Summary
Background
Quitting smoking is especially challenging for low-income smokers due to high stress, high smoking prevalence around them, and limited support for quitting. This study aimed to determine whether any of three interventions designed specifically for low-income smokers would be more effective than standard tobacco quitline services: a specialized quitline, the specialized quitline with social needs navigation, or the standard quitline with social needs navigation.
Methods
Using a randomized 2 × 2 factorial design, low-income daily cigarette smokers (n = 1944) in Missouri, USA who called a helpline seeking assistance with food, rent or other social needs were assigned to receive Standard Quitline alone (n = 485), Standard Quitline + Social Needs Navigation (n = 484), Specialized Quitline alone (n = 485), or Specialized Quitline + Social Needs Navigation (n = 490). The target sample size was 2000, 500 per group. The main outcome was 7-day self-reported point prevalence abstinence at 6-month follow-up. Multiple imputation was used to impute outcomes for those missing data at 6-month follow-up. Binary logistic regression analyses were used to assess differences between study groups.
Findings
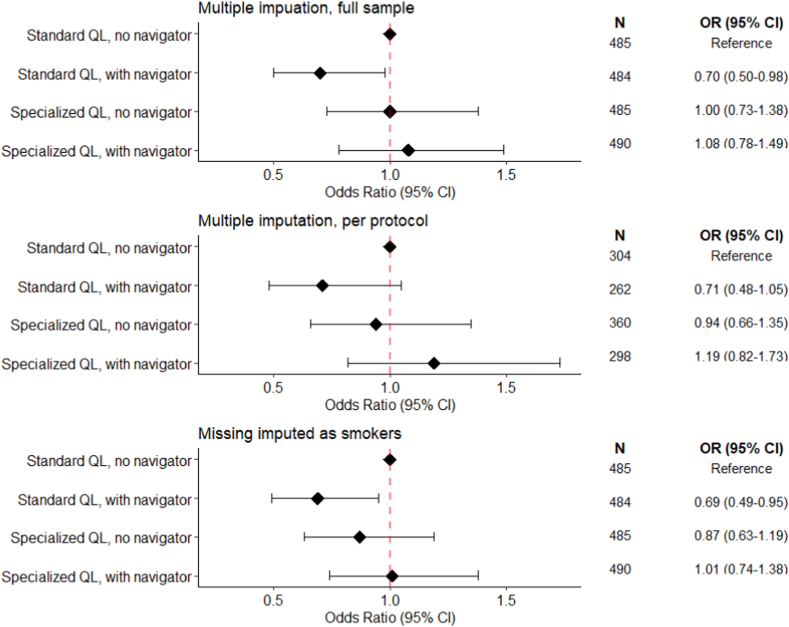
Participants were recruited from June 2017 to November 2020; most were African American (1111 [58%]) or White (666 [35%]), female (1396 [72%]), and reported <$10,000 (957 [51%]) or <$20,000 (1529 [82%]) annual pre-tax household income. At 6-month follow-up (58% retention), 101 participants in the Standard Quitline group reported 7-day point prevalence abstinence (20.8% of those assigned at baseline, 38.1% after imputation). Quit rates in the Specialized Quitline (90 quitters, 18.6%, 38.1%) and Specialized Quitline + Social Needs Navigation (103 quitters, 21.0%, 39.8%) were not different from the Standard Quitline. Quit rates for Standard Quitline + Social Needs Navigation (74 quitters, 15.3%, 30.1%) were significantly lower than Standard Quitline (OR = 0.70, 95% CI = 0.50–0.98).
Interpretation
A specialized version of a state tobacco quitline was no more effective than standard quitline services in helping low-income smokers quit. Adding social needs navigation to a standard quitline decreased its effectiveness.
Trial registration
ClinicalTrials.gov Identifier: NCT03194958.
Funding
National Cancer Institute: R01CA201429.
Keywords: Smoking, Cessation, Low-income, Health disparities, Health equity, Social needs, Minority health, Tobacco quitlines
Research in context.
Evidence before this study
We searched Google Scholar (October 1, 2022) for review articles published 2000–2022 using two search strategies: (1) “tobacco” or “smoking” AND “cessation” AND “barriers” AND “low income” or “low socioeconomic status”; and (2) “tobacco” or “smoking” AND “cessation” AND “telephone counseling” (or “counselling”) AND “systematic review.” Among the results, the U.S. Surgeon General’s Report on Smoking Cessation (2020) concluded that the proportion of U.S. smokers from racial or ethnic minority groups and/or households in poverty increased from 2000 to 2018, and smokers with the lowest levels of education were the least likely to have tried quitting. Another systematic review of 65 quantitative and qualitative studies identified three main barriers to cessation for low-income smokers: high stress, high prevalence and acceptability of smoking, and limited support in quitting. To make cessation services available population wide and regardless of income, free telephone tobacco quitlines—delivering evidence-based telephone cessation counseling—exist in every state and many countries. A 2019 Cochrane review of 104 studies reported moderate-certainty evidence for the effectiveness of telephone counseling for smoking cessation, with significant risk ratios compared to self-help or minimal interventions (RR = 1.35), brief interventions (RR = 1.30) and when added to pharmacotherapy for cessation (RR = 1.14). However, a review of 65 of the Cochrane-included studies that were conducted in the U.S. concluded that evidence for effectiveness was less clear among low-SES smokers, due to both mixed results and a paucity of studies that reported SES data.
Added value of this study
A specialized quitline designed to address unique barriers to quitting among low-income smokers did not yield significantly higher cessation rates than standard quitline services. Pairing standard quitline services with a social needs intervention to address low-income smokers’ financial stressors such as food, rent and utility payments significantly decreased cessation rates compared to the standard quitline alone. Findings suggest that when delivered simultaneously, a social needs intervention may actually interfere with standard quitline services among low-income smokers.
Implications of all the available evidence
In 2018, tobacco quitline services were available in 66 countries. Assuring these services are effective for and responsive to the needs of the most underserved smokers is essential for achieving health equity.
Introduction
Low-income smokers make up a disproportionate share of the U.S. smoking population1 and suffer a disproportionate burden of health consequences of smoking.2 Compared to other smokers, they are less likely to try quitting and to succeed.3,4 To identify barriers to cessation that are unique to low-income smokers, we searched Google Scholar (October 1, 2022) for review articles published 2000–2022 using “tobacco” or “smoking” AND “cessation” AND “barriers” AND “low income” or “low socioeconomic status” as search terms. Summarizing this literature, one systematic review identified three categories of barriers: high stress, high prevalence and acceptability of smoking, and limited support in quitting.5
Stress due to financial strain and other life challenges affects smoking, cessation and relapse. It increases tobacco cravings, number of cigarettes smoked per day and smoking intensity, and decreases ability to resist smoking.6, 7, 8 Studies suggest the relationship between socioeconomic status (SES) and smoking is largely mediated by stress,9,10 with smoking viewed by some low-SES smokers as a coping mechanism for life stressors.11 Greater financial strain is also associated with lower motivation to quit and increased relapse.12,13 Dealing with social needs such as overdue rent, unpaid bills or food insecurity likely supersede interests in quitting smoking.14,15 This is not simply prioritization, but also because having unmet social needs can diminish one’s cognitive capacity to focus on other goals, leading to shorter term thinking and decision-making that focuses on immediate needs.16,17 For example, although low-income smokers commonly cite health problems as a motive for quitting, they express less concern about future health problems than high-SES smokers.18,19
Smoking is also normative in the lives of many low-income smokers.20,21 On average, U.S. smokers report that 2.7 of their 5 closest friends smoke; however, the mean is even higher (>2.9) among low-income and low-education smokers.22 In a 5-state study, 66% of low-income smokers reported that half or more of their friends and relatives smoke.23,24 The odds of quitting decline and odds of relapse increase the larger the proportion of smokers in one’s social network.25 Cessation may also be more difficult for low-income smokers because they have fewer people supporting a quit attempt,11 are more likely to be targeted directly by tobacco marketing efforts,26 encounter tobacco and tobacco promotion in retail outlets near their homes,27 and have less control over tobacco exposure in their workplaces.28 Collectively, these norms increase exposure to cues that prompt smoking while reducing social pressure to quit.29,30
Low-income smokers are also less likely to get help quitting. Compared to higher income smokers, they are less likely to receive physician advice to quit31 and have lower awareness, acceptance, and use of evidence-based cessation methods, including nicotine replacement therapy (NRT).13,20,32 Many low-income smokers view assistance as unnecessary or ineffective,33,34 or a “last resort” for “desperate” smokers who are heavily addicted and can’t quit on their own.35 Yet low-income smokers tend to have greater nicotine addiction,11 so NRT and other assistance could be especially helpful. Among smokers who use NRT or other cessation services, those living in poverty have higher discontinuation rates than others.11,36 Low interest in and use of cessation assistance among low-income smokers may also reflect a dearth of proven programs designed for them,11,37 and incongruity between some staples of cessation assistance and low-income smokers’ needs.38 For example, many low-income smokers lack flexibility in their work schedules to receive telephone counseling, or lack money or insurance to acquire NRT.39
Multiple reviews5,11,37,38 have concluded that cessation interventions for low-SES smokers should address upstream factors such as living conditions and material needs that are often sources of stress; social and cultural norms that influence smoking and cessation; and support for quitting with access to evidence-based interventions. We tested the effects of two such interventions: social needs navigation to help smokers get help with food, rent and other social needs; and a specialized quitline designed to address unique factors that make cessation challenging for low-income smokers.
Methods
Study design
Using a randomized 2 × 2 factorial design, we assigned low-income smokers from a statewide community-based sample to receive either standard tobacco quitline services or specialized tobacco quitline services, each with or without social needs navigation. Effects on 7-day point prevalence abstinence were assessed at 6-month follow-up. Research design and methodological details are published in a study protocol.40 A CONSORT checklist is provided in Supplementary Table S1. The Human Research Protection Office at Washington University in St. Louis approved all study materials and methods.
Participants
Participants were callers to 211, a helpline commonly used by low-income individuals seeking help with social needs.41, 42, 43 After callers received standard 211 assistance, a random subset was screened by a 211 operator for initial study eligibility. Adults (≥18 years) who lived in Missouri, smoked tobacco daily, were ready to quit in the next 30 days, and willing to be contacted by the research team provided their name and phone number. The research team initiated contact within two business days; those who were pregnant, currently enrolled in a tobacco quitline, not comfortable speaking English, planning to move from Missouri, or having private health insurance that included quitline benefits covering NRT were ineligible. From June 1, 2017 to November 15, 2020, 1944 participants met all inclusion criteria, provided informed consent, enrolled in the study, and completed a baseline telephone interview.
Randomization and masking
After the baseline interview, participants were randomly assigned to a study group using a set of 2000 computer-generated numbers, 500 per group. The allocation sequence was stored separately from the baseline survey and randomly assigned, so interviewers were unaware of study group assignment.
Procedures
Participants were randomly assigned to receive either Standard Quitline or Specialized Quitline services, with or without Social Needs Navigation.
Standard tobacco quitline
This is the “usual care” intervention in the study, against which the other interventions are compared. Tobacco quitlines are recommended by the Community Preventive Services Task Force based on strong evidence that they increase cessation among those interested in quitting.44 The Missouri Tobacco Quitline uses Optum’s Quit For Life® program. Quit For Life® coaches are trained in behavior change science and motivational interviewing, and provide phone counseling and individually tailored plans to help smokers quit. Coaches initiate contact with a smoker, help them set a quit date in the next 30 days, and schedule future counseling sessions. Sessions last 10–15 min, spanning 1–3 months around the quit date. Smokers may contact the quitline outside of scheduled sessions for assistance. Coaches make three attempts to reach a smoker for each scheduled session. When study recruitment began in June 2017, the Missouri Tobacco Quitline provided up to four coaching sessions, access to online and texting programs supporting cessation counseling, a printed self-help Quit Guide, and 2 weeks of nicotine replacement therapy (gum or patches, hereafter NRT) to most smokers (excluding those with contraindications or Medicaid coverage providing NRT benefits available through a doctor).
Specialized tobacco quitline
Together with Optum, we adapted the standard quitline to address unique cessation barriers experienced by low-income smokers. Adaptations involved training and personnel, content and delivery, and implementation protocol. A subset of coaches trained to participate in research and interested in helping low-income smokers quit was selected and trained to understand the social context of smoking in low-income individuals. Training focused on life stressors, unmet social needs, social norms around smoking, lack of social support for quitting, and resistance to using NRT. Coaches learned to ask about these challenges during cessation counseling, and modify their approach accordingly. Because many low-SES individuals value lived experience and problem solving as expertise,45 coaches were encouraged to share how long they’ve been helping smokers quit, and whether they were former smokers.
Coaches adapted content and delivery of cessation counseling in multiple ways. As examples, to counter low knowledge about NRT, they explained what it is, how it works, that it improves success quitting, makes quitting easier, and encouraged them to try it. Common cessation tips that could be inappropriate for smokers of limited financial means (e.g., “buy straws to chew on”) or those living in small crowded spaces (e.g., “find a quiet place in your house”), were replaced with more suitable tips (e.g., “doodle or draw,” “brush your teeth”). Whenever possible, quit coaches linked participants’ experience dealing with social needs to their quitting goals (e.g., “money saved by not buying cigarettes can help pay the rent”), and emphasized it as a personal strength that could help with quitting (“if you can deal with your landlord, you are strong enough to quit smoking”).
Coaches were trained to use open-ended questions to elicit each smoker’s “story,” express empathy for their life challenges, and use concrete and plain language. Commonly used cessation jargon (e.g., “triggers,” “urge management”) and abbreviations (e.g., “NRT”) were replaced with alternatives from a plain language glossary developed for the project. The 50-page Quit Guide mailed to smokers in the Standard Quitline group was replaced by a 13-page version with more graphics, written at 5th grade reading level (vs. 7th in the 50-page version), and addressed cessation barriers for low-income smokers (e.g., cost of NRT).
Delivery protocols for cessation counseling also were adapted. Because low-income individuals change residences and phone numbers more often than others,46 coaches made up to five attempts to reach smokers for each counseling session (vs. three with Standard Quitline), and obtained collateral contact information to reach smokers through family or friends, if needed. Specialized Quitline sessions were allowed to last 25–30 min (vs. 15 with Standard Quitline), assuring adequate time for learning about a smoker’s life situation, building rapport, and providing support.
Social needs navigation
This phone-based intervention aimed to help participants address social needs (e.g., food, rent, utilities, employment, transportation, childcare) causing stress in their lives. Navigators helped participants identify and prioritize social needs, generate solutions, and develop action steps to address the needs. Navigators found local service providers to address specific needs, determined participant eligibility for assistance, made referrals to service providers, coached participants about contacting a service provider, advocated for participants to service providers; arranged for transportation if needed, provided reminders for scheduled appointments, and followed up with participants and service providers to evaluate progress resolving social needs.
The navigator called each participant assigned to this intervention within two weeks of them completing a baseline survey. Those reached and interested could receive navigation for up to three months. Navigation sessions included scheduled follow-up calls and participant-initiated calls, which were encouraged. The number and frequency of navigation sessions was driven by need; participants with complex or multiple needs could receive weekly sessions, while others met less often. There was no limit on number of navigation sessions. Navigation ended when participants no longer requested sessions, stopped responding, or reached the 3-month end date. Navigators made up to 20 attempts to reach participants, leaving voice messages on unanswered calls or sending texts or e-mails if participants preferred. Navigators did not initiate cessation-related discussion; they were blind to which quitline participants were assigned, and if smoking or cessation was mentioned by a participant, referred them to the Missouri Tobacco Quitline.
Outcomes
Research team members interviewed participants by phone at enrollment (baseline) and 3 and 6 months later (follow-up). Non-respondents at 3-month follow-up could still complete a 6-month interview, if reached. Administrative data from Optum captured use of both quitline interventions.
Smoking
The primary study outcome was self-reported 7-day point prevalence abstinence at 6-month follow-up, assessed by asking, “Have you smoked in the past 7 days?” (yes/no). Secondary outcomes included 7-day point prevalence abstinence at 3-month follow-up, 30-day point prevalence abstinence at 3-month follow-up, 24-h quit at 3-month follow-up, 30-day point prevalence abstinence at 6-month follow-up, and 24-h quit at 6-month follow-up. Baseline items used to describe the sample assessed age at smoking initiation, number of cigarettes smoked per day, time from waking to first cigarette, living or working with other smokers (the latter asked only among employed participants), ever trying to quit smoking, time since most recent quit attempt (recoded: ≤12 months/more), and ever using quit aids: nicotine patches, gum, lozenges, nasal spray, inhalers, or prescription medicines like “Chantix” or “Zyban, bupropion or Wellbutrin” (recoded: any/none). Responses to cigarettes per day and time to first cigarette are combined into the Heaviness of Smoking Index (HSI; range: 0–6).47
Use of interventions
Optum tracked each participant’s use of Standard or Specialized Quitline services: number and duration (in minutes) of sessions completed; whether the participant was sent NRT; and number of call attempts to reach each participant for each session. These data were recoded as completing 0, 1, or 2+ sessions; mean number of sessions completed; mean number of call attempts made for the first coaching session and per coaching session completed; and total minutes of coaching received.
Use of Social Needs Navigation was tracked by the navigator: number of sessions completed and number of call attempts to reach each participant for each session. These data were recoded as: completing 0, 1 or 2+ sessions; mean number of sessions completed; and mean call attempts per session completed.
Biochemical verification
Participants reporting 7-day point prevalence abstinence at 6-month follow-up were offered two options for remote biochemical verification: in-person carbon monoxide breath testing at a community center, or in-home urine cotinine testing. Participants completing either test received a gift card. Testing and procedural details are described elsewhere.48 We recorded whether participants accepted or declined testing, completed testing or did not, and whether the test result confirmed self-reported cessation.
Statistical analysis
Sample size determination
We estimated that 8–14% of smokers would quit by 6-month follow-up based on prior research49 and past cessation rates from Optum clients. We projected that 40% of participants would be lost to follow-up at 6 months based on prior intervention trials among 211 callers. Our sample size calculation assumed that those lost to follow-up would be considered smokers. We established 5% as the smallest meaningful difference in quit rates between study groups. Therefore, we aimed to recruit 2000 smokers (500 per group) to have 80% power to detect a 5% difference between any of the three intervention arms and the control group (Standard Quitline alone) using a two-sided α of 0.05 for a range of quit rates. Final enrollment was 1944.
Follow-up attrition
We compared the composition of study groups by sociodemographic and other variables at baseline and examined whether these variables were associated with attrition at 6-month follow-up using binary logistic regression.
Intervention use and secondary cessation outcomes
We examined differences between the Standard and Specialized Tobacco Quitlines by comparing the mean number of attempts to reach participants for counseling sessions, the mean duration in minutes of sessions, the mean number of sessions completed, and the proportion of participants completing any session, ≥2 sessions, and receiving NRT. For Social Needs Navigation, we describe the mean number of attempts to reach participants for navigation sessions, the mean number of sessions completed, and the proportion of participants completing any session, and ≥2 sessions. We compared intervention use and secondary cessation outcomes across study groups using chi-squared tests for categorical variables and t-tests for continuous variables.
Intervention fidelity
All quitline calls were recorded. Trained coders reviewed a 10% random sample of recordings blind to study condition. Coders classified each recording as being from either the Specialized or Standard Quitline, based on 13 criteria: the quit coach describing their own experience and expertise helping smokers quit; eliciting stories from the quitter; expressing empathy; using plain language; providing context-relevant insights, free or low-cost tips, directive planning, and directive medication advice; using a metaphor to endorse NRT use; troubleshooting medication use; highlighting the importance of next session; acknowledging that the next session could be with a different quit coach; and emphasizing the positive aspects of talking with a different quit coach. We report the proportion of recordings correctly classified; larger proportions indicate greater fidelity.
Because the Social Needs Navigation intervention was provided in-house by the research team, calls were reviewed by investigators in order to provide ongoing, iterative feedback to navigators in bi-weekly meetings.
Analyses of primary outcomes
We used binary logistic regression to compare 7-day point prevalence abstinence at 6-month follow-up between four groups: Standard Quitline alone, Standard Quitline + Social Needs Navigation, Specialized Quitline alone and Specialized Quitline + Social Needs Navigation. Abstinence rates for each study group were compared to the Standard Quitline (i.e., usual care, referent) using three dummy variables. We did not include control variables in the model, as none were significantly different between groups at baseline and there were no differences between study groups on demographic variables at follow-up. Missing data were imputed using multivariate imputation by chained equations to impute 95 complete datasets.50 We fit the regression model on each imputed dataset and pooled the estimates across models to obtain effect sizes for each study group. Details of the imputation are provided in the Supplementary Materials.
We also conducted two sensitivity analyses. First, we limited the analysis to participants who received the intervention to which they were assigned (e.g., completed at least one quitline session and/or social needs navigation call) and used the 95 imputed datasets to estimate intervention effects in this sample (hereafter, “multiple imputation, per protocol”). Second, we created a dataset where all participants who were missing data on the primary outcome (e.g., those lost to follow-up at the 6-month assessment) were assumed to be continued smokers and examined intervention effects under these assumptions (hereafter, “missing imputed as smokers”). For all analyses, we report odds ratios and 95% confidence intervals.
For biochemical verification, we compared the proportion of respondents in each study group that self-reported 7-day point prevalence abstinence at 6-month follow-up and (1) agreed to take a biochemical verification test; (2) completed a biochemical verification test; and (3) had their self-reported abstinence confirmed by biochemical verification test.
Data were managed in SAS version 9.4 (SAS Institute Inc) and analyses were conducted using R version 3.6.1.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
Participants
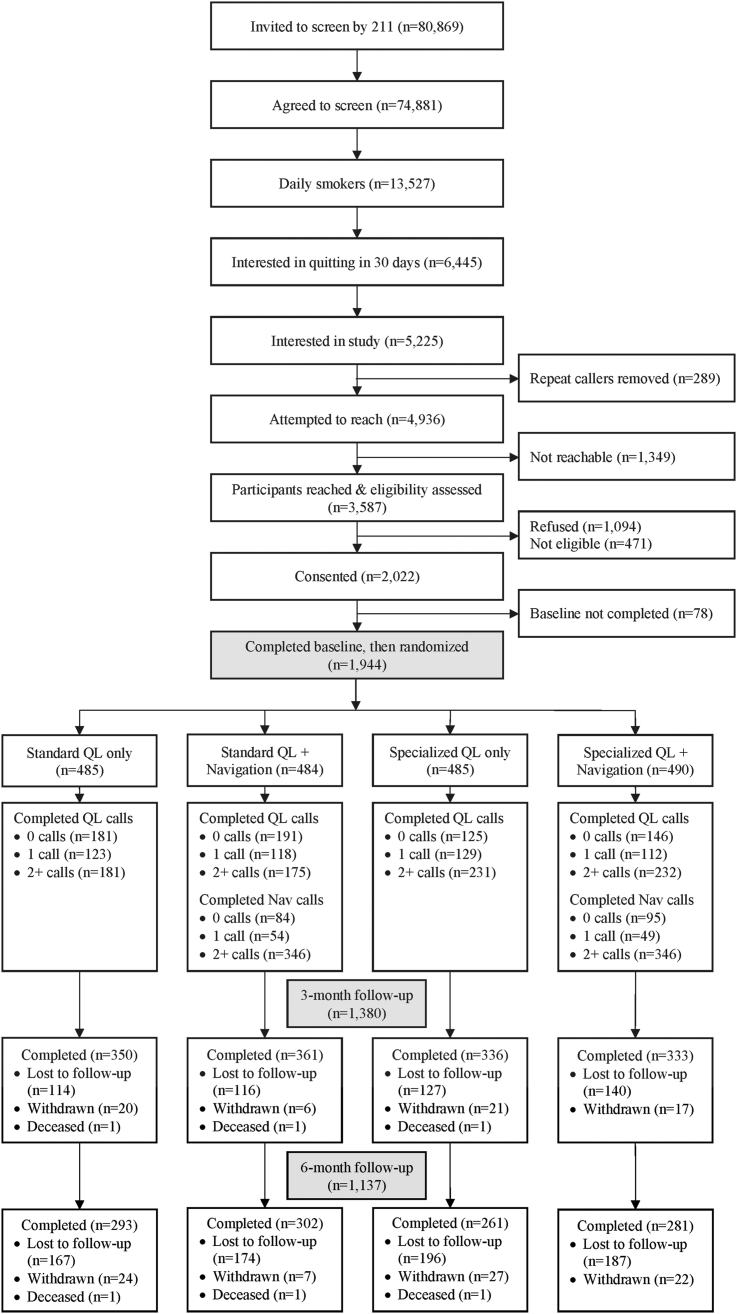
Over a 42-month enrollment period that included the first nine months of the COVID-19 pandemic (June 1, 2017 through November 15, 2020), partners at Missouri 211 invited 80,869 callers to be screened; 93% agreed to screening, 18% of those screened were daily smokers, and 48% were interested quitting in the next 30 days. Of these, 81% (n = 5225) were interested in the study and agreed to share contact information with the study team (CONSORT diagram, Fig. 1). Repeat callers (duplicates) were removed (n = 289). Participants providing verbal informed consent and completing a baseline interview (n = 1944) were randomized to one of the four study groups. Non-enrollment was due to not reaching individuals by phone (n = 1349), refusal to participate (n = 1094), ineligibility (n = 471), and not completing the baseline interview (n = 78).
Fig. 1.
CONSORT diagram of study recruitment, enrollment, randomization, and follow-up.
Over half of participants (957 of 1869; 51%) reported <$10,000 in annual pre-tax household income; 30% (588 of 1937) reported completing less than high school education. Most participants were women (1396 of 1944; 72%) and either Black (1111 of 1921; 58%) or white (666 of 1921; 35%). Average age was 48.4 years old (SD = 12.2). On average, participants smoked 15.6 cigarettes per day (SD = 9.2); 74% (1428 of 1936) allowed smoking inside their home, and 40% (784 of 1940) lived with another smoker. Most (1713 of 1942; 88%) had tried to quit before, and 48% (799 of 1680) reported a quit attempt in the past year (Table 1).
Table 1.
Demographic characteristics, smoking and cessation histories of participants at baseline, by study group.
| Sample characteristics | All participants n = 1944 |
Standard QL only n = 485 |
Standard QL + Navigation n = 484 |
Specialized QL only n = 485 |
Specialized QL + Navigation n = 490 |
|---|---|---|---|---|---|
| Frequency (%)a | |||||
| Demographics | |||||
| Age in years, mean (SD) | 48.4 (12.2) | 48.2 (12.1) | 48.6 (12.2) | 49.0 (12.5) | 47.8 (12.1) |
| Female | 1396 (71.8) | 349 (72.0) | 334 (69.0) | 357 (73.6) | 356 (72.7) |
| Race | |||||
| Black or African-American | 1111 (57.8) | 268 (55.6) | 275 (58.0) | 278 (57.8) | 290 (59.9) |
| White | 666 (34.7) | 179 (37.1) | 166 (35.0) | 164 (34.1) | 157 (32.4) |
| Other | 144 (7.5) | 35 (7.3) | 33 (7.0) | 39 (8.1) | 37 (7.6) |
| Hispanic | 55 (2.9) | 15 (3.1) | 13 (2.7) | 13 (2.7) | 14 (2.9) |
| Annual pre-tax household income | |||||
| <$10,000 | 957 (51.2) | 229 (49.4) | 222 (47.5) | 248 (53.6) | 258 (54.3) |
| $10,000–$19,999 | 572 (30.6) | 144 (31.0) | 155 (33.2) | 140 (30.2) | 133 (28.0) |
| ≥$20,000 | 340 (18.2) | 91 (19.6) | 90 (19.3) | 75 (16.2) | 84 (17.7) |
| Education | |||||
| <High school | 588 (30.4) | 148 (30.6) | 147 (30.4) | 151 (31.4) | 142 (29.0) |
| High school/GED | 580 (29.9) | 148 (30.6) | 128 (26.5) | 154 (32.0) | 150 (30.6) |
| >High school | 769 (39.7) | 187 (38.7) | 208 (43.1) | 176 (36.6) | 198 (40.4) |
| Smoking and cessation history | |||||
| Age in years at first cigarette, mean (SD) | 15.7 (5.6) | 15.9 (6.1) | 15.4 (4.8) | 15.8 (6.3) | 15.7 (5.2) |
| Cigarettes per day, mean (SD) | 15.6 (9.2) | 15.7 (9.4) | 15.3 (8.8) | 16.0 (9.3) | 15.4 (9.3) |
| Live with other smokers | 784 (40.4) | 186 (38.5) | 202 (41.7) | 200 (41.4) | 196 (40.0) |
| Allow smoking inside the home | 1428 (73.8) | 366 (76.3) | 349 (72.4) | 342 (70.7) | 371 (75.7) |
| Self-reported quit attempt, ever | 1713 (88.2) | 421 (86.8) | 434 (89.7) | 427 (88.0) | 431 (88.3) |
| Self-reported quit attempt, last 12 monthsb | 799 (47.6) | 200 (48.7) | 194 (45.5) | 210 (50.0) | 195 (46.1) |
| Past use of any pharmacological quit aidb | 1216 (71.0) | 291 (69.1) | 306 (70.5) | 308 (72.1) | 311 (72.2) |
Except where otherwise noted.
Only asked of those who self-reported a prior quit attempt (n = 1713).
Attrition
Follow-up interviews concluded in August 2021. Overall completion rates at 3-month (1380 of 1944; 71%) and 6-month (1137 of 1944; 58%) follow-up were similar to sample size projections (Fig. 1), although rates were slightly lower during the COVID-19 pandemic (243 of 372; 65% and 194 of 372; 52%, respectively). Participants who enrolled but did not complete the study were more likely to be younger (46 vs. 50 years old, OR = 0.97, 95% CI = 0.97–0.98), white (334 of 797; 42% vs. 332 of 1124; 30%, OR = 1.72, 95% CI = 1.42–2.08), heavier smokers (3.1 vs. 3.0 on HSI, OR = 1.08, 95% CI = 1.00–1.15), who had never tried to quit (115 of 805; 14% vs. 114 of 1137; 10%, OR = 1.50, 95% CI = 1.13–1.97); they also were less likely to have education beyond high school (298 of 806; 37% vs. 471 of 1131; 42%, OR = 0.82, 95% CI = 0.68–0.99). There was differential attrition by study group. Participants assigned to the Specialized Quitline alone were more likely than those assigned to the Standard Quitline alone to be lost to follow-up at 6 months (224 of 485; 46% vs. 192 of 485; 40%, OR = 1.31, 95% CI = 1.02–1.70).
Intervention use and secondary cessation outcomes
Participants assigned to receive the Specialized Quitline alone or Specialized Quitline + Social Needs Navigation completed more cessation counseling sessions than those assigned to receive the Standard Quitline alone or Standard Quitline + Social Needs Navigation, and were more likely to complete at least one session, two or more sessions, and receive NRT from the quitline. Cessation counseling sessions also lasted longer for participants in the Specialized Quitline alone and Specialized Quitline + Social Needs Navigation groups compared to the Standard Quitline alone or Standard Quitline + Social Needs Navigation groups, and total time spent receiving cessation counseling was greater, as well (Table 2).
Table 2.
Use of quitline and social needs navigation interventions and secondary cessation outcomes by study arm (n = 1944).
| Secondary outcomes | Standard QL only n = 485 |
Standard QL + Navigation n = 484 |
Specialized QL only n = 485 |
Specialized QL + Navigation n = 490 |
p-value |
|---|---|---|---|---|---|
| Mean (SD)a | |||||
| Quitline engagement | |||||
| Attempts to reach for coaching session 1 | 2.5 (0.9) | 2.5 (0.9) | 3.4 (1.7) | 3.5 (1.7) | <0.01 |
| Attempts per completed coaching session | 6.6 (4.0) | 6.4 (4.0) | 9.2 (6.4) | 9.0 (6.1) | <0.01 |
| Duration (in minutes) per coaching session | 18.1 (8.4) | 18.2 (8.4) | 20.0 (7.2) | 19.7 (6.3) | <0.01 |
| Duration (in minutes) across all sessions | 21.3 (22.4) | 21.3 (23.0) | 31.5 (27.5) | 29.8 (27.2) | <0.01 |
| Any coaching sessions, n (%) | 304 (62.7) | 293 (60.5) | 360 (74.2) | 344 (70.2) | <0.01 |
| Two or more coaching sessions, n (%) | 181 (37.3) | 175 (36.2) | 231 (47.6) | 232 (47.3) | <0.01 |
| Average number of coaching sessions | 1.3 (1.3) | 1.3 (1.3) | 1.7 (1.4) | 1.6 (1.4) | <0.01 |
| Participant received NRT, n (%) | 212 (43.7) | 207 (42.8) | 262 (54.0) | 242 (49.4) | <0.01 |
| Social needs navigation engagement | |||||
| Attempts per completed navigation session | NA | 3.5 (2.9) | NA | 3.5 (2.7) | 0.86 |
| Any navigation sessions, n (%) | NA | 400 (82.6) | NA | 395 (80.6) | 0.41 |
| Two or more navigation sessions, n (%) | NA | 346 (71.5) | NA | 346 (70.6) | 0.76 |
| Average number of navigation sessions | NA | 3.5 (2.8) | NA | 3.3 (2.7) | 0.15 |
| Secondary cessation outcomes | |||||
| 7-day point prevalence abstinence at 3-months, n (%) | 97 (27.7) | 80 (22.1) | 104 (30.9) | 105 (31.5) | 0.02 |
| 30-day point prevalence abstinence at 3-months, n (%) | 64 (18.3) | 60 (16.6) | 66 (19.6) | 70 (21.0) | 0.50 |
| 24-h quit at 3-month follow-up, n (%) | 278 (79.2) | 290 (80.3) | 270 (80.4) | 269 (80.8) | 0.96 |
| 30-day point prevalence abstinence at 6-months, n (%) | 65 (22.8) | 59 (19.8) | 69 (26.7) | 74 (26.7) | 0.15 |
| 24-h quit at 6-month follow-up, n (%) | 238 (82.6) | 246 (82.6) | 218 (83.8) | 232 (84.4) | 0.92 |
Bold signifies a statistically significant difference (p < 0.05) across the four study groups.
Except where otherwise noted as n (%).
Use of the Social Needs Navigation intervention did not differ among the two groups assigned to receive it. Of those assigned to receive Standard Quitline + Social Needs Navigation, 400 of 484 (83%) completed at least one navigation session and 346 of 484 (71%) completed two or more navigation sessions. Of those assigned to receive Specialized Quitline + Social Needs Navigation, 395 of 490 (81%) completed at least one navigation session and 346 of 490 (71%) completed two or more navigation sessions. The mean number of navigation session completed was 3.5 (SD = 2.8) for those assigned to the Standard Quitline + Social Needs Navigation and 3.3 (SD = 2.7) for those assigned to the Standard Quitline + Social Needs Navigation (Table 2).
The only secondary cessation outcome to differ between study groups was 7-day point prevalence abstinence at 3-month follow-up, which was lowest among those in the Standard Quitline + Navigation group (Table 2).
Intervention fidelity
Fidelity of the specialized quitline intervention was good, but declined over the study period. Overall, 246 of 340 (72%) of the quitline recordings we reviewed were correctly classified as either Specialized or Standard Quitline. However, this indicator of fidelity declined each year of the study, from 38 of 42 (90%) in Year 1 to 69 of 114 (61%) in Year 4.
Abstinence from smoking
Across all study groups, 368 of 1944 (18.9%) of participants reported 7-day point prevalence abstinence at 6-month follow-up. Among participants assigned to Standard Quitline alone (n = 485; 293 followed up), 101 reported 7-day point prevalence abstinence at 6-month follow-up (20.8% of those assigned at baseline; 34.5% of those followed-up; after imputation 38.1%). Abstinence rates for the other groups were: Standard Quitline + Social Needs Navigation (n = 484; 302 followed up), 74 reported abstinence (15.3% of baseline sample; 24.5% of those followed-up; after imputation 30.1%); Specialized Quitline alone (n = 485; 261 followed up), 90 reported abstinence (18.6% of baseline sample; 34.5% of those followed-up; after imputation 38.1%); and Specialized Quitline + Social Needs Navigation (n = 490; 281 followed up), 103 reported abstinence (21.0% of baseline sample; 36.7% of those followed-up; after imputation 39.8%).
The main outcome analysis using imputed datasets compared each study group to the Standard Quitline alone (i.e., control). Participants assigned to the Standard Quitline + Social Needs Navigation had significantly lower odds of quitting (OR = 0.70, 95% CI = 0.50–0.95). The odds of quitting were not significantly different for the Specialized Quitline alone or Specialized Quitline + Social Needs Navigation groups compared to the control group. Results of sensitivity analyses (per protocol and missing imputed as smokers) were similar (Fig. 2), as were analyses of biochemical verification outcomes (Supplementary Table S2).
Fig. 2.
Primary outcome analysis examining odds of reporting smoking cessation at 6-month follow-up by study group.
Discussion
The “control” condition in this study—standard tobacco quitline services—is an evidence-based intervention recommended based on strong evidence from multiple systematic reviews.44 As expected, it worked well: imputed analyses showed that 38.5% assigned to one of the Standard Quitline groups (i.e., Standard Quitline alone and Standard Quitline + Social Needs Navigation) reported 7-day point prevalence abstinence at 6-month follow-up. Contrary to study hypotheses, a specialized version of the quitline designed for low-income smokers was not significantly better. Among participants assigned to Specialized Quitline alone or Specialized Quitline + Social Needs Navigation, 43.3% reported 7-day point prevalence abstinence at 6-month follow-up.
Although the Social Needs Navigation intervention was widely used by participants in both groups assigned to receive it, it did not increase cessation. In fact, in the Standard Quitline + Social Needs Navigation group, it led to significantly lower quit rates than the Standard Quitline alone. One possible explanation is that smokers who are actively working to address unmet social needs don’t have the time and attention needed to simultaneously plan and execute a quit attempt.16,51 However, there was no such detrimental effect of Social Needs Navigation when it was combined with the Specialized Quitline. Quit rates for the Specialized Quitline + Social Needs Navigation group were similar to those in the Specialized Quitline alone and Standard Quitline alone groups. Perhaps some beneficial aspects of the Specialized Quitline intervention offset possible distraction or competition from Social Needs Navigation.
Prior studies evaluating social needs interventions suggest that although navigation helps connect people to services and resolve their needs, its effectiveness for changing health behaviors and improving health outcomes is mixed.52 A better understanding of pathways and mechanisms through which social needs affect health behaviors could improve interventions.53 Future studies might explore sequential interventions where social needs are addressed first, and health improvement interventions follow.
Analyses of intervention use showed that participants assigned to either group receiving the Specialized Quitline engaged with the intervention more than either group assigned to receive the Standard Quitline. They completed more cessation counseling sessions, spent more time per session talking with a quit coach, and were more likely to get NRT from the Quitline. In prior quitline research, completing multiple quitline sessions (as 466 of 975, 47%, did in the two Specialized Quitline groups) and receiving NRT (as 504 of 975, 52%, did in the two Specialized Quitline groups) are both associated with increased odds of cessation.54 Key features of the Specialized Quitline align closely with these intervention use outcomes. For example, we allowed Specialized Quitline coaches to make more call attempts to reach a smoker and talk longer if a smoker was interested. The Specialized Quitline also emphasized overcoming resistance to NRT. These design features may have improved participant engagement (Table 2), even though group differences in engagement did not translate into higher rates of cessation among those receiving the intervention. Not all attributes of the Specialized Quitline were specifically evaluated in follow-up interviews, so we don’t know whether or how other aspects of this approach (e.g., content, delivery) influenced intervention use, or whether they could have contributed to higher attrition rates (e.g., more call attempts being viewed as bothersome).
The research partnerships upon which the study was built provide additional insights and opportunities for tobacco control efforts. Using two simple screening questions administered to a small sample of its total callers, a 211 helpline in one state identified over 13,000 very low-income, racially diverse daily smokers, half of whom wanted to quit. Because 211s exist in every state and collectively receive 12–15 million calls per year,55 they would be an excellent partner for state tobacco quitlines to proactively reach more low-income smokers and connect them to proven cessation assistance. Optum, the quitline service provider in the study, demonstrated the feasibility of delivering the Specialized Quitline intervention with existing staff, systems and infrastructure.
Although the study sample was recruited through a statewide service and included participants from 293 ZIP codes in Missouri, generalizability remains a limitation. Participants are from one state and had to call 211 to be eligible. Thus, in nearly all cases, they were actively seeking assistance with social needs at the time of enrollment. This helps explain some of the defining sample characteristics. For example, compared to 65 studies we recently reviewed examining phone counseling for cessation,37 our sample is among a very small number with such low-income levels. Although remote biochemical verification was largely acceptable to the participants who used it,48 usage was low. This aligns with prior research,56 and suggests biochemical verification may not add appreciably to confidence in self-reported cessation in minimal contact community intervention trials.
Fidelity of the Specialized Quitline intervention declined over time. In post-hoc analyses we found that fidelity declined most in three (out of 13) criteria, which seemed to account for the increasing misclassification. These were: using a metaphor to endorse NRT use, acknowledging that the next quitline session could be with a different quit coach, and emphasizing the positive aspects of talking with a different quit coach. One possible explanation is that as new quitline staff were hired and trained over the course of the study, these elements of the specialized quitline inadvertently received less emphasis. We don’t know whether or how declines in these specific features may have impacted study outcomes.
We recognize that the 58% 6-month follow-up rate may seem low to some. However, this was a community-based field trial conducted with an extremely low-income sample that was selected because they were actively seeking help with social needs such as rent and utility payment assistance. Such populations are transient and can have high rates of turnover in phone service. Also, the final year of data collection for the study took place in the midst of a global pandemic during which recruitment and response rates dropped significantly in telephone survey research nationally in the U.S.57 and in our study. Despite these considerable obstacles, the retention rate was similar to comparable studies from our team.58
Study findings have implications for population-level cessation services such as tobacco quitlines, and their ability to reach, engage and help low-income smokers quit. Proactive screening for smoking through social needs helplines is not currently standard practice for quitlines, but in this study helped identified thousands of low-income smokers interested in quitting. Adaptations to make quitline services more responsive to the unique needs of low-income smokers increased use of telephone cessation counseling and receipt of NRT. Even though greater intervention use did not translate into higher cessation rates at 6-month follow-up, it may have longer-term benefits not tracked in this study, such as higher rates of re-engagement in cessation efforts in the future.59 Although having unmet social needs is associated with higher rates of smoking in low-income adults,60 supplementing standard quitline services with a social needs intervention resulted in lower cessation rates and is therefore not recommended. We conclude that specialized quitline services for low-income smokers confer modest benefits related to increased engagement with a cessation intervention, but do not lead to higher cessation rates within six months. Helping low-income smokers address unmet social needs appears to be detrimental to simultaneous cessation efforts.
Contributors
MK is PI of the study. He collaborated with Co-PI AM and RG, CC, TT, CR, and DS on developing the study design, interventions, assessments, and other aspects of the research. He collaborated with RG to draft the manuscript, collect and integrate feedback from all authors, and submit the final version of the manuscript. RG conducted statistical analyses and created data tables under the supervision of QF, and worked with IJ to manage and clean all study data. RG, IJ, QF, and AM accessed and verified the underlying data reported in the manuscript. At the direction of PIs, LG, TB, CR, and JW coordinated community partnerships with 211 and MDHSS, developed and implemented all study protocols, including recruitment, enrollment and data collection, and managed the efforts of interviewers and research assistants. KC and VH coordinated quitline involvement in the study, including integrating the baseline survey and quitline enrollment into a single assessment. RP and KE coordinated involvement of 211 helplines in the study. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. All authors read and contributed to writing this paper and reviewed and approved the final version.
Data sharing statement
Because study data are confidential, they are not publicly available. De-identified data or aggregate may be made available in response to reasonable requests to the corresponding author (mkreuter@wustl.edu). The study protocol is available at https://doi.org/10.1016/j.cct.2019.03.009.
Declaration of interests
KC declares that she is employed by OptumHealth, received grant funding from NIDA, NCI, and the Cancer Prevention Research Institute of Texas, and has no other competing interests. RP and KE declare that they are employed by United Way and have no other competing interests. VH declares that she is employed by the Missouri Department of Health and Senior Services (MDHSS) and has no other competing interests. MK, RG, CC, TT, CR, DS, IJ, JW, TB, LG, and AM declare that parts of their salary were supported by a research grant from the National Cancer Institute (R01CA201429). All other authors declare no competing interests.
Acknowledgements
The study was supported by a research grant from the National Cancer Institute (R01CA201429). The content of the paper is the sole responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank all study participants for their time and effort. We thank 211 of Missouri and Illinois for their support and recruitment efforts, Optum quitline team members who have contributed to the final study design and implementation (Terry Bush, Alula Torres, Erica Salmon, Ryan Hedrix, Michael Kaplan), and Washington University Health Communication Research Laboratory Call Center Team and others who contributed to the conduct of the study (Audrey Smith, Jennifer Staten, Balaji Golla, Timothy Poor, Eileen Michael, Merriah Croston, Alina Luke, Cindy Charles, Courtney Guntly).
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lana.2023.100529.
Appendix A. Supplementary data
References
- 1.Drope J., Liber A., Cahn Z., et al. Who's still smoking? Disparities in adult cigarette smoking prevalence in the United States. CA Cancer J Clin. 2018;68:106–115. doi: 10.3322/caac.21444. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services . U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2014. The health consequences of smoking: 50 years of progress. A report of the surgeon general.https://www.ncbi.nlm.nih.gov/books/NBK179276/pdf/Bookshelf_NBK179276.pdf [Google Scholar]
- 3.Zhuang Y., Gamst A., Cummins S., Wolfson T., Zhu S. Comparison of smoking cessation between education groups: findings from two US national surveys over two decades. Am J Public Health. 2015;105(2):373–379. doi: 10.2105/AJPH.2014.302222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reid J., Hammond D., Boudreau C., Fong G.T., Siahpush M., ITC Collaboration Socioeconomic disparities in quit intentions, quit attempts, and smoking abstinence among smokers in four western countries: findings from the International Tobacco Control Four Country Survey. Nicotine Tob Res. 2010;12:S20–S33. doi: 10.1093/ntr/ntq051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Twyman L., Bonevski N., Paul C., Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2014-006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jahnel T., Ferguson S.G., Shiffman S., Schüz B. Daily stress as link between disadvantage and smoking: an ecological momentary assessment study. BMC Public Health. 2019;19(1):1284. doi: 10.1186/s12889-019-7631-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKee S.A., Sinha R., Weinberger A.H., et al. Stress decreases the ability to resist smoking and potentiates smoking intensity and reward. J Psychopharmacol. 2011;25(4):490–502. doi: 10.1177/0269881110376694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Childs E., De Wit H. Effects of acute psychosocial stress on cigarette craving and smoking. Nicotine Tob Res. 2010;12(4):449–453. doi: 10.1093/ntr/ntp214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Martinez S.A., Beebe L.A., Thompson D.M., Wagener T.L., Terrell D.R., Campbell J.E. A structural equation modeling approach to understanding pathways that connect socioeconomic status and smoking. PLoS One. 2018;13(2) doi: 10.1371/journal.pone.0192451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parnia A., Siddiqi A. Socioeconomic disparities in smoking are partially explained by chronic financial stress: marginal structural model of older US adults. J Epidemiol Community Health. 2020;74(3):248–254. doi: 10.1136/jech-2019-213357. [DOI] [PubMed] [Google Scholar]
- 11.Hiscock R., Bauld L., Amos A., Fidler J., Munafó M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. 2012;1248(1):107–123. doi: 10.1111/j.1749-6632.2011.06202.x. [DOI] [PubMed] [Google Scholar]
- 12.Rogers E., Palacios J., Vargas E., et al. Financial hardship, motivation to quit and post-quit spending plans among low-income smokers enrolled in a smoking cessation trial. Subst Abuse. 2019;13 doi: 10.1177/1178221819878765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siahpush M., McNeill A., Borland R., Fong G. Socioeconomic variations in nicotine dependence, self efficacy, and intention to quit across four countries: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Supplement III):iii71–iii75. doi: 10.1136/tc.2004.008763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kerner J.F., Dusenbury L., Mandelblatt J.S. Poverty and cultural diversity: challenges for health promotion among the medically underserved. Annu Rev Public Health. 1993;14:355–377. doi: 10.1146/annurev.pu.14.050193.002035. [DOI] [PubMed] [Google Scholar]
- 15.Chisholm J., Burbank V. Evolution and inequality. Int J Epidemiol. 2001;30(2):206–211. doi: 10.1093/ije/30.2.206. [DOI] [PubMed] [Google Scholar]
- 16.Mullainathan S., Shafir E. Times Books; New York: 2013. Scarcity: why having too little means so much. [Google Scholar]
- 17.Senn T., Walsh J., Carey M. The mediating roles of perceived stress and health behaviors in the relation between objective, subjective, and neighborhood socioeconomic status and perceived health. Ann Behav Med. 2014;48:215–224. doi: 10.1007/s12160-014-9591-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vangeli E., West R. Sociodemographic differences in triggers to quit smoking: findings from a national survey. Tob Control. 2008;17(6):410–415. doi: 10.1136/tc.2008.025650. [DOI] [PubMed] [Google Scholar]
- 19.Pisinger C., Aadahl M., Toft U., Jørgensen T. Motives to quit smoking and reasons to relapse differ by socioeconomic status. Prev Med. 2011;52(1):48–52. doi: 10.1016/j.ypmed.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 20.Honjo K., Tsutsumi A., Kawachi I., Kawakami N. What accounts for the relationship between social class and smoking cessation? Results of a path analysis. Soc Sci Med. 2006;62(2):317–328. doi: 10.1016/j.socscimed.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 21.Burgess D., van Ryn M., Noorbaloochi S., et al. Smoking cessation among African American and white smokers in the Veterans Affairs health care system. Am J Public Health. 2014;104(S4):S580–S587. doi: 10.2105/AJPH.2014.302023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hitchman S.C., Fong G.T., Zanna M.P., Thrasher J.F., Chung-Hall J., Siahpush M. Socioeconomic status and smokers’ number of smoking friends: findings from the International Tobacco Control (ITC) Four Country Survey. Drug Alcohol Depend. 2014;143:158–166. doi: 10.1016/j.drugalcdep.2014.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kegler M., Haardorfer R., Bundy L., et al. Do partial home smoking bans signal progress toward a smoke-free home? Health Educ Res. 2016;31(1):24–35. doi: 10.1093/her/cyv066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bundy L., Haardoerfer R., Kegler M., et al. Disseminating a smoke-free homes program to low socioeconomic status households in the United States through 2-1-1: results of a national impact evaluation. Nicotine Tob Res. 2020;22(4):498–505. doi: 10.1093/ntr/nty256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blok D.J., de Vlas S.J., van Empelen P., van Lenthe F.J. The role of smoking in social networks on smoking cessation and relapse among adults: a longitudinal study. Prev Med. 2017;99:105–110. doi: 10.1016/j.ypmed.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 26.Brown-Johnson C., England L., Glantz S., Ling P. Tobacco industry marketing to low socioeconomic status women in the USA. Tob Control. 2014;23(e2):e139–e146. doi: 10.1136/tobaccocontrol-2013-051224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cantrell J., Anesetti-Rothermel A., Pearson J., Xiao H., Vallone D., Kirchner T. The impact of the tobacco retail outlet environment on adult cessation and differences by neighborhood poverty. Addiction. 2015;110(1):152–161. doi: 10.1111/add.12718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention Current cigarette smoking among adults-United States, 2005-2013. MMWR Morb Mortal Wkly Rep. 2014;63(47):1108–1112. [PMC free article] [PubMed] [Google Scholar]
- 29.Galea S., Nandi A., Vlahov D. The social epidemiology of substance use. Epidemiol Rev. 2004;26(1):36–52. doi: 10.1093/epirev/mxh007. [DOI] [PubMed] [Google Scholar]
- 30.Christakis N.A., Fowler J.H. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tibuakuu M., Okunrintemi V., Jirru E., et al. National trends in cessation counseling, prescription medication use, and associated costs among US adult cigarette smokers. JAMA Netw Open. 2019;2(5) doi: 10.1001/jamanetworkopen.2019.4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carpenter M.J., Ford M.E., Cartmell K., Alberg A.J. Misperceptions of nicotine replacement therapy within racially and ethnically diverse smokers. J Natl Med Assoc. 2011;103(9–10):885–894. doi: 10.1016/s0027-9684(15)30444-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pateman K., Ford P., Fitzgerald L., et al. Stuck in the catch 22: attitudes towards smoking cessation among populations vulnerable to social disadvantage. Addiction. 2016;111(6):1048–1056. doi: 10.1111/add.13253. [DOI] [PubMed] [Google Scholar]
- 34.Roddy E., Antoniak M., Britton J., Molyneux A., Lewis S. Barriers and motivators to gaining access to smoking cessation services amongst deprived smokers–a qualitative study. BMC Health Serv Res. 2006;6(1) doi: 10.1186/1472-6963-6-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Waters E.A., McQueen A., Caburnay C.A., et al. Perceptions of the US National Tobacco Quitline among adolescents and adults: a qualitative study, 2012-2013. Prev Chronic Dis. 2015;12:E131. doi: 10.5888/pcd12.150139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burns E.K., Levinson A.H. Discontinuation of nicotine replacement therapy among smoking-cessation attempters. Am J Prev Med. 2008;34(3):212–215. doi: 10.1016/j.amepre.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 37.Garg R., McQueen A., Evbuoma-Fike E., Kreuter M. Re-examining phone counseling for smoking cessation: does the evidence apply to low-SES smokers? Patient Educ Couns. 2022;105(7):1783–1792. doi: 10.1016/j.pec.2021.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Wijk E.C., Landais L.L., Harting J. Understanding the multitude of barriers that prevent smokers in lower socioeconomic groups from accessing smoking cessation support: a literature review. Prev Med. 2019;123:143–151. doi: 10.1016/j.ypmed.2019.03.029. [DOI] [PubMed] [Google Scholar]
- 39.Garg R., McQueen A., Roberts C., et al. Stress, depression, sleep problems and unmet social needs: baseline characteristics of low-income smokers in a randomized cessation trial. Contemp Clin Trials Commun. 2021;24 doi: 10.1016/j.conctc.2021.100857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McQueen A., Roberts C., Garg R., et al. Specialized tobacco quitline and basic needs navigation interventions to increase cessation among low income smokers: study protocol for a randomized controlled trial. Contemp Clin Trials. 2019;80:40–47. doi: 10.1016/j.cct.2019.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kreuter M.W. Reach, effectiveness, and connections: the case for partnering with 2-1-1 to eliminate health disparities. Am J Prev Med. 2012;43(6S5):S420–S421. doi: 10.1016/j.amepre.2012.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Daily L.S. Health research and surveillance potential to partner with 2-1-1. Am J Prev Med. 2012;43(6S5):S422–S424. doi: 10.1016/j.amepre.2012.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thompson T., Kreuter M.W., Boyum S. Promoting health by addressing basic needs: effect of problem resolution on contacting health referrals. Health Educ Behav. 2016;43(2):201–207. doi: 10.1177/1090198115599396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guide to Community Preventive Services Tobacco use: quitline interventions. https://www.thecommunityguide.org/findings/tobacco-use-quitline-interventions
- 45.Lutrell W. Working-class women's ways of knowing: effects of gender, race, and class. Sociol Educ. 1989;62:33–46. [Google Scholar]
- 46.Garboden P.M., Leventhal T., Newman S. Estimating the effects of residential mobility: a methodological note. J Soc Serv Res. 2017;43(2):246–261. [Google Scholar]
- 47.Heatherton T.F., Kozlowski L.T., Frecker R.C., Rickert W., Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84(7):791–800. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 48.Garg R., McQueen A., Wolff J., et al. Comparing two approaches to remote biochemical verification of self-reported cessation in very low-income smokers. Addict Behav Rep. 2021;13 doi: 10.1016/j.abrep.2021.100343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stead L., Hartmann-Boyce J., Perera R., Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2013;8 doi: 10.1002/14651858.CD002850.pub3. [DOI] [PubMed] [Google Scholar]
- 50.van Buuren S., Groothuis-Oudshoorn K. MICE: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(1):1–67. [Google Scholar]
- 51.Mani A., Mullainathan S., Sharif E., Zhao J. Poverty impedes cognitive function. Science. 2013;341(6149):976–980. doi: 10.1126/science.1238041. [DOI] [PubMed] [Google Scholar]
- 52.Gottlieb L., Wing H., Adler N. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med. 2017;53(5):719–729. doi: 10.1016/j.amepre.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 53.Kreuter M., Thompson T., McQueen A., Garg R. Addressing social needs in health care settings: evidence, challenges, and opportunities for public health. Annu Rev Public Health. 2021;42:329–344. doi: 10.1146/annurev-publhealth-090419-102204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Matkin W., Ordonez-Mena J.M., Hartmann-Boyce J. Telephone counseling for smoking cessation. Cochrane Database Syst Rev. 2019;5(5) doi: 10.1002/14651858.CD002850.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kreuter M., Garg R., Javed I., Golla B., Wolff J., Charles C. 3.5 million social needs requests during COVID-19: what can we learn from 2-1-1? Health Aff Blog. 2020 https://www.healthaffairs.org/do/10.1377/forefront.20200729.432088/full/ [Google Scholar]
- 56.Cha S., Ganz O., Cohn A.M., Ehlke S.J., Graham A.L. Feasibility of biochemical verification in a web-based smoking cessation study. Addict Behav. 2017;73:204–208. doi: 10.1016/j.addbeh.2017.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Krieger N., LeBlanc M., Waterman P.D., Reisner S.L., Testa C., Chen J.T. Decreasing survey response rates in the time of COVID-19: implications for analyses of population health and health inequities. Am J Public Health. 2023;113(6):667–670. doi: 10.2105/AJPH.2023.307267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kreuter M., Garg R., Li L., et al. How do social needs cluster among low-income individuals? Popul Health Manag. 2021;24(3):322–332. doi: 10.1089/pop.2020.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wiseman K.P., Aycock C.A., Mallawaarachchi I., et al. Predictors of re-engagement after relapse in a tobacco quit line intervention: secondary analysis from a randomized clinical trial. Int J Environ Res Public Health. 2023;20(2):1229. doi: 10.3390/ijerph20021229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thompson T., McQueen A., Croston M., et al. Social needs and health-related outcomes among Medicaid beneficiaries. Health Educ Behav. 2019;46(3):436–444. doi: 10.1177/1090198118822724. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.