Dear Editor,
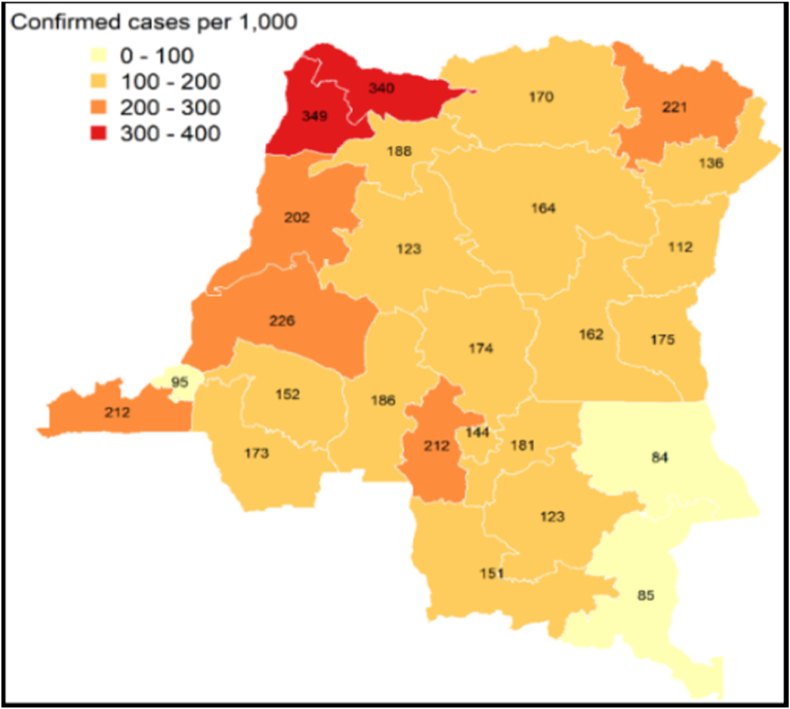
In DR Congo, a country where the health system is paralyzed by numerous potentially epidemic diseases, its healthcare system is confronted with malaria which causes a very high number of cases of deaths among people vulnerable to malaria [1]. This high frequency of deaths is caused by the presence of the Plasmodium falciparum parasite throughout the national territory of the country and is the cause of serious forms and complications of malaria in DR Congo [2] (see Fig. 1).
Fig. 1.
Distribution of malaria cases by provinces in DR Congo [5].
Source: Programme National de lutte contre le Paludisme. Plan Strategique National de lutte contre le Paludisme 2020–2023.
On the road to malaria elimination, the DR Congo's healthcare system which is poorly equipped with healthcare equipment, is unable to provide effective care to the malaria vulnerable people. While progress in the fight against malaria depends on the strength of the healthcare system, the level of investment in malaria elimination strategies and other factors, such as environmental determinants as well as the social, demographic, and economic realities of the country [3].
In DR Congo, about 30% of its population lives within 5 km of healthcare facilities while 70% do not have access to health care due to geographic and economic barriers in the country [4]. This shows a concentration of healthcare facilities in high economic income sites compared to low-income areas, resulting in a failure to fill these gaps in the provision of malaria control services. To put an end to the high morbidity and mortality rate of Malaria in DR Congo, the Congolese government should seek public health partners to strengthen its healthcare facilities and equipment in order to provide access to eliminate the associated risk factors of malaria, strengthening malaria healthcare, especially the primary healthcare centers, for the entire population and ensuring the health security of its population, as well as educating the Congolese population about the complications of malaria. It is also important for the Congolese government to also stimulate investment in the development and deployment of a new generation of malaria control tools and equipment to meet the global malaria targets for 2030. Several new malaria vector control tools and technologies have been submitted to the World Health Organization. If these tools are found to be effective in combating the disease [5], the Congolese government and its Ministry of Public Health should make new recommendations to support malaria control reform. As vector control is an essential component of strategies to combat and eliminate malaria, this should be a priority for the Congolese government because it prevents malaria infection and reduces its transmission. The use of insecticide-treated nets, spraying of insecticides, proper drainage system, and cutting down the bushes, against mosquitoes have been known as the main elements in vector control. Measures should be continued to prevent a recurrence of transmission in DR Congo but, also, the Congolese government should strengthen the improvement of malaria surveillance by mobilizing a medical team to carry out the continuous and systematic collection, analysis and interpretation of malaria data, as well as implementation research on malaria, and the One Health approach in preventing malaria.
Ethics approval and consent to participle
Not applicable.
Consent for publication
Not applicable.
Funding
The authors did not receive any financial support for this work.
Authors’ contribution
Conception: Aymar AKILIMALI and Rodrigue Fikiri BAVURHE, Funding Acquisition: Olivier NYAKIO, Supervision: Olivier NYAKIO, Investigation: Rodrigue Fikiri BAVURHE and Fabrice KIBUKILA, Project administration: Aymar AKILIMALI, Validation: Olivier NYAKIO, Visualisation: Malik Olatunde ODUOYE and Bonk MUHOZA, Software: Rodrigue Fikiri BAVURHE, Chrispin BIAMBA and Hugues CAKWIRA, Manuscript preparation: Bonk MUHOZA, Ricardo Bisimwa RUSENYI, Alain BALUME, Rodrigue Fikiri BAVURHE and Malik Olatunde ODUOYE, Manuscript editing: Bonk MUHOZA, Gaston MASIMANGO, Rodrigue Fikiri BAVURHE and Hugues CAKWIRA, Manuscript review: All authors, Final approval of manuscript: All Authors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
The authors would like to gratefully acknowledge the staff of Medical Research Circle for excellent technical support.
Handling Editor: Patricia Schlagenhauf
Contributor Information
Rodrigue Fikiri Bavurhe, Email: rodfikbav@gmail.com.
Aymar Akilimali, Email: aymarakilimali@gmail.com.
Bonk Muhoza, Email: bonkmuhozagasambi73@gmail.com.
Chrispin Biamba, Email: uwezobiambachrispin@gmail.com.
Malik Olatunde Oduoye, Email: malikolatunde36@gmail.com.
Gaston Masimango, Email: gastonmasimango03@gmail.com.
Hugues Cakwira, Email: huguescakyr@gmail.co.
Alain Balume, Email: alvinbalume@gmail.com.
Ricardo Bisimwa Rusenyi, Email: rrusenyi@gmail.com.
Fabrice Kibukila, Email: fabricekibukila92@gmail.com.
Olivier Nyakio, Email: oliviernyakio@yahoo.fr.
References
- 1.Ntamabyaliro N.Y., Burri C., Lula Y.N., Ishoso D., Engo A.B., Ngale M.A., et al. Knowledge of antimalarials and health seeking behaviour of households in case of Suspected malaria in democratic Republic of the Congo. Trav Med Infect Dis. 2021;6(3):157. doi: 10.3390/tropicalmed6030157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Akilimali A., Bisimwa C., Aborode A.T., Biamba C., Sironge L., Balume A., et al. Self-medication and anti-malarial drug resistance in the democratic Republic of the Congo (DRC): a silent threat. Trop Med Health. 2022 Oct 4;50(1):73. doi: 10.1186/s41182-022-00466-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Organisation mondiale de la santé. Questions et réponses/Paludisme. 6 avril 2022. https://www.who.int/fr/news-room/questions-and-answers/item/malaria
- 4.Bahizire E., D'Alessandro U., Dramaix M., Dauby N., Bahizire F., Mubagwa K., et al. Malaria and iron load at the first antenatal visit in the Rural South Kivu, democratic Republic of the Congo: is iron Supplementation Safe or could it Be harmful? Am J Trop Med Hyg. 2018;98(2):520–523. doi: 10.4269/ajtmh.17-0585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Organisation mondiale de la santé. Paludisme. 6 décembre 2021. https://www.who.int/fr/news-room/fact-sheets/detail/malaria