Med. 2013;19(5):576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Nguyen TT, Kosciolek T, Daly RE, et al. Gut microbiome in Schizophrenia: altered functional pathways related to immune modulation and atherosclerotic risk. Brain Behav Immun. 2021;91:245–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Zhu F, Ju Y, Wang W, et al. Metagenome-wide association of gut microbiome features for schizophrenia. Nat Commun. 2020;11(1):1612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Johnson SB, Riis JL, Noble KG.. State of the art review: poverty and the developing brain. Pediatrics. 2016;137(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Matheson SL, Shepherd AM, Pinchbeck RM, Laurens KR, Carr VJ.. Childhood adversity in schizophrenia: a systematic meta-analysis. Psychol Med. 2013;43(2):225–238. [DOI] [PubMed] [Google Scholar]
- 75. O’Donoghue B, Roche E, Lane A.. Neighbourhood level social deprivation and the risk of psychotic disorders: a systematic review. Soc Psychiatry Psychiatr Epidemiol. 2016;51(7):941–950. [DOI] [PubMed] [Google Scholar]
- 76. Luby J, Belden A, Botteron K, et al. The effects of poverty on childhood brain development: the mediating effect of caregiving and stressful life events. JAMA Pediatr. 2013;167(12):1135–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Barch D, Pagliaccio D, Belden A, et al. Effect of hippocampal and amygdala connectivity on the relationship between preschool poverty and school-age depression. Am J Psychiatry. 2016;173(6):625–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Noble KG, Houston SM, Brito NH, et al. Family income, parental education and brain structure in children and adolescents. Nat Neurosci. 2015;18(5):773–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Ku BS, Aberizk K, Addington J, et al. The association between neighborhood poverty and hippocampal volume among individuals at clinical high-risk for psychosis: the moderating role of social engagement. Schizophr Bull. 2022;48(5):1032–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. LoPilato AM, Goines K, Addington J, et al. Impact of childhood adversity on corticolimbic volumes in youth at clinical high-risk for psychosis. Schizophr Res. 2019;213:48–55. [DOI] [PubMed] [Google Scholar]
- 81. Crossley NA, Zugman A, Reyes-Madrigal F, et al. ; ANDES Network. Structural brain abnormalities in schizophrenia in adverse environments: examining the effect of poverty and violence in six Latin American cities. Br J Psychiatry. 2021;218(2):112–118. [DOI] [PubMed] [Google Scholar]
- 82. Karcher NR, Schiffman J, Barch DM.. Environmental risk factors and psychotic-like experiences in children aged 9-10. J Am Acad Child Adolesc Psychiatry. 2021;60(4):490–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Morr M, Liu X, Hurlemann R, Becker B, Scheele D.. Chronic loneliness: neurocognitive mechanisms and interventions. Psychother Psychosom. 2022;91(4):227–237. [DOI] [PubMed] [Google Scholar]
- 84. Goff DC, Zeng B, Ardekani BA, et al. Association of hippocampal atrophy with duration of untreated psychosis and molecular biomarkers during initial antipsychotic treatment of first-episode psychosis. JAMA Psychiatry. 2018;75(4):370–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Harnett NG, Wheelock MD, Wood KH, et al. Negative life experiences contribute to racial differences in the neural response to threat. Neuroimage. 2019;202:116086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Clark US, Miller ER, Hegde RR.. Experiences of discrimination are associated with greater resting amygdala activity and functional connectivity. Biol Psychiatry Cogn Neurosci Neuroimaging 2018;3(4):367–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Whalley HC, Simonotto E, Moorhead W, et al. Functional imaging as a predictor of schizophrenia. Biol Psychiatry. 2006;60(5):454–462. [DOI] [PubMed] [Google Scholar]
- 88. Goh KK, Chen C-H, Lane H-Y.. Oxytocin in schizophrenia: pathophysiology and implications for future treatment. Int J Mol Sci . 2021;22(4):2146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Daskalakis NP, De Kloet ER, Yehuda R, Malaspina D, Kranz TM.. Early life stress effects on glucocorticoid-BDNF interplay in the hippocampus. Front Mol Neurosci. 2015;8:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. McEwen BS, Nasca C, Gray JD.. Stress effects on neuronal structure: hippocampus, amygdala, and prefrontal cortex. Neuropsychopharmacology. 2016;41(1):3–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Sapolsky RM, Krey LC, McEwen BS.. Glucocorticoid-sensitive hippocampal neurons are involved in terminating the adrenocortical stress response. Proc Natl Acad Sci USA. 1984;81(19):6174–6177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. McHugo M, Armstrong K, Roeske MJ, Woodward ND, Blackford JU, Heckers S.. Hippocampal volume in early psychosis: a 2-year longitudinal study. Transl Psychiatry. 2020;10(1):306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Allen P, Luigjes J, Howes OD, et al. Transition to psychosis associated with prefrontal and subcortical dysfunction in ultra high-risk individuals. Schizophr Bull. 2012;38(6):1268–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. van Erp TG, Hibar DP, Rasmussen JM, et al. Subcortical brain volume abnormalities in 2028 individuals with schizophrenia and 2540 healthy controls via the ENIGMA consortium. Mol Psychiatry. 2016;21(4):547–553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Froemke RC, Young LJ.. Oxytocin, Neural plasticity, and social behavior. Annu Rev Neurosci. 2021;44:359–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Selten JP, van der Ven E, Rutten BP, Cantor-Graae E.. The social defeat hypothesis of schizophrenia: an update. Schizophr Bull. 2013;39(6):1180–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Tang Y, Benusiglio D, Lefevre A, et al. Social touch promotes interfemale communication via activation of parvocellular oxytocin neurons. Nat Neurosci. 2020;23(9):1125–1137. [DOI] [PubMed] [Google Scholar]
- 98. Nagasawa M, Mitsui S, En S, et al. Social evolution. Oxytocin-gaze positive loop and the coevolution of human-dog bonds. Science. 2015;348(6232):333–336. [DOI] [PubMed] [Google Scholar]
- 99. Oettl L-L, Ravi N, Schneider M, et al. Oxytocin enhances social recognition by modulating cortical control of early olfactory processing. Neuron. 2016;90(3):609–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Marlin BJ, Mitre M, D’Amour JA, Chao MV, Froemke RC.. Oxytocin enables maternal behaviour by balancing cortical inhibition. Nature. 2015;520(7548):499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Freeman SM, Young LJ.. Comparative perspectives on oxytocin and vasopressin receptor research in rodents and primates: translational implications. J Neuroendocrinol. 2016;28(4):10.1111/jne.12382. doi: 10.1111/jne.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Ford CL, Young LJ.. Harnessing the healing power of love. Trends Mol Med. 2021;27(9):833–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Davis SR, Prince MA, Swaim RC, Stanley LR.. Comparing cannabis use motive item performance between American Indian and White youth. Drug Alcohol Depend. 2020;213:108086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Dias PC, Tavares E, Simões M, Cadime I.. Motives for cannabis use in a sample of portuguese users. Journal of Substance Use. 2020;25(6):672–676. [Google Scholar]
- 105. Garrison E, Gilligan C, Ladd BO, Anderson KG.. Social anxiety, cannabis use motives, and social context’s impact on willingness to use cannabis. Int J Environ Res Public Health. 2021;18(9):4882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Hawke LD, Wilkins L, Henderson J.. Early cannabis initiation: substance use and mental health profiles of service-seeking youth. J Adolesc. 2020;83:112–121. [DOI] [PubMed] [Google Scholar]
- 107. Keyes KM, Wall M, Feng T, Cerdá M, Hasin DS.. Race/ethnicity and marijuana use in the United States: diminishing differences in the prevalence of use, 2006-2015. Drug Alcohol Depend. 2017;179:379–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Thomas C, Freisthler B.. Evaluating the change in medical marijuana dispensary locations in Los Angeles following the passage of local legislation. J Prim Prev. 2017;38:265–277. [DOI] [PubMed] [Google Scholar]
- 109. Rhee JU, Vieira VM, Firth CL, Pedersen ER, Dunbar MS, Timberlake DS.. Concentration of cannabis and tobacco retailers in Los Angeles County, California: a spatial analysis of potential effects on youth and ethnic minorities. J Stud Alcohol Drugs. 2022;83(4):502–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Ambrose CA, Cowan BW, Rosenman RE.. Geographical access to recreational marijuana. Contemporary Econ Pol. 2021;39(4):778–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Mair C, Freisthler B, Ponicki WR, Gaidus A.. The impacts of marijuana dispensary density and neighborhood ecology on marijuana abuse and dependence. Drug Alcohol Depend. 2015;154:111–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Freisthler B, Gruenewald PJ, Treno AJ, Lee J.. Evaluating alcohol access and the alcohol environment in neighborhood areas. Alcohol Clin Exp Res. 2003;27(3):477–484. [DOI] [PubMed] [Google Scholar]
- 113. Novak SP, Reardon SF, Raudenbush SW, Buka SL.. Retail tobacco outlet density and youth cigarette smoking: a propensity-modeling approach. Am J Public Health. 2006;96(4):670–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Di Forti M, Marconi A, Carra E, et al. Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: a case-control study. The Lancet Psychiatry. 2015;2(3):233–238. [DOI] [PubMed] [Google Scholar]
- 115. Di Forti M, Quattrone D, Freeman TP, et al. ; EU-GEI WP2 Group. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU-GEI): a multicentre case-control study. The Lancet Psychiatry. 2019;6(5):427–436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Schinke SP, Fang L, Cole KC, Cohen-Cutler S.. Preventing substance use among Black and Hispanic adolescent girls: results from a computer-delivered, mother-daughter intervention approach. Subst Use Misuse. 2011;46(1):35–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Bloomfield MA, Ashok AH, Volkow ND, Howes OD.. The effects of Δ9-tetrahydrocannabinol on the dopamine system. Nature. 2016;539(7629):369–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Bagot KS, Milin R, Kaminer Y.. Adolescent initiation of cannabis use and early-onset psychosis. Subst Abus. 2015;36(4):524–533. [DOI] [PubMed] [Google Scholar]
- 119. Hartberg CB, Lange EH, Lagerberg TV, et al. Cortical thickness, cortical surface area and subcortical volumes in schizophrenia and bipolar disorder patients with cannabis use. Eur Neuropsychopharmacol. 2018;28(1):37–47. [DOI] [PubMed] [Google Scholar]
- 120. Arranz S, Monferrer N, Algora MJ, et al. The relationship between the level of exposure to stress factors and cannabis in recent onset psychosis. Schizophr Res. 2018;201:352–359. [DOI] [PubMed] [Google Scholar]
- 121. Belbasis L, Köhler C, Stefanis N, et al. Risk factors and peripheral biomarkers for schizophrenia spectrum disorders: an umbrella review of meta‐analyses. Acta Psychiatr Scand. 2018;137(2):88–97. [DOI] [PubMed] [Google Scholar]
- 122. Niemi-Pynttäri JA, Sund R, Putkonen H, Vorma H, Wahlbeck K, Pirkola SP.. Substance-induced psychoses converting into schizophrenia: a register-based study of 18,478 Finnish inpatient cases. J Clin Psychiatry. 2013;74(1):e9420155–e9420e99. [DOI] [PubMed] [Google Scholar]
- 123. Starzer MSK, Nordentoft M, Hjorthøj C.. Rates and predictors of conversion to schizophrenia or bipolar disorder following substance-induced psychosis. Am J Psychiatry. 2018;175(4):343–350. [DOI] [PubMed] [Google Scholar]
- 124. Feldman DE. Synaptic mechanisms for plasticity in neocortex. Annu Rev Neurosci. 2009;32:33–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Weinberger NM. Associative representational plasticity in the auditory cortex: a synthesis of two disciplines. Learn Mem. 2007;14(1-2):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Olney JW, Farber NB.. Glutamate receptor dysfunction and schizophrenia. Arch Gen Psychiatry. 1995;52(12):998–1007. [DOI] [PubMed] [Google Scholar]
- 127. Moghaddam B. Bringing order to the glutamate chaos in schizophrenia. Neuron. 2003;40(5):881–884. [DOI] [PubMed] [Google Scholar]
- 128. Moghaddam B. Targeting metabotropic glutamate receptors for treatment of the cognitive symptoms of schizophrenia. Psychopharmacology. 2004;174(1):39–44. [DOI] [PubMed] [Google Scholar]
- 129. Laruelle M. Dopamine transmission in the schizophrenic brain. In: Hirsch SR, Weinberger DR, eds. Schizophrenia. Malden, Massachusetts: Blackwell Publishing Company; 2003:365–386. [Google Scholar]
- 130. Clinton SM, Meador-Woodruff JH.. Abnormalities of the NMDA receptor and associated intracellular molecules in the thalamus in schizophrenia and bipolar disorder. Neuropsychopharmacology. 2004;29(7):1353–1362. [DOI] [PubMed] [Google Scholar]
- 131. Harrison PJ, Weinberger DR.. Schizophrenia genes, gene expression, and neuropathology: on the matter of their convergence. Mol Psychiatry. 2005;10(1):40–68. [DOI] [PubMed] [Google Scholar]
- 132. Pilowsky LS, Bressan RA, Stone JM, et al. First in vivo evidence of an NMDA receptor deficit in medication-free schizophrenic patients. Mol Psychiatry. 2006;11(2):118–119. [DOI] [PubMed] [Google Scholar]
- 133. Javitt DC, Zukin SR.. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148(10):1301–1308. [DOI] [PubMed] [Google Scholar]
- 134. Krystal JH, Karper LP, Seibyl JP, et al. Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry. 1994;51(3):199–214. [DOI] [PubMed] [Google Scholar]
- 135. Hackman DA, Kuan DC, Manuck SB, Gianaros PJ.. Socioeconomic position and age-related disparities in regional cerebral blood flow within the prefrontal cortex. Psychosom Med. 2018;80(4):336–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Bogorad MI, DeStefano JG, Linville RM, Wong AD, Searson PC.. Cerebrovascular plasticity: Processes that lead to changes in the architecture of brain microvessels. J. Cereb. Blood Flow Metab. 2019;39(8):1413–1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Djordjevic J, Djordjevic A, Adzic M, Radojcic MB.. Effects of chronic social isolation on Wistar rat behavior and brain plasticity markers. Neuropsychobiology. 2012;66(2):112–119. [DOI] [PubMed] [Google Scholar]
- 138. Logue J, Schoepfer K, Guerrero AB, Zhou Y, Kabbaj M.. Sex-specific effects of social isolation stress and ketamine on hippocampal plasticity. Neurosci Lett. 2022;766:136301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Bourque F, van der Ven E, Fusar-Poli P, Malla A.. Immigration, social environment and onset of psychotic disorders. Curr Pharm Des. 2012;18(4):518–526. [DOI] [PubMed] [Google Scholar]
- 140. Garcia M, Montalvo I, Creus M, et al. Sex differences in the effect of childhood trauma on the clinical expression of early psychosis. Compr Psychiatry. 2016;68:86–96. [DOI] [PubMed] [Google Scholar]
- 141. Henssler J, Brandt L, Müller M, et al. Migration and schizophrenia: meta-analysis and explanatory framework. Eur Arch Psychiatry Clin Neurosci. 2020;270(3):325–335. [DOI] [PubMed] [Google Scholar]
- 142. Varchmin L, Montag C, Treusch Y, Kaminski J, Heinz A.. Traumatic events, social adversity and discrimination as risk factors for psychosis - an umbrella review. Front Psychiatry. 2021;12:665957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Powell ND, Sloan EK, Bailey MT, et al. Social stress up-regulates inflammatory gene expression in the leukocyte transcriptome via β-adrenergic induction of myelopoiesis. Proc Natl Acad Sci USA. 2013;110(41):16574–16579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Cole SW, Capitanio JP, Chun K, Arevalo JM, Ma J, Cacioppo JT.. Myeloid differentiation architecture of leukocyte transcriptome dynamics in perceived social isolation. Proc Natl Acad Sci USA. 2015;112(49):15142–15147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Cole SW. The conserved transcriptional response to adversity. Curr. Opin. Behav. Sci. 2019;28:31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Heidt T, Sager HB, Courties G, et al. Chronic variable stress activates hematopoietic stem cells. Nat Med. 2014;20(7):754–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. McKim DB, Yin W, Wang Y, Cole SW, Godbout JP, Sheridan JF.. Social stress mobilizes hematopoietic stem cells to establish persistent splenic myelopoiesis. Cell reports. 2018;25(9):2552–2562.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Cacioppo JT, Cacioppo S, Capitanio JP, Cole SW.. The neuroendocrinology of social isolation. Annu Rev Psychol. 2015;66:733–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Irwin MR, Cole SW.. Reciprocal regulation of the neural and innate immune systems. Nat Rev Immunol. 2011;11(9):625–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Eisenberger NI, Moieni M, Inagaki TK, Muscatell KA, Irwin MR.. In sickness and in health: the co-regulation of inflammation and social behavior. Neuropsychopharmacology. 2017;42(1):242–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Cacioppo JT, Cacioppo S.. Loneliness in the modern age: an evolutionary theory of loneliness (ETL). J. Exp. Soc. Psychol. 2018;58:127–197. [Google Scholar]
- 152. Cacioppo JT, Hawkley LC.. Perceived social isolation and cognition. Trends Cogn Sci. 2009;13(10):447–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Moieni M, Irwin MR, Jevtic I, et al. Trait sensitivity to social disconnection enhances pro-inflammatory responses to a randomized controlled trial of endotoxin. Psychoneuroendocrinology. 2015;62:336–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Inagaki TK, Muscatell KA, Irwin MR, Cole SW, Eisenberger NI.. Inflammation selectively enhances amygdala activity to socially threatening images. Neuroimage. 2012;59(4):3222–3226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Eisenberger NI, Inagaki TK, Mashal NM, Irwin MR.. Inflammation and social experience: an inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain Behav Immun. 2010;24(4):558–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Wohleb ES, McKim DB, Sheridan JF, Godbout JP.. Monocyte trafficking to the brain with stress and inflammation: a novel axis of immune-to-brain communication that influences mood and behavior. Front Neurosci. 2015;8:447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Miller GE, Chen E, Finegood E, Shimbo D, Cole SW.. Prospective associations between neighborhood violence and monocyte pro-inflammatory transcriptional activity in children. Brain Behav Immun. 2022;100:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Lee MJ, Rittschof CC, Greenlee AJ, et al. Transcriptomic analyses of black women in neighborhoods with high levels of violence. Psychoneuroendocrinology. 2021;127:105174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Selten J-P, Booij J, Buwalda B, Meyer-Lindenberg A.. Biological mechanisms whereby social exclusion may contribute to the etiology of psychosis: a narrative review. Schizophr Bull. 2017;43(2):287–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Schalbroeck R. The social defeat hypothesis of schizophrenia: a parsimonious explanation for multiple psychosis risk factors? Psychol Med. 2020;53(1):286–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Ziauddeen H, Murray GK.. The relevance of reward pathways for schizophrenia. Curr Opin Psychiatry. 2010;23(2):91–96. [DOI] [PubMed] [Google Scholar]
- 162. Berridge KC. From prediction error to incentive salience: mesolimbic computation of reward motivation. Eur J Neurosci. 2012;35(7):1124–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Young JW, Geyer MA.. Developing treatments for cognitive deficits in schizophrenia: the challenge of translation. J Psychopharmacol. 2015;29(2):178–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Regan A, Fritz MM, Walsh LC, Lyubomirsky S, Cole SW.. The genomic impact of kindness to self vs. others: a randomized controlled trial. Brain Behav Immun. 2022;106:40–48. [DOI] [PubMed] [Google Scholar]
- 165. Nelson-Coffey SK, Fritz MM, Lyubomirsky S, Cole SW.. Kindness in the blood: a randomized controlled trial of the gene regulatory impact of prosocial behavior. Psychoneuroendocrinology. 2017;81:8–13. [DOI] [PubMed] [Google Scholar]
- 166. Moieni M, Irwin MR, Seeman TE, et al. Feeling needed: effects of a randomized generativity intervention on well-being and inflammation in older women. Brain Behav Immun. 2020;84:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Seeman T, Merkin SS, Goldwater D, Cole SW.. Intergenerational mentoring, eudaimonic well-being and gene regulation in older adults: a pilot study. Psychoneuroendocrinology. 2020;111:104468. [DOI] [PubMed] [Google Scholar]
- 168. Shah J, Mizrahi R, McKenzie K.. The four dimensions: a model for the social aetiology of psychosis. Br J Psychiatry. 2011;199(1):11–14. [DOI] [PubMed] [Google Scholar]
- 169. Millan MJ, Andrieux A, Bartzokis G, et al. Altering the course of schizophrenia: progress and perspectives. Nat Rev Drug Discov. 2016;15(7):485–515. [DOI] [PubMed] [Google Scholar]
- 170. Rigney N, de Vries GJ, Petrulis A, Young LJ.. Oxytocin, vasopressin, and social behavior: from neural circuits to clinical opportunities. Endocrinology. 2022;163(9):bqac111. doi:10.1210/endocr/bqac111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Ford CL, Young LJ.. Translational opportunities for circuit-based social neuroscience: advancing 21st century psychiatry. Curr Opin Neurobiol. 2021;68:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Ford CL, Young LJ.. Refining oxytocin therapy for autism: context is key. Nat Rev Neurol. 2022;18(2):67–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Le J, Zhang L, Zhao W, et al. Infrequent intranasal oxytocin followed by positive social interaction improves symptoms in autistic children: a pilot randomized clinical trial. Psychother Psychosom. 2022;91(5):335–347. [DOI] [PubMed] [Google Scholar]
- 174. Mitchell JM, Bogenschutz M, Lilienstein A, et al. MDMA-assisted therapy for severe PTSD: a randomized, double-blind, placebo-controlled phase 3 study. Nat Med. 2021;27(6):1025–1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Buffington SA, Di Prisco GV, Auchtung TA, Ajami NJ, Petrosino JF, Costa-Mattioli M.. Microbial reconstitution reverses maternal diet-induced social and synaptic deficits in offspring. Cell. 2016;165(7):1762–1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Sgritta M, Dooling SW, Buffington SA, Momin EN, Francis MB, Britton RA, Costa-Mattioli M.. Mechanisms underlying microbial-mediated changes in social behavior in mouse models of autism spectrum disorder. Neuron. 2019;101(2):246–259e246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Thompson A, Jones HJ, Heron J, Hibbeln J, Sullivan S, Zammit S.. Omega-3 and Omega-6 fatty acids and risk of psychotic outcomes in the ALSPAC birth cohort. Schizophr Res. 2020;224:108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Cirillo G, Di Pino G, Capone F, et al. Neurobiological after-effects of non-invasive brain stimulation. Brain Stimul. 2017;10(1):1–18. [DOI] [PubMed] [Google Scholar]
- 179. Ferro M, Lamanna J, Spadini S, Nespoli A, Sulpizio S, Malgaroli A.. Synaptic plasticity mechanisms behind TMS efficacy: insights from its application to animal models. J Neural Transm. 2022;129(1):25–36. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.