Abstract
OBJECTIVES:
To determine the 7-day incidence and risk factors of postoperative delirium (POD) occurring after prolapse surgery in women aged ≥60 years.
METHODS:
A prospective study of women ≥60 years undergoing prolapse surgery at a large academic center. The primary outcome is positive Confusion Assessment Method delirium screen administered in person or by telephone at the time of hospital discharge and postoperative days 1, 3, 5, and 7.
RESULTS:
This analysis included 165 patients, mean ± SD age of 72.5 ± 6.1 years, with median (IQR) years of education of 13 (12–16), and baseline Modified Mini-Mental Status (3MS) Exam score of 95 (92–98). Prolapse repair type was vaginal for 70% (n=115) and laparoscopic for 30% (n=50) of patients; most under general anesthesia, 151 (92.1%). The incidence of positive delirium screen during the first week after surgery was 12.1% (n=20). Most of these participants screened positive on postoperative day 0, 8.4% (n=14). In univariate analyses, a positive screen was associated with older age and fewer education years, lower 3MS exam score, greater baseline geriatric depression scale score, and greater frailty score. Lower 3MS score was the only variable that remained significant in the final model (adjusted odds ratio 0.84, 95% CI 0.75–0.95).
CONCLUSIONS:
One in 12 women ≥60 years deemed eligible for discharge on the day of prolapse surgery screens positive for delirium. The 7-day POD incidence is comparable to other elective non-cardiac surgery cohorts. Given the increasing trend toward same day discharge after major prolapse surgery, more research is needed to determine the impact of universal delirium screening as part of discharge assessments.
Keywords: cognitive impairment, older females, pelvic organ prolapse, perioperative neurocognitive disorders, postoperative delirium, surgical outcomes
Brief Summary:
This study reports the incidence of and risk factors for postoperative delirium in older patients after pelvic organ prolapse surgery.
Introduction:
Postoperative delirium (POD), characterized by an acute change in a patients mental status shortly after surgery, is associated with decreased quality of life, increased morbidity and mortality, and increased health care costs (1). Risk factors for POD include older age (mean 74 years (2)), sensory deprivation, functional impairment, preexisting cognitive impairment, and multiple co-morbidities(1,3–6). The incidence of postoperative delirium in older persons >60 years ranges 3 – 70%, varying by surgery type, surgery duration, patient population, and diagnostic criteria (1,2,4). One of the largest prospective studies assessing postoperative delirium reported a 9% incidence in a cohort of 1300 patients (including male and female patients) after major, elective noncardiac surgery (7). However, delirium is under-recognized due to the varied clinical presentations including hyperactive, hypoactive, and mixed forms(1,3,4). Additionally, the lack of uniform delirium screening in the postoperative setting likely contributes to its under-recognition. POD may be occurring more frequently in patient populations undergoing major elective noncardiac surgery (1,8).
Given the U.S. population of adults ≥65 years is expected to double from 40.2 million in 2010 to 88.5 million in 2050 (9), we can anticipate an increased prevalence of pelvic floor disorders, including pelvic organ prolapse (POP), and that more older patients will ultimately undergo surgical repair. Increasing POD recognition by health care professionals and caregivers may influence perioperative risk assessment and guide postoperative recovery planning.
We aimed to determine the incidence of POD in patients aged ≥60 years during the first week post-discharge from the hospital after POP surgery. We hypothesized the incidence would be similar to the 9% reported in other populations after major, noncardiac elective surgery (7). Secondarily, we aimed to identify risk factors associated with POD in our population and hypothesized that older age, frailty, and increased opioid use would be associated with postoperative delirium during the first week after prolapse surgery.
Methods:
Participants and Study Design
This is a prospective cohort study of women (biologic females at birth) 60 years and older who underwent surgery for symptomatic POP at the University of Pittsburgh Medical Center (UPMC) between October 2016 and December 2019. This study was performed with IRB study approval from the University of Pittsburgh (IRB#: STUDY19080233). Eligible patients were recruited into the study after they made the decision to pursue surgery and their urogynecologist placed surgical orders; a co-investigator or the principal investigator (PI) then consented and enrolled participants. Exclusion criteria included: 1) an established diagnosis of cognitive impairment (e.g., dementia), 2) uncompensated severe hearing and/or vision impairment, 3) antipsychotic medication use, 4) self-reported alcohol or drug abuse, and 5) inability to read or write in the English language. After patients were consented, a research assistant (RA) or the principal investigator (PI) administered a screening Modified Mini-Mental Status Examination (3MS) to assess for undiagnosed cognitive impairment (score < 84) (10). Those patients with a 3MS score of <84 were also excluded.
Covariates
Baseline demographic, social and clinical variables were collected within two weeks of scheduled prolapse surgery through participant interview, electronic medical record (EMR) review, questionnaire administration, and frailty assessment.
Clinical and sociodemographic variables collected included: age, race (self-defined), ethnicity, body mass index (calculated from weight/height from chart), medications, medical, surgical and psychiatric history, self-reported hearing and visual impairment, self-reported past or current substance use, number of years of education, employment status, number of dependents, home description, number of persons who live with participant, fall history and any assistive ambulation device use. Perioperative variables and post-operative outcomes abstracted from the electronic medical record included: procedure type and route, anesthesia administered, estimated blood loss, intraoperative complications, hospital length of stay and adverse events up to 6 weeks after surgery. We used Clavien-Dindo criteria to classify postoperative adverse events (13).
Questionnaire administration:
Given the known associations between depression, anxiety and pain symptoms with cognitive impairment, validated questionnaires assessing these symptoms were administered before surgery. Participants completed the following questionnaires to assess depression, anxiety, and pain, respectively: 1) Geriatric Depression Scale – Short Form (GDS), 2) Beck Anxiety Inventory (BAI), 3) Numerical Pain Rating Scale (NPRS). These instruments were selected because they are validated and have been used widely in older adult populations (11–15). We analyzed results from these questionnaires both continuously and categorically as specified for each questionnaire.
Frailty Assessment:
Frailty status was measured using the Fried Frailty Index. Components of this frailty index include weight loss, decreased hand grip strength, exhaustion, slowed walking speed, and low activity. Each criterion is given a score of 0 or 1. Total scores are used to determine frailty status classification as follows: 0 not frail, 1–2 intermediately frail, ≥3 frail (16).
Primary Outcome
The primary outcome was a positive Confusion Assessment Method (CAM) screening (17) which assesses postoperative delirium within 7 days after prolapse surgery. The CAM screen was administered by research personnel trained in accordance with guidelines by Inouye, et al. (18). The Short Portable Mental Status Questionnaire was used to generate observations that were used as the basis for CAM scoring. We used criteria that maximized the sensitivity of delirium detection. The CAM consists of the following criteria: 1) acute or fluctuating behavior, 2) inattention, 3) disorganized thinking, 4) altered level of consciousness, 5) disorientation, 6) memory impairment, 7) perceptual disturbance, 8) psychomotor retardation, 9) psychomotor agitation (15). Participants who have criteria 1 and at least one additional criterion (#3–9) are labeled with a positive CAM screen thus indicating postoperative delirium (15).
In our division’s clinical practice, most patients are discharged from the hospital on postoperative day 0 or 1 after meeting postoperative milestones (including pain control without intravenous analgesic medications, stable vital signs, and ability to tolerate oral food and drink). The CAM screen was first administered in person by a trained assessor (PI/RA) on the day of hospital discharge after the clinical team indicated patient was clinically appropriate for discharge to home. After discharge, a trained assessor administered the CAM by telephone to participants on postoperative days 1, 3, 5, and 7. Telephone administration of CAM has been validated as an accurate means to assess for delirium in prior research (16).
Positive delirium screen results were reported to the attending surgeon. No additional delirium screens were performed as part of the study protocol for these patients. Further evaluation and management of the positive CAM screen was determined by the surgical service and was not tracked as part of this study.
Sample Size Determination
We determined the sample size of the study aiming to estimate the incidence of POD with sufficient precision. Assuming an incidence of POD similar to that reported in major, non-cardiac surgery of 9% (2), a sample size of 140 participants would provide a 95% confidence interval (CI) of (0.048 – 0.15) around a 9% incidence with a half-width of 5.1%.
Statistical Analysis
Incidence of POD was estimated with percentage of participants with POD and the corresponding 95% confidence interval. There was no imputation for missing data in this cohort. Summary (mean ± standard deviation/median (interquartile range) for continuous variables and frequency and percentages for categorical variables, as appropriate) were used for evaluating the participant characteristics by the primary outcome, delirium screen result. Chi-square (or Fisher’s exact) for categorical variables and Student’s t-test (Mann Whitney U statistics) for continuous variables were used to compare participant characteristics across patients with or without positive delirium screen. In exploratory analysis to assess the risk factors of postoperative delirium, univariable logistic regression was performed to further evaluate associations between positive delirium screen and preoperative risk factors. Multivariable logistic regression was performed with forward additions and confirmed with backward removal techniques using candidate variables with p values <0.2 on univariable regression. All statistical analyses were conducted using STATA/SE 15.1 (STATACorp LLC, College Station, TX).
Results:
Figure 1 shows details of participant recruitment and enrollment. Analyses were conducted on 165 of 183 consented participants who provided baseline preoperative interview data.
Figure 1:
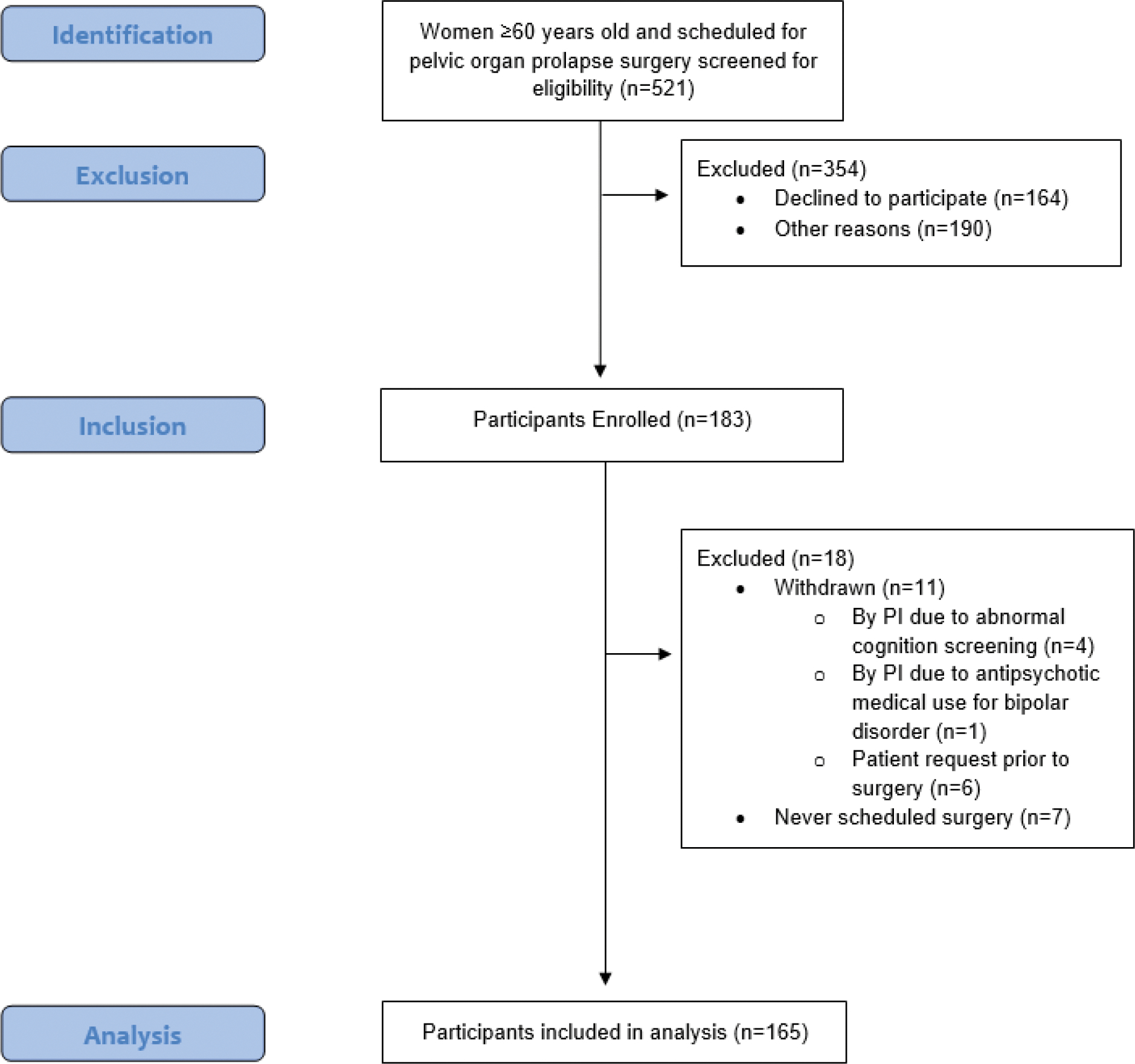
Flowchart of Study Participant Enrollment
Table 1 and 2 show the demographic and clinical factors of the study cohort. The mean (standard deviation (SD)) age for this cohort was 72.5 (6.1) years. The majority of participants were white (n=153, 93.3%). The median (interquartile range (IQR)) number of years of education was 13 (12–16), and the median (IQR) 3MS score was 95 (92–98). Procedures averaged 2 hours, with the majority of prolapse repair performed under general anesthesia, by vaginal route (44 non-mesh apical suspensions, 68 obliterative procedures, 3 mesh suspensions) compared to laparoscopic route (46 mesh sacrocolpopexy, 4 uterosacral ligament suspension). Most patients were discharged to home on the same day of surgery (n=136, 82.4%) with a median (IQR) length of stay of 0.7 (0.6–0.8) days. Median reported opioid use during the first week after surgery was 22.5 MMEs (equivalent to 3 oxycodone 5mg tablets). Adverse events were recorded on 111 participants within 6 weeks after surgery of which 2 were serious adverse events in two separate participants (retroperitoneal hematoma and return to the operating room for persistent surgical site bleeding).
Table 1.
Demographic and Clinical Factors by delirium screen result
| All Participants (n=165) | Participants without positive delirium screen (n=145) | Participants with positive delirium screen (n=20) | p-value | |
|---|---|---|---|---|
| Age, years | 72.5±6.1 | 72.1±5.9 | 75.4±6.5 | 0.02 |
| Race, white | 153 (93.3) | 135 (93.1) | 19 (95) | >0.99 |
| Education, years | 13 (12–16) | 13 (12–16) | 12 (12–13.5) | 0.04 |
| Subjective Hearing Loss | 45 (27.4) | 38 (26.2) | 7 (35) | 0.41 |
| Subjective Vision Loss | 90 (54.5) | 77 (53.1) | 13 (65) | 0.32 |
| Living Alone | 28 (17) | 23 (15.9) | 5 (20) | 0.34 |
| Chronic opioid use | 9 (5.5) | 9 (6.2) | 0 (0) | 0.60 |
| Subjective report of any falls in the past year | 33 (20) | 31 (21.4) | 2 (10) | 0.37 |
| ASA classification | 0.75 | |||
| 1 | 3 (1.8) | 3 (2.1) | 0 (0) | |
| 2 | 85 (51.8) | 73 (50.3) | 12 (60) | |
| 3 | 76 (46.3) | 69 (47.6) | 8 (40) | |
| Fried Frailty Index | 0.12 | |||
| Not Frail (score 0) | 31 (18.8) | 29 (20) | 2 (10) | |
| Prefrail/Intermediate (score 1–2) | 115 (69.7) | 102 (70.3) | 13 (65) | |
| Frail (score ≥3) | 19 (11.5) | 14 (9.7) | 5 (26.3) | |
| Fried Frailty Index Score, (range 0–5) | 1 (1–2) | 1 (1–2) | 1.5 (1–2.5) | 0.04 |
| Modified Mini-Mental Status Exam Score (range: 0–100) | 95 (92–98) | 96 (93–98) | 90.5 (86.5–95) | 0.002 |
| History of Depression | 26 (15.8) | 22 (15.2) | 4 (20) | 0.53 |
| Baseline Geriatric Depression Scale Score, (range 0–15) | 1 (0–2) | 1 (0–2) | 2 (1–4) | 0.03 |
| Baseline Geriatric Depression Scale Result (n=164) | 0.44 | |||
| No depression | 147 (89.6) | 130 (90.3) | 17 (85) | |
| Suggestive of depression | 17 (10.3) | 14 (9.7) | 3 (15) | |
| History of Generalized Anxiety Disorder | 39 (23.6) | 33 (22.8) | 6 (30) | 0.48 |
| Baseline Beck Anxiety Index Score, (range 0–22) | 4.5 (2–9) | 4 (2–8.5) | 6.5 (3–12) | 0.34 |
| Baseline Beck Anxiety Index Result | 0.33 | |||
| Minimal level of anxiety (score 0 –7) – score 1 | 110 (66.7) | 99 (68.2) | 11 (55) | |
| Mild level of anxiety (score 8 – 15) - score 2 | 38 (23) | 32 (22.1) | 6 (30) | |
| Moderate level of anxiety (score 16–25) – score 3 | 14 (8.5) | 12 (8.3) | 2 (10) | |
| Severe level of anxiety (score 26–63) – score 4 | 3 (1.8) | 2 (1.4) | 1 (5) | |
Data presented as mean ± standard deviation, median (interquartile range), n(%)
Table 2.
Intraoperative and Postoperative Clinical Factors by delirium screen result
| All Participants (n=165) | Participants without positive delirium screen (n=145) | Participants with positive delirium screen (n=20) | p-value | |
|---|---|---|---|---|
| Surgical Approach | 0.13 | |||
| Vaginal | 115 (69.7) | 98 (67.6) | 17 (85) | |
| Laparoscopic | 50 (30.3) | 47 (32.4) | 3 (15) | |
| Concomitant Hysterectomy | 98 (59.3) | 89 (61.4) | 9 (45) | 0.12 |
| Type of Anesthesia | 0.052 | |||
| General | 151 (91.5) | 135 (93.1) | 16 (80) | |
| Local with IV sedation | 2 (1.2) | 1 (0.07) | 1 (5) | |
| Regional | 12 (7.3) | 9 (6.2) | 3 (15) | |
| Duration of Surgery, hours | 2.3 ± 0.8 | 2.3 ± 0.8 | 2.4 ± 1.1 | 0.61 |
| Duration of Anesthesia, hours | 3.2 ± 0.9 | 3.2 ± 0.8 | 3.4 ± 1.2 | 0.36 |
| Use of inhalational gas | 37 (22.4) | 33 (22.8) | 4 (20) | 1.0 |
| Estimated blood loss, mL | 50 (25–100) | 50 (25–80) | 75 (45–112.5) | 0.06 |
| Length of Stay, days | 0.7 (0.6–0.8) | 0.7 (0.6–0.8) | 0.7 (0.6–0.75) | 0.88 |
| Total opioid use during first week after surgery, MMEs | 22.5 (1.6–61.6) | 22.9 (1.6–60.9) | 17 (7.5–87.5) | 0.62 |
| Adverse Events | 111 (67.3) | 96 (66.2) | 15 (75) | 0.61 |
| Adverse Event Grade* | 0.66 | |||
| No adverse event | 54 (32.7) | 49 (33.8) | 5 (25) | |
| Grade 1 | 63 (38.2) | 53 (36.6) | 10 (50) | |
| Grade 2a | 20 (12.1) | 18 (12.4) | 2 (10) | |
| Grade 2abx | 26 (15.8) | 23 (15.9) | 3 (15) | |
| Grade 2b | 0 (0) | 0 (0) | 0 (0) | |
| Grade 3 | 0 (0) | 2 (1.3) | 0 (0) | |
| Grade 4 | 0 (0) | 0 (0) | 0 (0) | |
| Grade 5 | 0 (0) | 0 (0) | 0 (0) | |
| Serious Adverse Events | 2 (1.2) | 2 (1.4) | 0 (0) | 1.0 |
Data presented as mean ± standard deviation, median (interquartile range), n(%)
by Clavien-Dindo criteria
Abbreviations/Definitions:
MMEs: morphine milligram equivalents
Serious Adverse Events: includes any grade 3, 4 or 5 adverse events by Clavien-Dindo criteria
The incidence of positive delirium screen was 12.1% (n=20). The majority of participants screened positive at the time they were deemed appropriate for discharge to home on postoperative day 0 (n=14, 8.5%). The remaining participants screened positive for delirium on postoperative day 1 (n=2), postoperative day 3 (n=2) and postoperative day 5 (n=2). No participants had a positive delirium screen on postoperative day 7. CAM screening was missed for 18 patients on postoperative day #1, 39 patients on postoperative day #3, 35 patients on postoperative day #5, and 28 patients on postoperative day #7. There were 10 women who missed 2 or more delirium screenings who never screened positive for postoperative delirium.
Participants with positive delirium screen at any point in time were relatively older (mean 75.4 vs. 72.1 years, p=0.02). Participants with a positive screen had lower preoperative 3MS score (median score 90.5 vs. 96, p=0.002). Greater frailty status score was associated with positive delirium screening (median score 1.5 vs. 1, p=0.04). Greater baseline GDS score was associated with positive delirium screen (median (IQR) score 2 (1–4) vs. 1 (0–2), p=0.03). However, scores suggestive of depression (>5) on the GDS did not differ significantly whether there was a positive or negative delirium screen. Type of anesthesia administered, specifically use of regional or local with intravenous (IV) sedation, and estimated blood loss did not significantly differ between participants with positive delirium screens and those without (p=0.052, p=0.06). None of the participants with a positive delirium screen had a history of chronic opioid use. Logistic regression was performed to assess the association between significant preoperative clinical factors and positive delirium screen. Only lower 3MS score remained significantly associated with positive CAM screen after controlling for age, baseline GDS score, number of education years, and frailty score (p=0.01, adjusted odds ratio 0.84, 95% CI 0.75–0.95) (Table 3).
Table 3.
Crude and adjusted odds ratios of significant preoperative risk factors for postoperative delirium
| Preoperative Variable | p-value | Unadjusted Odds Ratio | 95% CI | p-value | Adjusted Odds Ratio | 95% CI |
|---|---|---|---|---|---|---|
| Age, years | 0.03 | 1.09 | 1.01 – 1.18 | |||
| Baseline Geriatric Depression Scale Score | 0.08 | 1.19 | 0.98 – 1.43 | |||
| Education, years | 0.09 | 0.80 | 0.61 – 1.0 | |||
| Fried Frailty Index Score | 0.05 | 1.51 | 1.00 – 2.29 | |||
| Modified Mini-Mental Status Exam Score | 0.000 | 0.82 | 0.74 – 0.92 | 0.01 | 0.84 | 0.75 – 0.95 |
CI: confidence interval
Discussion:
We found a 12.1% incidence of postoperative delirium within 7 days after prolapse surgery in patients aged ≥60 years. This is greater than the 9% incidence of POD reported by Marcantonio et al. in a large prospective cohort study of approximately 1300 patients aged ≥50 years after elective noncardiac surgery (7). This difference may be related to few factors. First, the Marcantonio study initiated delirium screening on postoperative day 2, which is a longer interval after surgery compared to our study in which delirium screens were performed at the time participants were deemed appropriate for hospital discharge (often the same day of surgery). Marcantonio study participants were aged ≥ 50 years, which is a younger cohort compared to our study. Additionally, this study used the CAM or a review of data from the medical record and the hospital’s nursing intensity index to diagnosis postoperative delirium (7). Our study findings, however, are lower compared to the reported postoperative delirium incidence of 24% in the Successful Aging After Elective Surgery (SAGES) study (19). Participants in the SAGES study were similar to our study in that they were all aged ≥70 years. However, over 80% of SAGES participants underwent orthopedic surgery, and all participants had an anticipated hospital length of stay of at least 3 days (19). Our findings are consistent with a systematic review by Dasgupta et al., inclusive of 25 studies of men and women, that reported 5.1%–52.2% incidence of delirium after elective noncardiac surgery (20). In contrast, a retrospective study of 620 urogynecologic surgery patients aged ≥60 years admitted to the hospital overnight for extended recovery reported a 0.27% incidence of equivocal, “unable to assess” CAM screens with no positive CAM screens (21). Comparisons between this study and ours are limited as only the published abstract is available for review (17).
Prior research has reported the highest risk of POD within 48 hours after surgery (1). In our study, the majority of positive delirium screens were first recognized on postoperative day 0 in those meeting milestones for discharge, which has significant implications given the majority of participants in this cohort had same-day discharge after surgery. With earlier hospital discharge, the ability to recognize this clinical diagnosis is diminished. We did not collect data on management plans for those patients who screened positive for delirium. Clinically, patients were managed as per their surgeon. Although we did collect data on postoperative adverse events, we did not comprehensively measure healthcare needs and utilization for those patients with a positive CAM screen. While information regarding POD management and subsequent outcomes was not collected in this study, inclusion of these variables should be considered in future research as findings may greatly influence postoperative care recommendations. It is important that all health care professionals recognize the potential for POD to occur, including delayed development outside of hospital surveillance, and its negative impact on postoperative recovery. Informing family members and caregivers of the risk of delirium and education on physical and behavioral signs of postoperative delirium may increase early recognition particularly in our patients with short hospitalizations after surgery.
Our study found that positive delirium screen result was associated with older age, lower baseline 3MS score, and greater baseline GDS. Multiple studies have reported older age (greater than 60 years) as a risk factor for POD (7,8,22,23). Baseline cognitive impairment, objectively measured with Mini-Cog© or Mini-Mental Status examination, has been commonly reported as a risk factor for postoperative delirium (7,22,23). Notably, our study excluded patients with known cognitive impairment and those with a 3MS score concerning for undiagnosed cognitive impairment. Despite this exclusion, there was a significant association between positive delirium screen and lesser 3MS scores after adjusting for age and number of years of education. This highlights that patients who are considered cognitively normal (yet with weaker cognitive performance on general cognition screening) are vulnerable to delirium. Our findings further support the inclusion of preoperative cognitive evaluation for older women as part of a preoperative risk assessment which is recommended by the American College of Surgeons and the American Geriatric Society(24,25).
Our study findings do not corroborate the association between depression and POD by others (26,27). In our study cohort, participants with positive delirium screen had statistically significant greater GDS scores. However, most of the absolute scores did not meet criteria for “suggestive of depression” (score of >5) on the GDS questionnaire making the clinical relevance of this association less clear.
There was an association between positive delirium screen and use of regional or sedation anesthesia. This is likely related to baseline patient factors that may have influenced the surgical teams’ decision to use regional or local anesthesia rather than general anesthesia. These factors may include concern for baseline cognitive impairment or frail status. We did not collect information on reasoning for choice of anesthesia mode in this study and are therefore limited in understanding the bias that may have been introduced. Another consideration is the potential impact of anesthetic and sedative medications used with regional anesthesia and subsequent changes to oxygen saturations intraoperatively. Other studies comparing regional versus general anesthesia have found no significant differences in postoperative delirium between groups (28,29). Future studies will need larger sample sizes with more evenly distributed cohorts across each anesthesia mode to further evaluate the impact of type of anesthesia on postoperative delirium.
One major limitation to consider is the fluctuating nature of delirium, which may have led to an underestimation of POD incidence. Further, missing data was not imputed and a missed call was assumed as a “negative” screen in order to minimize overestimation of positive screening. We acknowledge that this missingness may possibly be related to the underlying postoperative delirium. Another consideration is that telephone assessment using CAM, while validated, may still limit evaluation as there may be visual cues indicating cognitive impairment that are not recognized. This can be overcome in future work through use of telemedicine video encounters. While we did perform baseline cognitive assessments preoperatively, we did not perform preoperative delirium screens. The possibility of the presence of preoperative delirium in the setting of a normal baseline cognition screen should be considered. Findings from our study have limited generalizability due to the racially homogenous nature and the average to above average education level of the cohort. Fewer education years is a risk factor for postoperative delirium (1,3). Thus, our findings may be an underestimation of the incidence in more educationally diverse populations. There was also a significant proportion of eligible patients who chose not to enroll in this study. Participation bias (i.e. patients not enrolling due to concern they may have underlying cognitive impairment that they do not want to reveal, patients enrolling because they are worried about postoperative delirium and want additional screening) may have influenced our study findings. We were unable to characterize this subset of patients who declined study participation which also limits generalizability of our findings. Additionally, we did not assess functional status and independence which limits our ability to study how a positive delirium screen may have altered functional ability during postoperative recovery.
We elected to not include patients with known cognitive impairment or with 3MS scores indicative of underlying cognitive impairment. We acknowledge that preexisting cognitive impairment is a reported independent risk factor for POD(1,3). However, our objective was to identify POD incidence in older urogynecologic patients who may not otherwise anticipate cognitive impairment postoperatively. This is another reason our findings may be an underestimation of POD in the general population.
Despite these limitations, strengths of this study include its prospective study design and use of the validated CAM to assess for postoperative delirium. Additionally, we were able to extend the postoperative assessment period beyond hospital discharge with use of CAM screening over the phone. Finally, this was especially important in this patient population given the short hospital length of stay patients experience. This is one of very few studies that has focused on identifying the incidence of postoperative delirium in an older urogynecologic surgery population.
In summary, positive delirium screen results in prolapse surgery patients was appreciated at an incidence similar to other elective non-cardiac surgery cohorts during the first 7 days of postoperative recovery. With the surgical field’s increasing frequency of same-day discharge after major surgery, our study findings highlight the importance of screening for delirium prior to hospital discharge for all surgical patients. Further, we must educate surgeons, primary care physicians and family members/caregivers about this potential outcome. This includes counseling our patients on the importance of having in-person social support during the first 3 days after surgery (the period one is at greatest risk of developing postoperative delirium). Increasing recognition of postoperative delirium is the first step to minimizing its negative impact on postoperative recovery. Future studies should focus on evaluating the impact of POD on functional status, independence and patient safety as well as assessing the need for postdischarge monitoring/evaluation for POD.
Acknowledgements/Funding:
This work was supported by the Audrey Hillman Fisher Foundation Grant, the American Urogynecologic Society Pelvic Floor Disorders Research Foundation Grant-Faculty Research Award, the National Institutes of Health NICHD Women’s Reproductive Health Research (WRHR) Career Development Program (5K12HD063087), and National Institutes of Health support through Clinical and Translational Sciences Institute (CTSI) at the University of Pittsburgh (UL1-TR-001857).
Footnotes
Financial Disclaimers/Conflicts of Interest: Author MF Ackenbom has received research funding support from the NIH NICHD (5K12HD063087), the American Urogynecologic Society Pelvic Floor Disorders Research Foundation, and the Audrey Hillman Foundation. Author EM Davis is a member of the US Preventive Services Task Force.
References
- 1.Schenning KJ, Deiner SG. Postoperative delirium in the geriatric patient. Anesthesiol Clin. 2015. Sep;33(3):505–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Silva AR, Regueira P, Albuquerque E, Baldeiras I, Cardoso AL, Santana I, et al. Estimates of Geriatric Delirium Frequency in Noncardiac Surgeries and Its Evaluation Across the Years: A Systematic Review and Meta-analysis. J Am Med Dir Assoc. 2020. Sep 30; [DOI] [PubMed] [Google Scholar]
- 3.Raats JW, Steunenberg SL, de Lange DC, van der Laan L. Risk factors of post-operative delirium after elective vascular surgery in the elderly: A systematic review. Int J Surg. 2016. Nov;35:1–6. [DOI] [PubMed] [Google Scholar]
- 4.Watt J, Tricco AC, Talbot-Hamon C, Pham B, Rios P, Grudniewicz A, et al. Identifying Older Adults at Risk of Delirium Following Elective Surgery: A Systematic Review and Meta-Analysis. J Gen Intern Med. 2018. Jan 26;33(4):500–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Janssen TL, Steyerberg EW, Faes MC, Wijsman JH, Gobardhan PD, Ho GH, et al. Risk factors for postoperative delirium after elective major abdominal surgery in elderly patients: A cohort study. Int J Surg. 2019. Sep 14;71:29–35. [DOI] [PubMed] [Google Scholar]
- 6.Marcantonio ER. Postoperative delirium: a 76-year-old woman with delirium following surgery. JAMA. 2012. Jul 4;308(1):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marcantonio ER, Goldman L, Mangione CM, Ludwig LE, Muraca B, Haslauer CM, et al. A clinical prediction rule for delirium after elective noncardiac surgery. JAMA. 1994. Jan 12;271(2):134–139. [PubMed] [Google Scholar]
- 8.Raats JW, van Eijsden WA, Crolla RMPH, Steyerberg EW, van der Laan L. Risk Factors and Outcomes for Postoperative Delirium after Major Surgery in Elderly Patients. PLoS One. 2015. Aug 20;10(8):e0136071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vincent GK, Velkoff VA. The next four decades: The older population in the United States: 2010 to 2050. US Census Bureau. Economics and Statistics Administration. 2010; [Google Scholar]
- 10.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987. Aug;48(8):314–318. [PubMed] [Google Scholar]
- 11.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988. Dec;56(6):893–897. [DOI] [PubMed] [Google Scholar]
- 12.Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clinical Gerontologist: The Journal of Aging and Mental Health. 1986; 5(1–2), 165–173. [Google Scholar]
- 13.Rodriguez CS. Pain measurement in the elderly: a review. Pain Manag Nurs. 2001. Jun;2(2):38–46. [DOI] [PubMed] [Google Scholar]
- 14.Bass DS, Attix DK, Phillips-Bute B, Monk TG. An efficient screening tool for preoperative depression: the Geriatric Depression Scale-Short Form. Anesth Analg. 2008. Mar 1;106(3):805–9, table of contents. [DOI] [PubMed] [Google Scholar]
- 15.Balsamo M, Cataldi F, Carlucci L, Fairfield B. Assessment of anxiety in older adults: a review of self-report measures. Clin Interv Aging. 2018. Apr 6;13:573–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg. 2010. Jun;210(6):901–908. [DOI] [PubMed] [Google Scholar]
- 17.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI. Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med. 1990. Dec 15;113(12):941–948. [DOI] [PubMed] [Google Scholar]
- 18.Inouye SK. The Confusion Assessment Method (CAM): training manual and coding guide. New Haven: Yale University School of Medicine. 2003; [Google Scholar]
- 19.Cizginer S, Marcantonio E, Vasunilashorn S, Pascual-Leone A, Shafi M, Schmitt EM, et al. The cognitive reserve model in the development of delirium: the successful aging after elective surgery study. J Geriatr Psychiatry Neurol. 2017. Nov;30(6):337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dasgupta M, Dumbrell AC. Preoperative risk assessment for delirium after noncardiac surgery: a systematic review. J Am Geriatr Soc. 2006. Oct;54(10):1578–1589. [DOI] [PubMed] [Google Scholar]
- 21.Reagan KM, O’Sullivan DM, Dicks RS. Incidence of Postoperative Delirium in Urogynecology Surgical Patients. Journal of Minimally Invasive Gynecology. 2015; 22(3):S14. [Google Scholar]
- 22.Ansaloni L, Catena F, Chattat R, Fortuna D, Franceschi C, Mascitti P, et al. Risk factors and incidence of postoperative delirium in elderly patients after elective and emergency surgery. Br J Surg. 2010. Feb;97(2):273–280. [DOI] [PubMed] [Google Scholar]
- 23.Litaker D, Locala J, Franco K, Bronson DL, Tannous Z. Preoperative risk factors for postoperative delirium. Gen Hosp Psychiatry. 2001. Mar;23(2):84–89. [DOI] [PubMed] [Google Scholar]
- 24.Mohanty S, Rosenthal RA, Russell MM, Neuman MD, Ko CY, Esnaola NF. Optimal Perioperative Management of the Geriatric Patient: A Best Practices Guideline from the American College of Surgeons NSQIP and the American Geriatrics Society. J Am Coll Surg. 2016. Jan 4;222(5):930–947. [DOI] [PubMed] [Google Scholar]
- 25.Colburn JL, Mohanty S, Burton JR. Surgical guidelines for perioperative management of older adults: what geriatricians need to know. J Am Geriatr Soc. 2017. Jun;65(6):1339–1346. [DOI] [PubMed] [Google Scholar]
- 26.Leung JM, Sands LP, Mullen EA, Wang Y, Vaurio L. Are preoperative depressive symptoms associated with postoperative delirium in geriatric surgical patients? J Gerontol A, Biol Sci Med Sci. 2005. Dec;60(12):1563–1568. [DOI] [PubMed] [Google Scholar]
- 27.Elsamadicy AA, Adogwa O, Lydon E, Sergesketter A, Kaakati R, Mehta AI, et al. Depression as an independent predictor of postoperative delirium in spine deformity patients undergoing elective spine surgery. J Neurosurg Spine. 2017. Jun 2;1–6. [DOI] [PubMed] [Google Scholar]
- 28.Li T, Li J, Yuan L, Wu J, Jiang C, Daniels J, et al. Effect of regional vs general anesthesia on incidence of postoperative delirium in older patients undergoing hip fracture surgery: the RAGA randomized trial. JAMA. 2022. Jan 4;327(1):50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patel V, Champaneria R, Dretzke J, Yeung J. Effect of regional versus general anaesthesia on postoperative delirium in elderly patients undergoing surgery for hip fracture: a systematic review. BMJ Open. 2018. Dec 4;8(12):e020757. [DOI] [PMC free article] [PubMed] [Google Scholar]


