Abstract
Background
People with diabetes tend to use many medications to treat diabetes and comorbidities. Nevertheless, the evolution of polypharmacy in newly diagnosed males and females has been little studied.
Objective
The objective of this paper was to identify and describe medication trajectories in incident diabetes cases according to sex.
Methods
Data were obtained from the Quebec Integrated Chronic Disease Surveillance System. We built a population-based cohort of community-dwelling individuals aged >65 years diagnosed with diabetes in 2014 who were alive and covered with the public drug plan until March 31, 2019. Latent class models were used to identify medication trajectory groups in males and females separately.
Results
Of the 10,363 included individuals, 51.4% were males. Females were older and more likely to have more medication claims than males. Four trajectory groups were identified for males and five for females. Most trajectories showed sustained and stable number of medications over time. For each sex, only one of the trajectory groups included a mean annual number of medications lesser than five. Slight increasing trends of medication use were detected in the trajectories composed of very high users, which included older, more comorbid individuals frequently exposed to potentially inappropriate medications.
Conclusions
Most males and females with incident diabetes had a high burden of medication following the year of diagnosis and were classified in a group of sustained medication use over time. The largest increase in medication was among those who had higher level of polypharmacy of questionable quality at baseline, raising concerns about the innocuity of such medication trajectories.
Keywords: Diabetes, Medication use, Older adults, Sex differences, Latent class models, Quebec
1. Introduction
Diabetes is one of the most common chronic diseases among older adults. In the province of Quebec, Canada, 21.2% of individuals aged 65 to 74 years, and 28.1% of those aged 75 years and older had a diagnosis of diabetes in 2019.1 Diabetes is also associated with many comorbidities such as coronary disease, stroke, peripheral arterial disease, and renal impairment.2 Over 97% of older persons with diabetes have at least one comorbidity and >40% have at least four.3 Understandably, the total health care costs related to diabetes are high; in 2022, the estimates were 15.4 billion dollars in Canada.4 As the population ages, these costs will increase over time. Optimal treatments that may prevent complications are thus essential to reduce the clinical and financial burden of this disease.
Medication plays an important role in treating and preventing diseases. Older adults with diabetes are particularly prone to use many medications, both to treat diabetes and other concomitant conditions. Indeed, the average number of medications used by older adults with diabetes in Quebec in 2014 was 12.5 As a result, most individuals with diabetes are exposed to polypharmacy, which is most commonly defined as the concomitant use of at least five medications.6,7 However, polypharmacy has been associated with adverse outcomes, such as increased falls, hospitalizations, and mortality.8 The adverse effects of polypharmacy are not only related to the number of medications but also to their appropriateness.9,10 In fact, a higher number of medications increases the risk of using potentially inappropriate medications,11 that is medications for which benefits are lower than their risks or for which other safer alternatives exist.12 Many lists can be used to identify potentially inappropriate medications, such as the Beers' criteria.13
Longitudinal studies can help to capture heterogeneity in medication use and to assess changes in individuals' medication use over time in order to better target high medications users, and those at higher risk of potentially inappropriate medication use. Latent class growth analysis (LCGA) is a special case of latent class growth mixture models that identify groups of individuals with similar patterns.14 This method has been used in the diabetes literature to study medication adherence patterns,15 depression or anxiety symptoms,16, 17, 18, 19, 20 patterns or health outcomes trajectories.21, 22, 23 However, to our knowledge, no study focused on medication patterns over time among older adults with incident diabetes. Exploring such patterns would help determine if, and to what extent, the burden of treating diabetes and comorbidities increases following diagnosis, and which patients are the most at risk of potentially inappropriate polypharmacy, which would help optimize pharmacotherapy.
Sex-differences exist in the prevalence of polypharmacy among older adults. Several studies have shown that females are generally more exposed to polypharmacy than males.24,25 However, according to a recent study in Canada, although the prevalence estimates of multimorbidity and polypharmacy were greater in females than males in 2003 and 2016, the absolute increase was greater for males over time,26 which narrowed the gap in 2016. To our knowledge, such a comparison of usage patterns between males and females has not been conducted in people newly diagnosed with diabetes.
The objectives of this paper were twofold: i) to identify trajectories of medications use in the four years following the diagnosis of diabetes, separately for males and females; ii) to describe the baseline characteristics associated with each trajectory, including medication classes and potentially inappropriate medications claimed in the year after the diagnosis.
2. Methods
The Quebec Integrated Chronic Disease Surveillance System (QICDSS) is a system developed and managed by the Institut national de santé publique du Québec (INSPQ) for chronic disease surveillance.27 The QICDSS includes five health administrative databases. Data on socio-demographic characteristics, eligibility and admissibility to the Quebec public health and drug insurance are included in the health insurance registry. The physician claims and hospitalization databases contain data on health services and hospitalizations, respectively. Data on death are recorded in the vital statistics death registry. Prescription medications information (e.g., name of the medications) is contained in the pharmaceutical services database. Medication data from the QICDSS cover >90% of community-dwelling adults aged 65 and older and these health administrative databases have been previously validated.28, 29, 30
The study population includes individuals aged 66 years or older as of April 1st, 2015, with a diagnosis of diabetes between April 1st, 2014, and March 31st, 2015. Individuals were followed until March 31st, 2019. We included participants who were entirely covered by the universal Public Prescription Drug Insurance Plan between April 1st, 2015, and March 31st, 2019, to better represent medication use. Individuals who were transferred to long-term care facilities were excluded because data on medications were not available. Finally, only individuals with at least three years of follow-up were included.
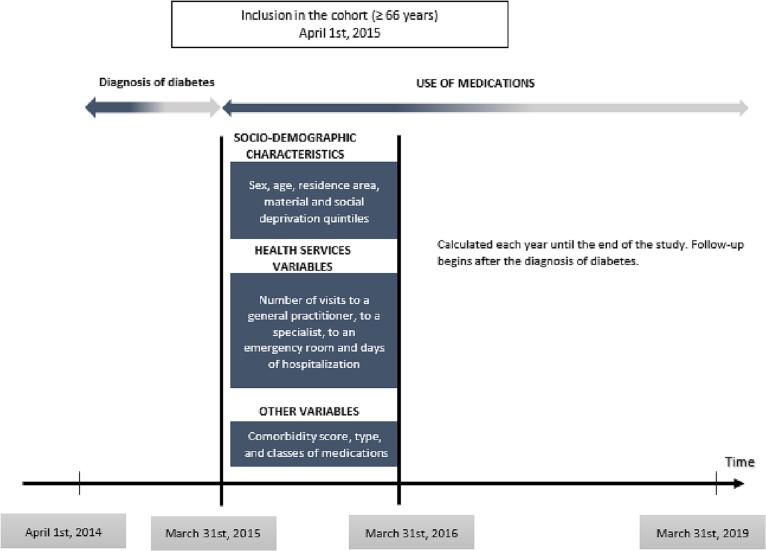
To identify individuals newly diagnosed with diabetes, we used a validated case definition (sensitivity = 94.6% and positive predictive value = 87.9%) routinely used in surveillance in Canada.5,31 Subjects with two physicians claims with a diagnosis of diabetes (International Classification of Diseases - 9th version, ICD-9: 250, ICD-10: E10-E14) within two years or one hospitalization with such a diagnosis code were considered as having diabetes.27 The date of diagnosis was the earliest of the second date of the physician claims, or the date of hospital discharge. The creation of the cohort is illustrated in Fig. 1.
Fig. 1.
Creation of the cohort of older adults newly diagnosed with diabetes in the province of Quebec, Canada.
The common denomination was used to identify the medications claimed by each subject.32 It corresponds to the 5th level of the Anatomical Therapeutical Chemical (ATC) classification. We considered subjects to be using a specific medication during a year if there was at least one claim for that medication during that year. For each fiscal year, we counted the total number of different medications claimed by each individual, regardless of the class of the medications.
We considered 11 baseline characteristics that were used as covariates. They included demographic variables [sex (male/female), age (in years), residence area (urban [≥10,000 inhabitants]/rural), material and social deprivation quintiles33], variables of health service utilization (number of visits to a general practitioner, a specialist, an emergency room and number of days of hospitalization), comorbidity score34 and medication variables (classes of medications, potentially inappropriate medications). The material and social deprivation quintiles,33 validated ecological proxies to socioeconomic status, were constructed from census data on the Quebec population, with quintile 1 comprising the most privileged and quintile 5 the most deprived subjects. The material deprivation quintile includes information on education, income, and employment status while the social deprivation quintile considers people who live alone in their homes, their marital status, and single-parent families. Comorbidities were assessed based on the combined comorbidity index of Charlson and Elixhauser (2018) that contains a list of 32 conditions with weights of comorbidities, using Charlson weights, ranging from 0 to 5.34 This index was validated in the Quebec population and provided high discrimination results in predicting mortality.34 We categorized the medication classes that were claimed following the year of diagnosis with the use of the 3rd level of the ATC classification. We also identified potentially inappropriate medications claimed in this period using the 2015 Beers criteria,13 which were previously adapted to our datasets (Table S1).11,35,36
We first described the characteristics of the included individuals using means and standard deviations for the continuous variables and proportions for the categorical variables. LCGA was used to identify groups of medication trajectories. Models with 1–10 trajectories were considered and the model with the lowest Bayesian information criterion (BIC) among those with at least 5% of individuals per group was selected. Once the number of groups was selected, the shapes of the trajectories were determined by modeling cubic polynomials and excluding higher order polynomial terms not significant at the 5% level. Participants were allocated to the trajectory group for which their posterior probability was highest. As recommended by several authors,22,37 we assessed the validity of trajectory groups using different procedures. We first computed three model adequacy criteria: the average posterior probability (values >70% indicate adequate classification), the odds of correct classification (values >5 suggest high accuracy in the assignment of trajectories) and the relative entropy (values above 0.8 imply less uncertainty in the classification). If any of the criteria were below the threshold, a model with fewer groups was considered. Then, we applied a method based on bootstrap to assess the uncertainty in the number of groups.38 We considered 100 bootstraps samples. All analyses were stratified by sex. Finally, for the second objective, we used descriptive statistics to present the characteristics of individuals in each trajectory. Analysis of variance and chi-square tests were used to assess statistical differences between demographic, health utilization and medication variables and identified trajectories with a level of significance α = 5%.
As a sensitivity analysis, we identified medication trajectories among participants newly diagnosed with diabetes and a comorbidity score of zero. This analysis aimed to better isolate the impact of the diagnosis of diabetes on medication use among individuals who do not present major comorbidities and therefore are not expected to use many medications at baseline.
Analyses were performed using SAS 9.4 software (SAS Institute, Cary, NC) and R.4.1.0 software (© 2021 The R Foundation for Statistical Computing, Austria, package FlexMix).39
The process for creating and for accessing the QICDSS data meet stringent standards of security and privacy. The use of these data was approved by the Commission d'accès à l'information du Québec and the government bodies (Régie de l'assurance de la maladie du Québec, Ministère de la Santé et des Services sociaux). This study meets all QICDSS data requirements for surveillance purposes and consent was not required for the participants.
3. Results
Table 1 presents the baseline characteristics of the 10,363 included individuals. Of them, 5330 (51.4%) were males. Participants were on average 74.2 years (standard deviation: SD = 6.3), had a mean comorbidity score of 2.7 (SD = 3.4) and a mean annual number of medications of 10.4 (SD = 5.9). Descriptively, females were older, more likely to be from an urban area, to be socially deprived, to claim more medications, and to have more encounters with a generalist in 2015 than males.
Table 1.
Characteristics of participants 66 years and older with a new diagnosis of diabetes, by sex, in the province of Quebec, Canada, 2015.
| Variables | Total (n = 10,363) | Males (n = 5330) | Females (n = 5033) |
|---|---|---|---|
| Age, mean (SD)1 | 74.2 (6.3) | 73.6 (5.8) | 74.9 (6.7) |
| Residence area2, n (%) | |||
| Urban | 8032 (77.6) | 4016 (75.3) | 4016 (79.8) |
| Rural | 2332 (22.4) | 1311 (24.6) | 1011 (20.1) |
| Material deprivation quintile2, n (%) | |||
| Quintile 1 (most privileged) | 1445 (15.4) | 776 (15.8) | 669 (15.0) |
| Quintile 2 | 1593 (17.0) | 852 (17.3) | 741 (16.6) |
| Quintile 3 | 1821 (19.4) | 944 (19.2) | 877 (19.6) |
| Quintile 4 | 2134 (22.8) | 1098 (22.4) | 1036 (23.2) |
| Quintile 5 (most deprived) | 2384 (25.4) | 1242 (25.3) | 1142 (25.6) |
| Social deprivation quintile2, n (%) | |||
| Quintile 1 (most privileged) | 1677 (17.9) | 943 (19.2) | 734 (16.4) |
| Quintile 2 | 1844 (19.7) | 1040 (21.2) | 804 (18.0) |
| Quintile 3 | 1895 (20.2) | 1040 (21.2) | 855 (19.1) |
| Quintile 4 | 1942 (20.7) | 938 (19.1) | 1004 (22.5) |
| Quintile 5 (most deprived) | 2019 (21.5) | 951 (19.4) | 1068 (23.9) |
| Comorbidity score, mean (SD)1 | 2.7 (3.4) | 2.8 (3.5) | 2.6 (3.3) |
| Number of medications used, mean (SD)1 | 10.4 (5.9) | 9.7 (5.7) | 11.2 (6.1) |
| Number of visits to a generalist, mean (SD)1 | 3.4 (3.0) | 3.2 (2.8) | 3.6 (3.2) |
| Number of visits to a specialist, mean (SD)1 | 5.3 (7.8) | 5.4 (8.1) | 5.1 (7.4) |
| Number of emergency visits, mean (SD)1 | 0.7 (1.4) | 0.6 (1.4) | 0.7 (1.3) |
| At least one emergency visits, n (%) | 3371 (32.5) | 1682 (31.6) | 1689 (33.6) |
| Length (in days) of hospitalization, mean (SD)1 | 2.0 (7.9) | 2.0 (8.3) | 1.9 (7.5) |
| Hospitalized at least one day, n (%) | 1587 (15.3) | 828 (15.5) | 759 (15.1) |
SD: Standard deviation.
Sum of counts for residence area, material and social deprivation quintiles does not equal the total number of subjects due to missing values.
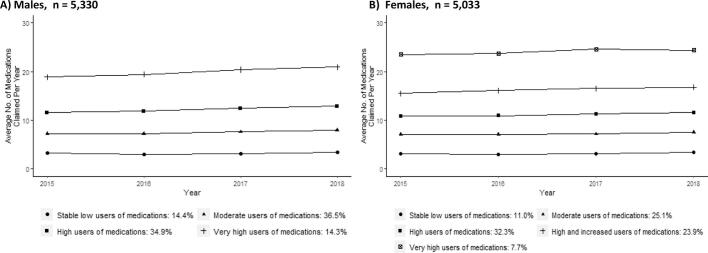
In the male subpopulation, the BIC suggested four groups of medication trajectories with quadratic shapes (Fig. 2 A, Table S2). All trajectories were characterized by sustained, stable number of medications claimed over the years, apart from the category that used the largest number of medications, whose claims tended to increase. >85% of the male subpopulation was included in trajectories with polypharmacy. Specifically, the largest group, identified as “moderate users of medications” (36.5%, 1946/5330), had an average of 7.1 different medications in 2015. Approximately 35% of individuals pertained to the “high users of medications” (34.9%, 1858/5330) group, that claimed an average of 11.5 different medications. “Stable low users of medications” (14.4%, 766/5330) consistently had low claims of medications (mean = 3.2). In contrast, 14.3% (760/5330) were included in the “very high users of medications” group, that claimed an average of 18.7 different medications and gradually increased the number of medications.
Fig. 2.
Trajectories of medications used among individuals with a new diagnosis of diabetes, by sex, in Quebec, Canada, n = 10,363.
Legend. The year refers to the fiscal year. For example, medications claimed between April 1st, 2015, and March 31st, 2016, were considered as the number used for 2015.
There were significant differences in baseline characteristics between the four groups. We observed a constant progression in the age of the individuals, their comorbidity score and their use of health services according to the increase in the number of medications in the trajectory groups (Table 2). Similarly, the proportion of users of the different classes of medications at baseline increased steadily from the trajectory of “stable low users of medications” to the one of “very high users of medications” (Fig. S1, A). Medication classes used in diabetes and cardiovascular diseases (lipid modifying agents, agents acting on the renin-angiotensin system, beta blocking agents and calcium channel blockers) were frequently claimed across all groups, with lipid modifying agents being the most frequent category. All in all, the relative importance of each medication classes used was very similar through the trajectories, except that in the “high users of medications” and the “very high users of medications” groups, a higher proportion of individuals claimed analgesics and drugs for acid related disorders. The pattern of use of potentially inappropriate medication was somewhat less related to the gradient of medication trajectories, but “high users of medications”, and especially “very high users of medications” were more likely to claim them. >40% of “very high users of medications” had a claim for potentially inappropriate medications of the central nervous system (Fig. S2).
Table 2.
Characteristics of older males newly diagnosed with diabetes by trajectory groups in Quebec, Canada, n = 5330, 2015.
| Stable low users of medications (n = 766) | Moderate users of medications (n = 1946) | High users of medications (n = 1858) | Very high users of medications (n = 760) | p-value | |
|---|---|---|---|---|---|
| Age, mean (SD)1 | 72.3 (5.3) | 73.1 (5.5) | 74.1 (6.0) | 75.0 (6.3) | <0.001 |
| Residence area, n (%) | |||||
| Urban | 594 (77.5) | 1508 (77.5) | 1362 (73.4) | 552 (72.7) | 0.004 |
| Rural | 172 (22.5) | 438 (22.5) | 493 (26.6) | 208 (27.4) | |
| Material deprivation quintile2, n (%) | 0.289 | ||||
| Quintile 1 (privileged) | 118 (16.3) | 312 (17.4) | 249 (14.5) | 97 (14.3) | |
| Quintile 2 | 115 (15.9) | 326 (18.1) | 291 (17.0) | 120 (17.7) | |
| Quintile 3 | 148 (20.4) | 337 (18.7) | 339 (19.8) | 120 (17.7) | |
| Quintile 4 | 166 (22.9) | 384 (21.4) | 378 (22.1) | 170 (25.1) | |
| Quintile 5 (deprived) | 177 (24.4) | 439 (24.4) | 455 (26.6) | 171 (25.2) | |
| Social deprivation quintile2, n (%) | 0.112 | ||||
| Quintile 1 (privileged) | 162 (22.4) | 354 (19.7) | 309 (18.1) | 118 (17.4) | |
| Quintile 2 | 152 (21.0) | 391 (21.7) | 355 (20.7) | 142 (20.9) | |
| Quintile 3 | 147 (20.3) | 394 (21.9) | 365 (21.3) | 134 (19.8) | |
| Quintile 4 | 129 (17.8) | 349 (19.4) | 325 (19.0) | 135 (19.9) | |
| Quintile 5 (deprived) | 134 (18.5) | 310 (17.2) | 358 (20.9) | 149 (22.0) | |
| Comorbidity score, mean (SD)1 | 1.5 (2.5) | 2.0 (2.7) | 3.2 (3.4) | 5.6 (4.3) | <0.001 |
| Number of medications used, mean (SD)1 | 3.2 (2.1) | 7.1 (2.2) | 11.5 (3.2) | 18.7 (6.0) | <0.001 |
| Number of visits to a generalist, mean (SD)1 | 2.0 (1.9) | 2.7 (2.2) | 3.5 (2.8) | 4.7 (3.8) | <0.001 |
| Number of visits to a specialist, mean (SD)1 | 2.6 (3.6) | 3.7 (4.9) | 6.3 (7.2) | 10.8 (14.6) | <0.001 |
| Number of emergency visits, mean (SD)1 | 0.2 (0.7) | 0.3 (0.8) | 0.7 (1.2) | 1.7 (2.5) | <0.001 |
| At least one emergency visits, n (%) | 128 (16.7) | 425 (21.8) | 672 (36.2) | 457 (60.1) | <0.001 |
| Length (in days) of hospitalization, mean (SD)1 | 0.5 (3.3) | 0.7 (5.7) | 2.1 (7.5) | 6.5 (14.8) | <0.001 |
| Hospitalized at least one day, n (%) | 43 (5.6) | 168 (8.6) | 331 (17.8) | 286 (37.6) |
SD: Standard deviation.
Sum of counts for residence area, material and social deprivation quintiles does not equal the total number of subjects due to missing values.
In the female subpopulation, the optimal model suggested by the BIC was five groups with quadratic shapes (Fig. 2 B,Table S2). Similar to the male subpopulation, all trajectories showed a sustained and stable number of medications except two which presented a trend toward increased use, but not as large as that identified in the male subpopulation. Nine out of ten (89%) women were included in trajectories with polypharmacy. The largest group “high users of medications” (32.3%, 1625/5033) claimed constant high number of medications over time (mean = 10.8 in 2015) (Fig. 2, B).
The differences in baseline characteristics between the groups followed the same patterns as observed in men; the more medications the trajectories include, the older the individuals, the higher their comorbidity score and the greater the use of health services (Table 3). However, the distribution of the classes of medications was more heterogeneous between the groups in female than male, and the proportions of users did not increase steadily across trajectories as was observed in the male subgroup (Fig. S1, B). For example, while lipid modifying agents, agents acting on the renin-angiotensin system and drug used in diabetes were again frequent medication classes, there was no evident increase in the proportion of users beyond the trajectory of “high users of medications”. The most frequent class of medications claimed in the two groups of very high use and high and increased use of medications were drugs for acid related disorders and analgesics, classes that were also identified among men. Trends for the use of potentially inappropriate medications were more present in females than males, with the proportion of users increasing with the increase in medication trajectories. The pattern was most prominent with central nervous system medications, where >50% of “very high users of medications” and “high and increased users of medications” had a claim for a medication in this category (Fig. S2).
Table 3.
Characteristics of older females newly diagnosed with diabetes by trajectory groups, Quebec, Canada, n = 5033, 2015.
| Stable low users of medications (n = 552) | Moderate users of medications (n = 1262) | High users of medications (n = 1625) | High and increased users of medications (n = 1205) | Very high users of medications (n = 389) | p-value | |
|---|---|---|---|---|---|---|
| Age, mean (SD)1 | 72.81 (5.92) | 73.81 (6.21) | 75.33 (6.84) | 76.22 (6.76) | 75.90 (7.06) | <0.001 |
| Residence area, n (%) | 0.001 | |||||
| Urban | 454 (82.2) | 1052 (83.4) | 1276 (78.6) | 940 (78.2) | 296 (76.1) | |
| Rural | 98 (17.8) | 210 (16.6) | 348 (21.4) | 262 (21.8) | 93 (23.9) | |
| Material deprivation quintile2, n (%) | 0.002 | |||||
| Quintile 1 (privileged) | 92 (17.6) | 183 (16.0) | 204 (14.3) | 157 (15.2) | 33 (9.7) | |
| Quintile 2 | 99 (19.0) | 171 (14.9) | 247 (17.3) | 168 (16.2) | 56 (16.5) | |
| Quintile 3 | 98 (18.8) | 254 (22.2) | 266 (18.6) | 178 (17.2) | 81 (23.9) | |
| Quintile 4 | 96 (18.4) | 261 (22.8) | 358 (25.1) | 252 (24.3) | 69 (20.4) | |
| Quintile 5 (deprived) | 136 (26.1) | 275 (24.0) | 351 (24.6) | 280 (27.1) | 100 (29.5) | |
| Social deprivation quintile2, n (%) | 0.475 | |||||
| Quintile 1 (privileged) | 102 (19.5) | 197 (17.2) | 227 (15.9) | 153 (14.8) | 55 (16.2) | |
| Quintile 2 | 100 (19.2) | 188 (16.4) | 260 (18.2) | 188 (18.2) | 68 (20.1) | |
| Quintile 3 | 96 (18.4) | 238 (20.8) | 261 (18.3) | 206 (19.9) | 54 (15.9) | |
| Quintile 4 | 110 (21.1) | 247 (21.6) | 332 (23.3) | 240 (23.2) | 75 (22.1) | |
| Quintile 5 (deprived) | 113 (21.6) | 274 (24.0) | 346 (24.2) | 248 (24.0) | 87 (25.7) | |
| Comorbidity score, mean (SD)1 | 0.93 (1.86) | 1.53 (2.44) | 2.46 (3.10) | 3.66 (3.49) | 5.42 (4.01) | <0.001 |
| Number of medications used, mean (SD)1 | 3.17 (2.23) | 7.02 (2.08) | 10.84 (2.65) | 15.60 (3.69) | 23.48 (5.65) | <0.001 |
| Number of visits to a generalist, mean (SD)1 | 2.21 (1.94) | 2.77 (2.10) | 3.37 (2.65) | 4.58 (3.65) | 6.48 (5.37) | <0.001 |
| Number of visits to a specialist, mean (SD)1 | 2.43 (3.53) | 3.13 (4.03) | 4.80 (5.54) | 7.15 (10.65) | 10.53 (9.70) | <0.001 |
| Number of emergency visits, mean (SD)1 | 0.21 (0.61) | 0.30 (0.77) | 0.56 (1.09) | 0.99 (1.48) | 2.07 (2.51) | <0.001 |
| At least one emergency visits, n (%) | 77 (13.9) | 245 (19.4) | 519 (31.9) | 587 (48.7) | 261 (67.1) | <0.001 |
| Length (in days) of hospitalization, mean (SD)1 | 0.32 (2.10) | 0.54 (2.64) | 1.41 (6.62) | 3.10 (9.62) | 7.50 (13.40) | <0.001 |
| Hospitalized at least one day, n (%) | 22 (4.0) | 89 (7.1) | 201 (12.4) | 263 (21.8) | 184 (47.3) | <0.001 |
SD: Standard deviation.
Sum of counts for material and social deprivation quintiles does not equal the total number of subjects due to missing values.
The three model adequacy criteria were above the recommended threshold suggesting adequate criteria for both subpopulations (Table S3). Of the 100 bootstraps samples, among the male subpopulation, 59 selected four groups and 35 six groups (Table S4), in which two groups contained no individuals and the trajectories obtained were the same as those of the four-group model. Among the female subpopulation, 86 of the 100 bootstrap samples selected five groups and seven selected four and six groups, respectively. These results support that the number of groups found is adequate. In addition, the results of the sensitivity analysis were similar to those of the main analysis; the trajectory groups of individuals with a comorbidity score of zero were predominantly like those in the general population (Supplementary material B, Fig. S3).
4. Discussion
In this population of individuals newly diagnosed with diabetes, we found that for both male and female, <15% had low medication claims or no polypharmacy. Trajectories of medication claims were mostly stable over time, but the increase of medications claims was faster among people who had claims for more medications at baseline. No trajectory suggested a decrease in medication, which could have been the result of deprescribing.
For most trajectories, there was no obvious increase in the number of medications claimed in the year following the diagnosis of diabetes. The fact that the number of medications was already very high immediately after the diagnosis of diabetes may partly explain this observation, as many cardioprotective medications, for example, were already used. Interestingly, the diagnosis of diabetes did not seem to cause prescribing cascades or lead to other conditions that would increase the use of medications, which is reassuring from a clinical and public health perspective. This also held true for the subpopulation with a comorbidity score of 0. However, the fact that the trajectories with the highest medication use were the ones where increasing trends were seen warrants caution, as these individuals already appeared the most vulnerable to the adverse effects of polypharmacy because of their baseline characteristics and the fact that they were more often exposed to potentially inappropriate medications. Other studies have described trajectories in other populations and found that more than half of included participants were in the trajectory of high level medications use over time.9,40 Although the study population was different than ours and does not include only newly diagnosed individuals, their results also show that high use of medications persists over time and is not only related to people with diabetes.
Differences in medication claims according to sex were observed. We found that females tended to have higher levels of medication claims than males, which is concordant with other studies.26 Differences in medication use at baseline was also significant between trajectories and sex. While medication classes pertaining to the prevention/treatment of cardiovascular comorbidities were consistently prominent in all male-specific trajectories, medication classes used at baseline were more heterogenous in female-specific trajectories. The diversity of medication classes can be explained by the use of sex-specific medications, such as calcium and vitamin D use in women. However, some gender disparities may also be present, as the use of cardioprotective treatments have been shown to be used less frequently among women than men.41 Of note, the use of analgesics was frequent for both men and women in trajectories with high medication use, suggesting that pain may represent a significant issue among those individuals. However, our analysis does not permit to evaluate if this condition was acute or chronic.
The use of potentially inappropriate medications was mostly problematic in trajectories with a high number of medications. Medications acting on the central nervous system was particularly significant, which is concordant with the results of a population-based study conducted in Taiwan from 2013 to 2015 in older adults with chronic diseases.42 Beers criteria recommend that tricyclic antidepressants, paroxetine and benzodiazepines, for example, should be avoided in older adults because of their associated increased risk of anticholinergic effects and cognitive impairment, among others.13 Furthermore, using a combination of three or more certain central nervous system medications can increase the risk of falls or fracture.13 Again, since the individuals in the trajectory groups with many medications presented characteristics that made them vulnerable, the associated risks might be even greater for this population frequently exposed to these medications.
In this article, we included the entire population that met the inclusion criteria, and the public drug plan covers a wide range of medications. Hence, we are able to describe a very accurate profile of medications claimed. Limitations of this study are related to the nature of the data. Because the data were extracted from health administrative databases, we do not have access to a clinical definition of diabetes. Therefore, we used a validated definition of diabetes to identify diabetes cases. The study population may include some false positives. We do not have the indication for the medications, or the clinical information needed to assess the appropriateness of the treatment. Then, we considered medication claims as use of medications, however, individuals may not use all medications. We also did not look at concurrent medication use. Hence, we have a picture over a whole year and medications taken over a short period of time or for an acute condition will have the same weight as medications taken chronically. Nevertheless, this is the most used way to study polypharmacy or potentially inappropriate medications because it allows an idea of the diversity and complexity of the medications that were used in the year.11,43,44 We also excluded the sickest people, that is, those who died and those who were admitted to long-term care. However, their consumption might have been different, since end-of-life care is associated with an increase in care, thus their inclusion would likely have generated heterogeneity. Data for non-prescription medications or natural medicines are not available; thus, our results likely underestimate the total number of medications received by older adults. Finally, because our results are based on data from a single province in Canada, they may not generalize to other countries. In particular, medication trajectories may be different in low- and middle-income countries or in jurisdictions where older adults do not benefit from public drug insurance.
5. Conclusion
In conclusion, both males and females newly diagnosed with diabetes have a significant baseline medication burden. In this first study to describe medication patterns in newly diagnosed individuals with diabetes, we observed that most individuals have sustained medication use over time and the increase in number of medications is more important among heavy users, which strengthens the importance of considering the longitudinal aspect of polypharmacy. Physicians must be aware that any additional medications will increase polypharmacy; therefore, they should regularly assess the appropriateness of all medications and deprescribe when possible.
Funding
This work was supported by a Collaborative Health Research Projects grant from the Canadian Institute of Health Research and the Natural Sciences and Engineering Research Council of Canada (grant number: CPG-170621). Miceline Mésidor is supported by a postdoctoral fellowship from the Fonds de recherche du Québec – Santé (FRQS). Caroline Sirois and Denis Talbot are holders of a Junior 2 salary awards from the FRQS. Marc Simard is supported by a PhD fellowship from the FRQS.
Authors contributions
MM, CS and DT developed the original idea and designed the analytical plan. MM conducted the literature review, completed the statistical analyses, and drafted the manuscript. MS, VB, and CB were involved in the creation of the cohort study. All authors critically reviewed and approved the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rcsop.2023.100294.
Appendix A. Supplementary data
Supplementary material
Data availability
Data used for the analysis are the propriety of the Ministère de la Santé et des Services sociaux du Québec and the Régie de l'assurance maladie du Québec. Access to these data is limited to authorized personnel of the Chronic Disease and Injury Surveillance Unit.
References
- 1.Institut national de santé publique du Québec . Institut national de santé publique du Québec; 2020. Prévalence du diabète pour la population d’un an et plus (SISMACQ). SP2–039. [Google Scholar]
- 2.Schernthaner G., Schernthaner-Reiter M.H. Diabetes in the older patient: heterogeneity requires individualisation of therapeutic strategies. Diabetologia. 2018;61(7):1503–1516. doi: 10.1007/s00125-018-4547-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iglay K., Hannachi H., Joseph Howie P., et al. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32(7):1243–1252. doi: 10.1185/03007995.2016.1168291. [DOI] [PubMed] [Google Scholar]
- 4.Bilandzic A., Rosella L. The cost of diabetes in Canada over 10 years: applying attributable health care costs to a diabetes incidence prediction model. Health Promot Chronic Dis Prev Can. 2017;37(2):49–53. doi: 10.24095/hpcdp.37.2.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gagnon M.E., Sirois C., Simard M., Plante C. Polypharmacy and pharmacological treatment of diabetes in older individuals: a population-based study in Quebec, Canada. Pharmacy (Basel) 2019;(4):7. doi: 10.3390/pharmacy7040161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Varghese D., Ishida C., Haseer Koya H. StatPearls Publishing; Treasure Island (FL): 2022. Polypharmacy. StatPearls. p. PMID: 30422548. [PubMed] [Google Scholar]
- 7.Sirois C., Domingues N.S., Laroche M.L., et al. Polypharmacy definitions for multimorbid older adults need stronger foundations to guide research, clinical practice and public health. Pharmacy (Basel) 2019;7(3) doi: 10.3390/pharmacy7030126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wastesson J.W., Morin L., Tan E.C.K., Johnell K. An update on the clinical consequences of polypharmacy in older adults: a narrative review. Expert Opin Drug Saf. 2018;17(12):1185–1196. doi: 10.1080/14740338.2018.1546841. [DOI] [PubMed] [Google Scholar]
- 9.Thapaliya K., Harris M.L., Byles J.E. Polypharmacy trajectories among older women with and without dementia: a longitudinal cohort study. Explor Res Cin Soc Pharm. 2021;3 doi: 10.1016/j.rcsop.2021.100053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fried T.R., Mecca M.C. Medication appropriateness in vulnerable older adults: healthy skepticism of appropriate polypharmacy. J Am Geriatr Soc. 2019;67(6):1123–1127. doi: 10.1111/jgs.15798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roux B., Sirois C., Simard M., Gagnon M.E., Laroche M.L. Potentially inappropriate medications in older adults: a population-based cohort study. Fam Pract. 2020;37(2):173–179. doi: 10.1093/fampra/cmz060. [DOI] [PubMed] [Google Scholar]
- 12.Laroche M.L., Charmes J.P., Merle L. Potentially inappropriate medications in the elderly: a French consensus panel list. Eur J Clin Pharmacol. 2007;63(8):725–731. doi: 10.1007/s00228-007-0324-2. [DOI] [PubMed] [Google Scholar]
- 13.American Geriatrics Society Beers Criteria Update Expert Panel American Geriatrics Society 2019 updated AGS beers criteria(R) for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674–694. doi: 10.1111/jgs.15767. [DOI] [PubMed] [Google Scholar]
- 14.van der Nest G., Lima Passos V., Candel M.J.J.M., van Breukelen G.J.P. An overview of mixture modelling for latent evolutions in longitudinal data: modelling approaches, fit statistics and software. Adv Life Course Res. 2020;43 doi: 10.1016/j.alcr.2019.100323. [DOI] [PubMed] [Google Scholar]
- 15.Alhazami M., Pontinha V.M., Patterson J.A., Holdford D.A. Medication adherence trajectories: a systematic literature review. J Manag Care Spec Pharm. 2020;26(9):1138–1152. doi: 10.18553/jmcp.2020.26.9.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whitworth S.R., Bruce D.G., Starkstein S.E., et al. Depression symptoms are persistent in type 2 diabetes: risk factors and outcomes of 5-year depression trajectories using latent class growth analysis. Diabet Med. 2017;34(8):1108–1115. doi: 10.1111/dme.13372. [DOI] [PubMed] [Google Scholar]
- 17.Chiu C.J., Tseng Y.H., Hsu Y.C., Wu S.T., Wray L.A. Depressive symptom trajectories in the first 10 years of diabetes diagnosis: antecedent factors and link with future disability in Taiwan. Soc Psychiatry Psychiatr Epidemiol. 2017;52(7):829–836. doi: 10.1007/s00127-016-1314-4. [DOI] [PubMed] [Google Scholar]
- 18.Chiu C.J., Tseng Y.H., Hsu Y.C., Wu S.T., Wray L.A. Correction to: depressive symptom trajectories in the first 10 years of diabetes diagnosis: antecedent factors and link with future disability in Taiwan. Soc Psychiatry Psychiatr Epidemiol. 2018;53(8):869. doi: 10.1007/s00127-018-1543-9. [DOI] [PubMed] [Google Scholar]
- 19.Whitworth S.R., Bruce D.G., Starkstein S.E., et al. Risk factors and outcomes of anxiety symptom trajectories in type 2 diabetes: the Fremantle diabetes study phase II. Diabet Med. 2020;37(10):1688–1695. doi: 10.1111/dme.14344. [DOI] [PubMed] [Google Scholar]
- 20.Deschenes S.S., Burns R.J., Schmitz N. Trajectories of anxiety symptoms and associations with incident cardiovascular disease in adults with type 2 diabetes. J Psychosom Res. 2018;104:95–100. doi: 10.1016/j.jpsychores.2017.11.015. [DOI] [PubMed] [Google Scholar]
- 21.Li J.C., Tian J., Wu S.L., et al. Effect of long-term systolic blood pressure trajectory on kidney damage in the diabetic population: a prospective study in a community-based Chinese cohort. Chin Med J (Engl) 2018;131(10):1199–1205. doi: 10.4103/0366-6999.231528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lennon H., Kelly S., Sperrin M., et al. Framework to construct and interpret latent class trajectory modelling. BMJ Open. 2018;8(7) doi: 10.1136/bmjopen-2017-020683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Botvin Moshe C., Haratz S., Ravona-Springer R., et al. Long-term trajectories of BMI predict carotid stiffness and plaque volume in type 2 diabetes older adults: a cohort study. Cardiovasc Diabetol. 2020;19(1):138. doi: 10.1186/s12933-020-01104-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ukhanova M., Markwardt S., Furuno J.P., Davis L., Noble B.N., Quinones A.R. Are there sex differences in potentially inappropriate prescribing in adults with multimorbidity? J Am Geriatr Soc. 2021;69(8):2163–2175. doi: 10.1111/jgs.17194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Linjakumpu T., Hartikainen S., Klaukka T., Veijola J., Kivela S.L., Isoaho R. Use of medications and polypharmacy are increasing among the elderly. J Clin Epidemiol. 2002;55(8):809–817. doi: 10.1016/s0895-4356(02)00411-0. [DOI] [PubMed] [Google Scholar]
- 26.Maxwell C.J., Mondor L., Pefoyo Kone A.J., Hogan D.B., Wodchis W.P. Sex differences in multimorbidity and polypharmacy trends: a repeated cross-sectional study of older adults in Ontario, Canada. PloS One. 2021;16(4) doi: 10.1371/journal.pone.0250567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blais C., Jean S., Sirois C., et al. Quebec integrated chronic disease surveillance system (QICDSS), an innovative approach. Chronic Dis Inj Can. 2014;34(4):226–235. [PubMed] [Google Scholar]
- 28.Tamblyn R., Lavoie G., Petrella L., Monette J. The use of prescription claims databases in pharmacoepidemiological research: the accuracy and comprehensiveness of the prescription claims database in Quebec. J Clin Epidemiol. 1995;48(8):999–1009. doi: 10.1016/0895-4356(94)00234-h. [DOI] [PubMed] [Google Scholar]
- 29.Wilchesky M., Tamblyn R.M., Huang A. Validation of diagnostic codes within medical services claims. J Clin Epidemiol. 2004;57(2):131–141. doi: 10.1016/S0895-4356(03)00246-4. [DOI] [PubMed] [Google Scholar]
- 30.Lambert L., Blais C., Hamel D., et al. Evaluation of care and surveillance of cardiovascular disease: can we trust medico-administrative hospital data? Can J Cardiol. 2012;28(2):162–168. doi: 10.1016/j.cjca.2011.10.005. [DOI] [PubMed] [Google Scholar]
- 31.Hux J.E., Ivis F., Flintoft V., Bica A. Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care. 2002;25(3):512–516. doi: 10.2337/diacare.25.3.512. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization Guidance on the use of International Nonproprietary Names (INNs) for pharmaceutical substances. 2017. https://cdn.who.int/media/docs/default-source/international-nonproprietary-names-(inn)/who-pharm-s-nom-1570.pdf?sfvrsn=8358367e_4&download=true
- 33.Pampalon R., Hamel D., Gamache P., Raymond G. A deprivation index for health planning in Canada. Chronic Dis Can. 2009;29(4):178–191. [PubMed] [Google Scholar]
- 34.Simard M., Sirois C., Candas B. Validation of the combined comorbidity index of Charlson and Elixhauser to predict 30-day mortality across ICD-9 and ICD-10. Med Care. 2018;56(5):441–447. doi: 10.1097/MLR.0000000000000905. [DOI] [PubMed] [Google Scholar]
- 35.Roux B., Sirois C., Simard M., Gagnon M.E., Laroche M.L. One-year persistence of potentially inappropriate medication use in older adults: a population-based study. Br J Clin Pharmacol. 2020;86(6):1062–1080. doi: 10.1111/bcp.14214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gagnon M.E., Sirois C., Simard M., Roux B., Plante C. Potentially inappropriate medications in older individuals with diabetes: a population-based study in Quebec. Canada Prim Care Diabetes. 2020;14(5):529–537. doi: 10.1016/j.pcd.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 37.van de Schoot R., Sijbrandij M., Winter S.D., Depaoli S., Vermunt J.K. The GRoLTS-checklist: guidelines for reporting on latent trajectory studies. Struct Equ Modeling. 2017;24(3):451–467. [Google Scholar]
- 38.Mésidor M., Sirois C., Simard M., Talbot D. A bootstrap approach for validating the number of groups identified by latent class growth models. Am J Epidemiol. 2023 doi: 10.1093/aje/kwad148. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 39.Leisch F. FlexMix: a general framework for finite mixture models and latent class regression in R. J Stat Softw. 2004;11(8):1–18. [Google Scholar]
- 40.Falster M.O., Charrier R., Pearson S.A., Buckley N.A., Daniels B. Long-term trajectories of medicine use among older adults experiencing polypharmacy in Australia. Br J Clin Pharmacol. 2021;87(3):1264–1274. doi: 10.1111/bcp.14504. [DOI] [PubMed] [Google Scholar]
- 41.Huebschmann A.G., Huxley R.R., Kohrt W.M., Zeitler P., Regensteiner J.G., Reusch J.E.B. Sex differences in the burden of type 2 diabetes and cardiovascular risk across the life course. Diabetologia. 2019;62(10):1761–1772. doi: 10.1007/s00125-019-4939-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang T.-C., Ku P.-J., Lu H.-L., Hsu K.-C., Trezise D., Wang H.-Y. Association between potentially inappropriate medication use and chronic diseases in the elderly. Int J Environ Res Public Health. 2019;16(12):2189. doi: 10.3390/ijerph16122189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Campeau Calfat A., Simard M., Ouali A., Blais C., Sirois C. Polypharmacy among older individuals with heart failure: trends between 2000 and 2017 in the province of Quebec. Canada Ther Adv Cardiovasc Dis. 2022;16 doi: 10.1177/17539447221113946. 17539447221113946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Simard M., Rahme E., Calfat A.C., Sirois C. Multimorbidity measures from health administrative data using ICD system codes: a systematic review. Pharmacoepidemiol Drug Saf. 2022;31(1):1–12. doi: 10.1002/pds.5368. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
Data used for the analysis are the propriety of the Ministère de la Santé et des Services sociaux du Québec and the Régie de l'assurance maladie du Québec. Access to these data is limited to authorized personnel of the Chronic Disease and Injury Surveillance Unit.