Abstract
Depression is a common concern among people with autism spectrum disorder (ASD) and is often associated with social skills and relationship challenges. The present data, from a randomized controlled trial, examined the effect of PEERS® on self-reported depressive symptoms via the Children’s Depression Inventory (CDI) among forty-nine adolescents with ASD. Findings revealed that many CDI subscale scores declined (p’s < 0.05) and were related to direct social contact on the Quality of Socialization Questionnaire at posttest (p’s < 0.05). Exploratory analyses uncovered that suicidality was less evident following PEERS®. Findings support the notion that social functioning and depression may be intimately intertwined in ASD; therefore, bolstering social skills in ASD may positively influence other domains of functioning, including mental health.
Keywords: autism spectrum disorder, social skills intervention, adolescence, depression, suicidality
Depression is characterized by persistent low mood and loss of interest in activities, along with symptoms such as fatigue, feelings of worthlessness, and sleep and appetite disturbances that negatively impact daily functioning (American Psychiatric Association, 2013). Depressive symptoms are commonly observed among people with autism spectrum disorder (ASD), as measured by self-report (Bitsika & Sharpley, 2015), parent-report (Mayes, Calhoun, Murray, Ahuja, & Smith, 2011), and structured clinical interview (Leyfer et al., 2006), with prevalence estimates of depression ranging between 10 to 54% among those with ASD. Among typically developing (TD) youth, research has identified multiple risk factors for depression; both contextual (i.e., parenting behaviors, life stressors, and peer relationships) and individual factors (i.e., genetics, neurobiological stress response, temperament, and cognitive functioning) appear to promote depressive symptoms in youth (Klein, Kujawa, Black, & Pennock, 2013). Although the manifestation of depression in ASD is variable and its etiology is not well understood (Magnuson & Constantino, 2011), social factors seem to be related to depression in ASD.
The social difficulties inherent in ASD may impede the formation and maintenance of high-quality friendships (Mendelson, Gates, & Lerner, 2016); cognitive capacities (i.e., theory of mind; Bauminger, Solomon, & Rogers, 2010) and verbal abilities (Bauminger et al., 2008) have been related to friendship quality and behaviors among youth with ASD. Moreover, the lack of social initiation observed in ASD (Humphrey & Symes, 2011) is likely exacerbated by deflated self-esteem due to unsuccessful social interactions (Denissen, Penke, Schmitt, & Van Aken, 2008). These feelings of rejection may contribute to social withdrawal, which further hinder additional attempts to initiate social interactions and, thus, result in fewer opportunities to form meaningful friendships. Isolation and feelings of loneliness related to poor quality or low quantity of friendships are linked with the development of depressive symptoms among youth with ASD (Mazurek & Kanne, 2010; Whitehouse, Durkin, Jaquet, & Ziatas, 2009).
Multiple studies suggest that factors such as IQ and autism severity are positively associated with levels of depressive symptoms in ASD (Mayes, Calhoun, Murray, & Zahid, 2011; Vickerstaff, Heriot, Wong, Lopes, & Dossetor, 2007); that is, higher IQ and greater autism severity are commonly seen with more severe depressive symptoms. Increased social challenges, coupled with heightened awareness, may confer risk for depression in ASD, perhaps especially among those who recognize their difficulties navigating social situations. Preliminary support for the role of social awareness in the development of depression comes from a study that identified that children and adolescents with ASD who were more likely to engage in social comparison were at greater risk for developing depressive symptoms (Hedley & Young, 2006).
Peer Victimization and Suicidal Ideation in ASD
Research has presented compelling evidence that youth with ASD are more often victims of teasing and bullying compared to their TD peers (Humphrey & Lewis, 2008; Zeedyk, Rodriguez, Tipton, Baker, & Blacher, 2014). Multiple factors may underlie the observed increased risk of victimization. In general, youth who are likely to suffer from bullying often occupy low sociometric status (Card et al., 2007), a measure of acceptance from one’s peer group, and display inappropriate expression of emotion and social behaviors (Garner & Hinton, 2010), both commonly observed among youth with ASD. Typically developing peers may also perceive youth with ASD as deviating from the norm due to socially-incongruent behavior, resulting in reduced peer acceptance and increased episodes of bullying (Humphrey & Hebron, 2015). Victimization has been linked to negative outcomes in TD populations, including depleted self-esteem, as well as depression and suicidal ideation (Malecki et al., 2015; Van der Wal, De Wit, & Hirasing, 2003). Similarly, victimization among ASD children is associated with quantity and quality friends, as well as internalizing and externalizing symptoms (Cappadocia, Weiss, & Pepler, 2012; Zeedyk et al., 2014).
The aforementioned factors pose risk for psychological distress and, at an extreme, suicidal ideation. Little research has examined suicidal thoughts and behaviors among youth with ASD, a critical gap in the literature (Segers & Rawana, 2014). Among the few studies that have investigated suicidality in ASD, rates have been found to be 28 times greater than in TD children; 14% of mothers reported that their child with ASD has problems with suicidal ideation and/or attempts (Mayes, Gorman, Hillwig-Garcia, & Syed, 2013) and 22% of parents endorsed that their youth with ASD mentioned death or suicide “often” or “very often” (Horowitz et al., 2017). Self-report has revealed even more alarming statistics, such that, among adults with ASD, 66% reported suicidal ideation and 35% reported plans or attempts at suicide (Cassidy et al., 2014). Depression and teasing have been identified as two of the most highly predictive factors of suicidal thoughts and behaviors in this population (Horowitz et al., 2017; Mayes, Calhoun, Murray, & Zahid, 2011; Storch et al., 2013) , similar to findings in TD youth (Bridge, Goldstein, & Brent, 2006). Thus, the challenges inherent in ASD, coupled with depressive symptoms, may confer significant vulnerability for suicidality. These associations and prevalence rates necessitate a better understanding of the phenomenology of suicidality in youth with ASD, as well as interventions that may reduce suicidal thoughts and behavior.
The Role of Friendships in Adolescence
Positive psychosocial adjustment has been related to optimal outcomes in adolescence (Armsden & Greenberg, 1987), with friendship having a protective effect on youths’ well-being (Hall-Lande, Eisenberg, Christenson, & Neumark-Sztainer, 2007). Social dynamics become particularly salient during adolescence as youth begin to shift their source of security, trust, and social support from parents to peers (Steinberg & Morris, 2001). Higher quality friendships are associated with greater feelings of self-worth, improved social competence, and better adjustment (Rubin et al., 2004). Further, friendships may buffer against vulnerability for and negative impacts of victimization in youth with ASD (Humphrey & Symes, 2010; Schmidt & Bagwell, 2007). Considering the social challenges experienced by youth with ASD, the benefits of high-quality friendships may not be as readily available to these adolescents.
Social Skills Intervention and Internalizing Symptoms in ASD
Evidence suggests strong links between social difficulties, friendships, and depression in ASD, thus, interventions aimed at increasing social skills and, in turn, cultivating friendships, have the potential to ameliorate symptoms of depression. Arming youth with ASD with the tools needed to better succeed within the social realm may increase successful peer interactions, boost self-confidence, facilitate the development of friendships, and, in turn, decrease depressive symptoms. Although an understudied area of research, preliminary support for this hypothesis has been identified by Hillier and colleagues (2011) in a sample of young adults with ASD receiving an eight-week social and vocational skills program called Aspirations. In this study, depressive symptoms, as measured by self-report, decreased following the intervention.
Additional support is provided by research surrounding a manualized, empirically-supported social skills intervention for people with ASD, the Program for the Education and Enrichment of Relational Skills (PEERS®), that has been found to increase social competence among both adolescents (Laugeson, Frankel, Gantman, Dillon, & Mogil, 2012) and young adults (Gantman, Kapp, Orenski, & Laugeson, 2012), and has been demonstrated to be equally efficacious for males and females with ASD (McVey et al., 2017). Some evidence suggests that PEERS® reduces internalizing symptoms such as social anxiety and loneliness (McVey et al., 2016; Schohl et al., 2014). Additionally, a cultural adaptation of the PEERS® intervention in Korea examined self-reported depressive symptoms via the total score on the Korean version of the CDI as a secondary outcome in response to PEERS®. The PEERS® intervention was translated into Korean and several sessions were culturally-modified as detailed in Yoo et al. (2014). The study revealed a decrease in general depressive symptoms, employing paired samples t-tests to examine changes from pre-treatment to post-treatment in their sample (Yoo et al., 2014). Considering the cultural and language differences between the United States and Korea (e.g., Kim & Choi, 1994) and the lack of testing group by time effects, however, additional research is needed to examine depressive symptoms in more depth among adolescents receiving PEERS® in the United States.
Summary and Aims of the Current Study
In sum, there appear to be strong links between social abilities, friendships, and depression in youth with ASD. Thus, interventions targeting social skills shown to facilitate development and maintenance of friendships may decrease depressive symptoms in adolescents with ASD. The aims of the current study were to extend previous work and examine: 1) whether a social skills intervention (PEERS®) impacts multiple dimensions of depressive symptoms among adolescents with ASD in the United States, 2) the relation between direct peer interactions and depression at intervention posttest, and 3) changes in self-reported suicidal ideation across intervention provision. It was hypothesized that receiving PEERS® would reduce multiple dimensions of self-reported depressive symptoms, that there would be negative relations between reports of social contacts and depressive symptoms, such that greater instances of direct peer interactions would be associated with fewer symptoms of depression, and that fewer participants would report suicidal ideation following the PEERS® intervention.
Method
Participants
Participants were part of a larger randomized controlled trial of PEERS® for adolescents. Efficacy of the intervention has been established by previous studies (Laugeson et al., 2012; Schohl et al., 2014) and, therefore, will not be reported upon in this study. Data from a final sample of forty-nine adolescents with ASD ages 11 to 16 was analyzed in this sub-study. Participants were randomly assigned to either the experimental (EXP; n = 24) or waitlist control (WL; n = 25) group; see Figure 1: CONSORT Diagram. Diagnosis of ASD was confirmed using the ADOS-G (Lord et al., 2000). The KBIT-2 (Kaufman, 1997) was used to assess IQ; participants had a full-scale IQ of 68 or higher. Demographics can be found in Table 1; the EXP and WL groups did not significantly differ on any demographic variables, as shown.
Figure 1.
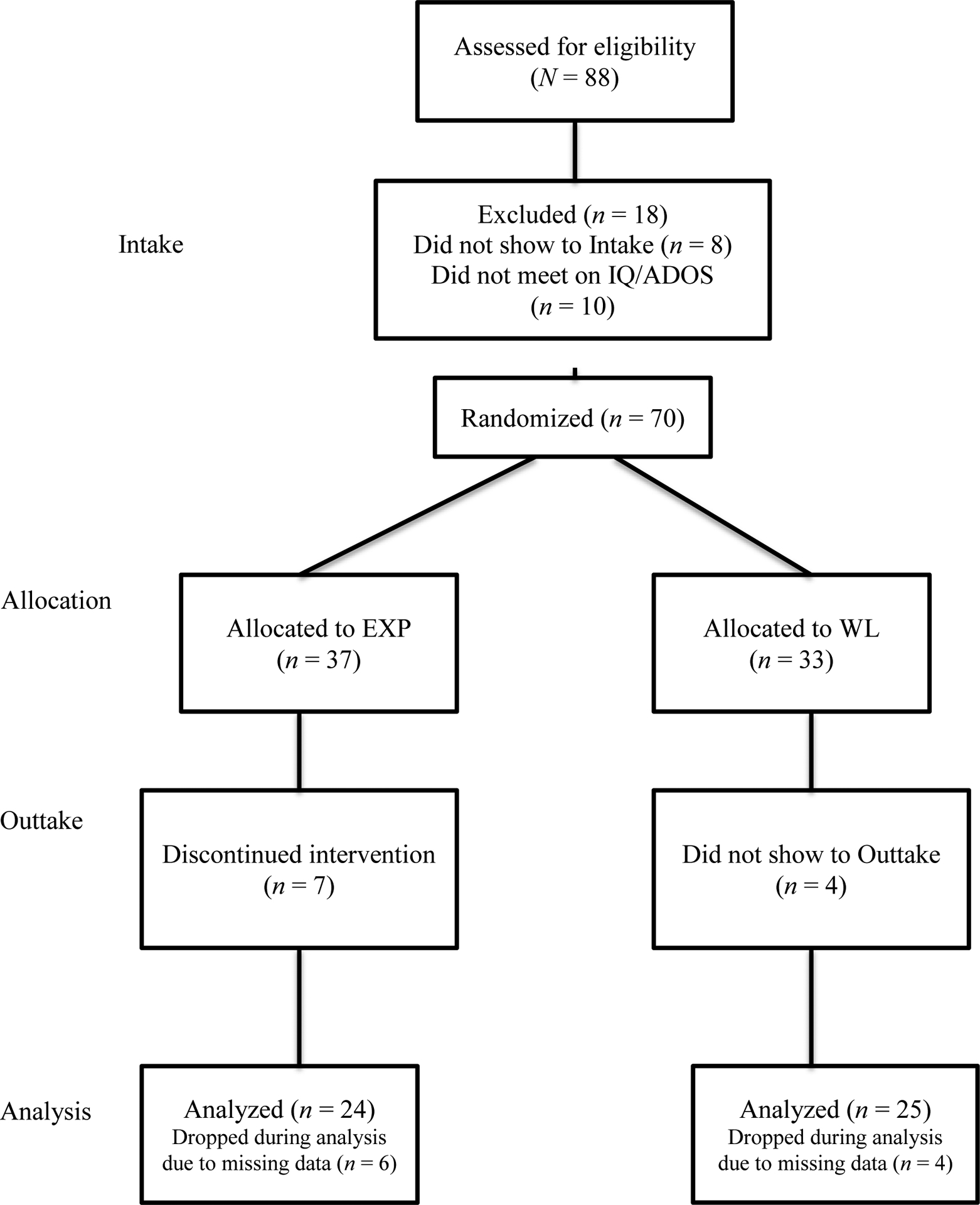
CONSORT Diagram
Table 1.
Participant Demographics by Group
| EXP (n=24) | WL (n=25) | |||||
|---|---|---|---|---|---|---|
| M(SD) | Range | M(SD) | Range | F/χ2 | p | |
| Age | 13.25 (1.07) | 12 – 15 | 13.52 (1.92) | 11–16 | 0.37 | 0.55 |
| FSIQ | 105.33 (12.70) | 69–144 | 104.24 (16.25) | 68–133 | 0.04 | 0.84 |
| ADOS-G | 11.58 (4.22) | 7–19 | 12.60 (4.77) | 7–23 | 0.62 | 0.43 |
| Gender | ||||||
| % Female | 8.3 | 8.0 | 0.002 | 0.97 | ||
| Race | ||||||
| % White | 75 | 76.0 | 2.34 | 0.67 | ||
| % Asian | 8.3 | 4.0 | ||||
| % Black | 8.3 | 8.0 | ||||
| % Biracial | 4.2 | 12.0 | ||||
| Ethnicity | ||||||
| % non-Latino | 83.3 | 96.0 | 2.68 | 0.26 | ||
| Household Income | ||||||
| % <25K | 0.0 | 20.0 | 7.38 | 0.19 | ||
| % 25K – 50K | 8.3 | 8.0 | ||||
| % 50K – 75K | 25.0 | 16.0 | ||||
| % 75K – 100K | 20.8 | 20.0 | ||||
| % > $100K | 37.5 | 36.0 | ||||
EXP – Experimental Group. WL – Waitlist Control Group. M – Mean. SD – Standard Deviation. FSIQ – Full-Scale Intellectual Quotient as measured by the Kaufman Brief Intelligence Test, Second Edition. ADOS-G – Autism Diagnostic Observation Schedule, Generic. K – Thousand.
Procedure
This study was approved by the Institutional Review Board (IRB) at Marquette University. Please see (Schohl et al., 2014) for details on procedures for selecting participants and inclusion criteria. Informed consent was obtained from all participants in this study. Participants provided self-report on the Children’s Depression Index (CDI; Kovacs, 1992) at two time points. The EXP group completed the CDI before and after PEERS®; the WL group completed reports on the CDI approximately 14 weeks apart and participated in PEERS® thereafter. In any instance in which suicidality was endorsed on item 9 of the CDI, a formal risk assessment was delivered by graduate students in the clinical psychology doctoral program per the clinic’s suicidal ideation protocol which involved safety planning, when appropriate. The PEERS® intervention was administered as described by the developers; details of the delivery of the PEERS® intervention can be found in (Schohl et al., 2014). In addition to generalized social skills training, PEERS® includes specific sessions focused on handling teasing and bullying (Table 2).
Table 2.
PEERS® Sessions and Associated Content
| Session Didactic | |
|---|---|
| 1 | Introduction and Conversational Skills I: Trading Information |
| 2 | Conversational Skills II: Two-Way Conversations |
| 3 | Conversational Skills III: Electronic Communication |
| 4 | Choosing Appropriate Friends |
| 5 | Appropriate Use of Humor |
| 6 | Peer Entry I: Entering a Conversation |
| 7 | Peer Entry II: Exiting a Conversation |
| 8 | Get-Togethers |
| 9 | Good Sportsmanship |
| 10 | Rejection I: Teasing and Embarrassing Feedback |
| 11 | Rejection II: Bullying and Bad Reputations |
| 12 | Handling Disagreements |
| 13 | Rumors and Gossip |
| 14 | Graduation and Termination |
Reprinted with permission of the authors.
Measures
The Children’s Depression Inventory (CDI; Kovacs, 1992) is a 27-item self-report questionnaire commonly used to assess depressive symptoms among youth ages 7 to 17 and has good reliability and validity in clinical (Carey, Faulstich, Gresham, Ruggiero, & Enyart, 1987) and non-clinical samples (Smucker, Craighead, Craighead, & Green, 1986). The CDI has been used previously with ASD samples (e.g., Lerner, Calhoun, Mikami, & De Los Reyes, 2012; Solomon, Miller, Taylor, Hinshaw, & Carter, 2012; Vickerstaff et al., 2007) and has shown evidence of promising psychometric properties in an ASD sample (Ozsivadjian, Hibberd, & Hollocks, 2014). Further, it has demonstrated sensitivity to treatment response in both ASD (Solomon, Goodlin-Jones, & Anders, 2004) and non-ASD samples (Pössel, Martin, Garber, & Hautzinger, 2013; Weisz, Thurber, Sweeney, Proffitt, & LeGagnoux, 1997). This measure yields a Total Score and the following subscale scores: Negative Mood (example item: “I am sad once in a while, many times, or all the time.”), Interpersonal Problems (example item: “I get along with people, I get into fights many times, or I get into fights all the time.”), Ineffectiveness (example item: “I can never be as good as other kids, I can be as good as other kids if I want to, or I am just as good as other kids.”), Anhedonia (example item: “I have fun in many things, some things, or nothing is fun at all.”), and Negative Self-Esteem (example item: “Nothing will ever work out for me, I am not sure if things will work out for me, or things will work out for me O.K.”). Suicidal ideation is reported on question 9 of the CDI that states: “‘I do not think of killing myself,’ ‘I think of killing myself but I would not do it,’ or ‘I want to kill myself.’” T-scores on the CDI were used in all analyses. Internal consistency for the present study was acceptable at pretest (α = 0.79) and good at posttest (α = 0.82), comparable to previous reports of internal consistency of self-report on the measure in an ASD sample (Ozsivadjian et al., 2014).
The Quality of Socialization Questionnaire (QSQ) is a 12-item parent-reported measure used to assess direct socialization via get-togethers (Laugeson & Frankel, 2011), developed as an upward adaptation of the Quality of Play Questionnaire (QPQ; Frankel et al., 2010). Following the procedure used in previous research (McVey et al., 2016; Schohl et al., 2014), the total number of get-togethers was identified by creating a composite score of the responses on the following two questions: “How many get-togethers did your child organize in the last month?” and “How many get-togethers was your child invited to last month?”. Given that only two items were included from this questionnaire, the psychometric properties were not evaluated for the purposes of the present study.
Results
SPSS version 24.0 was used to run all analyses (IBM Corp, 2016). Data on the CDI was missing for six participants in the EXP group and four participants in the WL group (Figure 1: CONSORT Diagram), and thus these participants were not included in analyses. Data were screened for normality and outliers. One data point for CDI Interpersonal Problems at pretest was Winsorized to the next highest value (84 to 75; Tabachnick & Fidell, 2013). Data on the QSQ were not normally distributed, therefore, non-parametric analyses were employed for analyses involving QSQ variables. Both IQ and age were unrelated to scores on the CDI (p’s > 0.05), and, thus, were not included as covariates in the following analyses. Repeated-measures ANOVAs were run to investigate change in the CDI Total Score and subscale scores across time for the EXP and WL groups. Paired samples t-tests were used as follow-up analyses to further probe Time by Group interactions and as exploratory analyses for non-significant interactions. Spearman’s correlations were employed to investigate associations between reported quantity of direct peer interactions via get-togethers and CDI scores. Lastly, endorsement of the CDI item reflecting suicidal ideation was examined at pretest and posttest.
Effect of PEERS® on CDI Scores
For the CDI Total Score, the main effect of Group was non-significant (F(1, 41) = 2.98, p = 0.09, partial η2 = 0.07). The main effect of Time was significant (F(1,41) = 8.11, p = 0.01, partial η2 = 0.16) and was further qualified by a significant Group by Time interaction (F(1,41) = 6.49, p = 0.01, partial η2 = 0.14). Paired samples t-tests revealed that the CDI scores for the EXP group significantly decreased across intervention (t(20) = 4.04, p = 0.001), while the WL group’s scores did not significantly change from pretest to posttest (t(21) = 0.20, p = 0.84) (Table 3).
Table 3.
CDI Scores for the EXP and WL Groups at Pretest and Posttest
| EXP | WL | |||||||
|---|---|---|---|---|---|---|---|---|
| Pretest | Posttest | Pretest | Posttest | |||||
| CDI Measures | M (SD) |
Range | M (SD) |
Range | M (SD) |
Range | M (SD) |
Range |
| Totala | 48.78 (8.18) |
37 – 68 | 43.05 (5.52) |
35 – 53 | 49.73 (8.46) |
36 – 66 | 49.41 (8.47) |
37 – 64 |
| Negative Mooda | 48.17 (8.27) |
36 – 66 | 42.42 (6.05) |
36 – 57 | 52.08 (9.10) |
39 – 80 | 49.08 (9.02) |
36 – 70 |
| Interpersonal Problems | 48.78 (9.35) |
42 – 75 | 46.74 (5.31) |
42 – 57 | 51.92 (8.47) |
42 – 74 | 50.33 (6.29) |
42 – 64 |
| Ineffectivenessc | 49.17 (6.96) |
39 – 64 | 46.26 (6.95) |
38 – 59 | 40.17 (10.46) |
38 – 70 | 48.87 (8.38) |
38 – 64 |
| Anhedoniaa | 50.61 (9.23) |
37 – 71 | 45.96 (7.65) |
37 – 60 | 50.71 (9.24) |
37 – 71 | 51.46 (8.94) |
37 – 71 |
| Negative Self-Esteemc | 46.87 (6.71) |
39 – 65 | 44.08 (4.72) |
39 – 55 | 45.67 (5.93) |
39 – 60 | 46.83 (6.58) |
40 – 60 |
Significant (p < 0.05) change from pretest to posttest for the EXP Group.
Significant (p < 0.05) change from pre- to posttest for the WL Group.
Marginally significant (p < 0.10) change from pre- to posttest for the EXP Group.
Marginally significant (p < 0.10) change from pre- to posttest for the WL Group. CDI – Children’s Depression Inventory. EXP – Experimental Group. WL – Waitlist Control Group.
For the Negative Mood subscale, the main effects of Time (F(1,45) = 10.37, p < 0.01, partial η2 = 0.19) and Group (F(1,45) = 7.26, p = 0.01, partial η2 = 0.14) were significant. The Group by Time interaction was non-significant (F(1,45) = 1.02, p = 0.32, partial η2 = 0.02). Planned analyses via paired-samples t-tests, however, revealed that scores on the Negative Mood subscale significantly decreased across intervention for the EXP group (t(23) = 3.80, p = 0.001), while there was no such change for the WL group (t(22) = 1.31, p = 0.33) (Table 3).
For the Interpersonal Problems subscale, the main effects of Time (F(1,45) = 2.18, p = 0.15, partial η2 = 0.05) and Group (F(1,45) = 3.40, p = 0.07, partial η2 = 0.07) were non-significant, as was the interaction between Time and Group (F(1,45) = 0.03, p = 0.85, partial η2 = 0.001). Planned analyses via paired-samples t-tests similarly revealed that neither the EXP (t(22) = 1.110 p = 0.28) nor the WL group (t(23) = .98, p = 0.33) changed significantly across time on the Interpersonal Problems subscale (Table 3).
For the Ineffectiveness subscale, the main effects of Time (F(1,45) = 1.40, p = 0.23, partial η2 = 0.03) and Group (F(1,45) = 0.41, p = 0.52, partial η2 = 0.01) were non-significant, as was the interaction between Time and Group (F(1,45) = 0.94, p = 0.34, partial η2 = 0.02). Planned analyses via paired-samples t-tests, however, revealed that the Ineffectiveness subscale had a marginally-significant decrease across intervention for the EXP group (t(22) = 2.05, p = 0.052), while there was no significant change for the WL group (t(23) = 0.13, p = 0.90) (Table 3).
For the Anhedonia subscale, the main effects of Time (F(1,45) = 2.55, p = 0.12, partial η2 = 0.05) and Group (F(1,45) = 1.54, p = 0.22, partial η2 = 0.03) were non-significant, but the Group by Time interaction was significant (F(1,45) = 4.88, p = 0.03, partial η2 = 0.10). Paired-samples t-tests revealed that scores on the Anhedonia subscale significantly decreased across intervention for the EXP group (t(22) = 2.59, p = 0.02), while there was no such change for the WL group (t(23) = −0.45, p = 0.65) (Table 3).
For the Negative Self-Esteem subscale, the main effects of Time (F(1,46) = 0.73, p = 0.40, partial η2 = 0.02) and Group (F(1,46) = 0.28, p = 0.60, partial η2 = 0.01) were non-significant, but the Group by Time interaction was significant (F(1,46) = 4.32, p = 0.04, partial η2 = 0.09). Paired-samples t-tests revealed that the Ineffectiveness subscale had a marginally-significant decrease across intervention for the EXP group (t(23) = 1.93, p = 0.06), while there was no such change for the WL group (t(23) = −0.94, p = 0.36) (Table 3).
Relation Between the QSQ and CDI Scores
Multiple negative associations emerged between parent-reported number of get-togethers on the QSQ (M = 2.54, SD = 2.95, Range = 0 to 14) and self-report of depression on the CDI at posttest. These included the Total Score (rs(44) = −0.46, p < 0.01) as well as subscales of Negative Mood (rs(46) = −0.28, p = 0.06), Interpersonal Problems (rs(47) = −0.32, p = 0.03), Ineffectiveness (rs(46) = −0.38, p = 0.01), Anhedonia (rs(46) = −0.42, p < 0.01), and Negative Self-Esteem (rs(47) = −0.27, p = 0.06).
Endorsement of Suicidal Ideation at Pretest and Posttest
All endorsement of suicidal ideation in this sample was reported at the midlevel (i.e., “I think of killing myself but would not do it”). In the EXP group, 19% (n = 4) endorsed the midlevel of suicidal ideation at pretest, while 0% endorsed any level of suicidal ideation at posttest. In the WL group, however, 18% (n = 3) endorsed the midlevel of suicidal ideation at pretest and this increased to 30% (n = 5) at posttest. Of the five participants who endorsed suicidal ideation at posttest in the WL group, two had also endorsed at pretest, while three changed from not endorsing to endorsing across time.
Discussion
Findings from the current study provide support for the notion that social interactions and co-occurring difficulties, specifically depressive symptoms, are intimately intertwined for individuals with ASD. Therefore, bolstering social skills among youth with ASD seems to influence other domains of functioning, including mental health.
In this study, PEERS® functioned to reduce self-reported depressive symptoms, which is in line with the hypotheses. Subscales of the CDI including: Negative Mood, Ineffectiveness, Anhedonia, and Negative Self-Esteem demonstrated significant or marginally significant decreases in the experimental group after receiving PEERS®, while the waitlist control group showed no significant change. The Interpersonal Problems subscale, however, did not significantly decrease in the experimental group. This null finding is surprising, as PEERS® specifically targets social and interpersonal skills. It may be that the effects of PEERS® on interpersonal challenges, as measured by the CDI, is delayed; perhaps this domain of depression is less malleable and requires a longer duration of repeated social interactions to elicit change. This is merely speculation, however, as the data from the present study did not allow for the direct testing of this hypothesis. Therefore, this possibility requires direct investigation, namely via longer-term study following intervention (i.e., months or years later). As mentioned previously, although some literature exists, only a handful of studies have examined treatment response employing CDI subscales (e.g., Bursuk, 1998; Nolan et al., 2002). Additionally, the items of the Interpersonal Skills subscale may be a limiting factor; the items do not necessarily tap into social skills per se but, rather, a desire to be with others and to obey directions from other people.
As hypothesized, there were strong negative associations between the reported number of direct peer interactions and depressive symptoms, such that those with greater numbers of peer interactions reported fewer depressive symptoms. This association was found across all subscales of the CDI, suggesting that interactions with peers during get-togethers may be protective against the experience of multiple dimensions of depressive symptoms in ASD. Causality cannot be inferred from this data, however; it might be that adolescents with fewer symptoms of depression are more likely to initiate social engagement and, in turn, spend more time with peers.
Although exploratory in nature, the data for the suicidal ideation item on the CDI revealed important changes across time. For those who received PEERS® in the experimental group, suicidal ideation decreased, such that there was no evidence for suicidal ideation at posttest. Equally as important is the increase in the number of participants in the waitlist group who endorsed suicidal ideation across time. This finding highlights the importance of bolstering social skills among youth with ASD during adolescence. It also suggests that, in the future, youth in the waitlist group should be evaluated following the completion of PEERS® for suicidal ideation and, perhaps, emphasis should be placed on coordinating care with a primary doctor, psychologist, and/or psychiatrist throughout wait period, especially when suicidal ideation is endorsed at pretest.
Although not directly examined here, the decreases in depressive symptoms after PEERS® may be rooted in multiple mechanisms of change. It might be that providing the skills necessary to facilitate friendships and succeed in social situations bolsters self-confidence to approach new social situations. If such social interactions are indeed successful, this may foster friendships, in turn, ameliorating loneliness, isolation, and ultimately lessening symptoms of depression. Another possibility is that increased social abilities may lead to less isolation via appropriately handling, and potentially preventing, additional teasing and bullying – two areas of focus in the PEERS® intervention. Further, participation in PEERS® itself may have served as a source of support and social contact, a possibility that remains outside of the scope of the present data. Future work is needed to further investigate what might be driving the decline in depressive symptoms following a social skills intervention.
Additionally, there might be moderators of this effect, serving to facilitate or hinder the ability of a social skills intervention to impact depressive symptoms. Recently, researchers have begun to consider repetitive thinking as a key component of depressive symptoms in ASD (Gotham, 2017). Although not addressed in this study, it might be important to consider how repetitive thinking might moderate the efficacy of PEERS® on changes in depressive symptoms. Additionally, the current study was unable to examine the potential moderating impact of other services participants might have been be receiving concurrently with PEERS®, although participants are asked not to begin any new services while they are receiving the PEERS® intervention. Therefore, future work might benefit from examining the role of such concurrent services.
This study is not without its limitations. The measure of depressive symptoms utilized in this study was self-report; there are concerns in the literature regarding the ability of youth with ASD to accurately report on their emotions and feelings (e.g., Hill, Berthoz, & Frith, 2004). It would be important for future research to gather information regarding depressive symptoms from multiple informants. Additionally, the post-intervention measure of depression was collected immediately following the intervention for the experimental group, thus, it cannot be concluded from these data whether these effects are durable and would maintain, disappear, or perhaps improve well past completion of the intervention. Future research should examine depressive symptoms longitudinally following intervention in youth with ASD. As this study did not include a treatment as usual or treatment comparison group, it cannot be determined whether these findings are specific to PEERS® or whether other interventions would have similar outcomes in terms of depressive symptoms. Additionally, as the waitlist control group did not receive an alternate form of arranged group contact during their wait period, it cannot be determined what role the social interaction during PEERS® sessions might have played in the observed decrease in depressive symptoms. This is an important consideration for future randomized controlled trial study designs in ASD, especially considering the association between peer interactions and depressive symptoms. Importantly, the sample size of the present study was relatively small and homogenous in terms of race/ethnicity and family income and, thus, findings may not be generalizable to the broader ASD population.
This study provides evidence that addressing social skills challenges among adolescents with ASD can lead to improvement in other areas of functioning, specifically depressive symptoms. These findings further support the idea that challenges in the social world are linked with mental health in ASD and, thus, improving social functioning can have positive impacts that reverberate across multiple aspects of life for adolescents with ASD.
Funding:
This project was funded by the Autism Society of Southeastern Wisconsin, Marquette University, and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Numbers UL1TR001436 and KL2TR001438. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Conflict of Interest:
Hillary K. Schiltz declares that she has no conflict of interest. Alana J. McVey declares that she has no conflict of interest. Bridget K. Dolan declares that she has no conflict of interest. Kirsten S. Willar declares that she has no conflict of interest. Sheryl Pleiss declares that she has no conflict of interest. Jeffrey S. Karst declares that he has no conflict of interest. Audrey M. Carson declares that she has no conflict of interest. Christina Caiozzo declares that she has no conflict of interest. Elisabeth M. Vogt declares that she has no conflict of interest. Brianna D. Yund declares that she has no conflict of interest. Amy Vaughan Van Hecke declares that she has no conflict of interest.
References
- Armsden GC, & Greenberg MT (1987). The inventory of parent and peer attachment: Individual differences and their relationship to psychological well-being in adolescence. Journal of Youth and Adolescence, 16(5), 427–454. [DOI] [PubMed] [Google Scholar]
- Association, A. P. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub. [DOI] [PubMed] [Google Scholar]
- Bauminger N, Solomon M, Aviezer A, Heung K, Gazit L, Brown J, & Rogers SJ (2008). Children with autism and their friends: A multidimensional study of friendship in high-functioning autism spectrum disorder. Journal of Abnormal Child Psychology, 36(2), 135–150. [DOI] [PubMed] [Google Scholar]
- Bauminger N, Solomon M, & Rogers SJ (2010). Predicting friendship quality in autism spectrum disorders and typical development. Journal of Autism and Developmental Disorders, 40(6), 751–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitsika V, & Sharpley CF (2015). Differences in the prevalence, severity and symptom profiles of depression in boys and adolescents with an autism spectrum disorder versus normally developing controls. International Journal of Disability, Development and Education, 62(2), 158–167. [Google Scholar]
- Bridge JA, Goldstein TR, & Brent DA (2006). Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry, 47(3‐4), 372–394. [DOI] [PubMed] [Google Scholar]
- Bursuk LI (1998). The effects of a school-based cognitive-behavioral intervention program on the depression scores of sixth-grade students: A comparison outcome study.
- Cappadocia MC, Weiss JA, & Pepler D (2012). Bullying experiences among children and youth with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(2), 266–277. [DOI] [PubMed] [Google Scholar]
- Card NA, Isaacs J, Hodges EVE, Zins JE, Elias MJ, & Mahr CA (2007). Correlates of school victimization: Implications for prevention and intervention. Bullying, Victimization, and Peer Harassment: A Handbook of Prevention and Intervention, 339–366. [Google Scholar]
- Carey MP, Faulstich ME, Gresham FM, Ruggiero L, & Enyart P (1987). Children’s Depression Inventory: Construct and discriminant validity across clinical and nonreferred (control) populations. Journal of Consulting and Clinical Psychology, 55(5), 755. [DOI] [PubMed] [Google Scholar]
- Cassidy S, Bradley P, Robinson J, Allison C, McHugh M, & Baron-Cohen S (2014). Suicidal ideation and suicide plans or attempts in adults with Asperger’s syndrome attending a specialist diagnostic clinic: a clinical cohort study. The Lancet Psychiatry, 1(2), 142–147. [DOI] [PubMed] [Google Scholar]
- Corp I (2016). IBM SPSS Satistics for Mac. Armonk, NY: IMB Corp. [Google Scholar]
- Denissen JJA, Penke L, Schmitt DP, & Van Aken MAG (2008). Self-esteem reactions to social interactions: evidence for sociometer mechanisms across days, people, and nations. Journal of Personality and Social Psychology, 95(1), 181. [DOI] [PubMed] [Google Scholar]
- Frankel F, Myatt R, Sugar C, Whitham C, Gorospe CM, & Laugeson E (2010). A randomized controlled study of parent-assisted children’s friendship training with children having autism spectrum disorders. Journal of Autism and Developmental Disorders, 40(7), 827–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gantman A, Kapp SK, Orenski K, & Laugeson EA (2012). Social skills training for young adults with high-functioning autism spectrum disorders: A randomized controlled pilot study. Journal of Autism and Developmental Disorders, 42(6), 1094–1103. [DOI] [PubMed] [Google Scholar]
- Garner PW, & Hinton TS (2010). Emotional display rules and emotion self‐regulation: Associations with bullying and victimization in community‐based after school programs. Journal of Community & Applied Social Psychology, 20(6), 480–496. [Google Scholar]
- Gotham K (2017). Repetitive Thinking as a Pathway to Anxiety and Depression in Autism Spectrum Disorder. In Paper Symposium at Biennial Meeting of the Society for Research in Child Development. Austin, TX. [Google Scholar]
- Hall-Lande JA, Eisenberg ME, Christenson SL, & Neumark-Sztainer D (2007). Social isolation, psychological health, and protective factors in adolescence. Adolescence, 42(166), 265. [PubMed] [Google Scholar]
- Hedley D, & Young R (2006). Social comparison processes and depressive symptoms in children and adolescents with Asperger syndrome. Autism, 10(2), 139–153. [DOI] [PubMed] [Google Scholar]
- Hill E, Berthoz S, & Frith U (2004). Brief report: Cognitive processing of own emotions in individuals with autistic spectrum disorder and in their relatives. Journal of Autism and Developmental Disorders, 34(2), 229–235. [DOI] [PubMed] [Google Scholar]
- Hillier AJ, Fish T, Siegel JH, & Beversdorf DQ (2011). Social and vocational skills training reduces self-reported anxiety and depression among young adults on the autism spectrum. Journal of Developmental and Physical Disabilities, 23(3), 267–276. [Google Scholar]
- Horowitz LM, Thurm A, Farmer C, Mazefsky C, Lanzillo E, Bridge JA, … Siegel M (2017). Talking About Death or Suicide: Prevalence and Clinical Correlates in Youth with Autism Spectrum Disorder in the Psychiatric Inpatient Setting. Journal of Autism and Developmental Disorders, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphrey N, & Hebron J (2015). Bullying of children and adolescents with autism spectrum conditions: A “state of the field”review. International Journal of Inclusive Education, 19(8), 845–862. [Google Scholar]
- Humphrey N, & Lewis S (2008). Make me normal’The views and experiences of pupils on the autistic spectrum in mainstream secondary schools. Autism, 12(1), 23–46. [DOI] [PubMed] [Google Scholar]
- Humphrey N, & Symes W (2010). Responses to bullying and use of social support among pupils with autism spectrum disorders (ASDs) in mainstream schools: A qualitative study. Journal of Research in Special Educational Needs, 10(2), 82–90. [Google Scholar]
- Humphrey N, & Symes W (2011). Peer interaction patterns among adolescents with autistic spectrum disorders (ASDs) in mainstream school settings. Autism, 15(4), 397–419. [DOI] [PubMed] [Google Scholar]
- Kaufman AS (1997). KBIT-2: Kaufman Brief Intelligence Test. Minneapolis, MN: NCS Pearson. Inc. [Google Scholar]
- Kim U, & Choi S-H (1994). Individualism, collectivism, and child development: A Korean perspective. In Greenfield P & Cocking R (Eds.), Cross-cultural roots of minority child development (pp. 227–257). New York, NY: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Klein D, Kujawa A, Black S, & Pennock A (2013). Depressive Disorders. In Beauchaine T & Hinshaw S (Eds.), Child and Adolescent Psychopathology (2nd ed., pp. 543–575). New Jersey: John Wiley & Sons, Inc. [Google Scholar]
- Kovacs M (1992). Children’s depression inventory: Manual. Multi-Health Systems. [Google Scholar]
- Laugeson EA, & Frankel F (2011). Social skills for teenagers with developmental and autism spectrum disorders: The PEERS treatment manual. Routledge. [DOI] [PubMed] [Google Scholar]
- Laugeson EA, Frankel F, Gantman A, Dillon AR, & Mogil C (2012). Evidence-based social skills training for adolescents with autism spectrum disorders: The UCLA PEERS program. Journal of Autism and Developmental Disorders, 42(6), 1025–1036. [DOI] [PubMed] [Google Scholar]
- Lerner MD, Calhoun CD, Mikami AY, & De Los Reyes A (2012). Understanding parent–child social informant discrepancy in youth with high functioning autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(12), 2680–2692. [DOI] [PubMed] [Google Scholar]
- Leyfer OT, Folstein SE, Bacalman S, Davis NO, Dinh E, Morgan J, … Lainhart JE (2006). Comorbid psychiatric disorders in children with autism: interview development and rates of disorders. Journal of Autism and Developmental Disorders, 36(7), 849–861. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, … Rutter M (2000). The Autism Diagnostic Observation Schedule—Generic: A standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders, 30(3), 205–223. [PubMed] [Google Scholar]
- Magnuson KM, & Constantino JN (2011). Characterization of depression in children with autism spectrum disorders. Journal of Developmental and Behavioral Pediatrics: JDBP, 32(4), 332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malecki CK, Demaray MK, Coyle S, Geosling R, Rueger SY, & Becker LD (2015). Frequency, power differential, and intentionality and the relationship to anxiety, depression, and self-esteem for victims of bullying. In Child & Youth Care Forum (Vol. 44, pp. 115–131). Springer. [Google Scholar]
- Mayes SD, Calhoun SL, Murray MJ, Ahuja M, & Smith LA (2011). Anxiety, depression, and irritability in children with autism relative to other neuropsychiatric disorders and typical development. Research in Autism Spectrum Disorders, 5(1), 474–485. [Google Scholar]
- Mayes SD, Calhoun SL, Murray MJ, & Zahid J (2011). Variables associated with anxiety and depression in children with autism. Journal of Developmental and Physical Disabilities, 23(4), 325–337. [Google Scholar]
- Mayes SD, Gorman AA, Hillwig-Garcia J, & Syed E (2013). Suicide ideation and attempts in children with autism. Research in Autism Spectrum Disorders, 7(1), 109–119. [Google Scholar]
- Mazurek MO, & Kanne SM (2010). Friendship and internalizing symptoms among children and adolescents with ASD. Journal of Autism and Developmental Disorders, 40(12), 1512–1520. [DOI] [PubMed] [Google Scholar]
- McVey AJ, Dolan BK, Willar KS, Pleiss S, Karst JS, Casnar CL, … Van Hecke AV (2016). A Replication and Extension of the PEERS® for Young Adults Social Skills Intervention: Examining Effects on Social Skills and Social Anxiety in Young Adults with Autism Spectrum Disorder. Journal of Autism and Developmental Disorders, 46(12), 3739–3754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McVey AJ, Schiltz H, Haendel A, Dolan BK, Willar KS, Pleiss S, … Vogt E (2017). Brief Report: Does Gender Matter in Intervention for ASD? Examining the Impact of the PEERS® Social Skills Intervention on Social Behavior Among Females with ASD. Journal of Autism and Developmental Disorders, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendelson JL, Gates JA, & Lerner MD (2016). Friendship in school-age boys with autism spectrum disorders: A meta-analytic summary and developmental, process-based model. American Psychological Association. [DOI] [PubMed] [Google Scholar]
- Nolan M, Carr A, Fitzpatrick C, O’Flaherty A, Keary K, Turner R, … Tobin G (2002). A comparison of two programmes for victims of child sexual abuse: a treatment outcome study. Child Abuse Review, 11(2), 103–123. [Google Scholar]
- Ozsivadjian A, Hibberd C, & Hollocks MJ (2014). Brief report: the use of self-report measures in young people with autism spectrum disorder to access symptoms of anxiety, depression and negative thoughts. Journal of Autism and Developmental Disorders, 44(4), 969–974. [DOI] [PubMed] [Google Scholar]
- Pössel P, Martin NC, Garber J, & Hautzinger M (2013). A randomized controlled trial of a cognitive-behavioral program for the prevention of depression in adolescents compared with nonspecific and no-intervention control conditions. Journal of Counseling Psychology, 60(3), 432. [DOI] [PubMed] [Google Scholar]
- Rubin KH, Dwyer KM, Booth-LaForce C, Kim AH, Burgess KB, & Rose-Krasnor L (2004). Attachment, friendship, and psychosocial functioning in early adolescence. The Journal of Early Adolescence, 24(4), 326–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt ME, & Bagwell CL (2007). The protective role of friendships in overtly and relationally victimized boys and girls. Merrill-Palmer Quarterly, 53(3), 439–460. [Google Scholar]
- Schohl KA, Van Hecke AV, Carson AM, Dolan B, Karst J, & Stevens S (2014). A replication and extension of the PEERS intervention: examining effects on social skills and social anxiety in adolescents with autism spectrum disorders. Journal of Autism and Developmental Disorders, 44(3), 532–545. [DOI] [PubMed] [Google Scholar]
- Segers M, & Rawana J (2014). What do we know about suicidality in autism spectrum disorders? A systematic review. Autism Research, 7(4), 507–521. [DOI] [PubMed] [Google Scholar]
- Smucker MR, Craighead WE, Craighead LW, & Green BJ (1986). Normative and reliability data for the Children’s Depression Inventory. Journal of Abnormal Child Psychology, 14(1), 25–39. [DOI] [PubMed] [Google Scholar]
- Solomon M, Goodlin-Jones BL, & Anders TF (2004). A social adjustment enhancement intervention for high functioning autism, Asperger’s syndrome, and pervasive developmental disorder NOS. Journal of Autism and Developmental Disorders, 34(6), 649–668. [DOI] [PubMed] [Google Scholar]
- Solomon M, Miller M, Taylor SL, Hinshaw SP, & Carter CS (2012). Autism symptoms and internalizing psychopathology in girls and boys with autism spectrum disorders. Journal of Autism and Developmental Disorders, 42(1), 48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, & Morris AS (2001). Adolescent development. Annual Review of Psychology, 52(1), 83–110. [DOI] [PubMed] [Google Scholar]
- Storch EA, Sulkowski ML, Nadeau J, Lewin AB, Arnold EB, Mutch PJ, … Murphy TK (2013). The phenomenology and clinical correlates of suicidal thoughts and behaviors in youth with autism spectrum disorders. Journal of Autism and Developmental Disorders, 43(10), 2450–2459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, & Fidell LS (2013). Using Multivariate Statistics (6th ed.). [Google Scholar]
- Van der Wal MF, De Wit CAM, & Hirasing RA (2003). Psychosocial health among young victims and offenders of direct and indirect bullying. Pediatrics, 111(6), 1312–1317. [DOI] [PubMed] [Google Scholar]
- Vickerstaff S, Heriot S, Wong M, Lopes A, & Dossetor D (2007). Intellectual ability, self-perceived social competence, and depressive symptomatology in children with high-functioning autistic spectrum disorders. Journal of Autism and Developmental Disorders, 37(9), 1647–1664. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Thurber CA, Sweeney L, Proffitt VD, & LeGagnoux GL (1997). Brief treatment of mild-to-moderate child depression using primary and secondary control enhancement training. Journal of Consulting and Clinical Psychology, 65(4), 703. [DOI] [PubMed] [Google Scholar]
- Whitehouse AJO, Durkin K, Jaquet E, & Ziatas K (2009). Friendship, loneliness and depression in adolescents with Asperger’s Syndrome. Journal of Adolescence, 32(2), 309–322. [DOI] [PubMed] [Google Scholar]
- Yoo H, Bahn G, Cho I, Kim E, Kim J, Min J, … Bong G (2014). A Randomized Controlled Trial of the Korean Version of the PEERS® Parent‐Assisted Social Skills Training Program for Teens With ASD. Autism Research, 7(1), 145–161. [DOI] [PubMed] [Google Scholar]
- Zeedyk SM, Rodriguez G, Tipton LA, Baker BL, & Blacher J (2014). Bullying of youth with autism spectrum disorder, intellectual disability, or typical development: victim and parent perspectives. Research in Autism Spectrum Disorders, 8(9), 1173–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]


