Abstract
Objective
To evaluate the feasibility, acceptability, and preliminary efficacy of a stepped-care parenting program implemented during COVID-19 among families of behaviorally at-risk children with neurological or neurodevelopmental disorders aged 3–9 years.
Methods
Stepped-care I-InTERACT-North increased psychological support across 3 steps, matched to family needs: (1) guided self-help (podcast), (2) brief support, and (3) longer-term parent support. The intervention was provided by clinicians at The Hospital for Sick Children. Recruitment occurred via hospital and research cohort referral. A single-arm trial using a pragmatic prospective pre–post mixed-method design was utilized to assess accrual, engagement, acceptability, and preliminary efficacy.
Results
Over 15 months, 68 families enrolled (83% consent rate) and 56 families completed stepped-care (Step 1 = 56; Step 2 = 39; Step 3 = 28), with high adherence across Steps (100%, 98%, and 93%, respectively). Parents reported high acceptability, reflected in themes surrounding accessibility, comprehension, effectiveness, and targeted care. Positive parenting skill increases were documented, and robust improvement in child behavior problems was apparent upon Step 3 completion (p =.001, d = .390). Stepped-care was as effective as traditional delivery, while improving consent and completion rates within a pandemic context.
Conclusions
This stepped-care telepsychology parenting program provides a compelling intervention model to address significant gaps in accessible mental health intervention while simultaneously balancing the need for efficient service. Findings inform program scalability beyond COVID-19 and emphasize the value of stepped-care intervention in delivering and monitoring mental health treatment.
Keywords: child behavior, COVID-19, early brain injury, mental health, neurodevelopmental, parenting, stepped-care, telepsychology
Introduction
The COVID-19 pandemic both magnified and added to the crisis of mental health service access, and accentuated the importance of improving service models. Globally, the pandemic created considerable disruption in the lives of children and caregivers, with evidence that children and youth with pre-existing mental health diagnoses were at disproportionate risk for deterioration (Bentenuto et al., 2021; Cost et al., 2022). Children susceptible to emotional dysregulation and behavioral challenges were especially impacted by reduced structure in routine, suspension in services, and increased parental stress associated with COVID-19 (Stark et al., 2020; Williams, Deotto, et al., 2022). Rates of mental health decline during COVID-19 were highest in children with Attention Deficit Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD) (Bentenuto et al., 2021; Cost et al., 2022; Nonweiler et al., 2020; Zhang et al., 2020), and children with early brain injury and their families also represented a vulnerable group (Ransom et al., 2022; Williams, Deotto, et al., 2022).
The pandemic’s shadow is likely to cast long and more profoundly among children with neurological and neurodevelopmental conditions and their families. Higher incidence of tantrums, noncompliance, and oppositionality have been well documented across pediatric acquired brain injury populations, including children with a history of stroke, traumatic brain injury, prematurity, and epilepsy (Donders & Hunter, 2018; Hayes et al., 2018; Narad et al., 2019; Spittle et al., 2009). Children with neurodevelopmental disabilities are also at known emotional and behavioral risk, which can lead to significant disruption in family relationships, social functioning, and academic achievement (Carter Leno et al., 2021; Shephard et al., 2019). Families with pre-pandemic medical and psychological challenges were likely to experience further deterioration given the added parenting responsibilities of childcare and homeschooling during COVID-19, with simultaneous reduction in external social support (Stark et al., 2020; Williams, Deotto, et al., 2022). Indeed, disruption to academic learning, normative social experiences, and therapeutic services are predicted to have long-term consequences on vulnerable children (Colvin et al., 2022) and underscores the need for accessible and tailored interventions.
The importance of providing psychological support during the pandemic and its recovery period is well-established (Racine et al., 2020; Schwartz et al., 2021), yet there is a dearth of evidenced-based, personalized, and accessible mental health interventions that are adeptly suited for children with neurological or neurodevelopmental risk. Given the strong relationship between parenting sensitivity and child psychosocial outcomes, programs that optimize parent mental health and positive parenting strategies represent promising methods of intervention for child behavior (Lieneman et al., 2017; Wiggins et al., 2009). Existing programs provide practical strategies for child behavior management, but do not incorporate psychoeducation or content that addresses the varied impacts of brain injury, condition, or neurodevelopment on child functioning. Access is also a concern, as there are currently few pathways to early parenting support in tertiary care environments. Currently, there is no formal, evidence-based family treatment for children with early serious medical conditions at our tertiary-care institution or other local hospitals/clinics, and parents are eager for ways to enhance their child’s wellbeing (Vyas et al., 2021; Williams et al., 2018). Across pediatric clinical care centers, families of children with complex medical histories report major gaps in services that meet their child’s emotional and behavioral needs (McKevitt et al., 2019; Soufi et al., 2017).
Importantly, and often overlooked, is the fact that common intervention implementation efforts require appropriate matching to needs of families, and sensitivity to the reality of placing another demand on already stressed parents. Widely used interventions are often time-intensive, require commitment to set 9–5 schedules and are not individualized to family needs (Kennedy et al., 2021; Vyas et al., 2021). In the current pandemic, stepped-care services—offering the most effective, least resource-intense treatment, and then stepping-up to more resource-heavy treatment as needed—offered a particularly relevant solution to consider (Bower & Gilbody, 2005; Holmes et al., 2020). Informed by patient-oriented approaches, stepped-care models can enhance service effectiveness and user satisfaction through collaborative assessment of therapeutic need and decision making regarding higher intensity service (Campbell et al., 2019; Clark et al., 2018).
I-InTERACT-North: A Telepsychology Parenting Intervention for Child Behavior
Internet-based, virtual treatments established before COVID-19, such as I-InTERACT-North (Internet based-Interacting Together Everyday, Recovery After Childhood Traumatic brain injury-Canadian adaptation), are particularly well-suited for transition into stepped-care delivery due to the adaptable intensity of online content and therapist engagement in addition to the attractiveness of virtual care delivery during a time of social restrictions (Burek et al., 2021; Ford et al., 2023; Wade et al., 2017). The program involves 7 online learning modules each accompanied by 1:1 parent-coaching sessions provided in the family’s home by videoconferencing (Burek et al., 2021). I-InTERACT-North was designed to treat emotional and behavior regulation challenges in early-to-mid-childhood (ages 3–9 years) by utilizing common concepts from parent training programs that foster parental warmth and responsivity through play as well as parenting consistency and predictability in the home (Eyberg, 1988; Lieneman et al., 2017; Webster-Stratton, 1999; Wiggins et al., 2009). These components have longstanding evidence of effectiveness in optimizing child behavior and reducing parental distress (Jones et al., 2008).
I-InTERACT-North was adapted from the program I-InTERACT Express from Cincinnati Children’s Hospital Medical Center (Wade et al., 2017), which was designed for pediatric traumatic brain injury patients and their families. I-InTERACT-North expanded psychoeducational components to include children with a wide variety of developmental, congenital, and neonatal conditions impacting brain function and behavior (i.e., ADHD, ASD, neonatal stroke, hypoxic ischemic encephalopathy, congenital heart disease, epilepsy, and prematurity). The transdiagnostic focus allowed I-InTERACT-North to be offered to a wide range of Canadian families; the program highlighted the varied impacts of brain injury or condition on neurodevelopment, while continuing to leverage the telepsychology and modular format of the original program (Antonini et al., 2014; Wade et al., 2017).
Transitioning to Stepped-Care I-InTERACT-North
During the first year of COVID-19, our group completed an open-label pilot feasibility trial of the transdiagnostic I-InTERACT-North program at The Hospital for Sick Children among families following neonatal medical illness/brain injury with high acceptability and preliminary indices of improvement in child behavior and parent stress (Williams, Burek, et al., 2022). However, an elevated rate of program non-completion was noted due to withdrawal prior to starting the intervention (18% of participants) and drop-out prior to finishing the full intervention (27% of participants). Barriers reported by families included parental burnout and competing time demands. This was especially true during periods of heightened restrictions (i.e., increased public health measures and extensive closures), where families reported poor daily structure in routine and inadequate emotional bandwidth to partake in interventions. Following feedback from parent participants and program therapists, in 2021 our group transitioned the program into a stepped-care approach, Stepped-Care I-InTERACT-North.
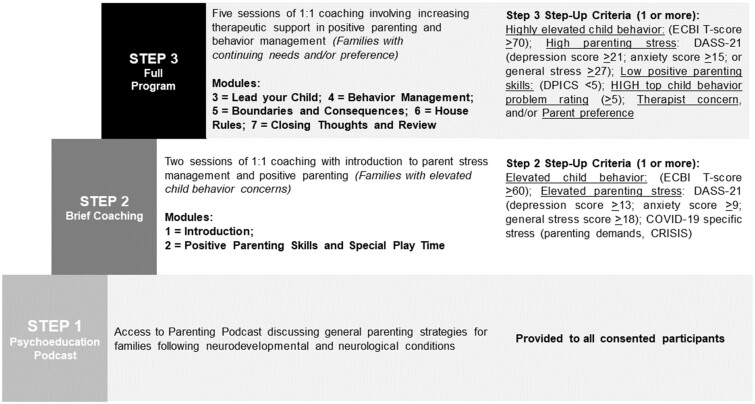
As shown in Figure 1, the I-InTERACT-North program was adapted into stepped-care following the Bower and Gilbody (2005) stepped-care model, which recommends that interventions be divided into stages of “briefer minimal interventions” that progress from the “least restrictive” option (usually encompassing guided self-help) to a stage of brief intervention, and then to a final step that provides maximal therapeutic resources (Bower & Gilbody, 2005, p. 11). A 3-step model was also recommended by our family advisory committee to address variability in service needs, time availability, and emotional resources amongst families. Committee members consisted of parents who had previously participated in the I-InTERACT-North intervention.
Figure 1.
Model of Stepped-Care I-InTERACT-North.
The 3 steps included: (1) guided self-help, (2) brief parent support, and (3) longer-term parent support for families with increased concerns. Our initial step included a 30-min podcast discussing parenting strategies during times of stress with specific reference to the pandemic context (i.e., balancing work from home, remote schooling, etc.). The podcast was recommended by our family advisory committee due to its accessible format. In Step 2, parents completed 2 online learning modules and two 1:1 virtual sessions with a therapist, which introduced positive parenting and Special Play Time with initial coaching in parent–child play interactions. Step 3 provided families with 5 additional online learning modules and 1:1 virtual coaching sessions with the same therapist. Later sessions presented more complex behavior management strategies, such as implementation of rules and consequences in the home and community, as well as additional practice and coaching to consolidate positive parenting skills. All sessions considered COVID-19 specific concerns, such as methods to optimize consistency, assisting parenting in setting up child-focused routines, and promotion of parent mental health. Figure 1 highlights stepped-care criteria for progressing to Steps 2 and 3.
The specific objectives of the current study included: (1) To determine the feasibility and adherence of Stepped-Care I-InTERACT-North during COVID-19, as assessed by accrual, refusal, dropout rates, and participation (i.e., step completion data) among eligible parents of children with pre-existing neurological or neurodevelopmental risk. (2) To investigate stepped-care acceptability during COVID-19 from the perspectives of parent participants. (3) To examine preliminary efficacy in changes in positive parenting skills and child behavior. (4) To compare the feasibility, adherence, and preliminary efficacy of Stepped-Care I-InTERACT-North during COVID-19 to data from our full-length I-InTERACT-North program administered during the first year of the pandemic.
Criteria for implementation success was based on prior studies, with accrual rates ≥65%, attrition rates ≤20%, adherence rates ≥75%, and minimal missing questionnaire data. With respect to qualitative content surrounding acceptability, we anticipated themes surrounding flexible, personalized, accessible, and effective care. Using intent-to-treat analyses, we hypothesized that there would be a significant decrease in child behavior problems and intensity. In comparison to our prior pilot, it was expected that stepped-care implementation would allow for higher rates of program engagement and completion due to the unique format and introduction of pandemic-specific therapeutic content.
Materials and Methods
Participants
Human subjects and institutional research ethics board (REB) approval was granted by The Hospital for Sick Children (REB #1000072960). Data collection took place between January 2021 and March 2022, a length of time encompassing changing public health mandates and varying periods of service closures. Provincial shutdowns spanned from January—February 2021 and then again from April to June 2021. Recruitment included (1) Clinical Referral: Pediatric patients from The Hospital for Sick Children with early brain injury, associated medical conditions, and/or ADHD who were referred to the program due to behavioral or emotional concerns by their health care provider and (2) Clinical Research Cohort Referral: A neurodevelopmental research cohort of children diagnosed with ADHD and/or ASD from the Province of Ontario Neurodevelopmental Disorders (POND) Network, a research cohort of over 3000 children with neurodevelopmental conditions associated with behavioral and emotional regulation difficulties. POND recruitment occurred across 4 Ontario centers: Holland Bloorview, SickKids, University of Western Ontario, and Queen’s University. Eligible parents were contacted and, if interested, research coordinators provided the research team the family’s contact information. Exclusion criteria consisted of: (a) Child was outside of program age-range (<3 or >9 years); (b) Family took part in prior I-InTERACT-North pilot studies or were participating in an equivalent family/parent therapy program; or (c) Major medical issues requiring ongoing inpatient care. Although interpreter services were available, all parents referred to this study were able to read and speak English. Comparative feasibility data included 2 previous recruitment phases of non-stepped-care program implementation completed during the first year of COVID-19 (Williams, Burek, et al., 2022) and pre-COVID-19 (Burek et al., 2021).
Intervention Procedure
Parents were contacted by phone by a research coordinator to discuss the study and were provided the opportunity to ask questions. If verbal consent was obtained, parents were sent electronic copies of the consent documentation and baseline questionnaires on REDCap (Research Electronic Data Capture). Participants were subsequently connected with a therapist to begin scheduling session appointments. Each participant proceeded on their own timeline, with the goal of scheduling sessions on a weekly or biweekly basis. Participants received a $25 Amazon e-gift card for completion of study measures at baseline and immediately post-intervention. Study participation took place in families’ homes through website access to podcast, online learning modules, and coaching sessions via videoconferencing. The online parenting modules were each approximately 30 min in length (https://i-interact.aboutkidshealth.ca/) and were followed by live, manualized videoconference sessions (1 hr of coaching per module) to individualize content and provide therapist-led coaching. Modules were completed independently by parents. Therapists offered flexibility in the timing of coaching sessions, including evening and weekend availability. Program therapists were doctoral students, post-doctoral fellows, and licensed clinical neuropsychologists. All underwent 12 hrs of formal training and subsequent individual and group supervision as described in Burek et al. (2021), along with 1 senior supervising clinical neuropsychologist (T.S.W.) with 4 years of program experience. Potential adverse events were monitored and mitigated through critical incident reporting forms and regular safety monitoring reviews. No safety issues or adverse events were identified during this study. The study authors followed the CONSORT/TREND checklist outlined by the Journal of Pediatric Psychology, which is available for review in Supplementary File 1.
Stepped-Care Referral Protocol
Following completion of baseline questionnaires, all consenting participants were provided with Step 1 of Stepped-Care I-InTERACT-North (podcast). The research team was informed of podcast completion when families completed 4 post-podcast questions that were provided online. Items included multiple-choice questions that quizzed podcast content along with open-ended parent feedback regarding the podcast. As outlined in Figure 1, families with elevated baseline levels of concern in child behavior, parent mental health, and/or COVID-19 specific stress were invited to participate in Step 2. Criteria for progressing to Step 3 were based on highly elevated baseline levels of concern in child behavior and/or parent mental health, in addition to indicators of therapy progress (i.e., in-session demonstrations of parenting skills, parent ratings of top behavior problems at the end of Step 2), and collaborative discussion between parents and their therapist (see Figure 1). Thresholds were taken from previous research on critical stepped-care indicators of clinical elevation (Kennedy et al., 2021).
Measures
Clinical and Demographic Information
Prior to the intervention, a background questionnaire was completed by participants to collect basic child and parent demographic information. In keeping with newer guidelines for reporting participant demographics, country of birth and heritage culture data were collected using a self-reported open ended text box (Flanagin et al., 2021). To preserve patient confidentiality and prevent identification, heritage data were reported according to updated categories proposed by Canadian Census data and the Canadian Institutes of Health Research (CIHR). Given that persons could report more than one ethnic origin, the total number of responses were greater than the total number of participants (Statistics Canada, 2021). Medical data were collected via chart reviews for children recruited through The Hospital for Sick Children.
Feasibility and Adherence of the Stepped-Care Program During COVID-19
Feasibility of Stepped-Care I-InTERACT-North during COVID-19 was evaluated according to the number of participants who were referred, eligible, approached, and consented, as well as the rates of refusal, and reason for refusal. From a stepped-care perspective, program adherence was assessed by reporting the number of families that were referred to each program step and calculating the enrollment rates and retention/completion rates for each step, time to completion for each step, and completion of baseline and post-intervention measures. Completion rates were calculated for each step to reflect the number of participants that finished the step out of the total number that consented to begin the step. In contrast, the adherence statistic included all participants that were recommended to higher steps (e.g., due to elevation in reported behavior concerns), including those who had declined and exited the program at the prior, lower step.
Acceptability of the Stepped-Care Program During COVID-19
Parent acceptability during COVID-19 was investigated by collecting feedback on program experiences and perceptions. After the podcast (Step 1), parents were prompted to provide feedback in an open-ended text box (How did you find the podcast?). At the conclusion of Step 2 or 3 (based on participation), parents were also asked to provide written feedback on the program and suggestions for future adaptation: Please let us know what questions or concerns you have that were not addressed in the program, as well as any other feedback you have related to your overall experience.
Preliminary Program Efficacy
Positive Parenting Skills
For participants in Steps 2 and 3, positive parenting skills were assessed through systematic blind coding of recorded parent–child interactions using the Dyadic Parent–Child Interaction Coding System (DPICS) (Eyberg et al., 2004). For this study, the DPICS was used to rate positive parenting behaviors (e.g., praise, responsiveness, and reflections) demonstrated during the five minutes of parent–child play at the end of each virtual session (termed “Special Play Time”). The DPICS was designed to be used as a behavioral observation measure of intervention outcomes, pre-, mid-, and post-treatment (Eyberg et al., 2004). The manual provides coding directions on every verbalization from parent to child. DPICS reliability and validity are adequate (Robinson & Eyberg, 1981), and, in our study, the average inter-rater reliability coefficient among trained blinded coders was 0.95, with double coding occurring for 20% of the sample. To assess changes in positive parenting across program steps, parent–child interactions were DPICS coded at pre-coaching (prior to Step 2) and then during each virtual coaching session. Coders were research staff rigorously trained on coding parent–child interactions according to DPICS manual specifications. Coders were blinded to session number/step, family background, child age and condition, and behavioral concerns.
Child Behavior
The Eyberg Child Behavior Inventory (ECBI) (Eyberg & Pincus, 1999) was used to assess changes in child behavior. Parents completed the ECBI prior to beginning the program, and then again after completing the program following Step 1, 2, or 3. The ECBI is a 36-item parent-report measure that assesses the frequency and severity of a child’s current problematic behavior on a 7-point intensity scale and yes/no problem scale. The ECBI yields a total problems T score (“Is this [behavior] a problem for you?”; clinical cut-off T-score = 60) and a total intensity T score (“How often does this [behavior] occur?”; clinical cut-off T-score = 60). It was designed to be used in conjunction with therapies focusing on parent–child interactions (i.e., PCIT). Test–retest reliability on the ECBI is good (0.75 after 10 months), and appropriate internal consistency ratings have been reported (Cronbach’s α = 0.94) (Funderburk et al., 2003).
Top Problems
At the beginning and end of Step 2, parents were asked to provide in-session ratings of top child behavior problems on an 8-point Likert scale ranging from low (1) to high (8) problem severity, which informed step-up criteria for Step 3 (see Figure 1). A severity cut-off of 5 was utilized. This idiographic method of top problem measurement has demonstrated good convergent and divergent validity and is sensitive to treatment change (Kennedy, 2021).
Parent Stress and Mental Health
The Depression Anxiety and Stress Scale Short Form (DASS-21) is a 21-item self-report measure of internalizing symptoms and stress (Lovibond & Lovibond, 1996). The DASS-21 was administered to all parents at baseline and following program completion. The DASS includes 3 subscales (Depression, Anxiety, and Stress), each consisting of the sum of 7 items. This measure has strong internal consistency, adequate construct validity, and sensitivity to parent therapy (Antony et al., 1998; Lovibond & Lovibond, 1995; Norton, 2007).
Analysis
Participant characteristics were summarized and reported descriptively. The characteristics of completers versus non-completers (i.e., those that had withdrawn or were lost to follow-up) were compared inferentially through t-tests for continuous data and Chi-square tests for categorical data, and associated effect sizes were reported (i.e., Cohen’s d or Cramer’s V). Feasibility was assessed using descriptive statistics to indicate recruitment and adherence rates at each step of the program. Differences in feasibility and adherence rates between Stepped-Care and previous full-length I-InTERACT-North implementation were also assessed and reported using descriptive and inferential statistical comparisons (e.g., Chi-square for consent and completion rates). Sample size was informed by pilot study guidelines (Hertzog, 2008).
Parent text responses underwent qualitative analysis through a cross-case thematic analysis procedure (Khan & VanWynsberghe, 2008) involving thorough reading, coding, and theoretical notetaking within each participant case. During coding, sections of text were highlighted and the researchers developed shorthand labels (i.e., codes) to describe their content. Overarching themes were generated through identification of common codes and patterns across cases, and theme names utilized clear and succinct language (Braun & Clarke, 2006; Miles & Huberman, 1994). Transcriptions were analyzed separately by 2 members of the research team (A.D. and G.F.) to ensure consistency and accuracy, and only prevalent themes with high-agreement were retained and reported. Double coding occurred for 100% of acceptability data, with an inter-coder reliability coefficient of 96%.
Preliminary changes in child behavior across program steps were investigated using repeated measures intent-to-treat analysis of variance (ANOVA) tests. Program Step (1, 2, and 3) and time (pre- and post-intervention) were entered as independent variables, while the ECBI Child Behavior Problems Index or Behavior Intensity Index was entered as dependent outcome variable. An intent-to-treat ANOVA also investigated parenting changes using in-session DPICS ratings of positive parenting. Post-hoc tests consisted of individual paired t-tests. An alpha level of 0.05 was adopted and partial eta-squared (η2) and Cohen’s d effect sizes were calculated. One family did not complete post-study questionnaires, and their data was excluded from preliminary efficacy pre–post analyses. Analyses were conducted using IBM SPSS Statistics Software, Version 28.
Results
Feasibility
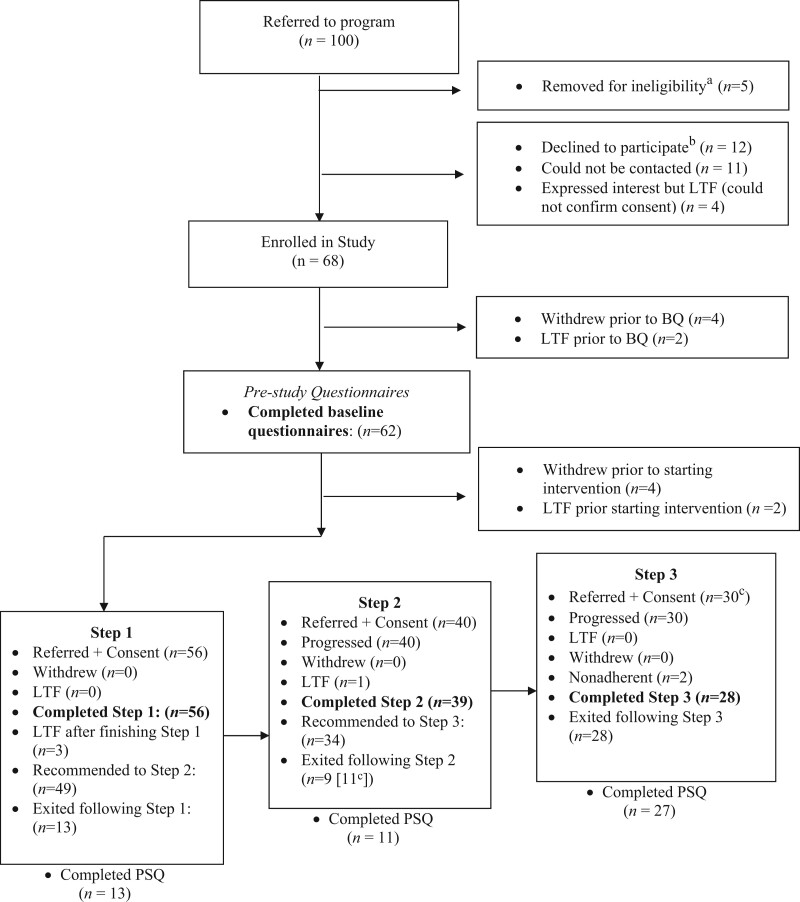
As shown in Figure 2 consort diagram, over a 15-month recruitment and follow-up phase (January 2021 to March 2022), 95 eligible families were referred to participate. Twelve eligible families declined. Fifteen families were unable to be contacted (i.e., lost to follow-up after 8 contact attempts), with 4 families having expressed interest in study enrollment before becoming lost to follow-up. In total, out of the 80 eligible families that could be contacted, 68 consented (85% consent rate) and were enrolled in the program. Child and family characteristics are summarized in Table I. Participant children had a wide range of neurological/brain injury and neurodevelopmental conditions. Among pediatric participants with early brain injury, participants with stroke experienced ischemic injury during the perinatal period with moderate to severe infarction. One child participant was born extremely premature with neonatal neuroimaging documenting reduced cortical sulcation and periventricular white matter abnormality. Participants with epilepsy had diverse etiology encompassing genetic risk factors and/or mild to moderate brain malformation (e.g., focal cortical dysplasia). As shown in Table I, there were no significant differences in family demographics or child clinical characteristics observed in program completers versus those who withdrew or were lost of follow-up. Additionally, there were no notable differences in participant demographics by step of completion, including child age, F(2, 60) = 1.09, p = .343, η2 = .035, and gender χ2(3) = 3.22, p = .359, Cramer’s V = .218. There were no statistically significant differences in baseline parent stress t(62) = 1.32, p = .193, d = 0.35, child behavior intensity t(62) = 1.38, p = .173, d = 0.37, or number of child behavior concerns, t(62) = 1.55, p = .127, d = 0.39, between the clinical patient and research cohort referral groups.
Figure 2.
Recruitment CONSORT diagram demonstrating study enrollment and adherence. Note: BQ = Background Questionnaires; LTF = lost to follow-up; PSQ = post-study questionnaires. aReasons for ineligibility: not affiliated with REB approved referral sources—Hospital for Sick Children or POND Network (n = 3); outside of the specified age-range of the study (n = 1); had competed the original version of the program (n = 1). bProvided reasons included: lack of time (n = 6), feeling overwhelmed with current commitments or pandemic uncertainties (n = 2), and lack of interest (n = 4). cTwo families referred to Step 3 did not complete all sessions due to lack of time/family circumstances, but completed post-study questionnaires. They were classified as exiting after Step 2, although non-adherent to typical stepped-care protocol.
Table I.
Family Demographics and Child Clinical Characteristics
| Program completer (n = 52 families*) | Non-completer: withdrawn (n = 4) or LTF (n = 6) | p (Cramer’s V or Cohen’s d) | |
|---|---|---|---|
| Parent participating,an (%) | |||
| Mother | 47 (90%) | 10 (100%) | .583 (.255) |
| Father | 0 (0%) | 0 (0%) | |
| Mother and father together | 5 (10%) | 0 (0%) | |
| Parent-reported heritage culture,bn (%) | Low cell count precluded analysis* | ||
| Middle Eastern (Persian, Arabic/Islam) | 4 (6%) | 2 (17%) | |
| South Asian (Indian, East Indian, Pakistan) | 2 (3%) | 0 (0%) | |
| Caribbean (African descent or West-Indian) | 3 (4%) | 0 (0%) | |
| Canadian | 19 (27%) | 4 (33%) | |
| European (French, German, Greek, Italian, Irish, Scottish) | 17 (24%) | 4 (33%) | |
| American | 2 (3%) | 0 (0%) | |
| British | 9 (13%) | 0 (0%) | |
| Chinese | 1 (1%) | 0 (0%) | |
| Hispanic | 2 (3%) | 0 (0%) | |
| Jewish | 3 (4%) | 1 (8%) | |
| Christian | 2 (3%) | 1 (8%) | |
| Prefer not to say/no response | 6 (9%) | 0 (0%) | |
| Parent current age M (SD) | |||
| Mother | 40.02 years (5.84 years) | 40.20 years (6.16 years) | .929 (.029) |
| Father | 42.68 years (6.53 years) | 43.60 years (8.97 years) | .714 (.117) |
| Parent education,cn (%) | Low cell count precluded analysis* | ||
| High school diploma or less | 6 (12%) | 1 (10%) | |
| College/university | 46 (88%) | 9 (90%) | |
| Full-time employment status,cn (%) | Low cell count precluded analysis* | ||
| Full-time | 41 (79%) | 8 (80%) | |
| Part-time | 5 (10%) | 1 (10%) | |
| Not currently employed | 6 (11%) | 1 (10%) | |
| Marital status, n (%) | Low cell count precluded analysis* | ||
| Married/living with someone | 39 (75%) | 7 (70%) | |
| Separated/divorced | 5 (10%) | 2 (20%) | |
| Other/would rather not say | 8 (15%) | 1 (10%) | |
| English as primary language, n (%) | |||
| Yes | 51 (98%) | 9 (90%) | .299 (.168) |
| Other languages spoken at home,dn (%) | |||
| Yes | 37 (71%) | 9 (90%) | .098 (.376) |
| Age of child M (SD) | 7.26 years (2.20 years) | 7.86 years (1.09 years) | .486 (.345) |
| Gender of child—males, n (%) | 43 (83%) | 8 (80%) | .593 (.046) |
| Recruitment organization, n (%) | |||
| SickKids | 17 (33%) | 3 (30%) | .591 (.021) |
| POND | 35 (67%) | 7 (70%) | |
| Child conditions, n (%) | Low cell count precluded analysis* | ||
| ADHD | 27 (39%) | 5 (46%) | |
| ASD | 28 (41%) | 3 (27%) | |
| Stroke | 3 (3%) | 0 (0%) | |
| Epilepsy/seizures | 6 (9%) | 2 (18%) | |
| Preterm birth | 1 (2%) | 0 (0%) | |
| Genetic syndromese | 4 (6%) | 1 (9%) | |
| Child behavior and parent mental health, M (SD) | |||
| Pre-ECBI intensity T score | 58.35 (8.78) | 61.00 (6.83) | .370 (.336) |
| Pre-ECBI problem T score | 60.60 (10.58) | 65.40 (9.61) | .188 (.475) |
| Pre-DASS stress score | 14.12 (10.30) | 14.30 (8.71) | .958 (.019) |
| Pre-DASS anxiety score | 5.50 (7.59) | 6.50 (5.64) | .694 (149) |
| Pre-DASS depression score | 8.35 (10.36) | 7.50 (3.24) | .800 (.111) |
All parents were biological parents.
Counts reflect the total number of endorsed cultures/heritages within and across participants, as many parents provided more than 1 classification (e.g., bi-cultural influences).
Education and employment status were based on primary income earner.
Other languages included Arabic, Farsi, French, Italian, Greek, Ukrainian, Portuguese, Spanish, Tagalog, Urdu, Yoruba, and Amharic.
Genetic syndromes co-occurred with epilepsy.
One family that completed Step 3 did not complete all post-study questionnaires.
Adherence and Completion Rates
As shown in Figure 2, of the 68 families that consented, 4 withdrew and 2 were lost to follow-up prior to completing baseline questionnaires. In total, 62 families completed baseline questionnaires (91%). An additional 4 withdrew and 2 were lost to follow-up after submitting baseline questionnaires. Of the remaining 56 participants with baseline questionnaires, all were referred to Step 1 (podcast) and 56 families completed Step 1 (100% Step 1 completion rate and adherence rate). Three families were lost to follow-up after completing Step 1. Thirteen families exited and finished the study after Step 1, expressing that their needs had been met by the podcast/low child behavioral concerns (n = 7) or lack of time to continue to more intensive steps (n = 6). Nine of the 13 families that exited following Step 1 had been recommended to continue to Step 2 due to baseline elevations. In total, 49 families were recommended to progress to Step 2.
Following completion of Step 1, 40 families met step-up criteria, were referred to Step 2, and consented to this step. Of the 40 families that began Step 2, 39 completed all components (98% completion rate). One family was lost to follow-up after the introductory meeting. Given that 49 families from Step 1 were recommended to Step 2, a Step 2 adherence rate of 80% was calculated (39 completers/49 recommended to complete Step 2). Eleven families exited and finished the study following Step 2. Specifically, 5 families that completed Step 2 did not have highly elevated concerns, were not recommended to continue, and opted to exit at this stage. Six of the families that exited following Step 2 had elevated concerns and were recommended to step-up to Step 3, but chose not to continue due to lack of time. In total, 34 families were recommended to continue to Step 3 due to highly elevated baseline questionnaires (n = 14), and/or highly rated top 3 child behavior problems (n = 34), and/or low positive parenting on DPICS (n = 12) and/or therapist concerns about parenting skills (n = 10). Thirty families consented to begin Step 3 of the intervention and 28 families completed all sessions in Step 3 (93% completion rate). Two families that progressed to Step 3 did not complete all sessions due to lack of time/family circumstance. A Step 3 adherence rate of 82% was calculated (28 completers/34 recommended to complete Step 3).
On average, it took families 30 days to complete Step 1 (i.e., the time that elapsed between study consent and post-podcast questionnaire). However, completion timed varied considerably between 2 and 113 days. Parents that took more than 1 month to complete the podcast were less likely to complete subsequent steps, despite recommendations to continue. On average, parents took 47 days to complete Step 2 and 56 additional days to complete Step 3. One family took considerably longer to complete Step 2 (122 days) and Step 3 (134 days), with data points representing a statistically significant deviation from mean completion times. Therapist notes indicated difficulties with scheduling due to family commitments and inconsistent work hours.
Across all intervention steps, 52 families completed the study (completed study at: Step 1 = 13, Step 2 = 11, Step 3 = 28) out of the 68 families that had originally consented, for a total adherence rate of 76%. Upon study completion, 51 parents completed study post-questionnaires (51/52 questionnaire completion rate). One family did not complete post-questionnaires and could not be contacted.
Comparison to Non-Stepped-Care Program Feasibility and Adherence
As shown in Table II, in comparison to 2 previous recruitment phases of non-stepped-care program implementation during the first year of COVID-19 and pre-COVID-19, more families were referred to Stepped-Care I-InTERACT-North due to inclusion of the POND Network cohort, with a higher rate of consent and enrollment. Significantly higher overall adherence and lower rates of withdrawal were documented in stepped-care implementation when compared to data from the first-year of COVID-19 (see Table II). Accounting for the addition of the podcast to the current program, completion times from enrollment to study exit were shorter, as would be expected with stepped-care.
Table II.
Comparison of Stepped-Care COVID-19 Feasibility and Adherence to Previous Full Program Implementation Pilot Data
| Stepped-care COVID-19 feasibility (current study) | COVID-19 feasibility (Williams et al., 2022) | Pre-COVID-19 feasibility (Burek et al., 2021) | |
|---|---|---|---|
| Recruitment period | 15 months | 11 months | 7 months |
| Range | January 2021–March 2022 | March 2020–January 2021 | July 2019–January 2020 |
| Referralsa | 100 | 40 | 47 |
| Eligible | 95 | 35 | 47 |
| Declined | 12 (lack of time = 6) | 4 (lack of time = 2) | 9 (lack of time = 5) |
| Requested delay | 0 (0%) | 7 (17.5%) | 0 (0%) |
| Lost to follow-up | 15 (16%) | 2 (5%) | 15 (31%) |
| Consent and enrolledb | 68 (72%) | 22 (63%) | 23 (49%) |
| Intervention completion status | |||
| Withdrew before intervention started | 8 (12%) | 4 (18%) | 1 (4%) |
| Withdrew after intervention started | 0 (0%) | 6 (27%) | 1 (4%) |
| Completed entire interventionb,c | 52 (87%) | 12 (67%) | 19 (86%) |
| Time to completion, weeks M (SD) | Step 1: 4.3 (3.7) | 10.7 (4.16) | 10.0 (3.11) |
| Step 2: 6.8 (2.7) | |||
| Step 3: 8.0 (2.2) | |||
| Steps 2 + 3 (all 7 sessions): 8.9 (6.6) |
Greater number of stepped-care referrals in comparison to past recruitment periods is due to the addition of the POND Network in referral population.
Comparative analyses were calculated for consent [χ2(2) = 7.00, p = .030] and completion rates [χ2(1) = 3.89, p = .048] using Chi-square analyses. Statistically significant differences are bolded.
Across feasibility studies, samples were comparable in parent education, heritage culture, parent participating, parent age, and child age. Due to the addition of the POND neurodevelopmental disability research cohort, participants in the current study had significantly greater males and ADHD/ASD diagnoses in comparison to past implementation samples.
Acceptability
A cross-case qualitative thematic analysis yielded 3 prominent major themes and multiple sub-themes. High parent acceptability of stepped-care was reflected in the meta-theme of Program Precision and Targeted Care. Eighteen families expressed that the stepped-care format provided flexibility and control regarding the type and amount of services received, which was effectively matched to their availability, interest, and level of concern in the pandemic context. Many parents (n = 38) reflected that the Step 1 podcast was relatable and helpful for normalizing everyday parenting worries and difficulties. A subset of parents (n = 7) expressed that the information presented was too general and that they required more personalized strategies and intervention given the complexity of their child’s behavioral problems. Qualitatively, all 7 parents that felt that the podcast was too general progressed to Step 2 to receive direct coaching. Parents who had completed Steps 2 and 3 appreciated the opportunity to continue the program (i.e., “step-up” to the next program stage) to learn new strategies and consolidate parenting skills. Regarding program precision, families conveyed that stepped-care was applicable and relevant, and program strategies could be adapted to meet the unique diagnostic needs and circumstances of their family. One parent shared: We found some things in the program (like praise and broken record) worked really well. For other lessons, like time-out, it did not work for our older child but Dr. [psychologist] helped us to come up with modifications to help with behaviors. We really appreciated her flexibility and suggestions for our unique family situation.
The meta-theme of Accessibility and Comprehension was also emergent across acceptability data. The podcast was described as having an appropriate length, understandable content, and lively dynamic between speakers, who approached the subject from experience, which made the podcast easy to follow. Parents appreciated that they could listen to the podcast while completing other activities and shared that the audio format was more interesting than a text resource. With respect to stepped-care structure, the program was consistently described as easy to follow, and 11 completers of Step 3 shared that it was helpful to review skills in a way that was systematic, organized, and progressive. Across participants that completed Steps 2 and 3, there was a recurring theme that families felt well-supported through coaching. The subtheme of Booster Sessions was also evident in 7 Step 3 completers, where participants expressed interest in follow-up sessions in order to maintain skills and obtain coaching surrounding new potential challenges that may emerge over time: I feel as though it would be a good idea to review everything and refresh with a therapist every 6 months.
Finally, acceptability surrounded the overarching theme of Program Effectiveness, which was coded 30 times and encompassed enhanced parenting confidence across program steps. Following the podcast, parents shared that the information left them feeling more normal and less anxious about their parenting struggles and home situation during the pandemic. Following Step 3, a parent shared: I feel more equipped to deal with some of the difficult behaviors our son displays. I am more confident in my ability to parent our son in a positive and consistent manner. Data regarding improvement in child behavior, enhanced child emotion regulation, and strengthening of the parent–child relationship were emergent following Step 2, but the highest saturation of these efficacy themes was present in data units from Step 3: This program was so helpful in developing a stronger, more positive relationship with our son. He is clearly a less anxious little boy. Reduction in parent stress and increased harmony within the home environment was particularly notable in acceptability content from Step 3 completers: I feel that the stress has decreased, and the joy has increased in our home. In participants that completed coaching sessions, the parent–child connection was often described in the context of “Special Play Time” and the positive impact of skills implementation through play.
Preliminary Efficacy
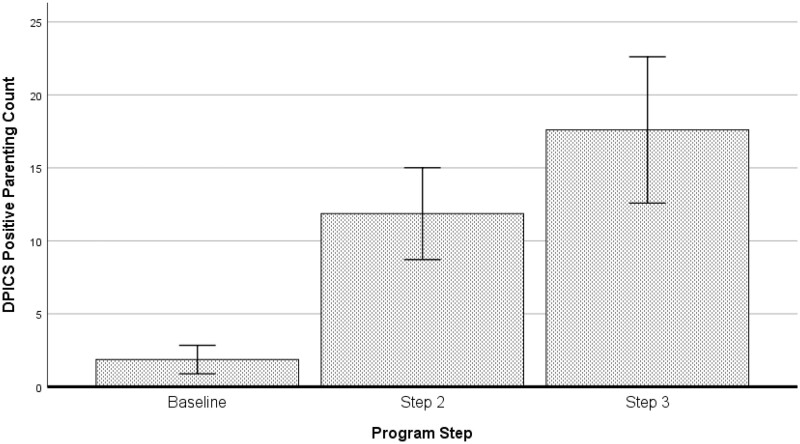
Positive Parenting Skill: Total DPICS counts of in-session positive parenting skills were analyzed for completers of Step 2 and 3, across baseline session and at the completion of Step 2 (for all), and at the completion of Step 3 (for participants completing Step 3). A significant time effect was detected, Wilk’s Lambda = 0.15, F(2, 13)=36.86, p < .001, η2 = .850, with increases in positive parenting skills across the program, M(SD): Baseline = 1.87 (1.89), Step 2 = 11.87 (6.09), Step 3 = 17.60 (9.71) (see Figure 3). Post hoc tests were significant across all comparisons (p < .041).
Figure 3.
In-session positive parenting skills across steps of program completion.
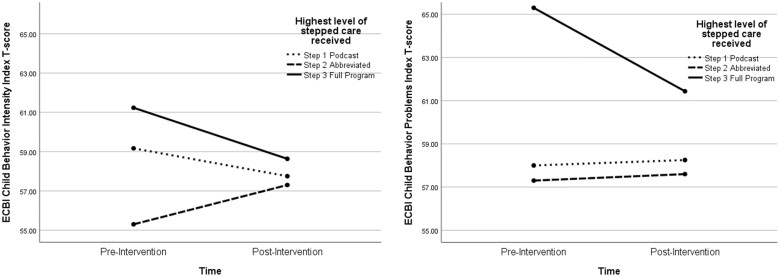
ECBI Child Behavior Problems: When pre and post ECBI Child Behavior Problems Index T-scores were entered as the dependent variable, the time by step interaction effect was non-significant, Wilk’s Lambda = 0.93, F(2, 49) = 1.94, p = .155, η2 = .073. However, the observed power to conduct the analysis was low (.38) due to small sample sizes within Steps 1 and 2. Graphical inspection of findings (see Figure 4) indicated a negative trend in Step 3 data, such that number of reported behavior problems reduced following Step 3 (Step 3: pre M = 65.30 to post M = 61.43). Mean T-scores for Steps 1 and 2 appeared stable over time. Individual paired t-tests confirmed a statistically significant decrease in child problem behavior specifically for Step 3 completers, t(29) = 3.85, p = .001, d = .390.
Figure 4.
Pre–post intervention analyses on parent-rated child behavior number and intensity according to the highest level of stepped-care completed by families. Note: Reflecting the stepped-care service model, baseline ECBI child behavior problems T-score significantly differed by program step, F(2, 61) = 3.65, p = .032, η2 = .107; Step 3 completers (M = 65.19, SD = 10.41, p = .019) reported highest baseline scores compared to completers of Step 2 (M = 56.55, SD = 7.54), and comparisons approached significance for Step 1 (M = 59.68, SD = 10.98, p = .057).
ECBI Child Behavior Intensity: When ECBI Child Behavior Intensity Index T-scores were entered as the dependent variable, the time by step interaction approached significance, Wilk’s Lambda = 0.89, F(2, 49) = 3.03, p = .058, η2 = .110, with limited observed power (.542). Graphical inspection of findings (see Figure 4) suggested a decline in behavior intensity following Steps 1 and 3, and also visually demonstrated a slight increase in behavior intensity following Step 2 completion. Individual paired t-tests confirmed significant pre–post intervention changes in child behavior intensity following Step 2 completion (Step 2: pre M = 55.30 to post M = 57.50; t(9) = 2.29, p = .049, d = .286), and Step 3 completion (Step 3: pre M = 61.23 to post M = 58.63; t(29) = 3.05, p = .005, d = .325), but did not meet significance for Step 1 (Step 1: pre M = 59.17 to post M = 57.75; t(11) = 0.89, p = .389, d = .142).
Comparison to Non-Stepped-Care Program Efficacy: Child behavior efficacy findings for Step 3 of Stepped-Care I-InTERACT-North are comparable to the efficacy of our previous pilot that reported significant decreases in child behavior problems, pre M = 65.82 (7.02) to post M = 56.72 (7.94); t(11) = 3.43, p =.006, d = 1.3, and child behavior intensity, pre M = 63.11 (6.39) to post M = 57.18 (6.38); t(11) = 3.51, p = .006, d = 0.93, after the completion of 7-sessions. Comparisons could not be made for Steps 1 and 2, given the non-stepped-care format of the previous program. It is important to note that efficacy findings from our previous pilot are based on small sample sizes (n = 12) due to lower referral numbers but also higher rates of program withdrawal.
Discussion
The current study presented the feasibility, acceptability, and initial efficacy of a pilot stepped-care parenting intervention for children with early brain injury and neurodevelopmental conditions that was offered during COVID-19. Stepped-Care I-InTERACT-North was designed to address the significant gap in accessible mental health intervention while balancing the need for efficient service provision (Bower & Gilbody, 2005). Our current study indicated high stepped-care program feasibility and acceptance amongst families of children who were at higher risk for deterioration during a time of high stress, service disruption, and poor consistency in routine.
Overall, Stepped-Care I-InTERACT-North received more referrals (augmented by partnership with an at-risk cohort) and higher rates of consent when compared to 2 previous recruitment phases of the standard program that occurred prior to and at the beginning of COVID-19. Parental fatigue and distress were exacerbated by the pandemic and impacted recruitment, consent, and adherence during standard program completion in the first year of COVID-19 (Williams, Burek, et al., 2022). Larger scale data have presented a similar picture, with reports of up to 50% decline in mental health service utilization during the pandemic, despite worsening rates of mental health concerns (Stephenson, 2021). In the stressful context of COVID-19, stepped-care implementation demonstrated improved adherence and lower rates of withdrawal, resulting in greater participant completion. In comparison to prior implementation, stepped-care completion times from enrollment to study exit were generally shorter due to the adoption of briefer interventions (i.e., Steps 1 and 2), which allowed for the matching of service length and intensity to family’s needs and availabilities. Many families expressed desire to continue the program and progressed due to elevated concerns, as reflected in the sizable number of participants that were referred to Steps 2 and 3. Our sample characteristics underscore the saliency of mental health concerns during the pandemic and likely reflect referral pathways of clinical pediatric hospital patients referred due to child behavior problems. Our second referral pathway, a cohort of children with ADHD and/or ASD, also represented a group with complex needs; indeed, children with neurodevelopmental disabilities were identified as a vulnerable group experiencing among some of the greatest rates of pandemic-related mental health decline (Bentenuto et al., 2021; Cost et al., 2022). Taken together, participants had a wide range of conditions, and findings suggest that treatment intensity thresholds within stepped-care models will be dependent upon context and population.
High program acceptability was reflected in qualitative themes derived from parent feedback on stepped-care implementation. The flexibility and control intrinsic to stepped-care methods were experienced as empowering and reassuring in the unpredictable and stress-inducing context of the pandemic, where service closures and time availability vacillated. Parents especially reflected on the advantages of targeted care and appreciated involvement in treatment decision making. Consistent with transdiagnostic stepped-care intervention guidelines (Cross & Hickie, 2017), parents conveyed that program psychoeducation and therapeutic strategies could be readily adapted to meet the unique concerns of their family. Acceptability data also converged with literature citing that stepped-care should standardize procedures with the explicit aim of enhancing efficiency (Bower & Gilbody, 2005). The program was perceived as appropriate in length, while also being comprehensive, systematic, organized, and progressive in its presentation. Finally, program effectiveness presented not only in follow-up behavioral ratings and observations but also in themes concerning enhanced parenting confidence and a stronger parent–child relationship. Efficacy thematic content was notable in Step 3 completers, who had greater therapeutic needs and, accordingly, received the most support. Post-program therapist check-ins were requested by a subset of Step 3 completers to refresh skills and troubleshoot future challenges, highlighting additional directions for future programming.
Preliminary efficacy analyses provided data trends and effect sizes that will be utilized towards the planning of future stepped-care trials. Steady increases in positive parenting skills were documented across the program. With respect to child behavior, findings were robust for Step 3 completers, where statistically significant decreases in child behavior problems and behavior intensity were observed. A significant increase in child behavior intensity was observed following the completion of Step 2 despite stability in the overall number of behavior problems. While this may seem surprising, an initial increase in behavior severity (e.g., tantrums) is often noted upon implementation of behavior principles with children (Wiggins et al., 2009). For instance, the principle of ignoring problem behavior is introduced at the conclusion of Step 2, and parents are advised that problem behavior often “gets worse before it gets better.” Decline in tantrums is typically observed later in the program due to consistency in implementing positive parenting skills (Burek et al., 2021). Results emphasize the importance of long-term follow-up, and it is predicted that reductions in child behavior would likely be observed in the months following Step 2, after parents have had the opportunity to consistently utilize behavioral conditioning principles (Schorr et al., 2020; Wade et al., 2011). Finally, higher levels of baseline child concerns for Step 3 completers may also account for the substantial decrease in reported child behavior concerns seen over time, as this group had clear treatment targets and more room for improvement.
Limitations
Several limitations must be taken into consideration when interpreting the results of this clinical trial. As noted above, the small sample size that exited the study following the completion of Step 1 or Step 2 resulted in low statistical power for the efficacy analyses. Due to high baseline concerns, many participants were recommended to complete all program steps, which resulted in a higher number of Step 3 completers than earlier steps. Future studies will need to incorporate greater variability in severity of baseline concerns within the referral population to better encapsulate intervention responses across steps, which could be of potential value for families of at-risk children who require mental health prevention services as opposed to intensive treatment. Despite our program being offered to all caregivers, mothers have represented the majority of our parent participants. The intervention attempts to balance ideal parenting practices with the reality of busy and stressed families; dual caregiver enrollment is not a requirement but is encouraged. Predominance of mothers is a common finding across many interventions, and there is evidence to suggest that reduced father enrollment may be entrenched in larger social systems that impact parental roles, such as cultural factors, gender expectations, and work schedules (Panter‐Brick et al., 2014). Anecdotally, several mothers shared that fathers participated in online module review. Going forward, we will continue to consider all of the ways in which primary caregivers engage with intervention content. Forthcoming data from our current codesign project will provide insight into ideal methods of family engagement.
The high proportion of male children in the study was reflective of the referral populations utilized, where males are more likely to be diagnosed with stroke, ADHD, autism, and externalizing problems (Fuentes et al., 2016; Ramtekkar et al., 2010; Whitlock et al., 2020). While representative of the gender divide in our target populations, we believe it is important to acknowledge potential impact on stepped-care findings. For instance, lower levels of hyperactivity and externalizing behavior sometimes seen in girls with ADHD may result in fewer female referrals or less utilization of higher program steps that provide greater intervention intensity. On a societal level, underdiagnosis of neurodevelopmental disability in girls can result in delayed access to needed therapeutic services (Young et al., 2020). Although multiple heritage cultures and linguistic backgrounds were described by participants, most of the sample identified with a Canadian and/or European background which may have reduced the generalizability of findings. Finally, in effort to reduce demands placed on participants, outcomes were assessed upon study completion. Administration of measures after each program Step would have provided additional valuable stepped-care data.
Clinical Implications and Future Directions
Our stepped-care adaptation of a telepsychology parenting program provides a compelling intervention model to address child behavior concerns while simultaneously seeking valuable efficiencies in the resources and time associated with implementation. In balance, however, the criteria and thresholds utilized for program step progression must be carefully considered to ensure appropriate fit to populations served with respect to severity of concerns, clinical presentation, and resources available to families. Results have important value for informing continued program adaptation to ensure broad application across settings and populations. Given that many participants progressed to Steps 2 and 3, consideration will need to be given to the continued inclusion of the psychoeducational podcast as an introductory step. Many families in tertiary care present with higher service needs and may benefit from direct referral into active therapeutic coaching components of I-InTERACT-North. However, as highlighted in our early pandemic research (Williams, Burek et al., 2022; Williams, Deotto et al., 2022), not all families have the emotional and/or time resources to partake in formal intervention coaching and could glean basic parenting strategies from self-led learning materials (Lal & Adair, 2014). Step 1 can also serve as a potential readiness screener to help parents determine if the program is an appropriate fit for their family. Provision of Step 1 in our care model may also be essential from a preventative perspective if Stepped-Care I-InTERACT-North were to be adopted in settings where behavioral concerns could potentially be milder (e.g., primary care or school care).
Our team is now actively working with families and community stakeholders to codesign clinical implementation pathways for scalability. Ongoing feedback considers the utility of psychoeducation for broad populations and options for adopting technology that would reduce stepped-care administrative burden. Our family advisory committee continues to play a key role in optimizing outcome assessment by providing active consultation on the selection of questionnaires that are practical, succinct, meaningful, and program-consistent. Close monitoring of program fidelity remains essential to preserve core intervention components, even when scaling-up delivery across diverse clinics. Our program continues to capitalize on the unique role of neuropsychologists, with increasing accountability in advocacy and service for families with mental health risk. It should be noted that although Stepped-Care I-InTERACT-North is a hospital-centerd intervention, our clinical stakeholders and family advisors have continually emphasized the importance of generalizing to community settings. Involving local health care providers in program implementation and continued co-design will be essential to engaging diverse families, upholding established and trusted therapeutic relationships in the community, and ensuring adaptability to family backgrounds, perspectives, and service needs.
Taken together, data from the current study suggests that stepped-care can provide a successful system of empowering families to be involved within their own treatment-course, while being at least as effective as traditional methods. Future directions following this feasibility trial include incorporation of booster sessions within the stepped-care model to bolster long-term maintenance of gains. Preventative consideration will also be given to opportunities for embedding Stepped-Care I-InTERACT-North within existing programs for medically or developmentally complex children who are at higher risk for mental health concerns. The program is now at a critical juncture for considering its transition from research to clinical implementation with the long-term goal of sustainability within clinical care/community pathways for children and families following early brain injury and associated medical conditions. Optimizing protective parenting strategies and parent–child relationships early in routine clinical care, before issues manifest, cannot only offset potential adverse neurodevelopmental sequelae, but can also help address mental health access disparities for at-risk children and families.
Supplementary Material
Acknowledgments
The authors would like to acknowledge the support of our participants, parent advisors, and therapists. We would also like to thank the POND Network and the Neonatal Follow-Up Clinic and Neurology teams at the Hospital for Sick Children for their support.
Contributor Information
Angela Deotto, Division of Neurology, Department of Psychology, The Hospital for Sick Children, Toronto, ON, Canada; Department of Psychology, Faculty of Health, York University, Toronto, ON, Canada.
Giulia F Fabiano, Division of Neurology, Department of Psychology, The Hospital for Sick Children, Toronto, ON, Canada.
Beryl Y T Chung, Division of Neurology, Department of Psychology, The Hospital for Sick Children, Toronto, ON, Canada; Schulich School of Medicine & Dentistry, Western University, London, ON, Canada.
Shari L Wade, Division of Physical Medicine and Rehabilitation, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA; Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH, USA.
Evdokia Anagnostou, Department of Pediatrics, Faculty of Medicine, University of Toronto, Toronto, ON, Canada; Bloorview Research Institute, Holland Bloorview Kids Rehabilitation Hospital, Toronto, ON, Canada.
Jennifer Crosbie, Department of Psychiatry, The Hospital for Sick Children Toronto, ON, Canada; Department of Psychiatry, University of Toronto, Toronto, Canada.
Elizabeth Kelley, Department of Psychology, Queens University, Kingston, ON, Canada.
Rob Nicolson, Department of Psychiatry, Western University, London, ON, Canada; Lawson Health Research Institute, London Health Sciences Centre, London, ON, Canada.
Brendan F Andrade, Department of Psychiatry, University of Toronto, Toronto, Canada; Margaret and Wallace McCain Centre for Child, Youth and Family Mental Health, Centre for Addiction and Mental Health, Toronto, ON, Canada.
Steven P Miller, Faculty of Medicine, BC Children’s Hospital, Vancouver, BC, Canada; Department of Pediatrics, Faculty of Medicine, University of British Columbia, Vancouver, BC, Canada.
Tricia S Williams, Division of Neurology, Department of Psychology, The Hospital for Sick Children, Toronto, ON, Canada; Department of Psychology, Faculty of Health, York University, Toronto, ON, Canada; Department of Psychiatry, University of Toronto, Toronto, Canada.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Author Contributions
Angela Deotto (Conceptualization [lead], Data curation [supporting], Formal analysis [lead], Investigation [lead], Methodology [lead], Visualization [lead], Writing—original draft [lead], Writing—review & editing [lead]), Giulia Fabiano (Formal analysis [equal], Project administration [lead], Validation [equal], Visualization [equal], Writing—original draft [equal], Writing—review & editing [equal]), Beryl Chung (Data curation [equal], Funding acquisition [supporting], Project administration [equal], Supervision [equal], Visualization [equal]), Shari L. Wade (Conceptualization [equal], Funding acquisition [equal], Resources [equal], Supervision [equal], Writing—review & editing [equal]), Evdokia Anagnostou (Funding acquisition [equal], Resources [equal], Supervision [equal], Writing—review & editing [equal]), Jennifer Crosbie (Resources [equal], Writing—review & editing [equal]), Elizabeth Kelley (Methodology [equal], Resources [equal], Writing—review & editing [equal]), Rob Nicolson (Investigation [equal], Methodology [equal], Writing—review & editing [equal]), Brendan Andrade (Methodology [equal], Supervision [equal], Writing—review & editing [equal]), Steven Miller (Conceptualization [equal], Funding acquisition [equal], Resources [equal], Writing—review & editing [equal]), and Tricia Williams (Conceptualization [equal], Data curation [equal], Formal analysis [equal], Funding acquisition [lead], Investigation [equal], Methodology [equal], Resources [lead], Software [lead], Supervision [lead], Writing—original draft [equal], Writing—review & editing [equal])
Funding
This work was supported by a Canadian Institutes of Health Research (CIHR) Operating Grant [FRN: 178854] and a combined COVID-19 Grant from the Garry Hurvitz-Centre for Brain and Mental Health and Edwin S.H. Leong Centre for Healthy Children.
Conflicts of interest
The authors have no conflicts of interest to declare.
Data Availability
Data are available on request.
References
- Antonini T. N., Raj S. P., Oberjohn K. S., Cassedy A., Makoroff K. L., Fouladi M., Wade S. L. (2014). A pilot randomized trial of an online parenting skills program for pediatric traumatic brain injury: improvements in parenting and child behavior. Behavior Therapy, 45(4), 455–468. 10.1016/j.beth.2014.02.003 [DOI] [PubMed] [Google Scholar]
- Antony M. M., Bieling P. J., Cox B. J., Enns M. W., Swinson R. P. (1998). Psychometric properties of the 42-item and the 21-item version of the DASS in clinical groups and a community sample. Psychological Assessment, 10(2), 176–181. 10.1037/1040-3590.10.2.176 [DOI] [Google Scholar]
- Bentenuto A., Mazzoni N., Giannotti M., Venuti P., de Falco S. (2021). Psychological impact of Covid-19 pandemic in Italian families of children with neurodevelopmental disorders. Research in Developmental Disabilities, 109, 103840. 10.1016/j.ridd.2020.103840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower P., Gilbody S. (2005). Stepped care in psychological therapies: access, effectiveness and efficiency. Narrative literature review. The British Journal of Psychiatry, 186, 11–17. 10.1192/bjp.186.1.11 [DOI] [PubMed] [Google Scholar]
- Braun V., Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. [Google Scholar]
- Burek B., Ford M. K., Hooper M., Green R., Kohut S. A., Andrade B. F., Ravi M., Sananes R., Desrocher M., Miller S. P., Wade S. L., Williams T. S. (2021). Transdiagnostic feasibility trial of internet-based parenting intervention to reduce child behavioural difficulties associated with congenital and neonatal neurodevelopmental risk: introducing I-InTERACT-North. The Clinical Neuropsychologist, 35(5), 1030–1052. 10.1080/13854046.2020.1829071 [DOI] [PubMed] [Google Scholar]
- Campbell L. A., Clark S. E., Ayn C., Chorney J., Emberly D., MacDonald J., MacKenzie A., Marsh D., Peacock K., Wozney L. (2019). The choice and partnership approach to community mental health and addictions services: a realist-informed scoping review protocol. BMJ Open, 9(12), e033247. 10.1136/bmjopen-2019-033247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark S., Emberly D., Pajer K., Delong E., McWilliam S., Bagnell A., Abidi S., Cassey B., Gardner W. (2018). Improving access to child and adolescent mental health care: the choice and partnership approach. The Journal of the Canadian Academy of Child and Adolescent Psychiatry, 27(1), 5–14. [PMC free article] [PubMed] [Google Scholar]
- Colvin M. K. M., Reesman J., Glen T. (2022). The impact of COVID-19 related educational disruption on children and adolescents: an interim data summary and commentary on ten considerations for neuropsychological practice. The Clinical Neuropsychologist, 36(1), 45–71. 10.1080/13854046.2021.1970230 [DOI] [PubMed] [Google Scholar]
- Cost K. T., Crosbie J., Anagnostou E., Birken C. S., Charach A., Monga S., Kelley E., Nicolson R., Maguire J. L., Burton C. L., Schachar R. J., Arnold P. D., Korczak D. J. (2022). Mostly worse, occasionally better: impact of COVID-19 pandemic on the mental health of Canadian children and adolescents. European Child & Adolescent Psychiatry, 31(4), 671–684. 10.1007/s00787-021-01744-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross S. P., Hickie I. (2017). Transdiagnostic stepped care in mental health. Public Health Research & Practice, 27(2), 1–5. 10.17061/phrp2721712 [DOI] [PubMed] [Google Scholar]
- Donders J., Hunter S. (Eds.) (2018). Neuropsychological conditions across the lifespan. Cambridge University Press. 10.1017/9781316996751 [DOI] [Google Scholar]
- Eyberg S. (1988). Parent-child interaction therapy: Integration of traditional and behavioral concerns. Child & Family Behavior Therapy, 10(1), 33–46. ( [Google Scholar]
- Eyberg S. M.Nelson M. M., Duke M., & Boggs S. R. (2004). Manual for the dyadic parent–child interaction coding system, third edition. Unpublished Rating Manual.
- Eyberg S. M., Pincus D. (1999). Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory–Revised: Professional manual. Psychological Assessment Resources. [Google Scholar]
- Flanagin A., Frey T., Christiansen S. L.; AMA Manual of Style Committee. (2021). Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA, 326(7), 621–627. 10.1001/jama.2021.13304 [DOI] [PubMed] [Google Scholar]
- Ford M. K., Roberts S. D., Andrade B. F., Desrocher M., Wade S. L., Kohut S. A., Williams T. S. (2023). Building I-INTERACT-North: participatory Action Research design of an online transdiagnostic parent-child interaction therapy program to optimize congenital and neurodevelopmental risk. Journal of Clinical Psychology in Medical Settings, 30(1), 204–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuentes A., Deotto A., Desrocher M., deVeber G., Westmacott R. (2016). Determinants of cognitive outcomes of perinatal and childhood stroke: A review. Child Neuropsychology, 22(1), 1–38. 10.1080/09297049.2014.969694 [DOI] [PubMed] [Google Scholar]
- Funderburk B. W., Eyberg S. M., Rich B. A., Behar L. (2003). Further psychometric evaluation of the Eyberg and Behar rating scales for parents and teachers of preschoolers. Early Education and Development, 14(1), 67–82. 10.1207/s15566935eed1401_5 [DOI] [Google Scholar]
- Hayes B. C., Doherty E., Grehan A., Madigan C., McGarvey C., Mulvany S., Matthews T. G., King M. D. (2018). Neurodevelopmental outcome in survivors of hypoxic ischemic encephalopathy without cerebral palsy. European Journal of Pediatrics, 177(1), 19–32. 10.1007/s00431-017-3028-3 [DOI] [PubMed] [Google Scholar]
- Hertzog M. A. (2008). Considerations in determining sample size for pilot studies. Research in Nursing & Health, 31(2), 180–191. 10.1002/nur.20247 [DOI] [PubMed] [Google Scholar]
- Holmes E. A., O'Connor R. C., Perry V. H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A. K., Shafran R., Sweeney A., Bullmore E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. 10.1016/s2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones K., Daley D., Hutchings J., Bywater T., Eames C. (2008). Efficacy of the incredible years programme as an early intervention for children with conduct problems and ADHD: long-term follow-up. Child: Care, Health and Development, 34(3), 380–390. 10.1111/j.1365-2214.2008.00817.x [DOI] [PubMed] [Google Scholar]
- Kennedy S. M., Lanier H., Salloum A., Ehrenreich-May J., Storch E. A. (2021). Development and implementation of a transdiagnostic, stepped-care approach to treating emotional disorders in children via telehealth. Cognitive and Behavioral Practice, 28(3), 350–363. 10.1016/j.cbpra.2020.06.001 [DOI] [Google Scholar]
- Khan S., VanWynsberghe R. (2008). Cultivating the under-mined: Cross-case analysis as knowledge mobilization. Qualitative Social Research, 9(1), 1–26. [Google Scholar]
- Lal S., Adair C. E. (2014). E-mental health: a rapid review of the literature. Psychiatric Services (Washington, D.C.), 65(1), 24–32. 10.1176/appi.ps.201300009 [DOI] [PubMed] [Google Scholar]
- Carter Leno V., Forth G., Chandler S., White P., Yorke I., Charman T., Pickles A., Simonoff E. (2021). Behavioural and physiological response to frustration in autistic youth: Associations with irritability. Journal of Neurodevelopmental Disorders, 13(1), 1–11. 10.1186/s11689-021-09374-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieneman C. C., Brabson L. A., Highlander A., Wallace N. M., McNeil C. B. (2017). Parent–child interaction therapy: current perspectives. Psychology Research and Behavior Management, 10, 239–256. 10.2147/PRBM.S91200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond P. F., Lovibond S. H. (1995). The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. 10.1016/0005-7967(94)00075-u [DOI] [PubMed] [Google Scholar]
- Lovibond S. H., Lovibond P. F. (1996). Manual for the depression anxiety stress scales. Psychology Foundation of Australia. [Google Scholar]
- McKevitt C., Topor M., Panton A., Mallick A. A., Ganesan V., Wraige E., Gordon A. (2019). Seeking normality: parents’ experiences of childhood stroke. Child: Care, Health and Development, 45(1), 89–95. 10.1111/cch.12622 [DOI] [PubMed] [Google Scholar]
- Miles M. B., Huberman M. A. (1994). Qualitative data analysis: an expanded sourcebook (2nd edn). Sage Publications. [Google Scholar]
- Narad M. E., Moscato E., Yeates K. O., Taylor H. G., Stancin T., Wade S. L. (2019). Behavioral health service utilization and unmet need after traumatic brain injury in childhood. Journal of Developmental and Behavioral Pediatrics: JDBP, 40(6), 451–457. 10.1097/DBP.0000000000000681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nonweiler J., Rattray F., Baulcomb J., Happe F., Absoud M. (2020). Prevalence and associated factors of emotional and behavioural difficulties during COVID-19 pandemic in children with neurodevelopmental disorders. Children, 7(9), 128. 10.3390/children7090128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton P. J. (2007). Depression Anxiety and Stress Scales (DASS-21): psychometric analysis across four racial groups. Anxiety, Stress, and Coping, 20(3), 253–265. [DOI] [PubMed] [Google Scholar]
- Panter‐Brick C., Burgess A., Eggerman M., McAllister F., Pruett K., Leckman J. F. (2014). Practitioner review: engaging fathers—recommendations for a game change in parenting interventions based on a systematic review of the global evidence. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 55(11), 1187–1212. 10.1111/jcpp.12280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N., Cooke J. E., Eirich R., Korczak D. J., McArthur B., Madigan S. (2020). Child and adolescent mental illness during COVID-19: a rapid review. Psychiatry Research, 292, 113307. 10.1016/j.psychres.2020.113307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramtekkar U. P., Reiersen A. M., Todorov A. A., Todd R. D. (2010). Sex and age differences in attention-deficit/hyperactivity disorder symptoms and diagnoses: implications for DSM-V and ICD-11. Journal of the American Academy of Child & Adolescent Psychiatry, 49(3), 217–228.e3. 10.1016/j.jaac.2009.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransom D. M., Caldwell C. T., DiVirgilio E. K., McNally K. A., Peterson R. L., Ploetz D. M., Sady M. D., Slomine B. S. (2022). Pediatric mTBI during the COVID-19 pandemic: considerations for evaluation and management. Child Neuropsychology, 28(3), 355–373. 10.1080/09297049.2021.1985101 [DOI] [PubMed] [Google Scholar]
- Robinson E. A., Eyberg S. M. (1981). The dyadic parent–child interaction coding system: standardization and validation. Journal of Consulting and Clinical Psychology, 49(2), 245–250. [DOI] [PubMed] [Google Scholar]
- Schorr E., Wade S. L., Taylor H. G., Stancin T., Yeates K. O. (2020). Parenting styles as a predictor of long-term psychosocial outcomes after traumatic brain injury (TBI) in early childhood. Disability and Rehabilitation, 42(17), 2437–2443. 10.1080/09638288.2019.1602676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz K. D., Exner-Cortens D., McMorris C. A., Makarenko E., Arnold P., Van Bavel M., Williams S., Canfield R. (2021). COVID-19 and student well-being: stress and mental health during return-to-school. Canadian Journal of School Psychology, 36(2), 166–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shephard E., Bedford R., Milosavljevic B., Gliga T., Jones E. J. H., Pickles A., Johnson M. H., Charman T.; BASIS Team (2019). Early developmental pathways to childhood symptoms of attention‐deficit hyperactivity disorder, anxiety and autism spectrum disorder. Journal of Child Psychology and Psychiatry, 60(9), 963–974. 10.1111/jcpp.12947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soufi S., Chabrier S., Bertoletti L., Laporte S., Darteyre S. (2017). Lived experience of having a child with stroke: a qualitative study. European Journal of Paediatric Neurology, 21(3), 542–548. 10.1016/j.ejpn.2017.01.007 [DOI] [PubMed] [Google Scholar]
- Spittle A. J., Treyvaud K., Doyle L. W., Roberts G., Lee K. J., Inder T. E., Cheong J. L. Y., Hunt R. W., Newnham C. A., Anderson P. J. (2009). Early emergence of behavior and social-emotional problems in very preterm infants. Journal of the American Academy of Child and Adolescent Psychiatry, 48(9), 909–918. 10.1097/CHI.0b013e3181af8235 [DOI] [PubMed] [Google Scholar]
- Stark A. M., White A. E., Rotter N. S., Basu A. (2020). Shifting from survival to supporting resilience in children and families in the COVID-19 pandemic: lessons for informing U.S. mental health priorities. Psychological Trauma, 12(S1), S133–S135. 10.1037/tra0000781 [DOI] [PubMed] [Google Scholar]
- Statistics Canada (2021, April 1). Ethnic origin of person. Standards, Data Sources and Methods. https://www23.statcan.gc.ca/imdb/p3Var.pl?Function=DEC&Id=103475 Retrieved 4 June, 2021.
- Stephenson J. (2021). Children and teens struggling with mental health during COVID-19 Pandemic. JAMA Health Forum, 2(6), e211701. 10.1001/jamahealthforum.2021.1701 [DOI] [PubMed] [Google Scholar]
- Vyas S. S., Ford M. K., Tam E. W. Y., Westmacott R., Sananes R., Beck R., Williams T. S. (2021). Intervention experiences among children with congenital and neonatal conditions impacting brain development: patterns of service utilization, barriers and future directions. The Clinical Neuropsychologist, 35(5), 1009–1029. 10.1080/13854046.2020.1871516 [DOI] [PubMed] [Google Scholar]
- Wade S. L., Cassedy A., Walz N. C., Taylor H. G., Stancin T., Yeates K. O. (2011). The relationship of parental warm responsiveness and negativity to emerging behavior problems following traumatic brain injury in young children. Developmental Psychology, 47(1), 119–133. 10.1037/a0021028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade S. L., Cassedy A. E., Shultz E. L., Zang H., Zhang N., Kirkwood M. W., Stancin T., Yeates K. O., Taylor H. G. (2017). Randomized clinical trial of online parent training for behavior problems after early brain injury. Journal of the American Academy of Child and Adolescent Psychiatry, 56(11), 930–939 e932. 10.1016/j.jaac.2017.09.413 [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C. (1999). The incredible years. BASIC. The parent and children series. A comprehensive course (revised). The Incredible Years. Inc.
- Whitlock A., Fulton K., Lai M. C., Pellicano E., Mandy W. (2020). Recognition of girls on the autism spectrum by primary school educators: an experimental study. Autism Research, 13(8), 1358–1372. 10.1002/aur.2316 [DOI] [PubMed] [Google Scholar]
- Wiggins T. L., Sofronoff K., Sanders M. R. (2009). Pathways triple P-positive parenting program effects on parent-child relationships and child behavior problems. Family Process, 48(4), 517–530. 10.1111/j.1545-5300.2009.01299.x [DOI] [PubMed] [Google Scholar]
- Williams T. S., Burek B., Deotto A., Ford M. K., Green R., Wade S. L. (2022). Pandemic perils and promise: implementation of a hospital-based virtual parenting intervention during COVID-19. Developmental Neurorehabilitation, 25(8), 505–517. [DOI] [PubMed] [Google Scholar]
- Williams T. S., Deotto A., Roberts S. D., Ford M. K., Desire N., Cunningham S. (2022). COVID-19 mental health impact among children with early brain injury and associated conditions. Child Neuropsychology, 28(5), 627–648. 10.1080/09297049.2021.1998407 [DOI] [PubMed] [Google Scholar]
- Williams T. S., McDonald K. P., Roberts S. D., Westmacott R., Ahola Kohut S., Dlamini N., Miller S. P. (2018). In their own words: developing the parent experiences questionnaire following neonatal brain injury using participatory design. Brain Injury, 32(11), 1386–1396. 10.1080/02699052.2018.1495844 [DOI] [PubMed] [Google Scholar]
- Young S., Adamo N., Ásgeirsdóttir B. B., Branney P., Beckett M., Colley W., Cubbin S., Deeley Q., Farrag E., Gudjonsson G., Hill P., Hollingdale J., Kilic O., Lloyd T., Mason P., Paliokosta E., Perecherla S., Sedgwick J., Skirrow C., Woodhouse E. (2020). Females with ADHD: an expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/hyperactivity disorder in girls and women. BMC Psychiatry, 20(1), 1–27. 10.1186/s12888-020-02707-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Shuai L., Yu H., Wang Z., Qiu M., Lu L., Cao X., Xia W., Wang Y., Chen R. (2020). Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian Journal of Psychiatry, 51, 102077. 10.1016/j.ajp.2020.102077 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available on request.