Abstract
Study Objectives
Persistent insomnia disorder (pID) is linked to neurocognitive decline and increased risk of Alzheimer’s Disease (AD) in later life. However, research in this field often utilizes self-reported sleep quality data - which may be biased by sleep misperception - or uses extensive neurocognitive test batteries - which are often not feasible in clinical settings. This study therefore aims to assess whether a simple screening tool could uncover a specific pattern of cognitive changes in pID patients, and whether these relate to objective aspect(s) of sleep quality.
Methods
Neurocognitive performance (Montreal Cognitive Assessment; MoCA), anxiety/depression severity, and subjective sleep quality (Pittsburgh Sleep Quality Index: PSQI; Insomnia Severity Index: ISI) data were collected from 22 middle-aged pID patients and 22 good-sleepers. Patients underwent overnight polysomnography.
Results
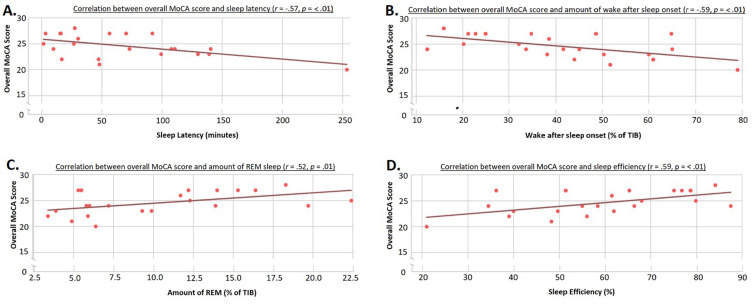
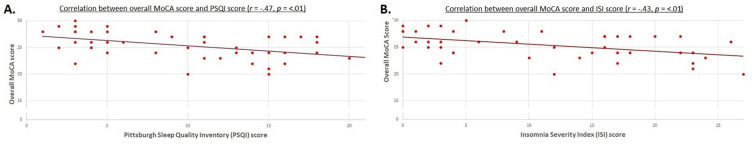
Compared to good-sleepers, patients had lower overall cognitive performance (average: 24.6 versus 26.3 points, Mann–Whitney U = 136.5, p = <0.006), with deficits in clock drawing and verbal abstraction. In patients, poorer overall cognitive performance correlated with reduced subjective sleep quality (PSQI: r(42) = −0.47, p = 0.001; and ISI: r(42) = −0.43, p = 0.004), reduced objective sleep quality (lower sleep efficiency: r(20) = 0.59, p = 0.004 and less REM-sleep: r(20) = 0.52, p = 0.013; and increased sleep latency: r(20) = −0.57, p = 0.005 and time awake: r(20) = −0.59, p = 0.004). Cognitive performance was not related to anxiety/depression scores.
Conclusion
Using a simple neurocognitive screening tool, we found that pID patients showed cognitive deficiencies that related to both subjective/self-reported and objective/polysomnographic measures of sleep quality. Furthermore, these cognitive changes resembled those seen in preclinical non-amnestic AD, and thus could indicate incumbent neurodegenerative processes in pID. Interestingly, increased REM-sleep was correlated with better cognitive performance. However, whether REM-sleep is protective against neurodegeneration requires further investigation.
Keywords: insomnia, sleep, neurodegeneration, Alzheimer’s disease, polysomnography, cognitive screening
Plain Language Summary
Neurodegeneration and sleep quality influence one another. Consequently, patients with neurodegenerative/dementing diseases often have poor sleep. Conversely, sleep disorders - like insomnia - increase a patient’s risk of developing dementias, making early identification of at-risk patients vital. We compared the performance of patients with insomnia to that of healthy peers using a simple screening tool. Patients not only had a lower overall cognitive status, but had particular difficulties in abstract thinking and clock drawing. When we compared the patients’ performance to their objective sleep quality, we found that patients who fell asleep faster, spent less of the night awake, and spent longer in “dream sleep” showed better performance on the cognitive screening test. These results are interesting for two reasons. Firstly, the cognitive difficulties faced by patients with insomnia are similar to those seen in mild cognitive impairment, a pre-stage of Alzheimer’s. This supports the idea that poor sleep quality, if left untreated, can cause similar cognitive difficulties as those found in dementing diseases. Secondly, dream sleep may be protective, possibly slowing down the rate of cognitive decline. Taken together, insomnia patients - and particularly those with reduced dream sleep - may benefit greatly from preventative intervention strategies.
Introduction
Changes in sleep patterns are closely linked to neurodegenerative processes,1 and are a common comorbidity in patients with dementing illnesses like Alzheimer’s disease (AD).2 This relationship between sleep quality and neurodegeneration is bi-directional,3 and several brain regions involved in regulating the sleep-wake cycle are important for cognitive functions.1 Consequently, poor sleep quality increases cognitive decline and dementia risk,3,4 making early identification of at-risk patients vital. One such risk state is insomnia, affecting 6–10% of adults.5 Indeed, meta-analyses indicate that patients with persistent insomnia disorder (pID) have a 1.5-fold higher risk of developing AD in later life.6–8 Furthermore, extensive neuropsychological testing shows that patients with pID show decline in similar cognitive domains9,10 to those in patients with amnestic mild cognitive impairment (aMCI), a transitional stage between normative aging and AD.
Using short screening tools, rather than extensive test batteries, to identify at-risk patients would be ideal in clinical settings. However, it remains unclear whether these are sensitive enough in this context. Previous studies utilizing screening tools to test for cognitive impairments in insomnia patients either did not directly examine how cognitive deficits related to polysomnographic data,11 or used self-reported measures of sleep quality to assess this relationship.12,13 Such self-reported questionnaires may yield unreliable sleep quality estimates due to sleep misperception (a frequently seen discrepancy between subjective estimates and objective measurements of sleep duration).14 Thus, objective polysomnographic data is vital in examining whether potential cognitive alterations observed through screening tools relate to sleep quality in patients with pID.
In summary, despite the importance of early identification of at-risk patients, research examining the relationship between early cognitive alterations in patients with pID, measured through screening tools, and specific aspect(s) of sleep quality, measured via polysomnography, is lacking. The aims of this study are therefore twofold. Firstly, we assessed whether a cognitive screening test could identify specific subdomains that were especially vulnerable in patients. For this, we utilized the Montreal Cognitive Assessment (MoCA),15 a short screening which measures of seven cognitive domains, and which is sensitive enough to detect relatively mild cognitive deficits, for example in aMCI.15,16 Secondly, we evaluated the relationship between patients’ cognitive performance and their objective sleep quality, obtained by polysomnography.
Materials and Methods
Demographic Data
We recruited 22 patients with pID and 22 matched healthy controls. The patients were diagnosed according to DSM V criteria,16 and had a disease duration of >1 year. Patients with comorbid insomnia, occurring in the presence of other medical/mental disorders, were excluded. Exclusion criteria in both groups included comorbid sleep disorders, inadequate sleep hygiene, alcohol/substance abuse, a history of neurological/psychiatric diseases, and intake of sleep-altering medication (stimulants/anti-depressants/sedatives). Eligibility was assessed through questionnaires and structured interviews.
Study Protocol
All participants completed the MoCA, obtaining an extra point if they had ≤12 years of education, as per guidelines.15 The Hospital Anxiety and Depression Scale (HADS-A/D)17 was used to quantify anxiety/depression symptoms. Premorbid intellectual functioning estimates were obtained using the German “Mehrfachwahl Wortschatz Intelligenz Test-B”.18
Sleep Quality
The Pittsburgh Sleep Quality Index (PSQI)19 and the Insomnia Severity Index (ISI)20 were used to assess self-reported sleep quality. All patients underwent one night of polysomnography (SOMNOmedics),21 sleeping ad libitum, at least one week prior to neuropsychological testing, ensuring that sleeping in a laboratory environment did not adversely impact test performance. An experienced staff member, who was blind to the study, scored the polysomnographic data according to the American Academy of Sleep Medicine Scoring Manual guidelines.22
Statistical Analysis
Means and standard deviations are given for normally distributed data, and medians and interquartile ranges for non-normally distributed data. The difference in overall cognitive performance was calculated with a one-tailed t-test, with an alpha of 0.05. Due to low variance in each subdomain, resulting in non-parametric data, intergroup differences for each subdomains were calculated with one-tailed Mann–Whitney U-tests. Multiple comparisons were controlled for using the Benjamini-Hochberg method, as this controls for false discoveries whilst avoiding being overly conservative.23 A false positive rate of 5% was used to calculate the critical values (q). Both objective and subjective sleep data were correlated to cognitive performance data, again corrected for multiple comparisons. To ensure psychological well-being did not confound cognitive performance in the patient group, the overall MoCA score was correlated to anxiety/depression scores using Pearson’s correlation coefficients. Confidence intervals were reported for all correlations. No data was missing or excluded from analysis, outlier analysis revealed no outliers, and all analyses were run with IBM SPSS, version 26.0.24
Results
There were no significant group differences in age, gender, education, and estimated intelligence (see Table 1). As expected, patients had worse subjective sleep quality (PSQI: t(42) = −10.53, p = <0.001) and insomnia severity (ISI: t(42) = −10.83, p = <0.001). Additionally, patients reported significantly higher anxiety (t(42) = −4.32, p = <0.001) and depression (t(42) = −3.80, p = <0.001) symptoms.
Table 1.
Demographic and Sleep Quality Data of Patients with pID and Healthy Controls
| pID Patients | Healthy Controls | p-value | |
|---|---|---|---|
| Sociodemographics: | |||
| Age (years) | 58.1 (12.2) | 55.3 (10.0) | p = 0.19 |
| Gender (n. male/ female) | 19 / 3 | 16 / 6 | p = 0.13 |
| Education (n. low/medium/high) | 3 / 12 / 7 | 1 / 15 / 6 | p = 0.25 |
| Estimated intelligence quotient (MWTB) | 112.6 (12.7) | 118.4 (14.2) | p = 0.08 |
| Self-assessment of anxiety and depression: | |||
| HADS Anxiety (max. 21 points) | 8.9 (5.1) | 3.7 (2.5) | p = <0.01* |
| HADS Depression (max. 21 points) | 7.5 (4.5) | 3.3 (2.6) | p = <0.01* |
| Subjective sleep quality: | |||
| PSQI (max. 21 points) | 14.3 (3.2) | 4.8 (2.8) | p = <0.01* |
| ISI (max. 28 points) | 18.5 (4.8) | 4.0 (4.1) | p = <0.01* |
| Objective polysomnographic sleep quality: | |||
| Sleep Efficiency (%) | 58.9 (17.8); CI: 50.97, 66.73 | ||
| Sleep-onset latency (minutes) | 52.2 [86.3]; CI:41.57, 96.11 | ||
| Wake after sleep onset (minutes) | 132.4 (52.0); CI:109.33, 155.41 | ||
| Sleep-stage transition index (/hour) | 14.5 [6.6]; CI: 13.8, 20.22 | ||
| Arousal index (/hour) | 18.9 [14.9]; CI: 15.5, 25.13 | ||
| Apnea/Hypopnea index (/hour) | 2.4 [4.3]; CI: 1.17, 8.29 | ||
| Periodic Limb Movement index (/hour) | 2.4 [6.1] CI: 2.21, 7.23 | ||
| Sleep stage distribution (% of Time In Bed): | |||
| Time Awake | 41.2 (17.8); CI:33.24, 49.06 | ||
| Light sleep | 34.2 (14.6); CI:27.76, 40.64 | ||
| Deep sleep | 13.9 (7.4); CI:10.60, 17.18 | ||
| REM sleep | 10.4 (5.6); CI:7.98, 12.90 | ||
Notes: Mean and standard deviation (in parentheses) given for normally distributed data. Medians and interquartile ranges (in square brackets) and are presented for non-normally distributed data. CI: 95% Confidence Intervals are given for polysomnographic data. Gender and education expressed as number of participants. An asterisk marks significant differences.
Abbreviations: n., number of; pID, persistent Insomnia Disorder; MWTB, Mehrfachwahl Wortschatz Intelligenz Test B; PSQ, Pittsburgh Sleep Quality Index; ISI, Insomnia Severity Index; HADS, Hospital Anxiety and Depression Scale; REM, Rapid Eye Movement.
Neurocognitive Performance
MoCA performance is presented in Table 2. In total, five participants from each group qualified for an additional point. Using a cut-off of ≤23 points, which has better specificity for detecting MCI than the previously used ≤26,25 we identified two good sleepers and seven patients with scores indicative of MCI.
Table 2.
MoCA Scores of Patients with pID and Good Sleepers
| Patients with pID | Good Sleepers | p value | q value | |
|---|---|---|---|---|
| Overall score (Max 30) | 24.6/2.2/20–28 | 26.3/2.4/20–30 | p = <0.006* | 0.006 |
| Subdomains: | ||||
| Visuospatial/executive (Max 5) | 4 (0.0) | 5 (1.0) | p = 0.006* | 0.013 |
| Abstraction (Max 2) | 1 (0.8) | 2 (1.0) | p = 0.009* | 0.019 |
| Attention (Max 6) | 5 (1.0) | 6 (1.0) | p = 0.123 | 0.025 |
| Recall (Max 5) | 4 (2.0) | 4 (2.0) | p = 0.309 | 0.031 |
| Naming (Max 3) | 3 (0.0) | 3 (0.0) | p = 0.401 | 0.038 |
| Language (Max 3) | 2 (1.0) | 2 (1.0) | p = 0.413 | 0.044 |
| Orientation (Max 6) | 6 (0.0) | 6 (0.0) | p = 0.496 | 0.050 |
Notes: Mean, standard deviation, and range of overall scores, and median and interquartile range (in parentheses) for each subdomain, as well as the maximum number of points possible on each subsection of the MoCA for both the healthy control group as well as for patients with pID. An asterisk marks significant differences. q values represent the significance threshold established using the Benjamini-Hochberg correction for multiple comparison.
Patients had worse overall cognitive performance (Mann–Whitney U = 136.5, n1 = 22, n2 = 22, p = <0.006, q = 0.006), and showed specific deficits in verbal abstraction (Mann–Whitney U = 141.5, n1 = 22, n2 = 22, p = 0.009, q = 0.019) and visuospatial/executive function (Mann–Whitney U = 134.5, n1 = 22, n2 = 22, p = 0.006, q = 0.013), mainly related to clock drawing. Naming, attention, language, memory, and orientation subdomains showed no intergroup differences. Patients’ overall cognitive performance was not related to their anxiety (r(20) = 0.07, p = 0.38, 95% C.I. [−0.36, 0.48], q = 0.03) or depression (r(20) = −0.13, p = 0.28, 95% C.I. [−0.52, 0.31], q = 0.05) scores.
Sleep Quality
To assess whether cognitive performance related to sleep quality, overall MoCA scores were correlated to patients’ sleep quality measures. Poorer MoCA scores were linked to worse objective polysomnographic measures, namely with lower sleep efficiency (r(20) = 0.59, p = 0.004, 95% C.I. [0.22, 0.81], q = 0.007), higher amounts of wake (% of time in bed) (r(20) = −0.59, p = 0.004, 95% C.I. [−0.81, −0.22]; q = 0.014), higher sleep latency (r(20) = −0.57, p = 0.005, 95% C.I. [−0.80, −0.20]; q = 0.021), and lower amounts of REM-sleep (r(20) = 0.52, p = 0.013, 95% C.I. [0.13, 0.77]; q = 0.029; see Figure 1). However, overall MoCA score did not correlate with the remaining polysomnographic parameters (see Supplementary Materials and Supplementary Figure 1). Due to low sub-score variability, correlations between MoCA sub-scores and sleep parameters were not calculated.
Figure 1.
Correlation between overall MoCA score and sleep latency (A); wake after sleep onset (B); REM sleep (C); and sleep efficiency (D) in patients with pID.
Abbreviation: TIB, Time in Bed.
Finally, worse overall MoCA performance was linked to poorer subjective sleep quality (PSQI: r(42) = −0.47, p = 0.001, 95% C.I. [−0.66, −0.18], q = 0.025 and ISI: r(42) = −0.43, p = 0.004, 95% C.I. [−0.66, −0.18], q = 0.050), where higher PSQI and ISI scores reflect poorer sleep quality; see Figure 2.
Figure 2.
Distribution of overall MoCA scores relative to scores on subjective, self-reported sleep quality measures. (A) PSQI: Pittsburgh Sleep Quality Inventory; (B) ISI: Insomnia Severity Index. Note that due to overlapping scores, some points in the scatterplot represent multiple data points.
Discussion
Using a screening tool, we found lower cognitive performance in pID patients compared to good sleepers, which was mainly attributable to deficiencies in verbal abstraction and clock drawing. These cognitive changes were significantly related to polysomnographic indices of insomnia severity and amount of REM-sleep in patients with pID.
Lower cognitive status in patients with insomnia, assessed via screenings, has been reported in some,12,26 but not in all studies.27 The overall MoCA score has been found to be significantly lower in pID patients, although differences in sub-scores were not assessed.11,28 Studies addressing domain-specific cognitive constraints have used extensive neuropsychological test batteries,10,26 although have failed to find a consistent pattern of results, likely due to the diversity of tests used. Nevertheless, given that insomnia patients are at higher risk for Alzheimer’s disease, the finding of specific deficiencies in clock drawing and verbal abstraction in this study seem noteworthy. Clock drawing, a singular screening test in its own right, can detect patients with an elevated risk of dementia.29 Moreover, in a 22-year prospective study, verbal abstract reasoning was one of the strongest predictors for the development of Alzheimer’s disease in the pre-clinical phase.30 Thus, this specific pattern of deficits observed here could be indicative of an incipient neurodegenerative process.
Lower cognitive performance has been linked to poorer subjective sleep.6–8 However, our results go beyond this by demonstrating that cognitive performance was also linked to objective polysomnographic sleep measures in patients with pID. Several different aspects sleep disturbances could account for this cognitive decline. For example, sleep fragmentation leads to an accelerated deposition of amyloid β.4 Conversely, animal models suggests that reduced slow-wave sleep lowers glymphatic system activity, leading to a build-up of amyloid β.31 Concurrently, elderly subjects with less slow-wave sleep showed increased brain atrophy at autopsy.32 Conversely, data on healthy older adults implicates REM-sleep duration as being predictive of cognitive decline.33,34 Consequently, different aspects of sleep quality reduction could lead to pathological cerebral processes, which may predispose people to neurocognitive decline.
However, we found no evidence linking cognitive performance and both deep (slow-wave) sleep, and arousal/sleep-stage transition indices (reflective of sleep fragmentation). Instead, increased REM-sleep was related to better cognitive performance, suggesting a protective role against cognitive decline. This supports similar findings in healthy older adults,35,36 with REM-sleep amount being predictive of cognitive outcome at a three-year follow-up.34 Nevertheless, our study is the first - to the best of our knowledge - to show this in pID patients. Given that our patients had no objective memory deficits, and that REM-sleep is vital for the integrity of episodic memory function,37 then it seems possible that some patients may be at a “pre-amnestic-MCI” neurodegenerative stage. Although speculative, longitudinal studies assessing whether the pattern of deficits observed in patients with pID later develops into one resembling aMCI are needed.
One alternative explanation for our results could be that cognitive difficulties resulted from chronic sleep deprivation. However, neither chronic nor acute sleep deprivation studies have shown negative effects on abstraction, executive functions, and visuospatial capabilities.38–40 Thus, our results are not explainable through mere reduction of sleep quantity. Nevertheless, experimental studies may not completely reflect sleep deprivation experienced in chronic disorders like insomnia. However, reduced sleep quantity could not explain why the amount of REM-sleep, but not slow-wave-sleep, is related to cognitive performance.
One limitation is that polysomnographic data were not collected from controls, and thus, intergroup differences in sleep quality could not be quantified. However, given group differences in cognition, and the correlations of these cognitive deficits with not only subjective but also objective measures of sleep quality in the patient group, the results of the current study support the conclusion that impaired sleep quality is related to a decline in cognitive abilities. Furthermore, patients did not have an acclimatization night, and may have experienced poorer sleep due to the “first-night-effect”. Another potential confound is the patients’ higher anxiety/depression scores, commonly seen in patients with pID.5 However, in our study, these scores did not correlate with cognitive performance, suggesting that psychological distress was not linked to cognitive deficits. Nevertheless, an indirect, mediating role is possible.41 Finally, the sensitivity and specificity of the MoCA in the context of insomnia needs further elucidation.
Conclusion
Taken together, neurocognitive deficits can be identified in patients with pID using a simple screening tool. Furthermore, insomnia severity and the amount of REM-sleep are closely related to these deficits. Whilst these results demonstrate that a screening tool may be sufficient in identifying patients at risk, this would nevertheless need verification through a longitudinal study.
Funding Statement
Research was funded by: German Research Foundation (Deutsche Forschungsgemeinschaft, DFG) Grant Number: SPP 1772 BU1327/4-1.
Abbreviations
AD, Alzheimer’s disease; aMCI, amnestic mild cognitive impairment; PID, persistent insomnia disorder; DSM V, Diagnostic and statistical manual of mental disorders, 5th edition; HADS-A/D, Hospital anxiety and depression scale, Anxiety/Depression; ISI, Insomnia severity index; MCI, mild cognitive impairment; MoCA, Montreal cognitive assessment tool; PSQI, Pittsburgh sleep quality index; TIB, Time in bed; REM, rapid eye movement.
Data Sharing Statement
As much of the data pertains to patient information, the data will not be made publicly available. However, the data that support the findings of this study are available upon reasonable request from the corresponding author.
Ethics Approval and Informed Consent
Ethical approval for this observational study was obtained from the Ethics Center at Friedrich-Schiller University (№ 4810-05/16), and written informed consent was given by each participant prior to participation. The study complies with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Yaffe K, Falvey CM, Hoang T. Connections between sleep and cognition in older adults. Lancet Neurol. 2014;13(10):1017–1028. doi: 10.1016/S1474-4422(14)70172-3 [DOI] [PubMed] [Google Scholar]
- 2.Iranzo A, Santamaria J. Sleep in neurodegenerative diseases. In: Chokroverty S, Billiard M, editors. Sleep Med. New York, NY: Springer; 2015:271–283. [Google Scholar]
- 3.Shamim SA, Warriach ZI, Tariq MA, et al. Insomnia: risk factor for neurodegenerative diseases. Cureus. 2019;11(10):e6004. doi: 10.7759/cureus.6004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Minakawa EN, Wada K, Nagai Y. Sleep disturbance as a potential modifiable risk factor for Alzheimer’s disease. Int J Mol Sci. 2019;20(4):803. doi: 10.3390/ijms20040803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3(5):S7–S10. doi: 10.5664/jcsm.26929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi L, Chen SJ, Ma MY, et al. Sleep disturbances increase the risk of dementia: a systematic review and meta-analysis. Sleep Med Rev. 2018;40:4–16. doi: 10.1016/j.smrv.2017.06.010 [DOI] [PubMed] [Google Scholar]
- 7.de Almondes KM, Costa MV, Malloy-Diniz LF, et al. Insomnia and risk of dementia in older adults: systematic review and meta-analysis. J Psychiatr Res. 2016;77:109–115. doi: 10.1016/j.jpsychires.2016.02.021 [DOI] [PubMed] [Google Scholar]
- 8.Bubu OM, Brannick M, Mortimer J, et al. Sleep, cognitive impairment, and Alzheimer’s disease: a systematic review and meta-analysis. Sleep. 2017;40(1):zsw032. doi: 10.1093/sleep/zsw032 [DOI] [PubMed] [Google Scholar]
- 9.Joo EY, Kim H, Suh S, et al. Hippocampal substructural vulnerability to sleep disturbance and cognitive impairment in patients with chronic primary insomnia: magnetic resonance imaging morphometry. Sleep. 2014;37(7):1189–1198. doi: 10.5665/sleep.3836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sexton CE, Sykara K, Karageorgiou E, et al. Connections between insomnia and cognitive aging. Neurosci Bull. 2020;36(1):77–84. doi: 10.1007/s12264-019-00401-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang P, Tan CW, Chen GH, et al. Patients with chronic insomnia disorder have increased serum levels of neurofilaments, neuron-specific enolase and S100B: does organic brain damage exist? Sleep Med. 2018;48:163–171. doi: 10.1016/j.sleep.2017.12.012 [DOI] [PubMed] [Google Scholar]
- 12.Cricco M, Simonsick EM, Foley DJ. The impact of insomnia on cognitive functioning in older adults. J Am Geriatr Soc. 2001;49(9):1185–1189. doi: 10.1046/j.1532-5415.2001.49235.x [DOI] [PubMed] [Google Scholar]
- 13.Guo H, Wei M, Ding W. Changes in cognitive function in patients with primary insomnia. Shanghai Arch Psychiatry. 2017;29(3):137. doi: 10.11919/j.issn.1002-0829.216097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fernandez-Mendoza J, Calhoun SL, Bixler EO, et al. Sleep misperception and chronic insomnia in the general population: the role of objective sleep duration and psychological profiles. Psychosom Med. 2011;73(1):88. doi: 10.1097/PSY.0b013e3181fe365a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- 16.Pinto T, Machado L, Bulgacov T, et al. Is the Montreal Cognitive Assessment (MoCA) screening superior to the Mini-Mental State Examination (MMSE) in the detection of mild cognitive impairment (MCI) and Alzheimer’s Disease (AD) in the elderly? Int Psychogeriatr. 2019;31(4):491–504. doi: 10.1017/S1041610218001370 [DOI] [PubMed] [Google Scholar]
- 17.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 18.Lehrl S. Mehrfachwahl-Wortschatz-Intelligenztest, B-Version. Straube: Erlangen; 1977. [Google Scholar]
- 19.Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 20.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2011;2:297–307. doi: 10.1016/S1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 21.DOMINO Ver. 2.9.0, SOMNOmedics, Randersacker, Germany 2020.
- 22.Berry RB, Brooks R, Gamaldo CE, et al. The American Academy of Sleep Medicine Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.5. Darien, Illinois: American Academy of Sleep Medicine; 2018. [Google Scholar]
- 23.Williams VS, Jones LV, Tukey JW. Controlling error in multiple comparisons, with examples from state-to-state differences in educational achievement. J Educ Behav Stat. 1999;24(1):42–69. doi: 10.3102/10769986024001042 [DOI] [Google Scholar]
- 24.IBM Corp. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp; 2019. [Google Scholar]
- 25.Carson N, Leach L, Murphy KJ. A re‐examination of Montreal Cognitive Assessment (MoCA) cutoff scores. Int J Geriatr Psychiatry. 2018;33(2):379–388. doi: 10.1002/gps.4756 [DOI] [PubMed] [Google Scholar]
- 26.Fortier-Brochu E, Morin CM. Cognitive impairment in individuals with insomnia: clinical significance and correlates. Sleep. 2014;37(11):1787–1798. doi: 10.5665/sleep.4172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Potvin O, Lorrain D, Forget H, et al. Sleep quality and 1-year incident cognitive impairment in community-dwelling older adults. Sleep. 2012;35(4):491–499. doi: 10.5665/sleep.1732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen L, Wei X, Liu C, et al. Brain iron deposition in primary insomnia — an in vivo susceptibility‐weighted imaging study. Brain Behav. 2019;9(1):e01138. doi: 10.1002/brb3.1138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park J, Jeong E, Seomun G. The clock drawing test: a systematic review and meta‐analysis of diagnostic accuracy. J Adv Nurs. 2018;74(12):2742–2754. doi: 10.1111/jan.13810 [DOI] [PubMed] [Google Scholar]
- 30.Elias MF, Beiser A, Wolf PA, et al. The preclinical phase of Alzheimer disease: a 22-year prospective study of the Framingham Cohort. Arch Neurol. 2000;57(6):808–813. doi: 10.1001/archneur.57.6.808 [DOI] [PubMed] [Google Scholar]
- 31.Rasmussen MK, Mestre H, Nedergaard M. The glymphatic pathway in neurological disorders. Lancet Neurol. 2018;17(11):1016–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gelber RP, Redline S, Ross GW, et al. Associations of brain lesions at autopsy with polysomnography features before death. Neurol. 2015;84(3):296–303. doi: 10.1212/WNL.0000000000001163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Scullin MK, Bliwise DL. Is cognitive aging associated with levels of REM sleep or slow wave sleep? Sleep. 2015;38(3):335–336. doi: 10.5665/sleep.4482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Song Y, Blackwell T, Yaffe K, et al. Relationships between sleep stages and changes in cognitive function in older men: the MrOS Sleep Study. Sleep. 2015;38(3):411–421. doi: 10.5665/sleep.4500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khazaie H, Tahmasian M, Ghadami MR, et al. The effects of chronic partial sleep deprivation on cognitive functions of medical residents. Iranian J Psychiatry. 2010;5(2):74. [PMC free article] [PubMed] [Google Scholar]
- 36.Lafortune M, Gagnon JF, Martin N, et al. Sleep spindles and rapID eye movement sleep as predictors of next morning cognitive performance in healthy middle‐aged and older participants. J Sleep Res. 2014;23(2):159–167. doi: 10.1111/jsr.12108 [DOI] [PubMed] [Google Scholar]
- 37.Olaithe M, Bucks RS, Hillman DR, et al. Cognitive deficits in obstructive sleep apnea: insights from a meta-review and comparison with deficits observed in COPD, insomnia, and sleep deprivation. Sleep Med Rev. 2018;38:39–49. doi: 10.1016/j.smrv.2017.03.005 [DOI] [PubMed] [Google Scholar]
- 38.Rauchs G, Bertran F, Guillery-Girard B, et al. Consolidation of strictly episodic memories mainly requires rapID eye movement sleep. Sleep. 2004;27(3):395–401. doi: 10.1093/sleep/27.3.395 [DOI] [PubMed] [Google Scholar]
- 39.Siegel JM. REM sleep: a biological and psychological paradox. Sleep Med Rev. 2011;15(3):139–142. doi: 10.1016/j.smrv.2011.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Smith MG, Wusk GC, Nasrini J, et al. Effects of six weeks of chronic sleep restriction with weekend recovery on cognitive performance and wellbeing in high-performing adults. Sleep. 2021;44:zsab051. doi: 10.1093/sleep/zsab051 [DOI] [PubMed] [Google Scholar]
- 41.Xu W, Tan CC, Zou JJ, et al. Sleep problems and risk of all-cause cognitive decline or dementia: an updated systematic review and meta-analysis. Cog Neurol. 2020;91:236–244. [DOI] [PMC free article] [PubMed] [Google Scholar]