Abstract
Aim
The aim of this study was to evaluate chest compression rates (CCR) with and without the use of a metronome during treatment of out-of-hospital cardiac arrest (OHCA).
Methods
We performed a retrospective cohort investigation of non-traumatic OHCA cases treated by Seattle Fire Department from January 1, 2013, to December 31, 2019. The exposure was a metronome running during CPR at a rate of 110 beats per minute. The primary outcome was the median CCR for all periods of CPR with a metronome compared to periods without a metronome.
Results
We included 2,132 OHCA cases with 32,776 minutes of CPR data; 15,667 (48%) minutes had no metronome use, and 17,109 (52%) minutes had a metronome used. Without a metronome, the median CCR was 112.8 per minute with an interquartile range of 108.4 – 119.1, and 27% of minutes were above 120 or less than 100. With a metronome, the median CCR was 110.5 per minute with an interquartile range of 110.0–112.0, and less than 4% of minutes were above 120 or less than 100. The compression rate was 109, 110, or 111 in 62% of minutes with a metronome compared to 18% of minutes with no metronome.
Conclusion
The use of a metronome during CPR resulted in increased compliance to a predetermined compression rate. Metronomes are a simple tool that improves achievement of a target compression rate with little variance from that target.
Keywords: Metronome, Cardiopulmonary resuscitation, Chest compression rate, Chest compressions, Out-of-hospital cardiac arrest, Cardiac arrest
Introduction
Effective chest compressions are key to high-performance cardiopulmonary resuscitation (CPR) and are influenced by the rate, fraction, depth, and recoil.[1], [2] Published evidence on compression rate specifically has shown rates below 100 and above 120 to be associated with worse clinical outcomes when compared to rates between 100–120.[3], [4], [5], [6] The latest American Heart Association guidelines reflects this evidence by recommending chest compression delivery at a rate of 100 – 120 compressions per minute.1
The use of audio or visual devices can improve compliance with chest compression rate targets.[7], [8], [9], [10], [11] Devices that provide real-time audio or visual feedback, including prompts, have been evaluated in multiple simulation-based studies, as well as some clinical studies, with consistent improvement in compression rates for both laypersons and medical providers.7 Simulation studies using a simple audio-based metronome only, without other prompts, also improved compression parameters.[8], [9] Beyond simulation studies, the use of a metronome in emergency department settings similarly improved compression rates.[10], [11] However, evidence to support the use of a simple audio metronome to guide compression rate in real-time, out-of-hospital situations is still limited.
The aim of this study was to evaluate CPR compression rates with and without the use of an audio metronome during treatment of out-of-hospital cardiac arrest (OHCA). We hypothesized that the use of a metronome would improve achievement of a target compression rate during treatment of OHCA.
Methods
Study setting, design, and data collection
This study was a retrospective cohort investigation of non-traumatic OHCA cases treated by Seattle Fire Department over seven years from January 1, 2013 to December 31, 2019. The study was approved by the University of Washington Institutional Review Board and followed the STROBE guidelines for an observational study (see STROBE Checklist, Supplemental Fig. 2).
The Seattle Fire Department is the primary responding emergency medical services (EMS) agency in Seattle, Washington and uses a tiered response model of firefighter-EMTs and firefighter-paramedics. Firefighter-EMTs are trained in basic life support (BLS) and use of an automated external defibrillator. From the start of the study period to January 2015, EMTs were trained at least one time a year in OHCA protocols, which included simulation training with a target of 110 chest compressions per minute during CPR. In January 2015, a CTM-40 Tuner and Metronome (DeltaLab, Thousand Oaks, CA), preset to 110 beats per minute, was added to each automated external defibrillator carrying case. EMTs were instructed to turn on the metronome as soon as operationally feasible and leave the metronome running throughout the resuscitation.
All defibrillators used during the study period recorded continuous transthoracic impedance, continuous ECG waveforms, and audio recordings of the case. The audio recordings and defibrillator data were abstracted to create a detailed registry of each OHCA case. The audio recordings were individually reviewed by a trained data abstractor, and the metronome turn on time was noted when it was first audible to the abstractor.
CODESTAT data review software (Version 12.0, Stryker Corporation, Kalamazoo, MI, USA) calculates a chest compression rate (CCR) for each minute of the case using the mean of compression-to-compression intervals for that minute, excluding the lowest and highest quartile intervals (Supplemental Fig. 1). This produces a trimmed mean, which reduces the influence of compression detection errors. In some cases, the software is unable to calculate a compression rate. This occurs if a manual defibrillator was not in “paddles” mode, there were an insufficient number of compressions during the one-minute epoch, or compressions were missed by the software algorithm. The software computes each interval based on when the defibrillator was turned on. The first and last compression periods typically start or end part way through a one-minute epoch, since chest compressions do not align precisely at the minute transition, and chest compression periods are not always precisely two minutes.
Study population, exposure, outcomes, and statistical analysis
All non-traumatic OHCA cases treated by the Seattle Fire Department were eligible for inclusion (Fig. 1). We excluded patients with the following characteristics: no defibrillator data or cases in which the defibrillator recording was missing audio, patients aged less than 18 years old, patients who first developed cardiac arrest after EMS arrival, patients that received advanced life support (ALS) care by providers who were not part of the Seattle Fire Department, or if there was a date/time mismatch between the defibrillators used on the same case.
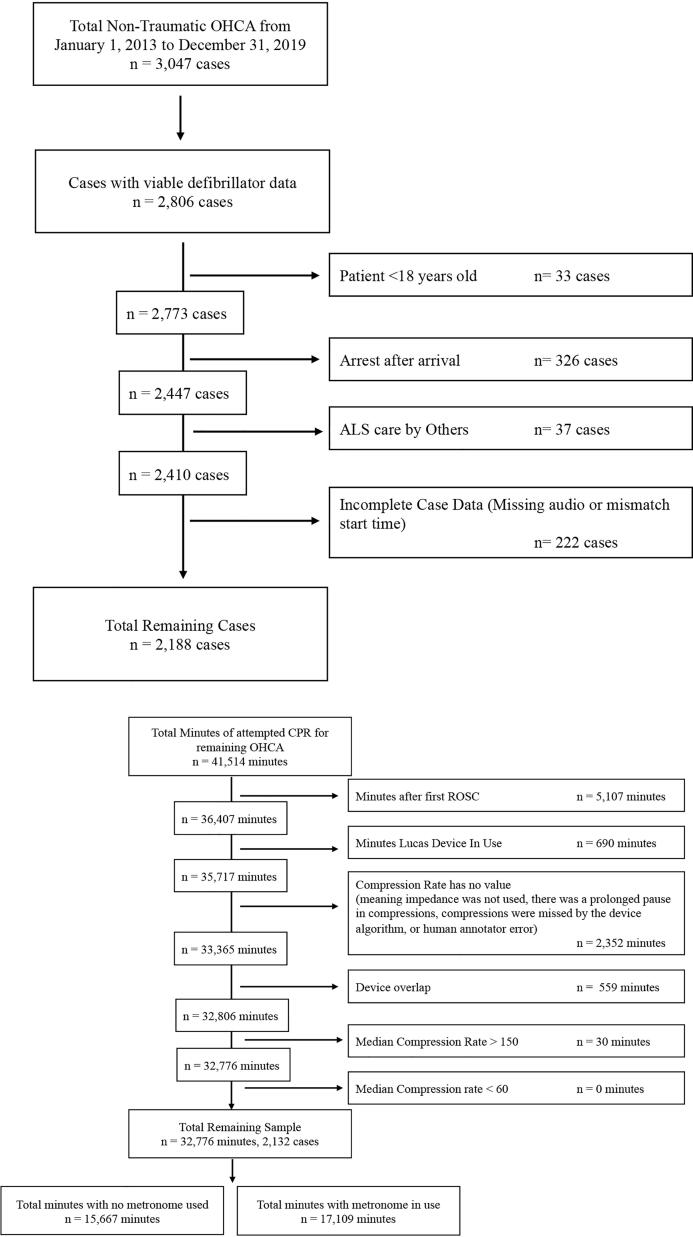
Fig. 1.
1a. Case Exclusions: Number of cases excluded for each exclusion criteria. 1b. Minute Exclusions: Individual minutes were excluded from a case if they meet any of the minute exclusion criteria. Abbreviations: OHCA: out of hospital cardiac arrest, ALS: advanced life support, ROSC: return of spontaneous circulation.
Among the included cases, unique CODESTAT minute epochs were excluded if they occurred after the patient’s first return of spontaneous circulation (ROSC), a LUCAS device was in use, the same minute was reported by more than one defibrillator, or a compression rate was not able to be calculated. Minutes with compression rates above 150 or below 60 were also excluded, as it was unlikely these values represented true observations. In cases where the same minute was reported by more than one defibrillator (cases often used both an automated external defibrillator and a manual defibrillator), the overlapping minutes from the first defibrillator were retained and repeat minutes from the second defibrillator were excluded.
Minutes without a metronome running were designated as “No Metronome”. Minutes when the metronome was running for the entire 60 seconds were designated as “Metronome”. If a minute contained the moment when the metronome was first audible, then that minute was designated as “Metronome” to reduce any potential bias towards a metronome effect.
The exposure in this study was a metronome running during EMS CPR. The primary outcome was the median compression rates for all periods with “Metronome” compared to periods with “No Metronome.” The total amount of minutes above 120 compressions per minute (CPM) and under 100 CPM were also reported for periods with “Metronome” and periods with “No Metronome”.
At the patient level, we compared baseline characteristics in two groups based on whether the metronome was used at any time in the case or not. Categorical variables were compared with the chi-square statistic and the Wilcoxon rank sum test for continuous variables. At the minute level, “No Metronome” minutes were compared to “Metronome” minutes using the Wilcoxon rank sum test. The two categorical variables, “Minutes over 120 CPM” and “Minutes under 100 CPM” were compared using a chi-square statistic. The Kruskal-Wallis test was used to compare compression rates by year. A p-value less than 0.05 was considered to be statistically significant. Skewness and kurtosis tests were used to assess normal distribution. Statistical analysis was performed using Stata version 17 (StataCorp, College Station, TX).
Results
There were 3,047 OHCAs during the study period, of which 2,806 cases had viable defibrillator data. An additional 618 cases were excluded, as shown in Fig. 1a. The resulting 2,188 cases contained 41,514 minutes of CPR. After excluding 8,738 ineligible minutes of CPR (Fig. 1b), 32,776 minutes of CPR remained across 2,132 cases. Of this total, 15,667 (48%) minutes had no metronome use, and 17,109 (52%) minutes had metronome use.
Metronome use increased consistently throughout the study period. During the first year after metronome deployment only 32% of cases used a metronome, but by 2019 metronomes were used in 88% of cases (Supplemental Table 1). The metronome was turned on early in the case; the median interval from the start of EMS CPR to the metronome start was 1.3 minutes for all cases that had a metronome (Table 1). This interval decreased consistently from 3.2 minutes in 2015 to 0.7 minutes in 2019 (Supplemental Table 1).
Table 1.
Out of hospital cardiac arrest patient characteristics.
| All Patients | Patients w/out any Metronome Used |
Patients w/ Metronome Ever Used |
||
|---|---|---|---|---|
| Demographics | Median/n (IQR/%) | Median/n (IQR/%) | Median/n (IQR/%) | p |
| Total patients | 2,132 | 1,043 | 1,089 | |
| Age, years | 63 (50–75) | 63 (50–75) | 63 (50–75) | 0.95 |
| Sex, male | 1,412 (66.3%) | 682 (65.4%) | 730 (67.0%) | 0.45 |
| Clinical Features | ||||
| Presumed Etiology | 0.19 | |||
| Primary Cardiac | 1,673 (78.5%) | 826 (79.2%) | 847 (77.9%) | |
| Primary Respiratory - non toxic | 109 (5.1%) | 50 (4.8%) | 59 (5.4%) | |
| Primary Respiratory - toxic | 208 (9.8%) | 111 (10.6%) | 97 (8.9%) | |
| Medical | 120 (5.6%) | 47 (4.5%) | 73 (6.7%) | |
| Other / Unknown | 22 (1.0%) | 9 (0.9%) | 13 (1.2%) | |
| Arrest Location | 0.043 | |||
| Home/Other Residence | 1,304 (61.2%) | 603 (57.8%) | 701 (64.4%) | |
| Public | 565 (26.5%) | 308 (29.5%) | 257 (23.6%) | |
| Healthcare Facility | 249 (11.7%) | 126 (12.0%) | 123 (11.3%) | |
| Other / Unknown | 14 (0.7%) | 6 (0.6%) | 8 (0.7%) | |
| Bystander Witnessed | 785 (36.8%) | 381 (36.5%) | 404 (37.1%) | 0.13 |
| Bystander CPR | 1,283 (60.2%) | 593 (56.8%) | 690 (63.4%) | <0.0001 |
| Initial Rhythm on EMS Arrival | 0.24 | |||
| VF or VT | 502 (23.6%) | 263 (25.2%) | 239 (21.9%) | |
| PEA | 482 (22.6%) | 235 (22.5%) | 247 (22.7%) | |
| Asystole | 1,052 (49.4%) | 505 (48.4%) | 547 (50.3%) | |
| Non-Shockable | 43 (2.0% | 14 (1.3%) | 29 (2.7%) | |
| Pulses on First Check | 36 (1.7%) | 16 (1.5%) | 20 (1.8%) | |
| Unknown | 17 (0.7%) | 10 (1.0%) | 7 (0.6%) | |
| Case Features | ||||
| Call to Dispatch, minutes | 0.63 (0.47–0.88) | 0.62 (0.47–0.85) | 0.65 (0.48–0.92) | 0.0006 |
| Call to Start EMS Compressions, minutes | 6.7 (5.6–8.1) | 6.5 (5.4–7.9) | 6.8 (5.7–8.2) | 0.0006 |
| Length of Resuscitation, minutes | 30.3 (22.2–39.4) | 30.0 (20.8–38.9) | 30.5 (23.4–39.7) | 0.012 |
| EMS Compressions to Metronome Start, minutes | 1.3 (0.6–3.2) |
There were significant differences observed between groups for Arrest Location, Bystander CPR, Call to Dispatch, Call to Start EMS Compressions, and Length of Resuscitation. There were no significant differences observed between other groups.
Data was missing from 10 cases for Age; 21 cases from Call to Start EMS Compressions; 32 cases from Length of Resuscitation, minutes; and 7 cases from EMS Compressions to Metronome Start.
Abbreviations: CPR: cardiopulmonary resuscitation, EMS: emergency medical services, VF/VT: ventricular fibrillation/ventricular tachycardia, PEA: pulseless electrical activity.
The median age of included patients was 63 years with an interquartile range of 50–75 years. Overall, 78.5% of patients had a presumed cardiac etiology, and 23.6% had an initially shockable cardiac arrest rhythm. The median length of resuscitation, defined by the time from the start of EMS CPR to ceasing efforts or arrival to hospital, was 30.0 minutes for cases without a metronome, and 30.5 minutes for cases with a metronome (Table 1).
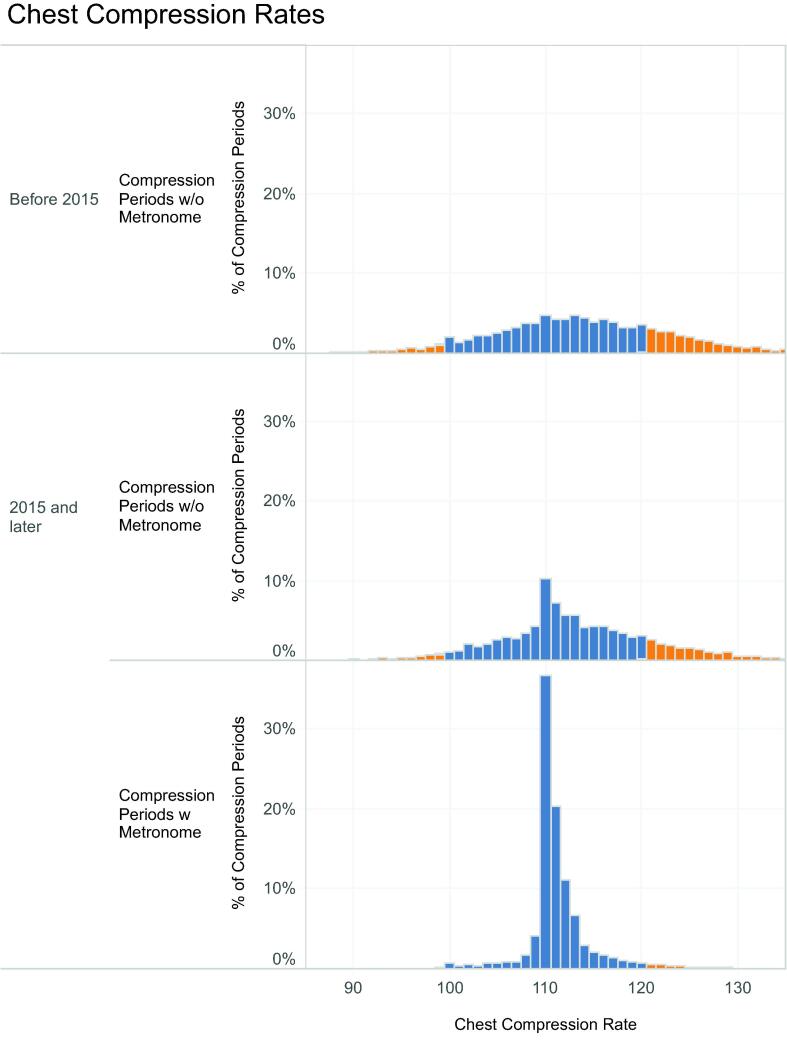
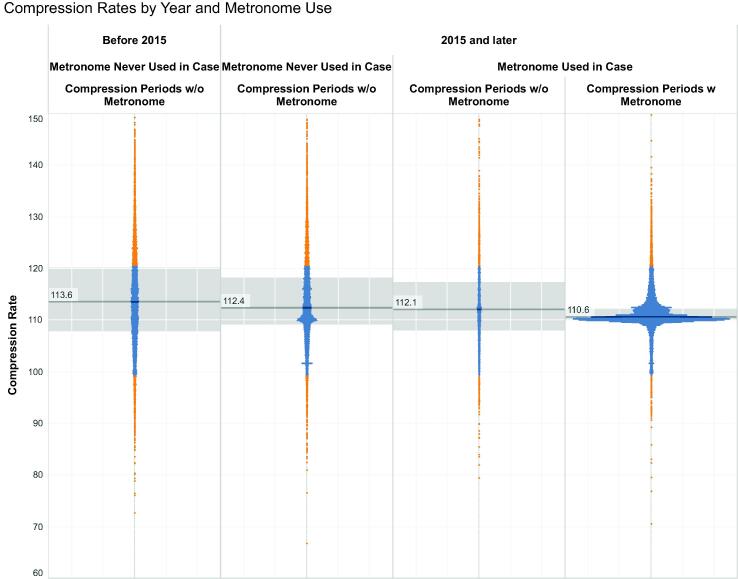
The observed chest compression rates are detailed in Table 2. Without a metronome, the median compression rate was 112.8, with a larger interquartile range of 108.4 – 119.1. The median compression rate for all minutes with a metronome was 110.5, with a much smaller interquartile range of 110.0 – 112.0. The compression rate was 109, 110, or 111 in 62% of all metronome minutes compared to 18% of no metronome minutes (Fig. 2). Of all minutes without a metronome, 21.8% were at a compression rate above 120 CPM and 5.4% were below 100. Of all minutes with a metronome, only 3% were above 120 CPM and 0.7% were below 100 (Table 2, Fig. 2, Fig. 3).
Table 2.
Overall Compression Rates.
| No Metronome | Metronome | p | |
|---|---|---|---|
| Total minutes | 15,667 | 17,109 | |
| Median Compression Rate | 112.8 | 110.5 | <0.0001 |
| IQR | 108.4–119.1 | 110.0–112.0 | |
| Minutes over 120 CPM | 3,413 | 513 | <0.0001 |
| Minutes over 120 CPM, % | 21.8% | 3.0% | |
| Minutes under 100 CPM | 846 | 128 | <0.0001 |
| Minutes under 100 CPM, % | 5.4% | 0.7% |
Overall median compression rates for all minutes without a metronome compared to minutes with a metronome.
Abbreviations: CPM: compressions per minute.
Fig. 2.
Overall Chest Compression Rates. Fig. 2 is a histogram showing the frequency of compression rates for periods without a metronome prior to 2015, periods without a metronome after 2015, and periods with a metronome. This illustrates a significant concentration around 110 compressions per minute with a metronome, while there is a much wider distribution for periods without a metronome.
Fig. 3.
Compression Rates by Year and Metronome Use. Fig. 3 is comprised of a single point (for every period of CPR data) at the observed compression rate for that period. The compression periods are grouped by those prior to 2015 (periods without a metronome) and after 2015. After 2015, the compression periods are displayed from cases without a metronome ever used in the case, periods without a metronome running (but with a metronome used later in the case) and periods with a metronome. There is a small concentration around 110 for minutes after 2015 without a metronome used in the case. This could represent a metronome running that was missed during data abstraction or represent evidence that providers have gotten better at targeting 110 compressions per minute even without a metronome, both potential limitations of the study.
Discussion
In this retrospective analysis of seven years of OHCA cases, we observed that EMS teams could reliably use a simple audio metronome. Metronome use was associated with delivered chest compression rates much closer to the target rate of 110 compressions per minute. We observed that during minutes of metronome use variance from that target rate was much lower, and less than 4% of minutes were outside of the 100–120 chest compressions per minute guideline window.
The accuracy and reduced variance observed with use of the metronome suggests it is a significant tool for improvement of chest compression delivery. Avoiding compression rates above 120 may be clinically significant, as excessively high compression rates are thought to decrease CPR diastole time and reduce cardiac output and coronary blood flow.12 Chest compression rate can influence compression depth, with faster compression rates reducing the delivery of optimal compression depth.[13], [14]
The optimal compression rate during CPR is an ongoing area of research.5 The use of a metronome to reliably achieve a precise compression rate is an adaptable way to evaluate the impact of different chest compression rates on patient-oriented survival outcomes.
In addition to the effectiveness of a metronome in guiding compression rates, its ease of use and low cost make implementation straightforward. The metronomes used in this study were purchased for about $25 each and are easily set to the desired rate. Metronome use was rapidly adopted and increased consistently over the study period.
Metronome use has very few drawbacks or negative effects. One previous simulation study observed a decreased compression depth during metronome use, suggesting that the metronome shifted focus from depth to rate.15 A follow up study proposed that a higher compression rate of 120 reduced any negative effect on compression depth observed at lower compression rates of 100–110.[15], [16] These studies were performed with individuals relatively less experienced in CPR than many EMTs and paramedics.
The use of a metronome may have contributed to improved compression rates even during intervals without a metronome (Fig. 2, Fig. 3). This potential learning effect from the use of a metronome was also described in a study using metronomes to train laypersons in CPR; individuals trained with a metronome achieved better compression rates in follow-up sessions even when no metronome was used.17 This learning effect from the metronome is both a benefit, as it provides continuous training for performing CPR at guideline rates; but it is also a potential limitation of the study. As compression rates improved since implementation of the metronome, the true effect of the intervention could be underestimated.
This study has limitations. Our study was performed with EMTs and paramedics trained and practiced in high performance CPR.18 From this training, they may have achieved target compression rates at a higher frequency than less practiced providers even without a metronome, potentially limiting the generalizability of the study. Additionally, although minutes with a LUCAS device in use were excluded, there were unexpected repeat observations of compression rates of 101.75. This is most likely explained by minutes that a LUCAS was in use, representing an incorrect recording of the LUCAS start times. The metronome turn-on time was recorded only once trained data abstractors could hear it on the defibrillator recording, therefore it is possible it was audible on scene, but not during data abstraction leading to an incorrect categorization of those CPR minutes. This effect may be visible in Fig. 3 in the 2015 and later cohort, with a small increase around 110 CPM within minutes marked as not using a metronome. This study did not include any analysis of outcomes or survival associated with metronome use. Additionally, the study did not evaluate any other markers of quality of CPR besides the compression rate. Using a metronome to achieve a target rate could influence other aspects of quality CPR like the compression depth. Ultimately, these limitations should be considered in the context of the study’s strengths of a relatively large sample size, detailed reporting of events, and granular timing of resuscitative care.
In conclusion, the audio metronome is an easily deployed, adaptable, and effective tool that helps achieve a target chest compression rate during CPR with little variance from that target.
CRediT authorship contribution statement
Jacob Kennedy: Conceptualization, Methodology, Formal analysis, Data curation, Writing – original draft, Writing – review & editing, Visualization. Kimberly Machado: Conceptualization, Methodology, Data curation, Writing – review & editing. Charles Maynard: Methodology, Formal analysis, Data curation, Writing – review & editing. Robert G. Walker: Software, Methodology, Writing – review & editing. Michael R. Sayre: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Visualization, Supervision. Catherine R. Counts: Conceptualization, Methodology, Formal analysis, Writing – review & editing, Visualization, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
We want to acknowledge the dedicated efforts of the telecommunicators and EMS professionals of the Seattle Fire Department and their continuous efforts to improve the care delivered to the community they serve.
Funding Sources/Disclosures
This study received no funding.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100417.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Merchant R.M., Topjian A.A., Panchal A.R., et al. Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S337–S357. doi: 10.1161/CIR.0000000000000918. [DOI] [PubMed] [Google Scholar]
- 2.Meaney P.A., Bobrow B.J., Mancini M.E., et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association [published correction appears in Circulation. 2013 Aug 20;128(8):e120] [published correction appears in Circulation. 2013 Nov 12;128(20):e408] Circulation. 2013;128:417–435. doi: 10.1161/CIR.0b013e31829d8654. [DOI] [PubMed] [Google Scholar]
- 3.Perkins G.D., Travers A.H., Berg R.A., et al. Part 3: Adult basic life support and automated external defibrillation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation. 2015;95:e43–e69. doi: 10.1016/j.resuscitation.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 4.Idris A.H., Guffey D., Pepe P.E., et al. Chest compression rates and survival following out-of-hospital cardiac arrest. Crit Care Med. 2015;43:840–848. doi: 10.1097/CCM.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 5.Idris A.H., Guffey D., Aufderheide T.P., et al. Relationship between chest compression rates and outcomes from cardiac arrest. Circulation. 2012;125:3004–3012. doi: 10.1161/CIRCULATIONAHA.111.059535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abella B.S., Sandbo N., Vassilatos P., et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation. 2005;111:428–434. doi: 10.1161/01.CIR.0000153811.84257.59. [DOI] [PubMed] [Google Scholar]
- 7.Kirkbright S., Finn J., Tohira H., et al. Audiovisual feedback device use by health care professionals during CPR: a systematic review and meta-analysis of randomised and non-randomised trials. Resuscitation. 2014;85:460–471. doi: 10.1016/j.resuscitation.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Çalışkan D., Bildik F., Aslaner M.A., Kılıçaslan İ., Keleş A., Demircan A. Effects of metronome use on cardiopulmonary resuscitation quality. Turk J Emerg Med. 2021;21:51–55. doi: 10.4103/2452-2473.309137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kern K.B., Stickney R.E., Gallison L., et al. Metronome improves compression and ventilation rates during CPR on a manikin in a randomized trial. Resuscitation. 2010;81:206–210. doi: 10.1016/j.resuscitation.2009.10.015. [DOI] [PubMed] [Google Scholar]
- 10.Rainey K., Birkhoff S. Turn the Beat On: An Evidenced-Based Practice Journey Implementing Metronome Use in Emergency Department Cardiac Arrest. Worldviews Evid Based Nurs. 2021;18:68–70. doi: 10.1111/wvn.12486. [DOI] [PubMed] [Google Scholar]
- 11.Khorasani-Zadeh A., Krowl L.E., Chowdhry A.K., et al. Usefulness of a metronome to improve quality of chest compressions during cardiopulmonary resuscitation. Proc (Bayl Univ Med Cent) 2020;34:54–55. doi: 10.1080/08998280.2020.1805840. [Published 2020 Aug 24] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris A.W., Kudenchuk P.J. Cardiopulmonary resuscitation: the science behind the hands. Heart. 2018;104:1056–1061. doi: 10.1136/heartjnl-2017-312696. [DOI] [PubMed] [Google Scholar]
- 13.Agostinucci J.M., Weisslinger L., Marzouk N., et al. Relation between chest compression rate and depth: the ENFONCE Study. Eur J Emerg Med. 2021;28:352–354. doi: 10.1097/MEJ.0000000000000802. [DOI] [PubMed] [Google Scholar]
- 14.Monsieurs K.G., De Regge M., Vansteelandt K., et al. Excessive chest compression rate is associated with insufficient compression depth in prehospital cardiac arrest. Resuscitation. 2012;83:1319–1323. doi: 10.1016/j.resuscitation.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 15.Oh J.H., Lee S.J., Kim S.E., Lee K.J., Choe J.W., Kim C.W. Effects of audio tone guidance on performance of CPR in simulated cardiac arrest with an advanced airway [published correction appears in Resuscitation. 2009 Mar;80(3):390] Resuscitation. 2008;79:273–277. doi: 10.1016/j.resuscitation.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 16.Chung T.N., Kim S.W., You J.S., Cho Y.S., Chung S.P., Park I. A higher chest compression rate may be necessary for metronome-guided cardiopulmonary resuscitation. Am J Emerg Med. 2012;30:226–230. doi: 10.1016/j.ajem.2010.11.026. [DOI] [PubMed] [Google Scholar]
- 17.Hafner J.W., Jou A.C., Wang H., Bleess B.B., Tham S.K. Death before disco: the effectiveness of a musical metronome in layperson cardiopulmonary resuscitation training. J Emerg Med. 2015;48:43–52. doi: 10.1016/j.jemermed.2014.07.048. [DOI] [PubMed] [Google Scholar]
- 18.Hanisch J.R., Counts C.R., Latimer A.J., Rea T.D., Yin L., Sayre M.R. Causes of Chest Compression Interruptions During Out-of-Hospital Cardiac Arrest Resuscitation. J Am Heart Assoc. 2020;9:e015599. doi: 10.1161/JAHA.119.015599. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.